预约演示
更新于:2025-05-07

A. Menarini Industrie Farmaceutiche Riunite Srl
更新于:2025-05-07
概览
标签
其他疾病
肿瘤
神经系统疾病
小分子化药
ADC
治疗性疫苗
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 32 |
| 树突状细胞疫苗 | 1 |
| 融合蛋白 | 1 |
| 治疗性疫苗 | 1 |
| 合成多肽 | 1 |
关联
91
项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的药物靶点 |
作用机制 ERα拮抗剂 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2023-01-27 |
靶点 |
作用机制 CD123抑制剂 |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2018-12-21 |
作用机制 PBPs抑制剂 [+1] |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2017-08-29 |
157
项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的临床试验NCT06923527
A Single Arm Phase II Trial of Circulating Tumor DNA-guided Adjuvant Therapy With Elacestrant in Hormone Receptor Positive HER2 Negative Breast Cancers at Risk for Late Recurrence (CATE)
This is a single-arm, phase II study examining elacestrant in the adjuvant treatment of patients with ER+ breast cancer who test positive for circulating tumor DNA (ctDNA) during the screening period of the trial.
开始日期2025-04-01 |
申办/合作机构  Yale University Yale University [+2] |
NCT06828848
An Open-label, Multicentre, Single-Arm Study to Evaluate the Safety, Tolerability, and Pharmacokinetics of VaboremⓇ (Meropenem-Vaborbactam) in Paediatric Population With Complicated Urinary Tract Infections, Including Acute Pyelonephritis
The goal of this clinical trial is to assess the pharmacokinetic (PK) and safety and tolerability of Vaborem ( fixed combination of meropenem and vaborbactam) in the paediatric population aged from 3 months to < 18 years with complicated urinary tract infection (cUTI) including acute pyelonephritis (AP) in need of hospitalisation and intravenous (IV) antibiotic administration.
All participants will receive Vaborem IV every 8 hours to treat cUTI and/or AP for 10 up to 14 days; switch to stepdown oral antibiotic is allowed after a minimum of 3 days of Vaborem. PK sample collection will occur after at least 6 doses administration.
Participant's clinical conditions will be monitored during the entire duration of their hospitalization and during scheduled visit/s after the completion of the treatment.
All participants will receive Vaborem IV every 8 hours to treat cUTI and/or AP for 10 up to 14 days; switch to stepdown oral antibiotic is allowed after a minimum of 3 days of Vaborem. PK sample collection will occur after at least 6 doses administration.
Participant's clinical conditions will be monitored during the entire duration of their hospitalization and during scheduled visit/s after the completion of the treatment.
开始日期2025-02-18 |
NCT06561152
Tagraxofusp and Low-Intensity Chemotherapy for the Treatment of CD123-Positive Relapsed or Refractory Acute Myeloid Leukemia (AML)
To determine the efficacy of the combination of tagraxofusp, cladribine, and cytarabine.
开始日期2025-02-10 |
申办/合作机构  Stanford University Stanford University [+1] |
100 项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的临床结果
登录后查看更多信息
0 项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的专利(医药)
登录后查看更多信息
419
项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的文献(医药)2025-04-25·Cancer Research
Abstract CT236: ELCIN: Elacestrant (Ela) in women and men with CDK4/6 inhibitor (CDK4/6i)- naive estrogen receptor- positive (ER+), HER2-negative (HER2-) metastatic breast cancer (mBC): An open-label multicenter phase 2 study
作者: Thummala, Anu R. ; Kaklamani, Virginia ; Gambioli, Angela ; Wasserman, Tomer ; Gradishar, William J. ; Theall, Kathy Puyana ; Sendur, Mehmet Ali ; Barrios, Carlos ; Santi, Patricia ; Dzagnidze, Giorgi ; Antone, Nicoleta Zenovia ; Zhang, Xiaoling ; Janjalia, Mikheil ; Dominguez, Manuel
2025-04-25·Cancer Research
Abstract CT255: ELEGANT: Elacestrant versus standard endocrine therapy (ET) in women and men with node-positive, estrogen receptor-positive (ER+), HER2-negative (HER2-), early breast cancer (eBC) with high risk of recurrence in a global, multicenter, randomized, open-label phase 3 study
作者: Wasserman, Tomer ; Bardia, Aditya ; Ignatiadis, Michail ; Beck, J. Thaddeus ; Barcenas, Carlos H. ; Schmid, Peter ; Nicacio, Leo Viana ; Tonini, Giulia ; Crozier, Jennifer ; Gradishar, William J. ; Scartoni, Simona ; Rugo, Hope S. ; Kaklamani, Virginia ; O’Shaughnessy, Joyce ; Tolaney, Sara M. ; De Laurentiis, Michelino ; Cameron, David A. ; Curigliano, Giuseppe
2025-04-25·Cancer Research
Abstract CT246: Tagraxofusp plus venetoclax and azacitidine in patients ineligible for intensive chemotherapy with previously untreated CD123+ acute myeloid leukemia: A phase 2 multicenter trial
作者: Lane, Andrew A. ; Tosolini, Alessandra ; Fathi, Amir ; Sekeres, Mikkael A. ; Gupta, Ira ; Kantarjian, Hagop M. ; Daver, Naval G. ; Garzon, Jessica ; Compagnoni, Anna ; Pemmaraju, Naveen
499
项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的新闻(医药)2025-04-30
Ad hoc announcement pursuant to Art. 53 LR Allschwil, Switzerland – April 30, 2025Idorsia Ltd (SIX: IDIA) today announced its financial results for the first quarter of 2025. Business highlights Q1 2025 QUVIVIQ™ (daridorexant): Strong performance and accelerating sales in Q1 2025 with total Idorsia-led net sales of CHF 25 m.QUVIVIQ EUCAN: Demand grew by 50% from Q4 2024 to Q1 2025, strongly driven by reimbursed markets. Overall, more than 10 million nights of sleep prescribed in Q1 2025.Daridorexant: Positive data with daridorexant in patients with chronic insomnia and nocturia published in the Journal of Sleep Research and assessing the transition from night to day published in Sleep Medicine.TRYVIO™ (aprocitentan): REMS requirement removed by US FDA.Aprocitentan: Effect of reducing blood pressure and proteinuria in Black patients with resistant hypertension published in HypertensionRestructured convertible bond debt: Tailored approach to remove large debt overhang.New funding: Bondholders to provide CHF 150 m new money facility.Viatris collaboration: Updated agreement removed significant cash requirement for 2025. Financial highlights Net revenue Q1 2025 of CHF 59 m.US GAAP operating expenses Q1 2025 of CHF 5 m (income) were positively impacted by a one-off gain from the amendment of the Viatris deal with non-GAAP operating expenses Q1 2025 of CHF 78 m.US GAAP operating income Q1 2025 of CHF 67 m and non-GAAP operating loss of CHF 17 m. Guidance for 2025 – unforeseen events excluded QUVIVIQ net sales of around CHF 110 m.SG&A expenses of around CHF 210 m, R&D expenses of around CHF 100 m, leading to non-GAAP operating expenses of around CHF 325 m.US GAAP loss for global business of around CHF 125 m. André C. Muller, Chief Executive Officer of Idorsia, commented:“Beyond the transformation of Idorsia’s financial situation, we made significant progress on multiple fronts in the first quarter. QUVIVIQ is taking off in Europe with a particularly impressive performance in France following the commercial partnership to call on GPs initiated in October 2024; we hope Germany will follow suit, as a similar partnership will kick-in from April 2025. In the US, we have implemented a focused commercialization approach for QUVIVIQ to maintain sales until the potential descheduling of the dual orexin receptor antagonist (DORA) class can be achieved. We received great news from the FDA, with the removal of the REMS requirement for TRYVIO allowing a shift toward broad product availability in retail pharmacies. This, together with the early positive prescribing experience in leading US hypertension centers of excellence gives us confidence of the potential of our antihypertensive drug. Lastly, we streamlined the R&D organization to invest in our promising refocused pipeline. All these achievements put us on a solid path to reach our 2025 goals.” Financial results US GAAP results First Quarterin CHF millions, except EPS (CHF) and number of shares (millions) 20252024Net revenue 5910Operating expenses 520Operating income 6731Net income 6330Basic EPS 0.330.17Basic weighted average number of shares 188.9179.1Diluted EPS 0.230.13Diluted weighted average number of shares 270.8233.3 Net revenue of CHF 59 m in Q1 2025 resulted from QUVIVIQ product sales (CHF 25 m), product sales to partners (CHF 1 m), and contract revenues (CHF 32 m), comprising a one-off exclusivity fee of CHF 32 m paid by an undisclosed party in relation to a potential aprocitentan deal, and non-cash revenue related to the R-Bridge royalty monetization agreement of CHF 1 m. This compares to net revenue of CHF 10 m in Q1 2024 from QUVIVIQ product sales. US GAAP operating expenses of CHF 5 m (income) in Q1 2025 and CHF 20 m (income) in Q1 2024 were impacted by a one-off gain of CHF 90 m (Viatris deal amendment) in 2025 and CHF 125 m (Viatris deal) in 2024, respectively. Excluding these one-off gains, US GAAP operating expenses at Q1 2025 decreased by CHF 20 m, mainly driven by R&D expenses of CHF 27 m decreasing by CHF 6 m compared to Q1 2024 (CHF 33 m), and SG&A expenses of CHF 54 m decreasing by CHF 14 m compared to Q1 2024 (CHF 68 m). US GAAP net income in Q1 2025 of CHF 63 m (CHF 27 m net loss excluding Viatris deal amendment) and CHF 30 m in Q1 2024 (CHF 95 m net loss excluding Viatris deal). Excluding these one-offs, the reduced net loss in Q1 2025 was primarily due to lower operating expenses from cost savings through the effective restructuring efforts announced in November 2024 and higher revenue. The US GAAP net income resulted in a basic net income per share of CHF 0.33 (diluted net income per share of CHF 0.23) in Q1 2025, compared to a basic net income per share of CHF 0.17 (diluted net income per share of CHF 0.13) in Q1 2024. Non-GAAP* measures First Quarterin CHF millions, except EPS (CHF) and number of shares (millions) 20252024Net revenue 5810Operating expenses (78)(96)Operating loss (17)(85)Net loss (25)(86)Basic and diluted EPS (0.13)(0.48)Basic and diluted weighted average number of shares 188.9179.1 * Idorsia measures, reports, and issues guidance on non-GAAP operating performance. Idorsia believes that these non-GAAP financial measurements more accurately reflect the underlying business performance and therefore provide useful supplementary information to investors. These non-GAAP measures are reported in addition to, not as a substitute for, US GAAP financial performance. Non-GAAP net loss in Q1 2025 amounted to CHF 25 m; the difference versus US GAAP net income was mainly driven by the one-off gain from the amendment of the Viatris Deal (CHF 90 m). The non-GAAP net loss resulted in a net loss per share of CHF 0.13 (basic and diluted) in Q1 2025, compared to a net loss per share of CHF 0.48 (basic and diluted) in Q1 2024. Viatris collaborationIn March 2024, Idorsia entered into a global research and development collaboration with Viatris, for the global development and commercialization rights to selatogrel and cenerimod. Idorsia received an upfront payment of USD 350 million (CHF 308 million) with Idorsia obligated to contribute USD 200 million for the development of selatogrel and cenerimod. Idorsia is entitled to potential development and regulatory milestone payments, and certain contingent payments of additional sales milestone payments and tiered royalties in the mid-single to low-double digit percentages on annual net sales. In February 2025, Idorsia reached an agreement with Viatris to update the terms of the collaboration. In exchange for a USD 100 million reduction to Idorsia’s contribution to the development costs due in 2025, Idorsia has agreed to a USD 250 million reduction in future potential regulatory and sales milestone payments, and an expansion of territorial rights to Viatris for cenerimod. The agreed royalties on future sales remain unchanged. Under the updated terms, Idorsia's contribution for the development of selatogrel and cenerimod is reduced to USD 100 million with no commitment in 2025. Idorsia has contributed USD 73 million in 2024 for the performance of development services, and the remaining USD 27 million will be paid in 2026. Restructured convertible bond debt and new funding securedOn February 26, 2025, Idorsia announced that it has reached an agreement with more than two-thirds of the holders of its outstanding convertible bond debt on the main terms of a holistic restructuring of the bonds and a CHF 150 million new money facility, to alleviate the short- to mid-term debt overhang of CHF 800 million while retaining upside potential of key assets beyond the value of the debt. As part of the holistic restructuring Idorsia will issue up to 27.5 million shares and up to 25.5 million warrants. When complete, the tailored solution secures future operations of Idorsia into 2026. More information can be found in the dedicated press release. Capital increaseIn connection with the holistic restructuring of the convertible bond debt and raising of additional funds, 35 million registered shares with a nominal value of CHF 0.05 each were created out of capital band and were listed on March 4, 2025. Financial guidance for 2025As previously announced, for the Idorsia-led portfolio in 2025, the company expects a continued acceleration of QUVIVIQ with net sales of around CHF 110 million, COGS of around CHF 15 million, SG&A expenses of around CHF 210 million, and R&D expense of around CHF 100 million, leading to non-GAAP operating expenses of around CHF 325 million. This performance would result in an Idorsia-led business non-GAAP operating loss of around CHF 215 million and US-GAAP operating loss of around CHF 260 million. The company expects US-GAAP EBIT for the partnered business of around CHF 135 million – updated to reflect the positive impact of the one-off exclusivity fee paid by an undisclosed party in Q4 2024 but recognized in Q1 2025 – and mainly driven by the amended deal with Viatris. This would result in a US-GAAP loss for the global business of around CHF 125 million. All amounts exclude unforeseen events and potential revenue related to additional business development activities. Arno Groenewoud, Chief Financial Officer, commented:“The updated agreement with Viatris, and the convertible debt restructuring, together with the new money facility agreed with our bondholders, has significantly changed the financial situation of Idorsia. That said, there are still several steps to implement in order to realize what was agreed. The restructuring of the bonds is moving forward with the first step approved by the court, allowing us to proceed to the next bondholder meetings. We are also making progress with putting the new money facility in place. The excellent uplift with QUVIVIQ in Europe and the tight cost-control means we are well on track with our financial performance targets.” Liquidity and indebtednessAt the end of the first quarter of 2025, Idorsia’s liquidity amounted to CHF 51 million. (in CHF millions) Mar 31, 2025Dec 31, 2024Liquidity Cash and cash equivalents 51106Total liquidity* 51106 Indebtedness Convertible loan 335335Convertible bond 797797Other financial debt 190189Total indebtedness 1,3221,321 *rounding differences may occur Commercial operationsIn the first quarter of 2025, QUVIVIQ™ (daridorexant) in the US, Germany, Italy, Switzerland, Spain, UK, Canada, Austria, France, and Sweden generated total product sales of CHF 25 million. Europe and Canada ProductMechanism of actionIndicationCommercially availableDual orexin receptor antagonistTreatment of adult patients with insomnia characterised by symptoms present for at least three months and considerable impact on daytime functioningSweden: Sept. 2024France: Mar. 2024Austria: Feb. 2024UK: Oct. 2023Spain: Sept. 2023Switzerland: Jun. 2023Germany: Nov. 2022Italy: Nov. 2022 Management of adult patients with insomnia, characterized by difficulties with sleep onset and/or sleep maintenanceCanada: Nov. 2023 QUVIVIQ (daridorexant) net sales in the first quarter of 2025 reached CHF 19.4 million in the Europe and Canada (EUCAN) region, a significant increase from CHF 3.5 million in the first quarter of 2024. In France, QUVIVIQ is reimbursed for moderate and severe chronic insomnia patients after, or as an alternative to, cognitive behavioral therapy for insomnia. The outstanding launch in France is driven by a combination of co-promotion with Menarini reflected by a new-to-brand share growing from 1.1% in September 2024 to 9.3% in January 2025 in the general practitioner (GP) segment, and a strong positioning to specialists in retail and hospital settings reflected by a solid new-to-brand share evolution from 9.7% in September 2024 to 14.4% in January 2025 in the psychiatrist segment. In Germany, QUVIVIQ was launched in November 2022 and is the only sleep medication in Germany that can be prescribed for long-term treatment of chronic insomnia. The progress made in Germany is reflected by the performance of QUVIVIQ on the market, with demand increasing by 20% quarter on quarter. In February 2025, Idorsia successfully concluded negotiations for the reimbursement price in Germany. Idorsia is expanding its commercial reach from specialist prescribers to GPs through a commercial partnership with Berlin-Chemie (a wholly owned subsidiary of the Menarini Group), which started in April 2025. In the UK, QUVIVIQ is recommended as first-line pharmaceutical treatment for patients with chronic insomnia, after, or as an alternative to, cognitive behavioral therapy for insomnia (CBT-I). QUVIVIQ was launched in October 2023 at NICE approval. The priority in the UK in 2024 was to secure regional access, and the team has achieved reimbursement throughout 85% of the UK, as well as raising awareness of QUVIVIQ among general practitioners. Increased access and awareness have started to translate into strong demand in the UK which grew by 48% from Q4 2024 to Q1 2025. In Canada, after being approved in April 2023, QUVIVIQ was launched in November 2023 to the private market, representing 55% of the Canadian insomnia market. To date, 85% of private Canadian lives are covered. The focus is now on public payers; the company submitted public reimbursement dossiers and expects decisions by the end of 2025. QUVIVIQ demand in Canada grew by 25% from Q4 2024 to Q1 2025. Austria will soon become the fourth EUCAN country to grant public reimbursement to QUVIVIQ, starting from June 1, 2025. This is a significant achievement in a country that has strict reimbursement rules and underpins the value QUVIVIQ brings to patients, physicians and the healthcare system. In Italy, QUVIVIQ is now officially available for all prescribers, following its publication in the Official Gazette in mid-March 2025, this includes GPs who represent nearly 80% of the total insomnia market. In Switzerland, Spain, and Sweden, where we are still negotiating for reimbursement, launches have been very successful despite the out-of-pocket costs for patients, particularly in Switzerland where we see a strong demand. Benjamin Limal, President of Europe and Canada region, commented:“Demand has grown by an impressive 50% quarter on quarter, mainly driven by reimbursed markets. Across Europe and Canada, more than 10 million nights of sleep have been prescribed in the first quarter of 2025. Recent successes in access and pricing, notably in Austria and Germany, reinforce our confidence for continued growth moving forward. QUVIVIQ has been strongly adopted by specialists and more and more general practitioners start prescribing QUVIVIQ due to our increased efforts with recent partnerships for the GP market.” For more information about QUVIVIQ in the EU, see the Summary of Product Characteristics. For more information about QUVIVIQ in Switzerland, see the Patient Information and Information for Healthcare Professionals. For more information on the marketing authorization of QUVIVIQ in Canada, see the Product Monograph. United States ProductMechanism of actionIndicationCommercially available sinceDual orexin receptor antagonistTreatment of adult patients with insomnia, characterized by difficulties with sleep onset and/or sleep maintenanceMay 2022 QUVIVIQ® (daridorexant) net sales in the first quarter of 2025 amounted to CHF 5.9 million in the US, compared to CHF 6.5 million in the first quarter of 2024. As of the end of the first quarter of 2025, more than 180,000 patients have been treated with QUVIVIQ since launch in the US, over 600,000 prescriptions have been dispensed, and the product has been prescribed by more than 50,000 healthcare professionals. Michael Moye, President and General Manager of Idorsia US, commented:“We have implemented a streamlined, focused, and more cost-efficient commercialization approach for QUVIVIQ to maintain sales until the potential descheduling of the dual orexin receptor antagonist (DORA) class can be achieved. Our commercialization partner, Syneos Health, is fully operational and executing a highly targeted digital marketing plan supporting 20 virtual sales reps. Syneos is now also executing educational programming and market access activities in support of the virtual representatives. We are seeing early, positive prescribing results in key customer areas.” For more information about QUVIVIQ in the US, see the Full Prescribing Information (PI and Medication Guide). ProductMechanism of actionIndicationCommercially available sinceDual endothelin receptor antagonistTreatment of hypertension in combination with other antihypertensive drugs, to lower blood pressure in adult patients who are not adequately controlled on other drugsOctober 2024 On March 19, 2024, the US Food and Drug Administration (FDA) approved TRYVIO™ (aprocitentan) for the treatment of hypertension in combination with other antihypertensive drugs, to lower blood pressure in adult patients who are not adequately controlled on other drugs. Lowering blood pressure reduces the risk of fatal and non-fatal cardiovascular events, primarily strokes and myocardial infarctions. The recommended dosage of TRYVIO is 12.5 mg orally once daily, with or without food. Following the approval, the US team rapidly established the positioning, branding, websites, materials, training and educational platforms, and field sales force and MSL coverage plans. TRYVIO was made available for prescription in October 2024 via Walgreens Specialty Pharmacy. There is ongoing engagement with hypertension experts at major cardiovascular and nephrology congresses and encouraging discussions with payors. In March 2025, the US FDA fully released TRYVIO from its REMS (Risk Evaluation and Mitigation Strategy) requirement to minimize the burden on the healthcare delivery system of complying with the REMS. The US FDA has determined that a REMS is no longer necessary to ensure the benefits of TRYVIO outweigh the risk of embryo-fetal toxicity and that labeling is sufficient for conveying the safety information. As a result, a rapid transition from specialty pharmacy to a wide retail pharmacy distribution model is underway. Funding for a field sales force and promotional activities continues to be dependent on a partnership deal. Michael concluded:“Early prescribing experience in leading US hypertension centers of excellence has been very positive, with prescribers confirming that they are seeing blood pressure reductions, safety and tolerability consistent with the Phase 3 study. The REMS removal and shift toward broad product availability in retail pharmacies has profoundly improved the potential of TRYVIO to reach millions of patients struggling with their hypertension on existing medication regimens.” For more information see the Full Prescribing Information including BOXED Warning (PI and Medication Guide). Research & DevelopmentOur drug discovery engine has produced innovative drugs with the potential to transform the treatment paradigm in multiple therapeutic areas, including CNS, cardiovascular, and immunological disorders, as well as orphan diseases. The company also has a vaccine platform for the discovery and development of glycoconjugate vaccines to prevent infection. The company has focused its drug discovery efforts, reducing the number of active projects in research and development and preparing some for out-licensing. The prioritization has resulted in a portfolio of assets where Idorsia intends to develop to the next inflection point before partnering, or when feasible and appropriate, developing further ourselves. The company expects new lucerastat data from a kidney biopsy sub-study (to the ongoing Phase 3 open-label extension study) in the second quarter of 2025, with further discussions on the regulatory pathway to follow. The results from a Phase 1 study of our Clostridium difficile infection vaccine are also expected in the coming months. The company will need to further prioritize activities in order to reduce costs and the decisions on which assets to advance will be taken based on the data when available and the results of ongoing out-licensing discussions for early-stage assets. In March 2025, “A randomized cross-over trial of daridorexant for the treatment of chronic insomnia and nocturia” was published in the Journal of Sleep Research. The new data provides evidence of the benefit of daridorexant, at a daily dose of 50 mg, in patients aged >=55 years with chronic insomnia and comorbid nocturia, with efficacy data on symptoms of both conditions, improvement in daytime functioning, and a good safety and tolerability profile. In April 2025, the “Effect of daridorexant on nighttime wakefulness and next-morning sleepiness: assessing the transition from night to day in insomnia disorder” was published in Sleep Medicine. The analysis of the Phase 3 data provides evidence that daridorexant reduces wakefulness throughout the entire night, while decreasing morning sleepiness and improving daytime functioning and alertness in patients with chronic insomnia disorder. Idorsia-led portfolioThe company will develop each asset to the next inflection point or seek a partner. CompoundMechanism of actionTarget indicationStatusQUVIVIQ™ (daridorexant)Dual orexin receptor antagonistInsomniaCommercialized by Idorsia in the US, Germany, Italy, Switzerland, Spain, the UK, Canada, Austria, France, and Sweden; approved throughout the EU.LucerastatGlucosylceramide synthase inhibitorFabry diseasePhase 3 open-label extension study ongoing – kidney biopsy sub-study results expected in Q2 2025 – regulatory pathway to be further discussed with FDA.DaridorexantDual orexin receptor antagonistPediatric insomniaPhase 2 in pediatric insomnia is ongoing.ACT-777991CXCR3 receptor antagonistVitiligoProof-of-concept study in preparation for patients with vitiligo. Unique precision medicine with a dual targeting of CD8+ CXCR3+ T cells offers potential for a first-in-class targeted systemic therapy for effective and safer treatment of immuno-dermatology and autoimmune disorders.ACT-1004-1239ACKR3 (CXCR7) receptor antagonistProgressive multiple sclerosis Proof-of-concept study in preparation for patients with progressive MS. Unique combination of re-myelination and anti-inflammatory effect with decreased inflammatory cell infiltration.IDOR-1117-2520CCR6 receptor antagonistPsoriasisProof-of-concept study in preparation for patients with psoriasis. Unique potential as a first-in-class, oral, targeted systemic therapy for effective treatment of Th17-driven immuno-dermatology and autoimmune disorders.ACT-1016-0707LPA 1 receptor antagonistImmune-mediated and fibrosis related disordersEntry-into-human package complete. Potential best-in-class due to insurmountable binding mode – proven inhibitory activity in preclinical models of inflammation and fibrosis.IDOR-1134-9712CFTR Type-IV correctorCystic FibrosisEntry-into-human package in progress. A unique corrector targeting an Idorsia-identified binding site on the Cystic Fibrosis Transmembrane regulator (CFTR) protein. Potential synergy with other molecules.IDOR-1141-8472Orexin 2 receptor agonistOrexin-related CNS disordersEntry-into-human package ready to begin. Potential best-in-class – sustained chronic efficacy in a preclinical model of narcolepsy.IDOR-1126-6421Undisclosed mechanismOrgan injury / fibrosisEntry-into-human package in progress. Broad potential of undisclosed mechanism for inhibiting organ injury and fibrosis – proven effectiveness in several preclinical models of organ injury. Synthetic Glycan Vaccine PlatformIdorsia will seek a partner for the platform or individual vaccines.IDOR-1134-2831Synthetic glycan vaccineClostridium difficile infectionIdorsia is conducting a Phase 1 clinical pharmacology study which will test the immune response of the vaccine and evaluate its safety and tolerability. Results expected in Q2 2025.IDOR-1142-0810Synthetic glycan vaccineKlebsiella pneumonia infection Entry-into-human package in progress. Further details including the current status of each project in our portfolio can be found in our innovation fact sheet.Idorsia partner-led portfolioFor Idorsia, partnerships are a way of gaining strategic access to technologies or products and fully exploiting our discovery engine and clinical pipeline. We seek suitable external project partners to maximize the value of internal innovation. On March 19, 2024, the US Food and Drug Administration (FDA) approved TRYVIO™ (aprocitentan) for the treatment of hypertension in combination with other antihypertensive drugs, to lower blood pressure in adult patients who are not adequately controlled on other drugs. See the commercial operations section above. On June 27, 2024, the European Commission (EC) approved JERAYGO™ (aprocitentan) for the treatment of resistant hypertension in adult patients in combination with at least three antihypertensive medicinal products. The recommended dose is 12.5 mg orally once daily. The dose can be increased to 25 mg once daily for patients tolerating the 12.5 mg dose and in need of tighter blood pressure (BP) control. For more information about JERAYGO in the EU, see the Summary of Product Characteristics. Aprocitentan is an innovative and highly differentiated drug, commercially available in the US and approved in Europe and UK for the millions of patients who are unable to bring their hypertension under control with existing medications. As the first drug to target the endothelin pathway in systemic hypertension, aprocitentan has blockbuster potential in uncontrolled hypertension, particularly for difficult to treat patients with chronic kidney disease and hypertension, and further potential beyond hypertension. The priority remains to partner aprocitentan, having been released from the exclusivity constraint with the undisclosed party, the company will resume discussions with alternative potential partners that recognize the value of aprocitentan. In April 2025, "Aprocitentan for Blood Pressure Reduction in Black Patients” was published in Hypertension. The publication reports preplanned analyses of the efficacy, tolerability and safety of aprocitentan in the subgroup of African American patients enrolled in the Phase 3 PRECISION study in patients with confirmed resistant hypertension. Aprocitentan, when added to a combination of at least three antihypertensive drugs (four in more than 50% of patients), produced clinically meaningful and sustained blood pressure reductions. Aprocitentan also markedly decreased proteinuria in the patients with proteinuria at baseline. As reported by the authors, aprocitentan was safe and well tolerated, even in those Black patients with chronic kidney disease. CompoundMechanism of actionTarget indicationPartner/statusTRYVIO™ (aprocitentan) Dual endothelin receptor antagonistSystemic hypertension in combination with other antihypertensivesTo be defined: worldwide development and commercialization rightsCommercially available in the USJERAYGO™ (aprocitentan)Dual endothelin receptor antagonistResistant hypertension in combination with other antihypertensivesTo be defined: worldwide development and commercialization rights Approved in the EU and UK; Marketing authorization applications under review in Canada, and SwitzerlandQUVIVIQ™ (daridorexant)Dual orexin receptor antagonistInsomniaNxera Pharma: license to develop and commercialize for Asia-Pacific region (excluding China)Launched for the treatment of insomnia in Japan; Phase 3 ongoing in South KoreaDaridorexantDual orexin receptor antagonistInsomniaSimcere: license to develop and commercialize for Greater China regionNDA submitted in Greater China; approved for the treatment of insomnia in Hong-KongSelatogrelP2Y12 inhibitorAcute myocardial infarctionViatris: worldwide development and commercialization rightsPhase 3 “SOS-AMI” program ongoingCenerimodS1P1 receptor modulatorSystemic lupus erythematosusViatris: worldwide development and commercialization rightsPhase 3 “OPUS” program ongoingDaridorexantDual orexin receptor antagonistPosttraumatic stress disorder (PTSD)US Department of Defense (DOD): Idorsia is supporting a clinical study sponsored by the US DOD to develop new therapies to treat PTSDACT-1002-4391EP2/EP4 receptor antagonistImmuno-oncologyOwkin: global license to develop and commercializePhase 1 ongoing Further details including the current status of each project in our partner-led portfolio can be found in our innovation fact sheet. Note to ShareholdersThe Annual General Meeting (AGM) of Shareholders to approve the Annual Report of the year ending December 31, 2024, will be held on Wednesday, May 28, 2025. In order to attend and vote at the AGM, shareholders must be registered in the company's shareholder register by May 19, 2025, 17:00 CEST, at the latest. Results Day CenterInvestor community: To make your job easier, we provide all relevant documentation via the Results Day Center on our corporate website: www.idorsia.com/results-day-center. Events Annual General Meeting of Shareholders on May 28, 2025Half-Year 2025 Financial Results reporting on July 30, 20259-Month 2025 Financial Results reporting on October 30, 2025 Notes to the editor About IdorsiaIdorsia Ltd is reaching out for more – we have more passion for science, we see more opportunities, and we want to help more patients. The purpose of Idorsia is to challenge accepted medical paradigms, answering the questions that matter most. To achieve this, we will discover, develop, and commercialize transformative medicines – either with in-house capabilities or together with partners – and evolve Idorsia into a leading biopharmaceutical company, with a strong scientific core. Headquartered near Basel, Switzerland – a European biotech hub – Idorsia has a highly experienced team of dedicated professionals, covering all disciplines from bench to bedside; QUVIVIQ™ (daridorexant), a different kind of insomnia treatment with the potential to revolutionize this mounting public health concern; strong partners to maximize the value of our portfolio; a promising in-house development pipeline; and a specialized drug discovery engine focused on small-molecule drugs that can change the treatment paradigm for many patients. Idorsia is listed on the SIX Swiss Exchange (ticker symbol: IDIA). For further information, please contactInvestor & Media RelationsIdorsia Pharmaceuticals Ltd, Hegenheimermattweg 91, CH-4123 Allschwil+41 58 844 10 10 investor.relations@idorsia.com – media.relations@idorsia.com – www.idorsia.com The above information contains certain "forward-looking statements", relating to the company's business, which can be identified by the use of forward-looking terminology such as "estimates", "believes", "expects", "may", "are expected to", "will", "will continue", "should", "would be", "seeks", "pending" or "anticipates" or similar expressions, or by discussions of strategy, plans or intentions. Such statements include descriptions of the company's investment and research and development programs and anticipated expenditures in connection therewith, descriptions of new products expected to be introduced by the company and anticipated customer demand for such products and products in the company's existing portfolio. Such statements reflect the current views of the company with respect to future events and are subject to certain risks, uncertainties and assumptions. Many factors could cause the actual results, performance or achievements of the company to be materially different from any future results, performances or achievements that may be expressed or implied by such forward-looking statements. Should one or more of these risks or uncertainties materialize, or should underlying assumptions prove incorrect, actual results may vary materially from those described herein as anticipated, believed, estimated or expected.
Attachment
Press Release PDF
上市批准引进/卖出财报
2025-04-24
Since its launch in 2015, it has been prescribed to more than 200,000 patients globally. The drug is currently approved for use in both men and women, expanding its market potential. Despite facing competition from other CDK4/6 inhibitors like Novartis' KISQALI and Eli Lilly's VERZENIO, IBRANCE maintains a strong position in the metastatic setting.
LAS VEGAS, April 24, 2025 /PRNewswire/ -- DelveInsight's "
IBRANCE Market Size, Forecast, and Market Insight Report" highlights the details around IBRANCE, a CDK4/6 inhibitor. The report provides product descriptions, patent details, and competitor products (marketed and emerging therapies) of IBRANCE. The report also highlights the historical and forecasted sales from 2020 to 2034 segmented into 7MM [the United States, the EU4 (Germany, France, Italy, and Spain), the United Kingdom, and Japan].
Pfizer's IBRANCE (palbociclib) Overview
IBRANCE is an oral medication that inhibits CDKs 4 and 6, which are crucial regulators of the cell cycle that drive cellular progression. In the U.S., IBRANCE is approved for treating adult patients with hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2-) advanced or metastatic breast cancer. It is used in combination with an aromatase inhibitor as a first-line endocrine therapy for postmenopausal women or men or with fulvestrant for patients whose disease has progressed after endocrine treatment. IBRANCE is currently authorized in over 90 countries and has been prescribed to more than 200,000 patients worldwide.
Learn more about IBRANCE projected market size for metastatic HR+/HER2− breast cancer @
IBRANCE Market Potential
The HR+ HER2- subtype is the most commonly found type of breast cancer, characterized by cancer cells that have estrogen and progesterone receptors but do not overexpress HER2. A patient's journey typically begins with the onset of concerning symptoms, leading to a comprehensive clinical evaluation and various imaging tests. DelveInsight estimates that approximately
211K new cases of HR+/HER2– breast cancer occurred in the US in 2024.
CDK4/6 inhibitors currently dominate the first-line treatment market and represent a significant advancement in the management of HR+/HER2-ve breast cancer. The data from large, randomized clinical trials are both strong and consistent. While single-agent endocrine therapies have shown limited benefits in the first and subsequent treatment lines for women with ER-positive metastatic breast cancer (mBC), combination therapies have emerged as a more effective option for many patients.
In recent years, the treatment landscape for HR+/HER2−ve breast cancer has been transformed with the introduction of highly active targeted therapies, including CDK4/6 inhibitors, mTOR inhibitors, PARP inhibitors, new oral SERDs, and PI3K inhibitors. These advances have expanded the range of treatment options and improved survival outcomes for these patients. The market for metastatic HR+/HER2− breast cancer in the 7MM is projected to grow during the forecast period (2025–2034) due to the introduction of several novel therapies in the market.
Discover more about the metastatic HR+/HER2− breast cancer market in detail @
Metastatic HR+/HER2− Breast Cancer Market Report
Emerging Competitors of IBRANCE
Some of the drugs in the pipeline include
Gedatolisib (Celcuity),
ARV-471 (Arvinas and Pfizer),
OP-1250 (Olema Pharmaceuticals),
KEYTRUDA (Merck), and
Rupitasertib (Evexta Bio), among others. In
December 2024, Arvinas and Pfizer presented preliminary data from the ongoing Phase 1b portion of the TACTIVE-U sub-study of vepdegestrant in combination with abemaciclib among patients with locally advanced or metastatic ER+/HER2- breast cancer at the San Antonio Breast Cancer Symposium (SABCS) 2024.
In
December 2024, Olema Pharmaceuticals presented clinical results from the ongoing Phase Ib/II study of palazestrant in combination with ribociclib in patients with ER+/HER2- advanced or metastatic breast cancer at SABCS 2024.
To know more about the number of competing drugs in development, visit @
IBRANCE Market Positioning Compared to Other Drugs
Key Milestones of IBRANCE
In
February 2021, Pfizer Inc. announced that the U.S. Patent and Trademark Office (USPTO) has granted a U.S. Patent Term Extension (PTE) certificate for IBRANCE. This extension prolongs the validity of U.S. Patent No. RE47,739 ('739) by over four years, now lasting until March 5, 2027.
In
April 2019, Pfizer announced that the FDA has approved a supplemental New Drug Application (sNDA) to broaden the uses of IBRANCE in combination with an aromatase inhibitor or fulvestrant, now including men with hormone receptor-positive (HR+), HER2-negative (HER2-) advanced or metastatic breast cancer.
In
March 2017, Pfizer Inc. revealed that the FDA has approved a supplemental New Drug Application (sNDA) for IBRANCE, its pioneering cyclin-dependent kinase 4/6 (CDK 4/6) inhibitor, following the positive outcomes from the confirmatory Phase 3 trial PALOMA-2.
In
September 2016, Pfizer Inc. announced that the European Medicines Agency's (EMA) Committee for Medicinal Products for Human Use (CHMP) had issued a positive recommendation for the marketing authorization of IBRANCE® (palbociclib) in the European Union (EU). This recommendation is for its use in treating women with hormone receptor-positive, HER2-negative (HR+/HER2-) locally advanced or metastatic breast cancer.
In
February 2016, Pfizer announced that the FDA has approved a new indication for IBRANCE 125mg capsules, expanding its use. The approval allows IBRANCE to be used in combination with fulvestrant for the treatment of hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2-) advanced or metastatic breast cancer in women whose disease has progressed after endocrine therapy.
In
February 2015, Pfizer announced that the FDA granted accelerated approval for IBRANCE in combination with letrozole to treat postmenopausal women with estrogen receptor-positive, human epidermal growth factor receptor 2-negative (ER+/HER2-) advanced breast cancer as the initial endocrine-based therapy for their metastatic disease.
Discover how IBRANCE is shaping the metastatic HR+/HER2− breast cancer treatment landscape @
IBRANCE Drug
IBRANCE Market Dynamics
IBRANCE is a targeted therapy that has revolutionized the treatment of hormone receptor-positive, HER2-negative breast cancer, particularly in
combination with aromatase inhibitors or letrozole. Developed by Pfizer, IBRANCE was one of the first
CDK4/6 inhibitors approved by the FDA for metastatic breast cancer, and its approval has significantly changed the treatment landscape. The drug works by inhibiting cyclin-dependent kinases 4 and 6, which are key regulators of the cell cycle, thus preventing cancer cells from proliferating. Its market dynamics have been shaped by the
growing demand for targeted therapies, as well as the
increasing focus on precision medicine and improved patient outcomes.
The global market for IBRANCE has been positively impacted by its proven
efficacy in clinical trials and its ability to extend progression-free survival in breast cancer patients. The drug's market dominance is underpinned by its
widespread acceptance and adoption by oncologists worldwide. However, competition is intensifying, with other CDK4/6 inhibitors such as
VERZENIO (abemaciclib) and KISQALI (ribociclib) entering the market, offering similar benefits but with some distinct clinical profiles. This competitive landscape has led to
strategic pricing and marketing strategies by Pfizer, aiming to maintain IBRANCE's market leadership while managing pressures from generic alternatives.
Additionally, the
evolving reimbursement landscape and regulatory policies around oncology drugs are crucial factors influencing the market dynamics. Health insurers and government healthcare programs often
scrutinize the cost-effectiveness of cancer treatments, which can impact the pricing and accessibility of IBRANCE in different markets. Another factor is the
rising focus on combination therapies, as IBRANCE is often used in conjunction with other drugs like letrozole, which boosts its efficacy and market potential. The shift toward personalized cancer treatment regimens is expected to continue fueling demand for CDK4/6 inhibitors like IBRANCE, especially in more advanced stages of breast cancer.
In terms of geographical markets, IBRANCE has seen significant uptake in
North America and Europe, where the healthcare infrastructure supports innovative cancer therapies. However, emerging markets, where the
economic barriers to accessing expensive cancer treatments can be higher, present a challenge to the widespread use of IBRANCE. Pfizer's ongoing efforts to expand in these regions, through
partnerships and pricing adjustments, will be key to ensuring continued growth in global market share. Overall, the IBRANCE market is poised for steady growth, driven by clinical advancements, increasing breast cancer diagnoses, and the continual push toward more targeted, effective therapies.
Dive deeper to get more insight into IBRANCE's strengths & weaknesses relative to competitors @
IBRANCE Market Drug Report
Table of Contents
Related Reports
Metastatic HR+/HER2− Breast Cancer Market
Metastatic HR+/HER2− Breast Cancer Market Insights, Epidemiology, and Market Forecast – 2034 report deliver an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key metastatic HR+/HER2− breast cancer companies, including
Merck, Arvinas, Olema Pharmaceuticals, Celcuity, Roche, AstraZeneca, Daiichi Sankyo, Eli Lilly, Sermonix Pharmaceuticals, Genentech, Veru Pharma, DualityBio, BioNtech, Evgen Pharma, Carrick Therapeutics, EQRx, G1 Therapeutics, Immutep, among others.
HR+/HER2− Breast Cancer Pipeline
HR+/HER2− Breast Cancer Pipeline Insight
– 2025 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key HR+/HER2− breast cancer companies, including
Regor Therapeuics, Seagen Inc., CytomX Therapeutics, Taizhou EOC Pharma, Chia Tai Tianqing Pharmaceutical Group, AstraZeneca, Daiichi Sankyo, Inc., Tyme, Inc., Seagen Inc., Context Therapeutics, Eisai Inc., Shanghai Hengrui Pharmaceutical Co., Ltd., Jiangsu Simcere Pharmaceutical Co., Kind Pharmaceuticals, Merus N.V., Atossa Therapeutics, Roche, among others.
Breast Cancer Market
Breast Cancer Market Insights, Epidemiology, and Market Forecast – 2034 report deliver an in-depth understanding of the disease, historical and forecasted epidemiology, market share of the individual therapies, and key breast cancer companies including
Veru, Sanofi, Roche, AstraZeneca, Eli Lilly, EQRx, Gilead, Sermonix Pharmaceuticals, Evgen Pharma, Tyme, Genentech, Daiichi Sankyo, among others.
Metastatic Breast Cancer Pipeline
Metastatic Breast Cancer Pipeline Insight – 2025 report provides comprehensive insights about the pipeline landscape, including clinical and non-clinical stage products, and the key metastatic breast cancer companies, including
Roche, RemeGen, SynCore Biotechnology, Allarity Therapeutics, Daiichi Sankyo Company, Jiangsu Alphamab Biopharmaceuticals Co., Ltd, Byondis B.V., Jiangsu Hansoh Pharmaceutical Co., Ltd., Shanghai Miracogen Inc., Ambrx, Inc., Daehwa Pharmaceutical Co., Ltd., Phoenix Molecular Designs, GlycoMimetics Incorporated, Rhizen Pharmaceuticals SA, Menarini Group, Samus Therapeutics, Inc., Hanmi Pharmaceutical Company Limited, Jiangxi Qingfeng Pharmaceutical Co. Ltd., Immutep Limited, Arvinas Inc., G1 Therapeutics, Mirati Therapeutics Inc., Chia Tai Tianqing Pharmaceutical, Shanghai Pharmaceuticals Holding Co., Ltd, Pfizer, OncoTherapy Science, Inc., Eisai Inc., Dizal Pharmaceuticals, Jiangsu Hengrui Medicine Co., Tyme, Inc, Orion Pharma, HiberCell, Inc., Rhizen Pharmaceuticals SA, Hutchison Medipharma Limited, OncoPep Inc., Taizhou Hanzhong biomedical co. LTD, among others.
About DelveInsight
DelveInsight is a leading Business Consultant and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve
.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
上市批准临床3期临床1期临床结果
2025-04-21
·医药健闻
跨国药企在中国重点资讯文 | 苏丁企业动态诺华诺华中国与首都医科大学附属北京天坛医院签署战略合作备忘录。双方将结合诺华中国在神经科学领域的产业优势与北京天坛医院在神经系统亚专科建设上的成果,在神经系统罕见病临床研究、学科建设、新药研发等方面展开全面合作。同时,由中国卒中学会发起、诺华中国支持的“神经免疫疾病规范诊疗能力提升项目——三一工程”正式启动,致力于实现神经免疫疾病的早诊早治和规范化诊疗。诺华邮件宣布,现任诺华中国肿瘤治疗领域肺癌领域和实体瘤产品组合负责人徐薇,将于2025年5月1日起担任诺华中国眼科、移植及中枢神经治疗领域负责人,并将加入国际业务部中国管理团队。徐薇的职业生涯始于2003年的诺华中国眼科治疗领域,并先后在多家跨国药企的多个治疗领域积累了丰富的行业知识和管理经验。礼来在第31届全国肿瘤防治宣传周首日,礼来携手本土合作伙伴信达生物、和黄医药齐聚上海,共话本土医药创新发展,探索加速惠及中国肿瘤患者的新模式。20年来,礼来在肿瘤领域积极探索以创新驱动的多元化业务模式,聚焦靶向治疗、免疫治疗以及克服肿瘤耐药药物的研发,已在中国获批上市9款创新药物,涵盖乳腺癌、肺癌、消化道肿瘤、血液肿瘤等10大癌种,并与本土战略伙伴建立了一条覆盖临床研究、生产质量到商业运营的端到端合作价值链。达伯舒(信迪利单抗注射液)是礼来和信达生物在中国共同开发的具有国际品质的创新PD-1抑制剂;爱优特(呋喹替尼胶囊)是礼来中国肿瘤产品组合中首个获批的肿瘤靶向治疗药物。安斯泰来由安斯泰来中国主办的“中国胃癌创新大会(2025 CGIC)”在广州举行。会议聚焦三大核心板块:中国晚期胃癌治疗范式演变、Claudin18.2(CLDN 18.2)靶点临床研究突破及精准医学动态风向。安斯泰来全球精准医学与诊断部门负责人Diarmuid Moran博士以“CLDN 18.2伴随诊断的开发:从生物标志物到临床应用”为题,深入阐述了伴随诊断试剂从靶点发现到标准化生产的全链条开发路径。安斯泰来中国副总经理及开发本部负责人王娜引领与会者共同踏上了一场关于以CLDN 18.2为作用靶点的创新药物的“发现之旅”,回顾了该药物研发历程中的关键节点与突破性进展。富士胶片富士胶片(中国)投资有限公司旗下富士胶片智慧医疗技术培训中心与上海健康医学院医学影像学院共同揭牌“上海健康医学院医学影像技术实践基地”。此次合作标志着双方自2018年以来的校企合作迈入全新阶段,未来双方将围绕超声、内镜、放射等医学影像技术领域,共同打造集教学、培训、科研于一体的综合性人才培养平台。美纳里尼《带状疱疹中西医结合诊疗专家共识(2025版)》4月17日在中国中西医结合学会皮肤性病专业委员会2025年学术年会上正式发布。美纳里尼作为《共识》制定的支持方,为推动这一重要共识的诞生贡献了关键力量。《共识》基于现有循证证据,充分考量中西医结合治疗带状疱疹的特点,权衡各种干预措施的利弊,围绕带状疱疹不同病程阶段、特殊人群及特殊部位等关键问题,形成中西医结合治疗带状疱疹的若干条推荐意见。勃林格殷格翰勃林格殷格翰升级蓝耳防控方案,推出PRRS COMBAT 2.0生物安全在线管理评估工具以及《后备母猪管理指南》手册,旨在为中国猪场提供更为全面、先进的蓝耳防控方案,提升猪群健康,助力中国养猪业高质量发展。勃林格殷格翰推出PRRS COMBAT 2.0生物安全在线管理评估工具,助力猪场提升蓝耳生物安全防控水平。PRRS COMBAT 2.0基于1.0版本迭代升级,集成了四大核心功能:定制化评估方案、风险等级评估、改善建议输出以及行业对标分析,助力客户精准且专业地评估猪场蓝耳病风险。百汇医疗上海百汇医院与上海闵行区诺达双语学校携手开展百汇艺术季活动,并首次以不插电音乐会及共创艺术展览的创新形式向社会和公众展现百汇医疗的可持续发展理念与社会服务精神。用独特的方式把医疗空间与艺术形式有效融合,将“地球保护”这一深刻主题用轻松与温暖的形式呈现给社会大众,并传播“地球保护从我做起”的价值观是此次活动非常重要的一环。上海德达心血管医院从4月8日起,由中国红十字基金会组织的上海德达心血管医院专家医疗团队,开始在新疆喀什地区的巴楚县、麦盖提县、英吉沙县等地开展“天使之旅”先天性心脏病患儿筛查救助行动。医疗专家团队和当地红十字会的志愿者携带便携设备深入县乡,针对0至14岁儿童进行先天性心脏病筛查。上海德达医院是全国首家外商独资心血管专科医院。欧加隆欧加隆携手连锁药房高济健康、线上购药平台美团买药,共同呼吁整合零售端健康管理优势资源,延伸痛风患者从院内到院外的全链条健康管理。作为倡议起点,欧加隆与丁香园合作推出的《痛风人自救指南》将于世界痛风日后陆续发放于全国连锁药店。这一疾病管理手册由权威专家指导科学信息,以易读、易懂、易用的内容,为零售药师提供专业指导,帮助患者科学管理疾病。欧加隆也将进一步深化与美团买药等伙伴的合作,推动“线上下单—药店快速响应—专业服务即时送达”的高效闭环。默沙东由新华网发起、默沙东支持的“畅跑马拉松,防护你我他”——“HPV男女共防计划”北半马主题活动新闻发布会4月18日在京举办。默沙东与多方携手,以创新形式集结大众的参与力量,共同开拓健康守护新赛道,以马拉松精神呼应全民健康防护,以期未来在全国范围内提升“男女共防HPV相关癌症及疾病”的科普认知,呼吁社会各界加强HPV感染男女共防的健康意识,助力共建HPV感染预防新生态。产业动态西门子医疗国产Atellica全自动生化免疫分析仪和国产Atellica全自动化学发光免疫分析仪正式获批上市。这一国际标杆产品的本土化生产标准着西门子医疗持续推进“在中国,为中国”战略的又一重要里程碑。西门子医疗将继续加大在中国的研发投入,深化本土合作。国家药品监督管理局批准了美敦力的“血管外植入式心脏除颤电极导线”和“血管外植入式心脏除颤电极导线导入器”两个创新产品注册申请。两个产品配套使用,与血管外植入式心律转复除颤器组合构成血管外植入式心律转复除颤器系统,放置在胸骨下,对发生或可能发生危及生命的室性心动过速的重大风险患者进行自动治疗。默沙东宣布,佳达修9[九价人乳头瘤病毒疫苗(酿酒酵母)](九价HPV疫苗)多项新适应证已获得国家药品监督管理局的上市批准,适用于16~26岁男性接种。这一获批使佳达修9成为中国境内首个且目前唯一获批、可适用于适龄男性女性接种的九价HPV疫苗,标志着中国正式进入了“男女共防HPV相关癌症及疾病”的新阶段。诺和诺德宣布,其每周一次长效生长激素Somapacitan注射液已被博鳌未来医院作为临床急需药品引进,可用于在生长激素缺乏症所致生长迟缓的3岁及以上儿童和青少年中替代内源性生长激素。在特许医疗政策的支持下,Somapacitan注射液是博鳌乐城国际医疗旅游先行区引进的首款儿童生长激素,也是该药品在国内首次落地。Somapacitan注射液是一种长效人生长激素蛋白衍生物。晖致医药申报的“布地奈德福莫特罗吸入气雾剂”获批上市。此次获批适应症覆盖中重度哮喘及慢性阻塞性肺疾病(COPD)两大领域,为呼吸系统疾病患者提供更具可及性的治疗选择。中国国家药监局药品审评中心(CDE)官网最新公示,礼来公司申报的米吉珠单抗注射液(mirikizumab)以及其皮下注射剂型的新适应症上市申请获得受理。本次该药申报上市的适应症为可能为治疗中重度活动性溃疡性结肠炎(UC)成人患者。日本兴和制药(Kowa Company)研发的佩玛贝特片(Pemafibrate)正式获得中国国家药监局(NMPA)批准,用于治疗血脂异常。佩玛贝特的核心竞争力体现在其对甘油三酯(TG)的显著降低效果。联系美通社+86-10-5953 9500info@prnasia.com
免疫疗法上市批准
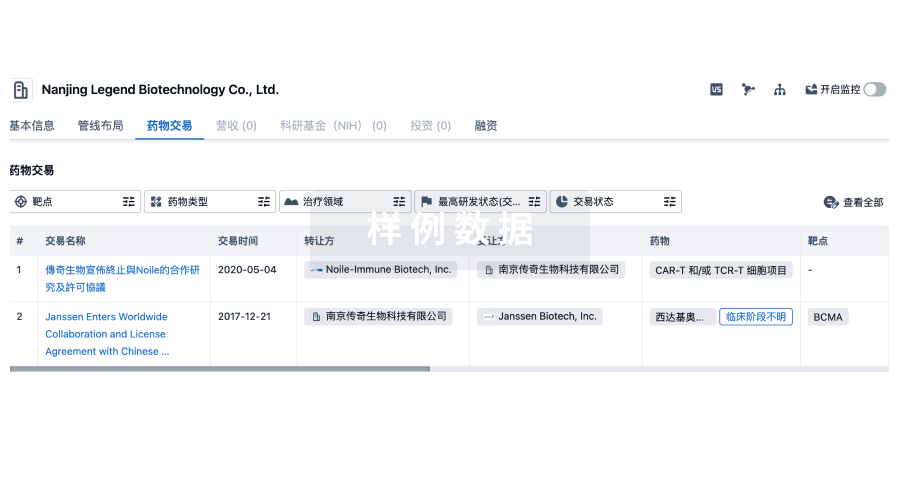
100 项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的药物交易
登录后查看更多信息
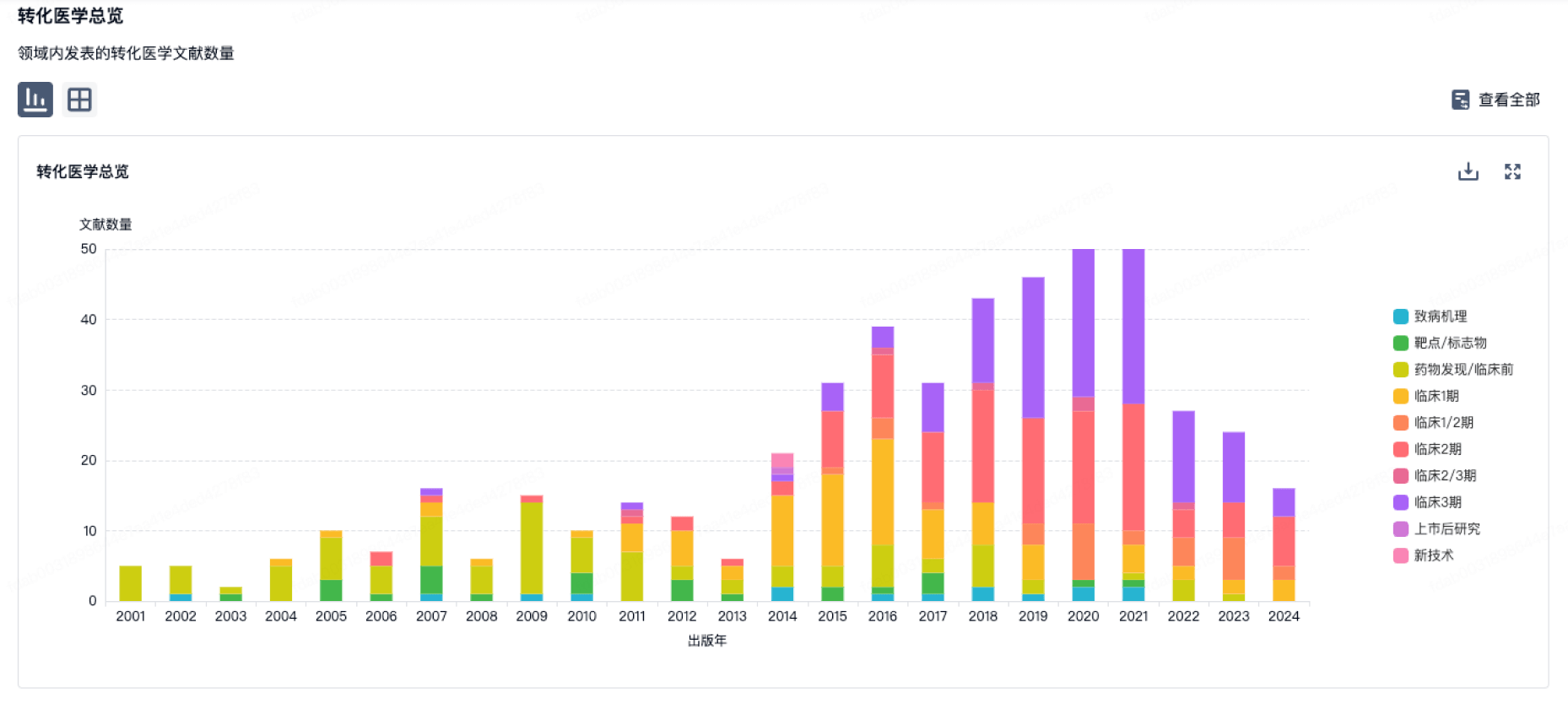
100 项与 A. Menarini Industrie Farmaceutiche Riunite Srl 相关的转化医学
登录后查看更多信息
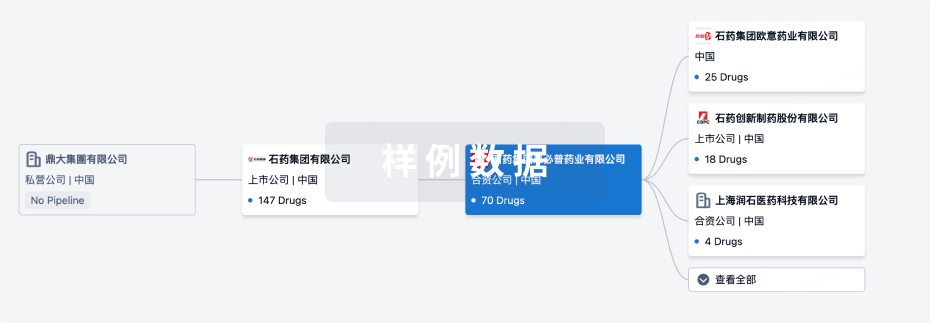
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月06日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
4
临床1期
临床2期
4
27
批准上市
其他
55
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
阿地溴铵/富马酸福莫特罗 ( M3 receptor x β2-adrenergic receptor ) | 慢性阻塞性肺疾病 更多 | 批准上市 |
氟尿嘧啶/水杨酸 ( COXs x TYMS ) | 光化性角化病 更多 | 批准上市 |
阿地溴铵 ( M3 receptor ) | 慢性阻塞性肺疾病 更多 | 批准上市 |
Tagraxofusp-ERZS ( CD123 ) | Blastic浆细胞样树突状细胞肿瘤 更多 | 批准上市 |
比拉斯汀 ( H1 receptor ) | 荨麻疹 更多 | 批准上市 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
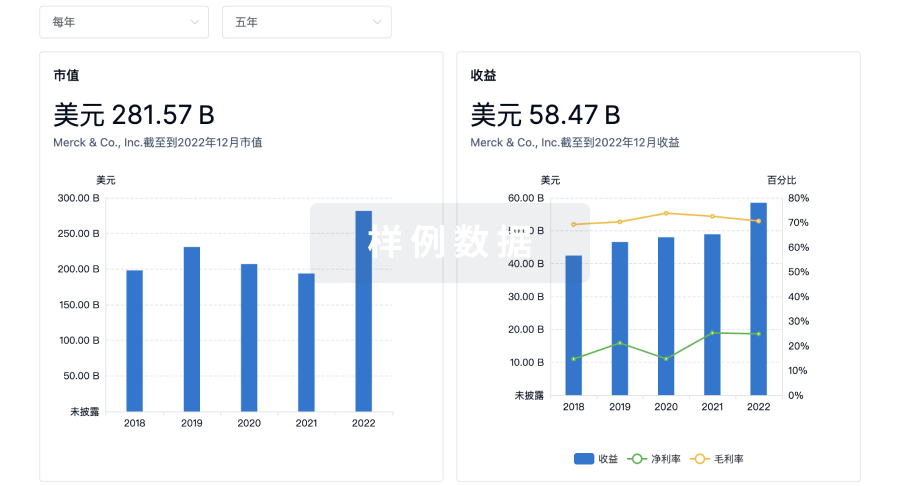
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用