预约演示
更新于:2025-05-07

Ascentage Pharma Group International Co., Ltd.
更新于:2025-05-07
概览
标签
肿瘤
血液及淋巴系统疾病
内分泌与代谢疾病
小分子化药
蛋白水解靶向嵌合体(PROTAC)
单克隆抗体
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 13 |
| 蛋白水解靶向嵌合体(PROTAC) | 2 |
| 肿瘤坏死因子 | 1 |
| 单克隆抗体 | 1 |
| 化学药 | 1 |
关联
28
项与 亞盛醫藥集團 相关的药物作用机制 Bcr-Abl T315I抑制剂 [+1] |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2021-11-24 |
作用机制 PD-1抑制剂 [+2] |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2018-12-17 |
靶点 |
作用机制 BTK抑制剂 |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2017-10-31 |
86
项与 亞盛醫藥集團 相关的临床试验NCT06817720
Phase II Study Assessing the Efficacy and Toxicity of Olverembatinib Monotherapy in Patients With Newly Diagnosed Chronic Myeloid Leukemia in Chronic Phase
To learn if olverembatinib can help to control newly diagnosed CML in the chronic phase.
开始日期2025-07-30 |
申办/合作机构 |
NCT06641414
A Global Multicenter, Double-blind, Randomized, Registrational Phase 3 Study of Lisaftoclax (APG-2575) in Combination With Azacitidine (AZA) in Patients With Newly Diagnosed Higher Risk Myelodysplastic Syndrome (HR-MDS) (GLORA-4).
A global multicenter, randomized, double-blind, placebo-controlled, pivotal phase III study. To evaluate overall survival (OS) of Lisaftoclax (APG-2575) combined with azacitidine (AZA) vs. placebo combined with azacitidine in newly diagnosed patients with HR-MDS.
开始日期2025-01-22 |
申办/合作机构 |
CTR20243841
APG-2575 (Lisaftoclax)联合阿扎胞苷(AZA)治疗新诊断的中高危骨髓增生异常综合征患者的一项国际多中心、随机、双盲、安慰剂对照的关键性注册临床3期研究(GLORA–4)
评估APG-2575 (Lisaftoclax)联合阿扎胞苷(AZA)对比安慰剂联合阿扎胞苷治疗新诊断的中高危骨髓增生异常综合征(Higher-risk MDS)受试者的有效性及安全性。
开始日期2025-01-22 |
申办/合作机构 |
100 项与 亞盛醫藥集團 相关的临床结果
登录后查看更多信息
0 项与 亞盛醫藥集團 相关的专利(医药)
登录后查看更多信息
95
项与 亞盛醫藥集團 相关的文献(医药)2025-04-21·Cancer Research
Abstract 5648: Effects of olverembatinib (HQP1351) in combination with BCL-2 inhibitor lisaftoclax (APG-2575) in T-cell acute lymphoblastic leukemia (T ALL)
作者: Zhai, Guoqing ; Min, Ping ; Yu, Huidan ; Yu, Zhou ; Zhai, Yifan ; Xiong, Yan ; Wu, Bingxing ; Yang, Dajun ; Liang, Zhiyan ; Peng, Bo
2025-04-21·Cancer Research
Abstract 1679: APG-2449, a novel focal adhesion kinase (FAK) inhibitor, enhances the antitumor activity of chemotherapy in preclinical models of small-cell lung cancer (SCLC) with activated FAK
作者: Liu, Daojie ; Yu, Zhou ; Zhai, Yifan ; Yang, Dajun ; Liang, Zhiyan ; Yao, Xinyi
2025-04-21·Cancer Research
Abstract 5651: Discovery of AS03157 as a highly potent and orally active antagonist of inhibitor of apoptosis proteins (IAPs)
作者: Han, Xiao ; Chen, Jianyong ; Liang, Zhiyan ; Hu, Jiantao ; Yu, Zhou ; Xiong, Yan ; Zhai, Yifan ; Yang, Dajun
2,152
项与 亞盛醫藥集團 相关的新闻(医药)2025-05-04
·健识局
5月1日,津药药业、江苏联环药业因涉嫌垄断地塞米松磷酸钠原料药,被天津市市场监督管理委员会行政处罚,合计被罚没超1.3亿元。此前4月23日,仙琚制药在年报中披露,涉嫌地塞米松磷酸钠原料药价格垄断,收到天津市市场监督管理委员会行政处罚告知书,罚没款预计为 1.95 亿元。值得一提的是,津药药业已经不是第一次垄断,津药药业及其下属公司天津天药此前已经因药品垄断被处罚3次,三次没收和罚款合计超亿元。更多消息,健识局整理如下:重磅政策一览1.涉嫌垄断,两家药企被罚超1.3亿元5月1日,津药药业、江苏联环药业公告:公司因对地塞米松磷酸钠原料药实施的垄断行为,收到天津市市场监督管理委员会下发的《行政处罚决定书》、《行政处罚告知书》。地塞米松磷酸钠注射剂是一款激素类抗炎药,为国家医保药品目录甲类药品,也是第九批国采采购金额最大的品种。据媒体报道,近两三年来,这款原本廉价的临床常用药品价格经历过暴涨和暴跌。公告显示,津药药业、江苏联环药业与具有竞争关系的其他经营者,就地塞米松磷酸钠原料药达成并实施“固定或者变更商品价格”垄断协议。津药药业被没收违法所得4276.44万元、并处2023年度销售额8%的罚款约1.32亿元,结合宽大情形,减免罚款额的80%,减免后实际罚款约2642.8万元。以上罚没款合计超过6919万元。江苏联环药业被没收违法所得约1790万元,并处2023年度销售额8%的罚款 约6162.7万元,结合宽大情形,减免罚款额的30%,减免后实际罚款约4314万元。合计被罚没约6163万元。医药卫生事件1.吴以芳辞任复星医药董事长4 月 30 日,复星医药发布公告,收到吴以芳的书面辞职函,辞任自2025年4月29日生效。吴以芳是复星医药老将,在复星医药工作逾二十年,曾任万邦生化副总经理、总裁、董事长兼首席执行官。2004 年万邦生化加入复星医药集团,吴以芳进入复星医药,2016年至今任复星医药首席执行官。2020年,吴以芳就任复星医药董事长职务。吴以芳的职位由陈玉卿接任。陈玉卿2010年加入复星医药,从人力资源岗位起步,任总裁助理兼人力资源部总经理、联席首席执行官等职。2.三甲医院院长被砍伤4月30日,经济观察报报道,南京鼓楼医院院长于成功在4月28日被人砍伤,目前已脱离危险。一位知情人士表示,行凶者长期尾随于成功,4月28日夜间,行凶者携带凶器尾随于成功至家中,将于成功及其妻子砍成重伤。目前未发现于成功接诊过该行凶者,行凶者也并非传闻中与于成功家人有情感纠纷。南京鼓楼医院又名南京大学医学院附属鼓楼医院,是一家知名三甲医院,建于1892年,是中国最早的西医院之一,有床位4300余张,在岗职工6200余人。于成功生于1965年,1997年博士毕业后进入南京鼓楼医院工作至今,是二级教授、博士生导师,擅长炎症性肠病诊治。3.葫芦娃药业被ST4月28日,葫芦娃药业发布公告称,因2024年度财报被出具保留意见审计报告且内控存在重大缺陷,公司股票自4月30日起被实施退市风险警示,股票简称变更为“ST葫芦娃”。葫芦娃药业财务问题由来已久。去年,海南证监局出具责令改正的决定,要求葫芦娃药业重述其2023年度财报。审计机构表示,截至审计报告日,葫芦娃药业尚未提供与上述重述事项相关的完整财务资料,以及相关原始资料,因此出具保留意见审计报告。近期葫芦娃药业人事变动频繁,公司总经理张铭芮入职不到两个月,就宣布辞职。2024年财报显示,公司实现营业收入14.14亿元,同比下降21.26%;归母净利润为-2.74亿元,同比下降2629.23%。一周药械盘点1.百济神州的BCL2抑制剂申报上市4月28日,CDE官网公示,百济神州的BCL2抑制剂索托克拉片的上市申请获得受理,并纳入优先审评,适用于治疗既往接受过治疗的慢性淋巴细胞白血病(CLL)/ 小淋巴细胞淋巴瘤(SLL)成人患者。目前,全球只有艾伯维/罗氏的维奈克拉一款BCL2抑制剂获批上市,2023年全球销售额超过20亿美元。根据百济神州介绍,与维奈克拉相比,索托克拉在临床前研究和肿瘤模型中均显示出更高的效力和靶点选择性,并有可能克服耐药性。除了百济神州之外,亚盛医药的BCL2抑制剂也已经递交上市申请;诺诚健华的同类品种处于III期临床阶段。艾伯维/罗氏在研的Bcl-xl/Bcl-2抑制剂Navitoclax也已进入III期临床。2.强生FcRn单抗获批上市4月30日,强生宣布尼卡利单抗获得FDA批准上市,用于治疗自身抗体阳性的12岁及以上青少年和成人全身型重症肌无力患者。尼卡利单抗是一款靶向FcRn的IgG1型单克隆抗体。2020年8月,强生以65亿美元价格收购Momenta,获得了这款药物。此前,全球已有两款FcRn单抗获得FDA批准上市,分别是Argenx/再鼎的艾加莫德α和优时比的罗泽利昔珠单抗。3.诺华重磅核药Pluvicto在华申报新适应症4月28日,CDE官网显示,诺华的镥[177Lu]特昔维匹肽在华申报新适应症。根据临床试验及注册申报进展,推测此次申报的适应症为前列腺癌。镥[177Lu]特昔维匹肽是诺华收购Endocyte获得的一款放射配体疗法,由靶向PSMA的小分子化合物与治疗性放射性核素镥177偶联而成,2022年3月首次获得FDA批准上市。据诺华财报,2024年该药物的全球销售额已达13.92亿美元。撰稿 | 李傲编辑 | 江芸 贾亭运营 | 雾纪插图 | 视觉中国三个月闭店14000家,疯狂时代终结迈瑞医疗增长神话崩塌,狂奔时代结束胰岛素市场发生重大变化,通化东宝上市以来首次亏损
高管变更带量采购
2025-05-02
“闷声发大财”的泽璟制药,开始被发现了。资深分析师:尧 今编审:苏 叶这是一家为数不多,大盘几乎涨了三年的未盈利创新药企。自2022年资本寒冬以来,整个行业面愁云密布。然而,泽璟制药涨幅却超400%,市净率显著高于行业平均,市值也翻了好几番,甚至已经超过了君实、荣昌、再鼎、诺诚健华等营收规模大了好几倍的药企。深挖各项数据后,这家药企似乎都在“闷声发展”。根据最新披露的2024财报,泽璟实现营业收入 5.33亿元,同比上年增长 37.91%;净利润-1.38亿,同比增长50.54%。2025年一季度延续这一趋势,实现营收1.68亿元,同比增长54.87%。但与亮眼股价和业绩涨幅形成鲜明反差的是,这家“小而美”的未盈利创新药企在大众印象中,却活得稍显透明。它成立于2009年,明明较不少创新药企成立时间更早,但却没什么名气,资本圈的相关讨论声也相对沉寂。外界对其最大认知,大多还停留在四五年前的“科创板首家适用第五套标准上市上市的未盈利企业”“国内首个氘代药研发者”两大标签。由此,外界不禁疑惑,泽璟用什么支撑起了高估值?迅速膨胀起来的估值背后,暗藏了投资者哪些预期?还有哪些潜在水面的风险点?CM10医药研究中心将从行业稀缺值、财务健康度、业务健康度等维度一一剖析。▲泽璟制药股价走势图,数据来源:百度股市通两大已上市产品的可预期验证它凭什么高估值?要回答这一问题,还得回归泽璟的核心竞争力——产品本身实力来论。一家年营收仅5亿左右的未盈利药企,之所以市值能超越众多营收规模数倍于己的同行,答案或藏于其“稀缺”的产品矩阵和可预期的商业化空间之中。一是已上市产品的稀缺性和可验证的商业化能力。目前,泽璟已上市两款药物,且均具有一定稀缺性和独特市场地位,分别为首个国产氘代药物甲苯磺酸多纳非尼片、国内唯一采用重组基因技术生产的人凝血酶产品重组人凝血酶。先看泽璟首个获批产品——甲苯磺酸多纳非尼片,这既是首个国产氘代药物,也是首个国产肝癌一线靶向药。作为泽璟的“现金牛”产品,多纳非尼已获批两大适应证。先是2021年6月获批一线治疗晚期肝癌适应证,成为继拜耳索拉非尼、卫材仑伐替尼后第三款被批准用于晚期肝细胞癌一线治疗的小分子靶向药物。后又于2022年8月再斩获一大适应证,用于治疗进展性、局部晚期或转移性放射性碘难治性分化型甲状腺癌。与索拉非尼、仑伐替尼相比,凭借安全性更优,且进入医保后价格优势显著,多纳非尼上市后销售额攀升明显。截至2024年底,多纳非尼已进入医院 1100 余家、覆盖医院 2000 余家、覆盖药房近1000家,销售持续放量。而2024年之所以营收涨幅超30%,便得益于多纳非尼片的销量增加。按照当前趋势,多纳非尼肝癌适应证应该仍有不少上升空间。再加上甲状腺癌适应证2022年获批后贡献增量,短时间业绩增长成为可预期。再看泽璟第二款上市产品——重组人凝血酶。这款产品的竞争格局就更为明了。凝血酶是一种重要的局部外用止血药物,由于血浆来源日益缺乏、血浆提取产品潜在残留病毒或免疫原性等安全性风险和血浆提取产品的生产成本日益升高等原因,中国市场上血源生化提取的多数凝血酶产品已经停产。根据卫健委《关于印发国家短缺药品清单的通知(国卫办药政发〔2020〕25 号)》,凝血酶属于《国家临床必需易短缺药品重点监测清单》中品种。而泽璟重组人凝血酶的稀缺性便得以体现,它是国内唯一采用重组基因技术生产的人凝血酶产品,于2024年1月获批上市,目前已进入医保目录,填补外科手术局部止血领域空白。全球同类产品仅有BMS的Recothrom,于2008年美国上市,不过该药物尚未进入国内市场。虽然凝血市场相较“小而美”,但是这款药的独特性,还是有望助泽璟在国内站稳一方脚跟。弗若斯特沙利文预测,外科手术局部止血市场将由2018年的73.0亿元增长至2030年的160.3亿元,年复合增长率为6.8%。对于这款药物,与自建团队进行多纳非尼片商业化不一样,泽璟这款商品未盲目选择自行商业化,而是选择了 “借力打力” 的商业化策略——与远大生命科学子公司远大辽宁达成独家合作,由后者负责大中华区的市场推广。目前,泽璟已累计收到合作方支付的独家市场推广权许可费人民币3.4亿元。此番考量背后不无道理。重组人凝血酶属于外科止血药品,泽璟制药的销售团队主要专注于肿瘤药物销售,与具备外科止血领域市场推广和销售实力的合作伙伴进行商业化合作,将更加有利于重组人凝血酶的市场推广和销售。泽璟看向远大生命科学,也是因为其在围术期和止血领域深耕多年,从而在止血药品入院和销售方面经验丰富。如以注射用矛头蝮蛇血凝酶为代表的止血产品,连续多年销量靠前。二是,泽璟的产品线并非孤立存在,可发挥更大协同效应。以首款上市的多纳非尼片为例,作为晚期肝癌一线治疗的核心药物,其主要覆盖肝胆外科领域;而 2024 年获批的重组人凝血酶,同样可应用于肝胆手术的止血环节。两者在临床场景上的高度契合,或有利于资源共享且提升市场推广效率。此外,临近上市的重组人促甲状腺激素,与多纳非尼新获批的甲状腺癌适应证形成 “诊断+辅助治疗” 搭档,未来或有望为核医学科提供一站式解决方案。这种产品间的聚焦与协同效应,或有助于其更好发挥自身优势。三是,泽璟在研基本无废管线,且具有稀缺价值拉升预期。纵观来看,无论是已临近上市产品,还是尚处临床阶段的在研管线,大多具备 “国产首创” 或 “全球前沿” 的竞争优势。高壁垒在研管线的预期与焦虑目前看来,与多数药企管线中存在 “哑弹” 不同,泽璟制药几乎无“废管线”。每款产品锚定市场空白,且研发都算是走在前列,算是一家梯度相对明晰的药企。细究到一众在研管线,最拉升泽璟当前预期,主要在于两款临近上市的产品——JAK抑制剂盐酸吉卡昔替尼片和注射用重组人促甲状腺激素。▲截图来自泽璟制药官网先看JAK抑制剂盐酸吉卡昔替尼片,这是一个拥有大适应证的大单品,目前共有11个适应证在研。其中进展最快的适应证为骨髓纤维化,已处于上市前审评审批阶段,这是首个提交治疗骨髓纤维化适应证NDA的国产JAK抑制剂类创新药物。目前,骨髓纤维化属于罕见病,治疗药物有限。全球范围内仅有芦可替尼、菲达替尼和帕瑞替尼三款靶向药物获批用于骨髓纤维化,但国内仅有诺华芦可替尼上市,是目前在我国唯一获批上市治疗骨髓纤维化的JAK抑制剂。也就是说,吉卡昔替尼片上市后将直接对标诺华这款产品。这一市场前景算是“小而美”。根据弗若斯特沙利文预测,目前国内骨髓纤维化患者规模或将超过6万人,2030年中国骨髓纤维化靶向药市场的临床可惠及人口渗透率将达到 30.7%,整体市场规模超过30亿元。更值得一提的是,借助这款药,泽璟大肆进军自免这一蓝海领域。不过其在斑秃、特应性皮炎等热门自免适应证中,几乎难抢到先发红利。其中,斑秃是吉卡昔替尼片布局自免领域进度最快的适应证,目前泽璟正推进重症斑秃适应证NDA资料准备工作。但是这一适应证在研情况还是颇为激烈的。泽璟斑秃适应证虽然研发进度靠前,但恐无法抢得国产首个名额了。斑秃这一市场空间较为可观。根据弗若斯特沙利文,2020年中国约有381.2万例斑秃患者,预计到2030年患者规模将达到464.9万人,患者规模大。相关指南和共识将 JAK 抑制剂作为斑秃系统疗法的首选治疗选择。迄今为止,国内已批准礼来巴瑞替尼及辉瑞利特昔替尼两款JAK抑制剂治疗斑秃,都是跨国药企。放眼国内企业,除泽璟外,还有恒瑞医药、石药集团等公司亦布局了JAK抑制剂。其中,针对重度斑秃这一适应证,恒瑞医药JAK抑制剂硫酸艾玛昔替尼片进度最为靠前,药物上市许可申请已于2024年下半年获国家药监局受理。这也意味着,在礼来、辉瑞产品相继在中国获批后,恒瑞很可能摘得“国产首个”。按照当前在研进度,待泽璟斑秃适应证上市后,市场或已较为激烈,不仅要从两大跨国巨头口中夺食,还需要从国内医药一哥恒瑞手中分羹,这对其商业化能力恐是一大较大考验。另一进度较为靠前的适应证是特应性皮炎,目前已处于III期阶段,竞争激烈程度同样不亚于此。此外,吉卡昔替尼片还被用于开展强直性脊柱炎(III期)、特发性肺纤维化(II 期)、移植物抗宿主病(II 期)、中重度斑块状银屑病(II 期)等自身免疫性疾病的临床试验,并于2022年获得了系统性红斑狼疮和重型新型冠状病毒肺炎适应证的临床试验批件。E药资本界认为,未来看点或在于,恒瑞若率先获批,将抢占斑秃市场;而对于泽璟而言,其选择骨髓纤维化这一“小而专”的适应证切入,有差异化定位,避开红海竞争,抢占国产JAK抑制剂在血液病领域的空白市场。若骨髓纤维化适应证先发优势确立,可反哺斑秃领域资源,但需追赶时间窗口。再则,还需考虑一大风险,大家都知道,FDA对JAK抑制剂的黑框警告(血栓、肿瘤风险)可能影响国内监管态度,安全性数据将成为核心审评因素。再看第二款临近上市产品——注射用重组人促甲状腺激素。这是中国首批取得用于甲状腺癌的辅助诊断和治疗临床试验批件的新药。从国内外竞争现状来看,目前国内尚无国产产品获批,全球仅默克的Thyrogen(重组人促甲状腺激素α)获批上市,国内已进口但未纳入医保,患者自费负担相对较重,为泽璟留了些生存口子。而其他国产药企进度大多落后于泽璟,如远大医药、智核生物等处于早期临床。海通证券最新预测,泽璟这款重组人促甲状腺素针对分化型甲状腺癌术后诊断的适应证有望于2025年获批上市,当年销售额达0.2亿元,次年收入达0.5亿元。除了这两款临近上市产品,泽璟生物还有8个处于临床I/II 期阶段的在研新药,投资者尤其对其双抗和多抗产品关注颇多。一款是ZG005(PD-1/TIGIT双抗)。Insight数据库显示,目前全球仅6款PD-1/TIGIT 双抗在研,尚无同类机制药物获批上市。其中阿斯利康Rilvegostomig进展最快,已进入入全球临床III期。泽璟PD-1/TIGIT双抗ZG005全球进度第二。另外国内还有信达IBI321在研,不过进度更靠后一些。另一款,ZG006是一款全球首创的DLL3三抗(CD3/DLL3/DLL3三抗),这款药物已于2024年8月获FDA颁发的孤儿药资格认定,主要针对小细胞肺癌适应证进行开发。横向对比ZG006和其他DLL3 CD3药物或DLL3 ADC,ZG006暂时展现出一定竞争力,ORR相比其他TCE药物接近翻倍。由于ZG005、ZG006等已获FDA临床试验批准,海外授权合作潜在可能性较高。再简单看下其它管线,VEGF/TGF-β双抗(ZGGS18)、LAG-3/TIGIT双抗(ZGGS15)等早期项目均进入Ⅰ/Ⅱ期,覆盖实体瘤及免疫微环境调控。不过,这些在研管线尚处研发早期,仍具有一定不确定风险。 推荐阅读 * 单日暴涨17%!创新药二哥提前盈利,引爆了什么?* 暴降90%,被集采重创的心血管“大玩家”,开始重生商业化与BD能力的大考在创新药企的估值逻辑中,已上市产品的商业化兑现程度,以及在研管线的BD潜力和潜在市场格局,都是重要的评估指标。市场普遍呈现 “赢家通吃” 特征,首款上市产品往往占据过半份额,后续产品市场空间逐级递减,尤其第四位及以后的产品往往难以获得更多市场预期。摆在泽璟面前的问题,同样如此。随着大产品即将上市,外界对其一大核心隐忧便在于,泽璟商业化能力能否匹配市场需求成为关键。其一,大产品上市后的商业化资源瓶颈。上市产品商业化打法,直接决定未来放量空间和机会。泽璟目前市净率显著高于行业平均,需警惕商业化不及预期带来的回调。要知道,对于目前已上市的两款产品,泽璟的商业化路径比较明晰了:一方面,自己搭建肿瘤销售团队,负责多纳非尼的商业化;另一方面,积极寻求外部合作,探索 CSO 等路径,选择与远大生命科学子公司合作推广重组人凝血酶。因同属肿瘤治疗领域,注射用重组人促甲状腺激素可借助现有商业化团队实现资源协同。相比之下,市场目光更聚焦于吉卡昔替尼片获批后的商业化策略。在最新披露的财报中,泽璟已透露,针对吉卡昔替尼片获批后的商业化工作,已提前积极布局,在现有商业化团队核心骨干架构的基础上,新增招聘擅长血液病领域的市场、医学和销售推广的优秀人才。尽管泽璟已着手血液病领域人才储备,但其“自建团队”的商业化模式成效存疑。随着自免适应证产品陆续获批,现有聚焦肿瘤领域的商业化团队将面临资源分散难题,团队扩建或成必然。这一挑战主要受两大因素制约:其一,现金流的可持续性,直接决定团队扩张与运营的资金保障;其二,市场竞争格局下,与头部企业的综合实力博弈,将考验其商业化资源整合与市场渗透能力。现金流压力。2025年一季度,泽璟营收增长但经营现金流净额骤降至-625.32万元(同比下滑107.02%),主因报告期内无大额市场推广授权款入账;同时销售费用同比大增56.49%,侵蚀利润空间。竞争格局严峻。骨髓纤维化适应证患者基数小,需直面诺华芦可替尼竞争;自免疾病市场虽大,但恒瑞、石药、礼来等已占据渠道与品牌优势。若吉卡昔替尼在斑秃等适应证安全性数据显著优于竞品,或存在突围机会。相较而言,泽璟商业化能力存在一些短板。比如销售团队经验不足,对比恒瑞、石药成熟的肿瘤/自免药销售网络,泽璟当前商业化团队规模较小,尚无太多重磅药物销售经验,可能影响市场渗透速度。还有一个老生常谈的问题——安全性数据仍需长期验证。JAK抑制剂类药物的黑框警告(血栓、肿瘤风险)是监管和医生处方的核心顾虑。尽管吉卡昔替尼片机制上有优势,但需大规模真实世界数据证明其风险低于同类产品,否则可能限制市场接受度。其二,纵观泽璟BD历史,在国际化合作方面,尚无经验可循。对于尚处早期研发阶段、已获FDA IND批准的ZG005、ZG006等管线,若参考康方生物AK112高达50亿美元的海外授权案例,考虑BD模式,可通过海外权益出让快速回笼资金。不过,这也将考验泽璟国际化能力,尤其体现在临床开发与BD经验。虽然在临床开发方面,泽璟凭借ZG005、ZG006成功获批FDA IND,已积累与美国监管机构的沟通经验,熟悉申报路径,能够有效降低合作伙伴的后期开发风险。然而在BD方面,泽璟经验明显不足。目前仅完成GS02 TIGIT单抗的国内授权交易,尚未开展与跨国药企的全球性合作。面对ZG006等复杂结构创新药,若把握不当,在国际授权谈判中议价能力不一定能充分体现。这并非不可解决。泽璟可通过多维度策略弥补国际化经验缺口:一方面,可引入具备跨国药企 BD 经验的高管及专业人才,快速提升团队国际化运作能力;另一方面,借助 CRO 机构或专业咨询公司的资源,加速积累行业经验。同样,在授权策略上,可采用分阶段推进模式,比如对早期非核心管线,参考荣昌生物与 Seagen 的合作模式,以技术授权形式快速积累交易经验并回笼资金;对晚期重磅产品如 ZG005,则优先将欧美市场权益授权给跨国药企,换取首付款与里程碑付款,同时保留中国市场自主开发权。E药资本界认为,泽璟若能在2025-2026年关键节点完成1-2笔全球授权交易,将有效验证其BD能力并再度打开市值空间。反之,若因经验不足导致交易条款不利或进度滞后,可能加剧 “重研发、轻变现” 的困境。因此,投资者需重点关注其 BD 团队组建进展,以及 2025 年关键临床数据披露后的合作动态,以此评估潜在风险与收益。总结作为一家小而美药企,泽璟已经逐渐走出了自己的节奏。对比君实生物、荣昌生物等同市值梯队药企,泽璟之所以能凭借5亿规模冲上去,与营收规模占优的它们一较高低,关键就在于差异化的产品定位与高效的协同布局:几乎没有“废管线”,具有差异性且进度领先,基本都能抢占一定市场。即便尚未商业化的产品,经 BD 合作潜力及潜在市场空间评估,前景同样总体向好。更具体来看,泽璟制药的当前市值逻辑源于两点,一是已验证的商业化能力(多纳非尼、重组凝血酶);二是高壁垒管线预期(双/三抗、JAK抑制剂)的双重支撑。不过,未来需关注ZG005/ZG006的临床数据披露及吉卡昔替尼的上市放量节奏。另外,不要忽略,这家药企本质上“科学家底色”浓厚,或也回答了其为何频繁能再创新药竞争中占据先发优势。如董事长盛泽林拥有30余年新药研发经验,曾任职于BMS等跨国药企,并主导全球首个氘代抗肿瘤药物多纳非尼的研发及上市;首席科学官盛泽琪博士曾任安进药物研发高管,主导多款抗体药物的开发;首席医学官吴济生曾负责多个国际多中心临床试验设计……但挑战仍在。当前,泽璟正处于从“小而美”向 “专而强”的战略转型关键期。未来 2-3 年,吉卡昔替尼的商业化成效与双抗管线临床进展,将成为检验其估值合理性的试金石,也决定其能否突破质疑,成为本土创新药企的“新明星”。一审| 黄佳二审| 李芳晨三审| 李静芝精彩推荐CM10 | 集采 | 国谈 | 医保动态 | 药审 | 人才 | 薪资 | 榜单 | CAR-T | PD-1 | mRNA | 单抗 | 商业化 | 国际化 | 猎药人系列专题 | 出海启思会 | 声音·责任 | 创百汇 | E药经理人理事会 | 微解药直播 | 大国新药 | 营销硬观点 | 投资人去哪儿 | 分析师看赛道 | 药事每周谈 | 医药界·E药经理人 | 中国医药手册创新100强榜单 | 恒瑞 | 中国生物制药 | 百济 | 石药 | 信达 | 君实 | 复宏汉霖 |翰森 | 康方生物 | 上海医药 | 和黄医药 | 东阳光药 | 荣昌 | 亚盛医药 | 齐鲁制药 | 康宁杰瑞 | 贝达药业 | 微芯生物 | 复星医药 |再鼎医药|亚虹医药跨国药企50强榜单 | 辉瑞 | 艾伯维 | 诺华 | 强生 | 罗氏 | BMS | 默克 | 赛诺菲 | AZ | GSK | 武田 | 吉利德科学 | 礼来 | 安进 | 诺和诺德 | 拜耳 | 莫德纳 | BI | 晖致 | 再生元
财报
2025-04-30
Roche's Susvimo FDA Approval Marks New Era in Diabetic Macular Edema Treatment Market | DelveInsight
Seven months after the FDA approved the reintroduction of Roche's eye implant Susvimo, the US agency has expanded its approved use to include treatment for diabetic macular edema, the primary cause of blindness related to diabetes. This marks the second approved indication for Susvimo, which was initially cleared in October 2021 as an alternative to frequent eye injections for wet age-related macular degeneration.
LAS VEGAS, April 30, 2025 /PRNewswire/ -- Diabetic macular edema is a complication that develops from diabetic retinopathy, a widespread consequence of diabetes and a leading cause of irreversible vision loss in working-age adults globally. Diabetic retinopathy occurs due to long-term damage to the retina's small blood vessels, leading to fluid leakage and swelling—especially in the macula. As per DelveInsight's analysis, there were about
1.9 million prevalent cases of DME across the 7MM in 2023, with numbers expected to grow at a notable CAGR during the forecast period.
The primary treatment for DME includes intravitreal injections, where the eye is numbed with drops before injecting medication directly into the vitreous humor. Common anti-VEGF drugs used include
AVASTIN, EYLEA, and LUCENTIS. Additionally, corticosteroids are beneficial in cases of DME linked to inflammatory eye conditions and can be delivered via eye drops, oral tablets, or periocular injections to help reduce inflammation. The US FDA approved sustained-release corticosteroid implants for more serious or longer-lasting conditions, are
OZURDEX, RETISERT, and ILUVIEN.
Learn more about the diabetic macular edema treatment @
New Treatment for Diabetic Macular Edema
EYLEA (Regeneron Pharmaceuticals) – Aflibercept is a recombinant fusion protein composed of the VEGF-binding regions derived from the extracellular domains of human VEGF receptors 1 and 2, linked to the Fc segment of human IgG1. It functions as a VEGF trap by binding to circulating vascular endothelial growth factors (VEGFs), thereby neutralizing VEGF-A, VEGF-B, and placental growth factor (PGF). This action inhibits the formation of new blood vessels in the tumor's choriocapillaris. In July 2014, the U.S. FDA approved EYLEA (aflibercept) Injection for treating diabetic macular edema (DME).
Ranibizumab (Genentech) – Marketed as LUCENTIS, ranibizumab is a monoclonal antibody fragment (Fab) derived from the same original mouse antibody as bevacizumab. It is an anti-angiogenic therapy used to treat the "wet" form of age-related macular degeneration (AMD), a leading cause of vision loss in older adults. Ranibizumab has shown comparable effectiveness to bevacizumab. Developed by Genentech, it is marketed in the U.S. by Genentech and internationally by Novartis. The FDA approved ranibizumab for the treatment of DME in 2012.
In February 2025, Roche announced that the FDA had approved Susvimo (ranibizumab injection) 100 mg/mL for treating diabetic macular edema (DME), a major cause of vision loss in adults with diabetes. This approval is based on positive one-year data from the phase III Pagoda trial, which demonstrated that Susvimo offered sustained improvements in vision for individuals with DME, with a safety profile consistent with what is already known for the drug. In the study, patients receiving Susvimo refills every six months experienced vision gains comparable to those receiving monthly intravitreal injections of 0.5 mg ranibizumab (9.6 letters versus 9.4 letters on an eye chart, equivalent to about two lines of vision improvement).
Susvimo delivers a specially formulated version of ranibizumab continuously through the Port Delivery Platform, offering a less frequent dosing alternative compared to other treatments that may require monthly eye injections. The FDA initially approved Susvimo in 2021 for the treatment of neovascular age-related macular degeneration (nAMD). Regulatory reviews in other countries are currently underway.
Learn more about the FDA-approved DME drugs @
Drugs for Diabetic Macular Edema Treatment
Key players, such as
Oculis, Rezolute, AsclepiX Therapeutics, and others, are evaluating their lead candidates in different stages of clinical development, respectively. They aim to investigate their products for the treatment of diabetic macular edema. The DME market has a promising outlook with the emerging therapies. Some of the drugs in the pipeline are
OCS-01, RZ402, AXT107, and others.
DME leads to significant vision loss in diabetics, affecting up to 7.9% of type 1 and 12.8% of type 2 diabetes patients.
AbbVie, in collaboration with
REGENEXBIO, is developing the gene therapy
ABBV-RGX-314. This therapy targets wet age-related macular degeneration, diabetic retinopathy (DR), and other chronic retinal diseases, potentially offering a breakthrough in treating these conditions.
Discover which therapies are expected to grab major DME market share @
Diabetic Macular Edema Market Report
OCS-01 is a high-concentration dexamethasone eye drop developed for diabetic macular edema (DME), utilizing the proprietary Optireach solubilizing platform. This technology enhances drug solubility, allows for higher concentrations, prolongs ocular retention, and improves bioavailability in eye tissues, including the retina.
Recently, in April 2025, Oculis announced the completion of patient enrollment for its Phase 3
DIAMOND-1 and DIAMOND-2 clinical trials evaluating OCS-01 eye drops for diabetic macular edema (DME). These pivotal registration studies aim to support global regulatory filings, including a New Drug Application (NDA) submission and potential approval by the U.S. FDA. Over 800 patients were enrolled across 119 sites in the U.S. and other countries.
The swift completion of enrollment in the DIAMOND program—comprising two double-masked, randomized, multi-center Phase 3 trials—is a significant milestone. These studies are assessing the efficacy and safety of OCS-01 over a 52-week treatment period in patients with DME. Topline results are anticipated in Q2 2026, followed by an NDA submission.
If approved, OCS-01 would be the first topical eye drop treatment for DME, offering a novel therapeutic option for early intervention and for patients who do not adequately respond to anti-VEGF therapies.
RZ402 is an oral small-molecule drug that selectively inhibits plasma kallikrein (PK) for the long-term treatment of DME. By blocking kallikrein activation, RZ402 aims to prevent bradykinin-driven vascular leakage and inflammation. Phase II results revealed a significant reduction in central subfield thickness (CST) across all dosing levels, with improvements of up to ~50 microns compared to placebo. The treatment was well tolerated and showed a favorable safety profile.
AXT107 targets two validated mechanisms for treating retinal vascular diseases: it inhibits the pro-angiogenic receptor VEGFR2 and activates the vessel-stabilizing Tie2 receptor. These effects are mediated through its interaction with integrins αvβ3 and α5β1. AXT107 is formulated as a microparticulate suspension designed for intraocular injection and is currently undergoing Phase I/II clinical trials, according to the company's development pipeline.
Discover more about drugs for DME in development @
Diabetic Macular Edema Clinical Trials
The anticipated launch of these emerging therapies for DME are poised to transform the market landscape in the coming years. As these cutting-edge therapies continue to mature and gain regulatory approval, they are expected to reshape the DME market landscape, offering new standards of care and unlocking opportunities for medical innovation and economic growth.
DelveInsight estimates that the market size for DME is expected to grow from
USD 3 billion in 2023, with a significant CAGR by 2034. Owing to the higher patient pool and higher diabetic macular edema treatment cost, according to the estimates, the United States had the highest market size in DME, i.e.,
~60% of the total market size of DME in the 7MM, in 2023, followed by Germany and Japan.
DelveInsight's analysis forecasts market growth due to the introduction of emerging therapies, expecting a rise in market size during the study period (2020–2034). The anticipated increase in market size is driven by advancements in treatment options, greater healthcare access, and a rising prevalence of the condition, which together foster higher demand for innovative and effective therapies.
DelveInsight's latest published market report, titled as
Diabetic Macular Edema Market Insight, Epidemiology, and Market Forecast – 2034
, will help you to discover which market leader is going to capture the largest market share. The report provides comprehensive insights into the DME country-specific treatment guidelines, patient pool analysis, and epidemiology forecast to help understand the key opportunities and assess the market's underlying potential. The DME market report proffers epidemiological analysis for the study period 2020–2034 in the 7MM segmented into:
Total Prevalent Cases of DME
Total Diagnosed Prevalent Cases of DME
Gender-specific Diagnosed Prevalent Cases of DME
Age-Specific Diagnosed Prevalent Cases of DME
Subgroup-specific Diagnosed Prevalent Cases of DME
The report provides an edge while developing business strategies by understanding trends shaping and driving the 7MM DME market. Highlights include:
10-year Forecast
7MM Analysis
Epidemiology-based Market Forecasting
Historical and Forecasted Market Analysis upto 2034
Emerging Drug Market Uptake
Peak Sales Analysis
Key Cross Competition Analysis
Industry Expert's Opinion
Access and Reimbursement
Download this DME market report to assess the epidemiology forecasts, understand the patient journeys, know KOLs' opinions about the upcoming treatment paradigms, and determine the factors contributing to the shift in the DME market. Also, stay abreast of the mitigating factors to improve your market position in the DME therapeutic space.
Related Reports
Diabetic Macular Edema Epidemiology Forecast
Diabetic Macular Edema Epidemiology Forecast – 2034 report delivers an in-depth understanding of the disease, historical and forecasted diabetic macular edema epidemiology in the 7MM, i.e., the United States, EU5 (Germany, Spain, Italy, France, and the United Kingdom), and Japan.
Diabetic Macular Edema Pipeline
Diabetic Macular Edema Pipeline Insight
– 2025 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key diabetic macular edema companies, including
Mylan Pharmaceuticals, Kodiak Sciences, Celltrion, Exonate, Opthea, AsclepiX Therapeutics, Allgenesis Biotherapeutics, Ascentage Pharma, Rezolute, Ocuphire Pharma, Oxurion, MingSight Pharmaceuticals, Adverum Biotechnologies, among others.
Diabetic Retinopathy Market
Diabetic Retinopathy Market Insights, Epidemiology, and Market Forecast – 2034 report delivers an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key diabetic retinopathy companies, including
Genentech, Inc., Regeneron Pharmaceuticals, Roche, Opthea Limited, Regenxbio, Kodiak Sciences Inc, Ocuphire Pharma, Eisai Co Ltd, Apexian Pharmaceuticals, Oculis, among others.
Diabetic Retinopathy Pipeline
Diabetic Retinopathy Pipeline Insight
– 2025 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key diabetic retinopathy companies, including
Kodiak Sciences, Novartis, Regenxbio Inc., OcuTerra Therapeutics, Ocular Therapeutix, Bayer, RemeGen, Roche, Ocuphire Pharma, Adverum Biotechnologies, Boehringer Ingelheim, Palatin Technologies, Valo Health, EyePoint Pharmaceuticals, Kubota Vision, MingSight Pharmaceuticals, Oxurion, Aerie Pharmaceuticals, AsclepiX Therapeutics, Ocugen, Ashvattha Therapeutics, Stealth BioTherapeutics, among others.
About DelveInsight
DelveInsight is a leading Business Consultant and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve
.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果临床3期上市批准临床2期
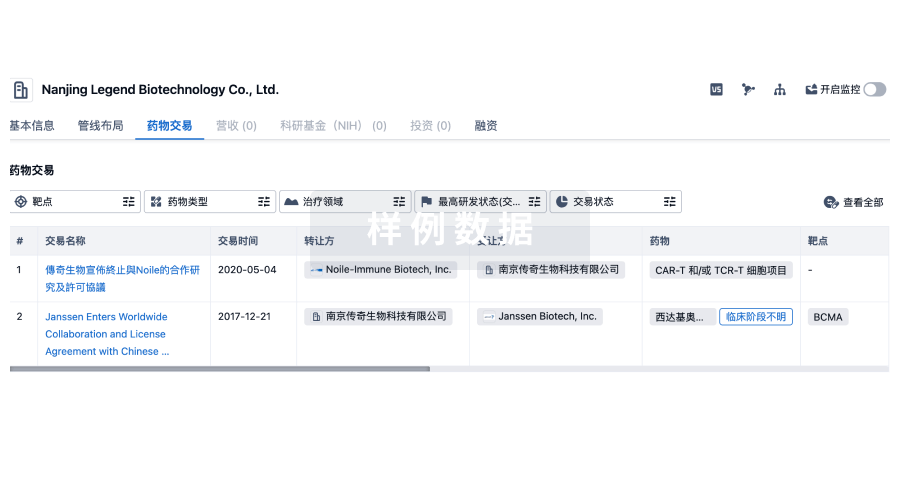
100 项与 亞盛醫藥集團 相关的药物交易
登录后查看更多信息
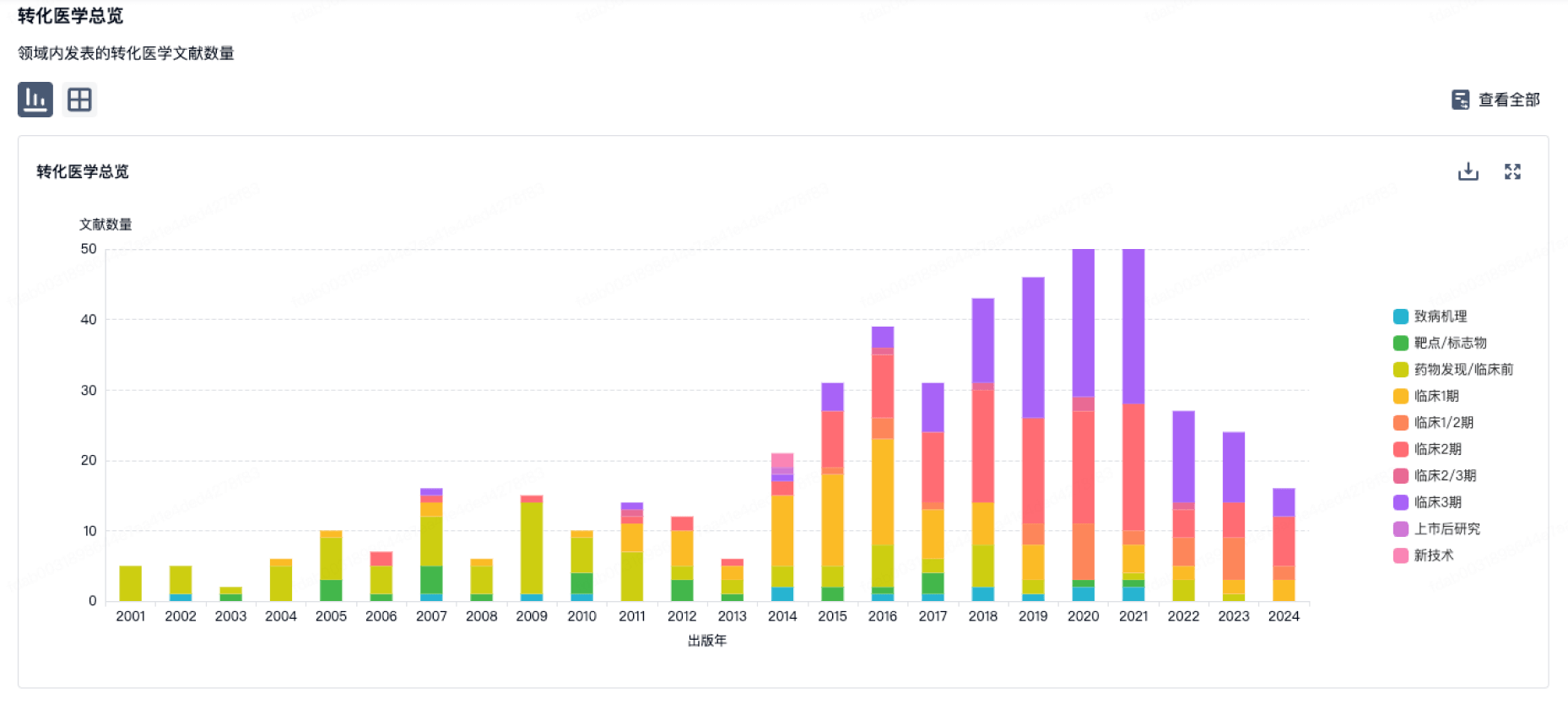
100 项与 亞盛醫藥集團 相关的转化医学
登录后查看更多信息
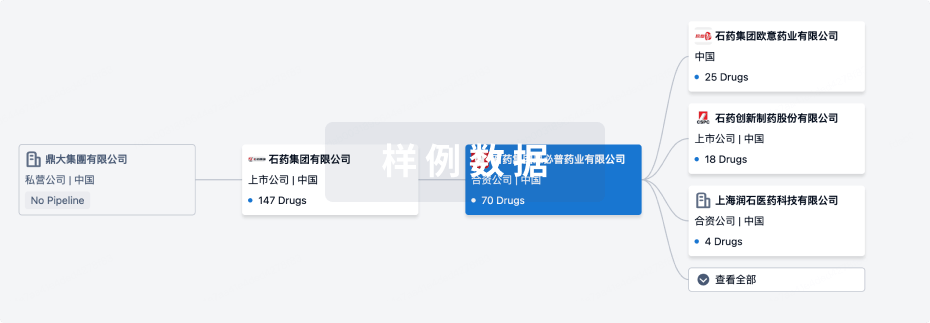
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月03日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
1
5
临床前
临床1期
2
6
临床2期
临床3期
2
1
申请上市
批准上市
1
10
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
奥雷巴替尼 ( Bcr-Abl T315I x c-Kit ) | 加速期慢性骨髄性白血病 更多 | 批准上市 |
力胜克拉 ( Bcl-2 ) | 慢性淋巴细胞白血病 更多 | 申请上市 |
APG-2449 ( ALK x FAK x ROS1 ) | 非小细胞肺癌 更多 | 临床3期 |
阿可替尼 ( BTK ) | 慢性淋巴细胞白血病 更多 | 临床3期 |
Alrizomadlin ( MDM2 x p53 ) | 骨髓增生异常综合征 更多 | 临床2期 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
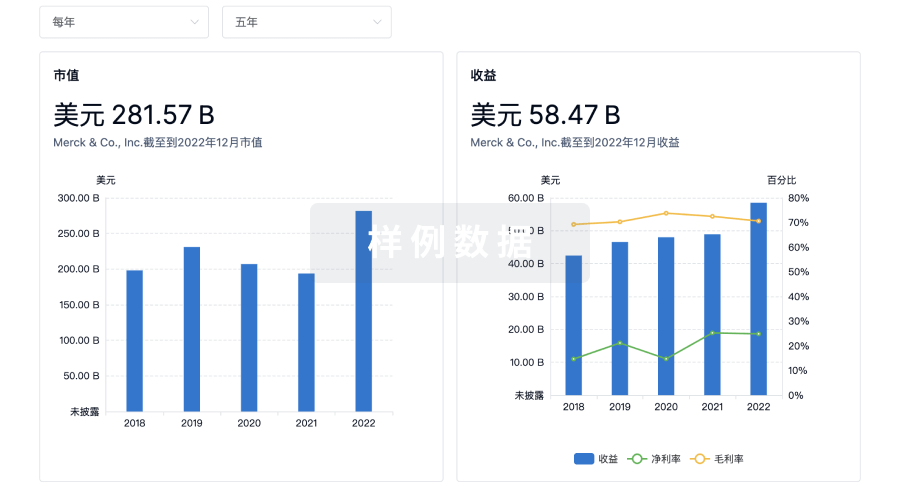
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

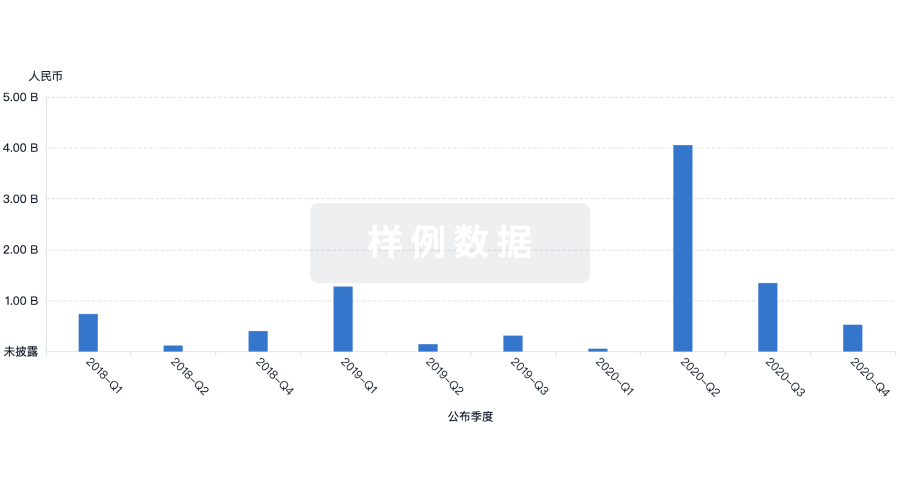
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
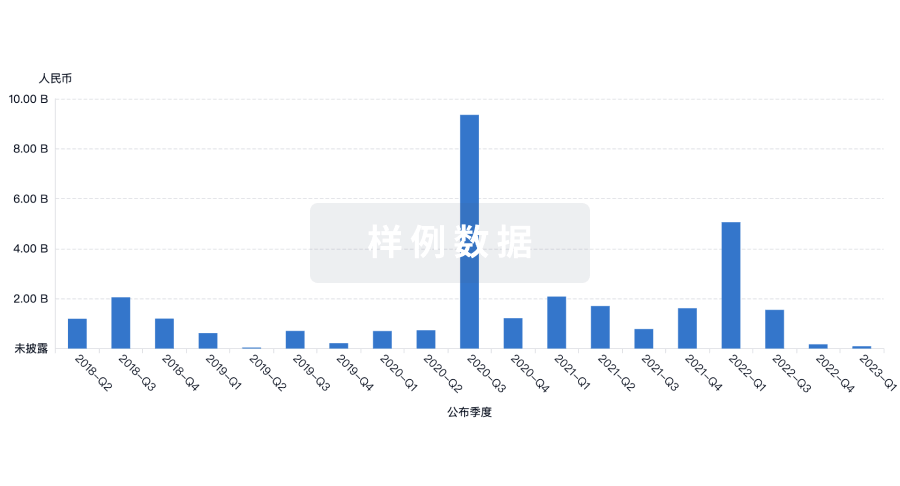
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用




