预约演示
更新于:2025-09-09

Zhejiang University
更新于:2025-09-09
概览
标签
肿瘤
其他疾病
免疫系统疾病
小分子化药
自体CAR-T
蛋白水解靶向嵌合体(PROTAC)
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 87 |
| 蛋白水解靶向嵌合体(PROTAC) | 15 |
| 化学药 | 8 |
| CAR-T | 8 |
| 合成多肽 | 7 |
关联
175
项与 浙江大学 相关的药物作用机制 CDC20抑制剂 [+1] |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2023-02-28 |
作用机制 GIPR激动剂 [+1] |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2022-05-13 |
靶点 |
作用机制 ERα拮抗剂 |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2022-01-10 |
815
项与 浙江大学 相关的临床试验NCT07157631
A Double-Blind, Randomized, Placebo-Controlled, Multi-Center Trial to Evaluate the Efficacy and Safety of Tranexamic Acid in Adult Liver Transplantation (ESTA Trial)
We propose a multi-center randomized trial to test the primary hypothesis that tranexamic acid is superior to placebo on blood loss in adult orthotopic liver transplantation within the initial 24 hours and that tranexamic acid is non-inferior to placebo for a composite of thrombotic events within the initial 7 postoperative days. Secondarily, we will determine whether tranexamic acid is superior to placebo on total postoperative drainage volume and blood product transfusion within the initial 3 postoperative days.
We propose to randomize patients to 2.0 g of tranexamic acid intravenously at the start of surgery or a comparable volume of 0.9% normal saline placebo. Because demonstrating safety will require more patients, our sample size is based on safety. Randomizing 1546 patients will provide 80% power for detecting a non-inferiority margin of 4% with a baseline incidence of 10% for composite thrombotic events within the initial 7 postoperative days.
We propose to randomize patients to 2.0 g of tranexamic acid intravenously at the start of surgery or a comparable volume of 0.9% normal saline placebo. Because demonstrating safety will require more patients, our sample size is based on safety. Randomizing 1546 patients will provide 80% power for detecting a non-inferiority margin of 4% with a baseline incidence of 10% for composite thrombotic events within the initial 7 postoperative days.
开始日期2025-09-29 |
申办/合作机构  河北医科大学第三医院 河北医科大学第三医院 [+16] |
NCT07144020
Donor Derived CD117 CAR-T Cells in the Treatment of Relapsed/Refractory Acute Myeloid Leukemia
A Clinical Study on the Safety and Effectiveness of Donor Derived CD117 CAR-T Cell in the treatment of Relapsed/Refractory Acute Myeloid Leukemia
开始日期2025-09-05 |
申办/合作机构  浙江大学 浙江大学 [+1] |
NCT07091188
A Culturally Adapted Digital Intervention to Promote Maternal Care Utilization Using Multifaceted Approaches (CALCIUM) Among an Ethnic Minority Community in China
Maternal healthcare utilization is crucial for reducing maternal mortality, yet remains low in many underserved regions. The CALCIUM intervention, a culturally tailored, digital platform-integrated intervention, was developed to promote antenatal care (ANC) and institutional deliveries in Liangshan Yi Autonomous Prefecture, an ethnic minority community in China. The CALCIUM intervention was developed to address barriers including limited healthcare awareness, traditional norms and low-quality services. This intervention will evaluate the effectiveness, and cost-effectiveness of improving maternal healthcare utilization and pregnancy outcomes in an ethnic minority community.
开始日期2025-09-01 |
申办/合作机构 |
100 项与 浙江大学 相关的临床结果
登录后查看更多信息
0 项与 浙江大学 相关的专利(医药)
登录后查看更多信息
122,138
项与 浙江大学 相关的文献(医药)2026-12-01·Nano-Micro Letters
Correction: Optimizing Exciton and Charge-Carrier Behavior in Thick-Film Organic Photovoltaics: A Comprehensive Review
作者: Yang, Yaxin ; Yin, Shouchun ; Chen, Hongzheng ; Zhan, Lingling ; Wei, Lu
2026-12-01·Nano-Micro Letters
Optimizing Exciton and Charge-Carrier Behavior in Thick-Film Organic Photovoltaics: A Comprehensive Review
Review
作者: Yang, Yaxin ; Yin, Shouchun ; Zhan, Lingling ; Chen, Hongzheng ; Wei, Lu
Abstract:
Organic photovoltaics (OPVs) have achieved remarkable progress, with laboratory-scale single-junction devices now demonstrating power conversion efficiencies (PCEs) exceeding 20%. However, these efficiencies are highly dependent on the thickness of the photoactive layer, which is typically around 100 nm. This sensitivity poses a challenge for industrial-scale fabrication. Achieving high PCEs in thick-film OPVs is therefore essential. This review systematically examines recent advancements in thick-film OPVs, focusing on the fundamental mechanisms that lead to efficiency loss and strategies to enhance performance. We provide a comprehensive analysis spanning the complete photovoltaic process chain: from initial exciton generation and diffusion dynamics, through dissociation mechanisms, to subsequent charge-carrier transport, balance optimization, and final collection efficiency. Particular emphasis is placed on cutting-edge solutions in molecular engineering and device architecture optimization. By synthesizing these interdisciplinary approaches and investigating the potential contributions in stability, cost, and machine learning aspects, this work establishes comprehensive guidelines for designing high-performance OPVs devices with minimal thickness dependence, ultimately aiming to bridge the gap between laboratory achievements and industrial manufacturing requirements.
2026-02-01·BIOMATERIALS
Self-assembled copper-amino acid nanoleaves for targeted treatment of deep-seated bacterial infections via chemodynamic therapy and cuproptosis-like death
Article
作者: Ni, Yanwen ; Chen, Yongcheng ; Ji, Jian ; Wang, Kaijun ; Li, Yuhang ; Li, Yutong ; Chen, Haojie ; Jin, Qiao
Transition metal ions such as Cu2+ are promising broad-spectrum bactericidal agents. However, transition metal ions are not used to treat deep-seated bacterial infections in clinic owing to easy deactivation by proteins and lack of targeting ability. Herein, hyaluronic acid (HA)-modified copper-N-acetyl-l-cysteine (NAC) nanoleaves (CNH NLs) are developed to treat deep-seated bacterial infections by targeted delivery of Cu2+ to infection sites. Cu-NAC nanoleaves (CN NLs) can be synthesized by coordinate assembly of Cu2+ and NAC, which are further coated with HA to obtained CNH NLs with targeting ability. CNH NLs are stable in neutral physiological environment, while can be easily decomposed in acidic infection sites, leading to rapid release of Cu2+. The released Cu2+ disrupts bacterial membranes, depletes glutathione, generates reactive oxygen species (ROS), and induces cuproptosis-like bacterial death, exhibiting potent activity against both planktonic bacteria and biofilms. The targeted accumulation and excellent therapeutic efficacy of CNH NLs is further confirmed on murine bacterial keratitis and pneumonia models, highlighting their therapeutic potential for deep-seated infections.
1,264
项与 浙江大学 相关的新闻(医药)2025-09-08
·生物世界
撰文丨王聪
编辑丨王多鱼
排版丨水成文
每年全球有 70 万例耐药性疾病导致的死亡,按照目前的趋势,到 2050 年这一数字预计将升至每年 1000 万,其中多重耐药(MDR)革兰氏阴性菌尤其令人担忧。抗菌肽(AMP)是解决耐药性问题的候选药物。据悉,监管机构已批准了 80 多种多肽类药物,还有 550-750 种多肽处于临床或临床前阶段。随着抗生素滥用情况日益严重,发现或生成抗菌肽的需求十分迫切。
2025 年 9 月 3 日,军事医学科学院姜永强、任洪广、刘鹏,国防科技大学黄震及安徽医科大学、华中科技大学、浙江大学、湖南大学的研究人员合作,在 Cell 子刊 Cell Reports 上发表了题为:EBAMP: An efficient de novo broad-spectrum antimicrobial peptide discovery framework 的研究论文。
该研究开发了一种基于 Transformer 的生成式 AI 模型——EBAMP,实现高效的从头设计生成广谱抗菌肽,能够同时对抗细菌和真菌,且具有低毒性和低耐药风险;
多肽是由氨基酸组成的寡聚体或聚合体,通常由 6-50 个氨基酸组成。在过去几十年中,多肽合成和修饰化学技术的进步促进了抗菌肽(AMP)的发现和转化。传统的多肽类药物发现依赖于从自然界中识别功能肽,这极大地限制了候选药物的搜索空间。此外,天然抗菌肽固有的局限性,例如生物活性低和细胞毒性副产物,促使人们研究新型抗菌肽的发现。
噬菌体展示和酵母展示等技术将搜索空间扩展到了序列库。然而,考虑到组成蛋白质/多肽的 20 种标准氨基酸,一个由 50 个氨基酸组成的多肽就有高达 2050 种不同的潜在序列,即使对于最先进的方法来说,筛选整个序列库也是一项无法完成的任务。为解决传统多肽类药物发现方法存在的问题,研究人员提出了机器学习和深度学习模型,以实现快速且准确的多肽类药物发现。
为解决现有的抗菌肽(AMP)设计生成方法的局限性,研究团队提出了一种名为 EBAMP 的两阶段生成-辨别框架,用于从头设计广谱抗菌肽,以同时对抗细菌和真菌。
EBAMP 结合了基于 Transformer 的生成式 AI 模型和先进的基于特征的筛选方法,以探索多肽空间并选择多目标候选多肽。对 256 个设计生成的抗菌肽序列的进一步实验测试表明,其中 96 个抗菌肽(37.5%)具有杀菌能力。排名前十的抗菌肽序列表现出低细胞毒性、低溶血性以及对多重耐药菌和真菌的强抗菌效果(2 μg/mL 浓度下)。
在体内小鼠全层皮肤伤口感染模型中,设计生成的抗菌肽对鲍曼不动杆菌(细菌)和耳念珠菌(真菌)显示出抑制作用,治疗效果与抗生素相当,但耐药性倾向更低。丙氨酸替代分析和分子动力学及一步揭示了这些抗菌肽的功能关键位点。
该研究的核心发现:
EBAMP 是一种用于从头设计生成广谱抗菌肽的有效框架;
生成的抗菌肽表现出低最小抑菌浓度(2 μg/mL)以及低毒性、低耐药风险;
在生成的 256 种候选抗菌肽中,有 37.5% 表现出实验性的抗菌活性。
总的来说,EBAMP 展示了大型生成式模型在广谱抗菌肽发现中的应用,并有望解决抗生素耐药性问题。
论文链接:
https://www-cell-com.libproxy1.nus.edu.sg/cell-reports/fulltext/S2211-1247(25)00986-6
设置星标,不错过精彩推文
开放转载
欢迎转发到朋友圈和微信群
微信加群
为促进前沿研究的传播和交流,我们组建了多个专业交流群,长按下方二维码,即可添加小编微信进群,由于申请人数较多,添加微信时请备注:学校/专业/姓名,如果是PI/教授,还请注明。
点在看,传递你的品味
2025-09-08
通过将高效细胞毒药物与高选择性单克隆抗体相结合,抗体偶联药物(ADC)已成为目前极具前景且迅速发展的新型抗癌疗法之一。9月6日—9日,2025年世界肺癌大会(WCLC2025)在西班牙巴塞罗那举行,齐鲁制药在大会上公布了 B7-H3 ADC新药QLC5508治疗既往经治广泛期小细胞肺癌(ES-SCLC)的Ⅰ期临床研究更新数据。该研究结果作为最新突破摘要(Late-Breaking Abstract,LBA)被大会录用为口头报告,由国际肺癌研究协会 (IASLC) 理事会2025~2027届主席、同济大学附属东方医院周彩存教授在“小细胞肺癌ADC新药(Novel ADCs in SCLC)”专场重磅发布。
周彩存教授现场报告
作为全球肿瘤学界极具影响力的盛会之一,世界肺癌大会一直是肺癌及其他胸部肿瘤领域前沿进展的重要学术交流平台。每年,来自世界各地的权威专家学者齐聚于此,探讨最新研究成果、分享临床实践经验,思考未来发展方向。
0A06.02. Safety and Efficacy of QLC5508 in Previously Treated Patients with Small Cell Lung Cancer: Updated Data from a Phase 1 Study
QLC5508治疗既往经治广泛期小细胞肺癌(ES-SCLC)I期临床研究疗效及安全性的更新数据
报告环节:0A06. Novel ADCs in SCLC
报告形式:Oral
报告时间:September 7, 2025, 04:57 PM-05:07PM
QLC5508(MHB088C)是一款基于SuperTopoi™ ADC平台开发的创新B7-H3靶向抗体偶联药物。今年 5 月,齐鲁制药以13.45亿元的价格从明慧医药引进了该产品大中华区权益。Ⅰ期临床试验ES-SCLC患者初步数据在此前举行的2025年美国临床肿瘤学会(ASCO)以口头报告形式初步公布,在既往经治的ES-SCLC患者中安全性和耐受性良好,同时也显示出了令人鼓舞的抗肿瘤活性。作为中国医药产业创新的杰出代表,齐鲁制药凭借最新更新的数据活跃国际学术舞台,充分彰显了中国在全球创新药物研发领域的崛起。
新数据展现临床潜力
联合用药开发值得期待
B7-H3(CD276)是B7家族的一员,在T细胞反应中起免疫调节作用,被认为是癌症免疫治疗的潜在新靶点。多项研究证实,B7-H3在大多数正常组织中低表达,广泛表达于前列腺癌、胰腺癌、乳腺癌、结直肠癌、肺癌和卵巢癌等多种人类恶性肿瘤。此外,B7-H3还与肿瘤细胞增殖、转移和治疗耐药相关及患者预后不佳有关。
QLC5508通过特异性结合肿瘤细胞表面的B7-H3,将强效的拓扑异构酶抑制剂有效载荷精准递送至肿瘤内部,从而实现高效的抗肿瘤活性。资料显示,其有效载荷SuperTopoiTM的效力比喜树碱(Dxd)高5至10倍。
此次WCLC2025大会,发布了Ⅰ期临床试验ES-SCLC患者生存和安全性的最新数据。截至2025年6月13日,在1.6 mg/kg Q2W、2.0 mg/kg Q2W和 2.4 mg/kg Q3W三个剂量水平共入组106例SCLC患者。其中近半数(47.2%)患者曾接受过二线或二线以上治疗,超半数患者(58.5%)既往接受过免疫治疗。安全性方面,最常见的≥3 级治疗相关不良事件(TRAE)为中性粒细胞计数减少(17.0%)和白细胞计数减少(10.4%)。
在疗效方面,QLC5508在1.6 mg/kg Q2W、2.0 mg/kg Q2W 和 2.4 mg/kg Q3W 三个剂量组确认的客观缓解率(ORR)分别为21.4%、42.2%、43.3%,疾病缓解率(DCR)分别为89.3%、84.4%、100%,中位无进展生存期(mPFS)分别为 5.55 个月、5.95 个月和 5.52 个月,中位总生存期(mOS)分别为 11.50 个月、11.73 个月和 11.50 个月。综上所述,QLC5508 在既往经治的 ES-SCLC 患者中显示出了优越的安全性、突出的抗肿瘤活性和长期的生存获益,2.0 mg/kg Q2W将作为后续进一步临床试验的推荐剂量。
目前,QLC5508正在进行包括肺癌、前列腺癌、食管癌等多个瘤种在内的Ⅱ、Ⅲ期临床试验。值得关注的是,在B7家族中除了B7-H3,还有包括B7-H1(PD-L1)、B7-1(CD80)、B7-2(CD86)等多个免疫检查点分子,尤其围绕B7-H1(PD-L1)已经有众多PD-1/L1产品获批上市,集中了肿瘤免疫治疗(IO)领域全球瞩目的“重磅炸弹”,众多药物之间的联合治疗潜力也备受行业期待。
当前,肿瘤免疫治疗已迎来2.0新时代,QLC5508未来有望联合齐鲁制药自研的已上市创新药PD-1/CTLA-4双功能组合抗体齐倍安®(QL1706,艾帕洛利托沃瑞利单抗),构建IO2.0+ADC的肿瘤治疗新格局。
全球创新惠及患者
让医药创新更具温度
聚焦未被满足的临床需求,QLC5508在全球开发取得的学术里程碑,以及目前展现出的细分赛道创新和联合用药潜力,仅仅是齐鲁制药坚持“用科技表达爱”的一个缩影。无论是外部授权引进还是内部自主研发,齐鲁制药以“有温度的创新”为核心理念,将科技创新与人文关怀深度融合,走出了一条独具特色的高质量发展之路。这条道路既承载着对生命健康的敬畏,也彰显着中国医药企业的责任担当。
科技创新从来不是空中楼阁,而是需要战略定力与资源沉淀的厚积薄发。齐鲁制药的研发投入强度从十年前的5%~8%提升至10%~12%,看似微小的百分比跃升,实则是企业战略重心的位移。2024年43.8亿元的研发投入,以及“十四五”期间超200亿元的累计投入承诺,勾勒出企业以真金白银护航创新的坚定姿态,诠释了企业的创新决心。
这种战略定力更体现在人才体系上。齐鲁制药5200余人的专职研发团队中,博士占比达34.4%,这支具有国际视野的科研梯队,与清华大学、浙江大学等国内顶尖学府,以及纽约纪念斯隆—凯特林癌症研究中心、美国国家癌症研究所(NCI)等国际权威机构开展合作。通过构建产学研用协同创新生态,齐鲁制药正突破一个个关键技术瓶颈,在创新药研发的深水区破浪前行。
在肿瘤治疗领域,齐鲁制药已形成多靶点、多机制的创新药管线布局。2023年6月获批上市的伊鲁阿克片(启欣可®)作为唯一一个同类药品临床研究数据全部在中国完成的ALK抑制剂,历经十年研发,中位无进展生存期达45.9个月,其疗效与安全性数据更贴合国内患者临床特征,上市首年即惠及超万名患者。
更具里程碑意义的是2024年9月获批的艾帕洛利托沃瑞利单抗注射液。作为全球首创的PD-1/CTLA-4双功能组合抗体,该药物依托齐鲁制药全球首创的MabPair®技术平台,实现同一细胞系覆盖两个靶点、表达两种抗体,且PD-1和CTLA-4两种单抗以2:1黄金比例结合,安全性更高、毒性更低、耐受性更佳、治疗效果叠加的双免疫疗法,为宫颈癌患者带来显著生存获益。
在生物药开发方面,齐鲁制药构建起涵盖ADC、双抗/多抗等前沿技术的全链条平台。如其注射用QLS5132作为针对CLDN6靶点的国内首个ADC药物,填补了国内该靶点创新药研发的空白,打破了国外在这一前沿领域的技术领先优势,为我国肿瘤靶向治疗开辟了新的路径;QLS4131注射液作为BCMA/GPRC5D/CD3三抗药物,在多发性骨髓瘤治疗领域已展现突破性疗效,4月底新增的系统性红斑狼疮适应症获批临床,进一步拓展了其应用范围。
作为立志于向创新型国际化迈进的中国医药企业,齐鲁制药依托中美六大研发中心的协同网络,全面推进创新药全球开发。目前,齐鲁制药已有80余项在研创新药物项目,其中20个处于临床阶段,今年6个获批临床的项目中4个实现中美双报。聚焦未被满足的临床需求,齐鲁制药正在加速重大疾病领域的布局,为临床急需、患者负担重的生命健康挑战提供突破性的用药解决方案。
来源:齐鲁制药
(推广)
创新药“狂飙”与CXO“转型”,BD潮涌下的产业变局与新机
第十一批国采允许复活,报价跟进最高有效申报价
1.55亿底价转让!"国药系"连续7次出手,边买边卖意欲何为?
www.yyjjb.com.cn
洞悉行业趋势
长按关注医药经济报
《中国处方药》
学术公众号
聚焦药学学术和循证研究
长按关注中国处方药
《医药经济报》
终端公众号
记录药品终端产经大事件
长按关注21世纪药店
抗体药物偶联物ASCO会议临床1期临床结果临床2期
2025-09-06
·药时空
呼吸道合胞病毒(RSV)是导致5岁以下婴幼儿及65岁以上老年人严重下呼吸道感染的重要病原体。RSV分为A和B两个亚型,其融合蛋白(F蛋白)以同源三聚体形式暴露于病毒表面,介导病毒与宿主细胞膜融合,是疫苗研发和抗体筛选的关键靶点。F蛋白在膜融合过程中由融合前高能态(pre-F)不可逆地转变为融合后低能态(post-F)。研究表明,pre-F状态下的Ø表位和V表位是F蛋白最强的中和抗体表位,而在post-F状态下,这些表位被遮挡,导致其诱导的中和抗体效能远低于pre-F状态。
目前获批上市的RSV疫苗(如GSK、Pfizer和Moderna公司研发的产品),以及进入临床试验阶段的以F蛋白为主要免疫原的候选疫苗,普遍采用点突变、引入二硫键及增强静电相互作用等策略,以稳定F蛋白于融合前(pre-F)构象。然而,这类基于pre-F的疫苗在储存过程中仍面临抗原构象由pre-F向融合后(post-F)不可逆转变的挑战,导致其保护效力显著下降。此外,现有以F蛋白为靶点的RSV疫苗多数仅针对单一A亚型,或通过简单混合A、B两种亚型抗原实现免疫,这可能引发免疫应答不均衡的问题。近年B亚型毒株的感染比例逐渐上升,因此研发更具广谱性的RSV疫苗已成为临床亟需。同时,疫苗相关性呼吸道疾病(Vaccine-associated enhanced respiratory diseases,VAERD)依旧是RSV疫苗研发中难以规避的重要挑战。
8月31日,中国科学院微生物研究所齐建勋研究员、高福院士以及王奇慧研究员在eBioMedicine 期刊联合发表了题为“Rational design of respiratory syncytial virus dimeric F-subunit vaccines in protein and mRNA forms”的研究论文。该研究基于免疫聚焦策略,借助人AI设计,获得了仅保留II、V和Ø表位的优势免疫原模块,最大限度的去除非中和表位。研究团队通过串联二聚体的构建策略,将A、B两种亚型的优势免疫原模块融合,开发出覆盖双亚型的融合抗原 scDimer AB。在此设计理念的指导下,他们成功研制出RSV单链二聚体重组亚单位蛋白疫苗及mRNA疫苗,突破了现有RSV疫苗设计的关键技术瓶颈。
生化数据显示,scDimer AB对Ø表位抗体Am22、V表位抗体CR9501及II表位抗体Palivizumab的亲和力均与经典构象稳定化抗原DS-Cav1相当;但其与III表位抗体MPE8的结合能力较弱,同时不与I表位抗体4D7和IV表位抗体101F发生结合。这一独特的结合特性精准实现了对优势中和表位的免疫聚焦,充分体现了设计理念的初衷。
在蛋白质热稳定性分析中,scDimer AB的Tm值达到83.27℃,显著高于已报道的RSV疫苗。在4℃保存100天或37℃保存28天后,其II、V及Ø表位与对应特异性抗体的结合能力仍超50%,充分展示出其卓越的结构稳定性与应用潜力
动物实验表明,scDimer AB诱导的pre-F结合抗体水平显著高于post-F结合抗体,与免疫DS-Cav1的小鼠相当,而post-F结合抗体水平则低于DS-Cav1,验证了其免疫聚焦效应。在中和抗体方面,scDimer AB无论以蛋白疫苗还是mRNA疫苗形式接种,均能诱导与DS-Cav1相当水平的中和抗体,且可中和RSV A型和B型毒株。棉鼠免疫攻毒保护实验显示,免疫组体内未检测到残留活病毒,表明疫苗可实现彻底的病毒清除。在细胞免疫方面,两种疫苗形式均能诱导较强的T细胞免疫反应。进一步地,序贯免疫(先进行mRNA免疫,后经鼻腔给予蛋白疫苗)相比单独mRNA疫苗免疫,动物鼻腔、肺灌洗液及血清中的IgA抗体水平显著提升,而IgG水平不变,提示联合免疫策略能有效增强黏膜免疫反应,有助于在呼吸道前端阻断病毒入侵,为RSV疫苗的设计与免疫策略优化提供了新思路。
Figure:基于RSV F蛋白的单链二聚体蛋白疫苗设计
综上所述,本研究提出了一种全新的RSV抗原设计策略,兼具免疫聚焦性、同时覆盖A型和B型基因型的广谱性、卓越的蛋白质稳定性以及强大的免疫原性。该策略不仅显著提升了疫苗的免疫效果,也为其他病毒疫苗的研发提供了新的思路与可借鉴的路径。
中国科学院微生物研究所助理研究员李晶,与中国科学院微生物研究所联合培养博士生马雪慧(浙江大学)、徐泽鹏(澳门大学)、博士生郭文静,温州医科大学硕士生陈佳钦,贵州省烟草科学研究院副研究员郭玉双为论文共同第一作者。齐建勋研究员、高福院士和王奇慧研究员为共同通讯作者。该研究获国家重点研发计划、国家自然科学基金等项目资助。
原文链接:https://pubmed-ncbi-nlm-nih-gov.libproxy1.nus.edu.sg/40886405/
识别微信二维码,可添加药时空小编
请注明:姓名+研究方向!
疫苗信使RNA临床研究
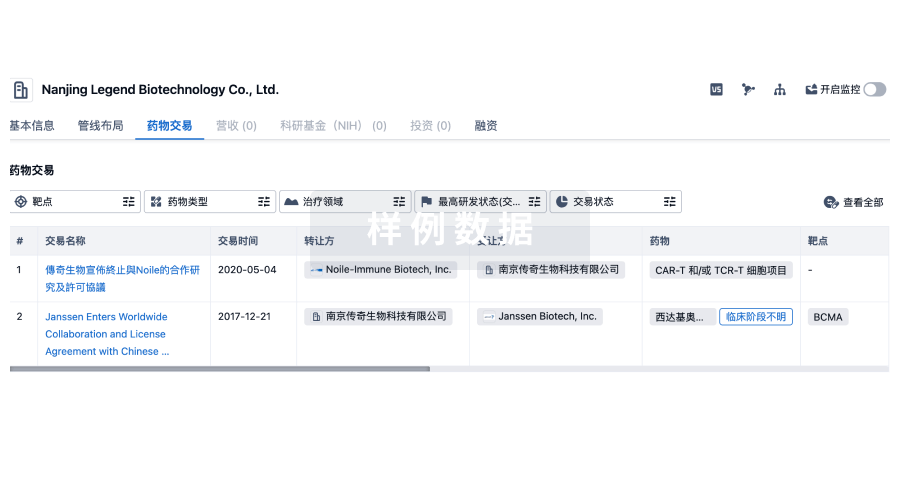
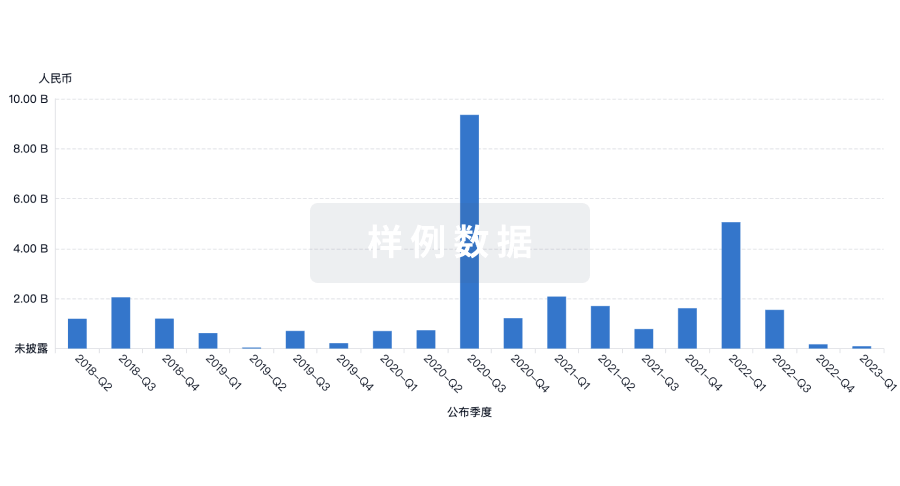
100 项与 浙江大学 相关的药物交易
登录后查看更多信息
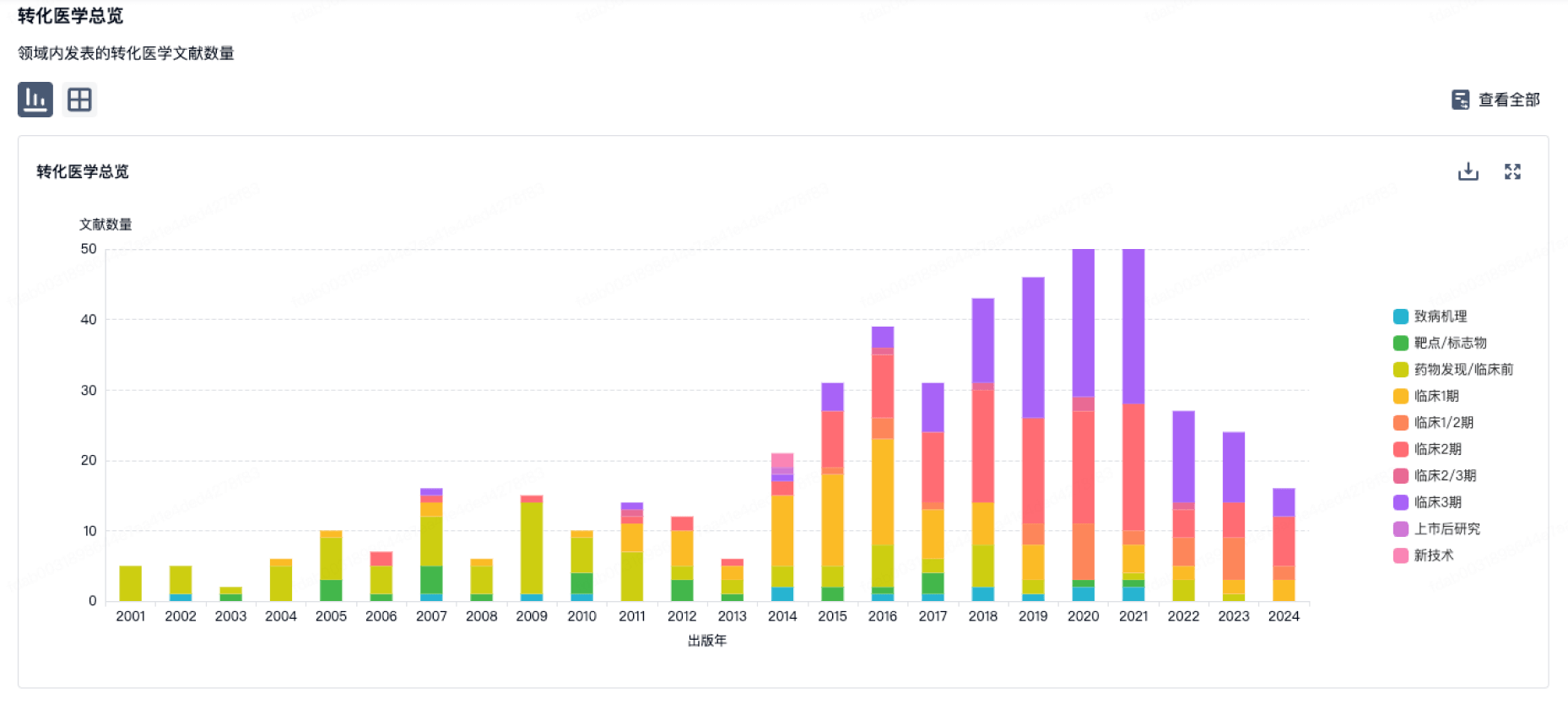
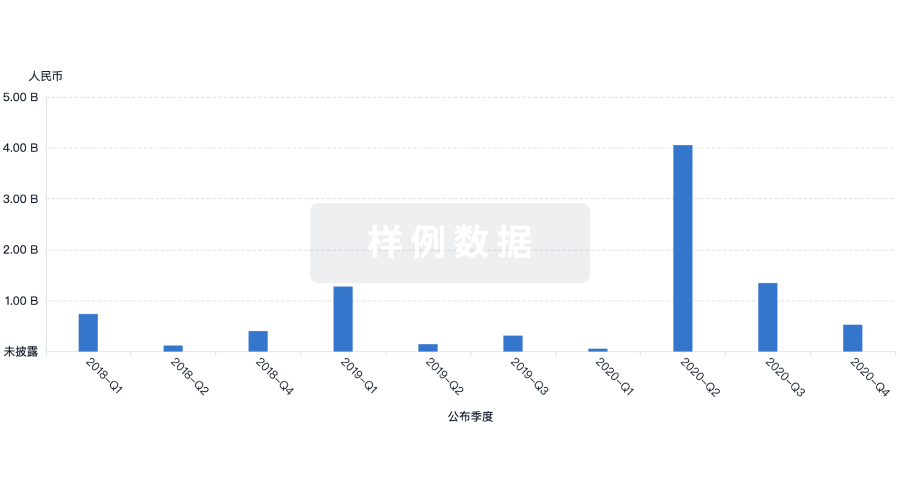
100 项与 浙江大学 相关的转化医学
登录后查看更多信息
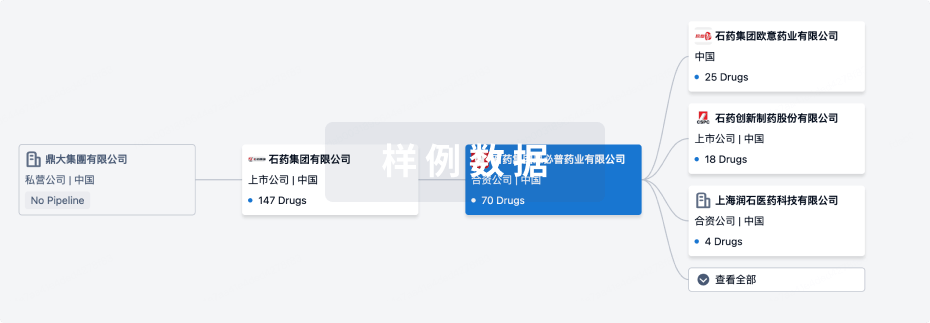
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月05日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
55
94
临床前
临床申请批准
2
22
临床1期
临床2期
2
1
临床3期
其他
31
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
紫杉醇 ( Tubulin ) | 高级别胶质瘤 更多 | 临床3期 |
辛萸贴片 | 复发性阿弗他溃疡 更多 | 临床2期 |
菊花舒心片 | 稳定型心绞痛 更多 | 临床2期 |
AL58805 ( PI3Ks x mTOR ) | 头颈部肿瘤 更多 | 临床1期 |
Anti-CD70 UCAR-T(Zhejiang University) ( CD70 ) | 晚期恶性实体瘤 更多 | 临床1期 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
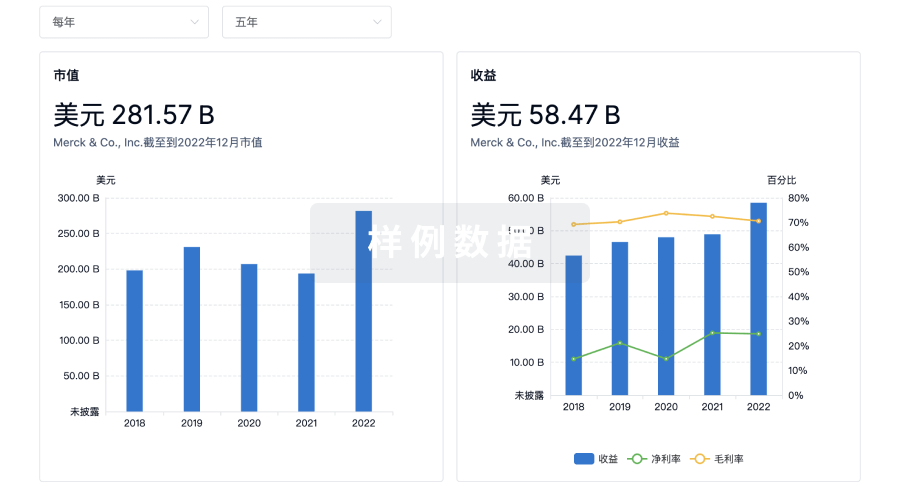
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用