预约演示
更新于:2025-08-15

RemeGen Co., Ltd.
更新于:2025-08-15
概览
标签
肿瘤
皮肤和肌肉骨骼疾病
消化系统疾病
ADC
Fc融合蛋白
融合蛋白
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| ADC | 12 |
| 双特异性抗体 | 7 |
| 单克隆抗体 | 5 |
| 融合蛋白 | 4 |
| Fc融合蛋白 | 2 |
关联
32
项与 荣昌生物制药(烟台)股份有限公司 相关的药物作用机制 HER2拮抗剂 [+1] |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2021-06-08 |
作用机制 APRIL抑制剂 [+2] |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2021-03-09 |
靶点 |
作用机制 PD-1抑制剂 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2019-12-26 |
107
项与 荣昌生物制药(烟台)股份有限公司 相关的临床试验NCT07105215
A Multicenter Phase I/II Clinical Study to Evaluate the Safety and Efficacy of RC278 for Injection in the Treatment of Locally Advanced Unresectable or Metastatic Malignant Solid Tumor
The primary objective is to evaluate the safety and tolerability of RC278; determine the maximum tolerated dose (MTD) and/or maximum administered dose (MAD) of RC278; and determine the recommended phase 2 dose (RP2D), and assess the efficacy of RC278 at the RP2D dose;
开始日期2025-09-30 |
申办/合作机构 |
NCT07100184
Efficacy and Safety of Disitamab Vedotin in Combination With Radiotherapy for Patients With HER2-Expressing High-Risk or Very High-Risk Non-Muscle Invasive Bladder Cancer
This study is an open, single-arm, single-center exploratory clinical study to explore the efficacy and safety of Disitamab Vedotin (RC-48) in combination with radiotherapy for the treatment of patients with HER2-expressing high-risk or very high-risk non-muscle invasive bladder cancer (NMIBC) without visible foci of disease after transurethral resection of bladder tumor (TURBT). The study plans to enroll 30 patients with high or very high risk HER2-expression NMIBC without visible lesions after TURBT. The study includes a screening period, a treatment period, and a survival follow-up period. This is a single-center study conducted at the Peking University First Hospital, and the PI is Prof. CuiJian Zhang.
开始日期2025-09-01 |
申办/合作机构 北京大学第一医院 [+1] |
NCT06962865
A Randomized, Open, Controlled, Multicenter Phase II Clinical Study of RC108 in Combination With Furmonertinib Versus Furmonertinib for the First-Line Treatment of EGFR-Mutated Combined MET-Positive Unresectable Locally Advanced or Recurrent Metastatic NSCLC
Evaluate the efficacy and safety of RC108 in combination with Furmonertinib against Furmonertinib for treatment of EGFR mutation combined with MET-positive unresectable locally advanced or recurrent metastatic NSCLC
开始日期2025-06-30 |
申办/合作机构 |
100 项与 荣昌生物制药(烟台)股份有限公司 相关的临床结果
登录后查看更多信息
0 项与 荣昌生物制药(烟台)股份有限公司 相关的专利(医药)
登录后查看更多信息
40
项与 荣昌生物制药(烟台)股份有限公司 相关的文献(医药)2025-08-01·INTERNATIONAL JOURNAL OF BIOLOGICAL MACROMOLECULES
Total flavonoids from Cortex Juglandis Mandshuricae inhibits pancreatic lipase activity and reduces fat accumulation in vivo
Article
作者: Wang, Yang ; Tian, Jinlong ; Yu, Hui ; Wang, Jiaxin ; Zhao, Pan ; Gao, Xinyu ; Yang, Xueqi ; Sun, Zihui
Pancreatic lipase (PL) is an essential metabolic key enzyme involved in triglyceride metabolism, hydrolysis and absorption. The aim of this study was to evaluate the inhibitory effects of total flavonoids from Cortex Juglandis Mandshuricae (TFC) on PL, alleviate lipid accumulation, and their possible interaction mechanisms in vitro and in vivo. The results showed that TFC had a significant inhibitory effect on PL. The interaction of TFC-PL complexes proceeded spontaneously, where the hydrophobic interactions was the main factor in the action. TFC induced static quenching of PL fluorescence and could alter the secondary structure of PL. In vivo, TFC significantly inhibited the lipid absorption (P < 0.05) and promoted the excretion (P < 0.05) in orally-administered lipid-containing rats. In addition, administration of TFC ameliorated liver and adipose tissue damage and inhibited lipid uptake in mice fed high-fat diets. More importantly, TFC significantly reduced the expression of PL and genes related to pancreatic lipase in pancreatic tissues (P < 0.05). The study suggests that the lipid-lowering effect of TFC may be through reducing PL activity and thereby inhibiting lipid uptake.
2025-07-01·BRITISH JOURNAL OF OPHTHALMOLOGY
Simultaneous inhibition of fibroblast growth factor-2 and vascular endothelial growth factor-a with RC28-E in diabetic macular edema: a phase 2 randomised trial
Article
作者: Zhang, Ming ; Song, Zongming ; Chen, He ; Liu, Xinyu ; Gao, Lei ; Sun, Bin ; Fang, Jianmin ; Wang, Wenxiang ; Zhuang, Wenjuan ; Gu, Xingwang ; Zhang, Wenfei ; Sun, Xuguang ; Dai, Hong ; Chen, Youxin ; Li, Lin ; Cheng, Shiyu
Objective:
To compare different doses and dosing regimens of RC28-E, a novel bispecific antibody that simultaneously binds vascular endothelial growth factor-A (VEGF-A) and fibroblast growth factor-2 (FGF-2), with conbercept in patients with diabetic macular edema (DME).
Design:
Prospective, randomised, active comparator-controlled, open-label, multicentre, phase 2 clinical trial.cente
Participants:
The trial enrolled patients aged 18 years or older with centre-involving DME, best-corrected visual acuity (BCVA) of 73 to 24 Early Treatment Diabetic Retinopathy Study (ETDRS) letters, and central subfield thickness (CST) of 300 µm or more.
Methods:
Patients were assigned randomly to one of five treatment regimens: 1.0 mg RC28-E for three initial monthly doses and then every 8 weeks (1.0mgQ8); 1.0 mg RC28-E for five initial monthly doses and then on a pro re nata (PRN) basis (1.0mgPRN); 2.0 mg RC28-E for three initial monthly doses and then every 8 weeks (2.0mgQ8); 2.0 mg RC28-E for five initial monthly doses and then on a PRN basis (2.0mgPRN); or 0.5 mg conbercept for three initial monthly doses and then on a PRN basis. Assessments were made at baseline and every 4 weeks thereafter.
Main outcome measures:
The primary endpoint was the change in BCVA compared with baseline at 24 and 52 weeks. Secondary endpoints included the change in CST from baseline at 52 weeks; the proportion of patients who gained/lost ≥15 letters, ≥10 letters and >0 letter in BCVA; and the number of injections and safety outcomes.
Results:
The trial enrolled 156 patients. Mean improvements in BCVA in the RC28-E groups at week 24 were 7.1, 11.0, 7.4 and 10.5 letters for 1.0mgQ8, 1.0mgPRN, 2.0mgQ8 and 2.0mgPRN regimens, respectively, versus 9.7 letters for the conbercept group (p=0.146). By week 52, the RC28-E groups exhibited respective mean BCVA enhancements of 5.5, 9.5, 9.2 and 9.7 letters, compared with 8.4 letters of the conbercept group (p=0.469). Mean reductions in CST in the RC28-E groups at week 52 were −163.2 µm, −136.9 µm, −142.5 µm and −153.6 µm, versus −160.7 µm for the conbercept group (p=0.948). The Per Protocol Set analysis indicated that at 24 weeks, the BCVA improvement in the 2.0mgPRN group was significantly greater than that in the conbercept group (14.0 vs 9.8, p=0.019). In patients with poor baseline glycaemic control (HbA1c ≥7.5%), the 2.0mgPRN group showed greater BCVA improvement than the conbercept group (14.4 vs 4.2, p=0.039) at week 52. During the maintenance phase, the 2.0mgPRN group had fewer injections (2.8, 95% CI 1.8 to 3.7) compared with the conbercept group (4.4, 95% CI 3.5 to 5.2). RC28-E was generally well tolerated. The incidence of ocular adverse events in study eyes was comparable between RC28-E groups (22.6% in 1.0mgQ8 group, 26.7% in 1.0mgPRN group, 34.4% in 2.0mgQ8 group, 25.0% in 2.0 mg PRN group) and conbercept group (32.3%). The number of ocular serious adverse events was 1 (1.0mgQ8), 0 (1.0mgPRN), 1 (2.0mgQ8), 2 (2.0mgPRN) and 0 (conbercept).
Conclusions:
Intravitreous RC28-E improved BCVA and CST in eyes with centre-involved DME. Compared with conbercept, the 2.0mgPRN regimen of RC28-E was recommended due to its superior efficacy in improving vision particularly for patients with poor glycaemic control, fewer treatment injections during the maintenance phase and comparable safety profile.
Trial registration number:
NCT04782115.
2025-06-01·INTERNATIONAL JOURNAL OF BIOLOGICAL MACROMOLECULES
Enhancing activity and stability of a GH8 chitosanase through conserved N-terminal and peripheral residue mutations for bioactive chitooligosaccharide production
Article
作者: Li, Yuanying ; Liao, Guiyan ; Wang, Xiao ; Qin, Qijian ; Fang, Wenxia ; Duan, Lian ; Jiang, Yongqiang ; Yu, Yi ; Wu, Chen ; Zhang, Yiwen ; Tong, Lige ; Wang, Bin
Chitosan, the second most abundant biopolymer after cellulose, has vast application potential. However, its high viscosity and poor solubility have limited its full utilization. Chitosan degradation primarily depends on GH46 family chitosanases, while the more stable GH8 family chitosanases have received less attention. This study, for the first time, reveals the critical role of the conserved N-terminal region in the catalytic activity and substrate binding of the GH8 family chitosanase BcCn8A using truncation mutagenesis and molecular dynamics simulations. Through evolutionary analysis and computationally assisted semi-rational design, the optimized mutant BcCn8A-ΔN4-V319L was obtained, showing a 310 % increase in specific activity and a 5 °C increase in optimal temperature. The engineered enzyme efficiently hydrolyzes chitosan into chitooligosaccharides (COSs) with antioxidant and anti-browning properties, making it suitable for applications like juice preservation. This work provides new insights into the regulatory roles of the N-terminal region and distal amino acid residues in GH8 family chitosanases, advancing their potential in functional oligosaccharide production.
4,714
项与 荣昌生物制药(烟台)股份有限公司 相关的新闻(医药)2025-08-15
WEEKLY REPORT
08/15
2025
产业简报
本期导读
本周要闻
产业洞察
产业研报
近期活动
最新课程
本 周 要 闻
SHINE CONSULTANT
行业快讯
News Flashes
中国抗体与中山大学香港高等研究院就生物医药创新研发等达成合作
中山大学香港高等研究院学术委员会委员聘任暨联合实验室揭牌仪式12日在港举行,未来将通过与世界知名高校教授建立联合实验室的方式,开展“加盟+合作”的柔性引才工作。
当日,中国抗体制药有限公司(简称“中国抗体”)与中山大学香港高等研究院有限公司(简称“中山大学香港高等研究院”)宣布签订全面战略合作协议(简称“合作协议”)。双方将整合科研与产业资源,携手推进生物医药创新研发与临床转化,为全球患者带来更高效的治疗方案。
根据合作协议,合作内容涵盖联合科研、设施资源共享、全链条技术支持、药物研发以及培训与知识交流5个领域,双方将推动培训计划及人员交流,提升针对衰竭性疾病治疗的专业研发能力。(中国新闻网)
荣昌生物:泰它西普治疗原发性干燥综合征Ⅲ期临床研究达到主要研究终点
《科创板日报》13日讯,荣昌生物(688331.SH)公告称,公司自主研发的BLyS/APRIL双靶点融合蛋白创新药泰它西普用于治疗原发性干燥综合征(pSS)的Ⅲ期临床研究,达到方案设计的临床试验主要研究终点。该研究是一项多中心、随机、双盲、安慰剂对照的Ⅲ期临床研究,旨在评价泰它西普用于治疗原发性干燥综合征患者的有效性和安全性。临床研究结果显示,泰它西普可持续有效改善干燥综合征患者的临床症状,显示良好的有效性和安全性。公司将尽快向国家药品监督管理局药品审评中心(CDE)递交上市申请,详细数据将在国际重大学术会议上公布。(财联社)
康众医能“AI+基层医疗”业务试点正式启动
近日,康众医疗控股子公司康众医能科技(浙江)有限公司(简称“康众医能”)与无锡市新吴区旺庄街道社区卫生服务中心正式签署《社区智慧医疗合作共建协议》,标志着康众医能“AI+基层医疗”业务模式试点全面启动。(证券时报)
海思科:获得创新药HSK47977片《药物临床试验批准通知书》
8月12日,海思科(002653.SZ)公告称,公司近日收到国家药品监督管理局下发的《药物临床试验批准通知书》,同意HSK47977片开展临床试验。该药品为公司自主研发的口服BCL6 PROTAC小分子制剂,用于治疗非霍奇金淋巴瘤。HSK47977片国内尚无同靶点药物进入临床阶段,是潜在的First-In-Class产品。此外,该药品已完成与FDA的Pre-IND沟通和IND申报递交,正在审评中,未来有望实现中美同步开发。创新药研发周期长、风险高,存在不确定性,投资者需谨慎决策。(每日经济新闻)
北陆药业:控股子公司碘美普尔化学原料药获批上市
北陆药业(300016)8月12日晚间公告,近日,公司控股子公司浙江海昌药业股份有限公司(简称“海昌药业”)收到国家药监局核准签发的碘美普尔《化学原料药上市申请批准通知书》。
碘美普尔为对比剂碘美普尔注射液的原料药,作为一种低渗透压、非离子型水溶性造影剂,碘美普尔注射液被广泛应用于CT增强成像和血管造影。与传统的高渗透压造影剂相比,它对患者的肾脏和心血管系统负担较小,尤其适合肾功能不全和高风险患者。由于其良好的显影效果和较低的副作用,已成为临床上优先选择的造影剂之一。(人民财讯)
人事变动
Personnel Changes
南京医药聘任四位副总裁 任期与公司第十届董事会任期一致
8月8日,南京医药(600713)发布公告,2025年8月7日至8日,公司第十届董事会第二次会议审议通过了关于聘任部分高级管理人员的议案。根据董事会的提名和人力资源规划委员会的审核,肖宏、彭玉萍、倪华安、蔡鸣宇四位人士被聘任为公司副总裁,任期与公司第十届董事会任期一致。(财中社)
凯莱英选举HAO HONG担任董事长兼首席执行官
8月6日,凯莱英发布公告称,公司于8月6日召开2025年第二次临时股东大会,完成第五届董事会选举,同日召开第五届董事会第一次会议,完成了第五届董事会董事长、各专门委员会委员的选举及高级管理人员的聘任。
第五届董事会由9名董事组成,执行董事为董事长HAO HONG、杨蕊、张达、职工代表董事洪亮,非执行董事为YE SONG、张婷,独立非执行董事为侯欣一、孙雪娇、谢维恺,任期自2025年第二次临时股东大会选举通过之日起3年。此外,公司董事会提名,同意聘任HAO HONG为公司首席执行官(CEO)。(北京商报)
产 业 洞 察
SHINE CONSULTANT
01
从“仿制”到“创新”:东阳光药重构传统Pharma价值逻辑
点击阅读全文
产 业 研 报
SHINE CONSULTANT
01
2023年中国企业医疗健康管理白皮书
02
2022年中国康复医疗行业研究报告
03
合成生物学产业链及应用场景
04
2023年家用医疗智能器械商业路径发展报告
05
医疗产业链中数字化场景发展现况及挑战
06
2022年药品市场生命周期研究之GLP-1RA篇
07
中国医疗器械行业数据报告(2025版)
点击阅读全文
活 动 预 告
SHINE CONSULTANT
2025(第九届)亚太生物医药合作峰会,8月28日-29日 · 上海
2025医药行业合规数智创新论坛,9月23日 · 上海
最 新 课 程
SHINE CONSULTANT
生物医药行业研究与投资逻辑(点击查看)
全面汇总:医药全行业研究分析框架与投资逻辑详解(点击查看)
联系我们
Sunny Sun 孙女士
T:021 6095 0241
M:189 6294 0579(微信同号)
E:sunny.sun@shine-consultant.com
会议咨询
媒体合作
商务合作
欢迎详询洽谈!
SHINE CONSULTANT
上海士研管理咨询有限公司成立于2005年,致力于为组织领导者提供沟通交流与专家智库平台。通过二十年沉淀与积累,覆盖了金融与投资、交通与运输、消费与文旅、医药与医疗、能源与资源、高科与电信、公用与政府等产业领域,服务着全球500强和万余家领导型企业,汇聚了百万余名机构决策者,并与千余家产业权威机构建立了战略伙伴关系。士研咨询秉承专业立身的理念发展队伍,现拥有百余名专业的资深人员,核心管理团队都具有十五年以上的专业经验。
临床3期引进/卖出高管变更
2025-08-15
·医药笔记
▎Armstrong
2025年8月15日,银诺医药在港交所挂牌上市,发行价18.68港元,发行市值85亿港元,募资6.3亿港元。
银诺医药成立于2014年,成立11年来建立了丰富的代谢类研发管线,核心产品为GLP-1新药依苏帕格鲁肽,于2025年1月获批上市治疗二型糖尿病,减重适应症于今年3月启动2b/3期临床试验,预计2026年四季度完成。
依苏帕格鲁肽的分子结构如下,为一款Fc融合的长效GLP-1新药。
二型糖尿病三期临床中,1mg、3mg依苏帕格鲁肽治疗24周HbA1c降低幅度分别为1.7%、2.2%,显著高于安慰剂组的0.5%。
总结
中国减重市场在快速增长,诺和诺德司美格鲁肽减重版2024年11月在中国商业化上市,今年上半年销售额9.7亿元人民币。司美格鲁肽降糖版上半年销售额36.1亿元人民币,合计达到45.8亿元人民币,仍然占据绝大部分市场份额。随着礼来替尔泊肽、信达生物玛仕度肽获批,未来将成为司美格鲁肽的有力竞争对手。
Armstrong技术全梳理系列
GPRC5D靶点全梳理;
CD40靶点全梳理;
CD47靶点全梳理;
补体靶向药物技术全梳理;
补体药物:眼科治疗的重要方向;
Claudin 6靶点全梳理;
Claudin 18.2靶点全梳理;
靶点冷暖,行业自知;
中国大分子新药研发格局;
被炮轰的“me too”;
佐剂百年史;
胰岛素百年传奇;
CUSBEA:风雨四十载;
中国新药研发的焦虑;
中国生物医药企业的研发竞争;
中国双抗竞争格局;
中国ADC竞争格局;
中国双抗技术全梳理;
中国ADC技术全梳理;
Ambrx技术全梳理;
Vir Biotech技术全梳理;
Immune-Onc技术全梳理;
亘喜生物技术全梳理;
康哲药业技术全梳理;
科济药业技术全梳理;
恺佧生物技术全梳理;
同宜医药技术全梳理;
百奥赛图技术全梳理;
腾盛博药技术全梳理;
创胜集团技术全梳理;
永泰生物技术全梳理;
中国抗体技术全梳理;
德琪医药技术全梳理;
德琪医药技术全梳理2.0;
和铂医药技术全梳理;
荣昌生物技术全梳理;
再鼎医药技术全梳理;
药明生物技术全梳理;
恒瑞医药技术全梳理;
豪森药业技术全梳理;
正大天晴技术全梳理;
吉凯基因技术全梳理;
基石药业技术全梳理;
百济神州技术全梳理;
百济神州技术全梳理第2版;
信达生物技术全梳理;
信达生物技术全梳理第2版;
中山康方技术全梳理;
复宏汉霖技术全梳理;
先声药业技术全梳理;
君实生物技术全梳理;
嘉和生物技术全梳理;
志道生物技术全梳理;
道尔生物技术全梳理;
尚健生物技术全梳理;
康宁杰瑞技术全梳理;
科望医药技术全梳理;
岸迈生物技术全梳理;
礼进生物技术全梳理;
康桥资本技术全梳理;
余国良的抗体药布局;
荃信生物技术全梳理;
安源医药技术全梳理;
三生国健技术全梳理;
仁会生物技术全梳理;
乐普生物技术全梳理;
同润生物技术全梳理;
宜明昂科技术全梳理;
派格生物技术全梳理;
迈威生物技术全梳理;
Momenta技术全梳理;
NGM技术全梳理;
普米斯生物技术全梳理;
普米斯生物技术全梳理2.0;
三叶草生物技术全梳理;
贝达药业抗体药全梳理;
泽璟制药抗体药全梳理;
恒瑞医药抗体药全梳理;
齐鲁制药抗体药全梳理;
石药集团抗体药全梳理;
豪森药业抗体药全梳理;
华海药业抗体药全梳理;
科伦药业抗体药全梳理;
百奥泰技术全梳理;
凡恩世技术全梳理。
抗体药物偶联物临床3期申请上市临床2期
2025-08-15
·药研发
「 本文共:5条资讯,阅读时长约:10分钟 」
药研资讯
1.中国医药子公司富马酸伏诺拉生原料药获批,强化消化领域布局。中国医药健康产业股份有限公司全资子公司天方药业有限公司宣布,其富马酸伏诺拉生原料药获国家药监局批准上市(包装规格20kg/桶)。该药主要用于治疗反流性食管炎及联合根除幽门螺杆菌,是消化系统治疗领域的关键品种。截至公告日,国内共有64个富马酸伏诺拉生原料药登记号,其中28个状态为“已批准”。该项目累计研发投入约1136万元,将强化公司“原料药+制剂”一体化战略。此次获批有望提升中国医药在高端原料药市场的竞争力,但商业化表现仍需关注政策与市场竞争影响。2.荣昌生物泰它西普全球首创:III期临床攻克原发性干燥综合征。荣昌生物宣布其双靶点融合蛋白创新药泰它西普(RC18)治疗原发性干燥综合征(pSS)的III期临床达到主要终点。该药是全球首个针对pSS适应症取得突破的生物药,填补了该领域治疗空白。pSS是一种系统性自身免疫病,我国患者超500万,此前缺乏有效治疗手段。泰它西普通过同时抑制BLyS和APRIL通路,调节B细胞异常活化,从机制上阻断疾病进展。若获批上市,将为患者提供首个靶向治疗方案,并巩固荣昌生物在自身免疫领域的领先地位。公司计划加速推进上市申请,预计2026年进入市场。3.百济神州皮下注射PD-1启动国内首个Ⅲ期临床,给药效率革命。百济神州启动PD-1抑制剂替雷利珠单抗皮下注射剂型的Ⅲ期临床试验,适应症为联合化疗治疗局部晚期不可切除或转移性胃/胃食管结合部腺癌。这是国内首个进入Ⅲ期阶段的皮下注射PD-1药物。与传统静脉注射相比,皮下注射可将给药时间从30-60分钟缩短至30秒,大幅提升患者依从性及医疗资源效率。替雷利珠单抗目前已覆盖尿路上皮癌、非小细胞肺癌等癌种,2025年上半年销售额达26.43亿元(同比+20.6%)。若该剂型获批,将巩固百济在PD-1赛道差异化优势,并与罗氏、BMS等国际巨头的皮下注射产品直接竞争。4.恒瑞医药新型ADC药物SHR-7782获批临床,攻坚晚期实体瘤。恒瑞医药公告其子公司苏州盛迪亚研发的SHR-7782注射液获国家药监局临床试验批准,拟用于治疗晚期实体瘤。该药为靶向Nectin-4的抗体偶联药物(ADC),目前全球仅安斯泰来的Padcev一款同类产品上市(2024年销售额19.49亿美元)。恒瑞计划开展SHR-7782联合阿得贝利单抗(PD-L1抑制剂)及化疗的Ib/II期研究,探索其在复发/转移性头颈鳞癌等适应症的潜力。此次获批凸显恒瑞在ADC多维度迭代策略——通过创新靶点组合(如Nectin-4+PD-L1)提升疗效,进一步拓展实体瘤治疗边界。5.美国开发mRNA广谱抗病毒药物,可高效抑制寨卡、新冠及流感病毒。哥伦比亚大学科研团队在《科学转化医学》发表突破性研究,利用I型干扰素刺激基因(ISG)开发出一套10-ISG组合,通过mRNA递送系统实现广谱抗病毒活性。该技术在动物实验中证实可高效抑制寨卡病毒、SARS-CoV-2和流感病毒复制,且未引发显著免疫毒性。这一突破为应对未来新发病毒疫情提供了技术储备,并可能颠覆传统抗病毒药物研发模式——从“一病一药”转向“一药多病”。目前,辉瑞、Moderna等企业已布局mRNA抗病毒平台,此次进展或将加速该领域临床转化。
股市资讯
8月14日A股医药公司涨幅TOP 3
九芝堂(000989.SZ) +10.00%
海创药业(688302.SH) +10.00%
荣昌生物(688331.SH) +10.00%
8月14日A股医药公司跌幅TOP 3
北大医药(000788.SZ) -7.36%
君实生物-U(688180.SH) -3.03%
润都股份(002923.SZ) -2.15%
8月14日港股医药公司涨幅TOP 3
荣昌生物-B(09995.HK) +14.00%
泰格医药(03347.HK) +4.76%
诺诚健华-B(09969.HK) +3.33%
评审动态
8月14日新药临床试验申请IND
8月8日新药上市申请NDA(8月9日至8月14日无新增数据)
END
临床3期抗体药物偶联物上市批准临床结果
100 项与 荣昌生物制药(烟台)股份有限公司 相关的药物交易
登录后查看更多信息
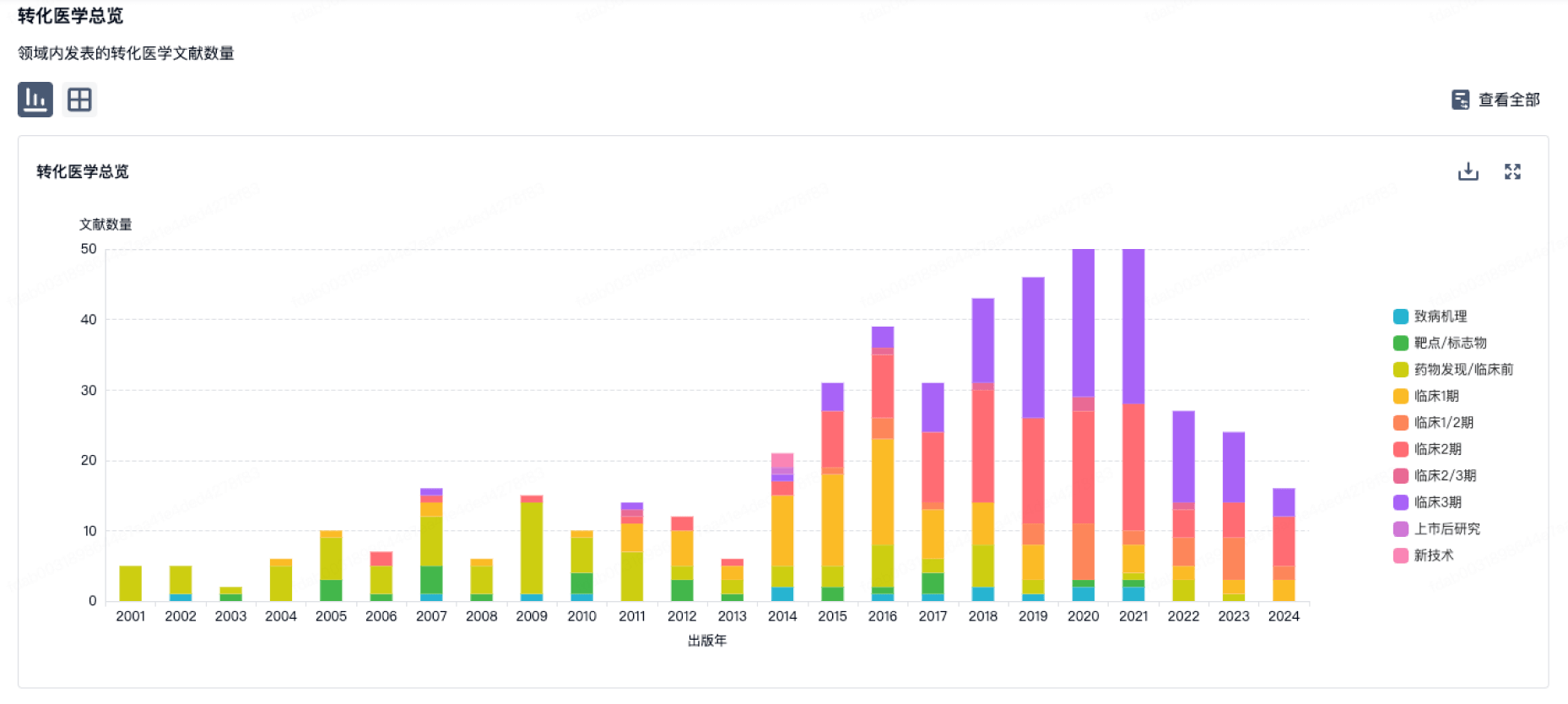
100 项与 荣昌生物制药(烟台)股份有限公司 相关的转化医学
登录后查看更多信息
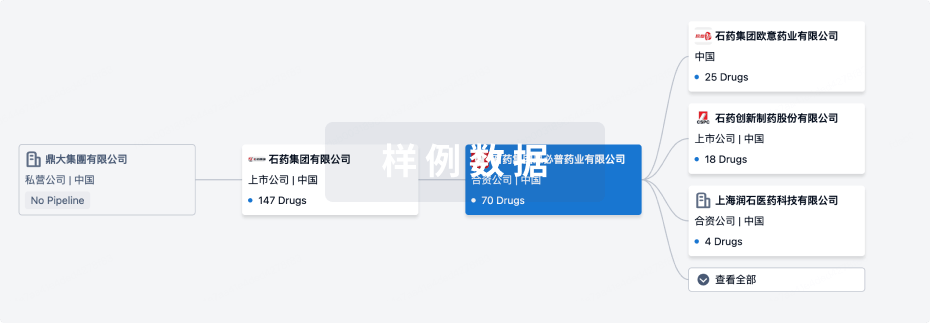
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月20日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
8
3
临床前
临床申请
8
2
临床1期
临床2期
8
1
临床3期
批准上市
2
9
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
泰它西普 ( APRIL x BAFF ) | 系统性红斑狼疮 更多 | 批准上市 |
Eflimrufusp alfa ( VEGF x bFGF ) | 糖尿病性黄斑水肿 更多 | 临床3期 |
维迪西妥单抗 ( HER2 x Tubulin ) | 晚期乳腺癌 更多 | 临床2期 |
替雷利珠单抗 ( PD-1 ) | 非肌层浸润性膀胱肿瘤 更多 | 临床2期 |
RC-148 ( PD-1 x VEGF ) | 晚期恶性实体瘤 更多 | 临床1/2期 |
登录后查看更多信息
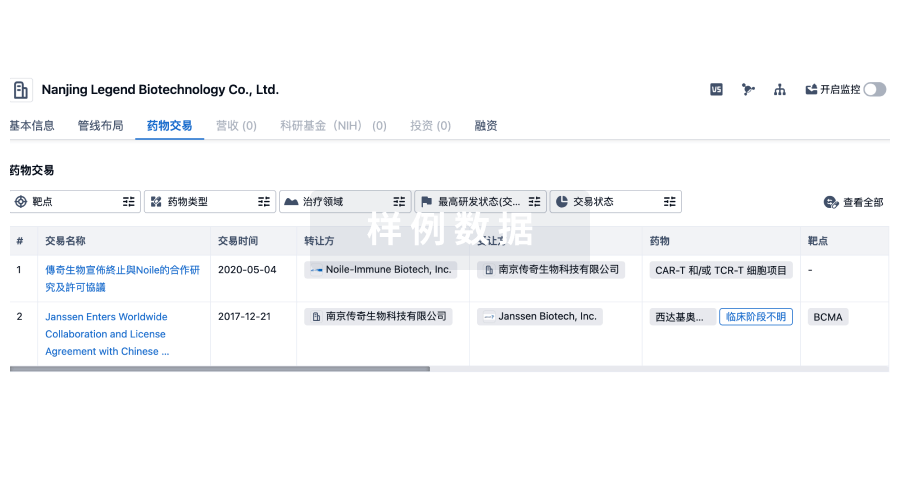
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
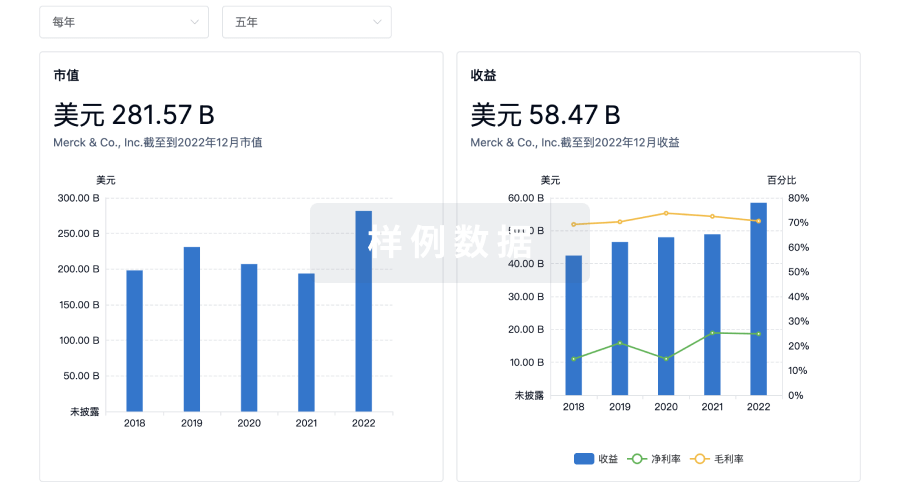
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
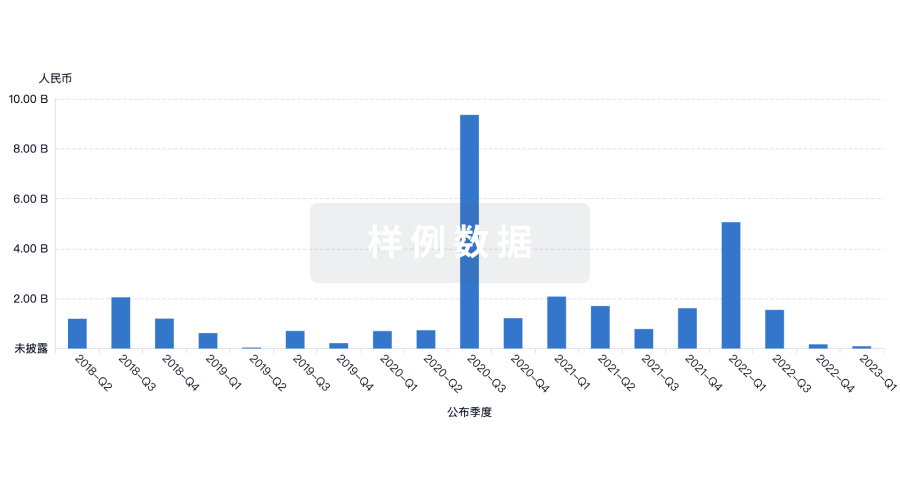
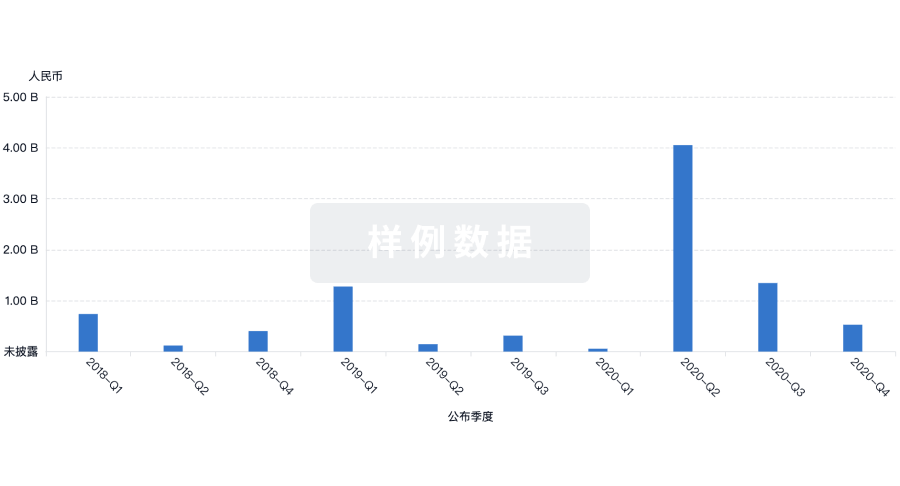
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
