预约演示
更新于:2025-05-07
Sanofi-Aventis Groupe SA
子公司|1995|France
子公司|1995|France
更新于:2025-05-07
概览
标签
其他疾病
心血管疾病
神经系统疾病
小分子化药
合成多肽
酶
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 3 |
| 酶 | 1 |
| 合成多肽 | 1 |
关联
7
项与 Sanofi-Aventis Groupe SA 相关的药物作用机制 HMG-CoA reductase抑制剂 [+2] |
在研机构 |
在研适应症 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期2019-03-26 |
靶点 |
作用机制 GLP-1R激动剂 |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期2013-06-28 |
作用机制 HMG-CoA reductase抑制剂 [+2] |
在研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2013-05-03 |
25
项与 Sanofi-Aventis Groupe SA 相关的临床试验CTR20242016
一项接受度普利尤单抗治疗结节性痒疹患者的前瞻性观察研究
主要目的:描述度普利尤单抗治疗结节性痒疹 (PN) 的真实世界使用模式;次要目的:描述接受度普利尤单抗治疗的 PN 患者的病史、社会人口统计学、疾病特征以及既往或合并用药;评价度普利尤单抗治疗 PN 的长期真实世界疗效;收集研究受试者的安全性数据
开始日期2024-10-21 |
申办/合作机构 |
CTR20232209
一项在中国 ≥6 岁至 <18 岁中度至重度特应性皮炎受试者中评估度普利尤单抗的药代动力学、安全性和有效性的 IV 期多中心研究
主要目的:在中国 ≥6 岁至 <18 岁 AD 儿童人群中评估度普利尤单抗的 PK。 次要目的:在中国 ≥6 岁至 <18 岁 AD 儿童人群中评估度普利尤单抗的安全性;在中国 ≥6 岁至 <18 岁 AD 儿童人群中评估度普利尤单抗的有效性
开始日期2023-08-23 |
申办/合作机构 |
CTR20230845
一项在患有慢性鼻窦炎伴鼻息肉(CRSwNP)且使用鼻用皮质类固醇进行背景治疗的中国成人受试者中评价度普利尤单抗疗效和安全性的随机、双盲、安慰剂对照研究
主要目的:在布地奈德鼻喷雾剂背景治疗下,评价度普利尤单抗相比于安慰剂在降低患有双侧鼻息肉(NP)中国受试者的内镜下鼻息肉评分(NPS)方面的疗效。次要目的:评价度普利尤单抗在降低鼻塞/鼻堵(NC)严重程度方面的疗效;评价度普利尤单抗改善症状总分(TSS)方面的疗效;评价度普利尤单抗在改善嗅觉方面的疗效;评价度普利尤单抗对患者生活质量的影响;评价度普利尤单抗减少需要全身性皮质类固醇(SCS)或 NP 手术治疗的受试者比例的效果;评价度普利尤单抗在患有双侧 NP 的中国受试者中的安全性。
开始日期2023-05-16 |
申办/合作机构 |
100 项与 Sanofi-Aventis Groupe SA 相关的临床结果
登录后查看更多信息
0 项与 Sanofi-Aventis Groupe SA 相关的专利(医药)
登录后查看更多信息
20
项与 Sanofi-Aventis Groupe SA 相关的文献(医药)2022-09-01·World Allergy Organization Journal
Environmental contributions to the interactions of COVID-19 and asthma: A secondary publication and update
Review
作者: López, Juan Felipe ; Galán, Carmen ; Rosário Filho, Nelson A ; Zakzuk, Josefina ; Urrutia-Pereira, Marilyn ; D'Amato, Gennaro ; Pomés, Anna ; Ansotegui, Ignacio J ; Aguttes, Margarita Murrieta ; Chong-Neto, Herberto Jose ; Cecchi, Lorenzo ; Annesi Maesano, Isabella ; Caraballo, Luis ; Peden, David
2021-01-01·Therapeutic Innovation & Regulatory Science4区 · 医学
Determining Minimum Wear Time for Mobile Sensor Technology
4区 · 医学
Review
作者: Byrom, Bill ; Bury, Denise P ; Wong, Susan ; McCarthy, Marie ; Geoghegan, Cindy
2020-10-01·Laboratory Animals4区 · 医学
The European Federation of the Pharmaceutical Industry and Associations’ Research and Animal Welfare Group: Assessing and benchmarking ‘Culture of Care’ in the context of using animals for scientific purpose
4区 · 医学
Article
作者: Robinson, Sally ; Williams, Bella ; Decelle, Thierry ; Reid, Kirsty ; Bertelsen, Thomas ; Chlebus, Magda ; Sparrow, Sue
3
项与 Sanofi-Aventis Groupe SA 相关的新闻(医药)2024-05-28
Sarclisa accepted for FDA priority review for the treatment of transplant-ineligible newly diagnosed multiple myeloma
FDA Priority Review granted based on positive results from IMROZ phase 3 study
If approved, Sarclisa would be the first anti-CD38 therapy in combination with standard-of-care treatment for patients with newly diagnosed transplant-ineligible multiple myeloma
Pivotal IMROZ phase 3 study results to be featured during oral presentation at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting
May 27, 2024. The U.S. Food and Drug Administration (FDA) has accepted for Priority Review the supplemental Biologics License Application (sBLA) for the investigational use of Sarclisa (isatuximab) in combination with bortezomib, lenalidomide and dexamethasone (VRd) for the treatment of patients with transplant-ineligible newly diagnosed multiple myeloma (NDMM). If approved, Sarclisa would be the first anti-CD38 therapy in combination with standard-of-care VRd in newly diagnosed patients not eligible for transplant, which would be the third indication for Sarclisa in multiple myeloma. The target action date for the FDA decision is September 27, 2024. A regulatory submission is also under review in the European Union (EU).
Dietmar Berger, M.D., Ph.D.
Chief Medical Officer, Global Head of Development at Sanofi
“Despite recent advancements in multiple myeloma treatment, there remains a significant unmet need for new frontline therapies, particularly for transplant-ineligible patients who can face poor outcomes from the disease. The filing acceptances, as well as the FDA’s Priority Review designation, reinforce our confidence in Sarclisa as a potential best-in-class treatment and represent a critical step toward advancing this combination in a difficult-to-treat cancer.”
The sBLA, as well as the submission in the EU, is based on positive results from the IMROZ phase 3 clinical study evaluating the investigational use of Sarclisa in combination with standard-of-care VRd. In December 2023, the study met its primary endpoint at a planned interim analysis for efficacy, demonstrating statistically significant improvement in progression-free survival (PFS) with Sarclisa in combination with VRd compared with VRd alone in transplant-ineligible patients with NDMM. The safety and tolerability of Sarclisa observed in this study was consistent with the established safety profile of Sarclisa and VRd.
The IMROZ study is the fourth phase 3 study investigating Sarclisa combinations in NDMM patients to show superiority versus standard-of-care VRd and KRd, reinforcing its best-in-class potential. Results from the IMROZ study will also be featured during an oral presentation at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting and during the plenary scientific session at the 2024 European Hematology Association (EHA) Annual Congress.
Priority Review is granted to regulatory applications seeking approval for therapies that have the potential to provide significant improvements in the treatment, diagnosis or prevention of serious conditions.
The investigational use of Sarclisa in combination with VRd in patients with transplant-ineligible NDMM is currently under clinical development, and its safety and efficacy for this indication have not been fully evaluated by any regulatory authority.
The global, randomized, multi-center, open-label IMROZ phase 3 clinical study enrolled 446 patients with newly diagnosed, transplant-ineligible MM across 21 countries and 104 centers. During the study, Sarclisa was administered through an intravenous infusion at a dose of 10 mg/kg once weekly for five weeks during first 42-day cycle and once every two weeks in cycles 2 to 4 in combination with subcutaneous bortezomib, oral lenalidomide and intravenous or oral dexamethasone. Then Sarclisa was administered every 2 weeks from cycle 5 to 17 and every 4 weeks in cycles 18+ during 28-day cycles in combination with lenalidomide and dexamethasone at the standard dose, until disease progression, unacceptable safety profile or patient’s decision to stop the study treatment.
The primary endpoint was progression-free survival. Key secondary endpoints include complete response rate, minimal residual disease (MRD) negativity rate for patients with a complete response, very good partial response or better rate, and overall survival. Other secondary endpoints were overall response rate, time to progression, duration of response, time to first response, time to best response, progression-free survival on next line of therapy, progression-free survival by MRD status, sustained MRD negativity greater than or equal to 12 months rate, safety, pharmacokinetic profile, immunogenicity, disease-specific and generic health-related quality of life, disease and treatment-related symptoms, health state utility, and health status.1
Sarclisa is a monoclonal antibody that binds to a specific epitope on the CD38 receptor on multiple myeloma (MM) cells, inducing distinct antitumor activity. It is designed to work through multiple mechanisms of action including programmed tumor cell death (apoptosis) and immunomodulatory activities. CD38 is highly and uniformly expressed on the surface of MM cells, making it a potential target for antibody-based therapeutics such as Sarclisa.
Based on the phase 3 ICARIA-MM study, Sarclisa is approved in >50 countries, including the U.S. and EU, in combination with pomalidomide and dexamethasone for the treatment of certain patients with relapsed refractory MM (RRMM) who have received ≥2 prior therapies, including lenalidomide and a proteasome inhibitor and who progressed on last therapy. Based on the phase 3 IKEMA study, Sarclisa is also approved in 50 countries in combination with carfilzomib and dexamethasone, including in the U.S. for the treatment of patients with RRMM who have received 1–3 prior lines of therapy and in the European Union for patients with MM who have received at least 1 prior therapy. In the U.S., the generic name for Sarclisa is isatuximab-irfc, with irfc as the suffix designated in accordance with Nonproprietary Naming of Biological Products Guidance for Industry issued by the U.S. Food and Drug Administration (FDA).
Sarclisa continues to be evaluated in multiple ongoing phase 3 clinical studies in combination with current standard treatments across the MM treatment continuum. It is also under investigation for the treatment of other hematologic malignancies, and its safety and efficacy have not been evaluated by any regulatory authority outside of its approved indication.
Multiple myeloma (MM) is the second most common hematologic malignancy,2 with more than 180,000 new diagnoses of MM worldwide yearly.3 Despite available treatments, MM remains an incurable malignancy with an estimated 52% five-year survival rate for newly diagnosed patients.4 Since MM does not have a cure, most patients will relapse. Relapsed MM is the term for when the cancer returns after treatment or a period of remission. Refractory MM refers to when the cancer does not respond or no longer responds to therapy.
We are an innovative global healthcare company, driven by one purpose: we chase the miracles of science to improve people’s lives. Our team, across the world, is dedicated to transforming the practice of medicine by working to turn the impossible into the possible. We provide potentially life-changing treatment options and life-saving vaccine protection to millions of people globally, while putting sustainability and social responsibility at the center of our ambitions.
1 ClinicalTrials.gov.Identifier#NCT03319667. https://clinicaltrials.gov/ct2/show/NCT03319667. Accessed March 2024.
2 Kazandjian D. Multiple myeloma epidemiology and survival: A unique malignancy. Semin Oncol. 2016;43(6):676-681. doi:10.1053/j/seminoncol.2016.11.004.
3 World Health Organization. Multiple Myeloma. 35-multiple-myeloma-fact-sheet.pdf (who.int). Accessed March 2024.
4 Fonseca, R., Usmani, S.Z., Mehra, M. et al. Frontline treatment patterns and attrition rates by subsequent lines of therapy in patients with newly diagnosed multiple myeloma. BMC Cancer. 2020: 20(1087). https://doi-org.libproxy1.nus.edu.sg/10.1186/s12885-020-07503-y
The content above comes from the network. if any infringement, please contact us to modify.
上市批准ASCO会议临床结果优先审批
2007-01-25
BETHESDA, Md., Jan. 25 /PRNewswire/ -- Sanofi pasteur, the vaccines business of the sanofi-aventis Group , is pleased that the members of an advisory committee to the U.S. Food and Drug Administration (FDA) voted nearly unanimously today that the company's pentavalent combination vaccine for use in pediatric patients is both safe and efficacious. Pentacel(R) (DTaP-IPV-Hib) vaccine(1) protects against diphtheria, tetanus, pertussis, polio, and Haemophilus influenzae type b (Hib).
According to the current Recommended Childhood and Adolescent Immunization Schedule from the Advisory Committee on Immunization Practices (ACIP) of the U.S. Centers for Disease Control and Prevention (CDC), up to 23 injections are needed through 18 months of age. The use of Pentacel vaccine could reduce that number of shots by seven.
The regulatory submission of Pentacel vaccine is based on results of clinical studies involving more than 5,000 children in multi-center trials(2) conducted in the U.S. and Canada. Pentacel vaccine is licensed for pediatric use in nine countries, including Canada, where it has been used universally in infants and young children since 1998 for the prevention of diphtheria, tetanus, pertussis, polio and Hib. Over 12.5 million doses of Pentacel vaccine have been distributed in Canada.
Pentacel vaccine is the first DTaP-based combination vaccine candidate for use in infants in the U.S. that includes both polio and Hib vaccine components. The diphtheria, tetanus, and pertussis components in Pentacel vaccine are based on the formulation in DAPTACEL(R) -- Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP vaccine) -- which was introduced by sanofi pasteur in the U.S. in 2002. In clinical trials, Pentacel vaccine was administered as a four-dose series -- at 2, 4, 6, and 15-18 months of age -- concomitantly with other recommended childhood vaccines.
Sanofi pasteur's U.S. operations in Swiftwater, PA has long been committed to providing vaccines to prevent childhood diseases. In 1987, it licensed the first Haemophilus influenzae type b (Hib) conjugate vaccine. And in 1996, it was the first company to license a diphtheria, tetanus, and acellular pertussis vaccine for use in infants -- Tripedia(R), Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed. In 2005, sanofi pasteur continued its tradition of innovation by introducing Menactra(R), Meningococcal (Groups A, C, Y and W-135) Polysaccharide Diphtheria Toxoid Conjugate Vaccine to protect against meningococcal disease in adolescents and adults, 11-55 years of age, and ADACEL(R), Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine Adsorbed as a booster dose for protection against tetanus, diphtheria and pertussis in both adolescents and adults 11-64 years of age.
About Diphtheria
Diphtheria is a disease caused by a bacterium, Corynebacterium diphtheriae, that usually affects the tonsils, throat, nose and/or skin. It is passed from person to person by droplet transmission, usually by breathing in diphtheria bacteria after an infected person has coughed or sneezed. Although diphtheria disease is rare in the U.S., it appears that C diphtheriae continues to circulate in areas of the country with previously endemic diphtheria. Diphtheria also occurs in many other parts of the world.
About Tetanus
Tetanus is a severe, frequently fatal disease caused by an exotoxin produced by Clostridium tetani, a bacterium that is found in the environment. Tetanus is not transmitted from person to person. Rather, Clostridium tetani enters the body through an open wound, including lacerations, abrasions and puncture wounds. The toxin causes neuromuscular dysfunction, with rigidity and spasms of skeletal muscles. The muscle spasms usually start in the jaw (which is why the disease is sometimes called "lockjaw") and neck and may spread to many other muscles, leading to generalized paralysis.
About Pertussis
Pertussis, a highly contagious disease of the respiratory tract, is caused by exposure to bacteria (Bordetella pertussis) found in the mouth, nose and throat of an infected person. Pertussis is primarily spread by direct contact with discharge from the nose or throat of infected individuals. Classic -- or severe pertussis -- as defined by the World Health Organization, consists of at least 21 days of cough illness (with the cough coming in spasms or paroxysms), associated whoops or post-cough vomiting, and laboratory confirmation. Despite widespread vaccination, reports of pertussis outbreaks continue to in the U.S. At particular risk are newborns and babies who have not yet been fully vaccinated against pertussis, iii who are more likely to have severe pertussis, and who face the possibility of serious complications and death. Over the last decade, 80% of pertussis deaths have occurred in infants under 6 months of age.(3)
About Polio
Poliomyelitis (polio) is a highly infectious disease caused by a virus that invades the nervous system and can cause severe paralysis. The virus enters the body through the mouth and multiplies in the intestine. Initial symptoms are fever, fatigue, headache, vomiting, stiffness in the neck, and pain in the limbs. One in 200 infections leads to irreversible paralysis (usually in the legs). Among those paralyzed, 5-10% dies when their breathing muscles become immobilized. Polio mainly affects children under five years of age. Naturally occurring polio was eliminated in the U.S. in 1979 and in the Western Hemisphere by 1991; however, worldwide efforts are continuing towards eradication of this contagious and devastating disease.
About Hib
Haemophilus influenzae type b (Hib) disease is caused by a bacterium that enters the body through the nose or throat and then can spread to cause meningitis (an infection of the coverings of the brain and spinal cord), blood stream infection, pneumonia, infection of the epiglottis, and other serious infections. Hib disease can cause mental retardation in young children and be a life-threatening infection. The Hib bacterium is still circulating in the U.S. today.(4) Ongoing vaccination is critical in preventing a resurgence of Hib, which was the leading cause of bacterial meningitis in children under five years of age before vaccines were introduced.
About sanofi-aventis
Sanofi-aventis is one of the world's leading pharmaceutical companies. Backed by a world-class R&D organization, sanofi-aventis is developing leading positions in seven major therapeutic areas: cardiovascular, thrombosis, oncology, metabolic diseases, central nervous system, internal medicine and vaccines. Sanofi-aventis is listed in Paris and in New York .
Sanofi pasteur, the vaccines business of the sanofi-aventis Group, sold more than a billion doses of vaccine in 2005, making it possible to protect more than 500 million people across the globe. The company offers the broadest range of vaccines, providing protection against 20 bacterial and viral diseases. For more information, please visit:
Forward Looking Statements
This press release contains forward-looking statements as defined in the Private Securities Litigation Reform Act of 1995. Forward-looking statements are statements that are not historical facts. These statements include financial projections and estimates and their underlying assumptions, statements regarding plans, objectives and expectations with respect to future events, operations, products and services, and statements regarding future performance. Forward-looking statements are generally identified by the words "expect," "anticipates," "believes," "intends," "estimates," "plans" and similar expressions. Although sanofi-aventis' management believes that the expectations reflected in such forward-looking statements are reasonable, investors are cautioned that forward-looking information and statements are subject to various risks and uncertainties, many of which are difficult to predict and generally beyond the control of sanofi-aventis, that could cause actual results and developments to differ materially from those expressed in, or implied or projected by, the forward-looking information and statements. These risks and uncertainties include those discussed or identified in the public filings with the SEC and the AMF made by sanofi-aventis, including those listed under "Risk Factors" and "Cautionary Statement Regarding Forward- Looking Statements" in sanofi-aventis' annual report on Form 20-F for the year ended December 31, 2005. Other than as required by applicable law, sanofi- aventis does not undertake any obligation to update or revise any forward- looking information or statements.
(1) The true name for Pentacel(R) vaccine is: Diphtheria and Tetanus
Toxoids and Acellular Pertussis Adsorbed, Inactivated Poliovirus and
Haemophilus b Conjugate (Tetanus Toxoid Conjugate) Vaccine Combined
(2) Herz A, Black S, Shinefield H, Noriega F, Greenberg, D. Safety of
DTaP-IPV//PRP-T (PENTACEL) administered at 2, 4, 6, and 15 to 18
months of age. Annual meeting of the Pediatric Academic Societies 2005
(3) Vitek CR, Pascual FR, Baugham, AL, Murphy TV. Increase in deaths from
pertussis from young infants in the United States in the 1990s. Pediar
Infect Dis J. 2003:22:628:634.6
(4) Donnelly, M.J, Herold, B.C., Jenkins, S.G., Daum, R.S. Obstacles to
the elimination of Haemophilus influenzae type b disease: Three
illustrative cases. Pediatrics. Vol. 112, No. 6, December 2003, pp.
1465-1466
sanofi pasteur
CONTACT: Pascal Barollier, International Media Relations, +33-(0)4-37-37-51-41, pascal.barollier@sanofipasteur.com, or Len Lavenda, U.S. MediaRelations, +1-570-839-4446, len.lavenda@sanofipasteur.com, both for sanofipasteur
Web site:
疫苗
2004-09-23
PARIS, Sept. 22 /PRNewswire-FirstCall/ -- The sanofi-aventis Group announced today the appointments within the Communications department of the Group, which is headed by Nicole CRANOIS, Senior Vice President, Communications.
- Jocelyne COUPAT, Vice President, International Relations
- Agnes GARCIA-GIBOT, Vice President, Internal Communications
and Corporate Image
- Michel JOLY, Vice President, Product PR
- William BRATTON, Deputy Vice President, Product PR
- Jean-Marc PODVIN, Vice President, Media Relations
- Robert SEBBAG, Vice President, Solidarity mission on access to
medicine
Are also members of the Communications Management Committee:
- Xavier LEGRAND DU LAURENS, Vice President, Communications France
- Miriam HENN, Vice President, Communications Germany
- Charles F. ROUSE, Vice President, Communications USA.
The sanofi-aventis Group is the world's 3rd largest pharmaceutical company, ranking number 1 in Europe. Backed by a world-class R&D organization, sanofi-aventis is developing leading positions in seven major therapeutic areas: cardiovascular disease, thrombosis, oncology, diabetes, central nervous system, internal medicine, vaccines. The sanofi-aventis Group is listed in Paris (EURONEXT: SAN) and in New York .
Important Information
In connection with its acquisition of Aventis, Sanofi-Aventis has announced that it is studying the feasibility of merging Aventis with and into Sanofi-Aventis, with Sanofi-Aventis continuing as the surviving corporation. In connection with any merger of Aventis into Sanofi-Aventis, Sanofi-Aventis will post-effective amendment to its registration statement on Form F-4 (File no. 333-112314), which will include a prospectus relating to the merger, and will documents with the SEC. Investors are urged to read the registration statement, including any preliminary prospectus or definitive prospectus (when available) relating to the merger, and any other relevant documents filed with the SEC, including all amendments and supplements, because they will contain important information. Free copies of the registration statement, as well as other relevant documents filed with the SEC, may be obtained at the SEC's web site at . At the appropriate time, Sanofi-Aventis will provide investors with information on how to obtain any merger-related documents for free from Sanofi-Aventis or from its duly appointed agents.
CONTACT: Jean-Marc Podvin
Vice President, Media Relations
Sanofi-Aventis
+331-53-77-4223
The sanofi-aventis Group
CONTACT: Jean-Marc Podvin Vice President, Media Relations ofSanofi-Aventis, +331-53-77-4223
Web site:
Company News On-Call:
疫苗并购
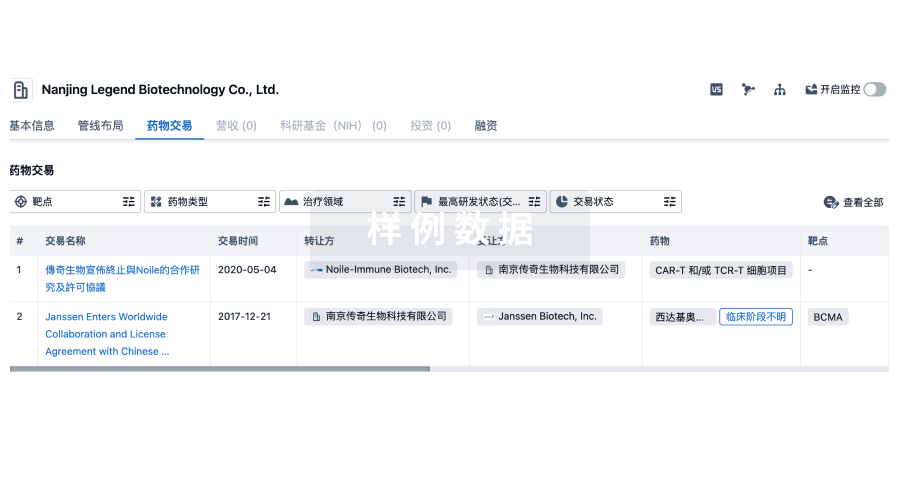
100 项与 Sanofi-Aventis Groupe SA 相关的药物交易
登录后查看更多信息
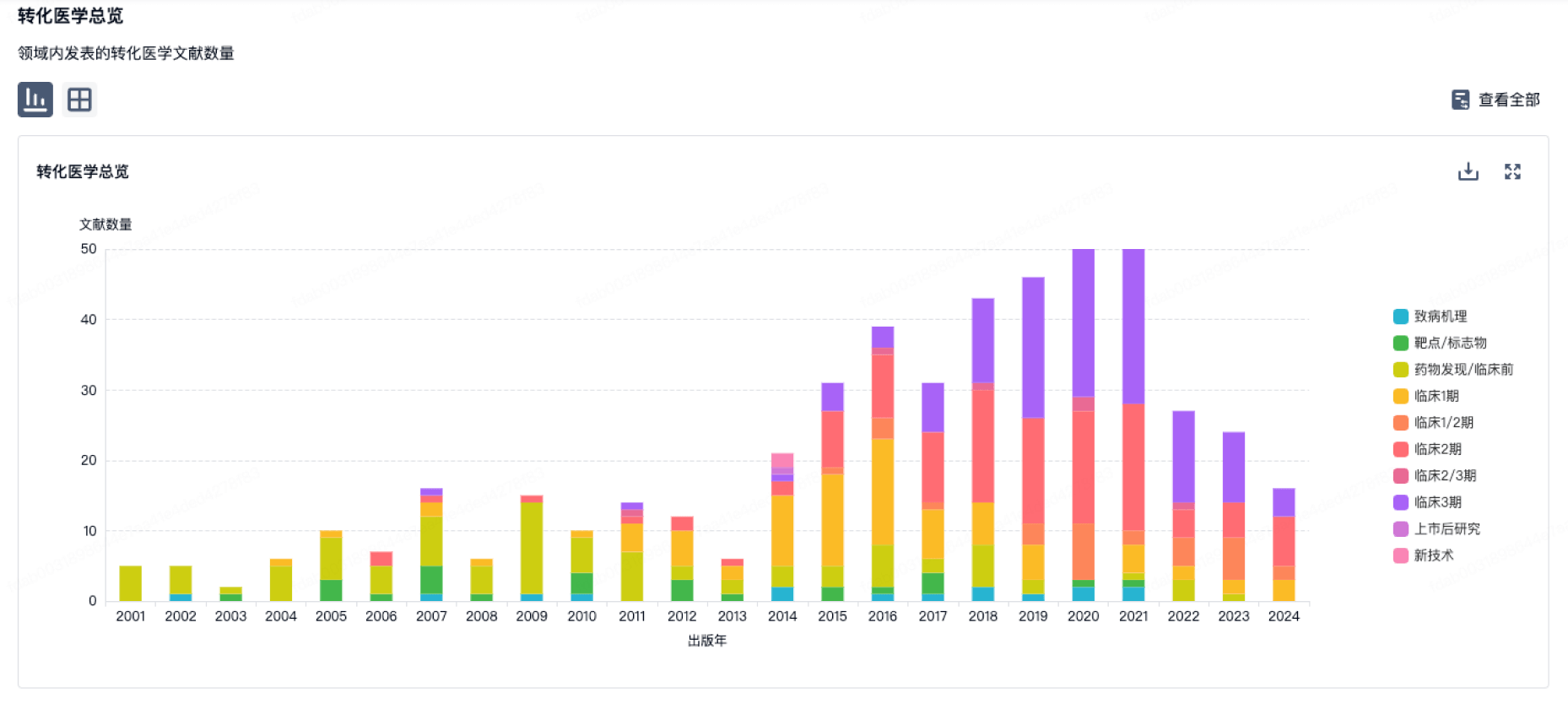
100 项与 Sanofi-Aventis Groupe SA 相关的转化医学
登录后查看更多信息
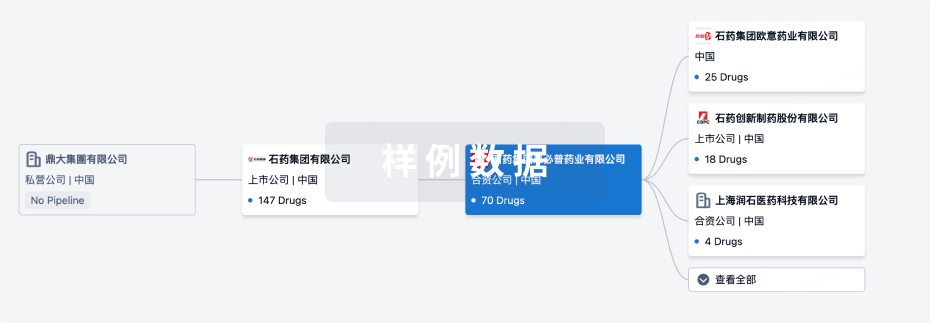
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月13日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
批准上市
5
2
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
氨磺必利 ( D2 receptor x D3 receptor ) | 精神分裂症 更多 | 批准上市 |
厄贝沙坦氢氯噻嗪 ( AT1R x NCC ) | 原发性高血压 更多 | 批准上市 |
利司那肽 ( GLP-1R ) | 2型糖尿病 更多 | 批准上市 |
硫酸氢氯吡格雷/阿司匹林 ( COXs x P2Y12 receptor x TBXA2R ) | 心肌梗塞 更多 | 批准上市 |
拉布立海 ( Uric acid ) | 高尿酸血症 更多 | 批准上市 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
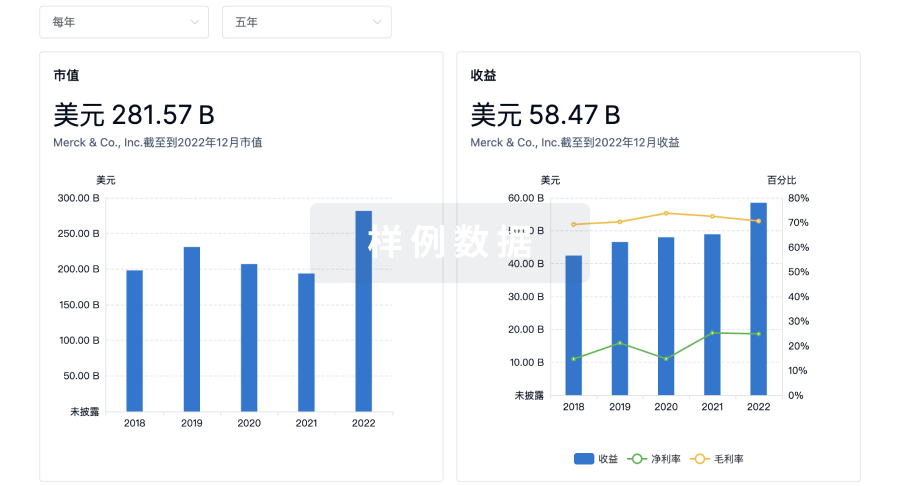
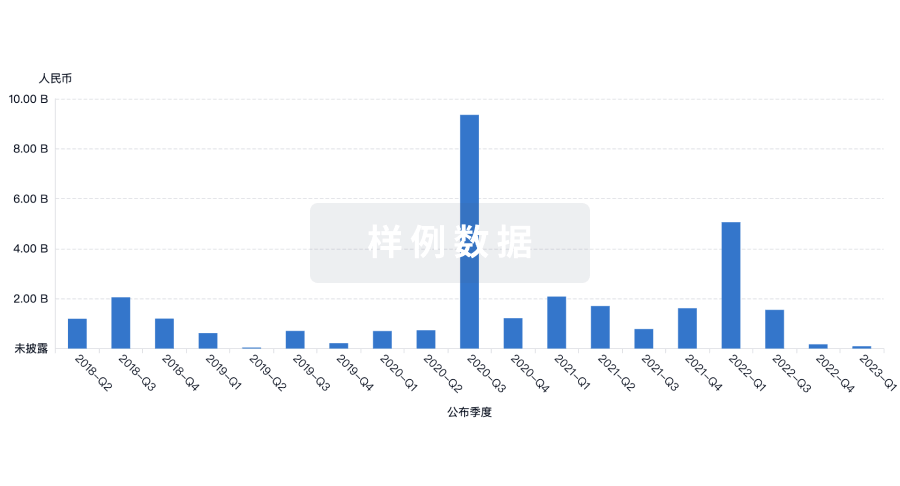
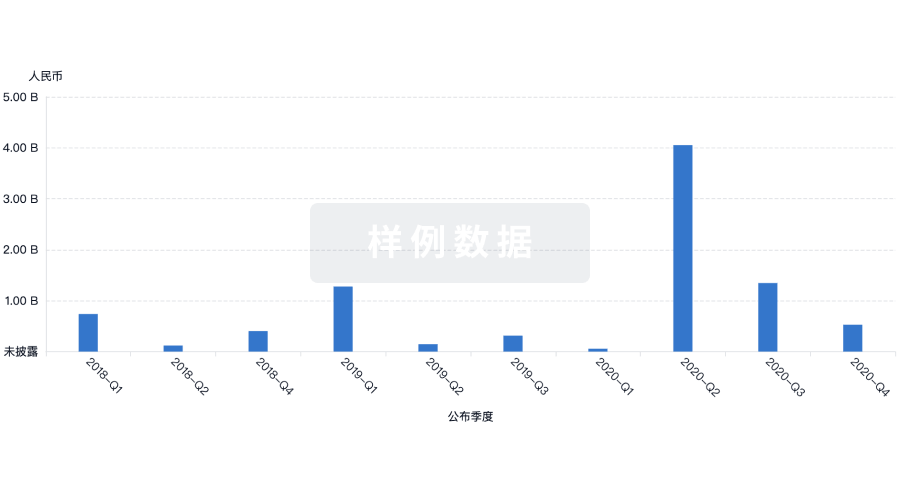
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



