预约演示
更新于:2025-08-01

Asieris Pharmaceuticals Co., Ltd.
更新于:2025-08-01
概览
标签
肿瘤
泌尿生殖系统疾病
感染
小分子化药
ADC
化学药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 9 |
| ADC | 3 |
| 化学药 | 1 |
关联
13
项与 江苏亚虹医药科技股份有限公司 相关的药物靶点- |
作用机制 光敏剂 |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 英国 [+22] |
首次获批日期2005-03-01 |
靶点 |
作用机制 METAP2抑制剂 [+1] |
在研机构 |
在研适应症 |
非在研适应症 |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 USP1抑制剂 |
在研机构 |
原研机构 |
在研适应症 |
最高研发阶段临床1/2期 |
首次获批国家/地区- |
首次获批日期- |
18
项与 江苏亚虹医药科技股份有限公司 相关的临床试验NCT06787950
A Phase I/IIa Clinical Study to Evaluate the Safety, Tolerability, Pharmacokinetics, Anti-tumor Activity of ASN-3186 in Patients with Advanced Solid Tumors.
This is a Phase I/IIa, open-label, multi-center, dose-escalation, and expansion study to evaluate the safety, tolerability, PK and preliminary anti-tumor activity of ASN-3186 when given orally in subjects with advanced solid tumors
开始日期2025-02-20 |
申办/合作机构 |
NCT06435039
A Phase 1, Open-Label, Randomized, Crossover Study to Evaluate the Safety, Tolerability and Pharmacokinetics of Single Ascending Doses of APL-1501 ER Capsules Compared to APL-1202 IR Tablets in Healthy Volunteers
The primary objective of the study is to assess safety and tolerability following administration of single doses of APL-1202 (immediate release) IR tablets and APL-1501 extended release (ER) capsules in healthy participants.
开始日期2024-06-21 |
申办/合作机构  Syneos Health, Inc. Syneos Health, Inc. [+1] |
NCT06034015
A Phase 1, Two-Part, Open-Label Study to Evaluate the Safety, Tolerability and Pharmacokinetics (PK) of Single Ascending Doses of APL-1501 Extended Release (ER) Capsules Compared to APL-1202 Immediate Release (IR) Tablets in Healthy Volunteers (Part A) and Multiple Ascending Doses of APL-1501 ER Capsules Compared to APL-1202 IR Tablets in Healthy Volunteers (Part B)
This is an integrated Phase 1, single centre, 2-part, open-label, dose-escalation study conducted in healthy volunteers to assess the safety, tolerability, and PK of APL-1501 ER capsules in comparison to APL-1202 IR tablets.
开始日期2023-09-09 |
申办/合作机构 |
100 项与 江苏亚虹医药科技股份有限公司 相关的临床结果
登录后查看更多信息
0 项与 江苏亚虹医药科技股份有限公司 相关的专利(医药)
登录后查看更多信息
1
项与 江苏亚虹医药科技股份有限公司 相关的文献(医药)2024-07-01·CELLULAR IMMUNOLOGY
Dopamine β-hydroxylase shapes intestinal inflammation through modulating T cell activation
Article
作者: Pan, Ke ; Lv, Jing ; Li, Heng ; Chen, Alice ; Bai, Yanfeng ; Shi, Weilin ; Sun, Qiaoling
BACKGROUND:
Inflammatory bowel disease (IBD) is a chronic and relapsing disease characterized by immune-mediated dysfunction of intestinal homeostasis. Alteration of the enteric nervous system and the subsequent neuro-immune interaction are thought to contribute to the initiation and progression of IBD. However, the role of dopamine beta-hydroxylase (DBH), an enzyme converting dopamine into norepinephrine, in modulating intestinal inflammation is not well defined.
METHODS:
CD4+CD45RBhighT cell adoptive transfer, and 2,4-dinitrobenzene sulfonic acid (DNBS) or dextran sodium sulfate (DSS)-induced colitis were collectively conducted to uncover the effects of DBH inhibition by nepicastat, a DBH inhibitor, in mucosal ulceration, disease severity, and T cell function.
RESULTS:
Inhibition of DBH by nepicastat triggered therapeutic effects on T cell adoptive transfer induced chronic mouse colitis model, which was consistent with the gene expression of DBH in multiple cell populations including T cells. Furthermore, DBH inhibition dramatically ameliorated the disease activity and colon shortening in chemically induced acute and chronic IBD models, as evidenced by morphological and histological examinations. The reshaped systemic inflammatory status was largely associated with decreased pro-inflammatory mediators, such as TNF-α, IL-6 and IFN-γ in plasma and re-balanced Th1, Th17 and Tregs in mesenteric lymph nodes (MLNs) upon colitis progression. Additionally, the conversion from dopamine (DA) to norepinephrine (NE) was inhibited resulting in increase in DA level and decrease in NE level and DA/NE showed immune-modulatory effects on the activation of immune cells.
CONCLUSION:
Modulation of neurotransmitter levels via inhibition of DBH exerted protective effects on progression of murine colitis by modulating the neuro-immune axis. These findings suggested a promising new therapeutic strategy for attenuating intestinal inflammation.
1,135
项与 江苏亚虹医药科技股份有限公司 相关的新闻(医药)2025-07-31
·氨基观察
氨基观察-创新药组原创出品作者 | 黄恺自免药王销售额大爆发。7月31日,赛诺菲公布2025H1业绩,上半年总营收198.89亿欧元,同比增长9.9%。赛诺菲的王牌产品度普利尤单抗(Dupixent)势头正猛,前六个月畅销73.12亿欧元(约80.15亿美元,+20.7%)。同一天,Argenx公布2025H1业绩,FcRn靶向新药Efgartigimod上半年大卖17.39亿美元,同比增长98%。艾伯维继续买买买。彭博新闻社周三援引知情人士的话说,艾伯维AbbVie正在谈判收购私营心理健康治疗公司Gilgamesh Pharmaceuticals,交易价值约10亿美元。在过去的一天里,国内外医药市场还有哪些热点值得关注?让氨基君带你一探究竟。/ 01 /市场速递1)药监局公开征求《互联网药品医疗器械信息服务备案管理规定(征求意见稿)》意见7月31日,据国家药监局消息,为贯彻落实《国务院关于修改和废止部分行政法规的决定》(中华人民共和国国务院令第797号)和《国务院关于深化“证照分离”改革进一步激发市场主体发展活力的通知》(国发〔2021〕7号),国家药监局组织起草了《互联网药品医疗器械信息服务备案管理规定(征求意见稿)》,现向社会公开征求意见。公开征求意见的时间是2025年7月31日—8月30日。/ 02 /医药动态1)海思科创新药HSK3486获FDA上市许可申请受理7月31日,海思科公告, HSK3486(环泊酚注射液)新药上市申请(NDA)符合FDA药品注册的有关要求,决定予以受理。2)亚虹医药创新药APL-1401Ⅰb期临床试验获积极初步结果7月31日,亚虹医药公告,APL-1401用于治疗中重度活动性溃疡性结肠炎的Ⅰb期临床试验获得了积极的初步结果。该研究剂量爬坡已完成,展现出良好的安全性,并在仅4周治疗周期中观察到积极的疗效信号。3)微芯生物CS231295片临床试验申请获得FDA批准7月31日,微芯生物公告,收到FDA签发的关于AuroraB选择性抑制剂CS231295开展治疗晚期实体瘤的I期临床试验的通知。4)华奥泰生物注射用HB0043获临床许可7月31日,据CDE官网,华奥泰生物注射用HB0043获临床许可,拟开展治疗化脓性汗腺炎的研究。/ 03 /海外药闻1)艾伯维拟收购Gilgamesh彭博新闻社周三援引知情人士的话说,艾伯维AbbVie正在谈判收购私营心理健康治疗公司Gilgamesh Pharmaceuticals,交易价值约10亿美元。2)度普利尤上半年销售额80亿美元7月31日,赛诺菲公布2025H1业绩,上半年总营收198.89亿欧元,同比增长9.9%。赛诺菲的王牌产品度普利尤单抗(Dupixent)势头正猛,前六个月畅销73.12亿欧元(约80.15亿美元,+20.7%)。3)Efgartigimod上半年大卖17.4亿美元7月31日,Argenx公布2025H1业绩,FcRn靶向新药Efgartigimod上半年大卖17.39亿美元,同比增长98%。PS:欢迎扫描下方二维码,添加氨基君微信号交流。
并购申请上市财报
2025-07-30
曾被誉为“欧洲市值之王”的诺和诺德,如今正遭遇前所未有的滑铁卢。撰文| Erin7月29日,市值一度“捅破天”的诺和诺德,股价暴跌21%,令一众股民彻夜难眠。如果将时间线拉长,真相更是“扎心”。过去一年,这家一度超越LVMH等消费品大亨、被誉为“欧洲市值最强王者”的制药巨头,市值一路从6350亿美元的巅峰滑落至了2394亿美元,整整蒸发了近4000亿美元。这个曾靠司美格鲁肽缔造“神药神话”的超级玩家,也正被现实按下价值重估键。而GLP-1“双姝”中的另一位——礼来,也应声下跌5.6%,市值一夜间跳水近400亿美元。去年,GLP-1凭借降糖减重“双王牌”、缔造庞大适应证“帝国”的能力,俨然成为资本市场最炙手可热的“黄金赛道”。从二级市场到上游供应链,从MNC巨头到Biotech,无不围绕它构建起“下一个百亿爆款”的商业故事。但一年过去,随着诺和诺德接连曝出临床研发受挫、业绩增长疲软、指引下调等利空信号,GLP-1产业链也迎来情绪逆转。资本正在重新审视:GLP-1还能火多久?增长是否已经触顶?头部玩家的剧烈震荡,是否意味着一个周期的更迭临近?“神药”的光辉,开始闪烁出危险信号。纵览现美股市值TOP50的制药企业,唯剩GLP-1“双姝”,以及深陷“中年危机”的再生元,还在“逆势滑坡”。欧洲市值大王的价值重估时刻仅一年时间,诺和诺德的市值就从超6300多亿美元高峰,跌至如今仅剩三分之一,是自身实力的衰落?还是市场给的预期过于膨胀?一切的起点其实可以追溯回2009年。彼时,礼来凭借全球首个GLP-1药物艾塞那肽率先占据优势,对诺和诺德在全球糖尿病巨头的地位形成了不小的威胁。但很快,诺和诺德以利拉鲁肽反击成功,重夺糖尿病治疗领域的话语权。而后来诺和诺德又再次“自己战胜自己”推出了更长效的司美格鲁肽,被称为“史上最好的糖尿病药物”。司美格鲁肽如同传奇一样的存在,上市首个完整年度(2018年)销售额仅4亿美元,到了2024年就已高达292.96亿美元,年复合增长率达154.6%。要知道,K药自2015年登陆市场,到2024年创下销售高峰,10年时间的年复合增长率也不过53.1%。爆炸性增长的背后,是诺和诺德对GLP-1赛道的重仓:从注射、口服到“超”长效制剂,从控糖、减重延伸至CKD、心血管、抗炎乃至MASH等更多适应证,每一次延展都在持续强化其市场壁垒。2023年,摩根大通更新预测:到2032年,礼来与诺和诺德将共占全球GLP-1类产品近90%的市场份额。市场对司美格鲁肽的未来充满想象,而对诺和诺德的预期也被无限拔高。然而,预期爬得越高,现实落差也将越大。过高的未来预期导致一点风吹草动,表现在诺和诺德的二级市场股票上可能就是一场风暴。2024年上半年,司美格鲁肽销售额达129.6亿美元,同比增速达两位数,表现出超越K药的态势,诺和诺德市值也在此刻冲上6350亿美元历史最高点。但几乎就在同一时间,这家巨头悄然迎来了命运的分界点。内部研发上,适应证拓展、新药开发临床进展开始不及预期;与此同时,外部又给的压力太大了——礼来持续在GIP/GLP-1双靶点药物替尔泊肽和口服药GLP-1药物Orforglipron的临床上屡获突破,两大原因导致诺和诺德市值在过去一年间“跌跌不休”,加上昨天暴跌的21%,如今,诺和诺德市值仅有2394.43亿美元,也就是说,仅仅1年时间就蒸发掉将近4000亿美元。临床进展的“滑铁卢”成为第一根导火索。2024年9月,诺和诺德发布新一代减重产品Monlunabant治疗肥胖与代谢综合征的2a期临床结果,尽管在高剂量组中体重确有下降,但效果远未达到市场预期,股价随即下跌近6%。而真正的重击来自2024年末,被寄予厚望的CagriSema未能达到业界期待的25%减重效果,仅为22.7%。市场情绪骤然转向,当天美股收盘,诺和诺德股价大跌17.82%,市值蒸发625亿美元,创下公司历史最大单日跌幅。风声鹤唳之下,每一个变量都被放大。今年4月,礼来再度发布Orforglipron临床结果,根据市场分析,作为全球首个成功完成III期研究的口服小分子GLP-1药物,Orforglipron的减重效果直逼甚至超越诺和诺德注射剂型Ozempic。诺和诺德股价当天应声下挫超10%。市场也愈发焦虑:司美格鲁肽的“神药”地位还撑多久?接二连三的临床数据不尽人意、竞争者步步紧逼,最终演化为公司层面的震荡。今年5月16日,诺和诺德董事会决定,让CEO周赋德卸任。两个月后,新的CEO上任。同时,公司发布公告,下调全年预期:虽然上半年营收增长18%(按固定汇率计算,下同),利润增长29%,但全年预期大幅下调至营收增长8%-14%,营业利润增长10%-16%,这两组数字在两个月前还是13%-21%和16%-24%。对此,投资者的心态“崩不住”了。一切像是一场连锁反应:临床数据不及预期-股价暴跌-投资者信心动摇-高管更替-增长下调-股价再跌。截至7月29日收盘,诺和诺德市值仅剩2394亿美元,一年时间,蒸发近4000亿美元。 推荐阅读 *美国最大PBM“站队”诺和诺德,礼来大跌10%,GLP-1“双姝”价格战开打!*大变天!2030年全球制药TOP10:礼来登顶,辉瑞“垫底”,BMS、GSK掉队!“霸主”失速,还带崩了谁?有意思的是,在诺和诺德的剧烈下跌带动下,29日收盘时,其竞争对手礼来也应声下跌5.6%。曾几何时,“礼来市值何时突破万亿美元”还是行业争相押注的话题,而如今,这一近在咫尺的梦想显出“镜花水月”之像,其市值也从2024年8月底的超9100亿美元高点,跌至目前的7230亿美元,短短一年蒸发逾1800亿美元。市场对GLP-1“霸主”的热情,似乎正在降温。从整体来看,美股市值TOP50的制药企业在经历了年初的普遍下行后,大多于年中迎来不同程度的修复反弹。无论是经历过内部调整的强生、削减开支的BMS,还是饱受业绩下滑困扰的GSK和福泰制药,即便在研发与业绩方面不及预期,二级市场情绪也在缓慢修复。可以说,全球资本市场对制药行业的整体信心正逐步回暖。唯独GLP-1主线上的两家家企业——诺和诺德、礼来,以及深陷“中年危机”的再生元,仍在“逆势滑坡”。据悉,再生元在过去一年时间中,市值蒸发超700亿美元。而市值跳水的背后其实也是产品青黄不接的困境:曾凭借阿柏西普、度普利尤单抗打造“爆款神话”,如今却7年未能推出新重磅产品,加上2025年Q1仅实现30.29亿美元营收,创下自2023年以来最差单季度表现,更加反映出产品线后继乏力的困境。更具风向标意义的是,诺和诺德的失速已开始向整个GLP-1产业链下游传导。例如,在司美格鲁肽销售高峰期曾大为受益的A股多肽“概念股”们,如诺泰生物、常山药业、圣诺生物等,在今天均出现不同程度下跌,截至收盘,分别下挫0.16%、2.4%、5.27%。资本对GLP-1板块的信心出现明显松动。但值得注意的是,尽管二级市场陷入调整,这些企业的基本面却依然稳健。根据诺泰生物、圣诺生物发布的2025年上半年业绩预告,诺泰预计归母净利润为3亿至3.3亿元,同比增长32.06%-45.27%;圣诺生物则预计归母净利润7702.75万元至9414.48万元,同比大幅增长253.54%-332.1%。无论是订单体量还是利润释放,GLP-1赛道的“红利余温”仍在持续。不过,需要警醒的是,一边是制药巨头业绩指引下调、市值承压,一边是产业链企业仍在兑现红利,矛盾背后,并非单一企业的问题,而是一场由“神药光环”缔造的估值神话,正在遭遇集体重估。诺和诺德的剧烈震荡,或许只是压垮市场情绪的第一根引线,真正被点燃的,是过度乐观、层层加码的GLP-1“神话”本身。过去几年,这条赛道被资本赋予了想象力满满的预期,而如今,现实以业绩数字的形式开始反噬,新的估值逻辑正在重写。从高涨热情下的预期走向冷静,也是将是一个进入新周期的拐点,这个拐点可能开始了。一审| 黄佳二审| 李芳晨三审| 李静芝精彩推荐大事件 | IPO | 融资&交易 | 财报季 | 新产品 | 研发日 | 里程碑 | 行业观察 | 政策解读 | 深度案例 | 大咖履新 | 集采&国谈 | 出海 | 高端访谈 | 技术&赛道 | E企谈 | 新药生命周期 | 市值 | 新药上市 | 商业价值 | 医疗器械 | IND | 周年庆大药企 | 竞争力20强 | 恒瑞 | 石药 | 中生制药 | 齐鲁 | 复星 | 科伦 | 翰森 | 华润 | 国药 | 云南白药 | 天士力 | 华东 | 上药创新药企 | 创新100强 | 百济 | 信达 | 君实 | 复宏汉霖 | 康方 | 和黄 | 荣昌 | 亚盛|康宁杰瑞|贝达|微芯|再鼎|亚虹跨国药企|MNC卓越|辉瑞|AZ|诺华|罗氏|BMS|默克|赛诺菲|GSK|武田|礼来|诺和诺德|拜耳供应链|赛默飞|药明|凯莱英|泰格|思拓凡|康龙化成|博腾|晶泰|龙沙|三星启思会 | 声音·责任 | 创百汇 | E药经理人理事会 | 微解药直播 | 大国新药 | 营销硬观点 | 投资人去哪儿 | 分析师看赛道 | 药事每周谈 | 中国医药手册
2025-07-29
全球营收TOP10大药企有半数都已加入COPD赛道混战,谁能突围而出?撰文| Kathy7月28日,恒瑞与GSK达成重磅合作,将共同开发至多12款创新药物。值得一提的是,协议包含一款潜在同类最优PDE3/4抑制剂(HRS-9821)的授权许可,该产品目前正处于慢性阻塞性肺疾病(COPD)治疗的临床开发阶段。短短20天,COPD赛道,突然之间变得刀光剑影。前有默沙东豪掷百亿并购,后有GSK霸气出手,并购、BD交易直接指向同一目标——COPD。这原本被视作研发“死亡谷”的领域,一夜之间成为全球资本与创新的焦点。COPD仅次于心血管疾病和肿瘤,是全球第三大致死原因,却因为疾病复杂、药物选择有限而长期缺乏突破。几十年间,制药巨头在这里折戟无数,TNF-α、CXCR2、PI3K等曾被寄予厚望的靶点接连失败,从近了说,就在默沙东和GSK“买买买”之际,罗氏正遭遇着一条COPD管线的失利。但“风浪越大,鱼越贵”,药企依然前赴后继至此,尤其是2024年以来的一连串事件改变了COPD的沉寂。先是Verona Pharma的全球首个PDE 3/4抑制剂恩塞芬汀上市;紧接着赛诺菲/再生元的度普利尤单抗在COPD适应证的成功,让这一沉寂已久的江湖迎来了新希望。资本闻风而动,COPD从冷门赛道变成了MNC掰手腕的竞技场:跨国巨头们高举资金长刀时,中国力量也在崛起,开始与MNC同场比武,尤其是当GSK“相中”恒瑞后,会不会有下一个大BD,发生在中国公司身上?MNC的刀锋已至COPD“沉默杀手”并非虚名。《柳叶刀·呼吸医学》研究显示,COPD是仅次于心血管疾病和癌症,稳居全球第三大致死原因。传统治疗依赖吸入性支气管扩张剂(LABA、LAMA)及糖皮质激素(ICS)三联疗法。它们能缓解症状、延缓病程,却无法逆转肺功能下降。患者依从性低、副作用显著、耐药性问题突出,且难以覆盖所有表型患者。尤其在急性加重阶段,现有药物的防控力有限,每一次急性加重都可能让患者的肺功能“掉下悬崖”,加速疾病走向不可逆。这种“高发病、高死亡、高未满足”的特征,使COPD成为全球最庞大、却最被低估的慢病市场之一。正因如此,每一次新药突破都带来资本与产业的巨大震荡。2024年GOLD指南首次承认精准靶向药物的价值,将Verona Pharma的PDE 3/4抑制剂恩塞芬汀与再生元/赛诺菲度的IL4Rα单抗普利尤单抗纳入推荐,意味着COPD的治疗策略正从“症状控制”走向“病程干预”,从“粗放”走向“精准”。这或许也是跨国药企开始重新审视COPD赛道的一次重要节点。而COPD赛道格局真正开始发生变化,还是要从过去这短短二十天的两笔重磅交易说起。7月9日,默沙东豪掷100亿美元收购Verona Pharma。Verona的核心产品正是恩塞芬汀,可以说默沙东来了一记后发制人的重拳。默沙东在呼吸领域并非主角,但拿下恩塞芬汀后,局面出现改变。作为全球首个PDE3/4抑制剂,恩塞芬汀兼具支气管扩张和抗炎双重作用,成功突破过去PDE4抑制剂副作用高、疗效有限的困局。自上市以来,恩塞芬汀仅8个月的销售额已突破1亿美元,预计峰值销售接近40亿美元。曾有分析师评价,这一产品的意义可类比当年IL-17抑制剂之于银屑病。而GSK对恒瑞的出手,则可以看作是呼吸领域“老江湖”的翻盘谋算。就在默沙东官宣收购后的20天,GSK以125亿美元和恒瑞医药达成共同开发至多12款创新药物的合作,其中最受关注的就是其中包含的同类最优的PDE3/4抑制剂HRS-9821的授权许可。GSK是呼吸领域的传统霸主,但近年来用于COPD治疗的全再乐(Trelegy)面临专利悬崖,市场压力剧增。进入2025年以来,GSK也开始重新布局和发力。其一是美泊利珠单抗(Nucala),通过精准患者分型在MATINEE试验中成功“翻盘”,在FDA获批作为辅助维持治疗,用于伴有嗜酸性粒细胞表型、病情控制不佳的成人COPD患者。第二步,便是重金签下恒瑞的HRS9821,锁定PDE3/4抑制剂里的下一个潜力药王。与此同时,赛诺菲、阿斯利康、罗氏也不甘示弱。赛诺菲凭度普利尤单抗率先进入COPD的生物制剂市场,阿斯利康和罗氏则在IL-33、TSLP、ST2等靶点修炼。风起之际,暗潮涌动,每一步棋都可能改变未来格局。默沙东与GSK已经出手了,谁将是下一个被资本下注的项目? 推荐阅读 * 涨停!默沙东700亿并购带飞的A股“小恒瑞”,成色几何?* 自免疯狂内卷,赛诺菲登顶,罗氏、诺华“狂飙”,谁压力山大?恒瑞之后,谁能突围“死亡谷”COPD研发的高风险几乎成为行业共识。过去二十年,新药研发屡屡折戟,PDE4抑制剂罗氟司特因副作用限制使用,TNF-α抑制剂在晚期临床失利,总体来看,大多数靶点虽有理论基础,但在II/III期试验中纷纷未达预设终点。即便成功者,也几乎是在失败后调整策略才重获新生。赛诺菲/再生元的度普利尤单抗是COPD首个生物靶向药,2024年7月率先在欧盟获批,通过靶向IL4/IL13通路,实现针对嗜酸性粒细胞型COPD的精准治疗。到2024年9月该适应证获得NMPA批准。但赛诺菲在这一赛道的研发也并非一帆风顺,另一重磅IL-33单抗Itepekimab在一项关键试验中失利。GSK曾在十几年前研发一款COPD创新项目256066,临床试验显示体外效力极高,但在轻度COPD患者中未能检测到炎症标志物的统计学显著变化,最终从GSK的研发管线中消失。今年5月,GSK在FDA获批上市的另一款新药——IL-5抗体Nucala在COPD赛道也曾经遭遇波折,其有两项III期研究,由于未能区分嗜酸性粒细胞亚群,都曾以失败告终。此后,GSK调整了临床试验策略,其中,命名为MATINEE的试验将入组人群精准锁定为高嗜酸粒细胞计数(≥300个/μL)的患者,并且排除了哮喘患者,才得以从这片“死亡谷”中逃出。阿斯利康围绕COPD也进行了广泛布局,同时推进了IL-5抗体、IL-33抗体、TSLP抗体等多款新药的COPD临床试验。其中Tezspire(TSLP单抗)在COPD的IIa期临床中获得优异疗效,并在2024年8月获得FDA的突破疗法认证。但另一款IL-33单抗托佐瑞单抗(tozorakimab)则在2024年9月的一项COPD II期研究中未能达到主要终点。罗氏也喜忧参半。IgG2单克隆抗体(mAb)阿斯特戈利单抗(astegolimab)在IIb期ALIENTO研究(NCT05037929)中,该药物达到了其主要终点——即在52周时显著降低年化急性加重率(AER)。然而,在III期ARNASA试验(NCT05595642)中,未能达到相同的首要终点。往更远了说,罗氏的口服PDE4抑制剂如罗氟司特,虽然获批用于部分重度COPD患者,但由于全身性副作用严重限制了临床应用。就在MNC前赴后继之时,中国本土药企亦在奋起追赶。无疑,恒瑞凭借最新交易成为了当下COPD赛道的焦点。其HRS9821在I期研究中已验证了其耐受性、安全性与药代特征。加之GSK 此次合作还包括另外11个早期项目,也被看作是恒瑞与全球TOP级MNC的深度绑定。恒瑞也因此在港股应声大涨24.54%,A股直接涨停。不只是恒瑞,中国力量正在从COPD的边缘角色演变为主角。这笔交易还带来了海思科的涨停、中国生物制药港股大涨7.09%。正大天晴的在研管线TQC3721的进度仅次于恩塞芬汀,吸入混悬液已完成 II 期临床,2025年6月10日获批 III 期临床,而吸入粉雾剂处于 I 期研究阶段。海思科的 HSK39004 吸入混悬液和吸入粉雾剂均处于 II 期临床阶段,进度稍慢于正大天晴。推动中国药企加速研发的原因自然离不开巨大的市场潜力。具体来看,在中国,COPD患者数量高达1亿,并且曾有统计,中国COPD患者中超过70%尚未被确诊,即使确诊者,规范化治疗率也不足30%。这意味着在诊断、治疗、管理等各个环节,都存在巨大的空白和未满足需求。对中国企业而言,属于COPD的刀锋也已经亮起。不论是默沙东的100亿还是GSK的125亿,都只是序幕。随着研发进入后期的管线越来越多,还会有更多刀光剑影:PDE3/4之后,下一个改变游戏规则的疗法会是谁?MNC会不会继续高价收购?中国创新能否持续跑出?属于COPD的江湖故事才刚刚开始。一审| 黄佳二审| 李芳晨三审| 李静芝精彩推荐大事件 | IPO | 融资&交易 | 财报季 | 新产品 | 研发日 | 里程碑 | 行业观察 | 政策解读 | 深度案例 | 大咖履新 | 集采&国谈 | 出海 | 高端访谈 | 技术&赛道 | E企谈 | 新药生命周期 | 市值 | 新药上市 | 商业价值 | 医疗器械 | IND | 周年庆大药企 | 竞争力20强 | 恒瑞 | 石药 | 中生制药 | 齐鲁 | 复星 | 科伦 | 翰森 | 华润 | 国药 | 云南白药 | 天士力 | 华东 | 上药创新药企 | 创新100强 | 百济 | 信达 | 君实 | 复宏汉霖 | 康方 | 和黄 | 荣昌 | 亚盛|康宁杰瑞|贝达|微芯|再鼎|亚虹跨国药企|MNC卓越|辉瑞|AZ|诺华|罗氏|BMS|默克|赛诺菲|GSK|武田|礼来|诺和诺德|拜耳供应链|赛默飞|药明|凯莱英|泰格|思拓凡|康龙化成|博腾|晶泰|龙沙|三星启思会 | 声音·责任 | 创百汇 | E药经理人理事会 | 微解药直播 | 大国新药 | 营销硬观点 | 投资人去哪儿 | 分析师看赛道 | 药事每周谈 | 中国医药手册
并购引进/卖出申请上市
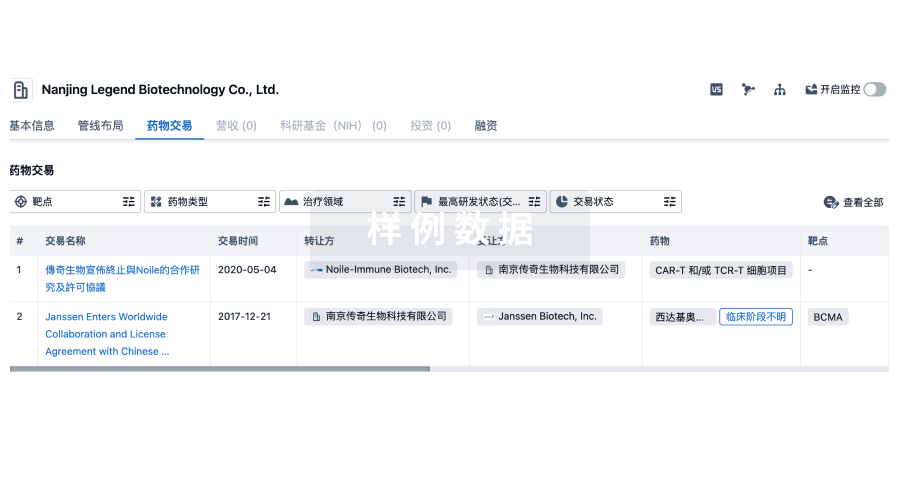
100 项与 江苏亚虹医药科技股份有限公司 相关的药物交易
登录后查看更多信息
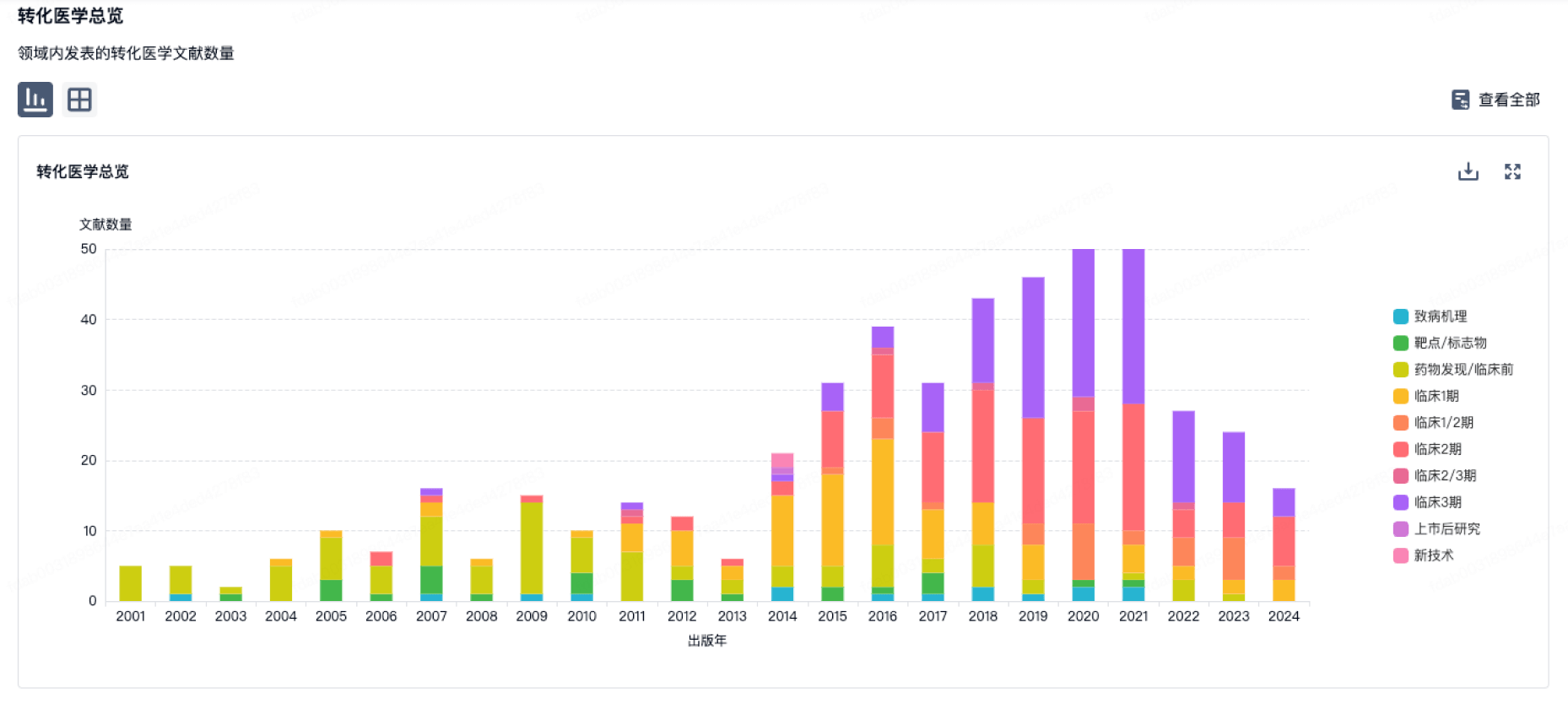
100 项与 江苏亚虹医药科技股份有限公司 相关的转化医学
登录后查看更多信息
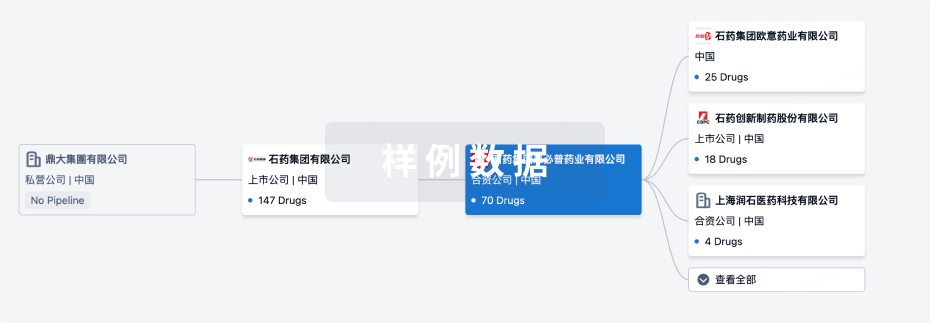
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月07日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
7
3
临床1期
临床2期
1
1
临床3期
批准上市
1
8
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
盐酸六氨基-γ-酮戊酸 | 宫颈鳞状上皮内病变 更多 | 申请上市 |
硝羟喹啉 ( METAP2 ) | 肌层浸润性膀胱癌 更多 | 临床1/2期 |
AT-012(Asieris Pharmaceuticals) ( USP1 ) | 晚期恶性实体瘤 更多 | 临床1/2期 |
APL-1301 ( METAP1 x METAP2 ) | 泌尿道感染 更多 | 临床1期 |
APL-1401 ( CD8 x DBH ) | 溃疡性结肠炎 更多 | 临床1期 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
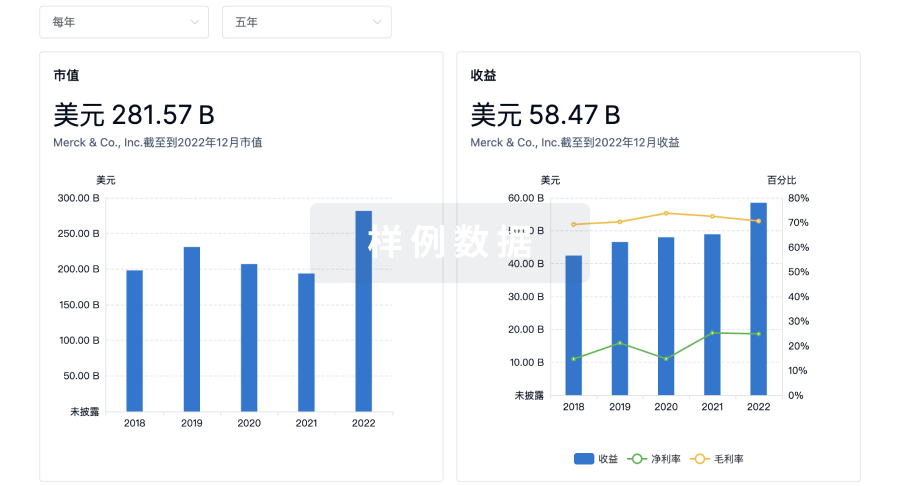
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
