预约演示
更新于:2025-05-07
Alpha-Thalassemia
α地中海贫血
更新于:2025-05-07
基本信息
别名 A-Thalassemia、ALPHA-THALASSEMIA、Alpha Thalassemia + [39] |
简介 A disorder characterized by reduced synthesis of the alpha chains of hemoglobin. The severity of this condition can vary from mild anemia to death, depending on the number of genes deleted. |
关联
19
项与 α地中海贫血 相关的药物靶点 |
作用机制 PKLR激动剂 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2022-02-17 |
作用机制 ACVR2B抑制剂 [+1] |
在研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2019-11-08 |
靶点 |
作用机制 SGLT2抑制剂 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2017-12-19 |
255
项与 α地中海贫血 相关的临床试验NCT06731166
Effectiveness of Video Monitoring and Care Transition for Heart Failure Patients (EVIT-HF): Randomized Clinical Trial
The goal of this clinical trial is to measure the effectiveness of video monitoring associated with the transition of care for patients with heart failure.
The main questions it aims to answer is: Is video monitoring superior to monitoring via audio calls in patients with heart failure?
Researchers will compare monitoring by video to a monitoring by audio to see if drug videomonitoring works to improve selfcare in heart failure and other outocomes.
Participants will:
intervention group receive video calls guided by cardiologist nurses at 7, 30, 60, 180 and 365 days after hospital discharge.
the control group will receive audio calls for data collection, at the same time mentioned.
The main questions it aims to answer is: Is video monitoring superior to monitoring via audio calls in patients with heart failure?
Researchers will compare monitoring by video to a monitoring by audio to see if drug videomonitoring works to improve selfcare in heart failure and other outocomes.
Participants will:
intervention group receive video calls guided by cardiologist nurses at 7, 30, 60, 180 and 365 days after hospital discharge.
the control group will receive audio calls for data collection, at the same time mentioned.
开始日期2025-06-01 |
申办/合作机构 |
NCT06892171
The Study of the Phenotype of Hereditary Xerocytosis
Hereditary xerocytosis is a dominant red blood cell membrane disorder characterized by an increased leakage of potassium from the interior to the exterior of the red blood cell membrane, leading to water loss, red cell dehydration, and chronic hemolysis. In 90% of cases, it is associated with heterozygous gain-of-function mutations in PIEZO1, a gene that encodes a mechanotransducer responsible for converting mechanical stimuli into biological signals. The remaining 10% of cases are linked to mutations in the GARDOS channel gene.
开始日期2025-03-01 |
NCT06591936
Genetic Profile of Alpha Thalassemia Children at Sohag University Hospital .
Genetic profile of alpha thalassemia children at sohag university hospital ,the aim to determine the prevelance , molecular character of the disorder, characterized by decreased synthesis of alpha -globin Recent work to provide mechanisms for phenotypic heterogeneity .
开始日期2024-08-01 |
申办/合作机构 |
100 项与 α地中海贫血 相关的临床结果
登录后查看更多信息
100 项与 α地中海贫血 相关的转化医学
登录后查看更多信息
0 项与 α地中海贫血 相关的专利(医药)
登录后查看更多信息
17,833
项与 α地中海贫血 相关的文献(医药)2025-12-31·Annals of Medicine
Prognostic value of remnant-like particle cholesterol in ischemic heart failure patients following percutaneous coronary intervention
Article
作者: Zhang, Biyang ; Dong, Shutong ; Chen, Zheng ; Ma, Meishi ; Sun, Tienan ; Zhao, Zehao ; Huang, Xin ; Zhou, Yujie
2025-12-31·Hematology
A rare −α
27.6
deletion compounded with the hemoglobin constant spring mutation identified in a Chinese couple
Article
作者: Xiao, Yan ; Zeng, Si-Fan ; Guo, Zhao-Yi ; Long, Min ; Li, Wei ; Xiu, Zi-Han ; Liu, Li-Yi ; Chen, Yu-Chen ; Zhang, Jing ; Zhang, Min
2025-12-31·Hematology
Comprehensive Hematological and molecular Characterization of hemoglobin Hekinan [α27(B8)Glu→Asp(α1),
HBA1
:c.84G > T] in a Large Thai cohort
Article
作者: Prapphal, Manussavee ; Suksusut, Amornchai ; Uaprasert, Noppacharn ; Jaitheang, Jidapa ; Rojnuckarin, Ponlapat ; Sutcharitchan, Pranee
94
项与 α地中海贫血 相关的新闻(医药)2025-04-12
·学术经纬
撰文 | 李雯婕 责编 | 周叶斌神经母细胞瘤是一种源于发育中周围神经系统的恶性肿瘤,具有高度异质性的分子特征和临床治疗结局。尽管采用了多模式综合治疗,高危神经母细胞瘤患者的生存率仍仅约50%,治疗现状不容乐观。部分高危患者中具有特定的分子特征,如节段性染色体畸变、MYCN扩增以及14%的患者存在ALK改变(突变/扩增)。复发的神经母细胞瘤中ALK和RAS-MAPK通路突变频率也显著升高。以往研究对于亚克隆突变在诊断时的临床意义尚未明确,不同回顾性研究由于采用的方法不同、对低频变异的检测灵敏度各异,导致相关报道存在矛盾。此外,克隆性与亚克隆性RAS 通路、TP53突变以及ATRX异常的预后意义也尚未见报道。近日,Yael P. Mossé等人在 Journal of Clinical Oncology 上发表题为 Frequency and Clinical Significance of Clonal and Subclonal Driver Mutations in High-Risk Neuroblastoma at Diagnosis: A Children's Oncology Group Study 的论文,采用统一、高灵敏度和特异性的超深度测序方法,对已完成的COG III期ANBL0532试验中的关键神经母细胞瘤相关基因进行检测,明确这些基因异常的发生率及其对患者预后的影响,定义具有预后意义的变异等位基因频率(VAF)阈值,为临床治疗决策提供更可靠的依据。首先,作者统计分析了242例高危神经母细胞瘤患者的基线特征。从分期来看,ALK异常患者中III期和IV期占比远高于ALK野生型患者,提示ALK状态可能与疾病进展相关。MYCN扩增在ALK异常患者中更常见,且二者共同发生对预后影响大。其次,作者运用定制的NGS panel,检测发现38%的患者肿瘤存在致病改变。其中,ALK异常的比例为24.8%,包括21.5%的激活突变和3.3%的异常扩增。RAS通路突变占7.9%,TP53致病性变异占4.5%,ATRX功能缺失性异常占9%。上述数据表明,多种基因的异常在高危神经母细胞瘤中较为常见,为后续研究这些异常与患者预后的关系提供了重要依据,也提示针对这些基因异常开发靶向治疗方案的潜在方向。再次,作者聚焦于ALK和RAS-MAPK通路变异(VAF≥5%)对高危神经母细胞瘤患者预后的影响。研究表明,携带任何ALK异常的患者预后较差,5年无事件生存率(EFS)和总生存率(OS)低于ALK野生型患者。其中,ALK扩增患者预后尤其不佳。携带VAF≥5%激活型ALK突变的患者,其EFS和OS也明显低于野生型。对于RAS通路,虽然整体突变组与野生型组无差异,但VAF≥5%的激活突变患者预后更差。这表明ALK和RAS-MAPK通路特定变异与不良预后相关,为临床风险评估和治疗决策提供了关键依据。图1:携带ALK突变患者的VAF分层预后图:携带RAS突变患者的VAF分层预后MYCN扩增与ALK异常在高危神经母细胞瘤中经常同时出现,且这种共现预示着较差的预后。同时存在MYCN扩增和ALK突变(VAF≥5%)的患者,5年EFS和OS明显低于MYCN扩增但ALK野生型的患者。不过,ALK突变(VAF≥5%)在无 MYCN 扩增的肿瘤中对预后的影响,因患者数量少难以定论。这表明 MYCN 扩增与 ALK 异常的共现是影响患者预后的重要因素,对评估病情和制定治疗策略有重要意义。图:MYCN扩增和ALK突变并存患者的EFS和OS由于TP53突变患者数量较少,对其预后影响的评估受限。而ATRX异常似乎对预后影响不明显,携带ATRX异常的患者与ATRX野生型患者相比,5年EFS和OS差异均无统计学意义。但总体样本量有限,这些结论仍需进一步研究验证。综上所述,本研究确定了高危神经母细胞瘤诊断时潜在可治疗的基因异常发生率,发现ALK改变的总体发生率高于以往报道,且不同ALK突变对患者预后影响不同。同时,该研究表明MYCN扩增与ALK突变共现频率较高,这类患者预后差,研究支持将VAF≥5%作为ALK异常患者接受ALK靶向药物劳拉替尼治疗的标准。此外,该研究强调了对高危神经母细胞瘤患者进行早期分子分层的重要性,为识别超高危患者和开发创新疗法提供依据。 撰文 责编 制作排版 | 车洁 校对 | uu延伸阅读针对难治恶性脑瘤的潜在 “first-in-class” 抗癌小分子有望在今年完成新药审评!*本文由深圳市拾玉儿童公益基金会“儿童肿瘤前沿”团队编译或约稿,文中图表均源引自文献原文。本文著作权归文章作者所有,欢迎个人转发分享,未经允许禁止转载,作者拥有所有法定权利,违者必究。如需转载,请留言或联系shiyu@curekids.cn。本文旨在分享儿童肿瘤科研前沿成果,不是治疗方案推荐。如需获得疾病治疗方案指导,请前往正规医院就诊。▼滑动查看更多▼原文摘要(Abstract)Purpose: Relapsed high-risk neuroblastomas (NBLs) are enriched for targetable mutations in ALK and RAS-MAPK pathways, yet the prognostic effect of these aberrations and relevance of subclonal mutations at diagnosis remain undefined. We describe the spectrum and clinical significance of clonal and subclonal pathogenic alterations in high-risk NBL.Methods: We developed a focused high-risk NBL sequencing panel including ALK, NRAS, KRAS, HRAS, BRAF, PTPN11, TP53, and ATRX genes for ultra-deep sequencing and applied this assay to 242 pretherapy tumors from patients enrolled on the phase III trial Children's Oncology Group ANBL0532. We assessed the effect of clonal and subclonal mutations on event-free survival (EFS) and overall survival (OS).Results: ALK-activating mutations occurred in 21.5% of tumors (n = 52, 30 clonal, 22 subclonal), and 3.3% (n = 8) showedALKamplification. EFS and OS for patients with anyALK-aberrant tumor were inferior to patients with wild-type (WT)ALKtumors (5-year OS 37.7%v66.3%; hazard ratio [HR], 1.992;P= .0007). EFS and OS for patients with tumors harboring activatingALKmutations ≥5% variant allele frequency (VAF) were inferior toALKWT (5-year OS 37.7%v66.3%; HR, 1.966;P= .0041). The 5-year EFS and OS for patients withALK-amplified tumors were 25.0%. RAS pathway mutations occurred in 7.9% of tumors (n = 19; four clonal, 15 subclonal), with EFS and OS for those with VAF ≥5% inferior to RAS-WT patients (5-year OS 19.1%v60.0%; HR, 3.021;P = .0168).Conclusion: Ultra-deep sequencing of high-risk NBLs demonstrates that oncogenic aberrations are more prevalent at diagnosis than previously recognized. ALK and RAS pathway aberrations confer inferior outcomes in patients treated with contemporary therapy, emphasizing the need for novel therapeutic approaches.DOI: 10.1200/JCO-24-02407👇点击此处,直达原文
临床3期临床结果申请上市AACR会议临床终止
2025-03-19
学术成果、战略签约、荣誉表彰......
三月激荡着上药人的昂扬斗志
研发创新、工业制造、商业流通
各板块开启“快进键”
奏响春日里的奋斗交响曲
上药研究院与上海市免疫治疗创新研究院开展融合交流
为深化“产学研医”合作,释放上海医药在全链条创新药发展实施过程中的企业内生动力,推动创新成果产业化,3月11日,依托创新免疫治疗全国重点实验室 ,上海市免疫治疗创新研究院执行院长、全重实验室副主任鲁林荣一行到访上药研究院,开展第一次学术交流和党建共建签约仪式。未来双方将共促党建与业务同频共振,拓展并深耕医药产业链党建联盟“朋友圈”,进一步加强合作纽带,共同推动医药创新与免疫治疗领域的发展,为我国生物医药产业发展贡献力量。
上药睿尔发表α-地中海贫血项目临床前研究成果
上药睿尔科研团队通过移植携带双α等位基因敲除的胚胎肝细胞到经辐射处理后的C57BL/6野生型小鼠体内,成功建立了国内首个具有α-地中海贫血特征的成年小鼠模型,这种模型在国内尚属首次,为后续研究提供了新的思路和方法。该团队不仅系统揭示了基于胚胎肝细胞移植技术构建α-地中海贫血小鼠模型的全流程方法学体系,并通过详实数据呈现包括血液学参数谱与多维度生理指标在内的完整表征,从而为后续α-地中海贫血研究提供严谨的技术参照体系与数据基准。相关研究内容发表在《Scientific Reports》,该学术期刊主要发表来自自然科学、心理学、医学和工程学领域的原创研究,是全球引用次数第五多的期刊。
上药第一生化与亚瑟医药签订战略合作协议
3月7日,上药第一生化与亚瑟医药举行战略合作签约仪式。本次战略签约是上药第一生化与亚瑟医药产品合作的起点,双方就合作的愿景、目标和实施方案进行了深入的交流与探讨,并达成了广泛的共识。此次合作将充分发挥双方在技术创新、原料制剂一体化、产业化应用及国际化等领域的优势,进一步整合资源,响应市场需求变化,推动科研成果落地,提升企业核心竞争力。
上药杏灵、上药中西荣获全国“安康杯”竞赛表彰
近期,中华全国总工会、应急管理部、国家卫生健康委员会联合印发了《关于表彰2022—2023年度全国“安康杯”竞赛先进集体和优秀个人的决定》(总工发 〔2025〕1号)。上海上药杏灵科技药业股份有限公司获全国“安康杯”竞赛优秀组织单位,上海中西三维药业有限公司硫酸羟氯喹班组获全国“安康杯”竞赛优胜班组。
《中国创新药械多元支付白皮书(2025)》发布
日前,由中国人寿再保险有限责任公司、上海镁信健康科技集团股份有限公司、波士顿咨询公司联合编写,由南开大学-镁信健康精算科技实验室提供学术支持,共同研究形成的《中国创新药械多元支付白皮书(2025)》正式发布。在国家倡导建立多层次保障体系的大背景下,构建创新药械的多元支付机制对患者、医疗卫生系统及社会价值巨大。作为上海医药旗下的创新孵化平台,镁信健康将与业界各方携手,不断助力健康中国建设迈向新台阶。
上药控股(山东)器械大健康平台正式投入运营
3月10日,上药(山东)医疗器械有限公司开业庆典在济南市槐荫区德迈国际信息产业园举行。公司将以本次庆典仪式为契机,以高水平一体化协同为舵,以专业化和科技创新为帆,坚定不移推进器械大健康省级平台建设战略目标达成,知重负重、勇挑大梁,奋力谱写器械大健康业态高质量发展新篇章。
上药云健康再获重磅认证
3月14日,上药控股下属上药云健康数字科技(上海)有限公司,正式宣布成功通过上海市科学技术委员会、上海市财政局、国家税务总局上海市税务局的联合评审,荣获《高新技术企业证书》(GR202431002422)。这是继上药云健康2023年入选“上海市专精特新中小企业”后,在科技创新领域获得的又一重要国家级资质认证。
山东省聊城市人民政府副市长祁学兰考察调研上药厦中
3月17日,山东省聊城市人民政府副市长祁学兰一行莅临上药厦中考察调研。祁副市长一行参观了公司中药制剂现代化生产基地,认真了解“新癀片”等产品的制药工序,对公司在技术创新、精益生产、质量体系建设等方面取得的工作成果予以充分肯定。漫步本草园,双方进行了真诚友好的沟通,共同展望未来,期待建立更加紧密、深入的合作交流。
免疫疗法
2025-02-28
今天是第18个国际罕见病日(Rare Disease Day),今年的主题是“More Than You Can Imagine”(中文主题:不止罕见),呼吁社会不仅关注罕见病本身,更要看到罕见病患者背后所展现出的无限生命力与可能性。正序生物原创碱基编辑疗法帮助全球β-血红蛋白病患者摆脱输血依赖,让罕见病患者实现“一次治疗,终身治愈”,焕发生命活力。
▲ 2025年国际罕见病日的主题海报(图源 rarediseaseday.org)
罕见病,又称“孤儿病”,是指流行率很低、很少见的疾病,通常为慢性、严重性疾病,常危及生命。根据世界卫生组织(WHO)的定义,罕见病是指患病率低于总人口0.65‰~1‰的疾病。据公开资料显示,全球已确认的罕见病超过7000种,其中包括地中海贫血症、镰刀型细胞贫血病、渐冻症、血友病、多发性硬化症、脊髓性肌萎缩症等。约80%的罕见病为遗传性疾病,全球罕见病患者约为3亿,我国罕见病患者超过2000万。
地中海贫血症与镰刀型细胞贫血病
地中海贫血症(Thalassemia)和镰刀型细胞贫血病(Sickle Cell Disease,SCD)是两种常见的遗传性血红蛋白病,均已被全球和中国纳入罕见病目录。
地中海贫血症主要分为α-地中海贫血和β-地中海贫血两种类型,全球范围内尤其在东南亚、地中海沿岸国家、中东地区以及我国南方地区发病率较高。据统计,东南亚地区约有3亿人携带地中海贫血症突变基因。
镰刀型细胞贫血病则是由于β-珠蛋白基因突变使红细胞呈镰刀状的遗传性疾病,全球约有3.5%的人口携带其突变基因,每年约有30万名婴儿出生时患有此病。该病在非洲、地中海地区、中东和印度等地区发病率较高,但在全球范围内仍符合罕见病的定义。
我国分别于2018年将镰刀型细胞贫血病纳入《第一批罕见病目录》、2023年将地中海贫血(重型)纳入《第二批罕见病目录》,旨在提高公众认知、推动政策支持,同时加速针对罕见病的技术开发和临床应用。
正序生物原创变形式碱基编辑技术为罕见病患者带来希望
近年来,随着基因编辑技术的飞速发展,碱基编辑技术(Base Editing)为罕见病的治疗带来了新的希望。作为全球领先的碱基编辑技术公司,正序生物利用自主知识产权的变形式碱基编辑器(transformer Base Editor,tBE)开发的创新疗法在罕见病治疗领域取得了突破性进展。
正序生物针对β-地中海贫血症开发的碱基编辑药物CS-101已在多例国内外患者中展现出卓越的疗效和安全性,成功帮助患者摆脱输血依赖,回归正常生活。快速、安全、长效的临床结果使CS-101具有成为全球最好(Best-in-Class)基因编辑药物和全球首创(First-in-Class)碱基编辑药物的潜力。同时,针对镰刀型细胞贫血病的IIT研究也在全球范围内稳步推进。该疗法不仅为β-地中海贫血症和镰刀型细胞贫血病患者带来了新的希望,也为其他罕见病的治疗提供了新的思路。
正序生物将持续致力于中国原创碱基编辑技术的临床转化,快速推进碱基编辑药物上市,为全球罕见病患者带来彻底治愈的曙光。
基因疗法临床研究
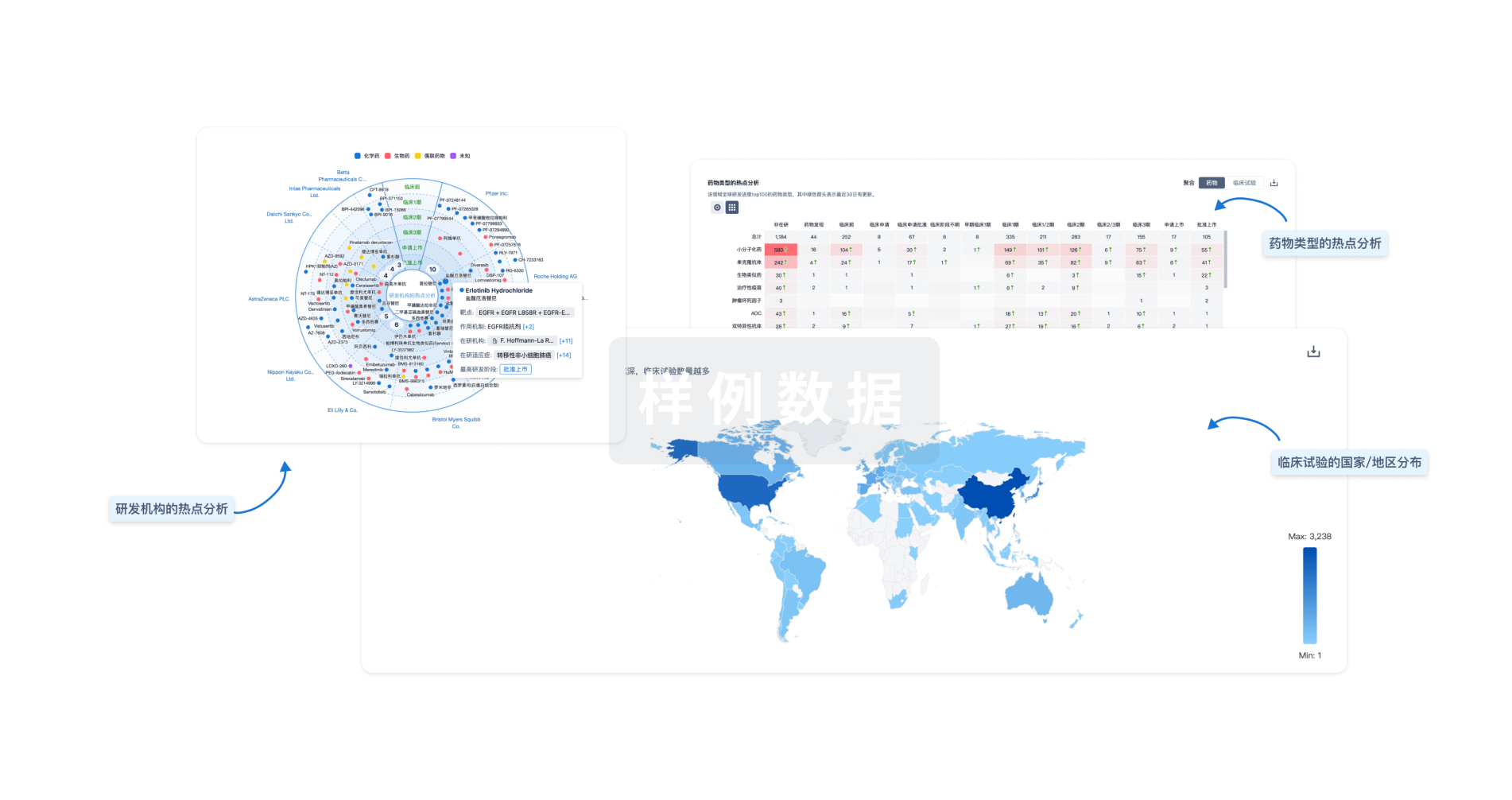
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用