预约演示
更新于:2025-05-07
Cervical Squamous Cell Carcinoma
宫颈鳞状细胞癌
更新于:2025-05-07
基本信息
别名 CERVICAL CANCER SQUAMOUS CELL、Carcinoma;cervix;squam cell、Cervical Squamous Cell Carcinoma + [38] |
简介 A squamous cell carcinoma arising from the cervical epithelium. It usually evolves from a precancerous cervical lesion. Increased numbers of sexual partners and human papillomavirus (HPV) infection are risk factors for cervical squamous cell carcinoma. Survival is most closely related to the stage of disease at the time of diagnosis. |
关联
37
项与 宫颈鳞状细胞癌 相关的药物作用机制 TOP1抑制剂 [+1] |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2024-11-22 |
靶点 |
作用机制 PD-1抑制剂 |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2019-12-26 |
靶点 |
作用机制 PD-1抑制剂 [+2] |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2019-05-29 |
116
项与 宫颈鳞状细胞癌 相关的临床试验ChiCTR2500101118
Efficacy and safety study of Camrelizumab in combination with neoadjuvant chemotherapy and concurrent chemoradiotherapy for locally advanced cervical cancer
开始日期2025-05-06 |
申办/合作机构- |
ChiCTR2500101420
A single-arm, single-center, open, prospective phase II clinical study of camrelizumab combined with nimotuzumab and first-line chemoradiotherapy for the treatment of recurrent and metastatic cervical cancer
开始日期2025-05-01 |
申办/合作机构- |
ChiCTR2500100115
To investigate the significance of vaginal scrubbing before amputation in abdominal radical hysterectomy of cervical cancer
开始日期2025-04-15 |
申办/合作机构- |
100 项与 宫颈鳞状细胞癌 相关的临床结果
登录后查看更多信息
100 项与 宫颈鳞状细胞癌 相关的转化医学
登录后查看更多信息
0 项与 宫颈鳞状细胞癌 相关的专利(医药)
登录后查看更多信息
4,414
项与 宫颈鳞状细胞癌 相关的文献(医药)2025-12-31·RNA Biology
Circular RNA Circ_0002762 promotes cell migration and invasion in cervical squamous cell carcinoma via activating RelA/nuclear factor kappa B (Nf-kB) signalling pathway
Article
作者: Ji, Lei ; Chen, Xiaoping ; Chen, Youguo
2025-08-01·Cellular Signalling
GRHL3 specifically initiated by the TP63 transcription factor promotes the metastasis of squamous cell carcinogenesis
Article
作者: Jana, Debnarayan ; Yan, Xi ; Wei, Sisi ; Bai, Hanyu ; Gao, Feng ; Wang, Dachi ; Zhao, Lianmei ; Xue, Yongxian ; Zhou, Wei ; Dai, Suli ; Wei, Xiaojian
2025-06-01·Modern Pathology
Cervical Human Papillomavirus–Independent Squamous Cell Carcinoma: A Clinicopathological Review and Outcomes Analysis Compared With Human Papillomavirus–Associated Squamous Cell Carcinoma
Article
作者: Roma, Andres ; Devins, Kyle M ; Allison, Douglas ; Turashvili, Gulisa ; Regauer, Sigrid ; Fadare, Oluwole ; Felix, Ana ; Dieguez, Nuria Carreras ; Morató, Alba ; Ieni, Antonio ; McCluggage, W Glenn ; Zannoni, Gian Franco ; Mateoiu, Claudia ; Erbagci, Ahmet ; Horn, Lars-Christian ; Ali-Fehmi, Rouba ; Parra-Herran, Carlos ; Patrichi, Andrei ; Pesci, Anna ; Mills, Anne ; Rakislova, Natalia ; Stolnicu, Simona ; Hoang, Lien ; Guerra, Esther ; Soslow, Robert A ; Ordi, Jaume ; Kir, Gozde ; Oliva, Esther ; Kheil, Mira
21
项与 宫颈鳞状细胞癌 相关的新闻(医药)2025-04-26
·今日头条
【导读】
宫颈鳞状细胞癌(CESC)是女性中最常见的癌症之一,放疗一直被用作主要治疗手段。然而,其疗效受到固有和获得性放射抵抗的限制。
4月22日,温州医科大学研究团队在期刊《Cell Death Discovery》上发表了研究论文,题为“HSP90 regulates dCK stability and inhibits ionizing radiation-induced ferroptosis in cervical cancer cells”,本研究中,研究人员发现dCK通过提高 SLC7A11 的活性和稳定性来抑制胰岛素抵抗(IR)诱导的铁死亡。利用数据库,研究人员预测 NEDD4L 可能是 dCK 的潜在泛素连接酶,而 WWP1/2 可能是 NEDD4L 的潜在泛素连接酶。本研究结果表明,HSP90通过招募泛素连接酶 WWP1/2 抑制 NEDD4L,从而调节 dCK 的稳定性。
总之,本研究揭示了 HSP90-WWP1/WWP2-NEDD4L-dCK-SLC7A11 轴是 HeLa 细胞中 IR 诱导铁死亡的关键调节因子。这些发现为宫颈癌的放射增敏潜在策略提供了宝贵的见解。
https://www-nature-com.libproxy1.nus.edu.sg/articles/s41420-025-02388-x#Abs1
背景知识
01
宫颈鳞状细胞癌(CESC)是全球育龄妇女癌症死亡的第二大原因。放疗一直是宫颈癌的主要治疗方法,尤其是对于局部晚期病例。然而,其固有的和获得的放射抵抗性导致预后不良,这在临床环境中是一个紧迫的问题。作为一种细胞毒性疗法,电离辐射(IR)通过在肿瘤细胞中诱导 DNA 双链断裂(DSBs)来发挥其治疗作用。当暴露于高能 IR 时,肿瘤细胞被破坏,导致各种类型的细胞死亡。铁死亡是一种最近发现的铁依赖性非凋亡性细胞死亡形式,其特征是细胞毒性脂质过氧化物的积累。许多研究表明,铁死亡在诸如放疗等癌症治疗中具有前景。然而,放疗与宫颈癌铁死亡之间的关系仍未明确。
dCK敲低促进了 HeLa 细胞的放射敏感性
02
研究人员分析了癌症基因组图谱(TCGA)数据库中dCK的表达水平,并证实其在宫颈鳞状细胞癌(CESC)组织中显著升高。通过 Kaplan-Meier 曲线显示,dCK 水平高与 CESC 患者的不良预后相关。结果表明 dCK 的上调具有时间依赖性。因此,研究人员通过转染 dCK shRNA 构建了稳定的 HeLa 细胞敲低模型,并检测了转染效率。经辐射照射后,dCK 敲低细胞在 48 小时的细胞死亡率显著增加。此外,dCK 敲低显著抑制了暴露于辐射的 HeLa 细胞的增殖。同样,集落形成实验表明 dCK 敲低增加了 HeLa 细胞的放射敏感性。综上所述,这些结果表明 dCK 敲低促进了辐射诱导的细胞死亡,并增强了 HeLa 细胞的放射敏感性。
dCK敲低促进了辐射诱导的 HeLa 细胞铁死亡
03
众所周知,辐射可导致多种细胞死亡形式。为了确定辐射处理后诱导的细胞死亡类型,研究人员将不同的细胞死亡抑制剂应用于 dCK 敲低的 HeLa 细胞。随后,这些细胞接受了 4 Gy 的辐射。Fer-1 减轻了辐射诱导的细胞死亡,这表明 dCK 敲低可能促进辐射诱导的铁死亡。
研究人员进行了多项测试以确认 dCK 敲低是否促进辐射诱导的铁死亡。正如预期的那样,与对照组相比,dCK 敲低的 HeLa 细胞内 Fe2+浓度显著升高;这种效应可能因辐射治疗而增强。然后,与 shControl 相比,经辐射或厄拉司汀处理后,通过 BODIPY C11 染色检测到的 dCK 敲低 HeLa 细胞的脂质过氧化显著增加,而这一现象可通过 Fer-1 逆转。此外,研究人员发现经辐射处理后,dCK 敲低的 HeLa 细胞中 PTGS2(铁死亡标志物)的 mRNA 表达增加,在铁死亡诱导剂和氧化应激诱导剂处理的细胞中也观察到了这种升高。同样,GPX4 的 mRNA 水平降低。这些发现表明,辐射诱导的铁死亡因 dCK 敲低而得到促进。
dCK敲低促进了辐射诱导的铁死亡
结论
04
通过本研究,研究人员得出结论:dCK可能是提高 HeLa 细胞放射敏感性的新治疗靶点,HSP90抑制剂可能有助于提高宫颈癌放疗的效果。
参考资料:
https://www-nature-com.libproxy1.nus.edu.sg/articles/s41420-025-02388-x#Abs1
【关于投稿】
转化医学网(360zhyx.com)是转化医学核心门户,旨在推动基础研究、临床诊疗和产业的发展,核心内容涵盖组学、检验、免疫、肿瘤、心血管、糖尿病等。如您有最新的研究内容发表,欢迎联系我们进行免费报道(公众号菜单栏-在线客服联系),我们的理念:内容创造价值,转化铸就未来!
转化医学网(360zhyx.com)发布的文章旨在介绍前沿医学研究进展,不能作为治疗方案使用;如需获得健康指导,请至正规医院就诊。
责任声明:本稿件如有错误之处,敬请联系转化医学网客服进行修改事宜!
微信号:zhuanhuayixue
热门推荐活动 点击免费报名
🕓 浙江|2025年5月9日
▶ 首届精准医学国际学术研讨会暨队列研究先锋计划颁奖仪式
🕓 上海|2025年6月12-15日
▶ 第七届上海国际癌症大会暨第十八届全国医学生物技术研讨会暨第六届中德双边论坛
🕓 上海|2025年7月17-18日
▶ 第四届长三角体外诊断产业高峰论坛
🕓 北京|2025年9月19-20日
▶ 第六届单细胞技术应用研讨会暨空间组学前沿研讨会
🕓 上海|2025年11月14-15日
▶ 第二届中国类器官转化医学大会
点击对应文字 查看详情
细胞疗法
2025-04-03
导语:2025 年 4 月,百济神州对外宣布,由于独立数据监测委员会判定其抗 TIGIT 抗体药物 ociperlimab 在非小细胞肺癌(NSCLC)的 III 期临床试验中难以达到总生存期(OS)这一主要终点,公司决定终止该药物的全球研发。这一消息的公布,不仅让 TIGIT 靶点的研发进程再次受挫,也让肿瘤免疫疗法领域的研发困境浮出水面 —— 在过去 4 年里,该靶点已累计投入超过 200 亿美元,但至今仍未取得突破性的临床成果。一、临床试验折戟:从寄予厚望到黯然退场试验设计与结果:此次开展的 AdvanTIG - 302 试验,旨在评估 ociperlimab 联合 PD - 1 抑制剂 Tevimbra,与默克 Keytruda 相比,在 PD - L1 高表达非小细胞肺癌患者中的疗效。中期分析结果显示,试验 “极有可能失败”,不过并未发现新的安全问题。行业影响:这是 2025 年 TIGIT 领域遭遇的第二例重大失败,此前罗氏的 tiragolumab 已在三项 III 期试验中败北。诺华曾在 2021 年以 3 亿美元的首付款引进 ociperlimab,然而两年后,由于 “风险收益比不理想”,便将权益退还给了百济神州。如今百济神州的放弃,进一步降低了该靶点的价值。二、靶点开发困境:机制复杂与竞争加剧TIGIT 的 “双重角色”:TIGIT 作为一种免疫检查点分子,既能够抑制 T 细胞的活化,又可以促进调节性 T 细胞(Tregs)的功能。这种复杂的机制使得药物设计的难度远远超过了 PD - 1/PD - L1。临床数据表明,TIGIT 抑制剂单药治疗的有效率不足 15%,而联合疗法则需要在 “毒性 - 疗效” 之间找到平衡。研发竞赛的 “幸存者偏差”:全球有 12 家药企在 TIGIT 领域投入了超过 200 亿美元,但仅有 2 款药物进入了 III 期试验,其中 40% 的项目已经终止开发。罗氏、GSK 等行业巨头仍在尝试联合疗法(如 TIGIT + PD - L1),但早期数据显示,有效率仅提升了 5 - 8%。三、行业反思:靶点选择与研发策略百济神州的战略转向:公司表示,将把资源集中在 “具有临床差异化的候选药物” 上,例如 BCL - 2 抑制剂、TROP2 ADC 等,并计划在 2025 年提交 6 项新药申请(NDA)。其 PD - 1 抑制剂 Tevimbra 在 2024 年的销售额达到了 28 亿美元,但目前正面临着同类药物的激烈竞争。行业专家观点:Mark Lanasa(百济神州):“我们必须对研发管线进行优化,将精力集中在能够真正改变患者预后的项目上。”行业分析师:Jefferies 指出,TIGIT 靶点需要重新评估,“它可能仅适用于特定的肿瘤微环境或者联合治疗”。四、未来展望:肿瘤免疫疗法的 “新战场”技术突破方向:双特异性抗体(如 TIGIT×CD3)、CAR - T 细胞疗法(如靶向 TIGIT 的 CAR - T)正在兴起,初步数据显示,有效率提升至 30%。表观遗传调控技术(如 EZH2 抑制剂)或许能够重塑肿瘤免疫微环境,为 TIGIT 药物提供新的发展机遇。市场趋势:2025 年,全球肿瘤免疫疗法市场预计将达到 1800 亿美元,而 TIGIT 靶点的占比不足 2%。投资者开始转向其他新兴靶点,如 LAG - 3、TIM - 3,相关的融资额同比增长了 45%。结语随着 ociperlimab 临床试验的终止,TIGIT 靶点的开发神话彻底破灭。这场研发马拉松给我们带来了深刻的教训:在追求 “下一代免疫疗法” 的热潮中,科学理性必须超越商业预期。而这,或许正是肿瘤免疫疗法迈向新阶段的必经之路。参考来源:https://www.biospace.com/business/beigene-scraps-tigit-candidate-after-underwhelming-lung-cancer-data识别微信二维码,添加生物制品圈小编,符合条件者即可加入生物制品微信群!请注明:姓名+研究方向!版权声明本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观不本站。
免疫疗法临床3期抗体药物偶联物细胞疗法引进/卖出
2025-02-26
·药时空
在漫长的抗癌历史中,人类首次看到了彻底消除一种癌症的曙光,这种癌症就是宫颈癌。
宫颈癌严重威胁着全球女性的健康。世界卫生组织数据显示,全球每年约有50万新增宫颈癌病例,约25万人因此失去生命,平均每两分钟就有一位女性确诊,每分钟就有一人离世。在中国,情况同样不容乐观,每年新增病例约12万,死亡约5万,并且近年来发病率呈上升趋势,发病年龄也逐渐年轻化。
不过,人类在对抗宫颈癌的征程中取得了重大突破。2006年,首个HPV疫苗诞生,这一成果意义非凡。美国20-24岁女性的宫颈癌发病率显著下降,2005-2012年降幅为33%,2012-2019年更是高达65%。2016年,HPV疫苗在中国获批,截至目前,中国已有5款HPV疫苗产品获批注册,包括3款进口和2款国产疫苗。但从中国免疫规划信息管理系统数据来看,2018-2020年,9-45岁适龄女性累计接种HPV疫苗2159.74万剂次,累计估算接种率仅为2.24%。
01 致病根源:HPV的深度解析
宫颈癌的发病原因十分明确,主要是由人乳头瘤病毒(HPV)的持续感染引起的。这一发现为人类战胜宫颈癌指明了方向。
宫颈由三种不同类型的上皮组成:宫颈外侧的复层鳞状上皮、宫颈内侧的单层柱状上皮和两者之间的转化区(图2)。鳞状上皮和柱状上皮之间的边界称为鳞柱交界处(SCJ)。在育龄妇女中,阴道偏酸的微环境刺激子宫颈柱状上皮发生鳞状化生,SCJ中的干细胞(储备细胞)被认为参与了这种转化。原始SCJ和新SCJ之间的区域称为转换区(TZ)。
图1:宫颈结构。宫颈由三种不同类型的上皮细胞组成。鳞状上皮和柱状上皮之间的边界称为鳞柱交界(SCJ)。储备细胞位于宫颈SCJ的基底层。SCJ:鳞柱交界处,TZ:转化区。
HPV是一种双链环状DNA病毒,“家族成员”众多,目前已发现超过200种亚型,可分为低危型和高危型。低危型HPV相对“温和”,主要引发一些良性病变,如生殖器疣。而高危型HPV则是导致宫颈癌的“罪魁祸首”,其中HPV16和HPV18型最为凶险,大约70%的宫颈癌病例都与它们的持续感染有关。
表1:致癌的HPV类型及比例
高危型HPV的危险源于其携带的特殊基因,如E6和E7基因。E6基因编码的蛋白质能与细胞内的p53蛋白结合,使p53蛋白失去抑癌功能,就像解除了细胞的“警报系统”,让细胞DNA损伤无法得到及时修复,从而容易发生癌变。E7基因编码的蛋白质则干扰细胞周期的正常调控,使细胞异常增殖,进一步增加了癌变风险。
表2:IARC按致癌风险对HPV进行的分组
HPV主要通过性接触传播,当皮肤或黏膜出现微小破损时,它便会趁机而入,瞄准上皮细胞,尤其是宫颈部位的黏膜上皮细胞。进入细胞后,HPV利用细胞内的物质和机制进行DNA复制。在这个过程中,如果人体免疫系统无法及时清除被感染细胞,随着病毒不断复制,细胞会逐渐发生异常变化,从正常细胞发展为癌前病变,最终可能恶变成宫颈癌。不过,从HPV感染到发展成宫颈癌,通常需要数年甚至数十年,这为预防和干预提供了时间窗口。
图2:宫颈癌的发生机制。A. 宫颈鳞状细胞癌与腺癌的发生机制。B.持续HPV感染期间,HPV基因组被整合到人基因组中。HPV整合有助于HPV E6/E7的持续表达,并引发各种基因改变,如癌基因扩增、染色体重排和HPV整合部位的染色体不稳定。
02 对抗武器:HPV疫苗的诞生与作用
HPV疫苗的问世,是人类抗击宫颈癌历程中的一个重要里程碑。它的研发过程凝聚了众多科研人员的心血。上世纪70年代,德国科学家哈拉尔德・楚尔・豪森提出宫颈癌可能由HPV感染引起的猜想,当时这一观点并未被广泛接受,但他坚持研究,最终在80年代初发现了多种与宫颈癌密切相关的病毒亚型,为HPV疫苗的研发奠定了理论基础。1991年,中国科学家周健和澳大利亚免疫学家伊恩・弗雷泽取得重大突破,发现HPV病毒的L1蛋白和L2蛋白能在体外合成病毒样颗粒(VLP),这些颗粒虽无传染性和致病性,却能激发人体免疫系统产生抗体,为疫苗研发开辟了新路径。
2006年,默沙东公司的四价HPV疫苗Gardasil率先在美国上市,可预防HPV6、11、16和18型病毒感染;2007年,葛兰素史克公司的二价HPV疫苗Cervarix在欧洲上市;2014年,默沙东的九价HPV疫苗Gardasil9获批,能预防90%以上的宫颈癌。在中国,2016年葛兰素史克的二价HPV疫苗获批进入市场,随后默沙东的四价、九价疫苗也相继获批,2019年国产二价HPV疫苗馨可宁上市,打破了国外疫苗的垄断局面,2022年沃森生物的二价HPV疫苗沃泽惠也成功上市。目前国内获批上市的HPV疫苗共有5种。不同的疫苗,适用人群和接种程序略有不同。
表3:国内获批上市的HPV疫苗
2025年1月8日,默沙东(MAD)刚刚宣布,四价人乳头瘤病毒疫苗(酿酒酵母)的多项新适应证已获得中国NMPA上市批准,适用于9~26岁男性接种。新闻稿表示,新适应证的获批标志着该产品成为中国境内首个且目前唯一获批、可适用于男性的HPV疫苗。
佳达修此次获批的新适应证可适用于9-26岁男性预防因HPV16、18引起的肛门癌,HPV6和11引起的生殖器疣(尖锐湿疣),以及由HPV6、11、16、18引起的以下癌前病变或不典型病变:1级、2级、3级肛门上皮内瘤样病变(AIN)。
HPV疫苗主要以合成的L1晚期蛋白病毒样颗粒作为靶抗原。接种疫苗后,人体免疫系统会将这些颗粒识别为外来“敌人”,激活B淋巴细胞产生抗体。这些抗体如同身体的“防御部队”,当HPV病毒入侵时,能与之中和,阻止病毒感染细胞。而且,免疫系统还会产生记忆B细胞,记住HPV病毒的特征,在未来再次遇到相同病毒时,迅速产生大量抗体,实现持久的免疫防护。
HPV疫苗在全球接种后成效显著。英国自2008年为12-13岁女孩接种HPV疫苗,到2019年年中,预防了大约450例宫颈癌和17200例癌前病变。在接种人群中,不同年龄段接种的女性宫颈癌发病率都大幅降低。瑞典的研究也显示,接种HPV疫苗的群体宫颈癌发病风险明显下降。
03 推广困境:HPV疫苗接种率低的难题
尽管HPV疫苗效果显著,但在全球范围内,其接种率却不尽如人意。世界卫生组织数据显示,2023年全球女孩首剂HPV疫苗覆盖率为27%,全程接种覆盖率为20%,与2030年90%的女孩在15岁前完成全程接种的目标差距较大。中国的接种率同样不容乐观,9-45岁女性HPV疫苗首剂累计覆盖率和全程累计覆盖率较低,9-14岁女孩首剂接种率仅为4.00%。
造成接种率低的原因是多方面的。首先,许多人对HPV疫苗了解不足,不清楚HPV病毒与宫颈癌的关系,对疫苗的作用和重要性认识不够,甚至存在误解,认为接种疫苗会对身体有不良影响。其次,疫苗宣传存在问题,宣传渠道单一,内容过于专业,还容易受到不实信息干扰,比如一些自媒体传播疫苗有严重副作用、接种后会导致不孕等虚假信息,让许多人对疫苗望而却步。再者,HPV疫苗属于自费疫苗,价格相对较高,这让一些经济条件差的家庭难以承受。最后,过去HPV疫苗供应短缺,尤其是九价疫苗“一苗难求”,即使现在供应有所缓解,部分地区仍存在疫苗不足的情况。
04 全球行动:消除宫颈癌的战略与努力
面对HPV疫苗接种率低的困境,全球并未放弃消除宫颈癌的目标。2020年11月17日,世界卫生组织启动《加速消除宫颈癌的全球战略》,这是全球194个国家首次共同承诺消除一种癌症,意义非凡。该战略制定了疫苗接种、筛查和治疗三个关键措施。在疫苗接种方面,目标是到2030年让90%的女孩在15岁之前完成接种;筛查方面,计划让70%的妇女在35岁和45岁之前接受高效检测方法筛查;治疗方面,要使90%确诊宫颈疾病的妇女得到治疗。
为响应这一号召,各国纷纷行动。英国为适龄女孩提供免费接种,并扩大接种年龄范围;美国疾病控制和预防中心大力呼吁提高接种率,还开展科普宣传活动。在中国,鄂尔多斯市准格尔旗和厦门市为适龄女学生免费接种HPV疫苗,积累了宝贵经验。此外,医疗机构和社会组织也积极参与,通过义诊、讲座、公益宣传等活动普及宫颈癌防治知识,为贫困地区妇女提供免费筛查和治疗服务。
宫颈癌有望被消灭,这是人类抗癌征程中的一个重大希望。虽然目前面临着HPV疫苗接种率低等挑战,但只要加大宣传力度,提高公众对HPV疫苗的认知和接受度;优化疫苗供应,降低接种成本;加强国际合作,共同推进全球宫颈癌防治工作,就一定能够跨越这些障碍,实现消除宫颈癌的目标。
参考资料:[1]人类历史上第一次有可能消灭的癌症.药闻窗.2023年08月12日.[2]人类抗癌路上可能首个被消灭的癌症!.癌友新日记.2025年02月17日.[3]哪个HPV型别致癌性最强?JAMA最新研究来了.华大基因健康.2024年01月11日.[4]最新综述:不同HPV基因型,可能具有不同宫颈病变自然病史.光动力技术.2023年10月25日.[5]刚刚!默沙东男性HPV疫苗在华获批!.医药观澜.2025年01月08日.
识别微信二维码,可添加药时空小编
请注明:姓名+研究方向!
疫苗
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
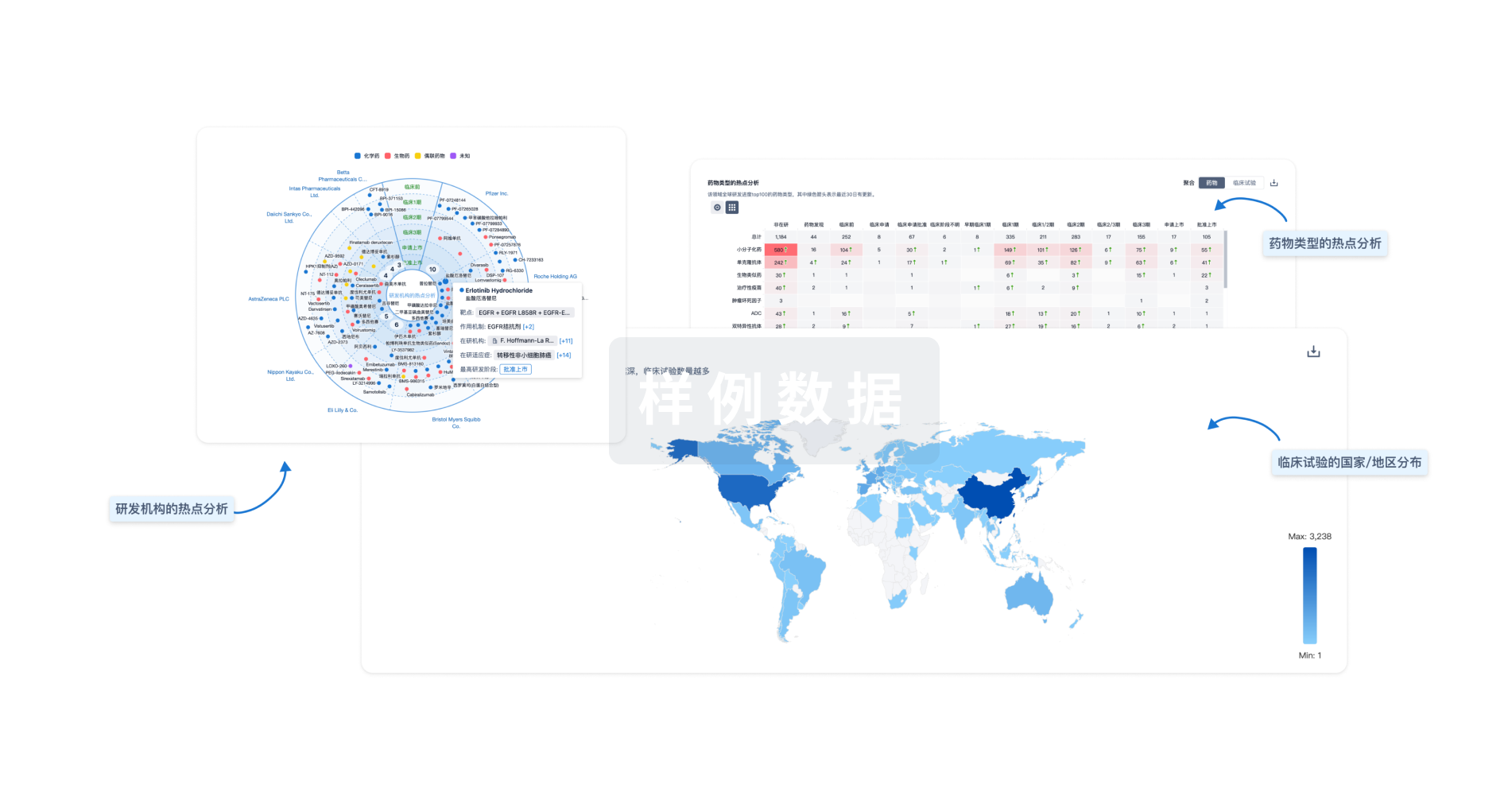
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


