预约演示
更新于:2025-08-03

TransThera Sciences (Nanjing), Inc.
更新于:2025-08-03
概览
标签
肿瘤
消化系统疾病
其他疾病
小分子化药
化学药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 13 |
| 化学药 | 2 |
关联
15
项与 药捷安康(南京)科技股份有限公司 相关的药物作用机制 Aurora A抑制剂 [+8] |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 S1PR1调节剂 |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
24
项与 药捷安康(南京)科技股份有限公司 相关的临床试验NCT07052253
An Open-label, Multicenter, Phase II Clinical Study of AK104/AK112 in Combination With TT-00420 Tablet in Patients With Advanced Hepatocellular Carcinoma.
An Open-label, Multicenter, Phase II Clinical Study of AK104/AK112 in Combination with TT-00420 Tablet in Patients with Advanced Hepatocellular Carcinoma(HCC).
开始日期2025-07-25 |
申办/合作机构  中山康方生物医药有限公司 中山康方生物医药有限公司 [+1] |
NCT06457919
A Phase 1b/2 Study Evaluating the Activity of Tinengotinib (TT-00420) in Combination With Androgen Receptor Signaling Inhibitors (ARSIs) in Patients With Metastatic Castration Resistant Prostate Cancer (mCRPC)
The purpose of this study is to find out whether tinengotinib in combination with abiraterone acetate and prednisone or enzalutamide is a safe treatment that causes few or mild side effects in people with metastatic castration-resistant prostate cancer (mCRPC).
开始日期2024-06-04 |
申办/合作机构 |
CTIS2023-505660-11-00
A Phase III, Randomized, Controlled, Global Multicenter Study to Evaluate the Efficacy and Safety of Oral Tinengotinib versus Physician’s Choice in Subjects with Fibroblast Growth Factor Receptor (FGFR) altered, Chemotherapy- and FGFR Inhibitor-Refractory/Relapsed Cholangiocarcinoma (FIRST-308) - TT420C2308
开始日期2024-04-25 |
申办/合作机构 |
100 项与 药捷安康(南京)科技股份有限公司 相关的临床结果
登录后查看更多信息
0 项与 药捷安康(南京)科技股份有限公司 相关的专利(医药)
登录后查看更多信息
4
项与 药捷安康(南京)科技股份有限公司 相关的文献(医药)2025-04-01·ANNALS OF ONCOLOGY
A model for decoding resistance in precision oncology: acquired resistance to FGFR inhibitors in cholangiocarcinoma
Article
作者: Qiang, X ; Borad, M ; Kambadakone, A R ; Shroff, R T ; Danysh, B P ; Flaherty, K T ; Leshchiner, I ; Martin, E E ; DiToro, D ; Lennerz, J K ; Saha, S K ; Lin, B ; Javle, M ; Chen, C T ; Iyer, R ; Sun, C ; Friboulet, L ; Harris, T ; Wang, H ; Reyes, S ; Li, L ; Cleary, J M ; Stone, J R ; Fan, J ; Gordan, J D ; Karasic, T ; Bensen, D C ; Iyer, S ; Kelley, R K ; Hoffman, I D ; Berchuck, J E ; Sootome, H ; Maurer, J ; Damjanov, N ; Baiev, I ; Goyal, L ; Peng, P ; Uboha, N V ; Wehrenberg-Klee, E ; Mody, K ; Parida, L ; Getz, G ; Walmsley, C ; Hollebecque, A ; Juric, D ; Nelson, K J ; Harris, W ; Majeed, U ; Zhang, K ; Zhu, A X ; Wu, F ; Facchinetti, F ; Hirai, H ; Vasseur, D ; Pinto, C
BACKGROUND:
Fibroblast growth factor receptor (FGFR) inhibitors have significantly improved outcomes for patients with FGFR-altered cholangiocarcinoma, leading to their regulatory approval in multiple countries. As with many targeted therapies, however, acquired resistance limits their efficacy. A comprehensive, multimodal approach is crucial to characterizing resistance patterns to FGFR inhibitors.
PATIENTS AND METHODS:
This study integrated data from six investigative strategies: cell-free DNA, tissue biopsy, rapid autopsy, statistical genomics, in vitro and in vivo studies, and pharmacology. We characterized the diversity, clonality, frequency, and mechanisms of acquired resistance to FGFR inhibitors in patients with FGFR-altered cholangiocarcinoma. Clinical samples were analyzed longitudinally as part of routine care across 10 institutions.
RESULTS:
Among 138 patients evaluated, 77 met eligibility, yielding a total of 486 clinical samples. Patients with clinical benefit exhibited a significantly higher rate of FGFR2 kinase domain mutations compared with those without clinical benefit (65% versus 10%, P < 0.0001). We identified 26 distinct FGFR2 kinase domain mutations, with 63% of patients harboring multiple. While IC50 assessments indicated strong potency of pan-FGFR inhibitors against common resistance mutations, pharmacokinetic studies revealed that low clinically achievable drug concentrations may underly polyclonal resistance. Molecular brake and gatekeeper mutations predominated, with 94% of patients with FGFR2 mutations exhibiting one or both, whereas mutations at the cysteine residue targeted by covalent inhibitors were rare. Statistical genomics and functional studies demonstrated that mutation frequencies were driven by their combined effects on drug binding and kinase activity rather than intrinsic mutational processes.
CONCLUSION:
Our multimodal analysis led to a model characterizing the biology of acquired resistance, informing the rational design of next-generation FGFR inhibitors. FGFR inhibitors should be small, high-affinity, and selective for specific FGFR family members. Tinengotinib, a novel small molecule inhibitor with these characteristics, exhibited preclinical and clinical activity against key resistance mutations. This integrated approach offers a blueprint for advancing drug resistance research across cancer types.
2024-04-04·The oncologist
First-In-Human Phase I Study of Tinengotinib (TT-00420), a Multiple Kinase Inhibitor, as a Single Agent in Patients With Advanced Solid Tumors
Article
作者: Rodon, Jordi A ; Ni, Shumao ; Sun, Caixia ; Fan, Jean ; Meric-Bernstam, Funda ; Piha-Paul, Sarina A ; Mott, Frank ; Xu, Binghe ; Tsimberidou, Apostolia M ; Peng, Peng ; Levin, Wendy J ; Conley, Anthony P ; Ngo, Brenda ; Ru, Qinhua Cindy ; Fan, Ying ; Dumbrava, Ecaterina E ; Wang, Hui ; Hong, David S ; Karp, Daniel D ; Ajani, Jaffer A ; Javle, Milind M ; Fu, Siqing ; Wu, Frank ; Raghav, Kanwal ; Qiang, Xiaoyan
Abstract:
Purpose:
This first-in-human phase I dose-escalation study evaluated the safety, pharmacokinetics, and efficacy of tinengotinib (TT-00420), a multi-kinase inhibitor targeting fibroblast growth factor receptors 1-3 (FGFRs 1-3), Janus kinase 1/2, vascular endothelial growth factor receptors, and Aurora A/B, in patients with advanced solid tumors.
Patients and Methods:
Patients received tinengotinib orally daily in 28-day cycles. Dose escalation was guided by Bayesian modeling using escalation with overdose control. The primary objective was to assess dose-limiting toxicities (DLTs), maximum tolerated dose (MTD), and dose recommended for dose expansion (DRDE). Secondary objectives included pharmacokinetics and efficacy.
Results:
Forty-eight patients were enrolled (dose escalation, n = 40; dose expansion, n = 8). MTD was not reached; DRDE was 12 mg daily. DLTs were palmar-plantar erythrodysesthesia syndrome (8 mg, n = 1) and hypertension (15 mg, n = 2). The most common treatment-related adverse event was hypertension (50.0%). In 43 response-evaluable patients, 13 (30.2%) achieved partial response (PR; n = 7) or stable disease (SD) ≥ 24 weeks (n = 6), including 4/11 (36.4%) with FGFR2 mutations/fusions and cholangiocarcinoma (PR n = 3; SD ≥ 24 weeks n = 1), 3/3 (100.0%) with hormone receptor (HR)-positive/HER2-negative breast cancer (PR n = 2; SD ≥ 24 weeks n = 1), 2/5 (40.0%) with triple-negative breast cancer (TNBC; PR n = 1; SD ≥ 24 weeks n = 1), and 1/1 (100.0%) with castrate-resistant prostate cancer (CRPC; PR). Four of 12 patients (33.3%; HR-positive/HER2-negative breast cancer, TNBC, prostate cancer, and cholangiocarcinoma) treated at DRDE had PRs. Tinengotinib’s half-life was 28-34 hours.
Conclusions:
Tinengotinib was well tolerated with favorable pharmacokinetic characteristics. Preliminary findings indicated potential clinical benefit in FGFR inhibitor-refractory cholangiocarcinoma, HER2-negative breast cancer (including TNBC), and CRPC. Continued evaluation of tinengotinib is warranted in phase II trials.
Yaoxue Jinzhan
Review on Cholangiocarcinoma Target Therapy
作者: Qiang Xiaoyan ; Wang Huimin ; Peng Peng ; Tian Yuwei
Cholangiocarcinoma(CCA) is a rare malignant tumor derived from uncontrolled proliferation of bile duct epithelial cells.Because of the asymptomatic early-stage manifestations, CCA is hard to diagnose until advanced stage, which is generally unresectable.The postoperative survival rate is quite low even after surgical resection.Gemcitabine combined with cisplatin is the first-line standard of care(SOC) for patients who do not need surgical resection, and their median overall survival time is less than 1 yr.In Apr. 2020, pemigatinib, an FGFR inhibitor approved by FDA, became the first target therapy for cholangiocarcinoma worldwide.This paper reviews the progress of target therapy for cholangiocarcinoma in recent years, aiming to provide reference for novel drug development and clin. practice for cholangiocarcinoma treatment.
108
项与 药捷安康(南京)科技股份有限公司 相关的新闻(医药)2025-08-02
·同写意
7月31日深夜,上交所网站悄然更新的一则信息在资本圈激起涟漪——珠海泰诺麦博制药股份有限公司(以下简称“泰诺麦博”),以科创板第五套标准递交的招股书获正式受理。这家专注于血液制品替代疗法的创新生物制药企业,成为科创板第五套标准宣布重启后,首家以此标准申请上市获得受理的企业。对此,中信证券医药首席分析师陈竹指出:从今年3月证监会党委会议指出稳妥恢复科创板第五套标准适用,到此刻,科创板第五套标准在暂停近两年后正式重启,意义重大。不仅为未盈利生物科技公司打通了融资血脉,更向市场传递出清晰的信号:中国资本市场正以前所未有的决心,为那些致力于解决人类健康难题的真正创新者铺就前行的道路。历经过去近三年的沉寂与调整,2025年,生物科技的“资本寒冬”正显现出全面解冻的迹象。科创板未盈利IPO再度开闸,港股市场生物医药企业IPO热度前所未有,企业信心逐步恢复。一连串的信号预示着,下半年,生物医药企业的IPO复苏潮仍将持续,创新药的春天正在到来!这一刻,重新站在聚光灯下的创新药企,以尖端技术为矛,借资本活水为盾,更顺畅地将科研理想的星火,熔铸成惠及全球患者的生命方舟——这或许才是资本市场与创新药产业深度融合的终极意义,也是政策暖流最终渴望抵达的彼岸。TONACEA01科创板未盈利IPO再开闸2019年,上海证券交易所新设科创板,并试点注册制,设置了五套上市标准。其中第五套标准是:“预计市值不低于人民币40亿元,主要业务或产品需经国家有关部门批准,市场空间大,目前已取得阶段性成果。医药行业企业需至少有一项核心产品获准开展二期临床试验,其他符合科创板定位的企业需具备明显的技术优势并满足相应条件”。过去两年,科创板第五套IPO窗口关闭,超30家生物医药企业撤回科创板IPO申请。今年以来,证监会多次释放“重启”信号,7月间终于迎来落地。2月7日,中国证监会发布《关于资本市场做好金融“五篇大文章”的实施意见》,指出要持续支持优质未盈利科技型企业发行上市,进一步提升对新产业新业态新技术的包容性。3月11日,中国证监会党委召开扩大会议,指出要增强制度包容性、适应性,支持优质未盈利科技企业发行上市,稳妥恢复科创板第五套标准适用,尽快推出具有示范意义的典型案例,更好促进科技创新和产业创新融合发展。直到6月18日的陆家嘴论坛上,中国证监会主席吴清明确表示:将在创业板正式启用第三套标准,支持优质未盈利创新企业上市,并重启未盈利企业适用于科创板第五套标准上市。同时在科创板创新推出6项改革措施:对于适用科创板第五套标准的企业,试点引入资深专业机构投资者制度;面向优质科技企业试点IPO预先审阅机制;扩大第五套标准适用范围,支持人工智能、商业航天、低空经济等更多前沿科技领域企业适用;支持在审未盈利科技企业面向老股东开展增资扩股等活动;完善科创板公司再融资制度和战略投资者认定标准;增加科创板投资产品和风险管理工具等。7月1日,采用该套标准上市的禾元生物,成为首家重启后获上市委会议通过的企业,并在7月4日提交注册,7月18日注册生效。之后,北芯生命也很快提交注册并生效。到现在,泰诺麦博上市申请获受理——未盈利生物医药企业IPO“开闸”逐步落实,企业直接融资渠道畅通,一级市场退出的“堰塞湖”也有望缓解。对此,陈竹分析指出,优质未盈利的生物医药等行业公司的融资通道打开,体现出国家对于创新药等行业的全方位支持。自2025年两会政府工作报告首次提出“制定创新药目录,支持创新药发展”以来,政府落实了包括北京、上海等地出台创新药械全产业链支持政策,国家医保局、国家卫健委出台《支持创新药高质量发展的若干措施》,并接连召开5场支持创新药械座谈会,国家医保局首次确认已制定“新上市药品首发价格机制”等举措。“近期国家对于创新药产业重新定位,政策优化和支持力度更加落到实处。本次第五套标准‘开闸’,进一步验证国家多维度支持创新产业发展的政策走向。”他具体说道。TONACEA02创新药行情如火如荼2025年,沉寂许久的创新药赛道正迎来系统性复苏。在港股市场上,生物科技板块也迎来了市场风向的逆转。恒生创新药指数自年初以来大幅上扬,部分相关指数涨幅甚至超过60%,显著跑赢人工智能等其他热门赛道。一边是创新药公司IPO的火热,今年上半年,映恩生物、恒瑞医药、药捷安康等10家公司成功登陆港交所,而后港股市场生物医药企业IPO热度持续,几乎每天都有一家公司提交招股书。另一边,二级市场的火热又反过来带动这一批创新药公司的融资活动,再次呈现出强劲的复苏态势。从映恩生物和恒瑞医药等代表性企业成功进行的大规模IPO,到荣昌生物、君实生物等已上市公司接连完成的再融资,无不预示着全球资本对香港生物科技板块的信心正在重塑。陈竹指出,上一轮医药股牛市(参考恒生生物科技指数2019年1月-2021年6月,区间涨幅152%,最高点29257),伴随着2018年港股18-A未盈利生物科技公司上市“开闸”、2019年科创板为创新药企开放融资通道等背景,为市场带来增量优质资产和流动性。“本轮创新药行情如火如荼,我们也看到港股多家18-A公司上市成功,而如今A股第五套标准重启,有望为创新药和医药板块带来更多资金关注,或将助推医药板块行情。”他具体分析到。一系列积极信号表明,创新药的春天正在到来,而且是以一种更为成熟和理性的方式。港交所发言人此前曾在采访中提到,“2025年港股市场回暖,受益于降息周期来临、政策支持、改革成效以及投资者情绪变化等多重因素。”固然有政策和整体大环境的加持,但这一轮创新药的火热,深植于产业基本面的蜕变,源自于行业里有一些比较确定的积极因素。商业端,已经有不少新生代创新药企在实际卖药过程中逐渐迎来盈利关口;技术端,大规模的BD浪潮证明了国内临床候选产品的质量,从而进一步带动中国创新药资产的全球话语权。这场由行业内生发展带动的资本市场狂欢,标志着中国创新药产业步入更理性、更可持续的价值成长新周期。经年之后,站在时间的注脚再回望2025,这一年必将深深镌刻于中国医药创新的编年史中——当资本活水奔涌的闸口,托举着中国生物科技军团扬帆出海的巨轮,这不仅是资本周期的华丽回旋,更是一个制造大国向创新策源地进化的历史性证言。
IPO
2025-07-25
·药时代
今天,港交所上演着激动人心的一幕,八旬老人敲响了中国TCE的第一股。2025年7月25日上午9时,维立志博联合创始人赖寿鹏先生以79岁高龄,亲自敲响上市钟声,标志着中国首个T细胞衔接器(TCE)企业正式登陆港股资本市场。这家成立于2012年的创新药企,在历经13年研发沉淀后,以35港元/股的发行价实现历史性跨越,首日收盘市值逼近130亿港元。在申购期间,该股认购热情空前高涨,认购倍数高达3029倍,远超今年港股平均148倍的水平,总冻结资金逼近3400亿港元,堪称资本市场少见盛事。如此“疯狂”现象的背后,是中国生物医药产业“触底反弹”的投射。今年以来,随着资本市场流动性改善,港股创新药板块迎来强势复苏。据港交所数据显示,截至2025年上半年,已有39家医疗健康企业排队等候上市,创新药企占据IPO数量首位。今年4月,映恩生物上市首日大涨超116%,6月23日正式登陆港交所的药捷安康,上市首日收涨78.71%;同年5月,恒瑞医药正式登陆香港联交所,完成两地上市的布局,成就今年以来国内规模最大的医药IPO项目。有业内人士调侃道“港交所的锣都不够用了”。其次,维立志博的“溢价”绝非偶然。自创立之初,该公司就确立了差异化的技术路线。构建了覆盖肿瘤免疫2.0(IO 2.0)、TCE和ADC三大领域的研发体系。其中,维立志博为解决《JAMA》披露的,全球双抗临床成功率仅8%的瓶颈,构建了LeadsBody、X-body、Linker-payload等多个一体化、AI驱动的技术平台,能够精准调节抗体亲和力与空间结构,有效降低细胞因子释放风险。基于此,维立志博已形成6款差异化TCE产品的矩阵布局,涵盖血液瘤、实体瘤及自身免疫性疾病三大治疗领域。中国TCE第一股可见一斑。其核心产品LBL-034(GPRC5D/CD3双抗)被视为中国原创TCE疗法进军全球血液瘤市场的标杆产品;LBL-058(DLL3靶向TCE-ADC)开创性地将TCE与ADC技术融合,用于治疗小细胞肺癌和神经内分泌肿瘤;而LBL-051(CD19/BCMA/CD3三抗)更与知名风投公司Aditum Bio达成NewCo合作,成立公司Oblenio Bio。而丰富的TCE资产,无疑给了投资人们无限的想象力。据不完全统计,2024年全球共发生了将近20笔交易,总金额超85亿美元,其中国内项目金额最高的两笔交易分别由同润生物和恩沐生物创下,累计金额为21.5亿美元。TCE之所以备受关注,离不开其技术优势。相比单抗,TCE拥有更高的靶向精准性;相比ADC,TCE拥有更优的安全性;相比CAR-T,TCE更具成本优势。就市场表现来看,全球已有10款TCE疗法获批上市,其中安进的TCE产品Blincyto(贝林妥欧单抗)2024年销售额已达12.16亿美元,成为首个突破“十亿美元分子”,市场潜力巨大。有分析师预测,该赛道2030年将突破120亿美元,年复合增长率达42%,增速远超ADC和CAR-T。维立志博上市的火热,是中国生物医药产业“复苏”的缩影。历经多年,“资本寒冬”的冷风早已吹进了各家药企的门户,融资困难、上市无望、只期望自己产品能以“合适”价格售出回报股东,即便运气好些港股上市,估值偏低也不过是“饮鸩止渴”。但冬天来了,春天还会远吗?在港股市场经历多年调整后,投资者对优质创新药企的估值体系正在重构。维立志博能以3029倍的超额认购,是一场资本与创新的双向奔赴。此外,A股市场同步推进制度创新。证监会宣布的创业板第三套上市标准和科创板第五套上市标准重启,为未盈利创新型企业开辟了多元化融资通道。这种监管层与市场端的双向发力,正在形成"创新突破-资本加持-产业升级"的良性循环。随着更多鼓励政策的落地,预计未来将有更多像维立志博这样的创新型企业脱颖而出,共同推动中国生物医药产业迈向全球价值链高端。IPO的繁荣离不开产业的蓬勃发展,而产业的持续创新与活力,才是推动资本市场良性循环的根本动力。参考资料:1.维立志博官微2.雪球3.资本寒冬下的中国药企,排队IPO4.超3000亿资金认购,八旬医学博士凭PD-L1双抗今日敲钟(动脉网)5.维立志博正式于港交所上市!募资1.89亿美元(医药魔方Invest)6.其他公开资料图片来源:即梦AI科济炸场后,实体瘤CAR-T东风再起!2025-07-24股价暴涨400%!IBD领域迎来新秀2025-07-23多款药物惨遭FDA拒批!居然因为...2025-07-23版权声明/免责声明本文为原创文章。本文仅作信息交流之目的,不提供任何商用、医用、投资用建议。文中图片、视频、字体、音乐等素材或为药时代购买的授权正版作品,或来自微信公共图片库,或取自公司官网/网络,部分素材根据CC0协议使用,版权归拥有者,药时代尽力注明来源。如有任何问题,请与我们联系。衷心感谢!药时代官方网站:www.drugtimes.cn联系方式:电话:13651980212微信:27674131邮箱:contact@drugtimes.cn点击这里,查看最新资讯!
免疫疗法IPO细胞疗法抗体药物偶联物
2025-07-17
·融中财经
导读THECAPITAL香港重返全球之巅,基石投资全面“开火”本文4795字,约6.8分钟作者 | 李冰之 编辑 | 吾人来源 | #融中财经(ID:thecapital)经过2022-2023年的低迷调整,香港IPO市场在2024年下半年开始复苏,并于2025年上半年强势反弹。恒生指数半年上涨约20%,港股主板共完成42宗IPO,募资额高达1067亿港元。这一轮热潮中,A+H上市的大型企业和新消费、新能源等行业新贵联袂登场,重塑香港“全球IPO中心”地位。在市场回暖的大背景下,基石投资者生态也发生了显著变化。原本被视作“保发行”的稳定器,如今变成资金抢占核心资产的门票。2023-2024年市场低迷期,不少IPO项目主要依赖本土战略基金、PE和产业资本作为基石,以提高发行确定性。而2025年上半年,约85%的新股在上市前成功引入基石,超四成的IPO引入5家以上的基石投资者,共出现了189家基石投资者投资了36家新上市公司,平均每家IPO引入4.4名基石。部分热门项目引入的基石投资者甚至超过20家,且资金体量和背景更为多元,覆盖了从主权基金、地方国资、银行理财子公司到海外长线机构、上下游战略合作方等。2025年6月单月就有15家新股在香港上市,7月初更是一度出现单日5家公司同日挂牌的盛况,当前在审申请约200家。2025年下半年港股IPO热度有望延续,基石投资也将继续扮演关键角色。热钱涌入,“打新吃肉”,一级市场火爆空前今年IPO认购热度持续飙升,超额认购倍数屡破纪录。据德勤统计,上半年97%的IPO获得超额认购,其中76%的新股超额认购倍数超过20倍,多只热门新股的认购更是达到千倍以上的夸张水平。布鲁可、蜜雪冰城、沪上阿姨等多个项目表现尤为抢眼,超额认购分别突破6000倍、5300倍和3600倍,一手中签率均低至10%。资金冻结规模同样惊人:布鲁可冻资超8000亿港元,蜜雪冰城更是达到了1.83万亿港元,打新热度已回升至2020年以来的高点。新股上市首日表现同样亮眼,映恩生物暴涨116.7%,药捷安康、云知声、沪上阿姨等涨幅均超40%,赚钱效应显著。与此同时,新股上市首日破发率下降至约 29%,延续了自 2021 年峰值以来的改善趋势。上半年,港股主板共有42宗IPO,首发募资金额合计约1067亿港元,同比激增约708%。这一募资额不仅大幅超过2024年全年约876亿港元,也超越了2023年全年的约463亿港元。港股IPO募资额时隔四年重返全球第一,占全球IPO募资总额的约四分之一,其中超大型A+H上市项目贡献了近四分之三的资金。宁德时代于5月在港二次上市,募资约409.63亿港元,成为2025年上半年全球最大IPO;恒瑞医药募资约113.62亿港元;老牌调味料龙头海天味业6约募资逾100亿港元;浙江制造巨头三花智控募资约90亿港元;新茶饮龙头蜜雪冰城的蜜雪集团募资约40亿港元,跻身港股上半年IPO募资额前五。从行业分布来看,上半年工业工程行业募资533亿港元居首,生物医药与消费行业IPO宗数并列第一,可见今年IPO项目主要集中在生物医药、新消费等热门赛道。在市场情绪推动下,一级市场资金快速聚集,散户和机构均热情高涨。与此同时,基石投资者在募资结构中占比大幅提升。上半年IPO上市的42家企业中,逾四成(16家)引入了5名以上基石投资者,对比之下2024年同期拥有3名以上基石的案例都凤毛麟角。宁德时代、恒瑞医药、三花智控、海天味业、蜜雪冰城5大IPO中,基石投资合计占总募资的约50%。不少项目基石认购股份占比达到20-30%。例如泰国椰子水品牌if引入11家基石,总认购约3950万美元,锁定了约26%的发行股份;7月4日上市的安井食品,6家基石合计认购约1177万股,占募资额近三成。由此可见,“打新吃肉”的效应重回港股,基石投资者热情高涨,新股一级市场和二级市场形成良性循环。热赛道速写:制造AI消费三线“并进”先进制造是募资王。宁德时代港股上市募资410亿港元,引入23家基石投资者,包括中石化、GIC、KIA等。三花智控吸引18家基石,中邮、工银理财皆在列;蓝思科技IPO从申报到上市仅用100天,10家基石中不乏小米旗下GreenBetter等产业资本。三家制造龙头在港股实现估值重估,体现了“科创+产能”型公司在港资本市场的融资效率回升。AI赛道表现亮眼。北京的AI语音解决方案提供商云知声(UniSound)获商汤、臻一资产、润建国际三大基石认购,基石占比三分之一;智能机器人赛道的极智嘉登陆港股,市值达220亿港元,首日上涨,成为AI+硬件代表。人工智能企业受益于特专科技18C机制,尽管尚未盈利,但仍获得强基石背书,标志着“新经济稀缺资产”标签仍有效。消费股一直是港股IPO的重要板块,今年更是火力全开。上半年涌现出一批新消费品牌的上市潮,从茶饮连锁到休闲食品,再到消费电子和黄金珠宝,各路消费公司争相叩关港交所。蜜雪冰城5258倍超额认购,基石阵容包括高瓴、红杉、美团龙珠等;沪上阿姨、古茗、IF等品牌集体涌入。海天味业二次上市募资逾百亿,基石包括GIC和HHLR。新茶饮和调味品的集中上市形成“港股消费第二波”,品牌+供应链+价格力成为资本衡量核心。新消费公司估值普遍偏高,但由于市场对其成长性的憧憬,认购异常踊跃,上市后往往出现炒高。投资者格外青睐具备社交话题和国民度的消费股,使之成为今年港股的火爆赛道。医药板块稳扎稳打。恒瑞医药获GIC、橡树资本等顶级基石力挺;映恩生物有15家基石,首日暴涨;药捷安康、维昇药业、觅瑞等也有康方生物、产业基金站台。生物医药企业逐步重建市场信任,基石投资人以长线视角切入,从未盈利生物科技到成熟药企各取所需。谁在下注?基石投资四大主力画像浮出水面在2025年港股IPO浪潮中,活跃的基石投资者阵容呈现出多元化格局,既包括境内的国资平台、银行理财资金、大型公募私募,也汇聚了境外的主权基金、国际资管巨头以及产业资本等。这些基石玩家的出场频率和投入力度相比此前有明显提升。一是“国家队”继续扩张势力版图。2025年上半年,不少内地拟上市企业积极争取来自公司注册地或主要项目所在地的政府产业基金作为基石,至少有14家港股上市IPO基石投资者里有国资支持。今年地方国资频频现身港股IPO基石名单,其中包括地方国资委直接控股的平台(如佛山发展、苏州工业园区基金)、国家级产业基金(如国调基金)、以及国企背景的投资机构(如深圳创新投、中邮理财)。全球动力电池龙头宁德时代港股上市时,其基石阵容中出现了中国邮政集团旗下的中邮理财,作为国有理财公司代表国家队资金参与战略配售;江苏常熟的正力新能引入了常熟市东南投控、苏州高端装备基金、江苏国企混改基金三家当地国资基石;创新药企药捷安康-B、映恩生物-B、维昇药业、觅瑞背后均有地方国资作为基石投资者,其中多为企业发源地的地方国资委旗下产业基金、国家级投资平台等国资力量,反映了地方政府对创新药研发的长期布局。2025年它们青睐新能源、医药、高端制造与本地龙头企业,既承担政策导向,又提升发行确定性。这类国资基金通过“压舱石”角色,为发行人稳定预期,同时也在地方产业政策引导下实现政府投资使命。地方国资作为基石还有信息优势——对当地企业了解深入,决策流程较快。因此,越来越多内地科创企业赴港IPO时会选择引入属地政府基金做基石,以求双赢:企业获得资金和政府背书,地方政府支持产业升级。二是外资全面回流。2024年上半年,港股IPO基石中鲜少有全球大型机构的身影;而2025年上半年,这些机构经常出现于大项目的基石名单。新加坡政府投资公司(GIC)、科威特投资局(KIA)、瑞银资管、施罗德、橡树资本、加拿大皇家银行等海外主权基金和资管巨头,纷纷出现在创新药龙头恒瑞医药、动力电池龙头宁德时代、消费品龙头海天味业等IPO的基石阵容中。外资偏好细分龙头与盈利能力强的企业,主要集中在大型发行中集体出手。从2022年中概股危机以来,外资一度谨慎观望,如今则大幅回流港股,港股IPO重新汇聚来自欧美、中东、东南亚的多元资本,通过基石投资提前锁仓,也反映其对中国核心资产的再定价。外资2025年上半年回流港股,背后是全球宏观逻辑的深层切换。美联储降息预期升温,美债收益率从高位回落,美元吸引力边际下降,全球资本开始寻找更具增长潜力的标的,而港股作为估值洼地,其挂钩的中国核心资产性价比凸显。与此同时,人民币资产迎来重估:中国经济复苏超预期,新能源、高端制造等板块企业盈利扎实增长,叠加政策确定性增强,外资对中国资产的长期价值预期修复,尤其像宁德时代、恒瑞医药这样的全球龙头,其稀缺性让配置需求上升。地缘层面,中美经贸沟通重启、供应链压力缓解,也弱化了外资的风险顾虑,推动其通过港股IPO基石等渠道主动布局,形成“美元退潮+人民币资产价值重估+风险缓和”的共振效应。三是产业链伙伴“抱团”参战。不少基石投资者本身就是发行人上下游产业链中的公司,出于战略协同和长期合作的考量入股。2025年上半年,多家新股的基石名单里出现业务合作伙伴或供应商的身影。宁德时代有中石化、三花智控有小米、沪上阿姨有华宝股份、药捷安康有康方生物。通过战略入股强化合作,既是协同,也是信号。IPO成为上下游合作进一步资本绑定的契机,尤其在新能源和消费领域,产业链投资日趋频繁,形成“生态式下注”。通过基石入股,这些产业投资者可巩固与上市公司的合作关系,实现资源共享、业务互补,并参与行业整合发展。四是金融机构全面参与。银行理财、头部公私募通过战略产品、主动认购方式打通港股投资通道。中邮理财和工银理财各出资2000万美元,成为三花智控IPO的基石投资者;同时,中邮理财还斥资5000万美元参与宁德时代基石认购,是宁德时代的23家基石投资者中唯一的银行理财机构。银行理财资金将此视为提升权益投资能力、服务科技企业融资的重要契机,通过推出“固收+港股IPO”策略产品,把握科技创新和先进制造领域的新股投资机会。此外,头部公募基金和私募股权基金今年频繁现身基石席位。红杉中国、高瓴、易方达、汇添富、景林资产等纷纷在if、映恩生物、安井食品等项目中现身。这些机构具备本土市场洞察和灵活配置优势,在港股打新热中积极扮演“压舱石”角色。一些知名企业家和富豪也通过投资机构曲线参与基石,例如农夫山泉董事长钟睒睒通过私募道合承光认购if椰子水品牌新股。可见,国内的各类资本——从官方背景、银行资金到市场化基金——正长线布局港股基石投资。今年香港IPO基石投资者的典型画像是:国资、外资、产业资本、金融机构多轮驱动。地方国资瞄准硬科技民族企业,国际资本青睐高成长龙头,金融机构抢抓投资机遇,产业伙伴谋求协同共赢。内地背景公司往往因对中国市场有深耕而获得本土国资和内资基金的特别青睐,同时如果是行业龙头也能引来全球长线资金争相入局。海外企业赴港上市(如东南亚消费品牌等)则主要吸引国际投资机构为基石,但若其业务与中国相关也会吸引部分中资参与(如if椰子水IPO就既有UBS瑞银等外资,也有红杉中国和钟睒睒等中资力量认购)。可以说,在港股这一国际化市场,资本对“好公司”的评判标准趋同:只要具备稀缺性和成长性,无论境内境外企业,都有望得到基石投资人的热捧。但具体到资金来源,境内资本出于政策指引和信息优势,更偏好支持中国内地企业,而国际资金更注重企业的全球竞争力和规模。结语2025年下半年,港股IPO市场热度不会降温。随着上市申请储备充裕,科技、消费、高端制造领域的龙头企业将持续登场,撑起“硬科技突围、消费升级、能源转型”的主线。 硬科技赛道里,特专科技18C机制仍会是未盈利创新企业的“加速器”,机器人、创新药械等领域的头部玩家将密集递表,基石投资者会更看重技术壁垒与商业化进度。消费端,A+H上市模式成主流,多家A股龙头借港股强化国际化布局,既能吸引国际资本,也让“双市场流动性溢价”更明显。能源转型领域,动力电池、光伏材料企业的赴港募资,会继续绑定产业链资本与地方国资,形成“产业+资本”的协同效应。 经历了2025年上半年的狂热,港股IPO节奏正加速向深水区挺进。对于基石投资人而言,这既是窗口期也是博弈期。机构策略上,基石投资会更向头部项目集中——国际长线资金盯紧高成长龙头,产业资本偏爱能形成生态协同的标的,中小项目则需靠稀缺性突围。尽管地缘与估值波动仍需警惕,但港股的离岸属性与人民币资产重估逻辑,会继续给市场托底。 一级市场“军备竞赛”仍将继续。资金会更偏好龙头,更在意估值,但只要故事够亮、结构够稳、基石够硬,香港IPO的繁荣就远未见顶。#基石投资 #打新策略 #港股IPO #新消费 #融中 # 线索爆料 # rzcj@thecapital.com.cn融中官方粉丝群 在这里,你可以获取丰富的股权投资行业资讯、热点报道;前沿行业报告、重点课题研究、最新业内动态。链接资本,连接市场,联结资源,共同打造创投交流新平台、合作共赢朋友圈。END开白/线上咨询:irongzhong媒体合作:010-84464881商务合作:010-84467811
IPO
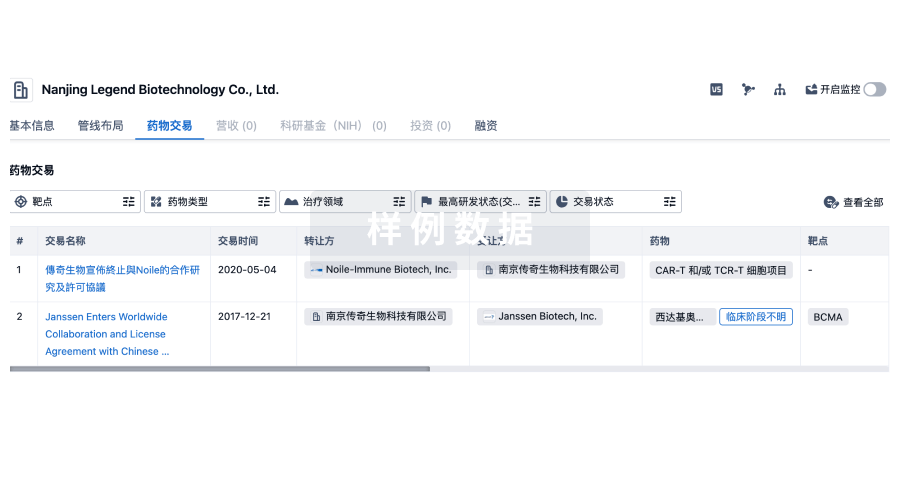
100 项与 药捷安康(南京)科技股份有限公司 相关的药物交易
登录后查看更多信息
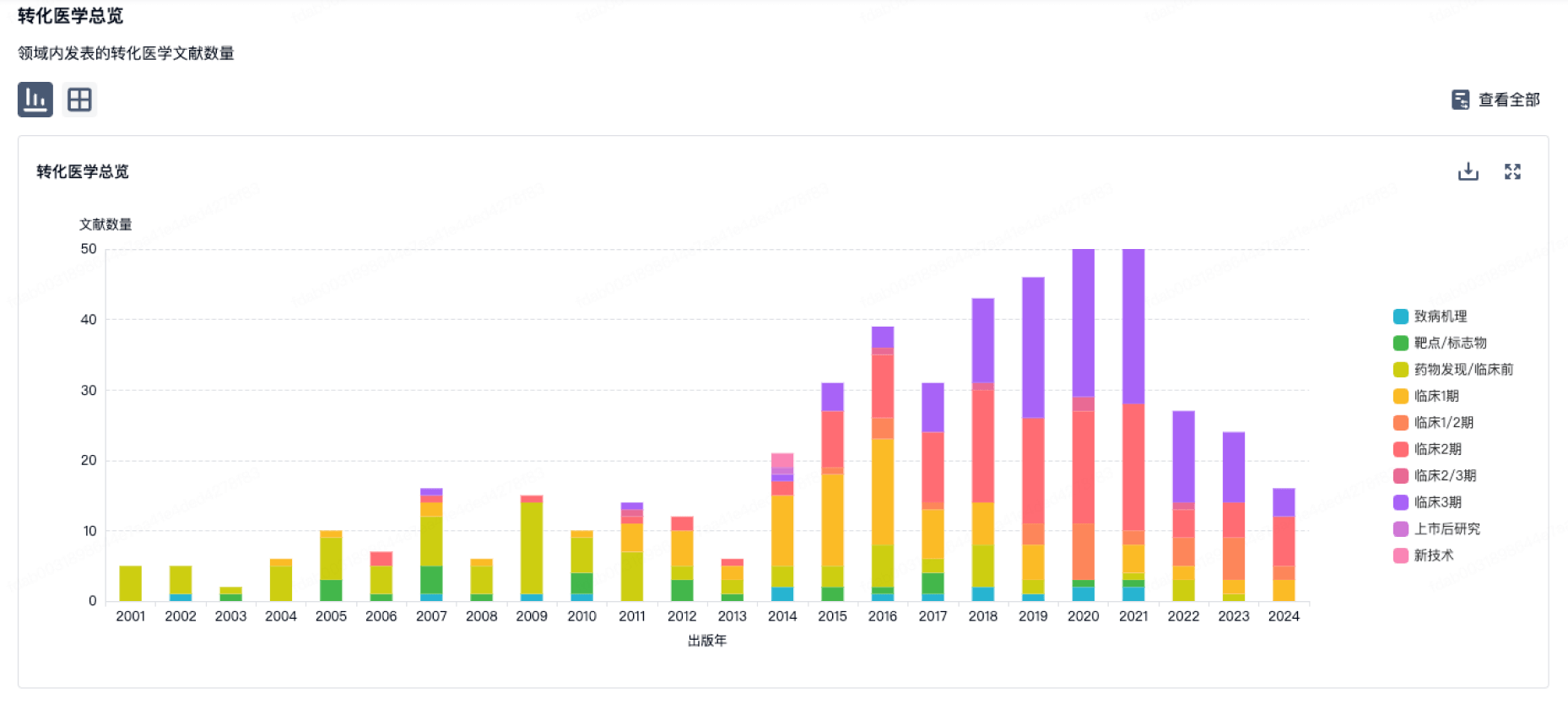
100 项与 药捷安康(南京)科技股份有限公司 相关的转化医学
登录后查看更多信息
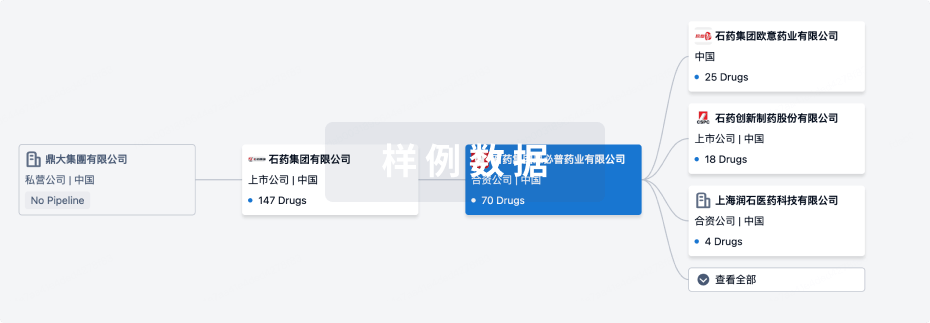
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月02日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
3
4
临床前
临床申请批准
1
4
临床1期
临床2期
2
1
临床3期
其他
3
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
替恩戈替尼 ( Aurora A x Aurora B x CSF-1R x FGFR1 x FGFR2 x FGFR3 x JAK1 x JAK2 x VEGFR ) | FGFR阳性胆管癌 更多 | 临床3期 |
TT-01688-CL ( S1PR1 ) | 重度特应性皮炎 更多 | 临床2期 |
LR-19019 | 特应性皮炎 更多 | 临床2期 |
TT-01488 ( BTK ) | 弥漫性大B细胞淋巴瘤 更多 | 临床1期 |
TT-00973 ( AXL x FLT3 ) | 晚期恶性实体瘤 更多 | 临床1期 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用