预约演示
更新于:2025-05-07

Sagent Pharmaceuticals, Inc.
更新于:2025-05-07
概览
标签
感染
遗传病与畸形
神经系统疾病
合成多肽
小分子化药
单克隆抗体
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 合成多肽 | 1 |
| 单克隆抗体 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| SARS-CoV-2 S protein(新冠病毒刺突蛋白) | 1 |
| DRDs(多巴胺受体家族) | 1 |
关联
3
项与 Sagent Pharmaceuticals, Inc. 相关的药物靶点- |
作用机制 细胞膜功能抑制剂 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2003-09-12 |
靶点 |
作用机制 DRDs激动剂 |
在研适应症 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期1964-10-24 |
作用机制 SARS-CoV-2 S protein抑制剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床2/3期 |
首次获批国家/地区- |
首次获批日期- |
3
项与 Sagent Pharmaceuticals, Inc. 相关的临床试验NCT04583592
A Multicenter, Randomized, Double-Blind, Placebo-Controlled Trial of the Efficacy of Camostat Mesilate for Treatment of COVID-19 in Outpatients
This is a randomized, double-blind, placebo-controlled study of camostat mesilate in ambulatory patients with confirmed COVID-19 with at least one risk factor for severe illness.
开始日期2020-11-09 |
申办/合作机构 |
NCT04518410
Adaptive Platform Treatment Trial for Outpatients With COVID-19 (Adapt Out COVID)
Drug studies often look at the effect one or two drugs have on a medical condition, and involve one company. There is currently an urgent need for one study to efficiently test multiple drugs from more than one company, in people who have tested positive for COVID-19 but who do not currently need hospitalization. This could help prevent disease progression to more serious symptoms and complications, and spread of COVID-19 in the community.
This study looks at the safety and effectiveness of different drugs in treating COVID-19 in outpatients. In Phase II, participants in the study will be treated with either a study drug or with placebo. In protocol version 7.0, participants in Phase III of the study will be treated with either a study drug or active comparator drug. Participants assigned to the bamlanivimab agent/placebo arm and will have 28 days of intensive follow-up following study drug administration, followed by limited follow-up through 24 weeks in phase II and in phase III. All other investigational agents and their corresponding placebo arms will involve 28 days of intensive follow-up, followed by limited follow-up through 72 weeks in phase II and phase III. Additional study visits may be required, depending on the agent.
This study looks at the safety and effectiveness of different drugs in treating COVID-19 in outpatients. In Phase II, participants in the study will be treated with either a study drug or with placebo. In protocol version 7.0, participants in Phase III of the study will be treated with either a study drug or active comparator drug. Participants assigned to the bamlanivimab agent/placebo arm and will have 28 days of intensive follow-up following study drug administration, followed by limited follow-up through 24 weeks in phase II and in phase III. All other investigational agents and their corresponding placebo arms will involve 28 days of intensive follow-up, followed by limited follow-up through 72 weeks in phase II and phase III. Additional study visits may be required, depending on the agent.
开始日期2020-08-19 |
NCT02449369
Intra-Venous Acetaminophen and Muscle Relaxants After Total Knee Arthroplasty (TKA). Prospective, Randomized, Open-label Trial to Determine if Switching From Oral to Intravenous Acetaminophen and Orphenadrine for 48 Hours After TKA Improves Outcomes.
This is a prospective, three-arm, randomized, open-label trial to determine if a new pain control protocol which includes regular dosing of intravenous acetaminophen and orphenadrine for 48 hours after total knee surgery reduces the need for opioid pain medication and reduces average pain scores.
开始日期2015-04-01 |
申办/合作机构 |
100 项与 Sagent Pharmaceuticals, Inc. 相关的临床结果
登录后查看更多信息
0 项与 Sagent Pharmaceuticals, Inc. 相关的专利(医药)
登录后查看更多信息
1
项与 Sagent Pharmaceuticals, Inc. 相关的文献(医药)2023-10-05·Clinical Infectious Diseases
One Week of Oral Camostat Versus Placebo in Nonhospitalized Adults With Mild-to-Moderate Coronavirus Disease 2019: A Randomized Controlled Phase 2 Trial
Article
作者: Jilg, Nikolaus ; Jagannathan, Prasanna ; Szurgot, Bob ; Currier, Judith S ; Murtaugh, William ; Corado, Katya ; Hughes, Michael D ; Chew, Kara W ; Chew, Kara ; Daar, Eric S ; Evering, Teresa ; Hoover, Keila ; Kantor, Amy ; Singh, Upinder ; Li, Jonathan ; Pillay, Sandy ; Jana, Atasi ; Colsh, Kelly ; Jennings, Cheryl ; Dragavon, Joan ; Rwakazina, Irene ; Newell, Matthew ; Kosmyna, Jan ; Riviere, Cynthia ; Smith, Davey M ; Greenfelder, Brian ; Hart, Phil A ; Fischer, William ; Smith, David ; Shahkolahi, Akbar ; Beck, Justine ; Greninger, Alexander L ; Patel, Nilam ; Giganti, Mark J ; Taiwo, Babafemi ; Eron, Joseph ; Perelson, Alan ; Gottesman, Joan ; Eron, Joseph J ; Fletcher, Courtney ; Cardoso, Sandra ; Coombs, Robert W ; Daar, Eric ; Currier, Judith ; Ritz, Justin ; Li, Jonathan Z ; Coombs, Robert ; Hosey, Lara ; Hughes, Michael ; Gapara, Morgan ; Moser, Carlee ; Javan, Arzhang Cyrus ; Roa, Jhoanna ; Wohl, David ; Ignacio, Rachel Bender ; Neytman, Gene ; Wohl, David A ; Sieg, Scott ; Pedersen, Susan ; Giganti, Mark
35
项与 Sagent Pharmaceuticals, Inc. 相关的新闻(医药)2024-12-08
·药筛
统计每周仿制药一致性评价申报、上市申请(12.2-12.08)
1、仿制药上市申请获批药品名称企业名称分类受理号阿戈美拉汀片深圳市泛谷药业股份有限公司;深圳信立泰药业股份有限公司4CYHS2302531阿戈美拉汀片杭州领业医药科技有限公司4CYHS2302278阿戈美拉汀片重庆华森制药股份有限公司4CYHS2301877阿帕他胺片齐鲁制药(海南)有限公司4CYHS2302520阿普米司特片常州制药厂有限公司4CYHS2301812阿普米司特片常州制药厂有限公司4CYHS2301811阿普米司特片常州制药厂有限公司4CYHS2301810阿普米司特片广东迈恒医药研发有限公司;广东隆赋药业股份有限公司4CYHS2301478阿普米司特片广东迈恒医药研发有限公司;广东隆赋药业股份有限公司4CYHS2301477阿普米司特片广东迈恒医药研发有限公司;广东隆赋药业股份有限公司4CYHS2301476阿奇霉素干混悬剂迪沙药业集团有限公司4CYHS2301207阿司匹林肠溶片仁合益康集团有限公司;河北仁合益康药业有限公司4CYHS2302409阿昔莫司胶囊浙江高跖医药科技股份有限公司;浙江赛默制药有限公司4CYHS2303120氨己烯酸口服溶液用散远大医药(中国)有限公司3CYHS2300027氨甲环酸注射液广州泽盛药业科技有限公司;山东辉成药业有限公司4CYHS2301435氨甲环酸注射液广州泽盛药业科技有限公司;山东辉成药业有限公司4CYHS2301434氨甲环酸注射液广州泽盛药业科技有限公司;山东辉成药业有限公司4CYHS2301436氨溴特罗口服溶液江西仁齐制药有限公司;湖南九典制药股份有限公司3CYHS2301066氨溴特罗口服溶液海南天盛保和生物科技有限公司;安徽永生堂药业有限责任公司3CYHS2300745氨溴特罗口服溶液南京卡文迪许生物工程技术有限公司;江苏云阳集团药业有限公司3CYHS2300568氨溴特罗口服溶液浙江康润制药有限公司3CYHS2300383氨溴特罗口服溶液浙江康润制药有限公司3CYHS2300382奥美沙坦酯氢氯噻嗪片宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2300248奥沙利铂注射液贵州阜康仁制药有限公司;哈尔滨医大药业股份有限公司3CYHS2300670巴氯芬口服溶液江苏天士力帝益药业有限公司;南京海纳制药有限公司3CYHS2301070苯磺酸氨氯地平片吉林敖东药业集团延吉股份有限公司4CYHS2301986比索洛尔氨氯地平片福建海西新药创制股份有限公司;广东安诺药业股份有限公司4CYHS2302208丙戊酸钠口服溶液安徽海斯美医药有限公司;扬州市三药制药有限公司4CYHS2301421玻璃酸钠滴眼液华熙生物科技股份有限公司;北京汇恩兰德制药有限公司4CYHS2301663布洛芬缓释胶囊南京华兴医药科技有限公司;湖北荆江源制药股份有限公司4CYHS2301450布洛芬混悬滴剂江苏万高药业股份有限公司4CYHS2302104醋酸维持液(含葡萄糖)石家庄四药有限公司3CYHS2301103醋酸维持液(含葡萄糖)石家庄四药有限公司3CYHS2301104达比加群酯胶囊Hetero Labs Limited5.2JYHS2000002达比加群酯胶囊Hetero Labs Limited5.2JYHS2000006达比加群酯胶囊Hetero Labs Limited5.2JYHS2000003达格列净二甲双胍缓释片南京正大天晴制药有限公司3CYHS2300498达格列净二甲双胍缓释片南京正大天晴制药有限公司3CYHS2300499达格列净片浙江华义制药有限公司4CYHS2301952达格列净片浙江华义制药有限公司4CYHS2301953达格列净片浙江华海药业股份有限公司4CYHS2300694达格列净片浙江华海药业股份有限公司4CYHS2300693地高辛注射液江苏联环药业股份有限公司3CYHS2301735地夸磷索钠滴眼液浙江尖峰药业有限公司4CYHS2302723地夸磷索钠滴眼液国药集团三益药业(芜湖)有限公司4CYHS2302234地诺孕素片博瑞制药(苏州)有限公司;浙江仙琚制药股份有限公司4CYHS2300580碘比醇注射液重庆圣华曦药业股份有限公司4CYHS2300167碘比醇注射液重庆圣华曦药业股份有限公司4CYHS2300166碘佛醇注射液成都倍特药业股份有限公司4CYHS2301601碘佛醇注射液成都倍特药业股份有限公司4CYHS2301602恩格列净片湖南迪诺制药股份有限公司4CYHS2302022二甲双胍恩格列净片(Ⅰ)杭州云柏医药科技有限公司;浙江赛默制药有限公司4CYHS2300814二甲双胍恩格列净片(Ⅴ)杭州云柏医药科技有限公司;浙江赛默制药有限公司4CYHS2300815二甲双胍维格列汀片(Ⅱ)宁波美诺华天康药业有限公司4CYHS2302306二羟丙茶碱注射液森淼(山东)药业有限公司;湖北津药药业股份有限公司3CYHS2301556二羟丙茶碱注射液浙江和泽医药科技股份有限公司;浙江康恩贝制药股份有限公司3CYHS2301480二羟丙茶碱注射液安徽长江药业有限公司;安徽恒星制药有限公司3CYHS2300942法莫替丁注射液南京康发生物科技有限公司;马鞍山丰原制药有限公司3CYHS2301437非诺贝特酸胆碱缓释胶囊鲁南贝特制药有限公司;吉林天衡英睿制药有限公司4CYHS2301088非诺贝特酸胆碱缓释胶囊鲁南贝特制药有限公司;吉林天衡英睿制药有限公司4CYHS2301087呋塞米注射液武汉久安药业有限公司;四川美大康佳乐药业有限公司3CYHS2301607呋塞米注射液武汉久安药业有限公司;四川美大康佳乐药业有限公司3CYHS2301606氟比洛芬钠滴眼液武汉先路医药科技股份有限公司;成都普什制药有限公司3CYHS2200829氟尿嘧啶注射液湖南赛隆药业(长沙)有限公司;山西普德药业有限公司3CYHS2301428复方聚乙二醇电解质散(III)安徽省先锋制药有限公司4CYHS2301384复方托吡卡胺滴眼液南京恒道医药科技股份有限公司;江苏大红鹰恒顺药业有限公司4CYHS2201645富马酸福莫特罗吸入溶液合肥国药诺和药业有限公司;江苏大红鹰恒顺药业有限公司4CYHS2302287钆布醇注射液常州四药制药有限公司4CYHS2301788钆特酸葡胺注射液山东新时代药业有限公司4CYHS2301815钆特酸葡胺注射液山东新时代药业有限公司4CYHS2301816钆特酸葡胺注射液山东新时代药业有限公司4CYHS2301817钆特酸葡胺注射液Joint Stock Company “FARMAK“5.2JYHS2300001枸橼酸坦度螺酮片山东京卫制药有限公司4CYHS2302793枸橼酸坦度螺酮片山东京卫制药有限公司4CYHS2302794骨化三醇软胶囊湖南银泽华浩生物科技有限公司;南通华山药业有限公司4CYHS2302334己酮可可碱注射液江苏慧聚药业股份有限公司;山西普德药业有限公司3CYHS2300543甲磺酸艾立布林注射液成都西岭源药业有限公司;健进制药有限公司4CYHS2300657甲磺酸仑伐替尼胶囊江苏康缘药业股份有限公司4CYHS2300794甲硫酸新斯的明注射液东阳祥昇医药科技有限公司;浙江北生药业汉生制药有限公司3CYHS2302055甲硫酸新斯的明注射液东阳祥昇医药科技有限公司;浙江北生药业汉生制药有限公司3CYHS2302054间苯三酚口腔崩解片浙江高跖医药科技股份有限公司;浙江赛默制药有限公司3CYHS2301786间苯三酚口腔崩解片湖南先施制药有限公司;浙江赛默制药有限公司3CYHS2301727间苯三酚注射液福建天泉药业股份有限公司4CYHS2302371间苯三酚注射液湖北午时医药研究院有限公司;湖北午时药业股份有限公司4CYHS2301535精氨酸培哚普利片杭州仟源保灵药业有限公司4CYHS2302479精氨酸培哚普利片杭州仟源保灵药业有限公司4CYHS2302478聚乙烯醇滴眼液上海阿尔福斯医药科技有限公司;浙江赛默制药有限公司3CYHS2300992卡贝缩宫素注射液成都诺和晟鸿生物制药有限公司;四川美大康佳乐药业有限公司4CYHS2301732卡铂注射液吉斯美(武汉)制药有限公司4CYHS2301789卡络磺钠注射液成都倍特药业股份有限公司3CYHS2201632卡络磺钠注射液成都倍特药业股份有限公司3CYHS2201631卡络磺钠注射液成都倍特药业股份有限公司3CYHS2201630卡前列素氨丁三醇注射液北京仁众药业有限公司;海南全星制药有限公司4CYHS2302262利奈唑胺干混悬剂广州一品红制药有限公司3CYHS2202052磷酸奥司他韦干混悬剂北京斯利安药业有限公司3CYHS2300958磷酸奥司他韦干混悬剂广东万方药业科技有限公司;哈尔滨三联药业股份有限公司3CYHS2200236磷酸奥司他韦胶囊浙江普洛康裕制药有限公司4CYHS2400689磷酸奥司他韦胶囊遂成药业股份有限公司4CYHS2400586磷酸奥司他韦胶囊遂成药业股份有限公司4CYHS2400588磷酸奥司他韦胶囊遂成药业股份有限公司4CYHS2400585磷酸奥司他韦胶囊天方药业有限公司4CYHS2302571磷酸特地唑胺片石药集团中诺药业(石家庄)有限公司4CYHS2302958硫酸镁钠钾口服用浓溶液丽珠集团丽珠制药厂;天大药业(珠海)有限公司4CYHS2301893硫酸镁钠钾口服用浓溶液南京知和医药科技有限公司;湖南嘉恒制药有限公司4CYHS2301299硫酸羟氯喹片西安海欣制药有限公司4CYHS2302632硫酸特布他林口服溶液成都利尔药业有限公司3CYHS2301327硫酸特布他林口服溶液成都利尔药业有限公司3CYHS2301326硫辛酸注射液江苏开元药业有限公司;江苏悦兴药业有限公司4CYHS2301872铝碳酸镁咀嚼片江右制药(常德)有限公司;江苏永安制药有限公司4CYHS2302099氯化钾颗粒山西普德药业有限公司3CYHS2301126氯化钾注射液黑龙江博宇制药有限公司;湖北科伦药业有限公司3CYHS2302209氯化钾注射液北京柏雅联合药物研究所有限公司;山东华鲁制药有限公司3CYHS2301723氯化钾注射液成都米子生物医药科技有限公司;山东华鲁制药有限公司3CYHS2301596氯化钾注射液成都欣捷高新技术开发股份有限公司;山东华鲁制药有限公司3CYHS2301578氯化钾注射液南京恩泰医药科技有限公司;江苏大红鹰恒顺药业有限公司3CYHS2301547氯雷他定糖浆合肥远志医药科技开发有限公司;安徽永生堂药业有限责任公司4CYHS2302039氯沙坦钾氢氯噻嗪片宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2301692罗库溴铵注射液中玉制药(海口)有限公司;海南中玉药业有限公司4CYHS2301828罗沙司他胶囊重庆煜洋药业有限公司;重庆圣华曦药业股份有限公司4CYHS2303610马来酸阿伐曲泊帕片山东良福制药有限公司4CYHS2302166马来酸阿伐曲泊帕片上海迪赛诺医药集团股份有限公司;江苏诚康药业有限公司4CYHS2301559马来酸阿法替尼片甘肃兰药药业有限公司4CYHS2101073马来酸阿法替尼片甘肃兰药药业有限公司4CYHS2101074马来酸氟伏沙明片湖南省湘中制药有限公司4CYHS2303021马来酸氟伏沙明片山东京卫制药有限公司4CYHS2302834马来酸氟伏沙明片安徽省先锋制药有限公司4CYHS2302391马来酸氟伏沙明片安徽省先锋制药有限公司4CYHS2302390吗啉硝唑氯化钠注射液山东齐都药业有限公司4CYHS2301112吗啉硝唑氯化钠注射液南京卡文迪许生物工程技术有限公司;江苏悦兴药业有限公司4CYHS2300474吗啉硝唑氯化钠注射液成都国为生物医药有限公司;成都正康药业有限公司4CYHS2202045美沙拉秦缓释胶囊北京福元医药股份有限公司3CYHS2302305美索巴莫注射液福安药业集团庆余堂制药有限公司3CYHS2301612米诺地尔搽剂乐福思健康产业股份公司;广东科伦药业有限公司3CYHS2400410米诺地尔搽剂乐福思健康产业股份公司;广东科伦药业有限公司3CYHS2400414米诺地尔搽剂乐福思健康产业股份公司;广东科伦药业有限公司3CYHS2400412莫匹罗星软膏珠海联邦制药股份有限公司中山分公司4CYHS2302064尼可地尔片东阳祥昇医药科技有限公司;浙江北生药业汉生制药有限公司4CYHS2302379尼莫地平注射液成都倍特药业股份有限公司4CYHS2302461帕拉米韦注射液山西阳和医药技术有限公司;山西国润制药有限公司3CYHS2301504帕拉米韦注射液湖北民康药业集团有限公司;湖北美林药业有限公司3CYHS2301271哌柏西利片石药集团欧意药业有限公司4CYHS2400665哌柏西利片南京正大天晴制药有限公司4CYHS2302060哌柏西利片南京正大天晴制药有限公司4CYHS2302061培哚普利氨氯地平片(Ⅲ)江苏万高药业股份有限公司4CYHS2300948苹果酸舒尼替尼胶囊Dr. Reddy's Laboratories Ltd.5.2JYHS2200003泊沙康唑肠溶片Hetero Labs Limited5.2JYHS2200053普伐他汀钠片北京柏雅联合药物研究所有限公司;湖南九典制药股份有限公司4CYHS2302458普拉洛芬滴眼液苏州欧康维视生物科技有限公司4CYHS2302684普拉洛芬滴眼液圣嘉(滨海)生物医药科技有限公司;山东光明药业有限公司4CYHS2302440氢溴酸伏硫西汀片杭州和康药业有限公司4CYHS2301881曲伏前列素滴眼液兆科(广州)眼科药物有限公司4CYHS2302009曲伏噻吗滴眼液兆科(广州)眼科药物有限公司4CYHS2301974屈螺酮炔雌醇片南通联亚药业股份有限公司4CYHS2200411乳果糖口服溶液海南斯达制药有限公司4CYHS2301323乳果糖口服溶液黑龙江中桂制药有限公司4CYHS2300689乳果糖口服溶液黑龙江中桂制药有限公司4CYHS2300690瑞巴派特片苏州旺山旺水生物医药股份有限公司;苏州特瑞药业股份有限公司4CYHS2301934瑞巴派特片北京金城泰尔制药有限公司4CYHS2301916舒更葡糖钠注射液弘和制药有限公司;吉林振澳制药有限公司4CYHS2300937舒更葡糖钠注射液中国大冢制药有限公司4CYHS2300867羧甲司坦口服溶液北京康晟百春生物科技有限公司;北京华润高科天然药物有限公司3CYHS2202114缩宫素注射液安徽百奥药业有限公司;成都利尔药业有限公司3CYHS2301105碳酸司维拉姆片国药集团致君(深圳)坪山制药有限公司4CYHS2301555替米沙坦氨氯地平片山西德元堂药业有限公司4CYHS2302154替米沙坦氨氯地平片康缘华威医药有限公司;江苏康缘药业股份有限公司4CYHS2301967酮咯酸氨丁三醇注射液福建天泉药业股份有限公司3CYHS2301620托拉塞米注射液海南斯达制药有限公司3CYHS2301008托拉塞米注射液海南斯达制药有限公司3CYHS2301009吸入用硫酸沙丁胺醇溶液山东新时代药业有限公司;山东华鲁制药有限公司4CYHS2302678吸入用乙酰半胱氨酸溶液陕西丽彩药业有限公司;太极集团四川太极制药有限公司4CYHS2302648西格列汀二甲双胍片(Ⅱ)浙江英格莱制药有限公司4CYHS2301433西他沙星片浙江麒正药业有限公司4CYHS2302628腺苷注射液北京布霖生物科技有限公司;华夏生生药业(北京)有限公司3CYHS2202062腺苷注射液华夏生生药业(北京)有限公司3CYHS2201223硝苯地平控释片山东新时代药业有限公司4CYHS2302043硝酸异山梨酯注射液安徽誉恒生物科技有限公司;国药集团国瑞药业有限公司4CYHS2302801熊去氧胆酸胶囊宜昌人福药业有限责任公司4CYHS2301832溴莫尼定噻吗洛尔滴眼液山东威智百科药业有限公司;山东海山药业有限公司4CYHS2302136亚叶酸钙注射液石家庄荣雾迪医药科技有限公司;扬州中宝药业股份有限公司4CYHS2302359盐酸艾司洛尔注射液湖南赛隆药业(长沙)有限公司;湖南赛隆药业有限公司3CYHS2301503盐酸奥布卡因滴眼液苏州欧康维视生物科技有限公司4CYHS2301731盐酸贝尼地平片重庆华邦制药有限公司4CYHS2302718盐酸丙卡特罗口服溶液江苏万高药业股份有限公司3CYHS2301818盐酸达泊西汀片齐鲁制药有限公司4CYHS2301837盐酸氮卓斯汀滴眼液合肥华威药业有限公司4CYHS2302951盐酸多巴酚丁胺注射液陕西顿斯制药有限公司3CYHS2302377盐酸多奈哌齐片宝龙药业有限公司4CYHS2201419盐酸多奈哌齐片保定天浩制药有限公司;山东步长制药股份有限公司4CYHS2101423盐酸多奈哌齐片泰荣(福建)药业有限公司;厦门力卓药业有限公司4CYHS2101184盐酸多柔比星脂质体注射液南京绿叶制药有限公司4CYHS2301507盐酸伐地那非片山东海雅医药科技有限公司;南京海纳制药有限公司4CYHS2301955盐酸氟西汀胶囊江西施美药业股份有限公司4CYHS2301682盐酸甲哌卡因注射液济南辰欣医药科技有限公司;辰欣药业股份有限公司3CYHS2301195盐酸甲氧氯普胺注射液安徽长江药业有限公司3CYHS2301976盐酸甲氧氯普胺注射液东阳祥昇医药科技有限公司;浙江北生药业汉生制药有限公司3CYHS2301782盐酸甲氧氯普胺注射液西洲医药科技(浙江)有限公司;浙江北生药业汉生制药有限公司3CYHS2301711盐酸罗匹尼罗缓释片植恩生物技术股份有限公司4CYHS2400314盐酸罗匹尼罗缓释片杭州和泽坤元药业有限公司;广州玻思韬控释药业有限公司4CYHS2301805盐酸莫西沙星氯化钠注射液湖北长联杜勒制药有限公司4CYHS2300870盐酸莫西沙星氯化钠注射液河北凯威恒诚制药有限公司;河北天成药业股份有限公司4CYHS2201999盐酸坦索罗辛缓释胶囊昆明积大制药股份有限公司4CYHS2301617盐酸异丙肾上腺素注射液成都米子生物医药科技有限公司;成都天台山制药股份有限公司3CYHS2302299盐酸左沙丁胺醇雾化吸入溶液海南斯达制药有限公司3CYHS2301485氧氟沙星滴耳液山东光明药业有限公司4CYHS2301752伊布替尼胶囊北京海步医药科技有限公司;北京亚宝生物药业有限公司4CYHS2300103依折麦布片江苏德源药业股份有限公司4CYHS2302773乙酰半胱氨酸泡腾片江苏和晨药业有限公司4CYHS2302616异氟烷山东新时代药业有限公司4CYHS2301172异氟烷山东新时代药业有限公司4CYHS2301171异烟肼注射液嘉实(湖南)医药科技有限公司;湖南五洲通药业股份有限公司3CYHS2301054吲哚布芬片北京诚济制药股份有限公司3CYHS2301349重酒石酸间羟胺注射液河南蓝图制药有限公司;江苏悦兴药业有限公司3CYHS2300889重酒石酸卡巴拉汀口服液百善科技(湖州)有限公司;浙江凯润药业股份有限公司3CYHS2301390重酒石酸去甲肾上腺素注射液武汉久安药业有限公司;朗天药业(湖北)有限公司3CYHS2302220注射用丁二磺酸腺苷蛋氨酸海南倍特药业有限公司4CYHS2300451注射用丁二磺酸腺苷蛋氨酸重庆药友制药有限责任公司4CYHS2300037注射用伏立康唑陕西博森生物制药股份集团有限公司4CYHS2302591注射用氯诺昔康福安药业集团湖北人民制药有限公司4CYHS2301667注射用尼可地尔海南皇隆制药股份有限公司3CYHS2302094注射用尼可地尔海南皇隆制药股份有限公司3CYHS2302095注射用尼可地尔重庆德诚永道医药有限公司;重庆华邦制药有限公司3CYHS2301328注射用头孢米诺钠山东宜和生物医药科技有限公司;山东润泽制药有限公司4CYHS2400781注射用头孢他啶阿维巴坦钠海南海灵化学制药有限公司;海口市制药厂有限公司4CYHS2301941注射用头孢唑肟钠陕西东科制药有限责任公司;上海欣峰制药有限公司4CYHS2301918注射用头孢唑肟钠陕西东科制药有限责任公司;上海欣峰制药有限公司4CYHS2301917注射用盐酸地尔硫卓舒美奇成都生物科技有限公司;峨眉山通惠制药有限公司4CYHS2303042注射用盐酸多西环素海南普利制药股份有限公司3CYHS2201635注射用盐酸多西环素海南普利制药股份有限公司3CYHS2201636注射用盐酸罗沙替丁醋酸酯海南倍特药业有限公司3CYHS2301212注射用吲哚菁绿南京亚东启天药业有限公司;南京海纳制药有限公司3CYHS2300560注射用唑来膦酸浓溶液岳阳新华达制药有限公司4CYHS2300851左卡尼汀口服溶液江苏百奥信康医药科技有限公司;湖南九典制药股份有限公司4CYHS2302472左氧氟沙星滴眼液上海阿尔福斯医药科技有限公司;浙江赛默制药有限公司4CYHS2300873ω-3脂肪酸乙酯90软胶囊扬子江药业集团有限公司4CYHS2300357
注:灰色字体部分受理号结论为不批准。
2、一致性评补充申请获批药品名称企业名称受理号阿奇霉素干混悬剂山东淄博新达制药有限公司CYHB2450159硫酸阿米卡星注射液宁波大红鹰药业股份有限公司;成都市海通药业有限公司CYHB2450025硫酸阿米卡星注射液宁波大红鹰药业股份有限公司;成都市海通药业有限公司CYHB2450026氯化钾注射液石药银湖制药有限公司CYHB2350676葡萄糖酸钙注射液西南药业股份有限公司;石家庄四药有限公司CYHB2350780盐酸林可霉素注射液四川美大康华康药业有限公司CYHB2350880中/长链脂肪乳注射液(C6-24)四川国瑞药业有限责任公司CYHB2350517注射用氨曲南海口市制药厂有限公司CYHB2450015注射用氨曲南海口市制药厂有限公司CYHB2450016
注:灰色字体部分受理号结论为不批准。
3、新增仿制药上市申请药品名称企业名称分类受理号阿戈美拉汀片沈阳华泰药物研究有限公司;沈阳福宁药业有限公司4CYHS2404197阿立哌唑口服溶液浙江浙北药业有限公司3CYHS2404139氨磺必利口服溶液广州艾格生物科技有限公司;湖北唯森制药有限公司3CYHS2404171奥卡西平片湖南省湘中制药有限公司4CYHS2404184奥美沙坦酯口崩片北京星昊盈盛药业有限公司3CYHS2404165苯磺酸左氨氯地平片四川新斯顿制药股份有限公司4CYHS2404138比拉斯汀片广州大光制药有限公司;广州博济生物医药科技园有限公司4CYHS2404193吡拉西坦片海南全星制药有限公司3CYHS2404192玻璃酸钠滴眼液重庆壹零柒陆医药科技有限公司;中山万汉制药有限公司4CYHS2404179玻璃酸钠滴眼液苏州惟佑基因生物科技有限公司;北京汇恩兰德制药有限公司4CYHS2404190布美他尼注射液石家庄四药有限公司3CYHS2404137布南色林片浙江金华康恩贝生物制药有限公司4CYHS2404187布瑞哌唑片天津药物研究院药业有限责任公司4CYHS2404169布瑞哌唑片天津药物研究院药业有限责任公司4CYHS2404170草酸艾司西酞普兰口服溶液海南广升誉制药有限公司;江苏欧歌制药有限公司3CYHS2404136草酸艾司西酞普兰片Maxmind Pharmaceutical S.L.;Macleods Pharmaceuticals Ltd.;Maxmind Biotechnology (Hainan) Co.,Ltd.5.2JYHS2400060草酸艾司西酞普兰片Maxmind Pharmaceutical S.L.;Macleods Pharmaceuticals Ltd.;Maxmind Biotechnology (Hainan) Co.,Ltd.5.2JYHS2400059达格列净片上海现代制药股份有限公司4CYHS2404177达格列净片上海现代制药股份有限公司4CYHS2404178多索茶碱口服溶液华益药业科技(安徽)有限公司3CYHS2404206多种微量元素注射液(Ⅲ)仁合益康汇泽药业河北有限公司4CYHS2404214二甲双胍恩格列净片(Ⅰ)宁波美舒医药科技有限公司;宁波美诺华天康药业有限公司4CYHS2404159二甲双胍恩格列净片(Ⅰ)宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2404147二甲双胍恩格列净片(Ⅲ)宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2404148二甲双胍恩格列净片(Ⅳ)宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2404150二甲双胍恩格列净片(Ⅴ)宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2404152二甲双胍恩格列净片(Ⅵ)宁波科尔康美诺华药业有限公司;宁波美诺华天康药业有限公司4CYHS2404154法莫替丁注射液广东君康药业有限公司;江西赣南海欣药业股份有限公司3CYHS2404140氟伐他汀钠缓释片浙江昂利康制药股份有限公司4CYHS2404228复方氨基酸注射液(20AA)四川科伦药业股份有限公司4CYHS2404196复方电解质醋酸钠葡萄糖注射液南京正科医药股份有限公司;湖南科伦制药有限公司3CYHS2404234复方电解质醋酸钠葡萄糖注射液南京正科医药股份有限公司;湖南科伦制药有限公司3CYHS2404233富马酸伏诺拉生片郑州韩都药业集团有限公司4CYHS2404141富马酸伏诺拉生片郑州韩都药业集团有限公司4CYHS2404143富马酸福莫特罗吸入溶液遂成药业股份有限公司4CYHS2404189富马酸喹硫平缓释片云南先施药业有限公司;山东药石药业有限公司4CYHS2404155富马酸喹硫平缓释片云南先施药业有限公司;山东药石药业有限公司4CYHS2404153腹膜透析液(乳酸盐-G1.5%)广东科泓药业有限公司4CYHS2404215格隆溴铵新斯的明注射液瑞阳制药股份有限公司3CYHS2404162环孢素软胶囊浙江美迪深生物医药有限公司;浙江仟源海力生制药有限公司4CYHS2404167黄体酮注射液南京卡文迪许生物工程技术有限公司;吉林敖东药业集团延吉股份有限公司3CYHS2404227甲氨蝶呤注射液国药一心制药有限公司;贵州阜康仁制药有限公司4CYHS2404151甲氨蝶呤注射液国药一心制药有限公司;贵州阜康仁制药有限公司4CYHS2404149甲钴胺片山东丹红制药有限公司;杨凌步长制药有限公司4CYHS2404182甲磺酸溴隐亭片浙江华海药业股份有限公司4CYHS2404204间苯三酚口腔崩解片南京海纳制药有限公司3CYHS2404166聚乙烯醇滴眼液广州仁恒医药科技股份有限公司;合肥华威药业有限公司4CYHS2404210克立硼罗软膏苏州天马医药集团天吉生物制药有限公司;南京海纳制药有限公司4CYHS2404142兰索拉唑肠溶胶囊石药集团中诺药业(石家庄)有限公司4CYHS2404172利丙双卡因乳膏国大(吉林)制药集团有限公司;南昌立健药业有限公司4CYHS2404200磷酸奥司他韦干混悬剂江西药都仁和制药有限公司3CYHS2404133磷酸奥司他韦胶囊石家庄四药有限公司4CYHS2404188硫酸特布他林注射液西安达莫制药有限公司;陕西金思铭生物技术有限公司3CYHS2404218硫酸特布他林注射液西安达莫制药有限公司;陕西金思铭生物技术有限公司3CYHS2404216罗沙司他胶囊河北紫薇山制药有限责任公司4CYHS2404211罗沙司他胶囊河北紫薇山制药有限责任公司4CYHS2404212吗啉硝唑氯化钠注射液南京黄龙生物科技有限公司;武汉福星生物药业有限公司4CYHS2404157美沙拉秦肠溶片南通联亚药业股份有限公司4CYHS2404195钠钾镁钙注射用浓溶液成都欣捷高新技术开发股份有限公司;山东华鲁制药有限公司3CYHS2404135尼莫地平片湖南科伦制药有限公司4CYHS2404237帕拉米韦氯化钠注射液石家庄四药有限公司4CYHS2404209帕拉米韦氯化钠注射液石家庄四药有限公司4CYHS2404208普拉洛芬滴眼液北京汇恩兰德制药有限公司4CYHS2404146乳果糖口服溶液陕西兴邦药业有限公司;陕西汉唐制药有限公司4CYHS2404221乳果糖口服溶液陕西兴邦药业有限公司;陕西汉唐制药有限公司4CYHS2404223乳果糖口服溶液陕西兴邦药业有限公司;陕西汉唐制药有限公司4CYHS2404219乳果糖口服溶液陕西兴邦药业有限公司;陕西汉唐制药有限公司4CYHS2404220乳果糖口服溶液陕西兴邦药业有限公司;陕西汉唐制药有限公司4CYHS2404222色甘酸钠滴眼液石家庄四药有限公司3CYHS2404207羧基麦芽糖铁注射液仁合益康集团有限公司;河北仁合益康药业有限公司4CYHS2404236羧基麦芽糖铁注射液仁合益康集团有限公司;河北仁合益康药业有限公司4CYHS2404235他达拉非片四川新斯顿制药股份有限公司4CYHS2404199他达拉非片四川新斯顿制药股份有限公司4CYHS2404198碳酸氢钠注射液南京赛瑞谱顿制药有限公司;江苏大红鹰恒顺药业有限公司3CYHS2404225碳酸氢钠注射液南京赛瑞谱顿制药有限公司;江苏大红鹰恒顺药业有限公司3CYHS2404224碳酸司维拉姆干混悬剂山东朗诺制药有限公司3CYHS2404201酮洛芬凝胶广州绿十字制药股份有限公司;乳源东阳光药业有限公司4CYHS2404174酮洛芬凝胶广州绿十字制药股份有限公司;乳源东阳光药业有限公司4CYHS2404173维生素B6注射液山西九康医药科技有限公司;扬州中宝药业股份有限公司3CYHS2404161西吡氯铵含片成都恒瑞制药有限公司3CYHS2404168缬沙坦氨氯地平片(Ⅰ)广州白云山医药集团股份有限公司白云山制药总厂4CYHS2404132盐酸氨溴索口服溶液合肥创新医药技术有限公司;上海海虹实业(集团)巢湖今辰药业有限公司4CYHS2404229盐酸氨溴索口服溶液合肥创新医药技术有限公司;上海海虹实业(集团)巢湖今辰药业有限公司4CYHS2404230盐酸氨溴索口服溶液合肥创新医药技术有限公司;上海海虹实业(集团)巢湖今辰药业有限公司4CYHS2404231盐酸氨溴索口服溶液合肥创新医药技术有限公司;上海海虹实业(集团)巢湖今辰药业有限公司4CYHS2404232盐酸氨溴索片山东济坤生物制药有限公司;山东鲁抗三叶制药有限公司4CYHS2404144盐酸丙卡特罗颗粒浙江恒研医药科技有限公司;浙江赛默制药有限公司3CYHS2404183盐酸丙卡特罗颗粒浙江恒研医药科技有限公司;浙江赛默制药有限公司3CYHS2404185盐酸丙卡特罗颗粒浙江恒研医药科技有限公司;浙江赛默制药有限公司3CYHS2404186盐酸氮卓斯汀滴眼液广东南国药业有限公司4CYHS2404226盐酸普罗帕酮注射液江苏润恒制药有限公司3CYHS2404163盐酸普罗帕酮注射液江苏润恒制药有限公司3CYHS2404164盐酸左沙丁胺醇雾化吸入溶液广州南新制药有限公司3CYHS2404181依帕司他片海南赛立克药业有限公司3CYHS2404160注射用厄他培南钠海南海灵化学制药有限公司4CYHS2404180注射用甲磺酸加贝酯南京泽恒医药技术开发有限公司;津药和平(天津)制药有限公司3CYHS2404194注射用赖氨匹林江西人可医药科技有限公司;山西普德药业有限公司3CYHS2404158注射用赖氨匹林江西人可医药科技有限公司;山西普德药业有限公司3CYHS2404156注射用硫酸艾沙康唑江苏迪赛诺制药有限公司4CYHS2404131注射用硫酸多粘菌素B合肥华威药业有限公司;山东豪瑞恩制药有限公司3CYHS2404191注射用硫酸多粘菌素B山东序列生物科技有限公司;博瑞制药(苏州)有限公司3CYHS2404145注射用氢化可的松琥珀酸钠成都米子生物医药科技有限公司;四川汇宇制药股份有限公司3CYHS2404176注射用氢化可的松琥珀酸钠成都米子生物医药科技有限公司;四川汇宇制药股份有限公司3CYHS2404175注射用头孢唑肟钠安徽杰玺医药有限公司;沈阳三九药业有限公司4CYHS2404203注射用头孢唑肟钠安徽杰玺医药有限公司;沈阳三九药业有限公司4CYHS2404202注射用吲哚菁绿江苏九旭药业有限公司3CYHS2404217左卡尼汀口服溶液山东新华制药股份有限公司;湖南九典制药股份有限公司4CYHS2404213左氧氟沙星滴眼液福建天泉药业股份有限公司;山东海山药业有限公司4CYHS2404205左乙拉西坦口服溶液温岭市创新生物医药科技股份有限公司;万邦德制药集团有限公司4CYHS2404134
4、新增一致性评价补充申报药品名称企业名称受理号艾司唑仑片新乡市常乐制药有限责任公司CYHB2450585布洛芬片山西太原药业有限公司CYHB2450590布洛芬片山西太原药业有限公司CYHB2450589硫酸奈替米星注射液青岛金峰制药有限公司CYHB2450591氯雷他定片浙江京新药业股份有限公司CYHB2450592乳酸钠林格注射液广东大冢制药有限公司CYHB2450595他克莫司胶囊浙江海正药业股份有限公司CYHB2450593他克莫司胶囊浙江海正药业股份有限公司CYHB2450594碳酸氢钠注射液国药集团容生制药有限公司CYHB2450596碳酸氢钠注射液湖北天圣药业有限公司CYHB2450588盐酸甲氧氯普胺注射液河南润弘制药股份有限公司CYHB2450586注射用奥美拉唑钠朗天药业(湖北)有限公司CYHB2450587注射用头孢他啶深圳信立泰药业股份有限公司CYHB2450598注射用头孢他啶深圳信立泰药业股份有限公司CYHB2450597
数据来源:摩熵药筛
用摩熵药筛小程序,随时随地查周报
一致性评价
2024-06-07
关注并星标CPHI制药在线
内包材,处理的方式
5月29日,FDA公布了一则召回通知,Sagent Pharmaceuticals 的多西紫杉醇(多西他赛)注射液因为可能含有颗粒物而全面召回。
图源 FDA
与以往的召回通知不同,这次直接在召回时就通知了颗粒物的来源可能性,瓶塞。
图源 FDA
对于注射剂而言,有几个指标是通用的,比如无菌,就是不得有活的微生物存在。毕竟一旦微生物随着注射剂进入人体,可能会将人体视为天然培养基而不断增殖。不同的微生物影响性不同,但以注射这种形式进入人体,势必是有害的。
再就是内毒素指标,我们可以粗略的将其理解为微生物的尸体,进入人体后会引起发烧。目前常用的是鲎试剂来检测内毒素,前几年有鲎试剂生产企业因动物保护等因素表示停产,一度引发注射剂药企震荡。
渗透压指标关系到药物组分在人体的运输发挥作用,保证药物能穿透膜或者不从膜里穿透出来。药典要求下除另有规定外,静脉输液及椎管注射用注射液按各品种项下的规定,照渗透压摩尔浓度测定法检查,应符合规定。
前面的属于生物因素,还有物理性因素,就是不溶性微粒,可以简单理解为颗粒物。因为颗粒物聚集,会引发静脉炎、肉芽肿以及心脏、肺、大脑的血凝,当然具体与颗粒数量、大小及病人状态有关。
关于不溶性微粒的来源,有的是药品配制过程中引入,环境、原辅料、注射用水、人员、设备都有可能有引发颗粒污染;有的是内包材因素,选择不适合的材质,会引发药液与内包材反应,导致脱屑等;有的是瓶子或者盖子没做好清洁,直接带入。
未见该召回药品的实物照片,但考虑到提及瓶塞结构,所以可能是卤化丁基橡胶塞子搭配西林瓶,当然尽管都是卤化丁基橡胶,但注射液和注射用冻干粉有不同的标准。如果是采用预灌封技术,那塞子的材质种类就可能是,氯化丁基橡胶活塞和溴化丁基橡胶活塞等。
图源 FDA
丁基橡胶塞子在灭菌或者储存过程中,可能会脱落不溶性颗粒,甚至有小分子物质逸出。在以前为了去除油性杂质,甚至会用到碱水浸泡,当然这个过程也容易引入杂质,现在多放弃了这个操作。也有了商业化的免洗无菌瓶塞,来了就能直接使用。
从药品审评中心公布的药包材登记数据看,注射用无菌粉末用溴化丁基橡胶塞、注射用无菌粉末用覆膜溴化丁基橡胶塞、注射用无菌粉末用覆聚氟乙烯/乙烯共聚物膜氯化丁基橡胶塞、注射用无菌粉末用覆四氟乙烯-六氟丙烯共聚物膜溴化丁基橡胶塞等多种,针对不同理化性质的注射液可以做针对性选择。
图源 药品审评中心网站
我们简单的分析一下,作为一个老产品,工艺方面引发的胶塞脱落颗粒概率不大,除非本身药品的理化性质出现了巨大差异,但如果那样的话,召回的理由就成了药品性能有问题。
如果不是免洗无菌胶塞,那么在清洗灭菌过程可能有对胶塞有损伤,比如冲洗震荡中一部分胶塞与器壁摩擦导致表面出现破损,而全自动灌装时无法察觉,使用到了产品上。那么在后期储存运输中,就有可能滑落,进入药品中。大颗粒的脱屑,理论上能在后面的灯检中发现问题,但未必此时就已经进入药液,所以有漏检概率。具体原因,以官方调查为准。
从这些年的注射剂召回数据看,瓶塞引发的质量问题确实不多。本次药品在临近有效期时才发现风险,也证实了橡胶塞老化或者出现问题需要一个时间的过度。并不是召回就意味着企业有问题,能发现问题,并予以纠正,比掩盖问题,把原因推给运输不当要好得多。
【企业推荐】
【智药研习社直播预告】
来源:CPHI制药在线
声明:本文仅代表作者观点,并不代表制药在线立场。本网站内容仅出于传递更多信息之目的。如需转载,请务必注明文章来源和作者。
投稿邮箱:Kelly.Xiao@imsinoexpo.com
▼更多制药资讯,请关注CPHI制药在线▼
点击阅读原文,进入智药研习社~
2024-05-30
The recall was attributed to a customer complaint of potential particulate matter from the drug's stopper.
Amid a shortage of standard-of-care chemotherapy drugs, Sagent Pharmaceuticals is pulling two lots of its docetaxel injection from U.S. shelves after receiving a report of potential particulate matter in a vial.
The recalled batches were distributed nationwide between October 2023 and April 2024 and are set to expire this December. Customers are being alerted by way of a FedEx package that includes instructions and necessary arrangements for the return of the product, according to an FDA notice.
Intravenous injection of a product that contains particulate matter poses serious health risks. So far, Sagent has not received word of any adverse events related to the recalled product.
Docetaxel is a generic chemotherapy used to treat a number of cancer types. Various doses of the drug already face shortages in the U.S., according to the American Society of Health-System Pharmacists (ASHP).
The FDA does not list a docetaxel shortage in its own database. Some docetaxel offerings from Mylan, Pfizer, Baxter, Sagent, Sandoz and Winthrop, among others, are still available, ASHP notes.
Back in September, Becker’s Hospital Review reported a shortage encompassing three-fourths of the U.S. docetaxel supply.
Doctors are recommended to weigh the available supply of the treatment before starting patients on a docetaxel-containing regimen, ASHP notes, as “no single agent” can be substituted for the chemo.
Generic chemotherapy shortages have run rampant for more than a year, prompting difficult choices for oncologists and increased danger for patients as supply is rationed. Alternative treatments can sometimes be “unconventional and unproven,” not to mention risky and extremely costly, the American Society of Clinical Oncologists (ASCO)’s chief medical officer Julie Gralow said in prepared testimony for a House hearing earlier this year.
The total number of U.S. drug shortages was at a record high in the first quarter, ASHP reported. The group was tracking 323 shortages at that time.

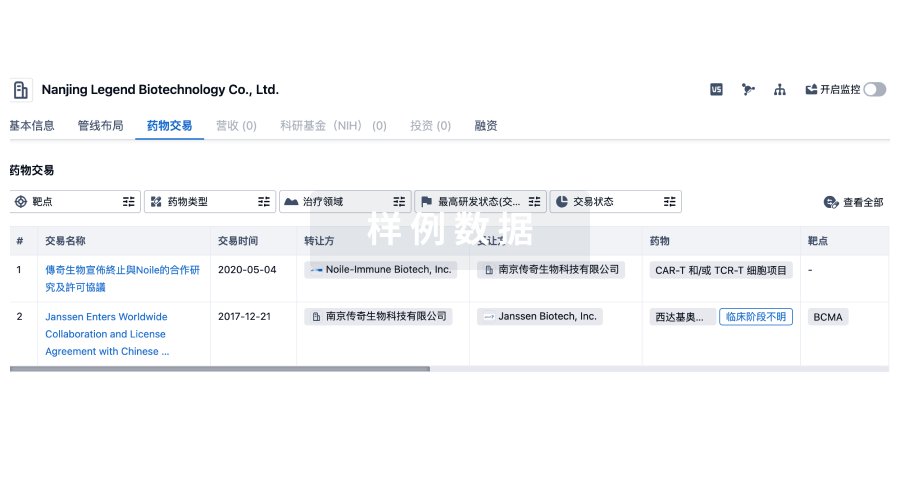
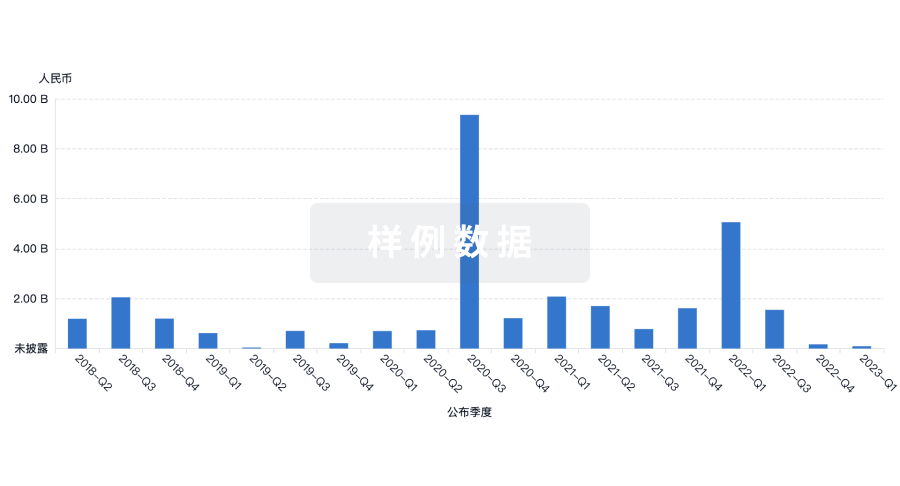
100 项与 Sagent Pharmaceuticals, Inc. 相关的药物交易
登录后查看更多信息
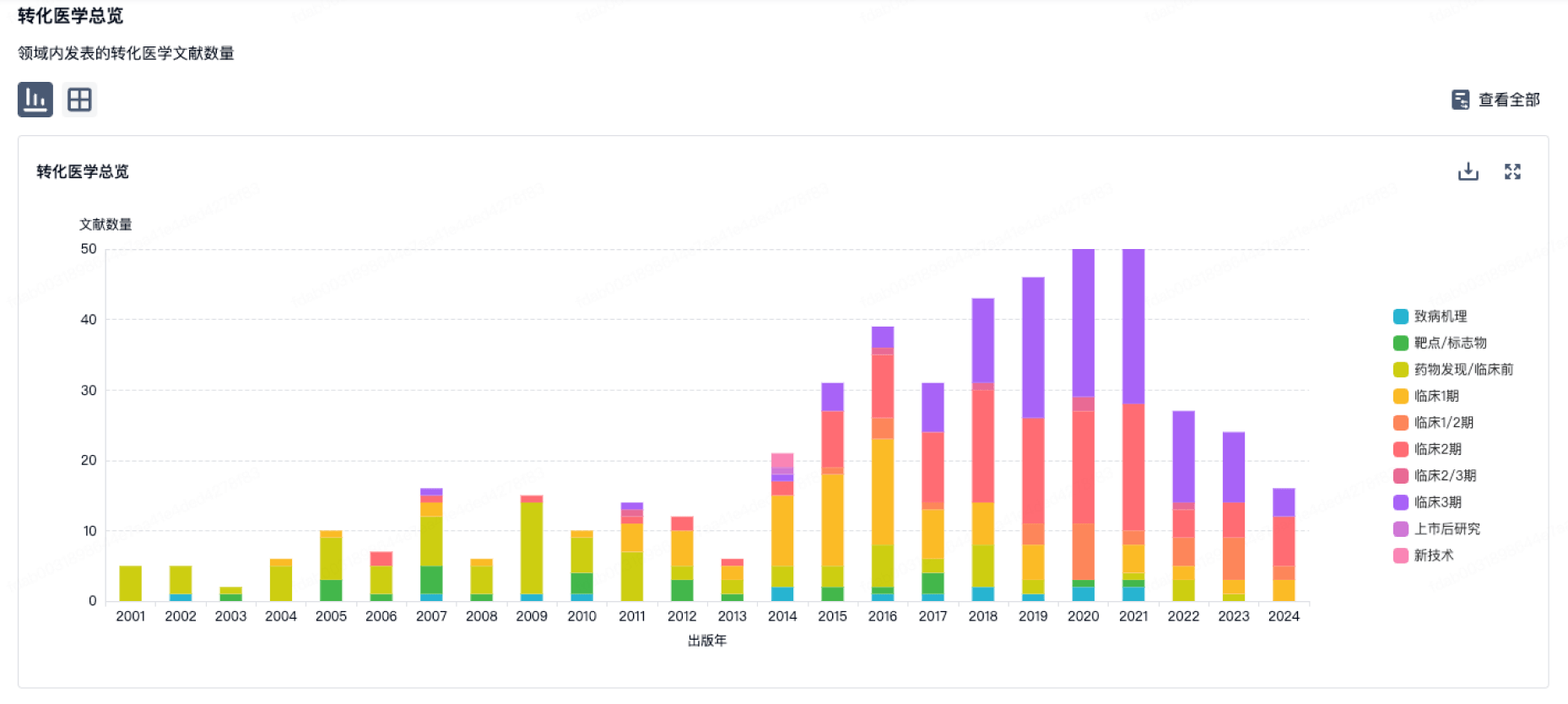
100 项与 Sagent Pharmaceuticals, Inc. 相关的转化医学
登录后查看更多信息
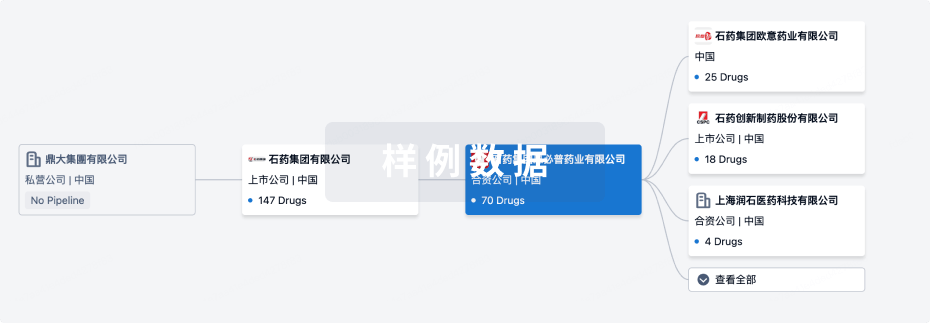
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年09月17日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床3期
1
2
批准上市
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
氟哌啶醇 ( DRDs ) | - | 批准上市 |
达托霉素 | 复杂皮肤和皮肤结构感染 更多 | 批准上市 |
BMS-986414 ( SARS-CoV-2 S protein ) | 新型冠状病毒感染 更多 | 临床3期 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
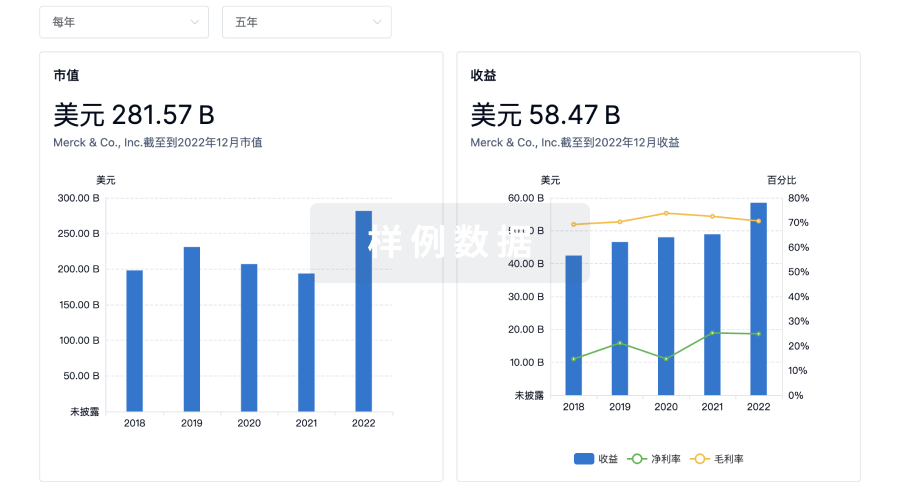
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

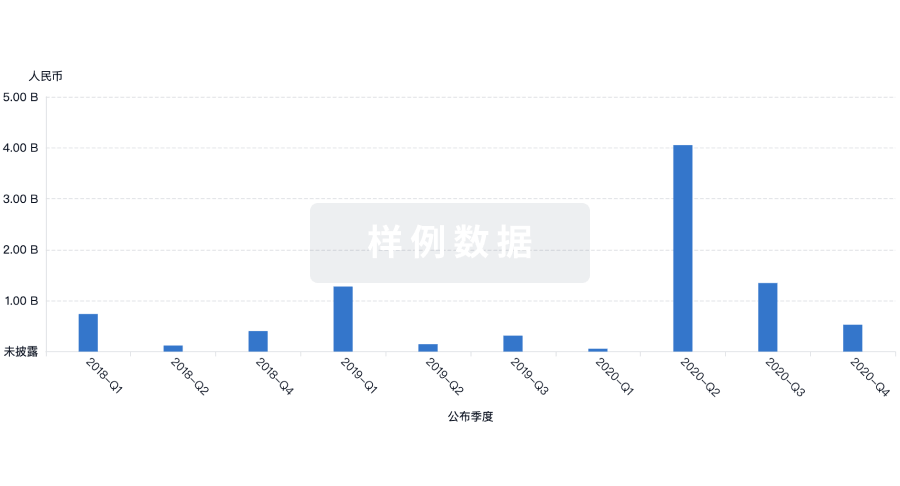
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用