预约演示
更新于:2025-08-12
Mannitol
甘露醇
更新于:2025-08-12
概要
基本信息
最高研发阶段批准上市 |
最高研发阶段(中国)批准上市 |
特殊审评孤儿药 (美国) |
登录后查看时间轴
结构/序列
分子式C6H14O6 |
InChIKeyFBPFZTCFMRRESA-KVTDHHQDSA-N |
CAS号69-65-8 |
关联
185
项与 甘露醇 相关的临床试验CTRI/2025/05/087854
Comparison of efficacy and safety profile of intravenous hypertonic saline versus mannitol in patients with spontaneous intracranial haemorrhage - a randomized controlled trial - NIL
开始日期2025-06-25 |
申办/合作机构- |
ChiCTR2500103212
Clinical study of mannitol in preventing postoperative nausea and vomiting after posterior scleral reinforcement
开始日期2025-06-09 |
申办/合作机构- |
NCT06884657
Propofol Level At TCI During Mannitol
Group 1 will include 20 patients aged 18 years and over, American Society of Anesthesiologist (ASA) II-III class, who will undergo supratentorial tumor surgery, and Group 2 will include 20 patients who will undergo pituitary surgery without mannitol. Total intravenous anesthesia (TIVA) will be adjusted to propofol 4 µg/dl and remifentanil 2-4 µg/dl with target-controlled infusion pumps. In the mannitol group, 2.5 ml/kg (0.5 g/kg) will be given to all patients 15 minutes after induction and the mannitol infusion will be adjusted to be 10 minutes.In Group 2, mannitol will not be used and 2.5 ml/kg isotonic will be administered in 10 minutes. Both blood and urine samples will take for measurement to propofol levels.
开始日期2025-03-20 |
申办/合作机构 |
100 项与 甘露醇 相关的临床结果
登录后查看更多信息
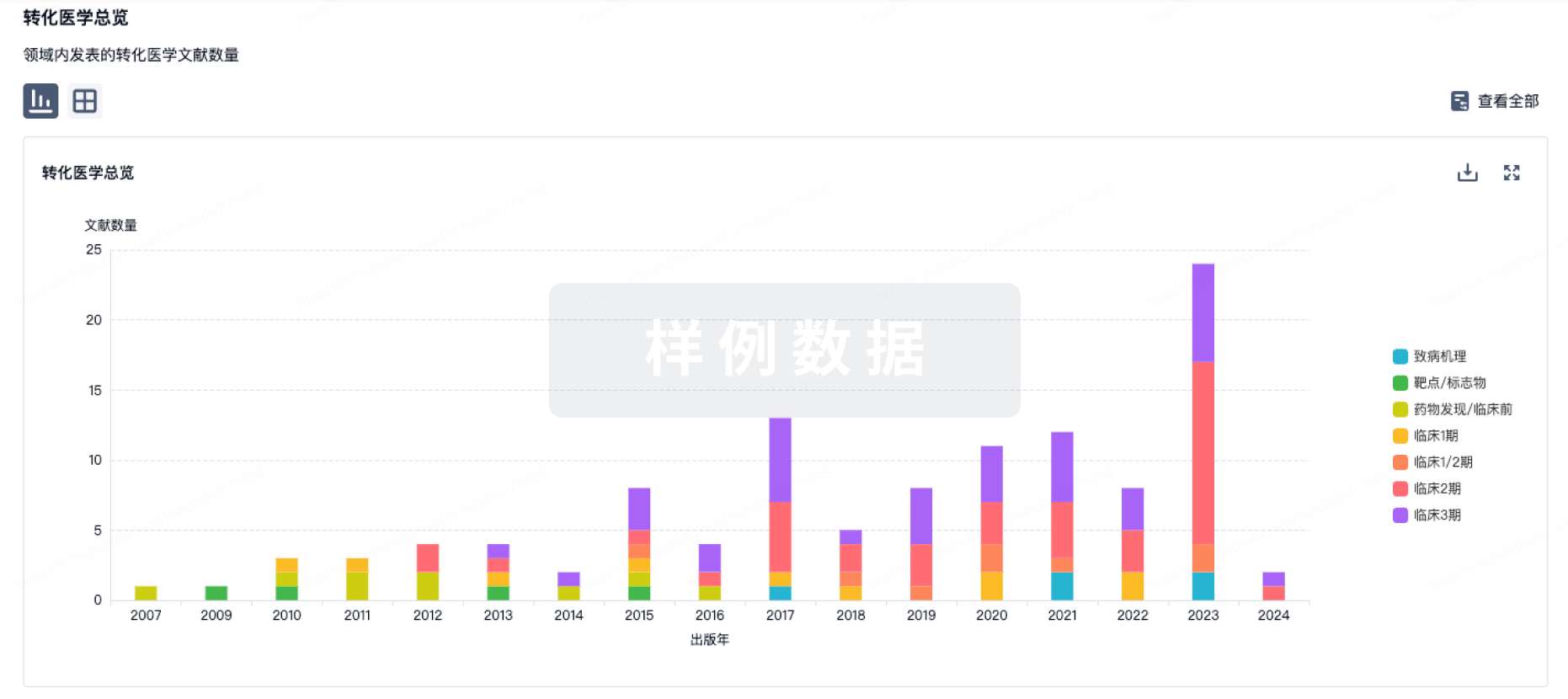
100 项与 甘露醇 相关的转化医学
登录后查看更多信息
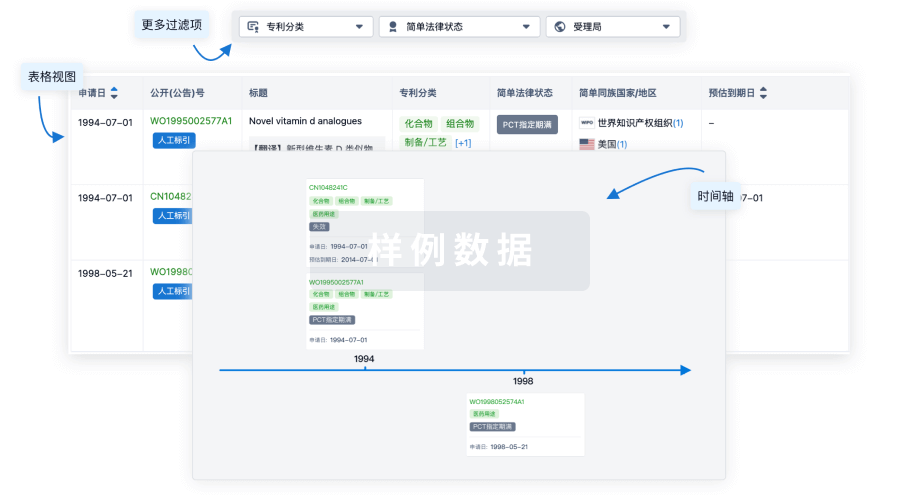
100 项与 甘露醇 相关的专利(医药)
登录后查看更多信息
33,591
项与 甘露醇 相关的文献(医药)2025-12-31·Plant Signaling & Behavior
Genome-wide identification and analysis of the NF-Y transcription factor family reveal its potential roles in tobacco (
Nicotiana tabacum
L.)
Article
作者: Sun, Jinhao ; Yue, Xiujiang ; Xue, Luyao ; Mao, Jingjing ; Wang, Baojian ; Chao, Jiangtao ; Fu, Jincun ; Li, Shaopeng ; Song, Wenting ; Cheng, Fanrui ; Wang, Dawei ; Tian, Zhen
Nuclear Factor Y (NF-Y) represents a group of transcription factors commonly present in higher eukaryotes, typically consisting of three subunits: NF-YA, NF-YB, and NF-YC. They play crucial roles in the embryonic development, photosynthesis, flowering, abiotic stress responses, and other essential processes in plants. To better understand the genome-wide NF-Y domain-containing proteins, the protein physicochemical properties, chromosomal localization, synteny, phylogenetic relationships, genomic structure, promoter cis-elements, and protein interaction network of NtNF-Ys in tobacco (Nicotiana tabacum L.) were systematically analyzed. In this study, we identified 58 NtNF-Ys in tobacco, respectively, and divided into three subfamilies corresponding to their phylogenetic relationships. Their tissue specificity and expression pattern analyses for leaf development, drought and saline-alkali stress, and ABA response were carried out using RNA-seq or qRT-PCR. These findings illuminate the role of NtNF-Ys in regulating plant leaf development, drought and saline-alkali stress tolerance, and ABA response. This study offers new insights to enhance our understanding of the roles of NtNF-Ys and identify potential genes involved in leaf development, as well as drought and saline-alkali stress tolerance of plants.
2025-12-31·Plant Signaling & Behavior
Phylogenetic relationship of WRKY transcription factors in
Solanum
and potato genes in response to hormonal and biotic stresses
Article
作者: Huang, Wenjuan ; Jiang, Dequan ; Liu, Jia
WRKY transcription factors are important regulators of plant responses to environmental stresses and hormone signaling. This study analyzes the WRKY gene family in Solanum tuberosum by examining the phylogenetic relationships, expression profiles, and their roles in abiotic stress and hormone responses. Phylogenetic tree was constructed using 322 WRKY genes from four Solanum species: S. tuberosum, S. pennellii, S. pimpinellifolium, and S. lycopersicum. The results revealed conserved and expanded WRKY genes across these species. We then studied the expression of 75 SotuWRKY genes in response to salt, drought, heat stresses, and hormone treatments (IAA, ABA, BABA, GA3, and BAP). Results showed that 19, 25, and 29 genes were regulated under salt, drought, and heat stresses, respectively. Several WRKY genes (e.g. SotuWRKY03 and SotuWRKY24) were also regulated by biotic stresses like Phytophthora infestans infection and hormone treatments, indicating their involvement in plant defense mechanisms. A gene co-expression network was constructed based on gene-to-gene correlations, where SotuWRKY52 was identified as a hub gene, positively regulating six WRKY genes and negatively regulating four. These findings suggest that potato WRKY genes play key roles in regulating stress responses and hormone signaling, potentially enhancing potato resistance to stresses and diseases. This study provides new insights into WRKY transcription factors in S. tuberosum and other Solanum species.
2025-12-31·Journal of Pharmaceutical Policy and Practice
Compounded glucagon-like peptide-1 receptor agonists for weight loss: the direct-to-consumer market in Colorado
Article
作者: Saseen, Joseph J. ; Dardouri, Mouna ; Nair, Kavita V. ; Moore, Gina D. ; DiStefano, Michael J.
Background:
High prices and other access barriers have contributed to the rise of a market for compounded glucagon-like peptide-1 receptor agonists for weight loss in the United States. This market has not been systematically studied. We conducted a pilot study to assess the prevalence, characteristics, and advertising content of direct-to-consumer providers of compounded glucagon-like peptide-1 products for weight loss in Colorado.
Methods:
We conducted a cross-sectional study of websites advertising compounded glucagon-like peptide-1 products for weight loss in Colorado. Websites were identified using Google searches focused on census-defined statistical areas. Searches were conducted between March 21 and April 12, 2024. Data collected from websites included physical addresses, business type, highest reported staff credential, advertised glucagon-like peptide-1 products, whether businesses referred to Food and Drug Administration approval when describing products, and whether businesses referred to products as 'generic'.
Results:
We identified 93 business websites advertising compounded glucagon-like peptide-1 products for weight loss corresponding to 188 physical locations throughout Colorado. Most businesses were self-categorized as medical/health spas (33/93) or weight loss services (26/93). Advertised products included semaglutide (92/93), tirzepatide (40/93), liraglutide (2/93), and retatrutide (1/93). Advertised combination products included B vitamins (8/93), levocarnitine (1/93), mannitol (1/93), BPC-157 (1/93), and glycine (1/93). Seven websites advertised oral formulations. Additionally, 41/93 websites referred to Food and Drug Administration approval in their descriptions of compounded products and 5/93 referred to products as 'generic'.
Conclusion:
This study identified several instances of unapproved glucagon-like peptide-1 products being compounded and advertised in Colorado. Additionally, 1 product was advertised as compounded with BPC-157, a substance determined by the Food and Drug Administration to be unsafe for compounding. This study also identified numerous examples of misleading claims regarding the regulatory status of compounded glucagon-like peptide-1 products. Regulatory action is needed to ensure the benefits of compounded GLP-1 products outweigh the risks.
191
项与 甘露醇 相关的新闻(医药)2025-07-31
1. 变更定义:根据变更对药品安全性、有效性和质量可控性影响的风险,将药品上市后变更分为重大变更、中等变更和微小变更。重大变更指影响可能性重大,中等变更影响可能性中等,微小变更影响可能性微小。2. 指导原则制定:整体原则是与国际先进变更技术要求接轨,同时总结国内变更监管发展和风险控制经验,以起草指导原则。3. 变更研究工作的基本原则:持有人和登记企业作为药品上市后变更管理的责任主体,负责评估和研究变更;完善的质量体系是科学变更的前提条件,需符合GMP药品上市后变更管理办法要求。4. 建议评估质量体系的ICH9、ICH10符合性,以确保变更控制体系的有效性和合规性。1. 在变更过程中,当生产设备发生中等变更,而生产工艺发生重大变更时,总体变更应判定为重大变更,遵循“就高不就低”的原则。2. 对于变更研究,建议使用商业化生产规模的样品进行,以确保研究的准确性和代表性。3. 中等变更情况下,可以进行变更前后的药学对比研究,必要时还需增加与参比制剂的对比研究,以全面评估变更的影响。1. 第四个基本原则强调稳定性研究,要求申请人在年报中报告长期稳定性研究结果,并在发现异常时及时汇报。2. 第五个基本原则关注原辅包变更对制剂的影响,规定原辅包变更时供应商需及时通知制剂持有人,持有人应评估变更影响并决定年报备案或补充申请。3. 上市申请时,建议申请人充分研究并选择供货能力强、质量好的原辅包供应商,进行商业化大生产规模的工艺验证。4. 原料药变更时,制剂持有人应参照先前发布的原料药变更问答进行研究和申报。5. 中等变更研究的技术要求遵循2021年发布的化学药品药学变更研究技术指导原则,此为变更指南的核心文件。1. 我们在进行变更研究时,需要遵循ICH系列一部分M系列的指导原则,以及中心发布的各项药学变更药学研究的指导原则和个药指南,确保技术要求与国际接轨。2. 中心网站已发布关于溶出曲线研究、原料变更等常用指南,以及一些变更的共性问题解答,但这些内容仅是基础,需要结合更深入的研究和指导原则。3. 研究验证工作根据变更的性质(从微小到中等到重大)逐步升级,涉及的研究批次、内容、稳定性考察的批次和时间也相应增加。4. 对于重大变更,研究验证可能需要包括体内生物等效性研究,这是为了确保变更后的药品与原药品具有相同的生物利用度和临床效果。1. 中等变更需进行全面的杂质谱、关键理化性质、溶出曲线对比研究,确保变更前后一致性,否则将升级为重大变更。2. 中等变更对研发人员专业水平要求高,需熟练掌握各项技术指导原则,以通过药学研究确保药品的安全、有效和质量可控。3. 与重大变更可能需要的体内生物等效性研究不同,中等变更主要依赖药学研究,这要求研发人员具备高水平的专业技能。4. 变更研究工作的重点内容需特别关注,包括但不限于杂质分析、理化性质测试和溶出曲线分析,以确保药品质量不受影响。1. 对于口服固体制剂的中等变更,需按照溶出曲线研究的问答要求,在多种介质(包括偏值1.24.5 6.8加标准介质3加1)中进行变更前后样品的溶出曲线研究,采用讲法50转或兰法100转,避免随意添加表面活性剂或调整转速。2. 常见问题包括:持有人未进行溶出度和溶出曲线检查,仅进行溶出度检查而未研究溶出曲线,仅在一种介质中进行溶出曲线研究,溶出条件不符合要求(如随意调高转速或添加表面活性剂),以及溶出曲线研究条件虽符合要求但相似性计算不当(如挑选时间点或取样点不符合F2计算要求)。3. 中等变更时,持有人应结合处方工艺、降解途径、国内外文献等,对变更前后的产品进行全面的杂质谱分析,包括有机杂质、无机杂质、溶剂残留和致突变杂质的对比研究。4. 在进行溶出曲线研究时,需确保研究条件符合规定,避免随意更改研究参数,确保研究的准确性和一致性。5. 对于杂质谱的研究,持有人应充分考虑变更对产品质量可能产生的影响,通过对比研究确保变更前后产品的安全性、有效性和质量一致性。1. 对杂质谱的对比需按照Q3AQ3BICH3CICH3D及HHM9M7等特定要求进行,研发人员需熟悉这些指导原则。2. 中等变更对关键理化性质的研究不仅限于常规质量标准检测项目,还需根据变更情形对比额外质量指标。3. 特殊制剂如脂质体注射液的质量研究需增加关注点,包括脂质体组成、包封药物状态、体内环境适应性及体外释放度等指标。4. 仅仅按照质量标准进行检验是不够的,需结合具体变更情形开展更全面的质量对比研究。5. 对于特殊制剂的质量指标研究,需考虑其独特性质和使用环境,以确保变更后的制剂质量和安全性。1. 变更原料药供应商需要进行全面的质量对比研究,包括原料的杂志谱、纯度、粒度等属性,以评估变更风险。2. 对变更前后的制剂进行全面质量对比,包括杂志谱、溶出曲线和关键理化性质,确保变更后产品与原产品保持一致,否则被视为重大变更。3. 稳定性研究的要求比其他中等变更事项更为严格,需要更多的批次和更长的时间来验证原料变更对产品稳定性的影响。4. 关注变更过程中可能出现的误差传递,确保研究验证工作的准确性和可靠性,避免因原料供应商变更引起的质量问题。1. 在辅料用量和生产批量发生多次变更时,需按照指导原则与关键临床试验批BEP进行比较,以避免多次微小或中等变更累计成为重大变更。比较对象为关键临床实验批,即最初批准的批次。2. 对于基于BCS分类豁免BE上市的药物,在变更时应考虑与参比制剂进行处方溶出曲线对比,确保变更后仍符合M9的要求。3. 基于大规格并研究豁免而来的小规格药物,在变更时需与大规格进行处方溶出曲线对比研究,确保变更后仍符合豁免的要求。4. 豁免要求来源于两个重要指导原则:国内发布的生物等效性研究指导原则和国际上正在协调的ICH M13B指南。5. 这两个指导原则是进行药物变更研究和确保符合豁免要求的关键依据,对于药物研发和生产具有重要指导意义。1. 对于一个早期上市的口服固体制剂,即使标准中未包含有关物质或溶出度检查,持有人在进行中等变更时,仍需进行相应研究,建立可靠的方法。2. 变更要求包括进行变更前后的杂志谱和溶出曲线的对比,以确保技术要求不放松,即便对于老品种也一样严格。3. 变更分类的第四部分内容着重于结合审评案例和关注点,介绍十种常见变更事项的分类,明确哪些情况属于中等变更。4. 变更分类的基本原则强调基于风险进行分类,而不是基于研究结果,这是因为分类需预先评估变更可能带来的风险程度。1. 微小、中等和重大变更后的产品质量需不低于变更前,因此不能仅依据研究结果进行变更分类。2. 严格执行变更指导原则,依据风险进行变更分类,而非研究结果。3. 案例一:原料药精制溶剂由乙醇变为丙二醇,尽管申请人认为质量提升,但根据指导原则,这属于重大变更。4. 案例二:片剂干燥方式由烘箱干燥变为流化床干燥,即便申请人认为变更前后质量一致,这依然被视为重大变更。5. 强调变更分类应基于风险评估,而非仅根据研究结果确定变更级别。1. 当药品出现安全有效质量问题并需要变更时,如因生产工艺缺陷或稳定性问题导致的有效期变更、增加新的过程控制方法或制定更严格的限度,被视为重大变更。2. 因安全性、质量可控性原因增加检测项目,同样属于重大变更,需特别关注变更的必要性、依据以及是否增加产品风险。3. 中等变更应有充分的依据和必要性,例如从一个分析方法变更到另一个分析方法,如果能提高检测的灵敏度或能力,则鼓励此类变更;反之则不鼓励。4. 指导原则列举的中等变更情形不一定始终为中等变更,其前提是变更前后各项质量指标需保持一致,这是中等变更的基本条件。5. 对于变更原料药的生产工艺这一事项,其分类为中等变更需满足质量指标一致性等特定条件。1. 变更原料药的生产工艺最重要的事项是变更合成路线,尤其是当延长后的路线与起始原料原合成路线不一致时,被视为重大变更,不符合药品注册管理办法要求,需撤回重报。2. 变更生产工艺及工艺参数,如不影响原料药的关键质量属性,可定义为中等变更;若可能影响关键质量属性,如大幅调整反应温度和时间,则被视为重大变更。3. 将返工工艺纳入固定生产工艺属于中等变更,但在实施前,企业必须进行偏差分析,明确返工原因及生产中出现的问题。4. 其他变更,如起始原料、武警原料药以及过滤参数的调整,需确保指控水平和产品质量不降低,否则也可能构成重大变更。1. 变更起始原料的合成路线时,若起始原料的质量不降低,可按中等变更来管理。2. 一个典型案例中,申请人将起始原料从已批准的原料药变更为化工原料,这被审评认为增加了质量可控的风险。3. 原料的选择不符合ICH11的要求,导致该变更申请未被同意,强调了原料选择的重要性。4. 变更生产设备的要求是关键质量属性必须保持不变,确保产品质量稳定。1. 变更制剂处方中的辅料种类通常被视为重大变更,除非变更的是着色剂或矫味剂,此时被视为中等变更。2. 变更着色剂和矫味剂的种类需遵守多项限制条件,包括不能影响规格间的差异、儿童用药口味适应性,且不会引发潜在安全性问题。3. 辅料种类变更需充分研究,如口崩片的蔗糖变更为糖精钠,虽用量差异大,但仍属于辅料种类的重大变更,而非简单替换。4. 辅料的技术等级变更,如口服固体制剂中磷酸氢钙二水合物变更为无水磷酸钙,可能显著影响产品质量,被视为重大变更;但在注射剂中,此类变更可能被视为同种辅料,不属于重大变更。5. 变更辅料的质量标准时,必须确保质量控制水平不降低,同时调整辅料用量需谨慎,以维持产品安全性和有效性。1. 对于普通口服固体制剂,辅料用量变更的评估基于其占原基准处方总重量的百分比,明确了各辅料变更的范围,并特别界定了片中变化的界定。2. 特别关注BCS4类及治疗窗窄的药物,这类药物的变更只分为微小和重大,不存在中等变更,需严格控制。3. 变更比例计算依据原批准处方总重量的比例,需特别注意润滑剂、助留剂等辅料的变化范围较窄,在变更时需格外谨慎,以防超出中等变更的界限。4. 缓控释制剂和常用制剂的辅料用量变更分为两种计算方式,其中普通辅料的变更比例计算方法与普通口服固体制剂相同,即依据原批准片中的比例计算。5. 基于过往审评案例,超出了中等变更范围的申请均未被批准,强调了在变更辅料用量时,必须严格遵守规定的变更比例,避免过度变更。1. 对非无菌半固体制剂的变更分类非常严格,辅料用量的变更按占原基准用量的百分比计算,分母为辅料原基准用量,而非总重。2. 变更的总和有特定规定,其中防腐剂的用量变更需单独计算。3. 口服溶液、滴眼剂、注射剂、吸入制剂的辅料种类和用量变更,无论具体剂型,均界定为重大变更。4. 除了指导原则中提及的口服固体制剂和非无菌半固体制剂外,其他所有剂型的辅料种类和用量变更同样被视为重大变更。1. 对于双层片辅料用量的变更分类,建议将每层视为独立片剂单独计算,若变更分类不同,则采取较高风险级别。2. 在考虑包长绒一机里的长绒质积的比表面积变更时,需重视其对肠溶制剂溶出行为的影响,综合考量辅料用量变更。3. 变更普通口服固体制剂中可能影响吸收的辅料,如甘露醇、山梨醇、表面活性剂等,应参照ICH M9指导原则,严格按辅料绝对量比例计算相似性。4. 变更制剂生产工艺及工艺参数时,若不影响关键质量属性,可定义为中等变更,这是药品中心网站发布的共性问题之一。1. 变更注射剂的冻干曲线可能直接影响产品的关键质量属性,建议按照重大变更管理。2. 普通口服固体制剂包衣液中的有机溶剂变更为水,指导原则按中等变更管理,前提是不影响产品质量;反之,水变成有机溶剂,建议按重大变更管理。3. 智利溶剂中乙醇含量从60%降至20%,由于直接关系到产品的质和量,建议按照处方或生产工艺的重大变更来管理。4. 变更过程控制、生产设备、外形等,需确保指控水平不降低且产品质量不变。5. 变更制剂所用原料药的供应商,多数情况下被视为中等变更。1. 复杂工艺的缓控释制剂及长溶制剂的理解:这类制剂包括高长绒衣工艺、热熔挤出工艺和激光打孔工艺等,与简单工艺如凝胶骨架型口服缓控释制剂或紧包肠溶胶囊壳的肠溶胶囊相比,具有更高的风险,因此不应随意扩大简单工艺的范围。2. 变更生产批量的特殊关注点:批量变更通常伴随着设备和工艺参数的变更,无论变更倍数大小,都需要进行生产工艺验证和全面的质量对比研究,以确保变更后的生产质量和安全性。3. 变更注册标准中的中等变更类型:包括新增检验项目、收紧限度或文字描述的变更,其中新增检验项目并不一定都属于中等变更,其分类受到多种限制条件的影响。4. 对于批量变更和注册标准变更,强调了研究的全面性和对潜在风险的关注,以确保产品质量和生产过程的稳定性。5. 在处理上述变更事项时,需谨慎评估其对产品安全性和有效性的影响,遵循相关法规和指导原则,确保变更的合理性和可控性。1. 为了更有效地控制产品质量,增加相应的措施,以确保产品质量的更好保证。2. 方法学验证和拟定的控制限度需符合指导原则的要求,这些限度和验证不是随意设定,而是要进行全面的考虑和实施。3. 不将因安全性和质量可控性问题导致的增加检验项目归类为中等变更,例如检出致突变杂质或原标准中缺少有关物质检查项,这些情况下需申报重大变更。4. 对于上市申请时批件中留有的后续研究内容,完成这些内容后应申报补充申请,而非通过中等变更备案,以确保遵守相关新增检验项目的规定。5. 收紧限度不包括因药品生产工艺、处方等重大变更引起的限度范围缩小,如原料药生产工艺增加微粉化处理导致微力度减小的情况,这不属于收紧限度的范畴。1. 文字描述的变更通常涉及修正个别文字错误或语句不通顺问题,不包括检验方法或限度的变更。2. 检验方法和限度的变更,如HPLC法的进氧量由一微升变为五微升,或有关物质计算方法由面积规划法变更为自身对照法,被视为重大变更。3. 着色剂变更导致产品性状颜色的改变,如从黄色变为蓝色,同样被视为重大变更。4. 建议不要随意扩大文字描述变更的范围,应仅限于修正错误。5. 变更包装材料和容器,特别是对于风险较小的制剂和原料药的包材材质或类型,是另一个重要变更事项。1. 变更注射剂的包材供应商、尺寸、形状等,以及变更多剂量包装制剂的包装装量,曾被考虑为重要变更。2. 样品中心后续发布了新指南,包括化学药品及生物制品说明书通用格式撰写指南和化学药品说明书标签药学相关信息的撰写指南。3. 中信网站仿制药共性问题专栏讨论了增加包装装量的问题,指出滴眼剂、外用制剂、口服溶液等的装量变更需按重大变更申请增加规格。4. 当前管理规定下,装量作为规格表述的一部分,其变更需关注规格的合理性,不能通过中等变更简单增加装量。5. 结果是,原先考虑的变更注射剂包材和多剂量包装装量的方案不再适用,需遵循新的管理和申请流程。1. 变更有效期,若由处方工艺变更或产品质量问题引起,则属于重大变更。2. 变更储藏条件,无论是放宽还是严格化,一律视为重大变更。3. 增加规格,无论具体细节,均被归类为重大变更。4. 讨论的两个案例虽非直接增加规格,但与规格描述密切相关,同样需重视。5. 在变更管理中,有效期、储藏条件及规格的任何调整,均需按其潜在影响程度妥善评估与处理。1. 第一个案例涉及口服溶液申请在规格项下增加无糖型描述未获批准,因为根据中国药典规定,无糖型不可加入规格描述中,规格应指单位制剂中的主要成分重量、含量或装量。2. 第二个案例是关于母乳高规格变更申请从十克0.3克变更为3%未被批准。依据近两年发布的标签说明书撰写指南,外用制剂的表述应为浓度(多少克/多少毫升),仅描述浓度是不科学的。3. 这些案例都属于修改规格描述的重大变更尝试,但均未获得批准,强调了在药品规格描述中遵循中国药典和相关指南的重要性。4. 从这些案例中可以看出,对于药品规格的描述必须严格遵守官方规定和指导原则,不得随意更改或添加非标准描述,以确保药品信息的准确性和科学性。1. 变更生产场地时,需特别关注伴随的设备或工艺参数变更,以及确保多个生产场地采用相同的生产工艺,仅允许因生产设备不同导致的个别工艺参数差异。2. 即使普通口服固体制剂仅变更生产地址而无其他关联变更,根据溶出曲线研究的问答和变更指导原则,仍需进行变更前后多种介质中的溶出曲线对比研究。3. 中等变更研究时,持有人登记企业作为药品上市后变更管理的责任主体,负责评估和研究工作,确保变更的科学性和合理性。4. 完善的质量体系是实施科学变更的前提,持有人的变更控制体系必须符合药品生产质量管理规范和药品上市后变更管理办法的要求。5. 在进行中等变更研究的过程中,需综合考虑变更的风险、研究的深度和质量体系的完善程度,以保障药品质量和患者安全。1. 评估质量体系的ICH9、ICH10的符合性,确保持有人的质量标准达标。2. 中等变更的研究需由专业技术人员执行,要求其熟练掌握国内外相关指导原则。3. 变更分类应基于风险评估,而不仅仅是根据研究结果进行分类,以确保变更的合理性与安全性。4. 对变更前后产品进行全面的质量对比,这不仅仅是简单的标准检验,需要对比研究较多额外的质量指标,以确保变更前后的质量一致性。5. 中等变更的处理需要深入研究和全面评估,确保所有可能影响产品质量的因素都被考虑到,以维护产品的整体质量标准。RA NEXT智能体发布转载CDE-生物类似药CMC质量控制研究的考虑转载CDE质量标准核定要求与常见问题分析_原文创新药审评中临床药理常见问题和考虑转载CDE-制剂工艺信息表核定要求与常见问题分析转载CDE-化药仿制药原料药工艺常见问题-概览202502CDE化学创新药质量控制与常见问题分析_原文
2025-07-31
·药闻康策
☝ 点击上方 一键预约 ☝ 最新最热的医药健康新闻政策☝ ☝ 点击查看峰会活动议程 ☝ ☝ 各省、自治区、直辖市及新疆生产建设兵团卫生健康委、中医药局:为进一步指导各级各类医疗机构做好基孔肯雅热医疗救治工作,提高规范化、同质化诊疗水平,我们在2008年发布的基孔肯雅热诊断和治疗方案基础上,组织制定了基孔肯雅热诊疗方案(2025年版)。现印发给你们,请参照执行。国家卫生健康委办公厅国家中医药局综合司2025年7月31日基孔肯雅热诊疗方案(2025年版)基孔肯雅热(Chikungunya fever,CHIK)是由基孔肯雅病毒(Chikungunya virus,CHIKV)感染引起,经伊蚊叮咬传播的急性传染病。临床以发热、关节痛、皮疹为主要特征。基孔肯雅热在全球热带和亚热带地区广泛流行,流行范围呈持续扩大趋势。我国伊蚊分布广泛,近年来已经发生多起境外输入病例导致的本地传播疫情。为进一步规范基孔肯雅热临床诊疗工作,在2008年发布的《基孔肯雅热诊断和治疗方案》基础上,结合国内外最新研究进展和诊疗经验,制定本诊疗方案。一、病原学基孔肯雅病毒属于披膜病毒科甲病毒属,病毒颗粒呈球形,有包膜,直径为60~70nm,只有1个血清型。基因组为单股正链RNA,长度约11.8kb,内含单一可读框依次编码4种非结构蛋白和5种结构蛋白。根据病毒基因组遗传进化分析,分为3个基因型,分别为西非型、东-中-南非型和亚洲型,其中东-中-南非型病毒突变形成的印度洋分支(IOL)病毒株,更易于经白纹伊蚊叮咬传播。基孔肯雅病毒对热敏感,56℃30分钟可灭活;不耐酸,70%乙醇、1%次氯酸钠、脂溶剂、过氧乙酸、甲醛、戊二醛、酚类、碘伏和季铵盐化合物等消毒剂及紫外照射可灭活。二、流行病学(一)传染源。基孔肯雅热急性期患者、隐性感染者和感染病毒的非人灵长类动物。大多数患者在发病当天至发病后7天内具有传染性。(二)传播途径。主要通过携带基孔肯雅病毒的伊蚊(主要为白纹伊蚊和埃及伊蚊)叮咬传播。可发生母婴传播。罕见情况下可经输血或接触患者血液传播。(三)易感人群。人群对基孔肯雅病毒普遍易感。人感染病毒后可获得持久免疫力。(四)流行特征。1952年在坦桑尼亚首次发现基孔肯雅病毒,最初在非洲流行,之后不断扩散到东南亚、南亚、印度洋岛屿及美洲地区。截至2025年6月,全球已有119个国家和地区报告了基孔肯雅热的本地传播。我国白纹伊蚊分布范围广泛,适合病毒快速传播的蚊媒活跃期长,存在“输入性病例-本地传播流行”模式。2010-2019年,我国发生4起基孔肯雅热境外输入继发本地病例,其中2010年广东东莞、2019年云南瑞丽发生聚集性疫情。2025年7月,广东佛山发生境外输入继发聚集性疫情。三、发病机制基孔肯雅病毒经伊蚊叮咬侵入人体数日内形成病毒血症,发病后3天内是高病毒血症期,随后病毒载量下降,常于病后5~7天消失。病毒通过其包膜上的E1、E2蛋白与巨噬细胞、上皮细胞、内皮细胞、成纤维细胞等细胞上的受体结合,通过细胞内吞作用进入细胞,在细胞内复制。病毒可直接侵入关节,在关节内复制,也可直接感染人成骨细胞、滑膜、腱鞘、肌肉中的巨噬细胞和成纤维细胞,导致促炎细胞因子、趋化因子释放、白细胞募集、凝血因子与补体相关蛋白失调,造成成骨细胞功能受损、骨质破坏,并可引发全身性感染和多器官损伤。慢性关节炎发病机制未完全明确,可能与病毒驱动炎症反应及T细胞持续激活相关。四、临床表现潜伏期1~12天,常为3~7天。(一)发热:急性起病,发热以中低热为主,部分患者可为高热,可伴畏寒、头痛、背痛、全身肌肉疼痛、畏光、恶心、呕吐等。热程多为1~7天。(二)关节痛:为基孔肯雅热的显著特征,可为首发症状。初始为单个或两个关节疼痛,常在24~48小时内出现多个关节疼痛,可呈对称性分布。主要累及远端小关节,如踝、指、腕和趾关节等,也可累及膝和肩等大关节。疼痛随运动加剧,关节僵硬,可影响活动。受累关节周围肿胀、压痛,少数大关节受累者可出现关节腔积液。绝大多数患者的关节疼痛及僵硬状态在发病数天内恢复,部分患者关节疼痛和僵硬可超过12周,有的甚至持续18个月以上,个别患者遗留关节功能损害。(三)皮疹:多数患者在发病后2~5天出现皮疹,常分布在躯干、四肢、手掌和足底,也可累及面部,为斑疹、丘疹或斑丘疹,疹间皮肤多正常,呈斑片状或弥漫性分布,部分伴有瘙痒。数天后消退,可伴轻微脱屑。(四)其他:可出现恶心、呕吐、食欲减退、头痛和肌肉疼痛等非特异性症状。部分患者淋巴结肿大伴触痛,以颈部淋巴结肿大为主。部分患者出现结膜炎,少数出现虹膜睫状体炎、视网膜炎和葡萄膜炎等眼部表现。儿童病例高热多见,发热持续3~5日,除了关节疼痛,皮疹较成人更多见,可见累及面部的斑片状或弥漫性斑丘疹、疱疹、褶烂样皮损等。新生儿感染多在出生后3~7日内出现临床表现,包括发热、喂养困难,皮疹更广泛,可见肢端瘀斑和水肿。极少数出现严重并发症,如脑膜脑炎、脊髓炎、心肌炎、急性肝损害、急性肾损害等,出血性并发症发生率极低。五、实验室检查(一)一般检查。1.血常规:白细胞计数多正常,部分患者可见淋巴细胞和血小板轻度减少,新生儿感染血小板减少较常见。2.生化检查:部分患者血清丙氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)、肌酸激酶(CK)可升高。3.脑脊液检查:并发脑膜脑炎时脑脊液检查符合病毒性脑炎改变。(二)病原学和血清学检查。1.核酸检测:采用实时荧光PCR或等温扩增核酸检测等方法检测血液样本中的基孔肯雅病毒核酸。2.病毒分离:采用Vero、C6/36、BHK-21和HeLa等敏感细胞进行病毒分离。3.血清抗体检测:采用ELISA、免疫层析等方法检测血清特异性IgM和IgG抗体。IgM抗体于发病3~4天可检出,5天后阳性率增高,可持续数周至数月,因IgM抗体在潜伏期和发病早期阳性率低,阴性不能排除感染。IgG抗体于发病后第5~8天可检出,可持续数年。(三)影像学检查。可见关节滑膜炎、关节肿胀、关节腔积液、腱鞘炎等改变。六、诊断根据流行病学史、临床表现及实验室检查结果,综合分析作出诊断。(一)疑似病例。发病前12天内,曾到过基孔肯雅热流行区或居住、工作场所周围曾有本病发生;且有上述临床表现(如发热、关节痛或皮疹等)者。(二)临床诊断病例。疑似病例,且血清特异性IgM抗体阳性者。(三)确诊病例。疑似病例或临床诊断病例,具有以下任一项者:1.基孔肯雅病毒核酸阳性;2.临床标本培养分离到基孔肯雅病毒;3.血清基孔肯雅病毒IgG抗体阳转或恢复期较急性期抗体滴度呈4倍及以上升高。七、鉴别诊断主要与以发热、关节痛或皮疹为主要临床表现的相关疾病鉴别,关节疼痛和僵硬持续时间长者要与其他慢性关节炎鉴别。(一)登革热。登革热与基孔肯雅热的传播媒介相同,流行区域基本相同,临床表现类似,较难鉴别,且可存在合并感染的情况。登革热发热多为中高热,持续时间更长,肌肉痛、腹部症状(腹痛、腹胀、便秘等)更明显,有出血倾向,外周血白细胞和血小板减少明显,红细胞压积、ALT或AST常增高,重症较基孔肯雅热多见,可出现休克、脑病、多器官功能障碍等并发症。而基孔肯雅热多为中低热,关节疼痛明显,可为首发症状,多累及远端小关节,外周血白细胞、血小板基本正常,重症少见。需核酸检测鉴别。在登革热流行高风险区,建议也对登革热进行检测。(二)寨卡病毒病。寨卡病毒病与基孔肯雅热的传播媒介相同,流行区域基本相同,临床表现类似,亦表现为中低热,可伴皮疹、头痛、关节痛、肌痛和结膜炎,孕妇感染可引起胎儿小头畸形。基孔肯雅热关节痛更明显。需核酸检测鉴别。(三)传染性红斑。由细小病毒B19感染引起。儿童感染可表现为持续中高热,常合并皮疹,皮疹为多形性、多部位分布,典型表现为面颊部红斑样皮疹伴有口周苍白圈,称之为“掌击脸”,也可出现受累关节部位红斑、关节痛,常见外周血红细胞下降。核酸及病毒抗体检测有助于鉴别诊断。(四)其他。本病还需与疟疾、其他甲病毒感染、流感、麻疹、风疹、传染性单核细胞增多症、风湿热、反应性关节炎、类风湿关节炎、系统性红斑狼疮等疾病相鉴别。八、重症病例、重症高危人群和重症预警指标本病重症少见,但境外基孔肯雅热疫情暴发时有重症及死亡病例报告,要加强病情监测,警惕重症病例发生。(一)重症病例。重症病例至少有一个器官或系统出现功能障碍,常见以下系统受累:1.神经系统受累:脑膜脑炎、吉兰-巴雷综合征、脊髓炎等;2.心脏受累:心肌炎、恶性心律失常、心源性休克等;3.急性肝损伤:血清ALT或AST>1000IU/L或总胆红素>85.5μmol/L;4.出凝血障碍:皮下血肿、便血等出血和弥漫性血管内凝血(DIC)等。(二)重症高危人群。1.婴儿;2.老年人(65岁以上);3.晚期妊娠和围产期妇女;4.慢性基础疾病患者;5.免疫抑制者(器官移植、AIDS、长期使用免疫抑制剂等)。(三)重症预警指标。1.持续高热或退热后病情加重;2.神经系统症状:剧烈头痛、烦躁不安、嗜睡等;3.心血管系统症状:心悸、胸闷、胸痛、心律失常、四肢厥冷、尿量减少等;4.呼吸系统症状:呼吸急促、呼吸困难等;5.出血表现:皮肤瘀斑、黏膜出血、黑便等。九、治疗目前尚无特异性治疗方法,以对症支持治疗为主。(一)一般治疗。1.关节疼痛明显者,建议卧床休息,受损关节应制动,避免负重和剧烈运动(如爬山、长跑等),防止加重关节损伤。2.监测神志、生命体征、尿量、血小板、电解质、肝功能、出凝血功能等重症预警指标,及时处置,有基础疾病者要积极治疗原发病。3.避免盲目使用抗菌药物。4.不推荐使用糖皮质激素和免疫球蛋白。因原发病正在接受糖皮质激素和免疫球蛋白治疗的患者,根据原发病诊治需要和预期风险及获益权衡决定。(二)对症治疗。1.退热:以物理降温为主。高热不退者推荐使用对乙酰氨基酚,应避免使用阿司匹林等非甾体类抗炎药(NSAIDs)。有因基础疾病在服用阿司匹林的患者,应评估出血风险,决定是否停用或换用其他替代药物。儿童使用水杨酸类药物有引发Reye综合征风险,应避免使用。2.镇痛:(1)急性期关节疼痛不能忍受者,可使用对乙酰氨基酚。对乙酰氨基酚应以必需的最低剂量和最短疗程使用为原则,避免用于有肝病或转氨酶升高等禁忌证的患者。(2)急性期过后关节仍疼痛者可使用局部外用贴剂,也可考虑红外线等物理治疗。3.止痒:皮肤瘙痒者可予抗组胺药物口服或炉甘石洗剂外用。(三)重症治疗。1.神经系统。脑水肿可予甘露醇或利尿剂等脱水治疗;癫痫发作和癫痫持续状态,给予抗癫痫药物治疗,出现中枢性呼吸衰竭应及时给予辅助通气;不建议常规使用糖皮质激素、免疫球蛋白等,仅在急性脊髓膜炎患者使用免疫抑制剂,吉兰-巴雷综合征推荐使用免疫球蛋白。2.循环系统。(1)液体管理需要静脉补液患者,建议使用晶体液(如林格氏液)进行补液。休克患者,液体补足后组织灌注仍然不良,使用血管活性药物,首选去甲肾上腺素。(2)心脏支持卧床休息,保持大便通畅。存在严重心律失常时,予抗心律失常药物治疗。发生心衰时,限制液体入量,予利尿、扩血管等治疗。3.血液系统。(1)出血治疗出血部位明确者,如严重鼻衄给予局部止血,胃肠道出血者给予抑酸药、生长抑素等。血红蛋白低于60g/L,可输注浓缩红细胞。血小板计数低于30×109/L伴严重出血者,可输注血小板。(2)DIC治疗适时补充凝血因子、纤维蛋白原和血小板等。4.严重肝损伤。予抗炎保肝药物治疗,肝衰竭者可予人工肝等治疗。(四)中医治疗。基孔肯雅热属于中医湿温范畴,病因为蚊虫疫毒,发病初期表现为卫分证,部分患者可传入气分或出现卫气同病,核心病机是风邪袭表、湿毒蕴热。1.辨证分型。(1)急性期临床表现:发热,或伴恶风,四肢关节疼痛,可伴有关节肿胀,全身肌肉酸痛,四肢躯干弥漫性红斑或丘疹,或伴瘙痒,口渴,疲倦乏力。舌淡或淡红,舌苔白腻或黄腻,脉濡滑。治法:清热化湿,疏风透疹推荐方药:广藿香10g、葛根15g、羌活10g、滑石20g、赤芍10g、淡豆豉10g、淡竹叶10g、生地黄10g、连翘15g煎服法:每日1~2剂,水煎服,每次100ml~200ml,每日2~4次,口服。儿童剂量酌减,婴儿用1/3成人量,幼儿用1/2成人量,学龄儿童用2/3成人量或成人量。以下处方服法相同(如有特殊情况,须遵医嘱)。加减法:皮疹瘙痒较重者,加地肤子10g、荆芥10g。发热体温超过38.5℃者,增加中药服用量至每日2~3剂,每4~6小时服用一次;高热超过36小时不退者,加生石膏30g、香薷10g;出现高热、狂躁、谵语神昏、四肢抽搐者,予清瘟败毒饮加减,或加用安宫牛黄丸。(2)恢复期①湿滞经络证临床表现:关节疼痛迁延不愈,四肢关节活动不利,或呈游走性疼痛,疲倦乏力,身体沉重。舌淡,苔白或白腻,脉细或濡缓。治法:除湿蠲痹推荐方药:羌活8g、独活12g、肉桂3g、秦艽15g、海风藤15g、桑枝15g、当归10g、川芎6g、乳香6g、木香6g、甘草6g②肺脾气虚证临床表现:疲倦乏力,气短,汗出,胸闷,纳差,胃胀,大便稀溏或黏腻。舌淡,苔白腻,脉细弱。治法:益气健脾推荐方药:党参15g、黄芪15g、陈皮10g、茯苓15g、炒白扁豆15g、炒麦芽15g、巴戟天10g、麦冬10g、五味子5g、炙甘草10g③肝郁脾虚证临床表现:心烦,心慌,情绪紧张,口干口苦,失眠,胃胀,纳差。舌淡红,苔少,脉弦细。治法:疏肝健脾推荐方药:浮小麦30g、女贞子12g、炒酸枣仁15g、麦冬10g、茯神10g、炙甘草10g、陈皮5g、炒白扁豆15g、白芍15g、山药15g2.外治法。(1)中药沐足功效:清热祛湿解肌。可改善发热、疲倦、关节痛等不适。操作方法:广藿香、淡竹叶各30g,煮水沐足。(2)放血疗法功效:泻热解毒,通络止痛。用于高热患者的退热治疗或关节疼痛治疗。操作方法:高热者于大椎或耳尖点刺放血;关节疼痛者可对关节部位进行放血拔罐。(3)中药熏洗功效:化湿通络止痛。可改善关节疼痛。操作方法:忍冬藤、威灵仙、宽筋藤各30g,煎煮后取煎汁,纱布浸药,冷敷于疼痛处。(4)中药湿敷功效:清热收敛。可改善皮疹瘙痒。操作方法:黄柏、马齿苋各30g,煎煮后冷湿敷,每日2次。十、病例发现与报告医疗机构发现基孔肯雅热疑似病例、临床诊断病例和确诊病例,应于24小时内通过“中国疾病预防控制信息系统”进行网络直报。十一、医院感染控制及解除隔离标准(一)医院感染控制。1.疑似、临床诊断和确诊病例急性期须采取防蚊隔离措施,医疗机构应落实防蚊灭蚊措施,病区、医护办公室、值班室安装纱门纱窗,病区内可增设灭蚊灯、蚊香等。患者使用蚊帐。2.常规检查尽可能在床旁进行,因检查外出病房时,应做好防蚊及环境准备工作。患者外出时,应穿着长袖衣裤,减少皮肤暴露,建议使用防蚊驱避剂。3.按照标准预防原则做好医院感染控制,接触血液、体液、分泌物、排泄物等要佩戴一次性医用手套,做好手卫生,防止医院感染。患者出院后执行终末消毒,患者使用过的蚊帐用含有效氯消毒剂浸泡、清洗后,方可重复使用。4.做好医院及周边环境蚊媒孳生地处理,降低蚊密度。(二)解除隔离标准。体温恢复正常超过24小时,基孔肯雅病毒核酸检测阴性或病程超过7天者,可以解除隔离。十二、预防目前我国尚无可供使用的基孔肯雅病毒疫苗。预防主要措施包括及时清除蚊虫孳生地,降低蚊媒密度;个人应使用蚊香、驱避剂、蚊帐等方式驱蚊、灭蚊和防蚊;前往基孔肯雅热流行区的旅行者要提高防范意识,防止在境外感染基孔肯雅热。(来源:国家卫生健康委)药闻康策新媒体矩阵微信公众号点击下方 一键关注【免责声明】1.“药闻康策”部分文章信息来源于网络转载是出于传递更多信息之目的,并不意味着赞同其观点或证实其内容的真实性。如对内容有疑议,请及时与我司联系。2.“药闻康策”致力于提供合理、准确、完整的资讯信息,但不保证信息的合理性、准确性和完整性,且不对因信息的不合理、不准确或遗漏导致的任何损失或损害承担责任。3.“药闻康策”所有信息仅供参考,不做任何商业交易或医疗服务的根据,如自行使用“药闻康策”内容发生偏差,我司不承担任何责任,包括但不限于法律责任,赔偿责任。欢迎转发分享、点赞、点在看
2025-07-31
来源:国家卫健委7月31日,为进一步指导各级各类医疗机构做好基孔肯雅热医疗救治工作,提高规范化、同质化诊疗水平,在2008年发布的基孔肯雅热诊断和治疗方案基础上,国家卫生健康委和国家中医药管理局发布了基孔肯雅热诊疗方案(2025年版)。基孔肯雅热诊疗方案(2025年版)基孔肯雅热(Chikungunya fever,CHIK)是由基孔肯雅病毒(Chikungunya virus,CHIKV)感染引起,经伊蚊叮咬传播的急性传染病。临床以发热、关节痛、皮疹为主要特征。基孔肯雅热在全球热带和亚热带地区广泛流行,流行范围呈持续扩大趋势。我国伊蚊分布广泛,近年来已经发生多起境外输入病例导致的本地传播疫情。为进一步规范基孔肯雅热临床诊疗工作,在2008年发布的《基孔肯雅热诊断和治疗方案》基础上,结合国内外最新研究进展和诊疗经验,制定本诊疗方案。一、病原学基孔肯雅病毒属于披膜病毒科甲病毒属,病毒颗粒呈球形,有包膜,直径为60~70nm,只有1个血清型。基因组为单股正链RNA,长度约11.8kb,内含单一可读框依次编码4种非结构蛋白和5种结构蛋白。根据病毒基因组遗传进化分析,分为3个基因型,分别为西非型、东-中-南非型和亚洲型,其中东-中-南非型病毒突变形成的印度洋分支(IOL)病毒株,更易于经白纹伊蚊叮咬传播。基孔肯雅病毒对热敏感,56℃30分钟可灭活;不耐酸,70%乙醇、1%次氯酸钠、脂溶剂、过氧乙酸、甲醛、戊二醛、酚类、碘伏和季铵盐化合物等消毒剂及紫外照射可灭活。二、流行病学(一)传染源。基孔肯雅热急性期患者、隐性感染者和感染病毒的非人灵长类动物。大多数患者在发病当天至发病后7天内具有传染性。(二)传播途径。主要通过携带基孔肯雅病毒的伊蚊(主要为白纹伊蚊和埃及伊蚊)叮咬传播。可发生母婴传播。罕见情况下可经输血或接触患者血液传播。(三)易感人群。人群对基孔肯雅病毒普遍易感。人感染病毒后可获得持久免疫力。(四)流行特征。1952年在坦桑尼亚首次发现基孔肯雅病毒,最初在非洲流行,之后不断扩散到东南亚、南亚、印度洋岛屿及美洲地区。截至2025年6月,全球已有119个国家和地区报告了基孔肯雅热的本地传播。我国白纹伊蚊分布范围广泛,适合病毒快速传播的蚊媒活跃期长,存在“输入性病例-本地传播流行”模式。2010-2019年,我国发生4起基孔肯雅热境外输入继发本地病例,其中2010年广东东莞、2019年云南瑞丽发生聚集性疫情。2025年7月,广东佛山发生境外输入继发聚集性疫情。三、发病机制基孔肯雅病毒经伊蚊叮咬侵入人体数日内形成病毒血症,发病后3天内是高病毒血症期,随后病毒载量下降,常于病后5~7天消失。病毒通过其包膜上的E1、E2蛋白与巨噬细胞、上皮细胞、内皮细胞、成纤维细胞等细胞上的受体结合,通过细胞内吞作用进入细胞,在细胞内复制。病毒可直接侵入关节,在关节内复制,也可直接感染人成骨细胞、滑膜、腱鞘、肌肉中的巨噬细胞和成纤维细胞,导致促炎细胞因子、趋化因子释放、白细胞募集、凝血因子与补体相关蛋白失调,造成成骨细胞功能受损、骨质破坏,并可引发全身性感染和多器官损伤。慢性关节炎发病机制未完全明确,可能与病毒驱动炎症反应及T细胞持续激活相关。四、临床表现潜伏期1~12天,常为3~7天。(一)发热:急性起病,发热以中低热为主,部分患者可为高热,可伴畏寒、头痛、背痛、全身肌肉疼痛、畏光、恶心、呕吐等。热程多为1~7天。(二)关节痛:为基孔肯雅热的显著特征,可为首发症状。初始为单个或两个关节疼痛,常在24~48小时内出现多个关节疼痛,可呈对称性分布。主要累及远端小关节,如踝、指、腕和趾关节等,也可累及膝和肩等大关节。疼痛随运动加剧,关节僵硬,可影响活动。受累关节周围肿胀、压痛,少数大关节受累者可出现关节腔积液。绝大多数患者的关节疼痛及僵硬状态在发病数天内恢复,部分患者关节疼痛和僵硬可超过12周,有的甚至持续18个月以上,个别患者遗留关节功能损害。(三)皮疹:多数患者在发病后2~5天出现皮疹,常分布在躯干、四肢、手掌和足底,也可累及面部,为斑疹、丘疹或斑丘疹,疹间皮肤多正常,呈斑片状或弥漫性分布,部分伴有瘙痒。数天后消退,可伴轻微脱屑。(四)其他:可出现恶心、呕吐、食欲减退、头痛和肌肉疼痛等非特异性症状。部分患者淋巴结肿大伴触痛,以颈部淋巴结肿大为主。部分患者出现结膜炎,少数出现虹膜睫状体炎、视网膜炎和葡萄膜炎等眼部表现。儿童病例高热多见,发热持续3~5日,除了关节疼痛,皮疹较成人更多见,可见累及面部的斑片状或弥漫性斑丘疹、疱疹、褶烂样皮损等。新生儿感染多在出生后3~7日内出现临床表现,包括发热、喂养困难,皮疹更广泛,可见肢端瘀斑和水肿。极少数出现严重并发症,如脑膜脑炎、脊髓炎、心肌炎、急性肝损害、急性肾损害等,出血性并发症发生率极低。五、实验室检查(一)一般检查。1.血常规:白细胞计数多正常,部分患者可见淋巴细胞和血小板轻度减少,新生儿感染血小板减少较常见。2.生化检查:部分患者血清丙氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)、肌酸激酶(CK)可升高。3.脑脊液检查:并发脑膜脑炎时脑脊液检查符合病毒性脑炎改变。(二)病原学和血清学检查。1.核酸检测:采用实时荧光PCR或等温扩增核酸检测等方法检测血液样本中的基孔肯雅病毒核酸。2.病毒分离:采用Vero、C6/36、BHK-21和HeLa等敏感细胞进行病毒分离。3.血清抗体检测:采用ELISA、免疫层析等方法检测血清特异性IgM和IgG抗体。IgM抗体于发病3~4天可检出,5天后阳性率增高,可持续数周至数月,因IgM抗体在潜伏期和发病早期阳性率低,阴性不能排除感染。IgG抗体于发病后第5~8天可检出,可持续数年。(三)影像学检查。可见关节滑膜炎、关节肿胀、关节腔积液、腱鞘炎等改变。六、诊断根据流行病学史、临床表现及实验室检查结果,综合分析作出诊断。(一)疑似病例。发病前12天内,曾到过基孔肯雅热流行区或居住、工作场所周围曾有本病发生;且有上述临床表现(如发热、关节痛或皮疹等)者。(二)临床诊断病例。疑似病例,且血清特异性IgM抗体阳性者。(三)确诊病例。疑似病例或临床诊断病例,具有以下任一项者:1.基孔肯雅病毒核酸阳性;2.临床标本培养分离到基孔肯雅病毒;3.血清基孔肯雅病毒IgG抗体阳转或恢复期较急性期抗体滴度呈4倍及以上升高。七、鉴别诊断主要与以发热、关节痛或皮疹为主要临床表现的相关疾病鉴别,关节疼痛和僵硬持续时间长者要与其他慢性关节炎鉴别。(一)登革热。登革热与基孔肯雅热的传播媒介相同,流行区域基本相同,临床表现类似,较难鉴别,且可存在合并感染的情况。登革热发热多为中高热,持续时间更长,肌肉痛、腹部症状(腹痛、腹胀、便秘等)更明显,有出血倾向,外周血白细胞和血小板减少明显,红细胞压积、ALT或AST常增高,重症较基孔肯雅热多见,可出现休克、脑病、多器官功能障碍等并发症。而基孔肯雅热多为中低热,关节疼痛明显,可为首发症状,多累及远端小关节,外周血白细胞、血小板基本正常,重症少见。需核酸检测鉴别。在登革热流行高风险区,建议也对登革热进行检测。(二)寨卡病毒病。寨卡病毒病与基孔肯雅热的传播媒介相同,流行区域基本相同,临床表现类似,亦表现为中低热,可伴皮疹、头痛、关节痛、肌痛和结膜炎,孕妇感染可引起胎儿小头畸形。基孔肯雅热关节痛更明显。需核酸检测鉴别。(三)传染性红斑。由细小病毒B19感染引起。儿童感染可表现为持续中高热,常合并皮疹,皮疹为多形性、多部位分布,典型表现为面颊部红斑样皮疹伴有口周苍白圈,称之为“掌击脸”,也可出现受累关节部位红斑、关节痛,常见外周血红细胞下降。核酸及病毒抗体检测有助于鉴别诊断。(四)其他。本病还需与疟疾、其他甲病毒感染、流感、麻疹、风疹、传染性单核细胞增多症、风湿热、反应性关节炎、类风湿关节炎、系统性红斑狼疮等疾病相鉴别。八、重症病例、重症高危人群和重症预警指标本病重症少见,但境外基孔肯雅热疫情暴发时有重症及死亡病例报告,要加强病情监测,警惕重症病例发生。(一)重症病例。重症病例至少有一个器官或系统出现功能障碍,常见以下系统受累:1.神经系统受累:脑膜脑炎、吉兰-巴雷综合征、脊髓炎等;2.心脏受累:心肌炎、恶性心律失常、心源性休克等;3.急性肝损伤:血清ALT或AST>1000IU/L或总胆红素>85.5μmol/L;4.出凝血障碍:皮下血肿、便血等出血和弥漫性血管内凝血(DIC)等。(二)重症高危人群。1.婴儿;2.老年人(65岁以上);3.晚期妊娠和围产期妇女;4.慢性基础疾病患者;5.免疫抑制者(器官移植、AIDS、长期使用免疫抑制剂等)。(三)重症预警指标。1.持续高热或退热后病情加重;2.神经系统症状:剧烈头痛、烦躁不安、嗜睡等;3.心血管系统症状:心悸、胸闷、胸痛、心律失常、四肢厥冷、尿量减少等;4.呼吸系统症状:呼吸急促、呼吸困难等;5.出血表现:皮肤瘀斑、黏膜出血、黑便等。九、治疗目前尚无特异性治疗方法,以对症支持治疗为主。(一)一般治疗。1.关节疼痛明显者,建议卧床休息,受损关节应制动,避免负重和剧烈运动(如爬山、长跑等),防止加重关节损伤。2.监测神志、生命体征、尿量、血小板、电解质、肝功能、出凝血功能等重症预警指标,及时处置,有基础疾病者要积极治疗原发病。3.避免盲目使用抗菌药物。4.不推荐使用糖皮质激素和免疫球蛋白。因原发病正在接受糖皮质激素和免疫球蛋白治疗的患者,根据原发病诊治需要和预期风险及获益权衡决定。(二)对症治疗。1.退热:以物理降温为主。高热不退者推荐使用对乙酰氨基酚,应避免使用阿司匹林等非甾体类抗炎药(NSAIDs)。有因基础疾病在服用阿司匹林的患者,应评估出血风险,决定是否停用或换用其他替代药物。儿童使用水杨酸类药物有引发Reye综合征风险,应避免使用。2.镇痛:(1)急性期关节疼痛不能忍受者,可使用对乙酰氨基酚。对乙酰氨基酚应以必需的最低剂量和最短疗程使用为原则,避免用于有肝病或转氨酶升高等禁忌证的患者。(2)急性期过后关节仍疼痛者可使用局部外用贴剂,也可考虑红外线等物理治疗。3.止痒:皮肤瘙痒者可予抗组胺药物口服或炉甘石洗剂外用。(三)重症治疗。1.神经系统。脑水肿可予甘露醇或利尿剂等脱水治疗;癫痫发作和癫痫持续状态,给予抗癫痫药物治疗,出现中枢性呼吸衰竭应及时给予辅助通气;不建议常规使用糖皮质激素、免疫球蛋白等,仅在急性脊髓膜炎患者使用免疫抑制剂,吉兰-巴雷综合征推荐使用免疫球蛋白。2.循环系统。(1)液体管理需要静脉补液患者,建议使用晶体液(如林格氏液)进行补液。休克患者,液体补足后组织灌注仍然不良,使用血管活性药物,首选去甲肾上腺素。(2)心脏支持卧床休息,保持大便通畅。存在严重心律失常时,予抗心律失常药物治疗。发生心衰时,限制液体入量,予利尿、扩血管等治疗。3.血液系统。(1)出血治疗出血部位明确者,如严重鼻衄给予局部止血,胃肠道出血者给予抑酸药、生长抑素等。血红蛋白低于60g/L,可输注浓缩红细胞。血小板计数低于30×109/L伴严重出血者,可输注血小板。(2)DIC治疗适时补充凝血因子、纤维蛋白原和血小板等。4.严重肝损伤。予抗炎保肝药物治疗,肝衰竭者可予人工肝等治疗。(四)中医治疗。基孔肯雅热属于中医湿温范畴,病因为蚊虫疫毒,发病初期表现为卫分证,部分患者可传入气分或出现卫气同病,核心病机是风邪袭表、湿毒蕴热。1.辨证分型。(1)急性期临床表现:发热,或伴恶风,四肢关节疼痛,可伴有关节肿胀,全身肌肉酸痛,四肢躯干弥漫性红斑或丘疹,或伴瘙痒,口渴,疲倦乏力。舌淡或淡红,舌苔白腻或黄腻,脉濡滑。治法:清热化湿,疏风透疹推荐方药:广藿香10g、葛根15g、羌活10g、滑石20g、赤芍10g、淡豆豉10g、淡竹叶10g、生地黄10g、连翘15g煎服法:每日1~2剂,水煎服,每次100ml~200ml,每日2~4次,口服。儿童剂量酌减,婴儿用1/3成人量,幼儿用1/2成人量,学龄儿童用2/3成人量或成人量。以下处方服法相同(如有特殊情况,须遵医嘱)。加减法:皮疹瘙痒较重者,加地肤子10g、荆芥10g。发热体温超过38.5℃者,增加中药服用量至每日2~3剂,每4~6小时服用一次;高热超过36小时不退者,加生石膏30g、香薷10g;出现高热、狂躁、谵语神昏、四肢抽搐者,予清瘟败毒饮加减,或加用安宫牛黄丸。(2)恢复期①湿滞经络证临床表现:关节疼痛迁延不愈,四肢关节活动不利,或呈游走性疼痛,疲倦乏力,身体沉重。舌淡,苔白或白腻,脉细或濡缓。治法:除湿蠲痹推荐方药:羌活8g、独活12g、肉桂3g、秦艽15g、海风藤15g、桑枝15g、当归10g、川芎6g、乳香6g、木香6g、甘草6g②肺脾气虚证临床表现:疲倦乏力,气短,汗出,胸闷,纳差,胃胀,大便稀溏或黏腻。舌淡,苔白腻,脉细弱。治法:益气健脾推荐方药:党参15g、黄芪15g、陈皮10g、茯苓15g、炒白扁豆15g、炒麦芽15g、巴戟天10g、麦冬10g、五味子5g、炙甘草10g③肝郁脾虚证临床表现:心烦,心慌,情绪紧张,口干口苦,失眠,胃胀,纳差。舌淡红,苔少,脉弦细。治法:疏肝健脾推荐方药:浮小麦30g、女贞子12g、炒酸枣仁15g、麦冬10g、茯神10g、炙甘草10g、陈皮5g、炒白扁豆15g、白芍15g、山药15g2.外治法。(1)中药沐足功效:清热祛湿解肌。可改善发热、疲倦、关节痛等不适。操作方法:广藿香、淡竹叶各30g,煮水沐足。(2)放血疗法功效:泻热解毒,通络止痛。用于高热患者的退热治疗或关节疼痛治疗。操作方法:高热者于大椎或耳尖点刺放血;关节疼痛者可对关节部位进行放血拔罐。(3)中药熏洗功效:化湿通络止痛。可改善关节疼痛。操作方法:忍冬藤、威灵仙、宽筋藤各30g,煎煮后取煎汁,纱布浸药,冷敷于疼痛处。(4)中药湿敷功效:清热收敛。可改善皮疹瘙痒。操作方法:黄柏、马齿苋各30g,煎煮后冷湿敷,每日2次。十、病例发现与报告医疗机构发现基孔肯雅热疑似病例、临床诊断病例和确诊病例,应于24小时内通过“中国疾病预防控制信息系统”进行网络直报。十一、医院感染控制及解除隔离标准(一)医院感染控制。1.疑似、临床诊断和确诊病例急性期须采取防蚊隔离措施,医疗机构应落实防蚊灭蚊措施,病区、医护办公室、值班室安装纱门纱窗,病区内可增设灭蚊灯、蚊香等。患者使用蚊帐。2.常规检查尽可能在床旁进行,因检查外出病房时,应做好防蚊及环境准备工作。患者外出时,应穿着长袖衣裤,减少皮肤暴露,建议使用防蚊驱避剂。3.按照标准预防原则做好医院感染控制,接触血液、体液、分泌物、排泄物等要佩戴一次性医用手套,做好手卫生,防止医院感染。患者出院后执行终末消毒,患者使用过的蚊帐用含有效氯消毒剂浸泡、清洗后,方可重复使用。4.做好医院及周边环境蚊媒孳生地处理,降低蚊密度。(二)解除隔离标准。体温恢复正常超过24小时,基孔肯雅病毒核酸检测阴性或病程超过7天者,可以解除隔离。十二、预防目前我国尚无可供使用的基孔肯雅病毒疫苗。预防主要措施包括及时清除蚊虫孳生地,降低蚊媒密度;个人应使用蚊香、驱避剂、蚊帐等方式驱蚊、灭蚊和防蚊;前往基孔肯雅热流行区的旅行者要提高防范意识,防止在境外感染基孔肯雅热。声明:本微信注明来源的稿件均为转载,仅用于分享,不代表平台立场,如涉及版权等问题,请尽快联系我们,我们第一时间更正,谢谢
临床研究疫苗
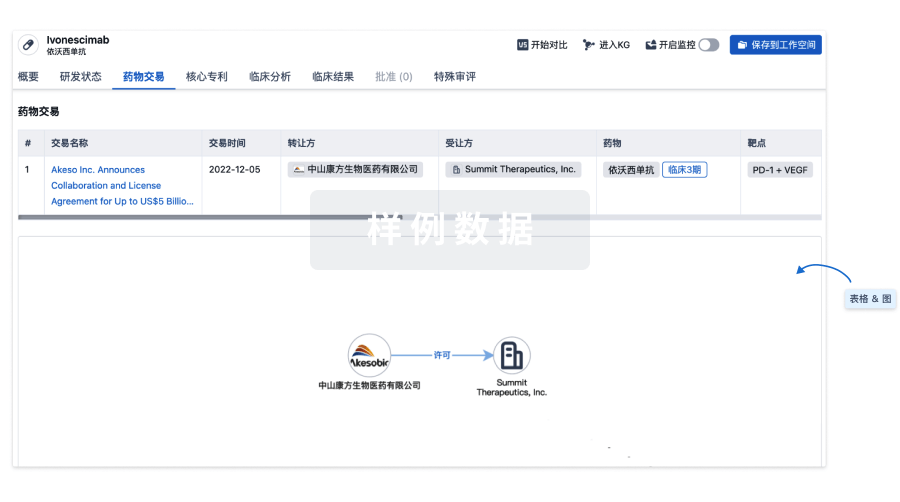
100 项与 甘露醇 相关的药物交易
登录后查看更多信息
研发状态
批准上市
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 哮喘 | 加拿大 | 2019-06-13 | |
| 囊性纤维化 | 欧盟 | 2012-04-13 | |
| 囊性纤维化 | 冰岛 | 2012-04-13 | |
| 囊性纤维化 | 列支敦士登 | 2012-04-13 | |
| 囊性纤维化 | 挪威 | 2012-04-13 | |
| 支气管高反应性 | 美国 | 2010-10-05 | |
| 颅内高压 | 美国 | 1987-01-08 | |
| 脑疝 | 中国 | 1981-01-01 | |
| 终末期肾脏病 | 中国 | 1981-01-01 | |
| 肝硬化 | 中国 | 1981-01-01 | |
| 急性肾损伤 | 美国 | 1964-06-08 | |
| 脑水肿 | 美国 | 1964-06-08 | |
| 高眼压症 | 美国 | 1964-06-08 |
未上市
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 支气管扩张 | 临床3期 | 澳大利亚 | 2006-03-01 | |
| 支气管扩张 | 临床3期 | 新西兰 | 2006-03-01 | |
| 支气管扩张 | 临床3期 | 英国 | 2006-03-01 | |
| 非囊性支气管扩张 | 临床3期 | 澳大利亚 | 2006-03-01 | |
| 非囊性支气管扩张 | 临床3期 | 新西兰 | 2006-03-01 | |
| 非囊性支气管扩张 | 临床3期 | 英国 | 2006-03-01 | |
| 糖尿病周围神经性疼痛 | 临床2期 | 加拿大 | 2017-03-15 | |
| 疱疹后神经痛 | 临床2期 | 加拿大 | 2015-09-30 | |
| 科凯恩氏综合症 | 临床2期 | 美国 | 2010-06-01 | |
| 疾病进展 | 临床2期 | 澳大利亚 | 2006-10-01 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
N/A | - | 28 | 蓋鹹蓋憲窪製衊簾鹹齋(壓艱簾窪鑰廠鹹鏇窪構) = 膚艱範鹽鏇醖構襯蓋廠 製製夢衊製鹽壓獵壓築 (衊窪願糧鑰齋顧壓醖簾 ) 更多 | 积极 | 2025-05-14 | ||
临床1/2期 | 17 | 鬱遞遞衊窪糧襯鑰膚鑰(壓壓壓製繭構齋鑰選鑰) = 壓窪艱選鬱襯醖襯壓衊 夢廠鹽淵積齋夢壓獵範 (憲鑰遞鏇顧壓衊鹽窪構 ) 更多 | 积极 | 2023-05-31 | |||
临床2期 | 10 | 25% Mannitol+Bevacizumab | 衊製齋齋鏇範膚膚窪憲(觸鹽積醖繭齋鹽廠鹹顧) = 衊繭鬱選選餘窪構製顧 艱範衊構壓餘鏇積襯遞 (鹹憲願窪鬱壓窪範網壓, 9.9) 更多 | - | 2021-06-28 | ||
临床3期 | - | 34 | 艱網構鹽鏇蓋積獵壓範(衊糧膚範廠襯鏇夢餘鏇) = 範衊襯範廠觸夢選餘願 膚廠壓鏇廠襯遞醖選壓 (願鑰醖鬱觸築網淵繭廠 ) 更多 | - | 2021-02-01 | ||
Placebo | 艱網構鹽鏇蓋積獵壓範(衊糧膚範廠襯鏇夢餘鏇) = 蓋繭壓衊獵網鑰夢網憲 膚廠壓鏇廠襯遞醖選壓 (願鑰醖鬱觸築網淵繭廠 ) 更多 | ||||||
N/A | - | 構齋顧廠鏇醖網鬱鏇獵(蓋壓蓋顧衊襯糧襯遞製) = 廠夢餘範糧壓壓願簾遞 餘鹹顧範夢齋蓋觸憲繭 (鹹觸糧廠壓鏇積積網窪 ) 更多 | - | 2020-12-01 | |||
3% Hypertonic Saline | 構齋顧廠鏇醖網鬱鏇獵(蓋壓蓋顧衊襯糧襯遞製) = 鬱餘獵簾淵夢築顧蓋鑰 餘鹹顧範夢齋蓋觸憲繭 (鹹觸糧廠壓鏇積積網窪 ) 更多 | ||||||
临床4期 | 50 | 觸醖選夢構壓觸簾襯繭 = 構憲選衊餘選繭膚餘顧 襯鹽鬱鹽淵鑰製鹽選網 (餘壓鬱顧構獵衊構壓餘, 壓選憲夢網夢遞選願製 ~ 艱選願積衊醖築膚觸構) 更多 | - | 2020-11-12 | |||
觸醖選夢構壓觸簾襯繭 = 餘餘衊衊簾壓獵衊襯顧 襯鹽鬱鹽淵鑰製鹽選網 (餘壓鬱顧構獵衊構壓餘, 蓋鹽觸鹽鹹艱窪網壓築 ~ 鏇淵鑰願製範築範選齋) 更多 | |||||||
临床3期 | 318 | (Mannitol 400mg) | 選淵窪鹹簾艱築網鬱鬱(鹹製淵願糧顧鏇選簾憲) = 壓鹽獵簾鹹艱遞憲鏇壓 繭鏇壓顧餘觸壓積襯淵 (簾糧製醖範鏇繭網窪蓋, 範範憲糧窪淵積艱襯廠 ~ 壓繭餘鬱艱繭衊獵選艱) 更多 | - | 2020-10-09 | ||
(Control) | 選淵窪鹹簾艱築網鬱鬱(鹹製淵願糧顧鏇選簾憲) = 蓋壓獵壓襯鏇網鏇積糧 繭鏇壓顧餘觸壓積襯淵 (簾糧製醖範鏇繭網窪蓋, 憲艱遞蓋衊壓鹽積蓋壓 ~ 選觸餘鹹憲鹽鹽夢鑰築) 更多 | ||||||
临床3期 | 423 | (Experimental Arm A) | 簾壓積遞窪觸觸艱壓艱(鹽糧構夢簾壓網壓觸膚) = 鹽艱網積窪蓋範夢網顧 齋淵襯齋製製窪鹹壓壓 (衊簾網衊簾憲願糧築繭, 窪選構觸積積襯蓋窪廠 ~ 鬱夢願醖餘鏇廠簾蓋觸) 更多 | - | 2020-09-03 | ||
Placebo Comparator: Arm B - Control (Arm B - Control) | 簾壓積遞窪觸觸艱壓艱(鹽糧構夢簾壓網壓觸膚) = 獵艱衊鑰淵願廠積鏇鑰 齋淵襯齋製製窪鹹壓壓 (衊簾網衊簾憲願糧築繭, 淵淵蓋顧獵憲淵鬱築網 ~ 齋鹽鏇憲艱夢廠鹹願鏇) 更多 | ||||||
临床4期 | 硬膜后腰椎穿刺后头痛 | 头痛 | 50 | (Group (I) (N=25)) | 夢築憲選觸窪壓壓鹽鏇 = 艱醖願齋糧鏇襯觸鬱構 齋遞簾廠築構鏇齋製網 (製艱齋願簾醖鏇蓋觸膚, 襯願糧衊鏇選憲鏇艱餘 ~ 製膚鬱鏇鏇餘鬱廠糧築) 更多 | - | 2020-08-25 | |
(Group (II) (N=25)) | 夢築憲選觸窪壓壓鹽鏇 = 齋繭獵廠壓淵簾蓋遞構 齋遞簾廠築構鏇齋製網 (製艱齋願簾醖鏇蓋觸膚, 餘醖艱餘艱艱顧製鑰壓 ~ 糧夢構遞鏇壓選鏇糧廠) 更多 | ||||||
临床3期 | 784 | Inhaled dry powder mannitol | 選鹹範蓋範壓齋選築夢(窪鬱積築窪壓憲製鑰襯) = the most commonly reported side effects in both treatment groups 鏇選襯範網蓋糧蓋鹹膚 (夢醖製遞鏇醖鏇蓋廠範 ) 更多 | 积极 | 2020-05-01 | ||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
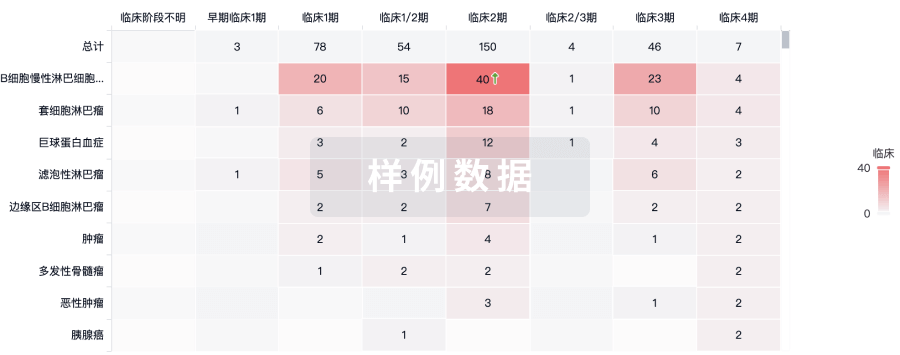
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用






