预约演示
更新于:2025-05-07
Recurrent Transformed B-Cell Non-Hodgkin Lymphoma
复发性转化型B细胞非霍奇金淋巴瘤
更新于:2025-05-07
基本信息
别名 Recurrent Transformed B-Cell Non-Hodgkin Lymphoma、Recurrent Transformed Indolent B-Cell Non-Hodgkin Lymphoma |
简介 The reemergence of B-cell non-Hodgkin lymphoma transformed after a period of remission. |
关联
16
项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的药物作用机制 CD20抑制剂 [+1] |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2023-05-19 |
作用机制 PI3Kα抑制剂 [+1] |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2017-09-14 |
19
项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的临床试验CTIS2024-513098-31-00
An Open Label, Phase 2 Clinical Trial of MEN1703 as Monotherapy and in Combination with Glofitamab in Patients with Relapsed or Refractory Aggressive B-cell Non-Hodgkin Lymphoma (JASPIS-01) - JASPIS-01
开始日期2025-03-11 |
申办/合作机构 |
NCT06458439
Phase IIa Trial to Evaluate Epcoritamab Administered Before and After CAR-T Cell Therapy in Patients With Relapsed or Refractory Large B-cell Lymphomas
This study investigates the feasibility and efficacy of epcoritamab treatment before CAR T cells. This study also investigates if, when patients have residual lymphoma after CAR T cells, epcoritamab can help to effectively treat that lymphoma.
开始日期2024-09-24 |
申办/合作机构 |
NCT06209619
Early, Risk Adapted CC-99282 + Rituximab Post CAR T-Cell Therapy for Non-Hodgkin's Lymphoma
This phase I trial tests the safety, side effects and best dose of CC-99282 with rituximab for the treatment of patients who have received chimeric antigen receptor (CAR) T cell therapy for non-Hodgkins lymphoma and in whom have had a sub-optimal response early on to CAR T-cell therapy. Immunotherapy with CC-99282 may induce changes in the body's immune system and may interfere with the ability of tumor cells to grow and spread. Rituximab is a monoclonal antibody. It binds to a protein called CD20, which is found on B cells (a type of white blood cell) and some types of cancer cells. This may help the immune system kill cancer cells. Giving CC-99282 with rituximab may be a safe and effective treatment option for patients who have received CAR-T cell therapy for relapsed or refractory non-Hodgkin's lymphoma.
开始日期2024-01-29 |
100 项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的临床结果
登录后查看更多信息
100 项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的转化医学
登录后查看更多信息
0 项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的专利(医药)
登录后查看更多信息
35
项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的文献(医药)2025-02-01·American Journal of Hematology
Outcomes of CD19 CAR T in Transformed Indolent Lymphoma Compared to De Novo Aggressive Large B‐Cell Lymphoma
Article
作者: Gaulin, Charles ; Thiruvengadam, Swetha Kambhampati ; Bezerra, Evandro ; Merryman, Reid ; Bailey, Neil ; Patel, Krish ; Falade, Ayo ; Habib, Alma ; Wang, Yan ; Bailey, Megumi ; Voorhees, Timothy ; Forman, Stephen J. ; Budde, Lihua E. ; Seshadri, Madhav R. ; Kittai, Adam S. ; Ayers, Amy A. ; Brown, Annette ; Palmer, Joycelynne ; Andreadis, Charalambos B. ; Jacobson, Caron ; Nastoupil, Loretta
2023-11-01·Annals of Hematology
Successful treatment of relapsed/refractory transformed aggressive B-cell lymphoma with polatuzumab vedotin combined with bendamustine and rituximab followed by non-myeloablative related HLA-haploidentical stem cell transplantation
Letter
作者: Kosugi, Shigeki ; Inoue, Yasuyuki ; Kanno, Masatoshi
2022-03-01·Seminars in Nuclear Medicine2区 · 医学
Dosimetric Approaches for Radioimmunotherapy of Non-Hodgkin Lymphoma in Myeloablative Setting
2区 · 医学
Review
作者: Ferrari, Mahila Esmeralda ; Wahl, Richard ; Paganelli, Giovanni ; Cicone, Francesco ; Cremonesi, Marta ; Sarnelli, Anna ; Belli, Maria Luisa ; Guidi, Claretta
8
项与 复发性转化型B细胞非霍奇金淋巴瘤 相关的新闻(医药)2024-09-19
·医药观澜
▎药明康德内容团队报道
9月18日,中国国家药监局药品审评中心(CDE)网站最新公示,和记黄埔医药的化学1类新药HMPL-760胶囊获批一项新的临床试验默示许可,适应症为联合R-GemOx(利妥昔单抗+吉西他滨+奥沙利铂)治疗复发/难治弥漫大B细胞淋巴瘤(R/R DLBCL)。公开资料显示,HMPL-760是一款第三代非共价BTK抑制剂,是和黄医药第十一个进入临床开发的潜在创新抗肿瘤候选药物。
图片来源:CDE官网
BTK是B细胞受体信号通路的关键组成部分,并在各种淋巴瘤的细胞增殖及存活中起重要调节作用。B细胞受体信号的异常激活与B细胞血液癌症的发生密切相关,B细胞血液癌症占所有非霍奇金淋巴瘤病例约85%。BTK是治疗某些血液癌症已确认的药物靶点,但BTK的C481S突变是一代和二代BTK抑制剂已知的耐药机制。
根据和黄医药公开信息,作为一种高选择性、非共价、三代BTK抑制剂,HMPL-760可针对野生型及C481S突变激酶,临床前数据表明,与一代BTK抑制剂相比,HMPL-760具更高的靶点特异性和有效性。BTK的C481S突变在对某些BTK抑制剂产生耐药性中扮演重要角色。
HMPL-760胶囊此前已经在中国获批临床试验,拟治疗B细胞非霍奇金淋巴瘤。根据中国药物临床试验登记与信息公示平台官网,一项评价HMPL-760治疗复发/难治B细胞非霍奇金淋巴瘤患者的安全性、药代动力学及初步疗效的多中心、开放性、1期研究正在进行中。
弥漫性大B细胞淋巴瘤是来源于成熟B细胞的侵袭性肿瘤,是最常见的非霍奇金淋巴瘤类型,约占全部非霍奇金淋巴瘤的25%~50%。此次HMPL-760胶囊再次获批临床,意味着这款在研新药将在复发/难治弥漫大B细胞淋巴瘤患者群体中开展临床研究。
参考资料:
[1] 中国国家药监局药品审评中心(CDE)网站.Retrieved Sep 18,2024, From https://www.cde.org.cn/main/xxgk/listpage/4b5255eb0a84820cef4ca3e8b6bbe20c
[2]和黄医药在中国启动BTK抑制剂HMPL-760治疗 经治B细胞非霍奇金淋巴瘤患者的I期临床试验 .Retrieved Sep 18,2024, From https://www.hutch-med.com/wp-content/uploads/2022/01/a220110_HKEX_C.pdf
本文由药明康德内容团队根据公开资料整理编辑,欢迎个人转发至朋友圈。转发授权或其他合作需求,请联系wuxi_media@wuxiapptec.com。
免责声明:药明康德内容团队专注介绍全球生物医药健康研究进展。本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。
临床1期临床申请申请上市ASH会议
2024-07-23
·益科思特
2024年7月22日,益科思特(北京)医药科技发展有限公司自主研发的双特异性抗体YK012(受理号:CXSL2400312),正式获得国家药品监督管理局药品审评中心的药物临床试验(IND)批准,用于治疗B细胞急性淋巴细胞白血病(B-ALL)。本次获批开展一项评价YK012治疗B细胞急性淋巴细胞白血病的安全性、耐受性、药代动力学特征和初步抗肿瘤疗效的多中心、开放性、Ib/Ⅱ期临床研究。
YK012是一款靶向CD19/CD3的创新型双特异性抗体,是继2022年获批 “复发/难治B细胞非霍奇金淋巴瘤”适应症后扩展的第二个适应症,是益科思特获得的第三个IND批准,标志着益科思特的创新型双特异性抗体的研发技术稳步走向成熟,逐渐经历临床研究的考验,有望最终转化为产品。
益科思特YK012是采用创新型免疫双特异性抗体质量源于设计(Quality by Design )的理念,基于益科思特独具优势特色的FIST平台进行开发的靶向CD19/CD3的双特异性抗体,是I类创新药物,定位为同类最佳(Best in class)。YK012与安进公司的贝林托欧单抗具有相似作用机理,但在分子结构、半衰期、生产水平以及毒性方面均显著优于贝林托欧单抗。YK012的NHL的I期临床研究已有15例患者接受治疗。截止当前,药物的安全性和耐受性良好,尽管还在剂量爬坡阶段,但已经观察到一些病例的肿瘤缩小现象。特别是在肿瘤负荷较重的患者中,通过多次给药,仍然可以展现疗效。综合临床前和临床阶段的研究结果表明,YK012可能具有更好的临床疗效和安全性,有望为难治和/或复发的ALL、NHL和自身免疫性疾病提供更好的选择。
益科思特(北京)医药科技发展有限公司由来自著名美国制药企业回国人员袁清安博士和孟庆武先生共同创立,在中美两地设有研发中心。公司充分利用中美两国的信息优势、技术优势和人才优势,致力于全球创新药物的研发,针对血癌、多发性骨髓瘤、三阴乳腺癌、肝癌和自身免疫性疾病等创新型双特异抗体药物的开发,多个项目具有长效、低毒、高产的技术创新特点,均为国际对标产品的更新换代产品。公司拥有完备的技术团队和管理团队,具备从初步构想到规模化生产的全链条技术平台。益科思特凭借其创新的双抗技术平台和高效的研发团队,已获得多项荣誉和资助。益科思特创新药物的研发均为全球布局,首个双特异抗体产品已取得国内外专利证书,并已获得国家药品监督管理局临床批件(编号2022LP00654、2024LP01666),NHL的I期临床进行中,ALL适应症的Ib/II期启动在即,治疗两个自身免疫性疾病的Pre-IND已经递交。第二个双特异抗体产品已取得相关专利证书,并已获得国家药品监督管理局临床批件(编号2024LP008),6月份第1例患者已入组。第三个产品已完成3批中试生产,预计2024年底申报新药临床。其他管线产品包括全球创新的靶点双抗药物研发均在有序推进中。
目前,公司正积极推进多个临床项目,并与国际知名机构进行商业合作洽谈,未来有望在全球市场上取得更大的突破。
益科思特秉承行医治,行拯救为医药人的使命和责任,不断推出1.1类新药进入临床研究,力争早日获批新药产品进入国际国内市场,使患者获益,拥抱健康。
临床申请临床1期
2024-01-10
·医药观澜
▎药明康德内容团队报道北京时间1月10日,君实生物首席执行官(CEO)李宁博士在第42届摩根大通医疗健康年会(J.P. Morgan Healthcare Conference,JPM)现场发表了演讲。在报告中,李宁博士介绍了君实生物的近期业务进展、技术平台和产品管线以及公司的国际化布局和商业化能力。(扫描文末二维码,可获得包括君实生物在内的近50家生物医药公司的JPM大会演讲PPT)。君实生物致力于创新疗法的发现、开发和商业化。根据报告,目前该公司已建立包含50+潜在候选药物的产品管线,其中4款产品已商业化,30款产品处于临床开发阶段。药物类型包括单抗、双抗、抗体偶联药物(ADC)、融合蛋白、小分子药物、核酸类药物,适应症涵盖肿瘤、自身免疫系统疾病、慢性代谢类疾病、神经系统疾病、感染类疾病等治疗领域。图片来源:君实生物2024JPM演讲报告截图四款产品实现商业化君实生物的核心产品抗PD-1单抗特瑞普利单抗已在中国获批7项适应症,涉及黑色素瘤、鼻咽癌、尿路上皮癌、食管鳞癌、非小细胞肺癌等癌种。同时,该药还有3项新适应症上市申请已获得NMPA受理。在国际化布局方面,特瑞普利单抗已获得美国FDA批准用于治疗鼻咽癌,其在黏膜黑色素瘤、鼻咽癌、软组织肉瘤、食管癌、小细胞肺癌领域也获得FDA授予2项突破性疗法认定、1项快速通道资格、1项优先审评资格和5项孤儿药资格。此外,欧洲药品管理局(EMA)、英国药品和保健品管理局(MHRA)、澳大利亚药品管理局(TGA)也已受理了特瑞普利单抗的上市申请。目前,通过权益合作,特瑞普利单抗的国际商业化网络已覆盖超过50个国家。君实生物与迈威生物合作开发的阿达木单抗生物类似药已获得NMPA批准8项适应症,用于治疗类风湿关节炎、强直性脊柱炎、银屑病、克罗恩病、葡萄膜炎、多关节型幼年特发性关节炎、儿童斑块状银屑病、儿童克罗恩病。此外,君实生物还有两款抗感染药物获批。图片来源:君实生物2024JPM演讲报告截图48款产品处于研发阶段根据报告,目前君实生物有48款产品处于研发阶段,包括18款处于临床前研究阶段的产品、26款处于1/2期临床阶段的产品以及4款处于3期临床阶段的产品。在本次报告中,李宁博士重点介绍了君实生物肿瘤领域产品管线的一些进展。对于特瑞普利单抗,君实生物目前仍在探索其作为单药和联合疗法治疗更多适应症的潜力,特别是针对早期肿瘤患者术后辅助/围手术期适应症,多个3期临床试验即将完成。与此同时,君实生物还建立了丰富的临床阶段肿瘤药物管线,其中包括:tifcemalimab(TAB004/JS004),一款重组人源化抗BTLA(B和T淋巴细胞衰减因子)单克隆抗体,正在中国和美国开展联合特瑞普利单抗治疗局限期小细胞肺癌的全球多中心3期临床,同时也在中国开展治疗经典型霍奇金淋巴瘤的3期临床;JS203,一款重组人源化抗CD20和CD3双特异性抗体,拟开发用于治疗复发/难治B细胞非霍奇金淋巴瘤,目前正在中国开展1/2期临床试验;JS207,一款PD-1 x VEGF双特异性抗体,已在中国获批针对晚期恶性肿瘤的临床试验;JS107,一款靶向肿瘤相关蛋白Claudin18.2的抗体偶联药物(ADC),拟开发用于治疗胃癌和胰腺癌等晚期恶性肿瘤,目前正在中国开展1/2期临床试验;JS105,君实生物与与润佳医药合作开发的一款PI3K-α口服小分子抑制剂,主要用于治疗内分泌方案治疗中或治疗后出现疾病进展的HR阳性、HER-2阴性、PIK3CA突变的晚期乳腺癌女性(绝经后)和男性患者,目前正在中国和美国开展临床试验。此外,君实生物也在本次大会上介绍了该公司在非肿瘤领域的一些产品进展。例如,在慢性代谢类疾病领域:该公司开发的抗PCSK9单抗昂戈瑞西单抗的上市申请已于2023年4月获得NMPA受理,用于治疗原发性高胆固醇血症(包括杂合子型家族性和非家族性)和混合型血脂异常以及成人或12岁以上青少年的纯合子型家族性高胆固醇血症;同时,君实生物还与润佳医药共同研发了一款靶向ANGPTL3信使RNA的siRNA药物JS401,该药已进入临床阶段,拟主要用于治疗高脂血症等。在自免和神经系统疾病的治疗领域,君实生物也开发了多款产品。其中:抗IL-17A单抗JS005拟用于治疗银屑病、脊柱炎,目前正在开展针对中重度斑块状银屑病的3期注册研究,并启动了针对强直性脊柱炎的注册临床试验沟通交流;抗CGRP单抗JS010拟用于成人偏头痛的预防性治疗,目前正在中国开展临床试验。第42届摩根大通医疗健康年会正在进行中。我们将会持续跟踪本届JPM大会进展,为大家分享来自更多中国创新药公司的最新进展和动态。扫描下方二维码,您可以获得近50家生物医药公司的2024年JPM大会演讲PPT。参考资料:[1]君实生物2024年JPM大会演讲报告本文由药明康德内容团队根据公开资料整理编辑,欢迎个人转发至朋友圈。转发授权请在「医药观澜」微信公众号留言联系我们。其他合作需求,请联系wuxi_media@wuxiapptec.com。免责声明:药明康德内容团队专注介绍全球生物医药健康研究进展。本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。
优先审批抗体药物偶联物临床3期孤儿药突破性疗法
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
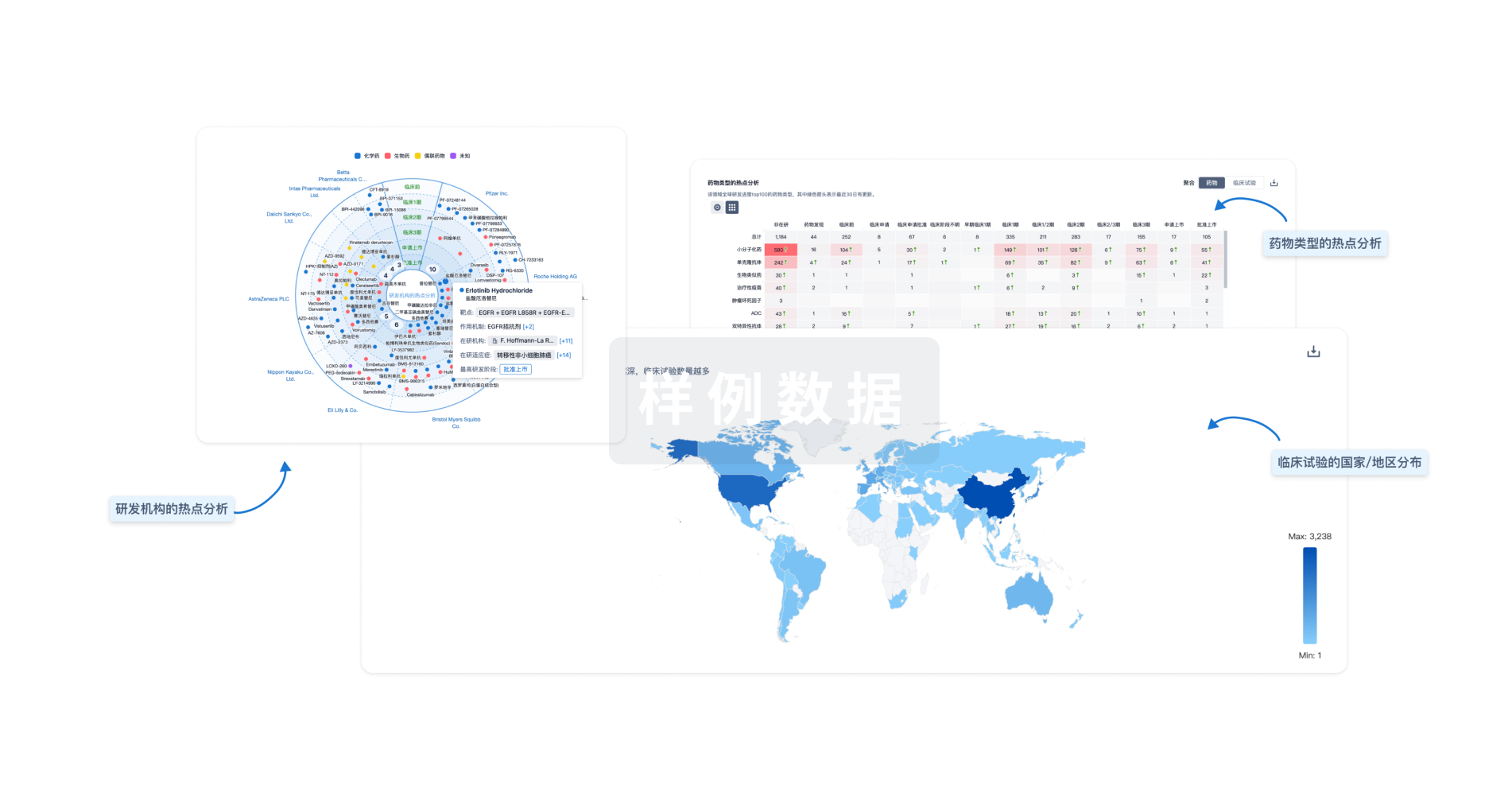
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用




