预约演示
更新于:2025-05-07
Biliary Tract Neoplasms
胆道癌
更新于:2025-05-07
基本信息
别名 BILIARY NEOPLASIA、Biliary Tract Cancer、Biliary Tract Cancers + [59] |
简介 Tumors or cancer in the BILIARY TRACT including the BILE DUCTS and the GALLBLADDER. |
关联
444
项与 胆道癌 相关的药物作用机制 TOP1抑制剂 [+1] |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期2024-12-27 |
作用机制 TOP1抑制剂 [+1] |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2024-11-22 |
靶点 |
作用机制 HER2拮抗剂 [+1] |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-11-20 |
2,490
项与 胆道癌 相关的临床试验NCT05091593
A Hybrid Type I Randomized Effectiveness-Implementation Trial of Remote Treatment of Depression in Rural Community Cancer Centers
In an effort to reduce rural-urban disparities and improve the quality of cancer care for these patients, the objectives of this study will be to: (1) adapt the intervention to maximize effectiveness for rural, low-income patients, (2) test the effectiveness of the adapted intervention, and (3) prepare for implementation of the intervention in rural, low-income communities.
开始日期2026-06-01 |
申办/合作机构 |
JPRN-UMIN000053251
Observational study of chemotherapy for unresectable intrahepatic cholangiocarcinoma - Observational study of chemotherapy for unresectable intrahepatic cholangiocarcinoma
开始日期2025-12-30 |
申办/合作机构 |
NCT05601206
Collaborative Care Intervention for Cancer Patients and Their Family Caregivers -LITE
To test the efficacy of a web-based stepped collaborative care intervention to reduce symptoms of depression, pain, and fatigue and improve health-related quality of life (HRQL) in advanced cancer patients and to reduce stress and depression, and fewer CVD risk factors in caregivers.
开始日期2025-11-14 |
申办/合作机构 |
100 项与 胆道癌 相关的临床结果
登录后查看更多信息
100 项与 胆道癌 相关的转化医学
登录后查看更多信息
0 项与 胆道癌 相关的专利(医药)
登录后查看更多信息
44,643
项与 胆道癌 相关的文献(医药)2025-12-31·Journal of Obstetrics and Gynaecology
The long noncoding RNA CCDC144NL-AS1: prognosis significance and potential biological functions in cervical carcinoma
Article
作者: Hu, Xuemei ; Guo, Hongyu ; Wang, Yulong ; Guo, Yuzhen
2025-12-31·International Journal of Hyperthermia
Outcomes of ultrasound-guided percutaneous ablation of >5
versus
≤ 5 colorectal liver metastases: a propensity score matching study
Article
作者: Zhou, Jingwen ; Chen, Yao ; Wang, Yimin ; Cui, Rui ; Liu, Guangjian ; Qin, Si
2025-12-31·Human Vaccines & Immunotherapeutics
Immunotherapy-induced microsatellite instability status shift in recurrent perihilar cholangiocarcinoma: A case report
Article
作者: Deng, Tan ; Yu, Hailing ; Liu, Hongbing
2,999
项与 胆道癌 相关的新闻(医药)2025-05-04
往期推荐产品动态依沃西一线治疗NSCLC获批上市(全球首个对比帕博利珠单抗获显著阳性结果的III期研究)产品动态美国重磅上市!派安普利单抗2个适应症获FDA批准上市,用于晚期鼻咽癌治疗产品动态康方生物爱达罗®(依若奇,IL-12/IL-23)治疗中重度斑块状银屑病适应症获批上市临床进展首个自研ADC澳洲临床入组!康方生物IO 2.0+ADC战略再进一步临床进展非肿瘤首个双抗|康方生物全球首创IL-4Rα/ST2(AK139)IND获受理,剑指呼吸系统及皮肤疾病领域临床进展依沃西方案对比替雷利珠方案1L治疗sq-NSCLC的Ⅲ期临床完成患者入组临床进展康方生物古莫奇(IL-17)单抗新药上市申请获NMPA受理数据发布荣登Nature Medicine!卡度尼利方案1L治疗胃癌Ⅲ期研究结果全文发表产品动态康方生物卡度尼利、依沃西纳入2024年国家医保目录临床进展头对头度伐利尤单抗方案,依沃西方案一线治疗胆道肿瘤III期临床完成首例患者入组临床进展全球首个CD47单抗实体瘤III期临床首例入组:依沃西联合莱法利一线治疗HNSCC(对比帕博利珠单抗)数据发布卡度尼利一线宫颈癌III期研究成果荣登《Nature Reviews Clinical Oncology》(影响因子高81.1)数据发布IGCS 2024 LBA & 《柳叶刀》主刊,卡度尼利1L宫颈癌III期研究PFS和OS双阳性结果重磅发布产品动态一线胃癌全人群获批!康方生物卡度尼利获批第二个适应症产品动态获FDA快速通道资格!依沃西国际多中心III期研究HARMONi完成入组,2L+EGFRm NSCLC数据发布全球首个对比帕博利珠单抗取得显著阳性结果的随机对照大III期研究——依沃西HARMONi-2重磅研究成果在WCLC发表临床进展康方生物卡度尼利联合方案治疗uHCC的III期临床研究完成首例患者入组临床进展针对PD-1/L1治疗进展晚期胃癌,卡度尼利+普络西(VEGFR-2)联合疗法Ⅲ期临床完成首例入组数据发布ASCO Oral & JAMA主刊丨Ⅲ期HARMONi-A研究重磅公布,依沃西疗法有望改变EGFR-TKI进展肺癌全球治疗标准临床进展史无前例!康方依沃西单药对比帕博利珠1L治疗PD-L1阳性NSCLC的III期临床获决定性胜出阳性结果产品动态康方生物双抗卡度尼利一线治疗晚期宫颈癌全人群的sNDA获CDE受理临床进展国际多中心注册性III期研究HARMONi-3中国启动:依沃西单抗联合化疗对比帕博利珠单抗联合化疗1L治疗sq-NSCLC产品动态高达50亿美金!康方生物与Summit就PD-1/VEGF双抗依沃西达成合作和许可协议产品动态全球首个肿瘤免疫治疗双抗——开坦尼®(PD-1/CTLA-4双抗,卡度尼利)获批上市
临床3期ASCO会议抗体药物偶联物上市批准临床结果
2025-04-30
·药通社
最近,由中国药科大学药学院尤启东教授和王磊教授课题组,以及海军军医大学基础医学院卢小玲教授,合作在知名学术期刊The Innovation(IF: 33.2)上发表了题为“Global first-in-class drugs approved in 2023-2024: Breakthroughs and insights” 的综述文章,阐述了2023-2024年间全球首创性小分子药物的突破与进展。本期公众号对该文进行了整理,供业内同行参考。首创新药(First-in-class, FIC)被视为新药研发的主要驱动力,具有创新靶点与作用机制。FIC药物在新药中的占比为学术界和制药研究提供了基础性指导。从全球视野来看,2023至2024年间共有81款FIC药物获批。其中小分子药物占比更高(51.9%),体现了新化学实体的发现成果;而以抗体类似物为主的大分子药物(48.1%)则随着新型生物技术的涌现呈现增长趋势。就适应症分布而言,肿瘤领域仍居首位(22.0%),共有18款FIC疗法获批,反映出该领域迫切的临床需求。在基于作用机制的创新方面,以各类酶为靶点的FIC药物最为常见(32.1%),共涉及26个新靶点发现。本综述将系统阐述2023-2024年间获批FIC药物的表现与特征,为全球新药研发提供突破性进展与战略洞见。引言药物研发领域的核心关注点在于首创新药(First-in-Class, FIC)的获批。美国食品药品监督管理局(FDA)将FIC药物定义为:通过作用于全新靶点与机制、具有区别于现有疗法作用机制的新获批药物,或针对未满足临床需求提供首次治疗选择的药物[1]。成功的FIC药物往往具有革命性意义,不仅能带来丰厚经济回报,更能为药物研发开辟新方向[2,3]。2024年获批的靶向claudin 18异构体2的单克隆抗体zolbetuximab-clzb(Vyloy)即属此类FIC药物[4,5]。该药物的获批同时验证了claudin 18.2靶向治疗的可行性,推动了针对该靶点的双特异性抗体、抗体偶联药物(ADC)等疗法的研发[6]。FIC药物的研发具有挑战性高、周期长、资源密集及风险大等特点[7,8]。通常这类药物需作用于新型候选靶点,并通过合理的药物分子设计实现对特定疾病的治疗作用,这使得新靶点的发现与验证至关重要[9]。该研发过程通常由临床数据或生物学研究驱动[10],其中新靶点的发现是FIC药物研发的限速步骤[11]。值得注意的是,FIC药物的靶点验证贯穿整个药物开发流程——从早期实验室研究阶段到上市后应用,持续评估药物的安全性、有效性以及新靶点与疾病的关联性[12]。另一大挑战在于针对新靶点的候选药物设计,该过程至少涉及发现、优化与验证三个阶段,往往耗时数年[13]。理解分子、靶点与疾病间的相互作用关系是开发FIC药物的关键。因此,既往报道的FIC药物案例对指导未来药物设计具有重要参考价值。2023至2024年间,上市药物数量取得显著进展,反映出对生物机制与疾病发病机理的认知持续深化。本研究汇总了中国国家药品监督管理局(NMPA)、美国食品药品监督管理局(FDA)、日本医药品医疗器械综合机构(PMDA)及欧盟欧洲药品管理局(EMA)四大官方药监机构的新药审批数据。基于FDA对创新药物的界定标准[14],我们从获批药物中筛选出首次在特定治疗领域获批的新分子实体(novel drugs)。统计显示,2023年1月至2024年10月期间共有1,035种药物上市,其中337种创新药物获得四大机构批准。在这337种创新药物中,81种首创新药(FIC)因其创新作用机制或新靶标而尤为突出。本综述重点分析了FIC药物(包括小分子FIC药物与大分子FIC药物)及其适应症与疾病靶点,列举了具有重大创新价值与临床意义的代表性FIC药物并阐释其作用机制与适应症。此外,我们还探讨了FIC药物研发趋势,并为未来FIC药物设计提出了建议。FIC药物研发推动新药获批鉴于FIC新药具有新颖的作用机制或靶点,其功能属性对于确立其在该类药物中的开创性地位和领先优势至关重要[15]。因此,通过对FIC靶点与机制的持续医学研发,有望开发出疗效更优的创新药物[7]。近年来,未满足的临床需求与个性化用药期待共同推动了对更高疗效及安全性的FIC药物研究[1]。从2023至2024年全球药物获批情况来看(图1),创新药物的地域分布呈现差异化特征。据我们统计,2023年1月至2024年10月期间共有1,035种新药获批,其中426种为创新药物。由于部分创新药物在多地获批,实际创新药物数量为337种,包含81种FIC药物(占比24.0%)(图1A;表1)[3,16,17]。 在美国,根据《2023年新药治疗审批报告》(Novel Drug Approvals for 2023 | FDA)、《2024年新药治疗审批报告》以及《2023年首仿药审批报告》(2023 First Generic Drug Approvals | FDA)的数据,美国食品药品监督管理局(FDA)全年共批准315个药物,其中创新药117个(占比37.1%),改良药/仿制药/生物类似药198个(占比62.9%)。在117个创新药中[18],93个由FDA药品评价与研究中心(CDER)批准,生物制品评价与研究中心(CBER)另批准24个创新治疗产品。其中包含51个首创新药(FIC)(图1B)。117个创新药与51个FIC药物的获批彰显了2023-2024年美国医药产业的重大成就。中国国家药品监督管理局(NMPA)同期批准352个药物,包含151个创新药(42.9%)、53个首仿药(15.1%)及148个改良药(42.0%)[16],其中22个为FIC药物(图1B)。基于审批数量提升与质量优化的双重突破,中国医药产业在2023-2024年取得显著进展。日本医药品医疗器械综合机构(PMDA)共批准223个药物,包括78个创新药(35.0%,含16个FIC药物)、142个改良药(63.7%)及3个生物类似药(1.3%)(图1B),其中近半数(49.8%)为采用新剂量的药物。欧盟药品管理局(EMA)批准的创新药数量(80个,含19个FIC药物,占比55.2%;图1B)显著超过仿制药/混合药/其他类型药物(65个,44.8%)。图1. 全球批准的新药、首创新药与其他药物的数量及占比情况。(A)新药、首创新药与改良型/混合型/仿制药/生物类似药的总体概况。由于部分新药在多个地区获批,实际新药数量为337个而非426个。(B)新药与改良型/混合型/仿制药/生物类似药的数量及占比,以及首创新药数量。中国将获批药物分为新药、改良型药物和首仿药物;美国分为新药、首仿药物、生物类似药和改良型药物;日本主要分为新药、生物类似药和改良型药物;欧盟则分为新药、新适应症药物、仿制药、生物类似药、混合型药物和其他药物。绿色、蓝色、青色和橙色分别对应中国、美国、日本和欧盟批准的药物。表1. 2023年1月~2024年10月期间全球获批的FIC新药↓扫码加入药通社交流群 ↓原始创新研究推动小分子首创新药的发展低分子量的小分子药物在靶点亲和力与选择性[20]、药代动力学特性[21]以及患者用药依从性[21]等方面具有独特优势[19]。根据来源差异,小分子药物可分为合成小分子药物、天然产物/衍生物、内源性物质/衍生物、核苷/氨基酸/葡萄糖衍生物等类别。2023至2024年间,共有173种新型小分子药物获批上市,其中42种首创新药(FIC)属于小分子药物。图3展示了这42种FIC小分子药物的化学结构。无论是新型小分子药物还是FIC药物,人工设计合成的合成小分子药物均占据最大比例(76.4%)。天然产物(6.3%)与内源性物质(8.6%)同样是FIC药物研发的重要来源,部分生物大分子的小分子单体(8.6%)则推动了包括葡萄糖、氨基酸及核苷衍生物在内的两类FIC小分子药物的开发(图2)。统计数据显示,多数药物是通过理性药物设计与分子筛选技术发现的。图2. 新型小分子药物与首创新分子药物的比例及分类。环形图展示了新型小分子药物的比例与分类,不同半径的饼图则呈现首创新分子药物的比例与分类。小分子药物主要包括合成小分子药物、内源性物质/衍生物、核苷/氨基酸/葡萄糖衍生物以及天然产物/衍生物。在42种首创新分子实体(FIC)小分子药物中(图3),吲哚类药物iptacopan(Fabhalta)是一种FIC补体因子B抑制剂[22],也是首个获批用于治疗阵发性睡眠性血红蛋白尿症(PNH)成人口服单药疗法[23]。针对PNH的治疗,C5抑制剂(如eculizumab单抗和ravulizumab单抗)虽代表先进治疗策略,但受限于患者对eculizumab单抗的不完全应答——这源于骨髓红系造血反应不足、残留血管内溶血及反复发作的血管外溶血(EVH)[24]。作为近端补体通路抑制剂,iptacopan在C3b介导的血管内溶血和终末补体通路介导的EVH中均展现出显著疗效[25]。相较于既往静脉注射的eculizumab单抗/ravulizumab单抗或皮下注射的pegcetacoplan,该药物突破了PNH患者持续性溶血性贫血的治疗困境,提供了口服给药选择[22];其治疗成本亦低于部分抗C5治疗方案[25],有效减轻患者经济负担。2024年获批的FIC因子D抑制剂danicopan(Voydeya)与iptacopan适应症相同,需特别指出的是,因子D位于iptacopan作用靶点因子B的上游[26]。不同于iptacopan,danicopan作为氨基吡啶衍生物[27],经FDA批准用于PNH成人患者EVH的C5靶向抗体附加治疗。与C5靶向抗体单药治疗相比,danicopan联合C5靶向抗体可有效控制EVH,并拓宽补体通路的治疗靶点覆盖范围[28,29]。图3. 42种FIC小分子药物的化学结构杂环化合物futibatinib(Lytgobi)是一种首创性FIC共价成纤维细胞生长因子受体(FGFR)激酶抑制剂[30,31],由日本医药品医疗器械综合机构(PMDA)批准用于治疗癌症化疗后进展的不可切除性FGFR2融合基因阳性胆道癌。FGFR信号通路与细胞增殖、凋亡、迁移及分化密切相关,抑制该通路已成为癌症治疗的有效策略[32]。该药物作为首个被发现可不可逆结合FGFR1-4的共价FGFR抑制剂[32],已针对多种癌症类型进入临床开发阶段[33]。值得注意的是,尽管目前有多种可逆性FGFR抑制剂处于研究阶段,但均已观察到获得性耐药现象[33-35]。Futibatinib凭借其共价不可逆抑制机制及较低的获得性耐药易感性,于2023年脱颖而出获批上市[33]。除对胆道癌的疗效外,该药物还对具有10种不同类型FGFR1-4异常的7种其他肿瘤类型显示治疗作用[33],因此有望拓展至更多疾病的治疗领域。在源自天然产物、内源性物质或某些生物大分子小单体的FIC小分子药物中,桦木三萜(Filsuvez)[36]——其活性成分属于天然产物[37]——已获FDA批准用于治疗6个月及以上儿童及成人患者的营养不良型和大疱性交界性表皮松解症(EB)相关创面。FDA还批准了一线治疗药物palovarotene(Sohonos)[38],这是一种二苯乙烯类化合物[39],用于治疗进行性骨化性纤维发育不良(FOP)的成人和儿童患者(女性≥8岁,男性≥10岁),以降低新发异位骨化体积。FOP的发病机制涉及激活素A受体I型(ACVR1)/激活素样激酶2(ALK2)基因的功能获得性突变[40]。激活素A与突变型ACVR1结合后,可激活下游SMAD家族成员1/5/8(SMAD1/5/8)信号通路,进而诱发软骨形成[41,42]。该药物通过靶向视黄酸受体γ有效阻断软骨形成过程,从而抑制异位骨化[42]。但需注意其具有明确的胎儿致畸性,并可能影响儿童生长发育[42]。FDA批准的首个Rett综合征[43]治疗药物trofinetide(Daybue)[44]是一种脑内源性三肽类似物(甘氨酰-脯氨酰-谷氨酸衍生物)。FIC药物牛磺罗定与肝素复方制剂(Defencath)[45]同样获得FDA批准,其中活性成分牛磺罗定是氨基酸牛磺酸的衍生物,作为广谱抗菌剂可通过破坏微生物细胞壁完整性[46]及抑制其与哺乳动物细胞粘附[47,48],用于治疗导管相关血流感染。Imetelstat(Rytelo)作为FDA批准的首个且唯一寡核苷酸端粒酶抑制剂[49],其13聚体核苷酸序列能与人端粒酶RNA组分互补结合,通过竞争性抑制导致端粒逐渐缩短并引发细胞死亡[50]。该药物适用于低危至中危-1型骨髓增生异常综合征(MDS),其III期临床试验证实可诱导持续的红细胞输注独立性(RBC-TI),这一机制优势确立了该药物的治疗价值[51]。总体而言,2023至2024年间获批的81种首创新药(FIC)中,有42种(51.9%)为小分子首创新药。具有悠久研发历史和成熟用药经验的小分子药物,仍是推动首创新药研发的重要动力。除对发病机制的深入研究与观察外,小分子药物开发来源正日趋多元化,为首创新药研发持续注入创新活力。抗体药物已成为FIC药物领域的新生力量根据美国食品药品监督管理局(FDA)的定义,生物制品通常是用于诊断、预防、治疗及治愈疾病的大型复杂分子[52]。近年来,各类副作用较少[53]的大分子药物发展迅猛,包括抗体、酶替代疗法、激素疗法、核酸疗法和疫苗等,这些药物在多种重大疾病治疗中发挥着关键作用:例如疫苗应用于传染性疾病,酶替代疗法或激素疗法用于治疗酶缺乏或激素缺乏相关疾病,其作用机制与小分子药物存在显著差异。在新型大分子药物中,抗体/抗体偶联药物(ADC)类别占比最高(40.0%),在39种FIC大分子药物中,有16种属于抗体或ADC类药物(图4)。抗体药物可表现为单克隆抗体、双特异性抗体及抗体偶联药物等多种形式[54]。此外,另有23种首创新药归属于其他大分子药物类别,包括多肽类、酶类、疫苗类及核酸类疗法(图4)。图4. FIC大分子药物的比例及分类 新型大分子药物的比例分类及首创大分子药物的数量与类别分布。新型大分子药物主要分为抗体/抗体偶联药物(ADC)、疫苗、核酸疗法、酶制剂、细胞疗法、多肽类、因子类、激素类、细胞因子、干扰素及其他类别。 在16种首创新药(FIC)抗体药物中,经欧洲药品管理局(EMA)和美国食品药品监督管理局(FDA)批准的塔奎妥单抗(Talvey)是一种靶向G蛋白偶联受体C类5组成员D(GPRC5D)与T细胞表面免疫调节膜蛋白CD3的双特异性抗体,用于治疗复发/难治性多发性骨髓瘤(MM)[56,57]。该药物与首个双特异性抗体teclistamab展现出相似的疗效特征和持续应答时间[58],同时拓展了T细胞募集双抗的已验证靶点清单[59]。人源化免疫球蛋白(Ig)G4单抗pozelimab是FDA批准用于治疗CHAPLE疾病的首创新药[60]。该疾病由补体调节蛋白CD55的基因缺失引起。在此批准前,超说明书使用依库珠单抗可改善该疾病症状,但对医疗基础设施薄弱和资源受限地区的患者而言,每两周静脉输注该药物存在显著挑战[61]。靶向补体蛋白C5的pozelimab是目前该疾病患者唯一获批的皮下注射制剂[61,62]。首个靶向claudin 18.2的单克隆抗体zolbetuximab-clzb(Vyloy)于2024年获得美国FDA批准上市。该药物联合含氟尿嘧啶和铂类化疗方案,适用于治疗CLDN18.2阳性、人表皮生长因子受体2(HER2)阴性、局部晚期不可切除或转移性胃或胃食管结合部(GEJ)腺癌成人患者的一线治疗。Claudin 18.2是CLDN18基因编码的两种亚型中的第二种亚型。与大多数作用于细胞膜表面靶点的靶向治疗药物不同,claudin 18.2是一种紧密连接蛋白,通常表达于非恶性胃上皮细胞的细胞旁间隙[6,63]。该药物的获批不仅拓展了肿瘤治疗策略的范畴,更激励研究者探索更多潜在治疗靶点[6]。在其他23种大分子FIC药物中,江苏豪森药业研发的合成肽类药物pegmolesatide(Saint Luolai)[17]适用于两类成人慢性肾脏病(CKD)贫血患者:未接受促红细胞生成刺激剂(ESA)治疗且未进行透析的患者,以及正在接受短效促红细胞生成素(EPO)治疗且进行透析的患者[64,65]。自模拟EPO的肽类药物培格司亭因致命性过敏反应撤市后[66,67],特异性ESA培莫沙肽取得了重要进展。其优势包括采用不含防腐剂的单剂量西林瓶包装及皮下给药途径[68]。该药物为每月给药一次的长效制剂,与现有EPO受体激动剂阿法依泊汀相比,在疗效和安全性方面均显示非劣效性[68-70]。Velmanase alfa-tycv(Lamzede)是首个获批用于治疗α-甘露糖苷贮积症(AM)非中枢神经系统(CNS)表现的长期酶替代疗法[71]。AM是一种由甘露糖苷酶α类2B成员1(MAN2B1)基因突变引起的罕见遗传性内分泌代谢疾病[72]。造血干细胞移植曾是该病的治疗手段,但对部分患者疗效不稳定,且可能导致表达性语言障碍和听力缺陷[73]。Velmanase alfa-tycv酶替代疗法可降低血清寡糖水平,改善患者听力和生活质量,现被视为标准治疗方案[73]。Arexvy是首个针对60岁以上呼吸道合胞病毒(RSV)感染患者的疫苗,于2023年6月获欧洲EMA批准[74]。该疫苗对RSV感染引起的下呼吸道疾病(LRTD)老年患者具有临床获益。另一款RSV疫苗Abrysvo[75]于2023年8月获EMA批准,其独特之处在于成为首个用于孕妇群体以预防婴儿RSV感染的疫苗[76]。值得注意的是,这两款RSV疫苗亦在美国和日本获批,惠及更广泛患者群体。百健与Ionis合作开发的first-in-class基因疗法tofersen(Qalsody)于2023年获美国FDA加速批准,用于治疗超氧化物歧化酶1(SOD1)基因突变相关的肌萎缩侧索硬化症(SOD1-ALS)[77]。2024年,该药物相继获得中国NMPA和EMA对相同适应症的批准。约2%的成年患者携带导致罕见病的SOD1基因突变。78 Tofersen作为反义寡核苷酸(ASO)药物,可与突变SOD1 mRNA结合形成复合物,经RNase H酶识别并切割[78],从而抑制该罕见病进展。这是首个针对SOD1-ALS的基因疗法[79],为该疾病提供了有效治疗手段[80]。随着生物技术的进步,大分子药物的研究方法日趋完善,新型大分子药物正被越来越多的患者所接受。大分子药物在首创新药(FIC)研发中具有独特优势,例如疗效更佳、不良反应较少以及作用机制特殊。在39个FIC大分子药物中,抗体药物占据主导地位,其中16个为获批的FIC药物。其余23个FIC大分子药物属于其他类型,这也表明FIC大分子药物正持续呈现多元化发展趋势[81,82]。此外,根据美国FDA既往数据,2011-2014年、2015-2018年和2019-2022年期间获批的FIC抗体/抗体偶联药物(ADC)数量分别为7个、20个和17个[1]。2023年1月至2024年10月期间已有8个药物获批,这一数字达到2019-2022年总获批量的半数,并超过2011-2014年期间的总和。这些数据表明抗体/ADC药物已成为FIC药物研发的新生力量。我们相信大分子药物未来将为患者提供更有效、更安全的治疗选择。癌症是FIC药物的主要适应症我们随后对2023年和2024年获批新药的疾病分布进行了分析。值得注意的是,这些药物的适应症广泛分布于17个疾病领域,其中2023年和2024年排名前两位的疾病领域均为癌症/肿瘤(272种药物,占比25.8%)和神经系统疾病(152种药物,占比14.7%)(图5A)。首创新药(FIC)的获批情况与新药整体分布相似。癌症/肿瘤是FIC药物最常见的靶向疾病(18种药物),血液疾病位列第二(12种药物),传染病排名第三(9种药物)(图5B)。图5. 药物适应症(疾病靶点)分布情况 (A) 2023年与2024年获批新药及首创新药(FIC)在不同疾病领域的数量统计。 (B) 获批药物中针对癌症/肿瘤适应症的占比情况。若获批药物包含首创新药适应症,则以棕色标注。(C) 获批药物中针对各类神经系统疾病适应症的占比情况。若获批药物包含首创新药适应症,则以棕色标注。作为一种全球性的重大公共卫生问题[83-86],癌症/肿瘤在所有疾病领域中占比最高[87-89]。在用于癌症/肿瘤治疗的所有药物中,针对肺癌(17.7%)、淋巴瘤(11.0%)和乳腺癌(10.6%)的治疗药物占据主导地位。首创新药(FIC)主要分布于乳腺癌、淋巴瘤、多发性骨髓瘤及肺癌等领域(图5B)。尽管某些癌症/肿瘤类型的获批药物数量少于肺癌、淋巴瘤或乳腺癌,但在神经胶质瘤、黑色素瘤和结直肠癌等疾病领域仍可见首创新药获批。这一现象可能预示着这些疾病正受到日益增长的关注。在癌症/肿瘤领域的药物中,γ-分泌酶抑制剂nirogacestat(Ogsiveo)作为首创新药获得美国FDA批准[90],用于治疗硬纤维瘤。该疾病是一种具有高复发率的罕见病,在nirogacestat获批前长期依赖手术治疗[91]。临床研究显示,nirogacestat不仅疗效显著且不良反应轻微,为患者提供了有效的治疗选择[92]。死亡受体4/5(DR4/5)激动剂aponermin联合沙利度胺与地塞米松治疗方案,首次在全球范围内获得中国国家药品监督管理局的上市许可[93]。在多种癌症中,DR4/5通过肿瘤坏死因子相关凋亡诱导配体(TRAIL)激活,进而诱导细胞凋亡[94]。该药物实质上是一种重组环状置换型人源TRAIL[93],相较于天然TRAIL具有更高的稳定性与更强的抗肿瘤活性[93]。当前尽管已有数种药物获批,多发性骨髓瘤对多数患者仍属不可治愈疾病[95]。aponermin的获批不仅为该疾病治疗提供了新策略,更证实了靶向TRAIL信号通路的可行性[96]。2024年,非小细胞肺癌(NSCLC)治疗领域取得新突破。我国国家药品监督管理局(NMPA)批准了全球首创新型双特异性单克隆抗体ivonescimab上市,该药物同时靶向程序性细胞死亡蛋白1(PD-1)与血管内皮生长因子(VEGF)-A,适用于治疗EGFR突变的局部晚期或转移性非鳞状NSCLC患者[97]。作为创新疗法,该药物在三期临床试验中联合化疗方案显著延长了无进展生存期,其疗效优势相较于PD-1抑制剂帕博利珠单抗亦得到验证[98,99]。该药物还能规避VEGF抑制剂与检查点抑制剂相关的部分不良反应[99]。获批药物的第二大疾病领域为神经系统疾病,其中主要适应症为注意力缺陷多动障碍(ADHD)(13.8%)、癫痫(11.2%)和阿尔茨海默病(AD)(9.9%)。首创新药(FIC)还分布于阿尔茨海默病(AD)、偏头痛、癫痫、硬化症等疾病领域(图5C)。该领域共有8个FIC药物获得上市许可(图5A)。偏头痛(4.6%)和杜氏肌营养不良症(2.6%)等神经系统疾病的获批药物相对较少,因此这些FIC药物可能推动相关疾病领域的新发展值得关注。在8个相关FIC药物中,omaveloxolone(Skyclarys)获得FDA批准上市,这被视为Friedreich共济失调(FA)治疗领域的重大里程碑,对罕见神经系统疾病领域具有突破性意义[100-102]。该药物是FDA批准的首个治疗罕见严重神经退行性疾病FA的疗法。该疾病由frataxin(FXN)基因内含子GAA重复序列扩增引起,导致frataxin蛋白水平降低及活性氧(ROS)产生[100],进而损伤神经系统[103]。该药物通过作用于核因子E2相关因子2(NRF2)通路[100],抑制泛素E3连接酶KEAP1(Kelch样ECH关联蛋白1)的激活——该蛋白调控NRF2的降解,从而促进新生成NRF2的积累,改善氧化应激和炎症应激,延缓疾病进展[104]。癫痫是一种因神经元活动异常导致患者反复发作的脑部疾病[105],全球患者超过7000万人[106]。欧洲药品管理局批准Ztalmy(活性成分ganaxolone)作为孤儿药[107],用于治疗2至17岁患有细胞周期蛋白依赖性激酶样5(CDKL5)缺乏症(CDD)患儿的癫痫发作[108]。该药物作为首创新药类固醇激素类似物,可产生神经活性A型γ-氨基丁酸(GABAA)受体变构调节作用[109,110],其特点在于既无类固醇激素活性,又能同时结合突触和突触外GABAA受体[109]。这一机制特征使其相较于仅作用于突触GABAA受体的苯二氮䓬类等调节剂具有显著优势[111-112]。Ganaxolone敏感的突触外γ-氨基丁酸A型受体能够在长时间癫痫发作期间维持功能性活动[112]。神经系统疾病的负担仍然十分沉重[113],而新上市的药品将为改善神经健康提供更多治疗策略。在血液及传染病领域,共有21种首创新药获批(图5A)。其中,促红细胞成熟首创新药luspatercept(Reblozyl)获得日本PMDA批准用于骨髓增生异常综合征相关贫血治疗。该药物亦是美国FDA批准用于该适应症的首个治疗方案[114,115]。Ⅲ期临床试验显示其具有持续疗效且安全性良好[116]。值得注意的是,该药物将通过降低红细胞输注需求及提升血红蛋白水平使日本患者获益[116,117]。Chikungunya活疫苗(Ixchiq)为全球首个chikungunya疫苗[118]。Chikungunya是由蚊媒传播的病毒感染性疾病,过去15年间全球报告病例约500万例,已在100多个国家出现流行,尤以非洲、东南亚和南美洲为甚[119]。该疫苗填补了该疾病预防领域的空白,满足了迫切的临床需求[120,121]。药物适应症的分类有助于我们理解药物研发的关键领域,并促进某些疾病治疗现状的更新。根据我们的统计数据显示,癌症是首创新药(FIC)的主要适应症领域。尽管用于治疗神经系统疾病的FIC药物数量不占主导地位,但该领域获批药物数量位居第二,这表明该领域部分疾病仍存在未被满足的临床需求,亟待突破性进展。我们预期未来获批的FIC药物将覆盖更多适应症,特别是目前治疗选择匮乏的疾病[122],如Rett综合征、硬纤维瘤和范可尼贫血(FA)等。激酶仍是FIC的关键靶点理想治疗靶点往往反映疾病的发生机制。药物靶点分类是对已获批药物作用机制的持续解析,这将促进疾病治疗。2023至2024年获批药物涵盖免疫相关蛋白、受体及其配体、酶、离子通道、因子和转运体等多类靶点,凸显了通过作用于多样关键靶点探索新型疗法的持续努力。在所有靶点中,酶类(330种药物,占获批靶向药物的36.5%)和激酶(148种药物)位居前列(图6A、6B)。FIC的靶点分布与获批药物相似,酶类是最常见的FIC药物靶点(26种药物),其中激酶在获批FIC药物数量上居首(11种药物)(图6C)。激酶作为蛋白质磷酸化调节剂,参与多种生物学功能和疾病机制[123]。首个蛋白激酶B(AKT)抑制剂[124]——阿斯利康的capivasertib(Truqap)获FDA[125]批准联合氟维司群,用于治疗伴有PIK3CA/AKT1/PTEN基因改变的激素受体(HR)阳性、HER2阴性局部晚期或转移性乳腺癌[126]成人患者。AKT是一种具有AKT1、AKT2和AKT3三种亚型的丝氨酸/苏氨酸蛋白激酶,最早于1977年被记录并于1991年鉴定[127,128]。Capivasertib作为竞争性抑制剂,通过占据AKT中ATP结合位点抑制所有AKT亚型,从而减弱AKT底物磷酸化并影响细胞生长增殖[129]。图6. 2023年与2024年获批药物的治疗靶点分析 (A) 2023年及2024年获批药物作用于各类靶点的比例分布,以及这些靶点类别中首创新药(FIC)的数量与分布情况。 (B) 针对不同酶类别的药物数量统计。若靶点为FIC药物作用靶点,则以紫色标注。(C) 作用于不同酶类型的FIC药物数量统计。在一类新型高选择性Janus激酶3(JAK3)与肝细胞癌中表达的酪氨酸激酶(TEC)双重抑制剂中[16,130],ritlecitinib(Litfulo)已获得中国国家药监局、美国FDA、日本PMDA及欧盟EMA批准,用于斑秃治疗[131]。JAK3与TEC酪氨酸激酶家族均属非受体型酪氨酸激酶,其抑制作用可调控参与斑秃发病机制的多个信号通路[132,133],但具体作用机制尚未完全阐明[134]。一项随机双盲、多中心IIb-III期临床试验证实,ritlecitinib对12岁及以上斑秃患者具有良好疗效与耐受性[135]。不同JAK亚型抑制剂可适用于不同疾病领域。2024年,中国国家药监局批准首创新药JAK1特异性抑制剂golidocitinib用于治疗至少经过一线系统治疗后进展或难治的复发/难治性外周T细胞淋巴瘤[136,137]。JAK1在STAT3磷酸化及活化过程中起关键作用,而JAK-STAT通路激活与T细胞恶性肿瘤密切相关。鉴于作用于其他JAK家族成员的分子存在较大副作用风险,选择性JAK1抑制剂被推定为理想治疗药物。临床试验显示golidocitinib具有优势性的获益-风险特征,这为其最终获批提供了依据[138]。除酶类靶点外,2023至2024年获批药物的作用靶点还涉及多个其他类型。例如,17.4%的获批药物作用于GPCRs,其中包含9个靶向GPCRs的首创新药(图6A)。在这9个首创新药中,内皮素A型受体(ETAR)与血管紧张素II(Ang II)1型受体(AT1R)双重拮抗剂DEARA类药物sparsentan(Filspari)获得加速批准,用于治疗具有快速疾病进展风险的原发性IgA肾病成人患者的蛋白尿症状[139]。IgA肾病是一种罕见自身免疫性疾病[140],其发病机制中AT1R与ETAR的激活与蛋白尿形成相关[141-142]。该药物是FDA批准的首个且唯一用于IgA肾病的非免疫抑制疗法,在保证疗效的同时提升了患者用药依从性[143]。其双靶点拮抗机制相比单靶点拮抗能产生更优的治疗效果[141],并可能通过抑制血管紧张素转换酶或阻断血管紧张素受体作为蛋白尿的一线治疗选择[143]。此外,FDA还批准了具有新型作用机制的xanomeline与曲司氯铵复方新药(Cobenfy)用于精神分裂症治疗[144]。Xanomeline是M₁和M₄毒蕈碱受体的选择性激动剂,而曲司氯铵为泛毒蕈碱受体拮抗剂[145]。由于对外周毒蕈碱受体的激活作用,xanomeline单药治疗可能引发不良事件[145];而曲司氯铵因其理化特性无法透过血脑屏障[145]。因此,这两种药物的联用方案既能减轻副作用又具有良好疗效[146]。更值得注意的是,该联合用药方案首次实现了不含D2多巴胺受体阻断活性的抗精神病药物治疗,而阻断D2受体曾是传统疗法的典型作用机制[144]。新治疗靶点的发现是首创药物研发的第一步[147]。分析已获批药物的靶点类型有助于我们理解新治疗靶点的研究趋势。尽管已有多种作用于激酶的药物上市,但在已知激酶中,仅十分之一被验证为癌症治疗靶点[148],且至少70%的激酶尚未作为药物靶点进行探索[149]。未来仍需开展更多激酶相关研究。除激酶外,G蛋白偶联受体、免疫相关蛋白及核激素受体均是具有重要研究潜力的靶点类别。前景展望2023至2024年间,全球范围内有多款首创新药(FIC)获批上市。美国FDA批准的FIC药物数量最为显著,中国NMPA、欧盟EMA及日本PMDA在FIC药物审批方面亦作出重要贡献。基于FDA 2011-2024年数据统计,2023年1月至2024年10月期间获批的FIC药物数量处于高位[1],其中小分子FIC药物与大分子FIC药物的获批数量基本持平。值得注意的是,FIC小分子药物与大分子药物广泛分布于更多药物类型中,这反映出传统药物设计与新型生物技术的协同发展与深度融合,有力推动了FIC药物的研发进程。多款FIC药物在癌症等疑难杂症及Rett综合征、多发性骨髓瘤、范可尼贫血等罕见病领域发挥关键作用,成为这些疾病的首选治疗方案或突破性疗法。然而,对于CHAPLE病、硬纤维瘤、阿尔茨海默病等仍缺乏有效治疗手段的疾病领域,尚需持续探索新的治疗方案以解决未满足的临床需求。激酶作为FIC药物研发的重要靶点,其生物学功能及基于激酶的药物设计仍需开展更深入的研究。尽管2023-2024年有多款药物获批,但药物研发领域仍存在巨大的突破空间。例如,许多难治性神经系统疾病仍需要突破性疗法或首创药物。此外,转运蛋白在新获批药物靶点中占比相对较少,因此针对这些潜在靶点的深入研究可能具有重要价值[150]。通过对部分候选药物的分析,2025年神经系统疾病领域可能取得进一步突破。具有潜在首创新药(FIC)特性的seltorexant [151](适应症为重度抑郁症)及suzetrigine [152](用于治疗中重度急性疼痛)已在Ⅲ期临床试验中显示出积极结果。从治疗靶点来看,首创DNA拓扑异构酶2抑制剂gepotidacin [153]及首个神经激肽1(NK-1)与神经激肽3(NK-3)受体双重拮抗剂艾elinzanetant [154]正在等待审批,这表明酶类与G蛋白偶联受体(GPCR)在2025年药物审批中或将继续占据主导地位。我们亦期待新靶点类型的探索将推动首创新药问世,并为疾病治疗开辟新途径。首创药物在药物研发领域持续发挥着引领作用。它们不仅显著提升了疾病治疗的有效性,还拓展了药物的新型作用机制,这些突破性进展不仅深化了人类对疾病病理学的认知,更彰显了全球公共卫生水平与生活质量的提升。我们预期药物研发将继续推动创新药物的进一步发展,以覆盖更广泛的疾病谱、惠及更多患者群体。投稿/企业合作/内容沟通:华籍美人(Ww_150525)*添加请注明备注及来意
抗体药物偶联物临床结果上市批准申请上市多肽偶联药物
2025-04-30
2025年4月29日,康方生物自主研发的中国首个且唯一自主创新的IL-12/IL-23“双靶向”单克隆抗体爱达罗®(依若奇单抗注射液)成功完成首批发货,满载依若奇单抗的车辆即刻启程,正式发往全国各大医疗终端,为我国约700万受银屑病困扰的患者带来更便捷、安全、高效的全新治疗选择。4月18日,国家药品监督管理局正式批准康方生物独立自主研发的依若奇单抗注射液上市,用于治疗中重度斑块状银屑病成人患者。依若奇单抗是中国首个且唯一自主创新的IL-12/IL-23“双靶向”Ⅰ类新药,也是康方生物自身免疫性疾病领域首个获批上市的Ⅰ类新药。康方生物联合创始人、高级副总裁王忠民博士在爱达罗®发货活动中表示:无论参加了多少次新药首批发货活动,我的内心仍旧激动,依若奇的发货更让我倍感骄傲。一方面,依若奇作为中国首个获批上市的国产IL-12/IL-23“双靶向”单抗新药,使得中国银屑病患者迎来了更为强效、长程、安全、便捷且经济的治疗新选择,践行了我们让中国患者率先用上全球最好药物的初衷。另一方面,依若奇的获批上市,标志着公司2019年及之前进入临床阶段的10个产品中,已有7个成功获批上市商业化,3个产品处于NDA或者关键临床后期阶段,获批产品中还包含2个全球首创的双抗新药。康方生物首席商业官、高级副总裁 郭永先生对依若奇单抗的临床应用前景充满信心:依若奇单抗开启了IL-12/IL-23单抗的国产化新时代。多项临床研究显示,依若奇单抗具有良好的疗效和优异的安全性,短期疗效显著,长期可稳定维持,不仅能有效改善皮损,还能显著提高患者生活质量。依若奇单抗的成功获批、上市后仅一周余即高效完成全国商业发货,体现了各部门团结的高效协同能力。公司将继续秉承以患者为中心、以学术为根本的理念,赢得广大医生和患者对依若奇单抗的广泛认可,为中国银屑病患者提供长期治疗的优选方案。银 屑 病银屑病是一种慢性、复发性的至今不可治愈的自身免疫性疾病,我国患病人数约700万,并呈逐年增加趋势。传统药物治疗效果欠佳,且可能伴随较多不良反应,患者期待疗效更持久且安全便捷的治疗选择。爱达罗®的上市,为患者提供了一种兼具强效、长程、安全、便捷且经济的治疗方案。在临床研究中,该药物充分展示出以下特性:三期注册临床研究显示,依若奇单抗短期疗效优异,两针即可显著改善皮损,长期强效持久。接受135mg依若奇注射液,在第0周和第4周各注射1针,第16周时PASI 75(银屑病面积和严重程度指数)达到79.4%,疗效显著。而接受每12周1次(Q12W)维持治疗,至第52周的PASI 75仍高达77.9%,疗效长期稳定。同时,依若奇单抗还能显著改善患者的生活质量,治疗16周后,因皮肤疾病对患者生活质量的影响程度下降超过55%;治疗至第52周时,该影响程度进一步下降至超过65%。此外,该药物安全性优异,不良事件发生率较低,首年仅需5次,维持期年度仅需4次皮下注射给药,用药便捷性高,可有效提高患者用药依从性。说明:本文作为康方生物的新闻发布,用于披露公司最新进展,并非产品推广广告,不构成康方生物的信息披露或投资建议。关于爱达罗®(IL-12/IL-23单抗,依若奇)爱达罗®(依若奇单抗注射液)是公司自主研发的新型人源化IL-12/1L-23单克隆抗体新药,获得国家“重大新药创制”科技重大专项课题支持,主要用于治疗银屑病、溃疡性结肠炎和其他自身免疫性疾病。爱达罗®通过阻断细胞因子IL-12和IL-23的生物学活性,以达到临床治疗自身免疫性疾病的作用。银屑病的发病与异常免疫反应相关,IL-12及IL-23是炎症反应及免疫反应中自然产生的细胞因子,拥有共同的p40亚基,其中IL-12诱导Th1细胞(辅助性T细胞1)增殖并释放干扰素与TNF-α(肿瘤坏死因子α),IL-23诱导Th17细胞(辅助性T细胞17)发育并释放IL-17(白介素-17)等,这些细胞因子在炎性反应及免疫反应中起到促进或具有重要作用。依若奇单抗通过靶向IL-12和IL-23的p40亚基并与之结合,同时抑制IL-12和IL-23与细胞表面受体的相互作用,进而减少T细胞对干扰素、TNF-α、IL-17等相关细胞因子的释放,阻断各自介导的细胞免疫反应,从而抑制银屑病的异常免疫反应。2025年4月,爱达罗®治疗中度至重度斑块状银屑病适应症获批上市,成为公司在自身免疫性疾病领域斩获的首个获批成果,也成为公司第7款进入商业化阶段的自主创新药物。关于康方生物康方生物(9926.HK)是一家集研究、开发、生产及商业化全球首创或同类最佳创新生物新药于一体的领先企业。自2012年成立以来,公司始终以患者为中心,以临床价值为导向,打造了独有的端对端康方全方位新药研究开发平台,建立了以Tetrabody双特异性抗体开发技术、抗体偶联(ADC)技术、mRNA技术及细胞治疗技术为核心的研发创新体系,国际化标准的GMP生产体系和运作模式先进的商业化体系,成为了在全球范围内具有竞争力的生物医药创新公司。公司已开发了50个以上用于治疗肿瘤、自身免疫、炎症、代谢疾病等重大疾病的创新候选药物,24个候选药已进入临床(包括15个双抗/多抗/双抗ADC),7个新药已在商业化销售,3个新药3个适应症的上市申请处于审评审批阶段。康方生物是全球迄今唯一拥有2个肿瘤免疫双抗新药的制药公司:2022年6月,公司全球首创的PD-1/CTLA-4双抗开坦尼®获批上市,是全球首个获批的肿瘤免疫治疗双抗新药,也是中国第一个双特异性抗体新药。目前开坦尼®一线治疗胃癌和治疗复发/转移性宫颈癌适应症已获批,一线治疗宫颈癌sNDA已受理,8个注册性/III期临床已开展。2024年5月,公司另一全球首创双抗新药依达方®获批上市,用于EGFR-TKI治疗进展的局部晚期或转移性nsq-NSCLC,是全球首个获批的“肿瘤免疫+抗血管生成”机制双抗新药。同期,依达方®在与全球“药王”帕博利珠单抗的随机、双盲、对照一线治疗PD-L1阳性NSCLC的“头对头”III期临床研究中获得显著阳性结果,依达方®可降低患者疾病进展/死亡风险达49%,依沃西成为全球迄今唯一在头对头III期临床研究中证明疗效显著优于“药王”帕博利珠单抗的药物。基于该研究结果,依沃西该项新适应症已于2025年4月获批上市,成为一线肺癌治疗新的标准治疗方案,为患者提供全新更优的“去化疗”选择。目前依达方®有12项注册性/III期临床已开展,包括3项国际多中心注册性III期临床研究。2024年12月,开坦尼®、依达方®均通过医保谈判被纳入国家新版医保目录。国际市场开发是康方生物核心发展战略,继2015年开中国先河将自主研发的CTLA-4单抗权益许可给默沙东公司之后,2022年12月,公司再次创造中国记录,以50亿美金+2位数百分比销售提成的方案,将依达方®部分海外权益许可给美国Summit公司,该合作创下了彼时中国新药对外许可的最高交易金额记录。2025年2月,Summit 与美国辉瑞(Pfizer)公司达成临床试验合作,共同推进依达方®联合辉瑞多款抗体偶联药物(ADCs)在多种实体瘤中的联合治疗疗法。安尼可®联合方案一线治疗转移性鼻咽癌和单药用以铂类为基础的化疗治疗失败的转移性鼻咽癌两项适应症于2025年4月获得美国食品药品监督管理局(FDA)批准上市。2024年9月,公司自主研发的伊喜宁®(伊努西单抗,PCSK9)治疗高胆固醇血症两项适应症获批,成为非肿瘤领域的首个获批产品。2025年4月,公司独立自主研发的爱达罗®(依若奇单抗,IL-12/IL-23“双靶向”单抗)获得批准上市,用于中重度斑块状银屑病成人患者的治疗。公司非肿瘤领域的产品协同效应和战略组合力进一步提升。康方生物期望通过高效及突破性的研发创新,开发国际首创及同类药物最佳疗法的新药,为全球患者提供更优疾病解决方案,成为全球领先的生物制药企业。往期推荐产品动态依沃西一线治疗NSCLC获批上市(全球首个对比帕博利珠单抗获显著阳性结果的III期研究)产品动态美国重磅上市!派安普利单抗2个适应症获FDA批准上市,用于晚期鼻咽癌治疗产品动态康方生物爱达罗®(依若奇,IL-12/IL-23)治疗中重度斑块状银屑病适应症获批上市临床进展首个自研ADC澳洲临床入组!康方生物IO 2.0+ADC战略再进一步临床进展非肿瘤首个双抗|康方生物全球首创IL-4Rα/ST2(AK139)IND获受理,剑指呼吸系统及皮肤疾病领域临床进展依沃西方案对比替雷利珠方案1L治疗sq-NSCLC的Ⅲ期临床完成患者入组临床进展康方生物古莫奇(IL-17)单抗新药上市申请获NMPA受理数据发布荣登Nature Medicine!卡度尼利方案1L治疗胃癌Ⅲ期研究结果全文发表产品动态康方生物卡度尼利、依沃西纳入2024年国家医保目录临床进展头对头度伐利尤单抗方案,依沃西方案一线治疗胆道肿瘤III期临床完成首例患者入组临床进展全球首个CD47单抗实体瘤III期临床首例入组:依沃西联合莱法利一线治疗HNSCC(对比帕博利珠单抗)数据发布卡度尼利一线宫颈癌III期研究成果荣登《Nature Reviews Clinical Oncology》(影响因子高81.1)数据发布IGCS 2024 LBA & 《柳叶刀》主刊,卡度尼利1L宫颈癌III期研究PFS和OS双阳性结果重磅发布产品动态一线胃癌全人群获批!康方生物卡度尼利获批第二个适应症产品动态获FDA快速通道资格!依沃西国际多中心III期研究HARMONi完成入组,2L+EGFRm NSCLC数据发布全球首个对比帕博利珠单抗取得显著阳性结果的随机对照大III期研究——依沃西HARMONi-2重磅研究成果在WCLC发表临床进展康方生物卡度尼利联合方案治疗uHCC的III期临床研究完成首例患者入组临床进展针对PD-1/L1治疗进展晚期胃癌,卡度尼利+普络西(VEGFR-2)联合疗法Ⅲ期临床完成首例入组数据发布ASCO Oral & JAMA主刊丨Ⅲ期HARMONi-A研究重磅公布,依沃西疗法有望改变EGFR-TKI进展肺癌全球治疗标准临床进展史无前例!康方依沃西单药对比帕博利珠1L治疗PD-L1阳性NSCLC的III期临床获决定性胜出阳性结果产品动态康方生物双抗卡度尼利一线治疗晚期宫颈癌全人群的sNDA获CDE受理临床进展国际多中心注册性III期研究HARMONi-3中国启动:依沃西单抗联合化疗对比帕博利珠单抗联合化疗1L治疗sq-NSCLC产品动态高达50亿美金!康方生物与Summit就PD-1/VEGF双抗依沃西达成合作和许可协议产品动态全球首个肿瘤免疫治疗双抗——开坦尼®(PD-1/CTLA-4双抗,卡度尼利)获批上市
上市批准临床3期
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
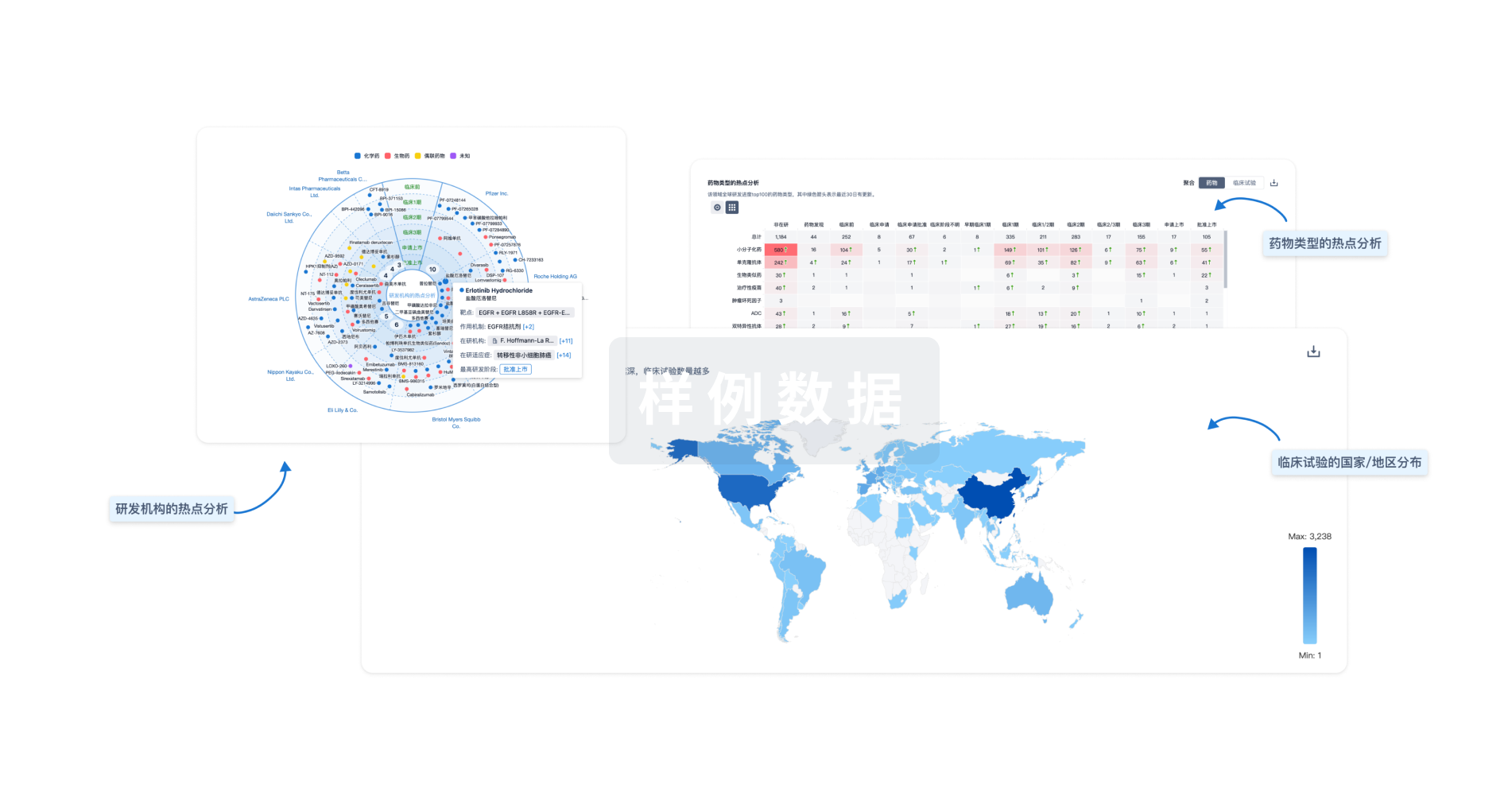
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用





