预约演示
更新于:2025-05-07
CDH3
更新于:2025-05-07
基本信息
别名 cadherin 3、cadherin 3, P-cadherin (placental)、cadherin 3, type 1, P-cadherin (placental) + [6] |
简介 Cadherins are calcium-dependent cell adhesion proteins. They preferentially interact with themselves in a homophilic manner in connecting cells; cadherins may thus contribute to the sorting of heterogeneous cell types. |
关联
22
项与 CDH3 相关的药物作用机制 CDH3 modulators [+1] |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
作用机制 CDH3抑制剂 [+1] |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点 |
作用机制 CDH3抑制剂 |
在研适应症 |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
17
项与 CDH3 相关的临床试验NCT06548672
A Phase Ia/Ib, Open-Label, Dose Escalation and Dose Expansion Study to Evaluate the Safety, Tolerability, Pharmacokinetics (PK), and Preliminary Efficacy of BC3195 in Patients With Locally Advanced or Metastatic Solid Tumors
This is a phase Ia/Ib, open-label, dose escalation and dose expansion study to evaluate the safety, tolerability, pharmacokinetics, and antitumor activity of BC3195 in subjects with locally advanced or metastatic solid tumors in whom standard treatment has failed (either due to disease progression or intolerance). This study will consist of two parts: Dose escalation (Part 1) and dose expansion (Part 2). Each part will include a screening period, a treatment period, and follow-up period.
开始日期2024-06-24 |
申办/合作机构 |
CTIS2022-502867-39-00
- 20220073
开始日期2023-10-23 |
申办/合作机构 |
CTR20231334
评估BC3195在局部晚期或转移性实体瘤患者中的安全性、耐受性、药代动力学特征以及初步有效性的开放性、首次人体剂量递增和剂量扩展Ia/Ib期临床研究
主要研究目的:
1、评价BC3195在局部晚期或转移性实体瘤患者中的安全性和耐受性;
2、探索最大耐受剂量(MTD)及II期试验推荐给药剂量(RP2D)。
次要研究目的:
1、探索BC3195在局部晚期或转移性实体瘤患者中的初步疗效;
2、考察BC3195在局部晚期或转移性实体瘤患者中的药代动力学特征;
3、考察BC3195在局部晚期或转移性实体瘤患者中的免疫原性。
探索性目的:
1、探索BC3195在局部晚期或转移性实体瘤患者中疗效相关的生物标志物。
开始日期2023-06-26 |
申办/合作机构 |
100 项与 CDH3 相关的临床结果
登录后查看更多信息
100 项与 CDH3 相关的转化医学
登录后查看更多信息
0 项与 CDH3 相关的专利(医药)
登录后查看更多信息
936
项与 CDH3 相关的文献(医药)2025-06-01·Laboratory Investigation
Clinicopathological Characteristics of a Distinct Tumor Phenotype: Invasive Lobular Carcinoma With Tubular Elements in the West German Study Group ADAPTcycle Trial
Article
作者: Harbeck, Nadia ; Jóźwiak, Katarzyna ; Radner, Martin ; Graeser, Monika ; Christgen, Matthias ; Kreipe, Hans ; Schaumann, Nora ; Kandt, Leonie D ; Eulenburg, Christine Zu ; Christgen, Henriette ; Gluz, Oleg ; Hillmann, Pia ; Kümmel, Sherko ; Burmeister, Sandy ; Raap, Mieke ; Gronewold, Malte ; Bartels, Stephan ; Lehmann, Ulrich
2025-04-15·Cancer
Prospects for radioimmunotherapy panaceas in gynecologic oncology
作者: Chauhan, Aman ; Kunos, Charles A.
2025-03-01·Biophysical Journal
Distinct roles of protrusions and collagen deformation in collective invasion of cancer cell types
Article
作者: Longmore, Gregory D ; Pathak, Amit ; Lee, Ye Lim
58
项与 CDH3 相关的新闻(医药)2025-04-01
·药时代
2023年,国产创新药出海迎来大爆发,出海授权数量首次超过从海外引进的数量,被我们称之为出海“元年”。2024年,国产创新药出海不仅在交易数量和交易总金额上更进一步,出海方式也开始呈现多模式并存。中国药企在延续License-out的同时,探索NewCo模式与国际资本合作,并推动自主商业化,逐步在欧美市场建立本地化运营能力,形成多元化国际化路径。经历了2023年与2024年的盛景,2025年的创新药出海将会迎来曾样的场景?据药时代不完全统计,2025年第一季度中国医药出海共计33笔,已披露金额超362亿美元。其中,启德医药与Biohaven、韩国AimedBio的大宗商务战略合作最为亮眼,协议总金额超130亿美元。就单笔交易而言,首付款最高的交易有两笔。3月24日,联邦制药将GLP-1/GIP/GCG三重受体激动剂UBT251除大中华区的权益授权给诺和诺德,首付款为2亿美元。另一起则发生于次日,恒瑞医药宣布将旗下Lp(a)口服小分子抑制剂HRS-5346除大中华区的权益授权给默沙东,首付款同样为2亿美元。在已披露信息中,2025年第一季度最为热门的出海领域仍是ADC。首先,ADC交易金额最高,达165.27亿美元。主要原因为启德130亿美元的大宗商务战略合作,便是基于旗下FGFR3靶点同类首创ADC以及旗下iLDC®和iGDC®ADC技术平台所达成的。注:笔者将百奥赛图与SOTIO的合作算入,虽出海实体是抗体,但交易本质是为了支持后者ADC候选药物SOT109的研发其次,ADC出海交易数量最高,共计有8笔。窥一斑而知全貌,这8笔交易恰好能在一定程度上,反映出目前MNC与Biotech面对ADC资产时的投资偏好。MNC更愿意尝试联合用药,在8笔交易中有两笔都是MNC的联合开发合作。其中包括宜联生物的B7H3 ADC与阿斯利康的度伐利尤单抗联合开发,以及智康弘义的CDH3 ADC与默沙东的K药联合开发。Biotech更愿意尝试新靶点的早资产。除了上述两笔联用组合,其他6笔交易均为临床早期阶段(信达生物的IBI3009为临床一期,其余均为临床前),且8笔交易中无HER2、Trop2这样的热门靶点。为此,药时代特别邀请了昭衍生物工艺开发下游纯化总监刘杰研究员,于2025年4月2日晚上7点至8点,与大家共同探讨抗体偶联药物的工艺开发与案例分享。回顾2025年第一季度,参与交易的中国创新药资产主要以早期阶段为主(临床前、I期、II期),资产占比达55%以上。该趋势符合目前国内药企出海现状,从转让方的角度来看,医保调整周期调为每年一次,意味着创新药商业化周期同步缩短,更面临降价压力;资本寒冬下每做一条管线,就代表有费用、人力成本的产生,即便是早期资产数据优异,也药考虑从哪“搞钱”,而当下就“搞钱”最难。从受让方的角度来看,III期之后资产本身价值就高,后期投入呈断崖式增长,选择早期资产本身价值相对较低,纵使失败也在可接受范围内,可以多买多试,毕竟一个新靶点新机制的首创类新药,竞争对手较少,且能填补未满足的临床需求,谁不想买回来查漏补缺?以小博大正当时。正因如此,当下火热的NewCo模式便是资本寒冬下的特殊产物。2024年,恒瑞、康诺亚、嘉和生物、岸迈生物、维立志博、康诺亚等多家药企均通过“NewCo”模式成功出海。2025年第一季度,通过“NewCo”模式出海的有和铂医药、科伦博泰、康诺亚等药企。值得注意的是,康诺亚半年内完成了三次NewCo。2024年7月,康诺亚将两款双抗新药CM512、CM536的大中华区外全球权益授权给Belenos Biosciences;同年11月,将BCMA/CD3双抗CM336授权给Platina Medicines Ltd;今年1月,又CD38单抗CM313授权给Timberlyne Therapeutics。不难看出,NewCo模式既能通过早期管线创造一定价值,又能通过股权,降低自身风险、参与公司决策,并锁定更多远期收益。但客观地讲,NewCo模式就是产品管线在短期里无法出手情况下的一种过渡性选择。是用时间来换空间,用一批新的资金、新的资本市场对产品的认可换未来产品上市、并购的交易机会,这是阶段性解决产品研发往前推动的合时宜的选择。如果国内资本市场退出是通畅的市场,相比NewCo、甚至license-out都不会有当下热度。在资本市场成熟时期,更多的出现的或许是收并购。小结:中国创新药出海的浪潮,既是技术突围的见证,也是全球化博弈的缩影。从License-out到NewCo模式,中国药企总能以更灵活的策略在资本寒冬中破局。然而,热潮之下暗藏隐忧。资本市场退出的不畅、同质化竞争的加剧,仍需政策、资本与技术的协同破冰。如何在“技术出海”与“价值闭环”间找到平衡,让中国创新药真正从“走出去”迈向“立得住”。这场跨越山海的征途,注定是一场耐力与远见的较量。图片来源:正文血液瘤龙头利刃出鞘2025-03-31 第四届World ADC Asia欢迎您!药时代朋友可享受10%优惠2025-03-30 FDA CBER主任Peter Marks博士的辞职信(附:中英文版本)2025-03-29 版权声明/免责声明本文为原创文章。本文仅作信息交流之目的,不提供任何商用、医用、投资用建议。文中图片、视频、字体、音乐等素材或为药时代购买的授权正版作品,或来自微信公共图片库,或取自公司官网/网络,部分素材根据CC0协议使用,版权归拥有者,药时代尽力注明来源。如有任何问题,请与我们联系。衷心感谢!药时代官方网站:www.drugtimes.cn联系方式:电话:13651980212微信:27674131邮箱:contact@drugtimes.cn点击这里,查看更多精彩!
引进/卖出抗体药物偶联物临床1期
2025-03-14
·医药观澜
▎药明康德内容团队报道
今日(3月14日),智康弘义宣布,已与默沙东(MSD)达成临床试验合作协议,将在全球范围内开展一项针对局部晚期或转移性实体瘤患者的1/2期临床试验,以评估智康弘义的BC3195(靶向CDH3的抗体偶联药物)与默沙东PD-1抑制剂KEYTRUDA(帕博利珠单抗)联合用药的效果。
根据协议条款,智康弘义将开展一项1/2期临床试验,以评估BC3195与帕博利珠单抗联用的安全性和有效性。智康弘义和默沙东各自保留其相应化合物的所有商业权利。该临床研究的招募工作预计将于2025年第四季度开始。
BC3195是智康弘义开发的新一代靶向CDH3的抗体偶联药物(ADC),该产品采用与CDH3蛋白具有较高亲和力并展现出良好内吞活性的抗体,同时采用经临床验证、具有“旁观者效应”的连接子和有效载荷vc-MMAE,以进一步提高临床开发成功率和满足未来不同场景临床需求。
根据智康弘义新闻稿介绍,BC3195在临床前研究中表现出优异的肿瘤抑制活性,在多个肿瘤模型中的肿瘤生长抑制率大于100%。2024年9月14日,智康弘义在欧洲肿瘤学会(ESMO)年会上公布了BC3195在1期临床试验中针对晚期实体瘤的安全性和有效性的最新临床数据。数据显示,BC3195具有可控的安全性和良好的PK特征;在NSCLC患者中显示出显著的抗肿瘤活性,其总体缓解率(ORR)达到36.4%,尤其是对携带EGFR突变的患者ORR达到80%。
BC3195目前正在中美同步进行开展1期剂量优化和剂量扩展研究。已有临床数据表明,BC3195具有可控的安全性和良好的PK特征,同时具有显著的抗肿瘤效果,在多个瘤种中观察到确认的PR。
智康弘义共同创始人、执行总裁王一维博士表示,在既往临床试验中,BC3195单药疗法已获得的临床数据令人振奋,这些数据表明BC3195能显著改善某些非小细胞肺癌和乳腺癌患者的抗肿瘤效果。智康弘义会持续推进这款ADC药物的临床开发,通过此次合作探索BC3195与KEYTRUDA的联合治疗潜力,将进一步验证公司药物发现与开发的差异化优势。
参考资料:
[1]智康弘义宣布与默沙东合作开展BC3195 ADC联合KEYTRUDA®(帕博利珠单抗)的临床研究. Retrieved Mar 14, 2025, from https://mp.weixin.qq.com/s/zBHWXOas_WbDOoBZ82dgyQ
本文由药明康德内容团队根据公开资料整理编辑,欢迎个人转发至朋友圈。转发授权及其他合作需求,请联系wuxi_media@wuxiapptec.com。
免责声明:药明康德内容团队专注介绍全球生物医药健康研究进展。本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。
抗体药物偶联物临床1期临床结果
2025-03-13
SHANGHAI, March 13, 2025 /PRNewswire/ -- BioCity Biopharmaceutics Co., Ltd., a clinical-stage biopharmaceutical company, today announced that it has entered into a clinical trial collaboration agreement with MSD (Merck & Co., Inc., Rahway, NJ, USA), to evaluate the combination of BioCity's BC3195 and MSD's anti-PD-1 therapy, KEYTRUDA® (pembrolizumab), in a global phase 1/2 trial in patients with locally advanced or metastatic solid tumors.
Under the terms of the agreement, BioCity will conduct a phase 1/2 clinical trial to evaluate the safety and efficacy of BC3195 in combination with KEYTRUDA. BioCity and MSD each retain all commercial rights to their respective compounds. The recruitment in the clinical study is expected in Q4 2025.
"We are encouraged by the clinical data we have seen thus far for BC3195 as monotherapy, which have demonstrated improved anti-tumour activity in patients with certain non-small cell lung and breast cancers. We now look forward to exploring the potential of BC3195 in combination with KEYTRUDA through this collaboration, as we continue to advance our clinical program and seek to further validate our differentiated drug discovery and development approach." Said by Ivy Wang, Co-founder and Executive President of BioCity.
KEYTRUDA® is a registered trademark of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
About BC3195
BC3195 is currently the only ADC targeting CDH3 (P-Cadherin) in clinical development globally. In preclinical studies, BC3195 binds to membrane CDH3 with strong affinity and is efficiently internalized. BC3195 is designed with a clinically validated, cleavable linker and payload (vc-MMAE) allowing for the destruction of targeted cancer cells, as well as surrounding cells, which is known as the bystander effect. In animal models, BC3195 demonstrated a favorable safety profile and robust antitumor activity with tumor growth inhibition ≥100% in some animals bearing well established cancers.
BC3195 is currently undergoing concurrent Phase I dose optimization and dose expansion in China and in US. BC3195 demonstrated a manageable safety profile and favorable PK characteristics, significant antitumor activity with confirmed PRs observed across multiple tumor types.
About BioCity
Founded in December 2017, BioCity is a clinical-stage biopharmaceutical company committed to developing novel and highly differentiated, modality-independent therapeutics for cancer and autoimmune disorders including chronic kidney diseases. BioCity has established a pipeline of more than 10 innovative drug candidates, including small molecules, monoclonal and bispecific antibodies, and antibody-drug conjugates (ADC).
Currently, BioCity has five core oncology assets in Phase 1/2 clinical development, including first-in-class CDH3-targeting ADC and GPC3-targeting ADCs, WEE1 and ATR inhibitors targeting the DNA damage response (DDR) pathway, and a monoclonal antibody targeting TIM-3 in collaboration with AstraZeneca. In addition, BioCity's SC0062, a highly selective ETA antagonist, is in phase 3 clinical development for IgA nephropathy and a global phase 3 registration trial is being planned.
For more information, please visit
Or LinkedIn BioCity Biopharma
Contact:
[email protected]
[email protected]
SOURCE BioCity Biopharma
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床1期引进/卖出临床3期抗体药物偶联物
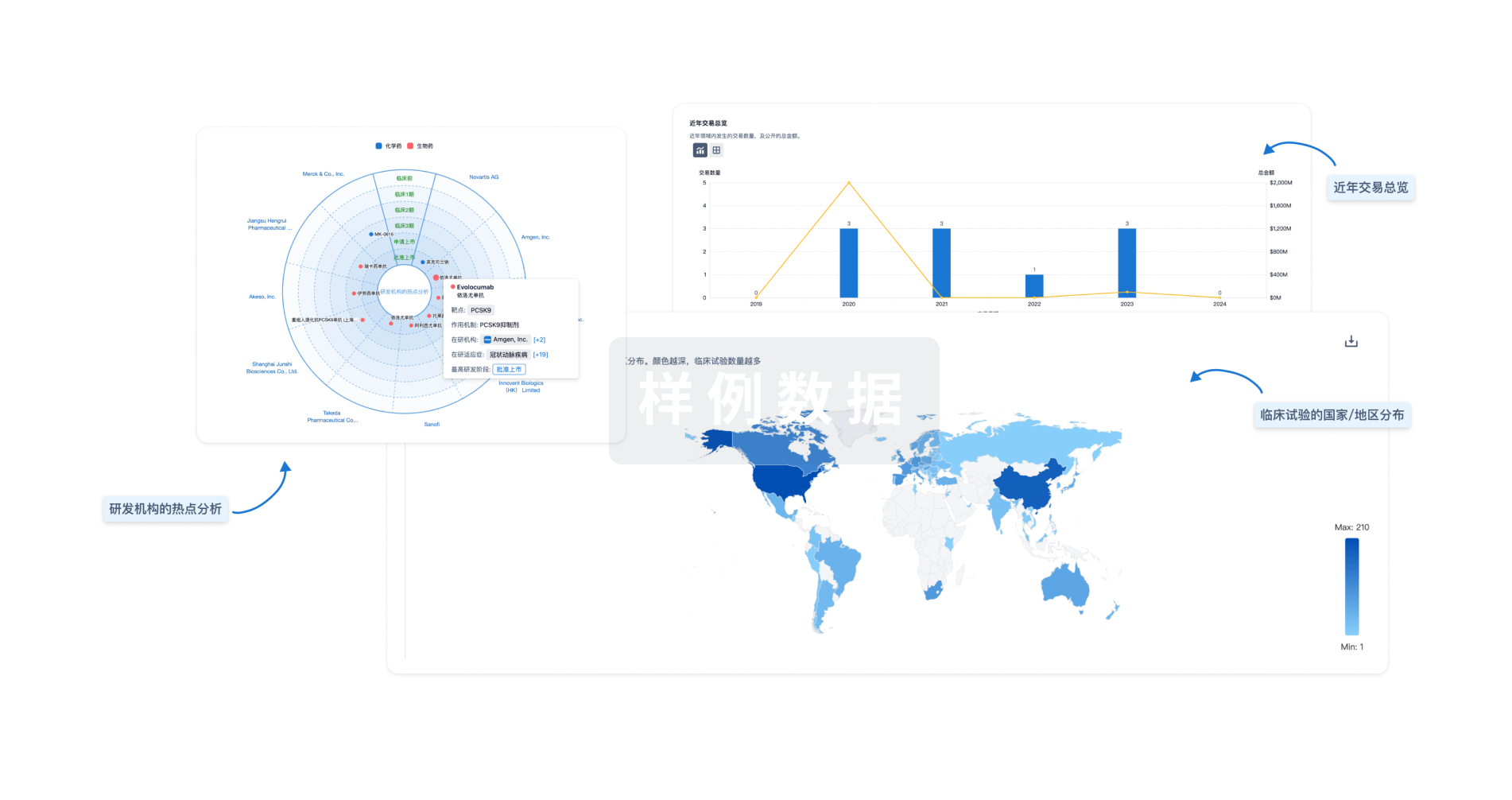
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用