预约演示
更新于:2025-05-07

CG Oncology, Inc.
更新于:2025-05-07
概览
标签
遗传病与畸形
肿瘤
其他疾病
溶瘤病毒
单克隆抗体
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 溶瘤病毒 | 1 |
| 单克隆抗体 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| CSF-2R(粒细胞 - 巨噬细胞集落刺激因子受体复合体) | 1 |
| PD-1(细胞程序性死亡-1) | 1 |
关联
3
项与 CG Oncology, Inc. 相关的药物靶点- |
作用机制 DNA烷化剂 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期1963-09-25 |
靶点 |
作用机制 CSF-2R刺激剂 |
在研适应症 |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
10
项与 CG Oncology, Inc. 相关的临床试验NCT06567743
A Phase 2, Multi-Arm, Multi-Cohort, Open-Label Study to Evaluate the Safety and Efficacy of Cretostimogene Grenadenorepvec in Participants With High-Risk Non-Muscle-Invasive Bladder Cancer (NMIBC)
This is a Phase 2, Multi-Arm, Multi-Cohort, Open-Label Study to Evaluate the Safety and Efficacy of Cretostimogene Grenadenorepvec in Participants with High-Risk Non-Muscle-Invasive Bladder Cancer.
开始日期2024-09-16 |
申办/合作机构 |
NCT06111235
A Phase 3, Randomized Study of Adjuvant Cretostimogene Grenadenorepvec Versus Observation for the Treatment of Intermediate Risk Non-Muscle Invasive Bladder Cancer (IR-NMIBC) Following Transurethral Resection of Bladder Tumor (TURBT)
This is a Phase 3, open-label, randomized trial designed to evaluate the RFS of TURBT followed by cretostimogene grenadenorepvec versus TURBT followed by observation for the treatment of participants with IR-NMIBC.
开始日期2023-12-14 |
申办/合作机构 |
CTR20231376
在卡介苗(BCG)无应答的非肌层浸润性膀胱癌患者中评价CG0070注射液局部多次给药的耐受性、安全性和初步疗效的单臂、开放、多中心、剂量递增Ⅰ期临床研究
评价溶瘤腺病毒CG0070多次给药(膀胱灌注)治疗BCG无应答的非肌层浸润性膀胱癌患者的安全性、耐受性,明确剂量限制性毒性(DLT)。
进一步确定CG0070多次给药最大耐受剂量(MTD)及推荐的II期临床剂量(RP2D)。
开始日期2023-11-14 |
申办/合作机构 |
100 项与 CG Oncology, Inc. 相关的临床结果
登录后查看更多信息
0 项与 CG Oncology, Inc. 相关的专利(医药)
登录后查看更多信息
4
项与 CG Oncology, Inc. 相关的文献(医药)2023-01-01·Methods in molecular biology (Clifton, N.J.)
Intravesical Infusion of Oncolytic Virus CG0070 in the Treatment of Bladder Cancer.
Article
作者: Moscu, Anay ; Grandi, Paola ; Darilek, Andrea ; Pradhan, Anu ; Li, Roger
2018-10-01·Urologic Oncology: Seminars and Original Investigations3区 · 医学
An open label, single-arm, phase II multicenter study of the safety and efficacy of CG0070 oncolytic vector regimen in patients with BCG-unresponsive non–muscle-invasive bladder cancer: Interim results
3区 · 医学
Article
作者: Packiam, Vignesh T ; Kroeger, Michael ; Trainer, Andrew ; Chamie, Karim ; Dumbadze, Igor ; Yeung, Alex W ; Steinberg, Gary D ; Kader, A Karim ; Clark, William ; Kuan, Arthur ; Davis, Ronald L ; Gutheil, John ; Lamm, Donald L ; Curran, Dominic ; Fand, Benjamin ; Barocas, Daniel A
Scientific Reports3区 · 综合性期刊
Myst2/Kat7 histone acetyltransferase interaction proteomics reveals tumour-suppressor Niam as a novel binding partner in embryonic stem cells
3区 · 综合性期刊
ArticleOA
作者: Bode, Daniel ; Skarnes, William ; Choudhary, Jyoti S ; Pardo, Mercedes ; Letney, Blake L ; Shen, Shihpei ; Tate, Peri ; Quelle, Dawn E ; Yu, Lu
280
项与 CG Oncology, Inc. 相关的新闻(医药)2025-04-29
▎Armstrong2025年4月28日,CG Oncology在美国泌尿外科学会(AUA)年会上公布了溶瘤病毒疗法Cretostimogene(CG0070)单药治疗非肌层浸润性膀胱癌(NMIBC)三期临床BOND-3的最新数据。受此消息影响,CG Oncology当天股价大涨25%,目前市值达到21亿美元。Cretostimogene为一款工程化5型腺病毒溶瘤病毒,嵌入了两种编码基因-肿瘤选择性启动子E2F-1和GM-CSF基因,可以选择性地在Rb调控缺陷的肿瘤细胞内复制,最终裂解肿瘤细胞,进而释放肿瘤抗原以及GM-CSF,通过双重杀瘤作用可以将抗肿瘤活性最大化。Cretostimogene围绕NMIBC进行了全方位布局,覆盖70%以上的NMIBC患者,此次更新的是三期临床BOND-3的数据,包括Cohort C和Cohort P。Cohort C针对高危、卡介苗不响应的伴原位癌(CIS)患者,Cohort P针对高危、卡介苗不响应Ta/T1患者,Cohort C取得NMIBC历史最佳的持久性疗效数据,同时没有发生3级及以上副作用,Cohort P则表现出有潜力的初步疗效信号。BOND-03的临床方案设计如下,Cohort C共入组112例对BCG无应答的高危NMIBC CIS患者,主要终点为任何时间的CR率,次要终点包括12个月CR率、DoR、PFS等。Cohort P入组75例BCG无应答的高危NMIBC Ta/T1患者,主要终点为任何时间的CR率,次要终点包括RFS、PFS等。Cohort C入组的多为经过多线治疗的患者,41.1%的患者接受过化疗。主要终点任何时间CR率为75.5%,12个月CR率为50.7%,24个月CR率为42.3%。24个月时,97.3%的患者没有进展到MIBC,响应患者中91.3%的患者避免了根治性膀胱切除术。24个月持续响应率达到58.3%,Cretostimogene的mDoR尚未达到,超过28个月,这也是NMIBC的历史最佳数据。在获得优异疗效的情况下,Cretostimogene的安全性表现十分出色,没有3级及以上副作用,没有停药事件。Cretostimogene获得了NMIBC疾病历史最佳疗效数据,同时也获得了最好的安全性数据,奠定了NMIBC基石疗法的地位。对于NMIBC Ta/T1患者,Cohort P同样表现出有潜力的疗效信号,3个月、6个月、9个月的RFS率均为90.5%。CG Oncology同时也在推进Cretostimogene的联合疗法,包括与PD-1抗体联用治疗卡介苗不响应的NMIBC患者,初步数据表明可以进一步提升疗效,以及与化疗联用治疗使用过卡介苗的NMIBC患者。总结CG0070的大中华区权益由乐普生物引入,CG Oncology在国外不断取得临床突破的同时,乐普生物也在同步积极推进国内的临床进展。乐普生物同时手握已上市的PD-1抗体普特利单抗可以形成互补,联合治疗NMIBC进一步提升疗效。乐普生物PD-1抗体已经获批上市,全球首创EGFR ADC已经处于上市审评阶段,引进的溶瘤病毒疗法CG0070也在三期临床中证实BIC地位,研发管线的全面开花,不断夯实乐普生物在大分子创新药领域的优势地位。Armstrong技术全梳理系列GPRC5D靶点全梳理;CD40靶点全梳理;CD47靶点全梳理;补体靶向药物技术全梳理;补体药物:眼科治疗的重要方向;Claudin 6靶点全梳理;Claudin 18.2靶点全梳理;靶点冷暖,行业自知;中国大分子新药研发格局;被炮轰的“me too”;佐剂百年史;胰岛素百年传奇;CUSBEA:风雨四十载;中国新药研发的焦虑;中国生物医药企业的研发竞争;中国双抗竞争格局;中国ADC竞争格局;中国双抗技术全梳理;中国ADC技术全梳理;Ambrx技术全梳理;Vir Biotech技术全梳理;Immune-Onc技术全梳理;亘喜生物技术全梳理;康哲药业技术全梳理;科济药业技术全梳理;恺佧生物技术全梳理;同宜医药技术全梳理;百奥赛图技术全梳理;腾盛博药技术全梳理;创胜集团技术全梳理;永泰生物技术全梳理;中国抗体技术全梳理;德琪医药技术全梳理;德琪医药技术全梳理2.0;和铂医药技术全梳理;荣昌生物技术全梳理;再鼎医药技术全梳理;药明生物技术全梳理;恒瑞医药技术全梳理;豪森药业技术全梳理;正大天晴技术全梳理;吉凯基因技术全梳理;基石药业技术全梳理;百济神州技术全梳理;百济神州技术全梳理第2版;信达生物技术全梳理;信达生物技术全梳理第2版;中山康方技术全梳理;复宏汉霖技术全梳理;先声药业技术全梳理;君实生物技术全梳理;嘉和生物技术全梳理;志道生物技术全梳理;道尔生物技术全梳理;尚健生物技术全梳理;康宁杰瑞技术全梳理;科望医药技术全梳理;岸迈生物技术全梳理;礼进生物技术全梳理;康桥资本技术全梳理;余国良的抗体药布局;荃信生物技术全梳理;安源医药技术全梳理;三生国健技术全梳理;仁会生物技术全梳理;乐普生物技术全梳理;同润生物技术全梳理;宜明昂科技术全梳理;派格生物技术全梳理;迈威生物技术全梳理;Momenta技术全梳理;NGM技术全梳理;普米斯生物技术全梳理;普米斯生物技术全梳理2.0;三叶草生物技术全梳理;贝达药业抗体药全梳理;泽璟制药抗体药全梳理;恒瑞医药抗体药全梳理;齐鲁制药抗体药全梳理;石药集团抗体药全梳理;豪森药业抗体药全梳理;华海药业抗体药全梳理;科伦药业抗体药全梳理;百奥泰技术全梳理;凡恩世技术全梳理。
临床结果临床3期临床2期突破性疗法
2025-04-29
·药研网
2025年4月28日,CG Oncology宣布,其创新基因治疗药物Cretostimogene Grenadenorepvec 在2025年美国泌尿科学会(AUA)年会上公布了最新III期临床试验BOND-003研究C队列的数据,数据表现卓越。受此消息影响,CG Oncology当天股价飙升25%。而其合作伙伴乐普生物今日上涨超7%!Cretostimogene grenadenorepvec 是一种具有双重作用机制的溶瘤免疫疗法,可选择性地复制和裂解癌细胞,同时增强对膀胱肿瘤的免疫反应。Cretostimogene grenadenorepvec 的作用机制有两种重要且互补的方式。首先,它在肿瘤细胞内复制,导致肿瘤细胞裂解和免疫原性细胞死亡。然后,癌细胞破裂后会释放肿瘤衍生抗原以及 GM-CSF,从而刺激全身免疫系统参与的抗肿瘤免疫反应。图源:CG Oncology官网此次BOND-003 C队列研究聚焦于高风险非肌层浸润性膀胱癌(NMIBC)患者,且均为对卡介苗(BCG)治疗无反应,伴有原位癌(CIS)及有无Ta/T1期病变。共入组112例。主要终点为任何时间的CR率,次要终点包括12个月CR率、DoR、PFS等。Cohort P入组75例BCG无应答的高危NMIBC Ta/T1患者,主要终点为任何时间的CR率,次要终点包括RFS、PFS等。研究截至2025年3月14日的数据如下:主要终点任意时间点完全缓解(CR)率高达75.5%。24个月时,完全缓解率达42.3%(Kaplan-Meier估计)中位持续缓解期(DOR)28个月且仍在延续中24个月时仅有2.7%患者发展为肌层浸润性膀胱癌,治愈率高达97.3%响应者中91.6%在24个月内避免了膀胱切除手术研究整体完成率高达97.3%此外,BOND-003 P队列(无CIS的Ta/T1病变患者)显示在3个月和9个月时局部高危肿瘤复发率低至9.5%,高危复发率自由生存(HG-RFS)达90.5%,且这是迄今规模最大的此类患者研究。安全性方面,cretostimogene grenadenorepvec表现极佳,无发生任何三级及以上相关不良事件,且不良反应中位恢复时长仅一天,显示出良好的耐受性和患者依从性。CG Oncology首席执行官表示,以上数据充分体现了cretostimogene grenadenorepvec在BCG无反应NMIBC中的最佳疗效及安全性,尤其是在长期维持缓解、膀胱功能保护方面显示了显著优势,满足了膀胱癌操作性免疫治疗市场的刚性需求。这一创新治疗有望成为膀胱癌治疗的核心骨干药物,极大改善患者生活质量,为公司商业化铺平道路。总结CG0070的大中华区权益由乐普生物引入,今年1月14日,乐普生物的溶瘤病毒疗法CG0070注射液已正式被CDE纳入突破性治疗,用于治疗对卡介苗(BCG)无应答的高危非肌层浸润性膀胱癌(NMIBC)患者。在国内,乐普生物正在开展一项Ⅰ期临床(CTR20231376),以在 BCG 无应答的非肌层浸润性膀胱癌患者中评价 CG0070 注射液局部多次给药的耐受性、安全性和初步疗效。End声明:本公众号所有发文章(包括原创及转载文章)系出于传递更多信息之目的,且注明来源和作者。本公众号欢迎分享朋友圈或大群,谢绝媒体或机构未经授权以任何形式转载至其他平台。转载/商务/投稿 | 联系微信15618157102(sum_Gmi)商务合作稿件征集点击了解详情往期回顾1关张、破产、裁员 | 2024年生物药企的阴影2全球第一款司美格鲁肽咀嚼软糖上市!3中国首个男性HPV疫苗获批上市!
免疫疗法临床3期临床2期临床结果
2025-04-29
·医药笔记
▎Armstrong2025年4月28日,CG Oncology在美国泌尿外科学会(AHA)年会上公布了溶瘤病毒疗法Cretostimogene(CG0070)单药治疗非肌层浸润性膀胱癌(NMIBC)三期临床BOND-3的最新数据。受此消息影响,CG Oncology当天股价大涨25%,目前市值达到21亿美元。Cretostimogene为一款工程化5型腺病毒溶瘤病毒,嵌入了两种编码基因-肿瘤选择性启动子E2F-1和GM-CSF基因,可以选择性地在Rb调控缺陷的肿瘤细胞内复制,最终裂解肿瘤细胞,进而释放肿瘤抗原以及GM-CSF,通过双重杀瘤作用可以将抗肿瘤活性最大化。Cretostimogene围绕NMIBC进行了全方位布局,覆盖70%以上的NMIBC患者,此次更新的是三期临床BOND-3的数据,包括Cohort C和Cohort P。Cohort C针对高危、卡介苗不响应的伴原位癌(CIS)患者,Cohort P针对高危、卡介苗不响应Ta/T1患者,Cohort C取得NMIBC历史最佳的持久性疗效数据,同时没有发生3级及以上副作用,Cohort P表现出有潜力的初步疗效信号。BOND-03的临床方案设计如下,Cohort C共入组112例对BCG无应答的高危NMIBC CIS患者,主要终点为任何时间的CR率,次要终点包括12个月CR率、DoR、PFS等。Cohort P入组75例BCG无应答的高危NMIBC Ta/T1患者,主要终点为任何时间的CR率,次要终点包括RFS、PFS等。Cohort C入组的多为经过多线治疗的患者,41.1%的患者接受过化疗。主要终点任何时间CR率为75.5%,12个月CR率为50.7%,24个月CR率为42.3%。24个月时,97.3%的患者没有进展到MIBC,响应患者中91.3%的患者避免了根治性膀胱切除术。24个月持续响应率达到58.3%,Cretostimogene的mDoR尚未达到,超过28个月,这也是NMIBC的历史最佳数据。在获得优异疗效的情况下,Cretostimogene的安全性表现十分出色,没有3级及以上副作用,没有停药事件。Cretostimogene获得了NMIBC疾病历史最佳疗效数据,同时也获得了最好的安全性数据,奠定了NMIBC基石疗法的地位。对于NMIBC Ta/T1患者,Cohort P同样表现出有潜力的疗效信号,3个月、6个月、9个月的RFS率均为90.5%。CG Oncology同时也在推进Cretostimogene的联合疗法,包括与PD-1抗体联用治疗卡介苗不响应的NMIBC患者,初步数据表明可以进一步提升疗效,以及与化疗联用治疗使用过卡介苗的NMIBC患者。总结CG0070的大中华区权益由乐普生物引入,CG Oncology在国外不断取得临床突破的同时,乐普生物也在同步积极推进国内的临床进展。乐普生物同时手握已上市的PD-1抗体普特利单抗可以形成互补,联合治疗NMIBC进一步提升疗效。乐普生物PD-1抗体已经获批上市,全球首创EGFR ADC已经处于上市审评阶段,引进的溶瘤病毒疗法CG0070也在三期临床中证实BIC地位,研发管线的全面开花,不断夯实乐普生物在大分子创新药领域的优势地位。Armstrong技术全梳理系列GPRC5D靶点全梳理;CD40靶点全梳理;CD47靶点全梳理;补体靶向药物技术全梳理;补体药物:眼科治疗的重要方向;Claudin 6靶点全梳理;Claudin 18.2靶点全梳理;靶点冷暖,行业自知;中国大分子新药研发格局;被炮轰的“me too”;佐剂百年史;胰岛素百年传奇;CUSBEA:风雨四十载;中国新药研发的焦虑;中国生物医药企业的研发竞争;中国双抗竞争格局;中国ADC竞争格局;中国双抗技术全梳理;中国ADC技术全梳理;Ambrx技术全梳理;Vir Biotech技术全梳理;Immune-Onc技术全梳理;亘喜生物技术全梳理;康哲药业技术全梳理;科济药业技术全梳理;恺佧生物技术全梳理;同宜医药技术全梳理;百奥赛图技术全梳理;腾盛博药技术全梳理;创胜集团技术全梳理;永泰生物技术全梳理;中国抗体技术全梳理;德琪医药技术全梳理;德琪医药技术全梳理2.0;和铂医药技术全梳理;荣昌生物技术全梳理;再鼎医药技术全梳理;药明生物技术全梳理;恒瑞医药技术全梳理;豪森药业技术全梳理;正大天晴技术全梳理;吉凯基因技术全梳理;基石药业技术全梳理;百济神州技术全梳理;百济神州技术全梳理第2版;信达生物技术全梳理;信达生物技术全梳理第2版;中山康方技术全梳理;复宏汉霖技术全梳理;先声药业技术全梳理;君实生物技术全梳理;嘉和生物技术全梳理;志道生物技术全梳理;道尔生物技术全梳理;尚健生物技术全梳理;康宁杰瑞技术全梳理;科望医药技术全梳理;岸迈生物技术全梳理;礼进生物技术全梳理;康桥资本技术全梳理;余国良的抗体药布局;荃信生物技术全梳理;安源医药技术全梳理;三生国健技术全梳理;仁会生物技术全梳理;乐普生物技术全梳理;同润生物技术全梳理;宜明昂科技术全梳理;派格生物技术全梳理;迈威生物技术全梳理;Momenta技术全梳理;NGM技术全梳理;普米斯生物技术全梳理;普米斯生物技术全梳理2.0;三叶草生物技术全梳理;贝达药业抗体药全梳理;泽璟制药抗体药全梳理;恒瑞医药抗体药全梳理;齐鲁制药抗体药全梳理;石药集团抗体药全梳理;豪森药业抗体药全梳理;华海药业抗体药全梳理;科伦药业抗体药全梳理;百奥泰技术全梳理;凡恩世技术全梳理。
临床结果AHA会议临床3期
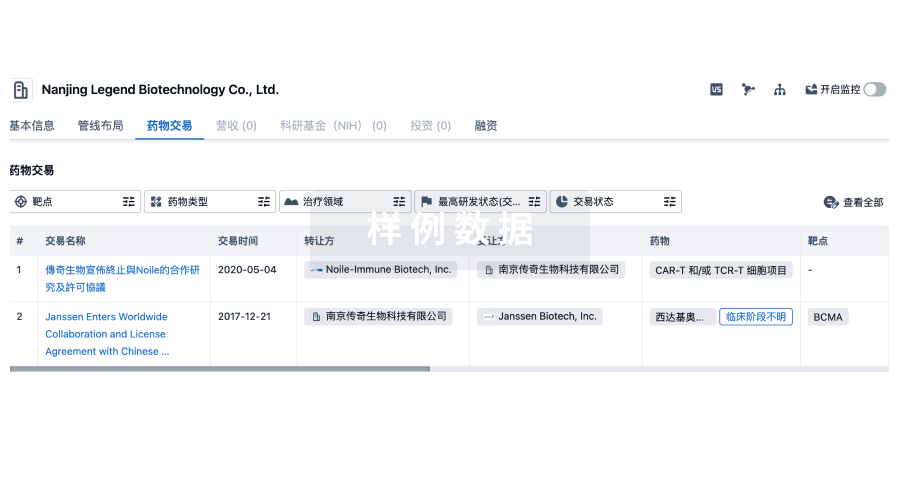
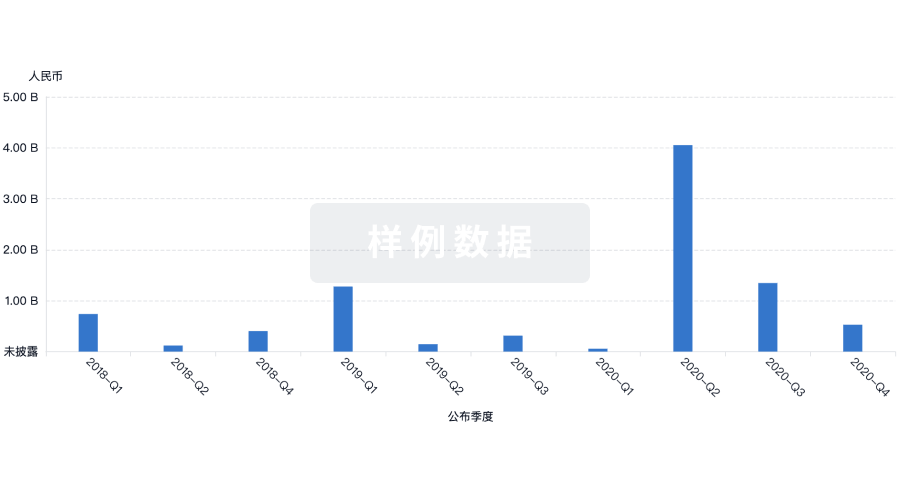
100 项与 CG Oncology, Inc. 相关的药物交易
登录后查看更多信息
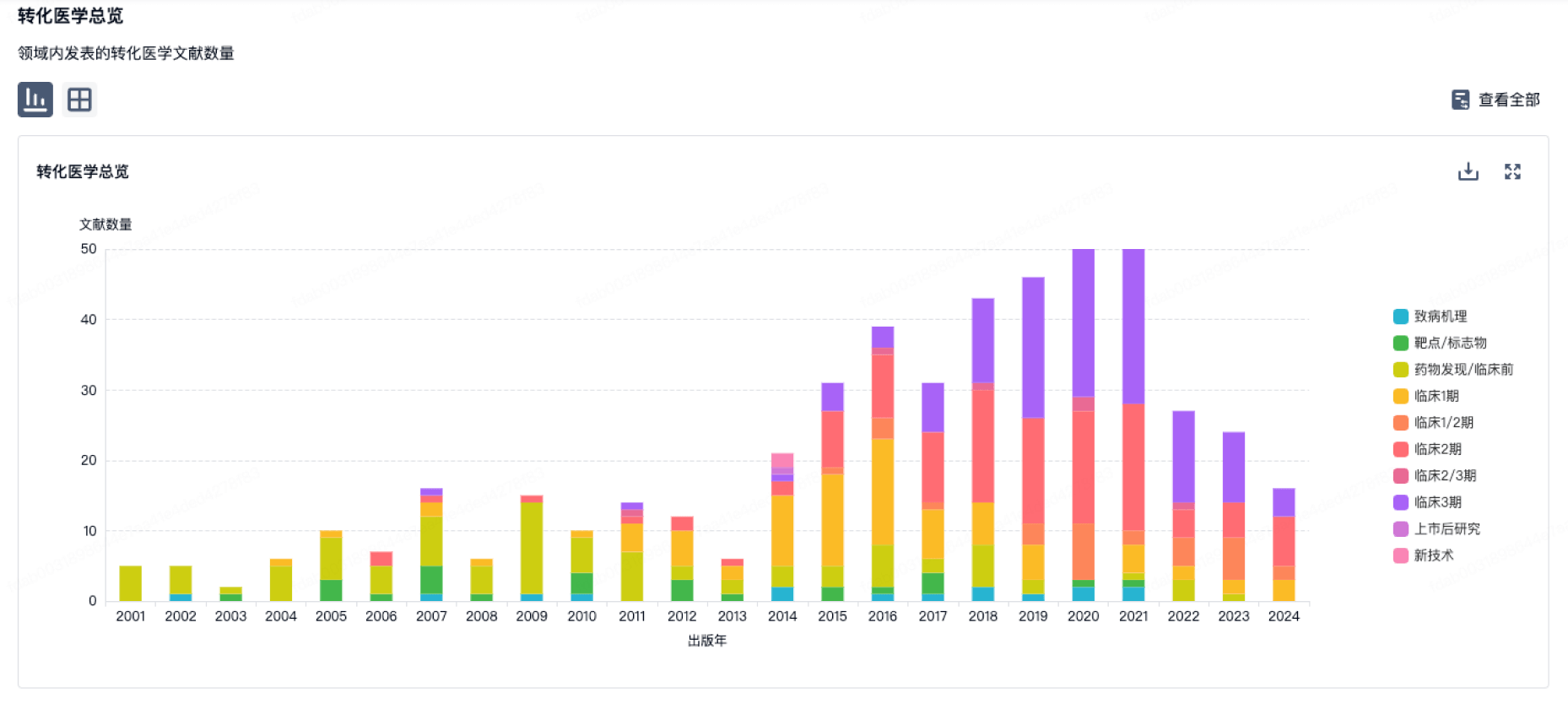
100 项与 CG Oncology, Inc. 相关的转化医学
登录后查看更多信息
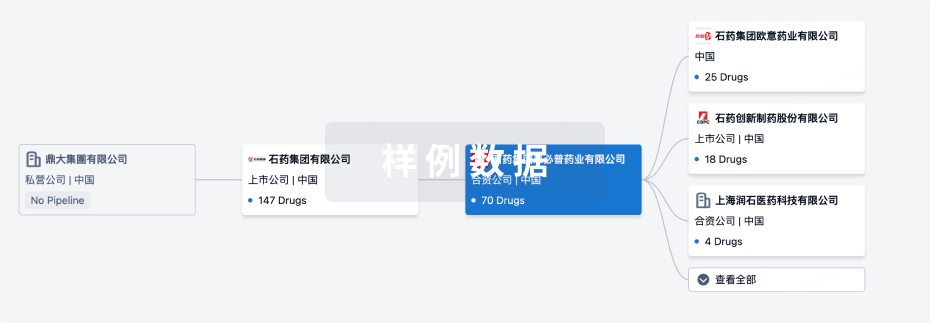
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年06月14日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床2期
1
1
临床3期
其他
1
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Cretostimogene Grenadenorepvec ( CSF-2R ) | 非肌层浸润性膀胱肿瘤 更多 | 临床3期 |
帕博利珠单抗 ( PD-1 ) | 非肌层浸润性膀胱肿瘤 更多 | 临床2期 |
丝裂霉素 | 原位癌 更多 | 终止 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
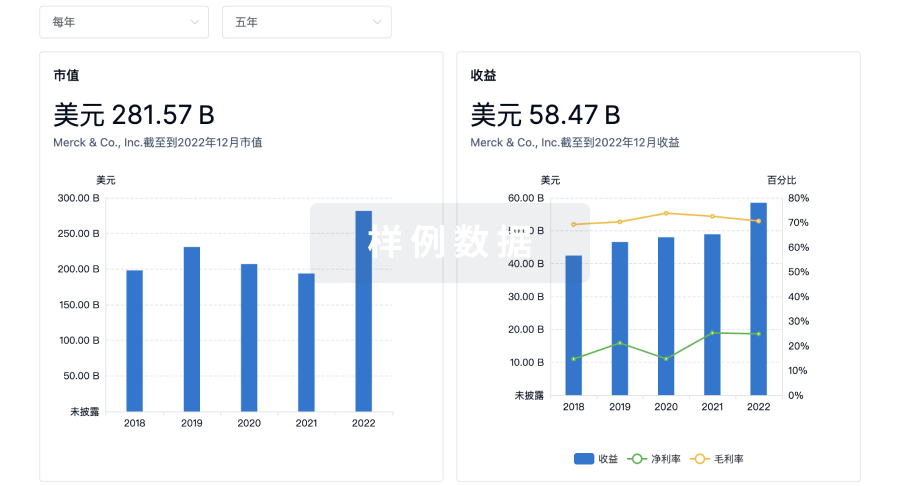
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
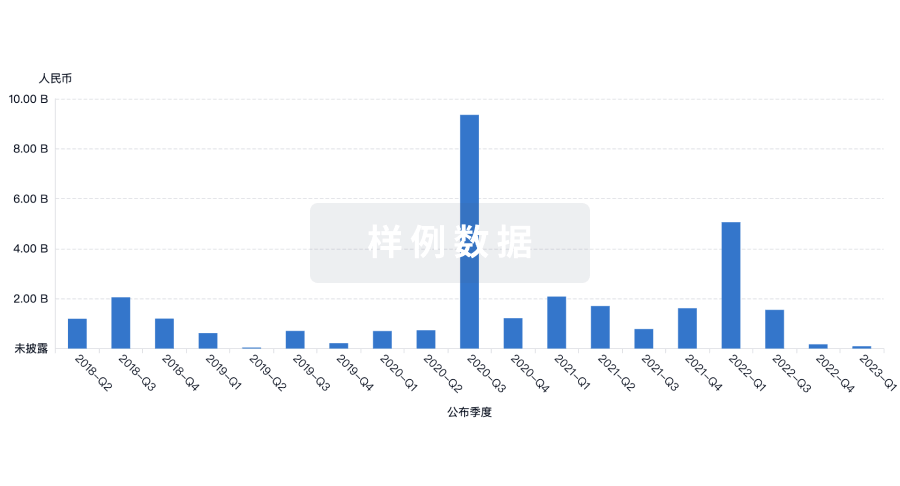
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


