预约演示
更新于:2025-05-07
GE Healthcare Ltd. (United Kingdom)
更新于:2025-05-07
概览
标签
肿瘤
其他疾病
神经系统疾病
小分子化药
诊断用放射药物
抗体偶联核素
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 诊断用放射药物 | 32 |
| 小分子化药 | 32 |
| 抗体偶联核素 | 5 |
| 核素偶联药物 | 4 |
| 化学药 | 4 |
关联
88
项与 GE Healthcare Ltd. (United Kingdom) 相关的药物作用机制 Mcl-1抑制剂 [+2] |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-09-27 |
靶点 |
作用机制 ERs拮抗剂 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2020-05-20 |
靶点 |
作用机制 KLK3抑制剂 |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2016-05-27 |
53
项与 GE Healthcare Ltd. (United Kingdom) 相关的临床试验ISRCTN17927667
A Phase IV, open-label, non-randomized, multicenter study to evaluate safety and efficacy of intravenous administration of Sonazoid™ for contrast-enhanced ultrasound liver imaging in paediatric patients
开始日期2024-07-29 |
申办/合作机构 |
NCT06129422
A Phase I Trial to Assess Safety, Tolerability, Pharmacokinetics, Radiation Dosimetry, and Positron Emission Tomography (PET) Imaging Properties of 89Zr-labeled hNd2 (NMK89) in Patients With Pancreatic Cancer Histologically Positive for MUC5AC
This trial will be a non-randomized, Phase I trial to evaluate safety, tolerability, biodistribution, radiation dosimetry, pharmacokinetics and PET imaging properties following an infusion of 37 MBq (1 mCi) of 89Zr-labeled hNd2* (NMK89) in patients with pancreatic cancer that are positive for MUC5AC. Image acquisition is conducted using a PET/CT machine.
* hNd2: Recombinant humanized Nd2 (anti-human MUC5AC monoclonal antibody)
* hNd2: Recombinant humanized Nd2 (anti-human MUC5AC monoclonal antibody)
开始日期2023-10-31 |
申办/合作机构 |
CTRI/2023/05/053235
A single-arm, multicentre, Post-marketing observational follow up on patients who have been given Gadolinium for clinical scans to detect all prospective adverse events immediately post dose and 6 (±2) weeks after administration of Omniscan
开始日期2023-06-05 |
申办/合作机构 |
100 项与 GE Healthcare Ltd. (United Kingdom) 相关的临床结果
登录后查看更多信息
0 项与 GE Healthcare Ltd. (United Kingdom) 相关的专利(医药)
登录后查看更多信息
308
项与 GE Healthcare Ltd. (United Kingdom) 相关的文献(医药)2025-04-22·JCI Insight
A toxic gain-of-function variant in MAPK8IP3 provides insights into JIP3 cellular roles
Article
作者: Nunes Bastos, Ricardo ; Crooke, Stanley T ; Zhang, Wei ; Mittal, Swapnil ; Foroughishafiei, Anahid ; Chung, Wendy K ; Skourti-Stathaki, Konstantina ; Thomas, Ria
2025-04-06·ICASSP 2025 - 2025 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP)
AAD-DCE: An Aggregated Multimodal Attention Mechanism for Early and Late Dynamic Contrast Enhanced Prostate MRI Synthesis
作者: Venkatesan, Ramesh ; Agarwal, Harsh ; Ramanarayanan, Sriprabha ; Sivaprakasam, Mohanasankar ; Ram, Keerthi ; M, Kishore Kumar ; Bharti, Divya ; S, Sadhana
2025-01-06·Molecular Pharmaceutics
Novel Radiotheranostic Ligands Targeting Prostate-Specific Membrane Antigen Based on Dual Linker Approach
Article
作者: Nakashima, Kazuma ; Tarumizu, Yuta ; Kazuta, Nobuki ; Maya, Yoshifumi ; Sato, Takumi ; Watanabe, Hiroyuki ; Ono, Masahiro
200
项与 GE Healthcare Ltd. (United Kingdom) 相关的新闻(医药)2025-04-29
·医药健闻
全球医疗行业每日重点资讯文 | 苏丁企业动态奥林巴斯公司(Olympus) 董事会一致决定任命美敦力前执行副总裁兼内外科产品组合总裁Bob White接替奥林巴斯董事、代表执行官、总裁兼首席执行官Yasuo Takeuchi,自2025年6月1日起生效。Bob还将在定于2025年6月举行的奥林巴斯股东大会上被提名为董事会候选人。在加入美敦力之前,Bob曾在GE医疗、Merge Healthcare和IBM医疗保健部门担任领导职务。德国医疗保健和材料集团默克(Merck KGaA)周一表示,已达成协议,将以39亿美元的股权价值收购美国生物技术公司SpringWorks Therapeutics,以加强其抗癌药物业务。SpringWorks总部位于美国康涅狄格州的斯坦福德,于2019年在纽约上市。该公司开发治疗癌症和罕见肿瘤的药物,目前在市场上有两种产品。诺和诺德(Novo Nordisk)取得了一场重大的法律胜利,这在很大程度上限制了配制药店营销或销售该制药商的畅销减肥药维格威(Wegovy)和糖尿病治疗药物奥泽美匹克(Ozempic)的更便宜且未经批准的仿制版本。得州联邦法官周四晚间作出关键裁决,驳回了复合药房行业协会的初步禁令申请,维持美国食品药品监督管理局(FDA)关于糖尿病药物Ozempic和减肥药Wegovy活性成分司美格鲁肽(semaglutide)“供应短缺状态已结束”的认定。安进(Amgen)正在加倍扩大其在美国的生产业务,并计划对其位于俄亥俄州中部的工厂进行重大升级。安进表示,该公司将投资9亿美元扩建其位于俄亥俄州新奥尔巴尼的生物制造工厂。该项目预计将使该州的安进的工作岗位总数达到750个,并将公司在俄亥俄州的总投资增加到14亿美元以上。艾伯维计划未来十年内在美国投资数十亿美元,目标是到2035年在美国投资100亿美元,以支持其当前的增长计划,并扩展到肥胖等新领域。这笔款项的一部分将专门用于建造四个新的美国生产设施,专门用于活性药物成分(API)、药品、肽和设备。赛默飞世尔科技(Thermo Fisher Scientific)表示,未来四年将在美国额外投资20亿美元。承诺的四分之三资金将支持赛默飞世尔的制造业务,而剩余的5亿美元将扩大其研发工作。赛默飞世尔已经拥有由64个美国工厂组成的广泛网络,覆盖37个州。该公司在其他43个国家也有业务。截至去年年底,该公司的全球员工人数约为125,000人,其中超过50,000人在美国工作。4月28日,恒瑞医药宣布,其发行H股计划正式获得中国证监会备案,拟发行不超过8.15亿股普通股赴港上市。这是继2000年A股上市后,恒瑞首次通过股权融资“补血”,也是其国际化战略的关键一步。依据此前披露的IPO计划,若成功登陆港股,恒瑞拟将募资20亿美元(约145亿元人民币)主要用于海外研发中心建设、全球多中心临床试验及国际化销售网络扩张。首药控股拟以自有及自筹资金不超过7.87亿元,在亦庄新城国际医药创新公园(BioPark)自主建设新的“首药控股新药研发与产业化基地”项目,并与北京经济技术开发区管委会签署《经济发展合作协议》。该合作协议生效后,公司将按照招拍挂供应程序取得项目宗地,建设包括研发中心、质控中心、临床试验中心、销售中心及生产基地在内的公司新总部,建设期3年。科源制药公告,拟收购山东宏济堂制药集团股份有限公司99.42%股权,交易作价约35.81亿元。同时拟定增募资不超7亿元。宏济堂是国内知名的阿胶产品生产企业。宏济堂与科源制药均为“力诺系”旗下公司,二者实控人均为高元坤。科源制药2023年4月登陆创业板上市,主要从事化学原料药及其制剂产品的研发、生产和销售。康弘药业公告,公司全资子公司北京康弘生物医药有限公司拟吸收合并北京弘健医疗器械有限公司、四川康弘中药材种植有限公司拟吸收合并成都康弘医药贸易有限公司、四川济生堂药业有限公司拟吸收合并四川济生堂兴尚生物科技有限责任公司。吸收合并后,北京康弘生物、康弘种植、济生堂存续经营,公司名称、股权结构保持不变。产业动态美敦力(Medtronic)宣布与Dragonfly Endoscopy达成战略合作,正式将后者研发的Dragonfly胰胆内窥镜系统引入美国市场。这一协议标志着胰胆疾病诊疗领域数十年来首次迎来重大技术升级。根据协议,美敦力将于2024年内率先在美国20家顶尖学术医疗中心及综合性医院启动Dragonfly系统的临床应用,未来三年逐步覆盖全美。美敦力宣布,其自主研发的全球最小直径无腔除颤导线OmniaSecure正式获得美国食品药品监督管理局(FDA)批准,用于右心室植入治疗危及生命的心律失常疾病。波士顿科学宣布,针对FARAPULSE脉冲电场消融(PFA)系统和辅助使用FARAPOINT PFA导管治疗持续性心房颤动(AF)患者的ADVANTAGE AF临床试验第二阶段达成12个月的主要安全性和有效性终点。该研究的主要结果已在圣地亚哥举行的第二届PFA现场手术峰会上公布,并同时在《Circulation》杂志上发表。益普生与上药控股有限公司达成战略合作协议。双方将围绕达菲林展开合作,通过加强资源整合和渠道覆盖,进一步推动达菲林产品在中国市场的深度覆盖。达菲林作为常用的促性腺激素释放激素类药物(GnRHa),在前列腺癌、中枢性性早熟、子宫内膜异位症、女性不孕症、子宫肌瘤的术前治疗等多种疾病中被广泛应用。复星医药控股子公司复宏汉霖与Alvogen Korea签订《许可协议》,复宏汉霖授予Alvogen Korea于许可区域(即韩国)及领域(即广泛期小细胞肺癌(ES-SCLC)、非鳞状非小细胞肺癌(nsNSCLC)、转移性结直肠癌(mCRC)、胃癌(GC)和食管鳞状细胞癌(ESCC)适应症)独家商业化斯鲁利单抗注射液的权利。Alvogen Korea应就许可产品向复宏汉霖支付至多1450万美元。基于许可产品于许可区域的年度净销售额达成情况,Alvogen Korea应依约向复宏汉霖支付至多9750万美元的商业销售里程碑款项。易瑞生物公告,公司与Chr. Hansen A/S(科汉森)签署合同,约定的2025-2029年度销售目标合计为7305.77万欧元,折合约6.01亿元人民币。合作内容包括公司在指定区域内授权科汉森独家销售、分销及推广公司产品,主要产品为乳中抗生素残留筛查测试、黄曲霉毒素M1筛查及定量测试、三聚氰胺及乳清掺假测试等。合同自2025年6月16日起生效,持续有效期为5年。以岭药业公告,公司全资孙公司万洋衡水制药有限公司提交的“来曲唑”化学原料药上市申请已获国家药品监督管理局批准。来曲唑是一种高效、选择性非甾体类芳香化酶抑制剂,用于乳腺癌治疗。君实生物宣布,由公司自主研发的抗PD-1单抗药物特瑞普利单抗注射液(拓益®)用于不可切除或转移性黑色素瘤的一线治疗的新适应症上市申请于近日获得国家药品监督管理局(NMPA)批准。这是特瑞普利单抗在中国内地获批的第12项适应症。信达生物宣布,第三代表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKI)靶向药物奥壹新(利厄替尼片)的新药上市申请获得国家药品监督管理局批准,用于具有表皮生长因子受体(EGFR)外显子19缺失(19DEL)或外显子21置换突变(L858R)的局部晚期或复发转移性非小细胞肺癌(NSCLC)成人患者的一线治疗。奥壹新(利厄替尼片)是目前唯一获批上市的,以萘胺结构为基础的第三代EGFR-TKI药物。清华人工智能医院正式揭牌成立,建设将分阶段进行,初期将在清华AI全面布局和多学科医工交叉的基础上,建设AI医院系统,依托北京清华长庚医院及北京清华长庚互联网医院试运行,以全科医学科和眼科、放射诊断科、呼吸科等专科为试点。未来,将构建“AI+医疗+教育+科研”生态闭环,促进优质医疗资源的高效扩容与均衡布局。联系美通社+86-10-5953 9500info@prnasia.com
高管变更IPO并购
2025-04-25
·生物谷
1. 全球TOP100:12家中国器械公司入榜近日,海外医疗器械网站Medical Device and Diagnostic industry发布了全球医疗器械企业TOP 100排名。按照2024年度企业营收情况,进入前十名榜单的企业分别为美敦力、强生、雅培、丹纳赫、Medline Industries、史赛克、西门子医疗、BD医疗、GE医疗、飞利浦。在本次全球TOP100的企业中,有12家中国医疗器械企业入选挺进全球百强。具体包括迈瑞医疗、威高集团、联影医疗、新华医疗、英科医疗、鱼跃医疗、微创医疗、中国同辐、乐普医疗、蓝帆医疗、东富龙科技、安图生物。2. “药王”K药皮下注射版侵权?Halozyme把默沙东告了Halozyme起诉默沙东,指控其K药皮下注射版侵犯多项专利,涉及关键技术酶,可能影响K药未来市场和营收,Halozyme要求高额销售额分成。3. 这款医疗器械国补30%爆卖,无惧关税冲击在沉睡的睡眠健康市场,一款家用医疗器械在电商平台爆卖。得益于最高30%的“国补”,家用无创呼吸机在电商平台销售量大增,怡和嘉业(呼吸机品牌为瑞迈特,目前已经启动公司名和证券简称统一更名为瑞迈特的工作)董事长在采访中表示国补政策对于呼吸机销量提升明显。此前,家用呼吸机在国内渗透率不足1%,国补是家用无创呼吸机市场的助燃剂,随着大众对家用无创呼吸机认知加深,这一市场增长表现亮眼。鱼跃医疗也在半年报中表示,家用呼吸机产品业务规模实现了较好增长。家用呼吸机市场蛋糕在变大,国内企业分到的份额也在变大。根据沙利文数据,2019年,国产龙头瑞迈特的国内市场份额还只有6.1%,2023年已经增加到30.6%。过去,由于国内市场容量有限,国内头部家用呼吸机企业海外市场收入反而比国内高。根据中国海关数据,2024年无创呼吸机出口金额高达27.17亿元。但在关税政策变化背景下,国内市场增长确定性更强。4. 一个月,顶刊+6,浙大医学创新生态催生全球医学突破新动能浙大医学院一个月内在顶刊发表6篇论文,涵盖多种疾病研究。学院鼓励原创探索与跨学科合作,创建良好学术生态,推动基础医学突破和前沿技术转化。其中,徐浩新团队发现溶酶体新氢离子通道,对帕金森病研究有重要意义。5. 这5家高校获批设立合成生物学本科专业教育部批准长治学院、淮阴师范学院、武汉轻工大学、湖南文理学院、深圳理工大学五所高校设立合成生物学本科专业。至此,国内有11家高校开设此专业。6. 荣昌生物获得上百家机构调研,核心管线开发进展成关注焦点荣昌生物获上百家机构调研,关注其核心管线开发进展。RC18、RC48国内外研发进展顺利,涉及多个治疗领域,公司财务状况有所改善,净亏损同比缩小。本文仅用于学术分享,转载请注明出处。若有侵权,请联系微信:bioonSir 删除或修改!
专利侵权
2025-04-14
·氨基观察
©氨基观察-创新药组原创出品作者 | 黄恺男性也可以打HPV疫苗了。4月14日,默沙东宣布,九价HPV疫苗多项新适应证已获得国家药品监督管理局的上市批准,适用于16~26岁男性接种。相比之下,国产疫苗慢了一拍。同日,万泰生物公告称,近日,九价HPV疫苗已经启动男性III期临床试验,并完成首例受试者入组。辉瑞再次饮恨减肥药。4月14日,辉瑞宣布,终止开发口服胰高血糖素样肽-1受体(GLP-1R)激动剂Danuglipron(PF-06882961)。在过去的一天里,国内外医药市场还有哪些热点值得关注?让氨基君带你一探究竟。/ 01 /市场速递1)上海:对医疗机构执业行为、药品器械流通、医保基金使用等实施穿透式监管4月14日,上海市政府常务会议指出,医疗卫生服务新业态、新模式不断涌现,要完善医疗卫生行业综合监管制度,以严的基调深化全面监管,从事后处置转向全过程监管,依托人工智能、大数据、区块链等技术,对医疗机构执业行为、药品器械流通、医保基金使用等实施穿透式监管,切实保障群众合法权益。2)GE医疗:对中国市场的承诺不变4月14日,对于美国关税政策影响,美国医疗器械厂商GE医疗表示,公司在中国市场已运营超过100年的历史,拥有很强的本土化布局和国产创新实力。公司在中国销售的绝大多数产品已经实现在中国境内生产。“公司对中国市场的承诺保持不变,将继续致力于为客户和病患提供服务。”/ 02 /医药动态1)百利药业注射用BL-B01D1获临床许可4月14日,据CDE官网,百利药业注射用BL-B01D1获临床许可,拟联合仑伐替尼治疗晚期肝癌。2)万泰生物九价HPV疫苗启动男性III期临床试验并完成首例受试者入组4月14日,万泰生物公告称,近日,九价HPV疫苗已经启动男性III期临床试验,并完成首例受试者入组。3)默沙东九价HPV疫苗获批男性适应证4月14日,默沙东宣布,九价HPV疫苗多项新适应证已获得国家药品监督管理局的上市批准,适用于16~26岁男性接种。4)兴和制药PPARα激动剂佩玛贝特片获批4月14日,据NMPA官网,兴和制药PPARα激动剂佩玛贝特片在正式获批,适应症为治疗血脂异常。/ 03 /器械跟踪1)微创旋律冠状动脉棘突球囊扩张导管获注册批件4月14日,据NMPA官网,微创旋律冠状动脉棘突球囊扩张导管获注册批件。2)长木谷医疗髋关节置换手术导航系统获注册批件4月14日,据NMPA官网,长木谷医疗髋关节置换手术导航系统获注册批件。/ 04 /数字医疗日报1)蚂蚁集团未来一年内将打造百位名医智能体矩阵4月14日,蚂蚁集团宣布发起“百大AI名医”计划,未来一年内,其将为全国百大名医打造AI分身(AI智能体),形成覆盖肿瘤、慢病等领域的智能体矩阵,从而缓解名医资源紧缺等问题,让患者有机会随时随地获取名医服务。/ 05 /海外药闻1)辉瑞终止开发口服GLP-1药物4月14日,辉瑞宣布,终止开发口服胰高血糖素样肽-1受体(GLP-1R)激动剂Danuglipron(PF-06882961)。2)口服Aβ抑制剂III期研究失败4月10日,Alzheon公布了口服Aβ抑制剂Valiltramiprosate治疗早期阿尔茨海默病患者的关键性III期APOLLOE4研究的结果。结果显示,治疗第78周,在总人群中,该研究未达到主要终点。PS:欢迎扫描下方二维码,添加氨基君微信号交流。
临床3期疫苗上市批准
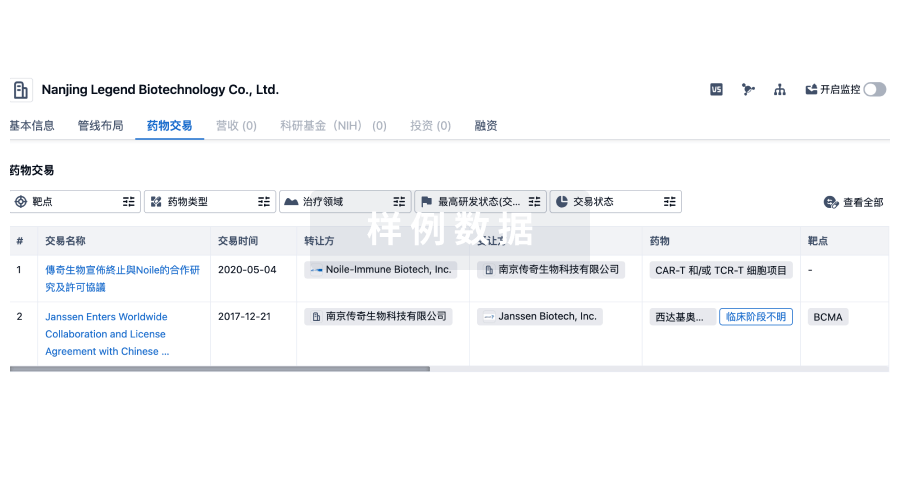
100 项与 GE Healthcare Ltd. (United Kingdom) 相关的药物交易
登录后查看更多信息
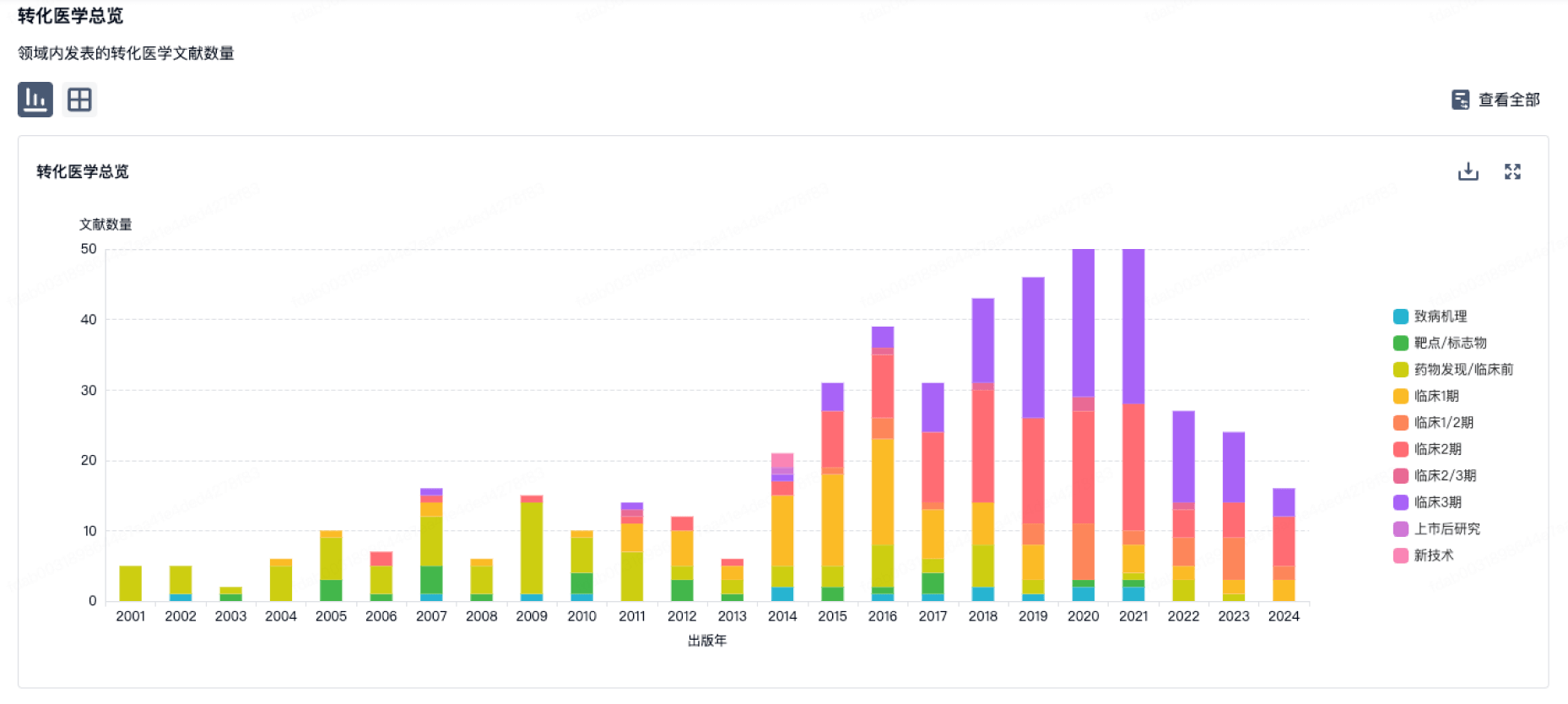
100 项与 GE Healthcare Ltd. (United Kingdom) 相关的转化医学
登录后查看更多信息
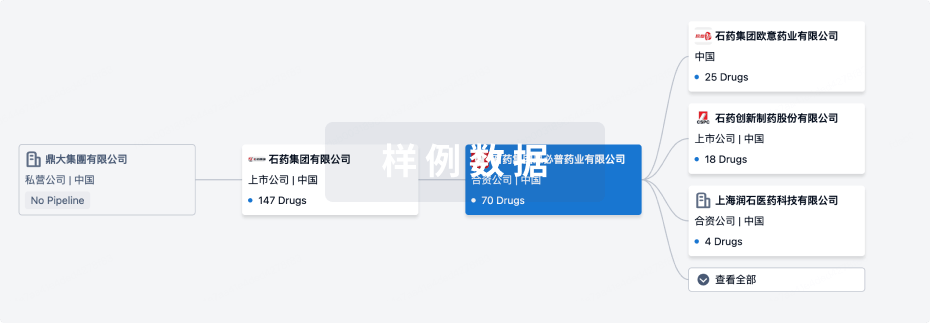
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月23日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
5
6
临床前
临床1期
1
2
临床2期
批准上市
35
39
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
碘[123I]苄胍 | 心脏衰竭 更多 | 批准上市 |
枸橼酸镓[67Ga] | 肿瘤 更多 | 批准上市 |
Flurpiridaz F 18 ( Mcl-1 x NQO1 ) | 冠心病 更多 | 批准上市 |
Technetium(99mTc) N-pyridoxyl-5-methyltryptophan | 肝病 更多 | 批准上市 |
Sodium Pertechnetate (99mTc) | 脑癌 更多 | 批准上市 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
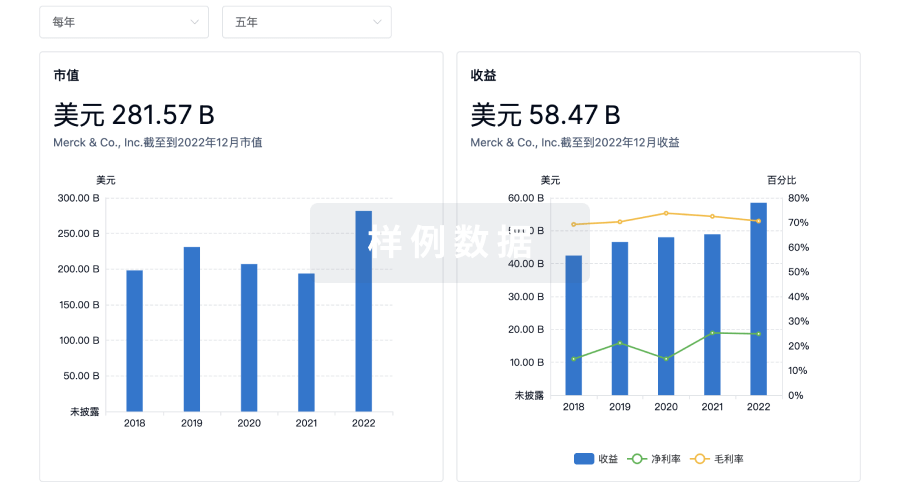
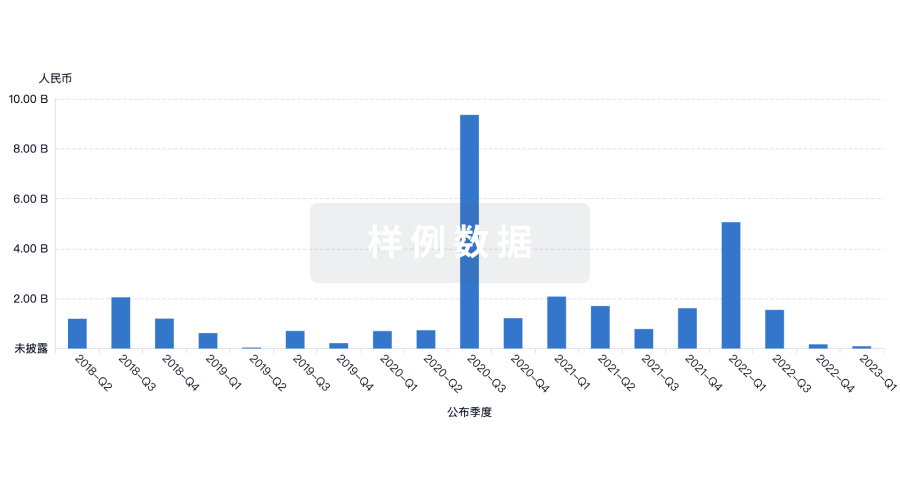
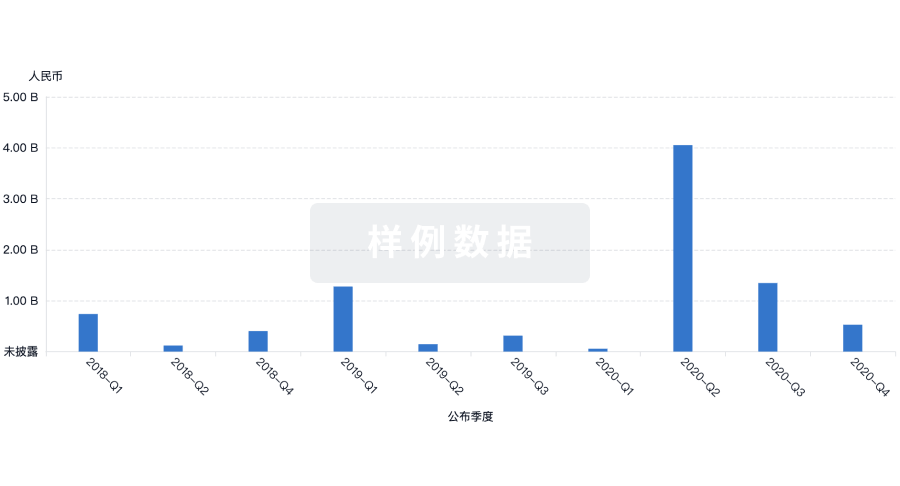
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用