预约演示
更新于:2025-08-27

Scilex Pharmaceuticals, Inc.
更新于:2025-08-27
概览
标签
神经系统疾病
其他疾病
皮肤和肌肉骨骼疾病
小分子化药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 4 |
关联
4
项与 Scilex Pharmaceuticals, Inc. 相关的药物作用机制 Opioid receptors拮抗剂 [+1] |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2006-04-13 |
靶点 |
作用机制 COX-2抑制剂 |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期1998-12-31 |
靶点 |
作用机制 微管蛋白抑制剂 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期1995-01-01 |
15
项与 Scilex Pharmaceuticals, Inc. 相关的临床试验NCT05096494
A Phase 2, Randomized, Double-blind, Placebo-controlled, Parallel Group, Multicenter Study to Evaluate the Safety and Efficacy of SP-103 in Subjects With Moderate to Severe Acute Lower Back Pain
This is a Phase 2, randomized, double-blind, placebo-controlled, parallel group, multicenter study to evaluate the safety and efficacy of SP-103 in subjects with moderate to severe acute lower back pain.
开始日期2022-04-29 |
申办/合作机构 |
NCT05002946
Phase 1, Open Label, Randomized, Single-dose, 3-Period, 3-Treatment Crossover Study to Evaluate the Pharmacokinetics of SP-104 Under Fasting and Fed Conditions and to Compare to Naltrexone Hydrochloride Tablets USP in Healthy Adult Subjects
This open-label, 3-period, 3-treatment, randomized study will characterize the pharmacokinetics and safety and tolerability of SP-104 under fasting and fed conditions as compared to the pharmacokinetics of Naltrexone Hydrochloride Tablets, USP, 50 mg in healthy adult subjects.
开始日期2022-01-11 |
申办/合作机构 |
NCT04958876
Phase 1, Double-blind, Randomized, 2-Period, 2-Treatment Crossover Study to Evaluate the Safety of SP-104 Compared to Immediate Release Naltrexone Capsules in Healthy Adult Subjects
Evaluate the safety and tolerability of 3-day repeat-dose of SP-104 compared to naltrexone hydrochloride immediate release.
开始日期2021-10-04 |
申办/合作机构 |
100 项与 Scilex Pharmaceuticals, Inc. 相关的临床结果
登录后查看更多信息
0 项与 Scilex Pharmaceuticals, Inc. 相关的专利(医药)
登录后查看更多信息
10
项与 Scilex Pharmaceuticals, Inc. 相关的文献(医药)2021-09-01·The Clinical journal of pain3区 · 医学
Safety of Epidural Steroid Injections for Lumbosacral Radicular Pain
3区 · 医学
Article
作者: Vought, Kip ; Cohen, Steven P. ; Greuber, Emileigh ; Lissin, Dmitri
Objective::
Epidural steroid injections (ESIs) are a commonly utilized treatment for lumbosacral radicular pain caused by intervertebral disc herniation or stenosis. Although effective in certain patient populations, ESIs have been associated with serious complications, including paralysis and death. In 2014, the US Food and Drug Administration (FDA) issued a safety warning on the risk of injecting corticosteroids into the epidural space. The aims of this article were to review the neurological complications associated with ESIs and to compare the formulations, safety, and effectiveness of commercially available corticosteroids given by transforaminal, interlaminar, or caudal injection.
Methods::
Serious adverse events associated with ESIs were identified by a search of the FDA Adverse Event Reporting System (FAERS) database. A MEDLINE search of the literature was conducted to identify clinical trials comparing the safety and effectiveness of nonparticulate and particulate corticosteroid formulations.
Results::
Neurological complications with ESIs were rare and more often associated with the use of particulate corticosteroids administered by transforaminal injection. Among the 10 comparative-effectiveness studies reviewed, 7 found nonparticulate steroids had comparable efficacy to particulate steroids, and 3 studies suggested reduced efficacy or shorter duration of effect for nonparticulate steroids.
Discussion::
The risk of complications for transforaminal ESI is greater with particulate corticosteroids. Nonparticulate corticosteroids, which are often recommended as first-line therapy, may have a short duration of effect, and many commercial formulations contain neurotoxic preservatives. The safety profile of ESIs may continue to improve with the development of safer, sterile formulations that reduce the risk of complications while maintaining efficacy.
2021-08-01·AAPS PharmSciTech3区 · 医学
Biorelevant In Vitro Skin Permeation Testing and In Vivo Pharmacokinetic Characterization of Lidocaine from a Nonaqueous Drug-in-Matrix Topical System
3区 · 医学
Article
作者: Vought, Kip ; Lissin, Dmitri ; Suzuki, Hiroaki ; Greuber, Emileigh ; Koplowitz, Barry ; Koplowitz, Luana Pesco ; Patel, Kalpana ; Shiramizu, Akira ; Usuda, Kazuhiro ; Maibach, Howard I
Abstract:
Recently, lidocaine topical systems utilizing nonaqueous matrices have been developed and provide efficient lidocaine delivery through the skin, such that lower concentrations of drug provide equivalent or greater drug delivery than drug-in-matrix hydrogel lidocaine patches. This study characterizes drug delivery from a nonaqueous lidocaine topical system with increasing drug load both in vitro and in vivo. Topical systems formulated with either 1.8% or 5.4% lidocaine were applied to healthy volunteers’ backs (n = 15) for 12 h in a single-center, open-label, four-treatment, four-period crossover pharmacokinetic study. Subjects were dosed with either three 1.8% systems or one, two, or three 5.4% systems in each period. Blood was collected for up to 48 h, and plasma lidocaine levels were measured with a validated HPLC method. In parallel, human and mouse skin models characterized the in vitro skin permeation profile. The pharmacokinetic profile was linear between one, two, and three lidocaine 5.4% applications. Application of three lidocaine 1.8% systems (108 mg lidocaine) was bioequivalent to one lidocaine 5.4% system (108 mg lidocaine). Both topical systems remained well adhered to the skin and irritation was mild. The 5.4% system had approximately threefold higher skin permeability than the 1.8% system in the mouse and human skin models. The results indicate increasing the drug load by three times results in triple the drug delivery both in vivo and in vitro. The relationship between the in vitro permeation and in vivo absorption correlates and is nonlinear.
2020-11-01·Pain1区 · 医学
Interpretation of chronic pain clinical trial outcomes: IMMPACT recommended considerations
1区 · 医学
Article
作者: Steigerwald, Ilona ; Bhagwagar, Zubin ; Schoenfeld, David ; Markman, John D ; Wasan, Ajay D ; Tobias, Jeffrey ; Dworkin, Robert H ; Singh, Jasvinder ; Tive, Leslie A ; Katz, Nathaniel P ; Cowan, Penney ; Farrar, John T ; Smith, Shannon M ; Lissin, Dmitri ; Wilson, Hilary D ; Evans, Scott R ; Kopecky, Ernest A ; Jensen, Mark P ; Turk, Dennis C ; Ellenberg, Susan S ; Strand, Vibeke ; Mease, Philip J ; Freeman, Roy L ; Iyengar, Smriti ; Kesslak, James Patrick ; Patel, Kushang V ; Kamp, Cornelia ; Burke, Laurie B ; Sampaio, Cristina ; Raja, Srinivasa N ; O'Connor, Alec B ; Jadad, Alejandro ; Junor, Roderick ; Garrison, Louis P ; McDermott, Michael P ; Eccleston, Christopher ; Rowbotham, Michael C
Abstract:
Interpreting randomized clinical trials (RCTs) is crucial to making decisions regarding the use of analgesic treatments in clinical practice. In this article, we report on an Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) consensus meeting organized by the Analgesic, Anesthetic, and Addiction Clinical Trial Translations, Innovations, Opportunities, and Networks, the purpose of which was to recommend approaches that facilitate interpretation of analgesic RCTs. We review issues to consider when drawing conclusions from RCTs, as well as common methods for reporting RCT results and the limitations of each method. These issues include the type of trial, study design, statistical analysis methods, magnitude of the estimated beneficial and harmful effects and associated precision, availability of alternative treatments and their benefit–risk profile, clinical importance of the change from baseline both within and between groups, presentation of the outcome data, and the limitations of the approaches used.
156
项与 Scilex Pharmaceuticals, Inc. 相关的新闻(医药)2025-08-21
Plus, news about Benchling, Invivyd, Immuneering, Scilex and Sana Biotechnology:
📉
Sarepta’s debt refinancing:
The biotech, which went through a complicated exchange with the FDA this summer over the safety of its Duchenne gene therapy, will extend its debt from 2027
to 2030
to improve its finances. “By extending the maturity of a meaningful portion of our convertible notes to 2030, we have completed a shareholder-friendly transaction,” CEO Doug Ingram said in a statement. Last week, the company had to
sell its stock position
in Arrowhead Pharmaceuticals to be able to pay a milestone fee to Arrowhead, which has siRNA programs that could drive the future of Sarepta’s pipeline under a
$10 billion biobuck pact
.
— Kyle LaHucik
🏭
As expected, Regeneron says FDA decisions on Eylea HD are delayed:
The regulator
pushed back
two decisions on Eylea’s high-dose formulations to the fourth quarter. The original decision date was Aug. 19. Regeneron is seeking approval for a pre-filled syringe, treatment for macular edema following retinal vein occlusion, and a broader dosing schedule for all indications.
It
previously disclosed
that it expected delays following an inspection of a third-party manufacturer site in Indiana, formerly owned by Catalent and now part of Novo Nordisk.
Scholar Rock
, another customer of the Indiana site, has said it doesn’t expect any PDUFA delays for its experimental spinal muscular atrophy drug called apitegromab. —
Anna Brown
💻
Benchling’s two deals:
The life sciences software startup “acquired the teams” of ReSync Bio and Sphinx Bio. The startups create “AI tools that power scientific workflows,” Benchling said. Earlier this year, Benchling
laid off 10%
of its staff. The San Francisco-based company partners with biopharmas like Merck and Moderna on AI research, bioanalytics and other functions. It raised a
$100 million Series F
in 2021.
— Kyle LaHucik
💰
Invivyd’s $50M stock sale:
The company, which has an authorized Covid-19 prevention drug called Pemgarda,
is selling
21.3 million shares at 52 cents apiece.
— Jaimy Lee
🏥 Immuneering gets $25M from PIPE:
The company
said
it expects to share updated overall survival and progression-free survival data from its Phase 2a trial of atebimetinib in pancreatic cancer “in the coming weeks.”
— Jaimy Lee
💵 Scilex raises $20M for Phase 3 trial:
Semnur Pharmaceuticals, Scilex’s parent company, and Denali Capital
inked
the private placement with an unnamed investor to help advance Scilex’s SP-102 into a second Phase 3 trial for lumbar radicular pain, or sciatica.
— Jaimy Lee
💸
Sana Biotechnology
ended up
raising $86.3 million, up from the $75.0 million it
intended
to bring in.
— Jaimy Lee
临床2期并购临床3期
2025-08-13
Denali’s registration statement on Form S-4 declared effective by the Securities and Exchange CommissionExtraordinary general meeting of Denali Capital Acquisition Corp. shareholders to approve the proposed business combination is scheduled to be held on September 3, 2025, at 9:00 a.m., Eastern TimePost-closing combined company will be renamed "Semnur Pharmaceuticals, Inc." in connection with the closing of the business combination PALO ALTO, Calif., Aug. 13, 2025 (GLOBE NEWSWIRE) -- Scilex Holding Company (“Scilex” or the “Company”) (Nasdaq: SCLX) , an innovative revenue-generating company focused on acquiring, developing and commercializing non-opioid pain management products for the treatment of acute and chronic pain and neurodegenerative and cardiometabolic disease, today announced that the registration statement on Form S-4 (the “Registration Statement”), related to the previously announced proposed business combination (the “Business Combination”) between Denali Capital Acquisition Corp. ("Denali") (OTCB: DNQAF), a special purpose acquisition company, and Semnur Pharmaceuticals, Inc. (“Semnur”), a majority-owned subsidiary of Scilex, has been declared effective by the U.S. Securities and Exchange Commission (the "SEC"). Denali will hold an extraordinary general meeting of shareholders (the “Meeting”) at 9:00 a.m., Eastern Time on Wednesday, September 3, 2025 to approve, among other things, the proposed Business Combination. Shareholders of record of Denali at the close of business on August 12, 2025 will be entitled to receive notice of, and to vote at, the Meeting. The Meeting will be held at the offices of US Tiger Securities, Inc. located at 437 Madison Avenue, 27th Floor, New York, New York 10022. The Business Combination is expected to close as soon as reasonably practicable after approval by Denali’s and Semnur’s shareholders and the satisfaction of other customary closing conditions as described in the Registration Statement. While the combined company has submitted an application to list the combined company’s common stock and warrants on The Nasdaq Stock Market LLC, approval has not yet been obtained and there can be no assurance that such listing application will be approved or that the combined company will meet the applicable listing standards. If the combined company is unable to obtain listing on a national securities exchange, the combined company’s securities will continue to trade on the OTC Markets following the Business Combination. For more information on Scilex Holding Company, refer to www.scilexholding.com For more information on Semnur Pharmaceuticals, Inc., refer to www.semnurpharma.com For more information on ZTlido® including Full Prescribing Information, refer to www.ztlido.com. For more information on ELYXYB®, including Full Prescribing Information, refer to www.elyxyb.com. For more information on Gloperba®, including Full Prescribing Information, refer to www.gloperba.com. https://www.facebook.com/scilex.pharm https://www.linkedin.com/company/scilex-holding-company/ info@scilexholding.com About Scilex Holding Company
Scilex is an innovative revenue-generating company focused on acquiring, developing and commercializing non-opioid pain management products for the treatment of acute and chronic pain and neurodegenerative and cardiometabolic disease. Scilex targets indications with high unmet needs and large market opportunities with non-opioid therapies for the treatment of patients with acute and chronic pain and is dedicated to advancing and improving patient outcomes. Scilex’s commercial products include: (i) ZTlido® (lidocaine topical system) 1.8%, a prescription lidocaine topical product approved by the U.S. Food and Drug Administration (the “FDA”) for the relief of neuropathic pain associated with postherpetic neuralgia, which is a form of post-shingles nerve pain; (ii) ELYXYB®, a potential first-line treatment and the only FDA-approved, ready-to-use oral solution for the acute treatment of migraine, with or without aura, in adults; and (iii) Gloperba®, the first and only liquid oral version of the anti-gout medicine colchicine indicated for the prophylaxis of painful gout flares in adults. In addition, Scilex has three product candidates: (i) SP-102 (10 mg, dexamethasone sodium phosphate viscous gel) (“SEMDEXA” or “SP-102”), which is owned by Semnur and is a novel, viscous gel formulation of a widely used corticosteroid for epidural injections to treat lumbosacral radicular pain, or sciatica, for which Scilex has completed a Phase 3 study and was granted Fast Track status from the FDA in 2017; (ii) SP-103 (lidocaine topical system) 5.4%, (“SP-103”), a next-generation, triple-strength formulation of ZTlido, for the treatment of acute pain and for which Scilex has recently completed a Phase 2 trial in acute low back pain. SP-103 has been granted Fast Track status from the FDA in low back pain; and (iii) SP-104 (4.5 mg, low-dose naltrexone hydrochloride delayed-release capsules) (“SP-104”), a novel low-dose delayed-release naltrexone hydrochloride being developed for the treatment of fibromyalgia. Scilex is headquartered in Palo Alto, California. About Semnur Pharmaceuticals, Inc. Semnur is a clinical late-stage specialty pharmaceutical company focused on the development and commercialization of novel non-opioid pain therapies. Semnur’s product candidate, SP-102 (SEMDEXA™), is the first non-opioid novel gel formulation administered epidurally in development for patients with moderate to severe chronic radicular pain/sciatica. Semnur Pharmaceuticals, Inc. is headquartered in Palo Alto, California About Denali Capital Acquisition Corp. Denali is a blank check company formed for the purpose of effecting a merger, share exchange, asset acquisition, share purchase, reorganization or similar business combination with one or more businesses or entities. Important Information and Where to Find It This press release relates to a proposed transaction between Semnur and Denali and does not contain all the information that should be considered concerning the potential Business Combination and is not intended to form the basis of any investment decision or any other decision in respect of the potential Business Combination. The Registration Statement has been declared effective by the SEC, which includes the related proxy/prospectus of Denali (the “Proxy Statement/Prospectus”). Denali is mailing a definitive Proxy Statement/Prospectus and other relevant documents, including a proxy card, to the holders of record of Denali’s ordinary shares at the record date, August 12, 2025. This communication is not a substitute for the Registration Statement, the definitive Proxy Statement/Prospectus or any other document that Denali will send to its shareholders in connection with the Business Combination. Investors and security holders of Denali are urged to read these materials (including any amendments or supplements thereto) and any other relevant documents in connection with the transaction that Denali files with the SEC when, and if, they become available because they will contain important information about Denali, Semnur and the proposed transactions. The Proxy Statement/Prospectus and other relevant materials in connection with the transaction (when and if they become available), and any other documents filed by Denali with the SEC, may be obtained free of charge at the SEC’s website (www.sec.gov). The documents filed by Denali with the SEC also may be obtained free of charge upon written request to: Denali Capital Acquisition Corp.437 Madison Avenue, 27th FloorNew York, NY 10022 Participants in the Solicitation Denali and its directors and executive officers may be deemed participants in the solicitation of proxies from Denali’s shareholders with respect to the proposed Business Combination. Information about Denali’s directors and executive officers and a description of their interests in Denali is included in the Proxy Statement/Prospectus for the proposed transaction and is available at the SEC’s website (www.sec.gov). Semnur and its directors and executive officers may also be deemed to be participants in the solicitation of proxies from the shareholders of Denali in connection with the proposed Business Combination. Information about Semnur’s directors and executive officers and information regarding their interests in the proposed transaction is included in the Proxy Statement/Prospectus for the proposed transaction. Non-Solicitation This press release is not a proxy statement or solicitation of a proxy, consent or authorization with respect to any securities or in respect of the potential transaction and shall not constitute an offer to sell or a solicitation of an offer to buy the securities of Denali, the combined company or Semnur, nor shall there be any sale of any such securities in any state or jurisdiction in which such offer, solicitation or sale would be unlawful prior to registration or qualification under the securities laws of such state or jurisdiction. No offer of securities shall be made except by means of a prospectus meeting the requirements of the Securities Act of 1933, as amended. Forward-Looking Statements This press release includes forward-looking statements that involve risks and uncertainties. Forward-looking statements are statements that are not historical facts and may be accompanied by words that convey projected future events or outcomes, such as “believe,” “may,” “will,” “estimate,” “continue,” “anticipate,” “intend,” “expect,” “should,” “would,” “plan,” “predict,” “potential,” “seem,” “seek,” “future,” “outlook” or variations of such words or by expressions of similar meaning. These forward-looking statements include, but are not limited to, statements regarding future events, the Business Combination between Semnur and Denali, the estimated or anticipated future results and benefits of the combined company following the Business Combination, including the likelihood and ability of the parties to successfully consummate the Business Combination, future opportunities for the combined company, and other statements that are not historical facts. These statements are based on the current expectations of management of the Company, Semnur and Denali and are not predictions of actual performance. These forward-looking statements are provided for illustrative purposes only and are not intended to serve as, and must not be relied on, by any investor as a guarantee, an assurance, a prediction or a definitive statement of fact or probability. Actual events and circumstances are difficult or impossible to predict and will differ from assumptions. Many actual events and circumstances are beyond the control of the Company, Semnur and Denali. These statements are subject to a number of risks and uncertainties regarding the Company’s, Semnur’s and Denali’s businesses and the Business Combination, and actual results may differ materially. These risks and uncertainties include, but are not limited to, general economic, political and business conditions; the inability of the parties to consummate the Business Combination or the occurrence of any event, change or other circumstances that could give rise to the termination of the merger agreement for the Business Combination; the outcome of any legal proceedings that may be instituted against the parties following the announcement of the Business Combination; the receipt of an unsolicited offer from another party for an alternative business transaction that could interfere with the Business Combination; the risk that the approval of the stockholders of Semnur or the shareholders of Denali for the potential transaction is not obtained; failure to realize the anticipated benefits of the Business Combination, including as a result of a delay in consummating the potential transaction or difficulty in integrating the businesses of Semnur or Denali; the risk that the Business Combination disrupts current plans and operations as a result of the announcement and consummation of the Business Combination; the ability of the combined company to develop and successfully market SP-102 or other products; the ability of the combined company to grow and manage growth profitably and retain its key employees; the amount of redemption requests made by Denali’s shareholders; the inability to obtain or maintain the listing or trading of the post-acquisition company’s securities on Nasdaq or OTC Markets, as applicable, following the Business Combination; and costs related to the Business Combination. There may be additional risks that Semnur and the Company presently do not know or that Semnur or the Company currently believe are immaterial that could also cause actual results to differ from those contained in the forward-looking statements. In addition, forward-looking statements provide Semnur’s, the Company’s and Denali’s expectations, plans or forecasts of future events and views as of the date of the communication. Semnur and the Company anticipate that subsequent events and developments will cause such assessments to change. However, while Semnur and the Company may elect to update these forward-looking statements at some point in the future, each of Semnur and the Company specifically disclaim any obligation to do so. These forward-looking statements should not be relied upon as representing Semnur’s or the Company’s assessments as of any date subsequent to the date of this communication. Accordingly, investors are cautioned not to place undue reliance on these forward-looking statements.
Contacts: Investors and MediaScilex Holding Company 960 San Antonio RoadPalo Alto, CA 94303Office: (650) 516-4310 Email: investorrelations@scilexholding.com Website: www.scilexholding.com SEMDEXA™ (SP-102) is a trademark owned by Semnur Pharmaceuticals, Inc., a majority-owned subsidiary of Scilex Holding Company. A proprietary name review by the FDA is planned. ZTlido® is a registered trademark owned by Scilex Pharmaceuticals Inc., a wholly-owned subsidiary of Scilex Holding Company. Gloperba® is the subject of an exclusive, transferable license to use the registered trademark by Scilex Holding Company. ELYXYB® is a registered trademark owned by Scilex Holding Company. Scilex Bio™ is a trademark owned by Scilex Holding Company, Inc. All other trademarks are the property of their respective owners. © 2025 Scilex Holding Company All Rights Reserved.
临床2期快速通道临床3期上市批准引进/卖出
2025-04-11
PALO ALTO, Calif., April 11, 2025 (GLOBE NEWSWIRE) -- Scilex Holding Company (Nasdaq: SCLX, “Scilex” or “Company”), an innovative revenue-generating company focused on acquiring, developing and commercializing non-opioid pain management products for the treatment of acute and chronic pain and, following the formation of its proposed joint venture with IPMC Company, neurodegenerative and cardiometabolic disease, today announced that it will effect a reverse stock split of its outstanding shares of common stock at a ratio of 1-for-35, to be effective as of 12:01 a.m. Eastern Time on April 15, 2025. Scilex’s common stock will begin trading on a reverse stock split-adjusted basis at the opening of the market on April 15, 2025. Following the reverse stock split, Scilex’s common stock will continue to trade on The Nasdaq Capital Market under the symbol “SCLX” with the new CUSIP number, 80880W 205. The reverse stock split is intended for Scilex to regain compliance with the minimum bid price requirement of $1.00 per share of common stock for continued listing on The Nasdaq Capital Market. The reverse stock split will not change the authorized number of shares of Scilex’s common stock. No fractional shares will be issued in connection with the reverse stock split, and stockholders who would otherwise be entitled to receive a fractional share in connection with the reverse stock split will instead receive a cash payment in lieu thereof equal to such fraction multiplied by the closing sales price of Scilex’s common stock as reported on The Nasdaq Capital Market on April 14, 2025. In addition, the reverse stock split will apply to Scilex’s common stock issuable (or deemed issuable, as applicable) upon the exercise or conversion, as applicable, of certain of Scilex’s outstanding warrants, shares of Series A Preferred Stock, convertible notes and stock options, with proportionate adjustments to be made to the exercise and conversion prices thereof, in each case in accordance with the respective terms of such warrants, shares of Series A Preferred Stock, convertible notes and stock options (and the applicable equity incentive plans). The reverse stock split will reduce the number of issued and outstanding shares of Scilex’s common stock from approximately 243 million to approximately 6.9 million. At Scilex’s special meeting of stockholders held on March 19, 2025, Scilex’s stockholders approved the reverse stock split in connection with Scilex’s common stock and gave Scilex’s board of directors discretionary authority to select a ratio for the reverse stock split ranging from 1-for-14 shares to 1-for-50 shares. Scilex’s board of directors approved the reverse stock split at a ratio of 1-for-35 on April 3, 2025. Continental Stock Transfer & Trust Company is acting as the exchange agent and paying agent for the reverse stock split. Stockholders holding their shares in book-entry form or in brokerage accounts need not take any action in connection with the reverse stock split. Continental Stock Transfer & Trust Company will provide instructions to any stockholders with certificates regarding the process in connection with the exchange of pre-reverse stock split stock certificates for ownership in book-entry form or stock certificates on a post-reverse stock split basis. Stockholders are encouraged to contact their bank, broker or custodian with any procedural questions. For more information on Scilex Holding Company, refer to www.scilexholding.com For more information on Semnur Pharmaceuticals, Inc., refer to www.semnurpharma.com For more information on ZTlido® including Full Prescribing Information, refer to www.ztlido.com. For more information on ELYXYB®, including Full Prescribing Information, refer to www.elyxyb.com. For more information on Gloperba®, including Full Prescribing Information, refer to www.gloperba.com. https://www.facebook.com/scilex.pharm https://www.linkedin.com/company/scilex-holding-company/ info@scilexholding.com About Scilex Holding Company Scilex Holding Company is an innovative revenue-generating company focused on acquiring, developing and commercializing non-opioid pain management products for the treatment of acute and chronic pain and, following the formation of its proposed joint venture with IPMC Company, in neurodegenerative and cardiometabolic disease. Scilex targets indications with high unmet needs and large market opportunities with non-opioid therapies for the treatment of patients with acute and chronic pain and is dedicated to advancing and improving patient outcomes. Scilex’s commercial products include: (i) ZTlido® (lidocaine topical system) 1.8%, a prescription lidocaine topical product approved by the U.S. Food and Drug Administration (the “FDA”) for the relief of neuropathic pain associated with postherpetic neuralgia, which is a form of post-shingles nerve pain; (ii) ELYXYB®, a potential first-line treatment and the only FDA-approved, ready-to-use oral solution for the acute treatment of migraine, with or without aura, in adults; and (iii) Gloperba®, the first and only liquid oral version of the anti-gout medicine colchicine indicated for the prophylaxis of painful gout flares in adults. In addition, Scilex has three product candidates: (i) SP-102 (10 mg, dexamethasone sodium phosphate viscous gel) (“SEMDEXA” or “SP-102”), a novel, viscous gel formulation of a widely used corticosteroid for epidural injections to treat lumbosacral radicular pain, or sciatica, for which Scilex has completed a Phase 3 study and was granted Fast Track status from the FDA in 2017; (ii) SP-103 (lidocaine topical system) 5.4%, (“SP-103”), a next-generation, triple-strength formulation of ZTlido, for the treatment of acute pain and for which Scilex has recently completed a Phase 2 trial in acute low back pain. SP-103 has been granted Fast Track status from the FDA in low back pain; and (iii) SP-104 (4.5 mg, low-dose naltrexone hydrochloride delayed-release capsules) (“SP-104”), a novel low-dose delayed-release naltrexone hydrochloride being developed for the treatment of fibromyalgia. Scilex Holding Company is headquartered in Palo Alto, California. About Semnur Pharmaceuticals, Inc. Semnur Pharmaceuticals, Inc. (“Semnur”), a wholly-owned subsidiary of Scilex, is a clinical late-stage specialty pharmaceutical company focused on the development and commercialization of novel non-opioid pain therapies. Semnur’s product candidate, SP-102 (SEMDEXA™), is the first non-opioid novel gel formulation administered epidurally in development for patients with moderate to severe chronic radicular pain/sciatica. Semnur Pharmaceuticals, Inc. is headquartered in Palo Alto, California Forward-Looking Statements This press release and any statements made for and during any presentation or meeting concerning the matters discussed in this press release contain forward-looking statements related to Scilex and its subsidiaries under the safe harbor provisions of Section 21E of the Private Securities Litigation Reform Act of 1995 and are subject to risks and uncertainties that could cause actual results to differ materially from those projected. Forward-looking statements include statements regarding Scilex’s ability to regain or remain in compliance with the continued listing standards of Nasdaq, Scilex’s proposed joint venture with IPMC Company and the potential development and commercialization of treatments for obesity, neurodegenerative, cardiometabolic disease. Risks and uncertainties that could cause Scilex’s actual results to differ materially and adversely from those expressed in our forward-looking statements, include, but are not limited to: Scilex’s ability to consummate a joint venture or any other transaction with IPMC Company and develop and commercialize treatments for obesity, neurodegenerative, cardiometabolic disease; risks associated with the unpredictability of trading markets and whether a market will be established for Scilex’s common stock; general economic, political and business conditions; risks related to COVID-19 (and other similar disruptions); the risk that the potential product candidates that Scilex develops may not progress through clinical development or receive required regulatory approvals within expected timelines or at all; risks relating to uncertainty regarding the regulatory pathway for Scilex’s product candidates; the risk that Scilex will be unable to successfully market or gain market acceptance of its product candidates; the risk that Scilex’s product candidates may not be beneficial to patients or successfully commercialized; the risk that Scilex has overestimated the size of the target patient population, their willingness to try new therapies and the willingness of physicians to prescribe these therapies; risks that the outcome of the trials and studies for SP-102, SP-103 or SP-104 may not be successful or reflect positive outcomes; risks that the prior results of the clinical and investigator-initiated trials of SP-102 (SEMDEXA™), SP-103 or SP-104 may not be replicated; regulatory and intellectual property risks; and other risks and uncertainties indicated from time to time and other risks described in Scilex’s most recent periodic reports filed with the Securities and Exchange Commission, including Scilex’s Annual Report on Form 10-K for the year ended December 31, 2024 and subsequent Quarterly Reports on Form 10-Q that the Company has filed or may file with the SEC, including the risk factors set forth in those filings. Investors are cautioned not to place undue reliance on these forward-looking statements, which speak only as of the date of this release, and Scilex undertakes no obligation to update any forward-looking statement in this press release except as may be required by law. Contacts:Investors and MediaScilex Holding Company 960 San Antonio RoadPalo Alto, CA 94303Office: (650) 516-4310 Email: investorrelations@scilexholding.com Website: www.scilexholding.com # # # SEMDEXA™ (SP-102) is a trademark owned by Semnur Pharmaceuticals, Inc., a wholly-owned subsidiary of Scilex Holding Company. A proprietary name review by the FDA is planned. ZTlido® is a registered trademark owned by Scilex Pharmaceuticals Inc., a wholly-owned subsidiary of Scilex Holding Company. Gloperba® is the subject of an exclusive, transferable license to use the registered trademark by Scilex Holding Company. ELYXYB® is a registered trademark owned by Scilex Holding Company. All other trademarks are the property of their respective owners. © 2025 Scilex Holding Company All Rights Reserved.
快速通道临床2期临床3期上市批准引进/卖出
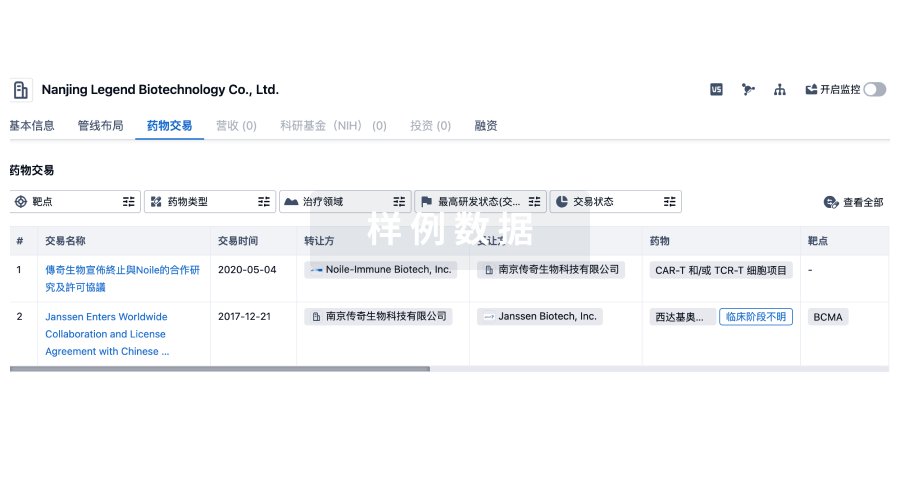
100 项与 Scilex Pharmaceuticals, Inc. 相关的药物交易
登录后查看更多信息
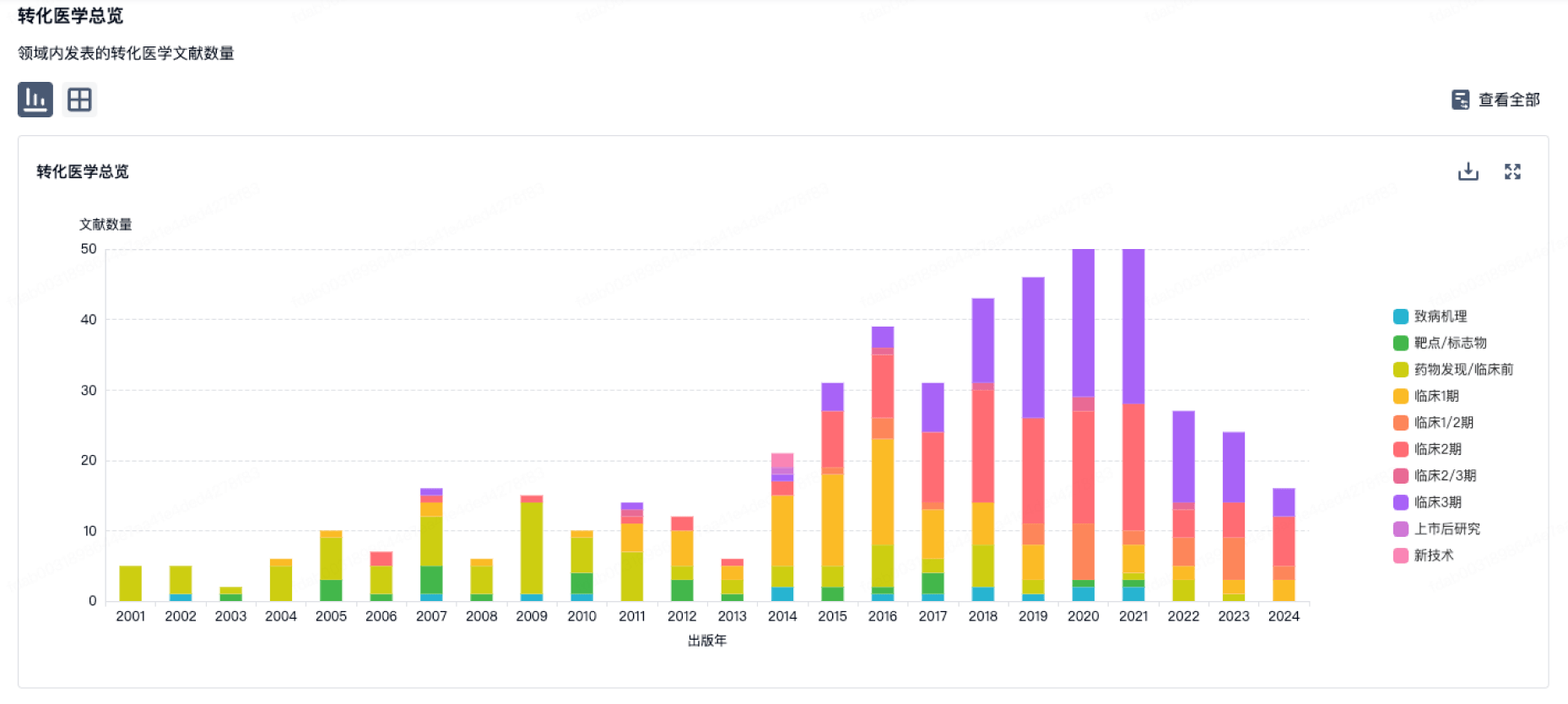
100 项与 Scilex Pharmaceuticals, Inc. 相关的转化医学
登录后查看更多信息
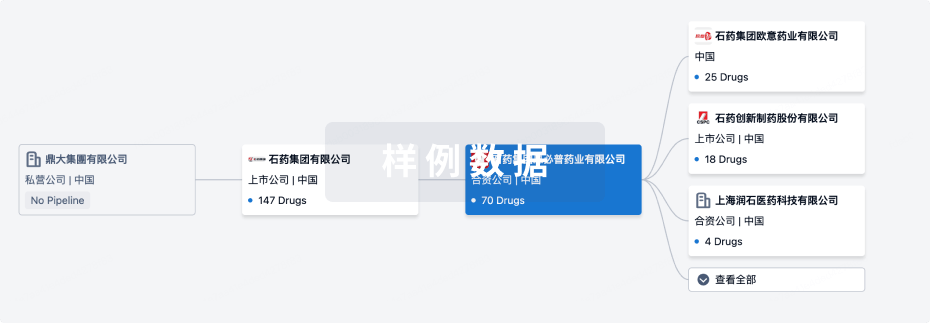
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年09月22日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床1期
1
3
批准上市
其他
1
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
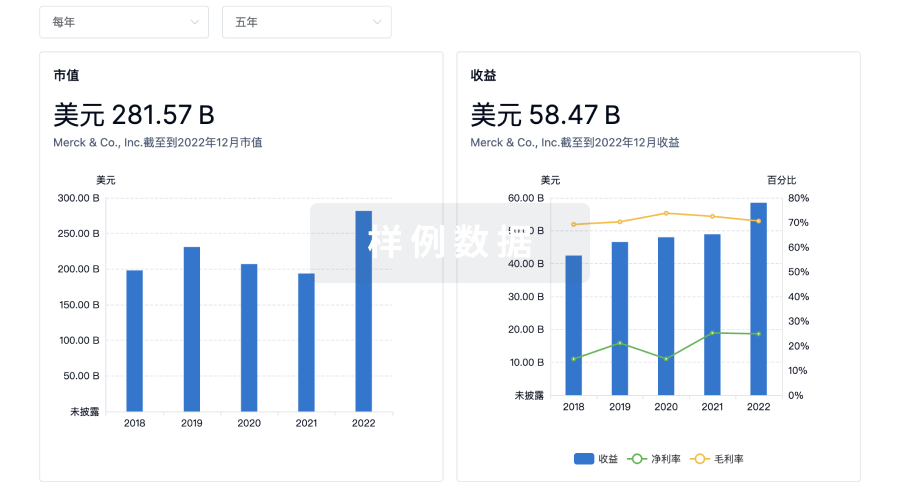
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
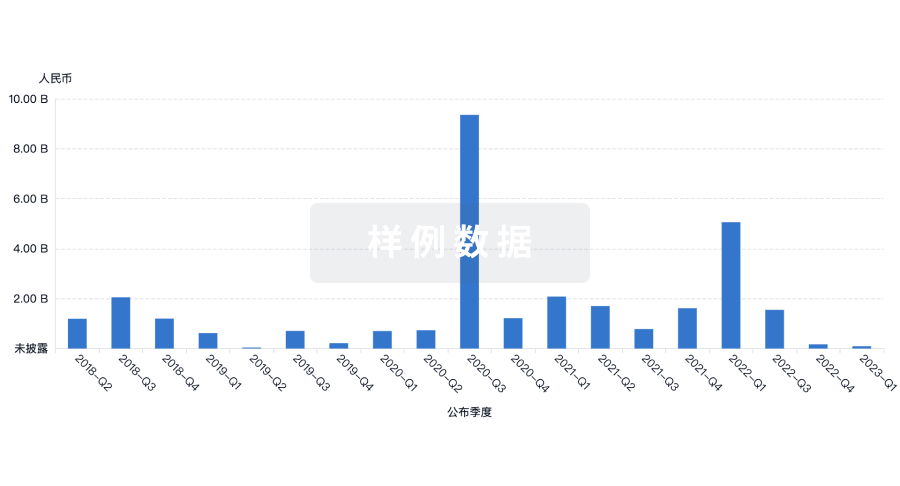
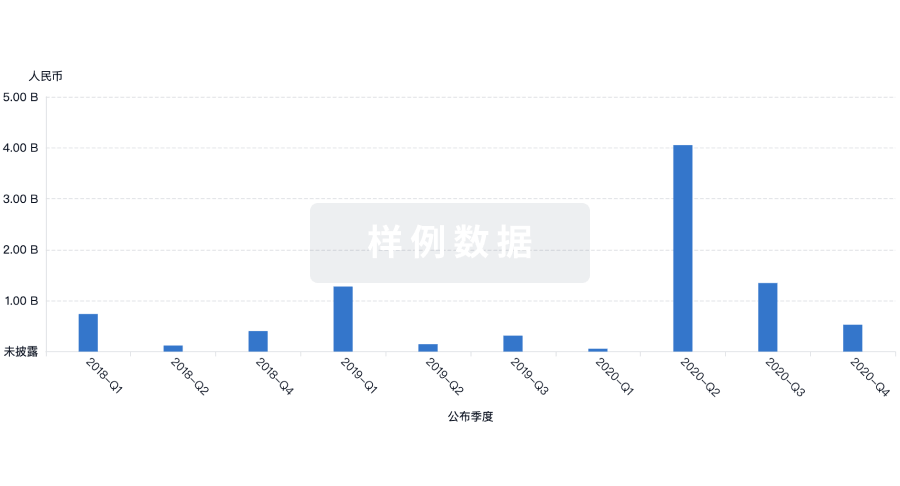
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



