预约演示
更新于:2025-05-07

University Medical Center of Utrecht
更新于:2025-05-07
概览
标签
皮肤和肌肉骨骼疾病
其他疾病
免疫系统疾病
小分子化药
诊断用放射药物
化学药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 4 |
| 诊断用放射药物 | 3 |
| 化学药 | 2 |
| 融合蛋白 | 1 |
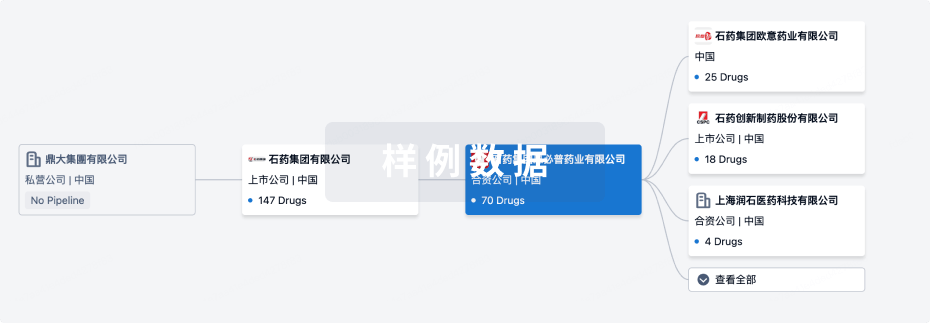
关联
12
项与 University Medical Center of Utrecht 相关的药物作用机制 骨吸收因子抑制剂 |
在研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期1977-09-01 |
靶点 |
作用机制 CD206抑制剂 [+1] |
在研适应症 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
作用机制 PKM2刺激剂 [+1] |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
849
项与 University Medical Center of Utrecht 相关的临床试验NCT05375708
A Multicenter Phase II Randomized Trial to Evaluate Systemic Therapy Versus Systemic Therapy in Combination with Stereotactic Radiotherapy in Patients with Metastatic Colorectal Cancer
A small number of colorectal cancer patients with limited oligometastases may be candidates for local treatment of metastases (e.g., resection, ablation). However, it is unclear if patients with more extensive metastatic disease benefit from local therapies to control visible metastasis.
The purpose of this study is to assess the impact of stereotactic body radiation therapy (SBRT) in combination with systemic therapy compared to systemic therapy alone on safety and efficacy in patients with metastatic colorectal cancer (mCRC) and ≤10 metastases.
The purpose of this study is to assess the impact of stereotactic body radiation therapy (SBRT) in combination with systemic therapy compared to systemic therapy alone on safety and efficacy in patients with metastatic colorectal cancer (mCRC) and ≤10 metastases.
开始日期2025-12-01 |
NCT05603104
A Randomised, Controlled Trial to Investigate the Effect of an Intensified Pharmacological Treatment for Schizophrenia, Major Depressive Disorder and Bipolar Depression in Subjects Who Had a First-time Treatment Failure on Their First-line Treatment.
Schizophrenia, bipolar and major depressive disorders collectively affect over 10 million people across the EU and are associated with annual healthcare and societal costs in excess of 100 billion Euros. When diagnosed with one of these disorders, patients are prescribed psychotropic medication such as antidepressants, mood stabilisers or antipsychotics. It is unknown whether this first-line treatment will be successful. After this first-line treatment fails, usually a second-line treatment is initiated, and when this is not successful either a third-line treatment is initiated. Third-line treatments are quite successful, especially when compared to second-line treatments. The research question is whether the third-line treatments (early-intensified treatments) would be more efficacious than the current second-line treatments (treatment as usual) for schizophrenia, bipolar and major depressive disorders. If this is indeed the case, this could lead to the prevention of unnecessary trials of ineffective treatments and adaptations of worldwide guidelines as well as a reduction of healthcare and societal costs.
开始日期2025-04-30 |
申办/合作机构 |
NCT05973786
A Randomised, Controlled Trial to Investigate the Effect of a Six Week Intensified Pharmacological Treatment for Bipolar Depression Compared to Treatment as Usual in Subjects Who Had a First-time Treatment Failure on Their First-line Treatment.
Bipolar disorders affect approximately 4.5 million people across the European Union (EU) and are associated with high annual healthcare and societal costs. Bipolar disorder I and II represent disorders that cause extreme fluctuation in a person's mood, energy, and ability to function, in which symptoms of (hypo)mania and depression alternate. The depressive episodes of bipolar disorders are often referred to as bipolar depression (BD). In other words: it is a phase/state of the disorder. For many patients with BD, the depressive polarity is often more pervasive and more debilitating than manic states, with estimates that depressed mood accounts for up to two-thirds of the time spent unwell, even with treatment. The burden of not received an effective treatment for BD is high: more severe psychopathology, higher rates of unemployment, more hospitalisations, lower quality of life, lower cognitive functioning, risk of suicide, comorbidities and poorer social and occupational functioning and thus more carer burden. For BD, the treatment guidelines are very heterogeneous, amongst other reasons because the disease is heterogeneous and treatments should be tailored to the patients. There is no clear treatment algorithm and it cannot yet be predicted which treatment will be effective. Especially the place of adjunctive antidepressants is under debate. Usually, for psychiatric disorders (including bipolar disorder), a patient is considered to be treatment-resistant is two medicinal treatments have been tried (in sufficient duration and dosage) without sufficient success. For BD, there is no consensus on when to consider a patient as treatment-resistant, but the most common definition is after one prior treatment failure. This raises the research question whether adjunctive antidepressants to treat BD should be introduced earlier in the treatment. Additionally, The INTENSIFY trial is part of the larger Horizon 2021 project, with the central goal of paving the way for a shift towards a treatment decision-making process tailored for the individual at risk for treatment resistance. To that end, we aim to establish evidence-based criteria to make decisions of early intense treatment in individuals at risk for treatment resistance across the major psychiatric disorders of schizophrenia, bipolar disorder and major depression.
开始日期2025-02-11 |
申办/合作机构 |
100 项与 University Medical Center of Utrecht 相关的临床结果
登录后查看更多信息
0 项与 University Medical Center of Utrecht 相关的专利(医药)
登录后查看更多信息
42,978
项与 University Medical Center of Utrecht 相关的文献(医药)2025-12-31·European Journal of Psychotraumatology
Raising a child bereaved by domestic homicide: caregivers’ experiences
Article
作者: Snetselaar, Hanneke ; Alisic, Eva ; Stroeken, Tielke ; Groot, Arend
2025-12-31·Global Health Action
Feasibility and impact of a patient support group care model on diabetes and hypertension care in informal settlements in Nairobi, Kenya: a quasi-experimental study
Article
作者: Levitt, Naomi S. ; Asiki, Gershim ; Mahone, Sloan ; Kibe, Victor ; Sanya, Richard E. ; Mbau, Lilian ; Klipstein-Grobusch, Kerstin ; Iddi, Samuel ; Kibe, Peter M. ; Karugu, Caroline H. ; Mburu, Lilian
2025-12-31·Gut Microbes
Mouse strain-specific responses along the gut-brain axis upon fecal microbiota transplantation from children with autism
Article
作者: Perez-Pardo, Paula ; Roussin, Léa ; Ahmed, Sabbir ; Pasterkamp, R. Jeroen ; Lin, Jake ; Maximin, Elise ; Rabot, Sylvie ; Adolfs, Youri ; Autio, Reija ; Peralta Marzal, Lucia N. ; Prince, Naika ; Philippe, Catherine ; Salenius, Karoliina ; Naudon, Laurent ; Monnoye, Magali ; Kraneveld, Aletta D. ; Garssen, Johan
72
项与 University Medical Center of Utrecht 相关的新闻(医药)2025-04-10
SAN DIEGO and CALGARY, AB, April 10, 2025 /PRNewswire/ -- Oncolytics Biotech® Inc. (NASDAQ: ONCY) (TSX: ONC), a leading clinical-stage company specializing in immunotherapy for oncology, was discussed by field-leading key opinion leaders (KOLs) during a recent event hosted by H.C. Wainwright.
Martine Piccart, M.D., Ph.D., an Honorary Professor of Oncology at the Université Libre de Bruxelles (ULB) and Scientific Director of Oncology at the Institut Jules Bordet, in Brussels, Belgium, offered a detailed overview of the HR+/HER2- metastatic breast cancer landscape and emphasized the need for new treatment innovations, such as pelareorep, that work to activate the immune system to recognize and kill cancer.
Alexander Eggermont, M.D., Ph.D., Professor of Clinical & Translational Immunotherapy at the University Medical Center Utrecht in the Netherlands and Board Member of the Comprehensive Cancer Center Munich of the Technical University Munich and the Ludwig Maximilians University, Munich, Germany, provided insights on the current standards for treating pancreatic ductal adenocarcinoma (PDAC), a cancer type known for its resistance to treatment, and the potential impacts that an immunotherapy such as pelareorep might have on the field.
A replay of the full conversation can be found by clicking here.
About Oncolytics Biotech Inc.
Oncolytics is a clinical-stage biotechnology company developing pelareorep, an intravenously delivered immunotherapeutic agent. Pelareorep has demonstrated promising results in two randomized Phase 2 studies in metastatic breast cancer and Phase 1 and 2 studies in pancreatic cancer. It acts by inducing anti-cancer immune responses and promotes an inflamed tumor phenotype -- turning "cold" tumors "hot" -- through innate and adaptive immune responses to treat a variety of cancers. Pelareorep has demonstrated promising results in two randomized Phase 2 studies in metastatic breast cancer and Phase 1 and 2 studies in pancreatic cancer.
Pelareorep has demonstrated synergies with multiple approved oncology treatments. Oncolytics is currently conducting and planning combination clinical trials with pelareorep in solid malignancies as it advances towards registrational studies in metastatic breast cancer and pancreatic cancer, both of which have received Fast Track Designation from the FDA. For further information, please visit: or follow the company on social media on LinkedIn and on X @oncolytics.
Logo:
Company Contact
Jon Patton
Director of IR & Communication
[email protected]
Investor Relations for Oncolytics
Mike Moyer
LifeSci Advisors
+1-617-308-4306
[email protected]
Media Contact for Oncolytics
Michael Rubenstein
LifeSci Communications
[email protected]
SOURCE Oncolytics Biotech® Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
免疫疗法快速通道临床2期临床结果
2025-03-27
Abbott's Volt™ PFA System is designed to provide a new therapy option for people battling heart rhythm disorders such as atrial fibrillation
Pulsed field ablation – or PFA – uses high energy electrical pulses for ablation procedures that may offer benefits to targeting and treating tissue in the heart
Abbott's Volt PFA System is designed to overcome limitations of existing PFA systems, providing improved workflows and a clearer indication of contact between the Volt PFA catheter and targeted tissue
ABBOTT PARK, Ill., March 27, 2025 /PRNewswire/ -- Abbott (NYSE: ABT) today announced it has received CE Mark in Europe for the Volt™ PFA System to treat patients battling atrial fibrillation (AFib). With the earlier-than-expected CE Mark, Abbott has begun commercial PFA cases in the EU with physicians who have already gained experience with the Volt PFA System within Abbott's PFA clinical studies. The company will further expand use of Volt in EU markets throughout the second half of the year.
Today, approximately 8 million Europeans over the age of 65 are living with AFib, a number expected to double over the next 30 years.1,2 People living with AFib face an increased risk of stroke, heart failure and death, and many rely on cardiac ablation to treat the condition effectively. The Volt PFA System builds upon Abbott's leading electrophysiology (EP) portfolio by providing a single-catheter PFA approach, improving workflow by allowing for mapping, pacing, and ablating with a single catheter to safely and effectively treat patients with AFib.
CE Mark approval for the Volt PFA System was granted based on strong results from Abbott's Volt CE Mark study, a global clinical trial conducted at centers in Europe and Australia. The trial showed the Volt PFA System achieved pulmonary vein isolation (PVI) – the method of destroying tissue causing a patient's AFib – in 99.1% of veins during ablation procedures with far fewer energy applications than on-market competitive PFA systems.3
Following approval, initial cases were completed by Prof. Helmut Puererfellner at Ordensklinikum hospital in Linz, Austria; Prof. Roland Tilz at the University Heart Center in Luebeck, Germany; Prof. Gian-Battista Chierchia at the University of Brussels in Belgium; and Prof. Peter Loh at the University Medical Center Utrecht in the Netherlands.
"The launch of Abbott's Volt PFA system marks a major milestone in the evolution of electrophysiology across Europe and signals we're moving beyond early therapy approaches to new systems that incorporate key physician feedback and clinical insights to optimize PFA therapy," said Prof. Puererfellner. "PFA is significantly changing our approach to treating patients and it's exciting to see the Volt PFA System build on the therapy's potential and bring new benefits to clinical teams so we can improve the lives of more patients battling conditions like AFib."
Volt™ PFA System: Driving New Advancement in the PFA Market
PFA works differently from traditional ablation approaches by delivering high energy electrical pulses to targeted areas of cardiac tissue causing abnormal heart rhythms. As a result, PFA can reduce the risk of damaging adjacent tissue in patients with complex disease or anatomy.
Yet current on-market competitive PFA systems have required several therapy applications with a catheter positioned in various locations due to a lack of visualization or contact assessment. By integrating with Abbott's EnSite™ X EP system, the Volt PFA System is designed to address such limitations and provide:
Simplified workflow. The single-catheter integrated approach of the Volt PFA system improves clinical workflow and provides real-time contact visualization to help physicians position the catheter for therapy delivery.
Efficient energy delivery. The proprietary balloon-in-basket design of the Volt™ PFA Catheter, Sensor Enabled™, allows for efficient energy transfer directly to the targeted tissue to stop the heart's erratic signals, minimizing the number of therapy applications needed.
Procedural flexibility. Patients undergoing a minimally invasive ablation procedure with the Volt PFA Catheter, Sensor Enabled, can be placed under light sedation or general anesthesia based on physician and hospital preference.
In addition, the Volt PFA catheter's integration with EnSite X system allows for clearer visualization and navigation for accurate positioning of the Volt PFA catheter to treat tissue. The One System Solution provided by EnSite X can accommodate all EP procedures and compatible technologies.
"While PFA is a relatively new therapy option, we've incorporated lessons learned from first-generation devices and designed the Volt system to simplify PFA procedures while making them more efficient," said Christopher Piorkowski, M.D., chief medical officer of Abbott's electrophysiology business. "Clinical data has also shown that the Volt catheter's cutting-edge design helps physicians achieve pulmonary vein isolation in fewer ablation attempts and less therapy applications for improved patient outcomes."
Clinical and Regulatory Progress Across Abbott's PFA Portfolio
Abbott's Volt PFA System is currently under evaluation in the VOLT-AF Investigational Device Exemption (IDE) Study. The study completed enrollment last year – four months ahead of the anticipated timeline. Nearly 400 patients are enrolled in the trial, and Abbott anticipates completing the 12-month follow-up for the study later this year.
In addition, the company has also made significant progress in clinical studies evaluating Abbott's focal PFA technology, which is designed to provide focused energy delivery for the creation of targeted lesions at specific points in the heart. Enrollment was recently completed ahead of schedule in Abbott's FOCALFLEX CE trial assessing the performance of the TactiFlex™ Duo Ablation Catheter, Sensor Enabled™. Enrollment is also underway in the FlexPulse IDE trial evaluating TactiFlex Duo in the U.S.
Abbott has also recently received regulatory approval in the U.S. and Europe for a 13F sizing of the company's Agilis™ NxT Steerable Introducer, Dual Reach™, which makes the Agilis system compatible with larger catheters, including those used for PFA therapy.
For U.S. important safety information go to:
Agilis™ NxT Steerable Introducer, Dual Reach™
EnSite™ X EP System
About Abbott
Abbott is a global healthcare leader that helps people live more fully at all stages of life. Our portfolio of life-changing technologies spans the spectrum of healthcare, with leading businesses and products in diagnostics, medical devices, nutritionals and branded generic medicines. Our 114,000 colleagues serve people in more than 160 countries.
Connect with us at and on LinkedIn, Facebook, Instagram, X and Youtube.
1 Fact Sheets for Press. European Society of Cardiology. (n.d.-a).
2 Atrial fibrillation set to affect more than 14 million over-65s in the EU by 2060. European Society of Cardiology. (n.d.).
3 Tilz, R.R. (2025, January 17) Acute results demonstrate safety and effectiveness of balloon-based pulsed field ablation system for de novo PVI in PAF and PersAF [Late Breaking Presentation]. AF Symposium 2025, Boston MA, USA.
SOURCE Abbott
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
2025-03-27
Abbott's Volt™ PFA System is designed to provide a new therapy option for people battling heart rhythm disorders such as atrial fibrillationPulsed field ablation – or PFA – uses high energy electrical pulses for ablation procedures that may offer benefits to targeting and treating tissue in the heartAbbott's Volt PFA System is designed to overcome limitations of existing PFA systems, providing improved workflows and a clearer indication of contact between the Volt PFA catheter and targeted tissueABBOTT PARK, Ill., March 27, 2025 /PRNewswire/ -- Abbott (NYSE: ABT) today announced it has received CE Mark in Europe for the Volt™ PFA System to treat patients battling atrial fibrillation (AFib). With the earlier-than-expected CE Mark, Abbott has begun commercial PFA cases in the EU with physicians who have already gained experience with the Volt PFA System within Abbott's PFA clinical studies. The company will further expand use of Volt in EU markets throughout the second half of the year.
Today, approximately 8 million Europeans over the age of 65 are living with AFib, a number expected to double over the next 30 years.1,2 People living with AFib face an increased risk of stroke, heart failure and death, and many rely on cardiac ablation to treat the condition effectively. The Volt PFA System builds upon Abbott's leading electrophysiology (EP) portfolio by providing a single-catheter PFA approach, improving workflow by allowing for mapping, pacing, and ablating with a single catheter to safely and effectively treat patients with AFib.
CE Mark approval for the Volt PFA System was granted based on strong results from Abbott's Volt CE Mark study, a global clinical trial conducted at centers in Europe and Australia. The trial showed the Volt PFA System achieved pulmonary vein isolation (PVI) – the method of destroying tissue causing a patient's AFib – in 99.1% of veins during ablation procedures with far fewer energy applications than on-market competitive PFA systems.3
Following approval, initial cases were completed by Prof. Helmut Puererfellner at Ordensklinikum hospital in Linz, Austria; Prof. Roland Tilz at the University Heart Center in Luebeck, Germany; Prof. Gian-Battista Chierchia at the University of Brussels in Belgium; and Prof. Peter Loh at the University Medical Center Utrecht in the Netherlands.
"The launch of Abbott's Volt PFA system marks a major milestone in the evolution of electrophysiology across Europe and signals we're moving beyond early therapy approaches to new systems that incorporate key physician feedback and clinical insights to optimize PFA therapy," said Prof. Puererfellner. "PFA is significantly changing our approach to treating patients and it's exciting to see the Volt PFA System build on the therapy's potential and bring new benefits to clinical teams so we can improve the lives of more patients battling conditions like AFib."
Volt™ PFA System: Driving New Advancement in the PFA Market PFA works differently from traditional ablation approaches by delivering high energy electrical pulses to targeted areas of cardiac tissue causing abnormal heart rhythms. As a result, PFA can reduce the risk of damaging adjacent tissue in patients with complex disease or anatomy.
Yet current on-market competitive PFA systems have required several therapy applications with a catheter positioned in various locations due to a lack of visualization or contact assessment. By integrating with Abbott's EnSite™ X EP system, the Volt PFA System is designed to address such limitations and provide:
Simplified workflow. The single-catheter integrated approach of the Volt PFA system improves clinical workflow and provides real-time contact visualization to help physicians position the catheter for therapy delivery.Efficient energy delivery. The proprietary balloon-in-basket design of the Volt™ PFA Catheter, Sensor Enabled™, allows for efficient energy transfer directly to the targeted tissue to stop the heart's erratic signals, minimizing the number of therapy applications needed.Procedural flexibility. Patients undergoing a minimally invasive ablation procedure with the Volt PFA Catheter, Sensor Enabled, can be placed under light sedation or general anesthesia based on physician and hospital preference.In addition, the Volt PFA catheter's integration with EnSite X system allows for clearer visualization and navigation for accurate positioning of the Volt PFA catheter to treat tissue. The One System Solution provided by EnSite X can accommodate all EP procedures and compatible technologies.
"While PFA is a relatively new therapy option, we've incorporated lessons learned from first-generation devices and designed the Volt system to simplify PFA procedures while making them more efficient," said Christopher Piorkowski, M.D., chief medical officer of Abbott's electrophysiology business. "Clinical data has also shown that the Volt catheter's cutting-edge design helps physicians achieve pulmonary vein isolation in fewer ablation attempts and less therapy applications for improved patient outcomes."
Clinical and Regulatory Progress Across Abbott's PFA Portfolio Abbott's Volt PFA System is currently under evaluation in the VOLT-AF Investigational Device Exemption (IDE) Study. The study completed enrollment last year – four months ahead of the anticipated timeline. Nearly 400 patients are enrolled in the trial, and Abbott anticipates completing the 12-month follow-up for the study later this year.
In addition, the company has also made significant progress in clinical studies evaluating Abbott's focal PFA technology, which is designed to provide focused energy delivery for the creation of targeted lesions at specific points in the heart. Enrollment was recently completed ahead of schedule in Abbott's FOCALFLEX CE trial assessing the performance of the TactiFlex™ Duo Ablation Catheter, Sensor Enabled™. Enrollment is also underway in the FlexPulse IDE trial evaluating TactiFlex Duo in the U.S.
Abbott has also recently received regulatory approval in the U.S. and Europe for a 13F sizing of the company's Agilis™ NxT Steerable Introducer, Dual Reach™, which makes the Agilis system compatible with larger catheters, including those used for PFA therapy.
For U.S. important safety information go to:Agilis™ NxT Steerable Introducer, Dual Reach™ https://abbo.tt/Agilis_ISI
EnSite™ X EP Systemhttps://www.cardiovascular.abbott/us/en/hcp/products/electrophysiology/mapping-systems/ensite-x.html
About Abbott Abbott is a global healthcare leader that helps people live more fully at all stages of life. Our portfolio of life-changing technologies spans the spectrum of healthcare, with leading businesses and products in diagnostics, medical devices, nutritionals and branded generic medicines. Our 114,000 colleagues serve people in more than 160 countries.
Connect with us at www.abbott.com and on LinkedIn, Facebook, Instagram, X and Youtube.
1 Fact Sheets for Press. European Society of Cardiology. (n.d.-a). https://www.escardio.org/The-ESC/Press-Office/Factsheets 2 Atrial fibrillation set to affect more than 14 million over-65s in the EU by 2060. European Society of Cardiology. (n.d.). https://www.escardio.org/The-ESC/Press-Office/Press-releases/Atrial-fibrillation-set-to-affect-more-than-14-million-over-65s-in-the-EU-by-2060 3 Tilz, R.R. (2025, January 17) Acute results demonstrate safety and effectiveness of balloon-based pulsed field ablation system for de novo PVI in PAF and PersAF [Late Breaking Presentation]. AF Symposium 2025, Boston MA, USA.
SOURCE Abbott
临床研究
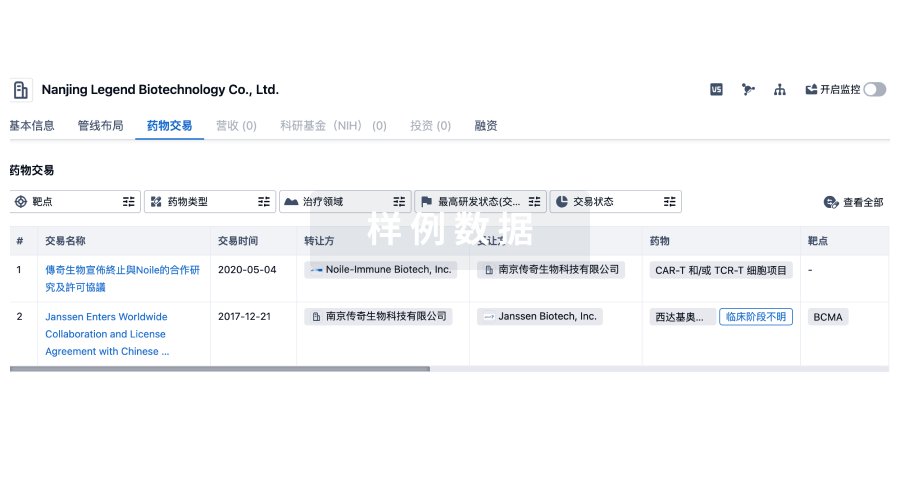
100 项与 University Medical Center of Utrecht 相关的药物交易
登录后查看更多信息
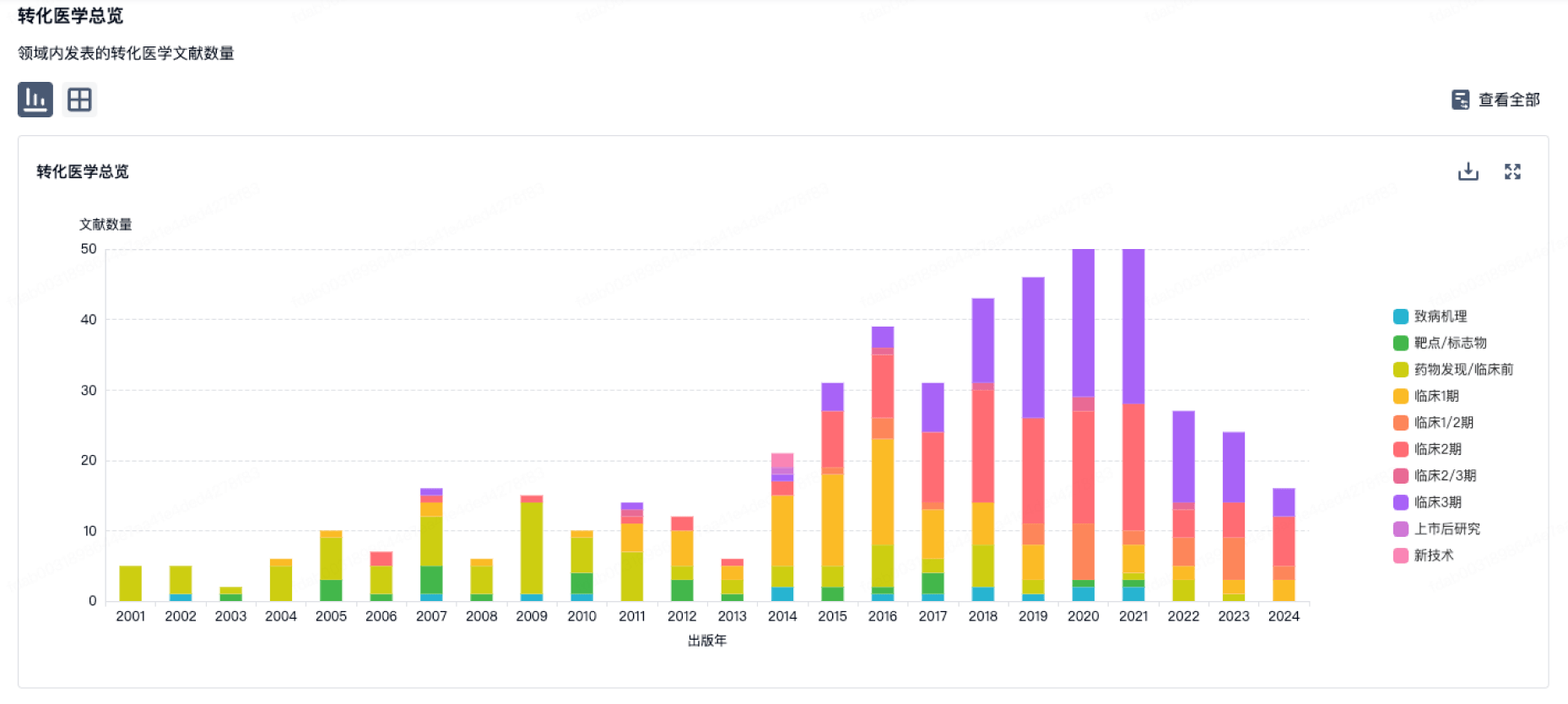
100 项与 University Medical Center of Utrecht 相关的转化医学
登录后查看更多信息
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年10月10日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
1
6
临床前
临床2期
1
2
临床3期
其他
2
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Gallium-68-tilmanocept ( CD206 ) | 子宫内膜癌 更多 | 临床3期 |
依替膦酸二钠 ( Bone resorption factor ) | 弹性假黄瘤 更多 | 临床3期 |
AZD-9567 ( GR ) | 类风湿关节炎 更多 | 临床2期 |
CL-04177 ( FOXO4 x p53 ) | 三阴性乳腺癌 更多 | 临床前 |
[18F]-MC-225 ( P-gp ) | HIV感染 更多 | 临床前 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
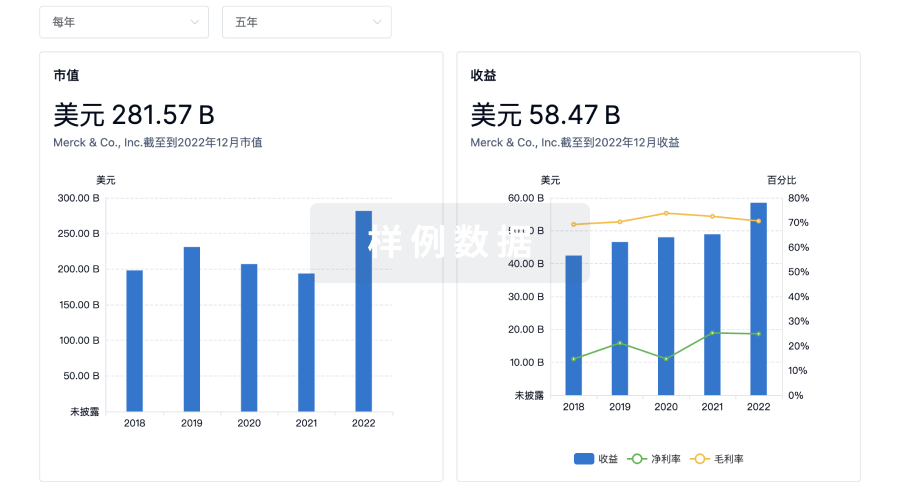
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


