预约演示
更新于:2025-05-07
Takayasu Arteritis
大动脉炎
更新于:2025-05-07
基本信息
别名 AORTIC ARCH SYNDROME、ARTERITIS TAKAYASU、ARTERITIS, TAKAYASU + [83] |
简介 A chronic inflammatory process that affects the AORTA and its primary branches, such as the brachiocephalic artery (BRACHIOCEPHALIC TRUNK) and CAROTID ARTERIES. It results in progressive arterial stenosis, occlusion, and aneurysm formation. The pulse in the arm is hard to detect. Patients with aortitis syndrome often exhibit retinopathy. |
关联
10
项与 大动脉炎 相关的药物靶点 |
作用机制 JAK1抑制剂 |
在研机构 |
原研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2019-08-16 |
靶点 |
作用机制 IL-6RA拮抗剂 |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期2005-04-11 |
95
项与 大动脉炎 相关的临床试验NCT06887062
Dual Endothelin Receptor Antagonism in Large Vessel Vasculitis (DERAIL-LVV)
Large vessel vasculitis is a disease that causes damage to blood vessels. This damage to blood vessels can increase the risk of patients with LVV developing cardiovascular disease, including heart attacks and strokes. A chemical produced in the body called endothelin may contribute to this increase in cardiovascular disease risk by causing the vessels to stiffen and blood pressure to increase.
It has previously been shown that by blocking the effects of endothelin, vessel stiffness and blood pressure improve. Bosentan is a tablet that blocks the effects of endothelin. The investigators plan to assess blood vessel function in those with LVV and participants without LVV. Participants with LVV will then be given Bosentan for 6 weeks to evaluate its impact on blood vessel function.
It has previously been shown that by blocking the effects of endothelin, vessel stiffness and blood pressure improve. Bosentan is a tablet that blocks the effects of endothelin. The investigators plan to assess blood vessel function in those with LVV and participants without LVV. Participants with LVV will then be given Bosentan for 6 weeks to evaluate its impact on blood vessel function.
开始日期2025-03-21 |
申办/合作机构 |
NCT06766552
A Multicenter Registry Study Assessing Patient Reported Outcome, Dosing Patterns, and Safety of Vunakizumab in Patients With General Rheumatic Diseases.
Ankylosing spondylitis, radiographically negative axial spondyloarthritis, psoriatic arthritis, polymyalgia rheumatica, Takayasu arteritis, giant cell arteritis, non-ocular Behcet's disease, and enthesitis-related arthritis are common diseases in rheumatology. Traditional anti-rheumatic drugs are less effective and have greater side effects than biological agents. At present, there has been no large-scale registration study on rheumatic autoimmune diseases such as spondyloarthritis in China. However, data such as patient characteristics, medication patterns, and patient outcome reports of different rheumatology diseases can often serve as a reference for rheumatology clinicians to reasonably select treatment methods for different patients. Therefore, a large-scale registration study is needed to fill the gap in multi-disease registration studies in rheumatology departments in China.
开始日期2025-01-30 |
申办/合作机构 |
NCT06807788
Evaluation of Platelet Aggregability in Patients with Takayasu's Arteritis
Inflammatory syndromes in general, and primary vasculitis specifically, present a high risk of cardiovascular involvement. Takayasu arteritis (TAK), for example, presents cardiovascular complications in up to 60% of cases. It is a systemic inflammatory disease that primarily affects large vessels, such as the aorta and its main branches. From a pathophysiological point of view, there are several causes that can lead to an exacerbated increase in cardiovascular risk in this population, including accelerated atherosclerosis, pro-inflammatory action of platelets and significant endothelial dysfunction.
In this context, the present case-control study intends to include 100 individuals (50 with TAK - case group, and 50 healthy volunteers - control group), matched by age and sex in a 1:1 ratio. The main objective of the study is to compare platelet aggregability in patients with TAK against healthy volunteers using the AggRAM® test. Among its secondary objectives is the analysis of platelet aggregability by other methods (Plateletworks, Chronolog, and PPAnalysis).
The study aims to significantly contribute to a better understanding of the potential influence of TAK on platelet aggregation and the response to antiplatelet agents, thereby contributing to a better understanding of the disease, with evident prognostic and therapeutic implications.
In this context, the present case-control study intends to include 100 individuals (50 with TAK - case group, and 50 healthy volunteers - control group), matched by age and sex in a 1:1 ratio. The main objective of the study is to compare platelet aggregability in patients with TAK against healthy volunteers using the AggRAM® test. Among its secondary objectives is the analysis of platelet aggregability by other methods (Plateletworks, Chronolog, and PPAnalysis).
The study aims to significantly contribute to a better understanding of the potential influence of TAK on platelet aggregation and the response to antiplatelet agents, thereby contributing to a better understanding of the disease, with evident prognostic and therapeutic implications.
开始日期2024-10-14 |
申办/合作机构 |
100 项与 大动脉炎 相关的临床结果
登录后查看更多信息
100 项与 大动脉炎 相关的转化医学
登录后查看更多信息
0 项与 大动脉炎 相关的专利(医药)
登录后查看更多信息
6,700
项与 大动脉炎 相关的文献(医药)2025-12-31·Annals of Medicine
CT Chest findings in IgG4-related disease
Article
作者: Nie, Yongkang ; Liu, Ye
2025-12-01·Current Cardiology Reports
Assessment of Coronary Microvascular Dysfunction in Patients with Systemic Vasculitis
Review
作者: Hakimjavadi, Ramtin ; Boczar, Kevin Emery ; Ahmed, Faisal ; Kadoya, Yoshito ; Sarwar, Shihab
2025-06-01·American Journal of Medicine Open
Analysis of Takayasu's Arteritis as a Risk Factor for Acute Coronary Syndrome
Article
作者: Arora, Shilpa ; Romero Noboa, Maria Emilia ; Manadan, Augustine M ; Kansal, Preeti
62
项与 大动脉炎 相关的新闻(医药)2025-04-14
点击上方的 行舟Drug ▲ 添加关注《抗体偶联药物药学研究与评价技术指导原则》解读来源《中国新药杂志》 2025年 第34卷 第6期作者李倩,武勇凯,韦薇,何伍国家药品监督管理局药品审评中心摘要近年来,随着技术的迭代和成熟,抗体偶联药物(antibody⁃drug conjugate,ADC)在肿瘤治疗领域比重日益凸显,申报数量与日俱增。截至2024年12月,全球已批准16个ADC产品上市,国内也有2个本土创新ADC产品获批上市,并有上百个ADC产品获批开展临床研究。为了规范和指导该类产品的研发与申报,国家药品监督管理局药品审评中心于2024年2月正式发布了《抗体偶联药物药学研究与评价技术指导原则》。本文结合该指导原则的起草思路,对指导原则的主要内容进行解读,以便业界更好地理解该指导原则,促进该类产品的上市申报。关键词抗体偶联药物;药学研究;指导原则_正文_抗体偶联药物(antibody⁃drug conjugate,ADC)是由靶向特异性抗原的抗体或抗体片段与有效载荷(payload)通过连接子(linker)偶联而成的一类创新型抗体药物。早在20世纪初德国科学家就提出了“魔法子弹”的概念[1],但直到2000年第一个ADC药物Mylotarg®才获批上市,用于治疗急性粒细胞白血病。然而,由于Mylotarg®的连接子不稳定,有效载荷在血浆循环中过早释放,从而导致严重的毒性反应,最终在2010年主动撤市。此后10年都没有新的ADC产品获批上市。得益于技术的快速发展,2019年ADC产品获批的数量翻了1番。截至2024年12月,全球共有16个ADC产品获批上市,其中有8款产品在我国获批上市,包括2个我国本土的ADC药物维迪西妥单抗和芦康沙妥珠单抗。作为抗肿瘤的研发热点药物,ADC虽然起步阶段的进展缓慢,但随着技术的迭代和成熟,引发了ADC产品的开发热潮,全球和我国ADC产品的临床试验数量均呈现出逐年递增的趋势。截至2024年3月,在国际临床试验注册平台(http://www. clinicaltrials. gov)上开展的ADC相关临床试验共计281项(关键词:antibody⁃drug conjugate)。其中美国以189项位居首位,中国以51项位居第2,欧盟和澳大利亚分别有15项和7项。除了肿瘤适应证以外,ADC临床研究也在拓宽适应证类型,如弥漫性皮肤系统性硬化症、大动脉炎等。我国ADC产品的研发总体格局与全球相似,而且我国ADC领域的研发进展较快,目前在研管线数量已经占到全球总量的40%~50%,但临床管线大多处于临床早期,未来几年可能会迎来上市的收获期。目前国内外尚未发布针对ADC产品药学研究的相关指导原则,为了快速推动ADC产品的研发和上市进程,国家药品监督管理局药品审评中心(以下简称“药审中心”)组织撰写了《抗体偶联药物药学研究与评价技术指导原则》,并于2024年2月正式发布。本文旨在结合ADC产品的特点,通过对该指导原则的起草背景、起草修订过程、起草思路、主要内容和重点问题说明等内容的介绍,以便业界更好地理解该指导原则,促进该类产品的研发申报。1起草背景起草前期对ADC产品相关的指导原则进行了调研,2022年2月美国FDA发布了针对ADC产品临床药理的指南草案“Clinical Pharmacology Considerations for Antibody⁃Drug Conjugates”[2]。2022年7月我国监管机构起草了《抗体偶联药物非临床研究技术指导原则(征求意见稿)》,并对外公开征求意见。截至2023年12月,国内外尚未发布针对ADC产品药学研究的相关指导原则,因此,该研究领域缺乏一定的监管共识。虽然ADC领域研发进展较快,但当前国内外上市的ADC产品数量较为有限,大部分此类产品仍处于临床前或临床研发阶段,即将迎来上市的收获期。这类产品的开发从起始物料、工艺再到质量控制涉及化学和生物学等多学科的参与,具有分子结构和生产过程复杂多样、产品异质性高等特点,产品设计、生产工艺、处方开发、质量研究和控制等方面均面临诸多挑战。基于以上现状,为了规范和指导ADC产品的研发与申报,需要制定符合当前行业研发需求的指导原则,统一ADC产品在申报上市阶段的研发和审评技术要求,快速推动ADC产品的研发和上市进程。文章内容由凡默谷小编查阅文献选取,排版与编辑为原创。如转载,请尊重劳动成果,注明【来源:凡默谷公众号】。2起草过程起草前期,起草小组广泛调研了国内外ADC产品相关指导原则的发布情况以及产品的研发情况,结合文献资料调研和既往国内已申报的产品信息,综合分析了当前我国此类产品的研发现状和特点,总体确定了指导原则的主体内容和结构框架。同时,根据实际审评过程中产品存在的问题和可能的发展趋势,撰写形成初稿。针对部分重点问题组织召开了第一次专家咨询会议,于2023年6月形成《抗体偶联药物药学研究与评价技术指导原则》征求意见稿,并通过药审中心网站向社会公开征求意见。在历时1个月的征求意见期间,共征集到31家企业共215条反馈意见。随后对反馈意见进行了逐条讨论和修订,于2023年11月召开了第二次专家咨询会议,对反馈意见比较集中的共性问题和指导原则全文进行了讨论,最终完成指导原则的修订。2024年2月18日药审中心正式发布了《抗体偶联药物药学研究与评价技术指导原则》。3起草思路该指南是基于当前对ADC产品的认知,主要针对ADC产品上市阶段的药学研究提出科学性建议和一般性技术要求,不具有强制性。由于ADC产品复杂多样,不同产品的生产工艺和控制策略也可能各不相同,且行业技术发展迅速,因此,在撰写指导原则时提出了基于风险的研发理念和具体品种具体分析的原则,申请人亦可基于产品研发的实际情况,采用其他等同或更有效的技术和方法开展研究,提供合理性依据和说明,并加强与监管机构的沟通交流。本指南基本覆盖了ADC产品上市阶段需要完成的药学研究,包括生产用物料、生产工艺和过程中控制、质量研究与质量标准、稳定性研究、包装及容器密封系统等,各个章节分别基于ADC产品的特点对特殊要求或考虑进行了具体描述。同时,为了回应业界关切,在指南的起草过程中,也充分考虑了国内产品的研发现状、存在的问题以及未来的发展趋势等,在本指导原则适当的章节中,结合审评经验,对不同研发阶段的基本要求做了原则性的说明。适时,可再考虑启动针对申报临床阶段的技术要求撰写。4主要内容该指南的整体框架基本按照生物制品药学研究与评价的主要方面进行撰写,共包括11个章节,除了前言、适用范围、一般原则、风险评估与控制等几个总括性章节外,主体内容包括生产用物料、生产工艺、质量研究与质量标准、稳定性研究、包装及容器密封系统等几个部分。下文将对指南中比较受关注和重点章节部分的内容做进一步说明,以便业界在开发和研究ADC产品时更好地理解指南的内容。由于ADC产品的结构复杂多样,对于已有成熟的技术指导原则覆盖的组成部分(如小分子部分、抗体部分等),可参考相应指导原则的要求,指南中不再赘述,但作为ADC产品的组成部分,本指南对需要额外或特别关注的内容在适当章节进行了阐述或列举。4.1 适用范围该指南主要适用于由抗体/抗体片段和有效载荷(如小分子细胞毒性药物)通过连接子偶联而成的ADC产品。目前狭义的ADC产品指抗体/抗体片段偶联小分子药物,考虑到偶联大分子(如重组蛋白、酶、细菌毒素等)、核素、细胞、寡核苷酸等产品的生产工艺、质量控制等存在较大区别,在一个指导原则中很难全部涵盖。因此,指南中对ADC产品的定义较为广泛,但在相关章节中主要以小分子为例进行了具体描述。其他类型的ADC产品可参考基本的理念和原则性的要求,并根据具体问题具体分析的原则开展研究。后续随着研发和审评经验的积累将适时撰写相关的审评考虑或技术指南。4.2 一般原则ADC产品的开发应遵循药品研发的一般规律。基于ADC产品的复杂性和特殊性,对产品设计、生产工艺、处方开发以及质量研究与控制等方面的特殊考虑进行了原则性说明。起草前期调研结果显示,国内外上市的ADC产品数量较为有限,大部分仍处于临床前或临床研发阶段,同时业界也比较关注临床试验阶段的药学技术要求。因此,指南在一般原则章节中对ADC产品不同研发阶段的基本要求也做了原则性的说明。整体上,在临床试验申报阶段,重点关注影响临床安全性的因素(如外源因子的控制、临床样品制备工艺的稳健性等),以保障临床受试者的安全。此外,非临床研究是评估产品在人体使用安全性的重要参考依据,需特别关注临床试验用样品与非临床研究用样品在生产工艺和质量方面的对比或桥接分析,临床试验用样品的质量应不劣于非临床研究用样品的质量。稳定性研究方面,稳定性研究数据应可以支持临床试验的开展,临床试验用样品的保存、运输和使用条件应在经过研究确认的条件范围内。4.3 生产用物料ADC产品是大分子和小分子结合的创新型抗体药物,生产用物料涉及化学和生物学等多学科参与,物料种类较多且存在引入外源因子或毒性化学材料的风险,需要基于风险评估进行全面的控制。该章节对常见的生产用物料的研究和质控要求做了介绍,并结合ADC自身和工艺的特点,对额外需要关注的内容进行了列举。对于化学结构和生产工艺较为复杂的起始物料,应结合起始物料的生产工艺,对其质量进行全面分析和合理控制,并对起始物料选择的合理性进行论证。此外,ADC生产过程中通常会使用有机溶剂以提高偶联反应的效率,因此生产过程中直接接触的材料应能够耐受有机溶剂且浸出物应符合相关要求。由于偶联了疏水性的小分子,对于疏水性较高的ADC产品还需要关注ADC分子与除菌滤膜的非特异性结合,选择合适的滤膜。对于酶法偶联的ADC产品,如果偶联酶为自制原材料,研究者应根据偶联酶的生产工艺开展相应的研究并提供全套药学研究资料;若系真核细胞表达的重组酶还应充分考虑外源病毒因子的控制,并参考ICH Q5A[3]等开展病毒清除研究。4.4 生产工艺ADC产品的生产工艺通常包括裸抗生产、小分子生产、ADC原液生产和制剂生产等多个生产环节。因此,指南从生产工艺开发、生产工艺的确认与验证两方面对小分子、裸抗、原液和制剂进行了介绍,包括工艺开发期间随着工艺步骤和参数的不断优化、规模放大、提高产品质量和稳定性等进行的工艺变更。总体来说,ADC产品在生产工艺和工艺验证方面的要求与常规化学原料药/重组蛋白类基本一致,指南对需要额外关注的内容进行了说明,例如:小分子的生产工艺开发,应参照化学原料药的要求开展。根据ADC修饰和偶联反应的化学特性,合理选择和设计连接子、有效载荷和ADC分子的合成/工艺路线,参照ICH Q11及其问答(Q&A)[4]合理选择化学合成用起始物料,并制定小分子的合成工艺和质量控制策略。对于光敏感性的小分子,在特定光照波段或高强度照射下会发生化学结构的变化,而这种化学结构的变化可能会影响ADC产品的质量属性。因此,需要在生产过程中采取适当的措施(如生产环境采用黄光替代白光、中间体储存容器避光等),并在制剂灌装过程以及储存条件和包装容器的选择上开展系统性研究。裸抗与常规抗体药物生产工艺类似,但除了需关注常规抗体生产的风险点外,还需要从ADC产品分子的设计和生产的整个过程关注其对ADC原液生产过程的影响以及对最终ADC产品质量的影响。对于裸抗溶液组分的开发,除了需要确保裸抗本身的稳定性之外,还可能需要考虑与后续偶联工艺的兼容性,必要时在偶联前进行缓冲液置换等操作。在工艺优化方面,ADC产品生产工艺和供应链的复杂性对评估变更的潜在影响提出了新的挑战。裸抗、小分子的可比性评估还需考虑是否需要对ADC原液/制剂进行可比性研究或生产规模的工艺确认,并关注裸抗、小分子变更产生的质量属性的差异是否会对后续偶联工艺或ADC关键质量属性产生不良影响。因此,指南仅提出了一般性的原则要求,希望申请人在产品实际开发过程中结合品种特点和生产工艺等,具体问题具体分析。后续可随着研发和评价经验的积累适时撰写变更相关的技术指南。4.5 质量研究与质量标准ADC产品的质量研究也包括小分子部分、裸抗部分和ADC原液/制剂部分。研究者应选择有代表性的样品对产品质量开展系统、深入的研究,并根据产品的特点、生产工艺、质量研究,结合非临床和临床数据制定科学合理的质量标准。小分子的质量研究可参考化学药物相关指导原则开展,除常规的杂质分析外,还应结合杂质的结构等研究分析对后续工艺和终产品质量的影响。由于在偶联反应完成后,可偶联杂质极难量化且难以去除,需重点关注可偶联杂质的风险,应制定严格的控制标准,并提供合理的依据。裸抗的质量研究和控制要求和抗体药物的要求基本一致,还需对可能影响偶联工艺的质量属性,如抗体的氧化水平等,进行充分的研究和合理的控制。原则上,裸抗、小分子部分的控制策略与单独作为抗体药物或化学原料药的常规控制策略基本一致,但是作为ADC产品的中间产品,裸抗和小分子的控制策略还应考虑对ADC原液和制剂的影响,以及综合考虑整体生产工艺的杂质等风险及控制。在指南中也贯穿了基于风险的研发理念,研究者可以基于对产品和工艺的深入理解,具体问题具体分析,合理制定中间产品的控制策略。关于小分子杂质的分析和控制将在后文中进行重点介绍。该章节主要对ADC部分的质量研究和控制进行了阐述,ADC原液/制剂除了需要关注大分子蛋白的质量属性和小分子相关的质量属性外,还需要考虑偶联引起的关键质量属性,采用适宜的、先进的分析技术,从结构确证、理化性质、生物学活性和杂质研究等角度进行全面研究,并根据产品特点、生产工艺、质量研究和稳定性研究,结合非临床和临床数据制定科学合理的质量标准。指南对常见的研究项目和分析方法进行了举例,所列举的项目并不一定包括全部的研究项目,也需要结合具体的品种特点以及技术的发展选择适宜的分析方法,如电荷变异体分析,需结合产品特性,如小分子的特性(尤其是电荷)以及偶联位点的选择(如赖氨酸、链间巯基、半胱氨酸等)等,需考虑小分子可能与分离介质产生非特异性的相互作用等情况,选择适宜的1种或多种方法进行分析。5重点问题说明5.1 关于小分子杂质的考虑基于目前ADC产品常见的合成路线,指南中采用“小分子”指代与裸抗偶联的组分,如裸抗首先与连接子反应后,进一步与有效载荷反应形成ADC原液,则连接子、有效载荷均为小分子。若首先合成有效载荷⁃连接子复合物,然后进一步与裸抗反应获得ADC原液,则有效载荷⁃连接子为小分子。在ADC产品中,小分子的质量控制还应考虑对后续生产工艺以及ADC产品关键质量属性的影响,尤其是杂质方面。杂质相关的风险,可以通过中间产品的质量控制以及下游步骤中稳健的纯化能力来进行控制。因此,需要基于对杂质的深入了解和研究,结合先验知识、风险评估等建立控制策略。对于小分子而言,杂质可能包括有机杂质(包括潜在的致突变杂质)、无机杂质以及残留溶剂等。以小分子为有效载荷⁃连接子为例,小分子杂质的来源可能包括合成小分子过程中产生以及在ADC层面产生(如ADC原液和制剂的生产或储存过程中)。基于杂质的类型、结构等特点,结合去向(杂质是否参与偶联反应)研究和清除(杂质是否通过后续工艺被去除)研究等综合评估风险,制定合理的杂质控制策略。根据药物开发的基本原则,在小分子中间产品的质控中对合成过程中产生的小分子杂质进行控制是最优的。尤其是可偶联的杂质,因为此类杂质一旦偶联后,很难分离和去除,因此需重点关注,参照化学原料药的要求制定严格的控制标准。对于不可偶联杂质,可根据后续工艺的清除能力建立合理的控制策略,提供充足的研究数据。在ADC层面产生的小分子相关杂质,来源可能是工艺添加或降解产物、副反应产物等。应开展充分的工艺表征、质量研究以及稳定性研究等,以便深入了解该类杂质的形成阶段和变化情况,制定合理的控制策略。对于游离的小分子杂质,例如:未与裸抗偶联的有效载荷⁃连接子、游离降解产物、残留溶剂、元素杂质等,后续工艺中的层析和/或超滤/渗滤等纯化步骤,可以去除该类杂质。而偶联在裸抗上的小分子杂质,由于目前的分析手段无法直接进行分离和去除,因此对该类杂质的分析和控制策略提出了挑战。基于当前的经验,可以在工艺表征和质量研究中通过强降解富集杂质,评估富集到的杂质的代表性,是否能够代表产品实际的生产过程、储存过程中产生的杂质,对此类杂质进行鉴定、毒性研究等,从而间接对该类杂质进行风险评估并进行控制。也可以在小分子中间产品研究中,模拟后续工艺和储存条件等,开展小分子杂质谱、降解谱等研究,建立潜在杂质库进行分析,间接对此类偶联杂质进行分析和评估。考虑到在ADC层面对该类杂质分析控制的难度较高,建议在工艺开发的早期对该类杂质进行研究,必要时通过优化工艺和处方、优化连接子的结构等方法减少杂质的产生。5.2 关于“混批”的考虑考虑到ADC产品的异质性高、工艺复杂等特点,小分子、裸抗和原液的多环节混批可能会给产品质量和可溯源性带来较大风险,应基于风险进行要求。因此,在本指南中仅提出原则性的建议“应关注上下游的匹配性,生产过程中应尽量避免混批操作”。随着偶联技术和分析技术的进步,ADC产品未来可能会具有更高的均一性,基于具体品种具体分析的原则,可以对“混批”操作有更灵活的要求。原则上不鼓励“混批”操作,申请人可以结合产品特点、工艺特点开展充分的研究和风险评估,基于风险的研发理念和具体品种具体分析的原则,提供充足的研究数据,建议研发者就具体问题与药审中心开展沟通交流。6总结和展望近年来,随着技术的不断进步和创新,ADC产品在肿瘤治疗领域取得了显著的成效。本文结合指南的起草背景、起草过程、主要内容、重点问题说明等,对指南进行了解读,以便业界能够更好地理解和应用该指南。基于ADC的分子结构特点,在分子设计和作用机制上可能会有更多的创新组合,也给药学研究带来了更多的挑战,例如:双载荷的ADC,偶联工艺更为复杂,尤其是双点双药这种连接方式,引入了双套机制,对于工艺开发、质控策略、分析方法等均提出了更高的要求。未来,随着对这类复杂治疗药物的深入理解和技术的进步,后续将逐步修订和完善指导原则。另外,对于创新程度较高的产品,可能需要更加灵活的监管方式,ADC产品需要更复杂的控制策略,对产品和工艺的深入理解可以为更加灵活的监管方式提供依据。也希望通过业界、政府、监管机构的共同努力,促进ADC产品为癌症患者提供更为精准和有效的治疗手段。参考文献详见《中国新药杂志》 2025年 第34卷 第6期文章信息源于公众号凡默谷,登载该文章目的为更广泛的传递行业信息,不代表赞同其观点或对其真实性负责。文章版权归原作者及原出处所有,文章内容仅供参考。本网拥有对此声明的最终解释权,若无意侵犯版权,请联系小编删除。学如逆水行舟,不进则退;心似平原走马,易放难收。行舟Drug每日更新 欢迎订阅+医药大数据|行业动态|政策解读
抗体药物偶联物上市批准申请上市临床1期
2025-04-09
The therapy was discovered and developed by AbbVie. Credit: © AbbVie Inc. All rights reserved.
The European Commission (EC) has granted marketing authorisation for AbbVie’s once-a-day treatment Rinvoq (upadacitinib) 15mg for adults with giant cell arteritis (GCA).
It is the first and only oral Janus kinase inhibitor approved in the European Union, Liechtenstein, Norway and Iceland, for this indication.
GCA is an autoimmune condition, predominantly affecting individuals over 50, with the highest incidence between 70 and 80 years of age.
The condition leads to the inflammation of the aorta, the temporal and cranial arteries, and other large and medium arteries.
The authorisation of Rinvoq is based on data from the multicentre Phase III SELECT-GCA trial, which was structured to assess the efficacy and safety of the therapy in 428 GCA subjects.
The trial met its primary and key secondary endpoints, demonstrating that 46.4% of subjects treated with 15 mg of the therapy plus a steroid taper regimen for 26 weeks achieved sustained remission at week 52 versus 29% of those on placebo with a steroid taper regimen.
AbbVie research and development, chief scientific officer and executive vice-president Roopal Thakkar stated: “The EC approval of Rinvoq in GCA provides patients and physicians with a new treatment option and the first oral advanced therapy for adults living with GCA – a particularly vulnerable population due to older age and frequent comorbidities.”
The therapy has previously gained approval in the EU for conditions including psoriatic arthritis, radiographic axial spondylarthritis and Crohn’s disease.
Rinvoq has been discovered and developed by company scientists and is currently under investigation for other immune-mediated inflammatory conditions.
It is also undergoing Phase III trials for alopecia areata, hidradenitis suppurativa, Takayasu arteritis, vitiligo and systemic lupus erythematosus.
In March 2025, the
company announced a $2.3bn licensing agreement
to acquire global rights to the long-acting amylin analogue, GUB014295, from Danish biotech Gubra.
临床3期上市批准引进/卖出临床结果
2025-04-08
RINVOQ is the first and only oral Janus kinase (JAK) inhibitor approved in the European Union (EU) to treat adult patients with giant cell arteritis (GCA)
The approval is supported by data from the pivotal Phase 3 SELECT-GCA trial which demonstrated that RINVOQ achieved the primary endpoint of sustained remission* and key secondary endpoints, including reduction in disease flares, lower cumulative steroid exposure and complete remission †1
This marks the eighth approved indication for RINVOQ in the EU2
NORTH CHICAGO, Ill., April 8, 2025 /PRNewswire/ -- AbbVie (NYSE: ABBV) today announced that the European Commission (EC) granted marketing authorization to RINVOQ® (upadacitinib; 15 mg, once daily) for the treatment of giant cell arteritis (GCA) in adult patients. RINVOQ is the first and only oral JAK inhibitor approved in the EU, as well as Iceland, Liechtenstein and Norway, for the treatment of adult patients with GCA.
"GCA is a challenging and often debilitating condition. Patients may endure headaches, jaw pain and muscle aches, with many fearing sudden and permanent vision loss,"3 said Prof. Dr. med. Wolfgang Schmidt, M.D., MACR, Waldfriede Hospital, Department of Rheumatology, Berlin, Germany, and SELECT-GCA trial investigator. "Results from the SELECT-GCA trial show that patients can achieve sustained remission and reduce their cumulative steroid exposure with RINVOQ, addressing important patient goals in the treatment of GCA."
GCA is an autoimmune disease that causes inflammation of the temporal and other cranial arteries, the aorta, and other large and medium arteries. GCA generally impacts patients older than 50 years, most commonly between the ages of 70 and 80 years.3
"The EC approval of RINVOQ in GCA provides patients and physicians with a new treatment option and the first oral advanced therapy for adults living with GCA – a particularly vulnerable population due to older age and frequent comorbidities,"3,4 said Roopal Thakkar, M.D., executive vice president, research & development, chief scientific officer, AbbVie. "This exciting milestone demonstrates our commitment to ongoing research and expanding indications in areas of high unmet need to help patients achieve better outcomes, including sustained disease remission."
The EC approval is supported by data from the Phase 3 SELECT-GCA trial, which was recently published in the New England Journal of Medicine.1 In this trial, primary and key secondary endpoints were achieved with RINVOQ 15 mg and a 26-week steroid taper regimen compared to placebo in combination with a 52-week steroid taper regimen.1
Primary endpoint results from the Phase 3 SELECT-GCA trial demonstrated:
Sustained remission*: 46.4% of patients receiving RINVOQ 15 mg in combination with a 26-week steroid taper regimen achieved sustained remission at week 52, compared with 29.0% of patients receiving placebo in combination with a 52-week steroid taper regimen (p=0.002).1
Key secondary endpoints included:
Reduction in disease flares: 34.3% of patients receiving RINVOQ 15 mg in combination with a 26-week steroid taper regimen experienced at least one disease flare through week 52 versus 55.6% of patients receiving placebo in combination with a 52-week steroid taper regimen (p=0.001).1
Lower cumulative steroid exposure: Through 52 weeks, cumulative steroid exposure was significantly lower for patients receiving RINVOQ 15 mg in combination with a 26-week steroid taper regimen than for patients receiving placebo in combination with a 52-week steroid taper regimen (median exposure of 1615 mg versus 2882 mg, respectively; p<0.001).1
Sustained complete remission†: 37.1% of patients receiving RINVOQ 15 mg in combination with a 26-week steroid taper regimen achieved sustained complete remission through week 52, compared with 16.1% of patients receiving placebo in combination with a 52-week steroid taper regimen (p<0.001).1
During the 52-week, placebo-controlled period, the safety profile of RINVOQ was generally consistent with that observed in other approved indications.2 Similar rates of serious adverse events were observed in patients receiving RINVOQ 15 mg and in those receiving placebo.1 Serious infections occurred in 5.7% of the RINVOQ 15 mg group and 10.7% of the placebo group.1 The proportions of patients with events of interest were balanced across treatment groups for incidence of malignancy (excluding nonmelanoma skin cancer; 1.9% in the RINVOQ 15 mg group vs 1.8% in the placebo group) and venous thromboembolism (3.3% in the RINVOQ 15 mg group vs 3.6% in the placebo group).1 There were no adjudicated major adverse cardiac events (MACEs) in the RINVOQ 15 mg group, compared with two events in the placebo group.1 Four treatment-emergent deaths were reported, two in the placebo group and two in the RINVOQ 15 mg group. Of the two treatment-emergent deaths in the RINVOQ 15 mg group, one was attributed to COVID-19 and the other was adjudicated as an unexplained cause.1
RINVOQ is approved in the EU for the treatment of adults with radiographic axial spondylarthritis, nonradiographic axial spondylarthritis, psoriatic arthritis, rheumatoid arthritis, ulcerative colitis, Crohn's disease, adults and adolescents with atopic dermatitis, and now adults with GCA.2
*Sustained remission is defined as having an absence of GCA signs and symptoms from week 12 through week 52 and adherence to the protocol-defined steroid taper over the course of the study term.1
†Sustained complete remission is defined as having an absence of GCA signs and symptoms from week 12 through week 52, adherence to the protocol-defined steroid taper, and normalization of both erythrocyte sedimentation rate and high-sensitivity C-reactive protein from week 12 through week 52.1
About Giant Cell Arteritis
Giant cell arteritis (GCA), also known as temporal arteritis, is an autoimmune disease of medium and large arteries, characterized by granulomatous inflammation of the three-layered vessel wall, which affects temporal and other cranial arteries as well as the aorta and other large arteries.3,5 GCA can cause headache, jaw pain, and changes in or loss of vision, including sudden and permanent loss of vision.3 It is the most common vasculitis affecting adults in western countries.3 White women over the age of 50 – most commonly between the ages of 70 and 80 years – have the highest risk of developing GCA. Although women are more likely than men to develop GCA, research suggests that men are more likely to have ocular manifestations with their disease.6
About SELECT-GCA
SELECT-GCA (M16-852) is a Phase 3, multicenter, randomized, double-blind placebo-controlled study designed to evaluate the safety and efficacy of upadacitinib in 428 patients with GCA. The study consists of two parts. The first part, which is reported in this release, evaluated the efficacy of upadacitinib in combination with a 26-week corticosteroid taper regimen compared with placebo in combination with a 52-week corticosteroid taper regimen. In addition, the study assessed the safety and tolerability of upadacitinib in these patients. The efficacy and safety of withdrawing versus continuing upadacitinib in maintaining remission in participants who achieved sustained remission in the first part will be evaluated in the second part of the study.7
Top-line results of part one of the study were shared in April 2024. For more information regarding this study, please visit ClinicalTrials.gov (identifier: NCT03725202).
About Upadacitinib (RINVOQ®)
Discovered and developed by AbbVie scientists, RINVOQ is a selective and reversible JAK inhibitor that is being studied in several immune-mediated inflammatory diseases.2,8 In human cellular assays, RINVOQ preferentially inhibits signaling by JAK1 or JAK 1/3 with functional selectivity over cytokine receptors that signal via pairs of JAK2.2 Upadacitinib (RINVOQ) is being studied in Phase 3 clinical trials for alopecia areata, giant cell arteritis, hidradenitis suppurativa, Takayasu arteritis, systemic lupus erythematosus and vitiligo.9-14
EU Indications and Important Safety Information about RINVOQ® (upadacitinib)2
Indications
Giant cell arteritis
RINVOQ is indicated for the treatment of giant cell arteritis (GCA) in adult patients.
Rheumatoid arthritis
RINVOQ is indicated for the treatment of moderate to severe active rheumatoid arthritis (RA) in adult patients who have responded inadequately to, or who are intolerant to one or more disease-modifying anti-rheumatic drugs (DMARDs). RINVOQ may be used as monotherapy or in combination with methotrexate.
Psoriatic arthritis
RINVOQ is indicated for the treatment of active psoriatic arthritis (PsA) in adult patients who have responded inadequately to, or who are intolerant to one or more DMARDs. RINVOQ may be used as monotherapy or in combination with methotrexate.
Axial spondyloarthritis
Non-radiographic axial spondyloarthritis (nr-axSpA)
RINVOQ is indicated for the treatment of active non-radiographic axial spondyloarthritis in adult patients with objective signs of inflammation as indicated by elevated C-reactive protein (CRP) and/or magnetic resonance imaging (MRI), who have responded inadequately to nonsteroidal anti-inflammatory drugs (NSAIDs).
Ankylosing spondylitis (AS, radiographic axial spondyloarthritis)
RINVOQ is indicated for the treatment of active ankylosing spondylitis in adult patients who have responded inadequately to conventional therapy.
Atopic dermatitis
RINVOQ is indicated for the treatment of moderate to severe atopic dermatitis (AD) in adults and adolescents 12 years and older who are candidates for systemic therapy.
Ulcerative colitis
RINVOQ is indicated for the treatment of adult patients with moderately to severely active ulcerative colitis (UC) who have had an inadequate response, lost response or were intolerant to either conventional therapy or a biologic agent.
Crohn's disease
RINVOQ is indicated for the treatment of adult patients with moderately to severely active Crohn's disease who have had an inadequate response, lost response or were intolerant to either conventional therapy or a biologic agent.
Important Safety Information
Contraindications
RINVOQ is contraindicated in patients hypersensitive to the active substance or to any of the excipients, in patients with active tuberculosis (TB) or active serious infections, in patients with severe hepatic impairment, and during pregnancy.
Special warnings and precautions for use
RINVOQ should only be used if no suitable treatment alternatives are available in patients:
65 years of age and older;
patients with history of atherosclerotic cardiovascular (CV) disease or other CV risk factors (such as current or past long-time smokers);
patients with malignancy risk factors (e.g. current malignancy or history of malignancy)
Use in patients 65 years of age and older
Considering the increased risk of MACE, malignancies, serious infections, and all-cause mortality in patients ≥65 years of age, as observed in a large randomised study of tofacitinib (another JAK inhibitor), RINVOQ should only be used in these patients if no suitable treatment alternatives are available. In patients ≥65 years of age, there is an increased risk of adverse reactions with RINVOQ 30 mg once daily. Consequently, the recommended dose for long-term use in this patient population is 15 mg once daily.
Immunosuppressive medicinal products
Use in combination with other potent immunosuppressants is not recommended.
Serious infections
Serious and sometimes fatal infections have been reported in patients receiving RINVOQ. The most frequent serious infections reported included pneumonia and cellulitis. Cases of bacterial meningitis and sepsis have been reported with RINVOQ. Among opportunistic infections, TB, multidermatomal herpes zoster, oral/esophageal candidiasis, and cryptococcosis have been reported. RINVOQ should not be initiated in patients with an active, serious infection, including localized infections. RINVOQ should be interrupted if a patient develops a serious or opportunistic infection until the infection is controlled. A higher rate of serious infections was observed with RINVOQ 30 mg compared to 15 mg. As there is a higher incidence of infections in the elderly and patients with diabetes in general, caution should be used when treating these populations. In patients ≥65 years of age, RINVOQ should only be used if no suitable treatment alternatives are available.
Tuberculosis
Patients should be screened for TB before starting RINVOQ. RINVOQ should not be given to patients with active TB. Anti-TB therapy may be appropriate for select patients in consultation with a physician with expertise in the treatment of TB. Patients should be monitored for the development of signs and symptoms of TB.
Viral reactivation
Viral reactivation, including cases of herpes zoster, was reported in clinical studies. The risk of herpes zoster appears to be higher in Japanese patients treated with RINVOQ. Consider interruption of RINVOQ if the patient develops herpes zoster until the episode resolves. Screening for viral hepatitis and monitoring for reactivation should occur before and during therapy. If hepatitis B virus DNA is detected, a liver specialist should be consulted.
Vaccination
The use of live, attenuated vaccines during or immediately prior to therapy is not recommended. It is recommended that patients be brought up to date with all immunizations, including prophylactic zoster vaccinations, prior to initiating RINVOQ, in agreement with current immunization guidelines.
Malignancy
Lymphoma and other malignancies have been reported in patients receiving JAK inhibitors, including RINVOQ. In a large randomised active controlled study of tofacitinib (another JAK inhibitor) in RA patients ≥50 years of age with ≥ 1 additional CV risk factor, a higher rate of malignancies, particularly lung cancer, lymphoma, and non-melanoma skin cancer (NMSC), was observed with tofacitinib compared to tumour necrosis factor (TNF) inhibitors. A higher rate of malignancies, including NMSC, was observed with RINVOQ 30 mg compared to 15 mg. Periodic skin examination is recommended for all patients, particularly those with risk factors for skin cancer. In patients ≥65 years of age, patients who are current or past long-time smokers, or patients with other malignancy risk factors (e.g., current malignancy or history of malignancy), RINVOQ should only be used if no suitable treatment alternatives are available.
Hematological abnormalities
Treatment should not be initiated, or should be temporarily interrupted, in patients with hematological abnormalities observed during routine patient management.
Gastrointestinal Perforations
Events of diverticulitis and gastrointestinal perforations have been reported in clinical trials and from post-marketing sources. RINVOQ should be used with caution in patients who may be at risk for gastrointestinal perforation (e.g., patients with diverticular disease, a history of diverticulitis, or who are taking nonsteroidal antiinflammatory drugs (NSAIDs), corticosteroids, or opioids). Patients with active Crohn's disease are at increased risk for developing intestinal perforation. Patients presenting with new onset abdominal signs and symptoms should be evaluated promptly for early identification of diverticulitis or gastrointestinal perforation.
Major adverse cardiovascular events
MACE were observed in clinical studies of RINVOQ. In a large randomised active-controlled study of tofacitinib (another JAK inhibitor) in RA patients ≥50 years of age with ≥1 additional CV risk factor, a higher rate of MACE, defined as CV death, non-fatal myocardial infarction and non-fatal stroke, was observed with tofacitinib compared to TNF inhibitors. Therefore, in patients ≥65 years of age, patients who are current or past long-time smokers, and patients with history of atherosclerotic CV disease or other CV risk factors, RINVOQ should only be used if no suitable treatment alternatives are available.
Lipids
RINVOQ treatment was associated with dose-dependent increases in lipid parameters, including total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol.
Hepatic transaminase elevations
Treatment with RINVOQ was associated with an increased incidence of liver enzyme elevation. Hepatic transaminases must be evaluated at baseline and thereafter according to routine patient management. If alanine transaminase (ALT) or aspartate transaminase (AST) increases are observed and drug-induced liver injury is suspected, RINVOQ should be interrupted until this diagnosis is excluded.
Venous thromboembolism
Events of deep venous thrombosis (DVT) and pulmonary embolism (PE) were observed in clinical trials for RINVOQ. In a large randomised active-controlled study of tofacitinib (another JAK inhibitor) in RA patients ≥50 years of age with ≥1 additional CV risk factor, a dose dependent higher rate of VTE including DVT and PE was observed with tofacitinib compared to TNF inhibitors. In patients with CV or malignancy risk factors, RINVOQ should only be used if no suitable treatment alternatives are available. In patients with known VTE risk factors other than CV or malignancy risk factors (e.g. previous VTE, patients undergoing major surgery, immobilisation, use of combined hormonal contraceptives or hormone replacement therapy, and inherited coagulation disorder), RINVOQ should be used with caution. Patients should be re-evaluated periodically to assess for changes in VTE risk. Promptly evaluate patients with signs and symptoms of VTE and discontinue RINVOQ in patients with suspected VTE.
Hypersensitivity reactions
Serious hypersensitivity reactions such as anaphylaxis and angioedema have been reported in patients receiving RINVOQ. If a clinically significant hypersensitivity reaction occurs, discontinue RINVOQ and institute appropriate therapy.
Hypoglycemia in patients treated for diabetes
There have been reports of hypoglycemia following initiation of JAK inhibitors, including RINVOQ, in patients receiving medication for diabetes. Dose adjustment of anti-diabetic medication may be necessary in the event that hypoglycemia occurs.
Medication Residue in Stool
Reports of medication residue in stool or ostomy output have occurred in patients taking RINVOQ. Most reports described anatomic (e.g., ileostomy, colostomy, intestinal resection) or functional gastrointestinal conditions with shortened gastrointestinal transit times. Patients should be instructed to contact their healthcare professional if medication residue is observed repeatedly. Patients should be clinically monitored, and alternative treatment should be considered if there is an inadequate therapeutic response.
Giant Cell Arteritis
RINVOQ monotherapy should not be used for the treatment of acute relapses as efficacy in this setting has not been established. Glucocorticoids should be given according to medical judgement and practice guidelines.
Adverse reactions
The most commonly reported adverse reactions in RA, PsA, and axSpA clinical trials (≥2% of patients in at least one of the indications) with RINVOQ 15 mg were upper respiratory tract infections, blood creatine phosphokinase (CPK) increased, ALT increased, bronchitis, nausea, neutropenia, cough, AST increased, and hypercholesterolemia. Overall, the safety profile observed in patients with psoriatic arthritis or active axial spondyloarthritis treated with RINVOQ 15 mg was consistent with the safety profile observed in patients with RA.
The most commonly reported adverse reactions in AD trials (≥2% of patients) with RINVOQ 15 mg or 30 mg were upper respiratory tract infection, acne, herpes simplex, headache, blood CPK increased, cough, folliculitis, abdominal pain, nausea, neutropenia, pyrexia, and influenza. Dose dependent increased risks of infection and herpes zoster were observed with RINVOQ. The safety profile for RINVOQ 15 mg in adolescents was similar to that in adults. With long-term exposure, skin papilloma was reported in adolescents in the RINVOQ 15 mg and 30 mg groups.
The most commonly reported adverse reactions in the UC and CD trials (≥3% of patients) with RINVOQ 45 mg, 30 mg or 15 mg were upper respiratory tract infection, pyrexia, blood CPK increased, anemia, headache, acne, herpes zoster, neutropenia, rash, pneumonia, hypercholesterolemia, bronchitis, AST increased, fatigue, folliculitis, ALT increased, herpes simplex, and influenza. The overall safety profile observed in patients with UC was generally consistent with that observed in patients with RA. Overall, the safety profile observed in patients with CD treated with RINVOQ was consistent with the known safety profile for RINVOQ.
The most common serious adverse reactions were serious infections.
The safety profile of RINVOQ with long-term treatment was generally similar to the safety profile during the placebo-controlled period across indications.
Overall, the safety profile observed in patients with GCA treated with RINVOQ 15 mg was generally consistent with the known safety profile for RINVOQ.
This is not a complete summary of all safety information.
See RINVOQ full Summary of Product Characteristics (SmPC) at
Globally, prescribing information varies; refer to the individual country product label for complete information.
About AbbVie in Rheumatology
For more than 20 years, AbbVie has been dedicated to improving care for people living with rheumatic diseases. Anchored by a longstanding commitment to discovering and delivering transformative therapies, we pursue cutting-edge science that improves our understanding of promising new pathways and targets, ultimately helping more people living with rheumatic diseases reach their treatment goals. For more information, visit AbbVie in rheumatology.
About AbbVie
AbbVie's mission is to discover and deliver innovative medicines and solutions that solve serious health issues today and address the medical challenges of tomorrow. We strive to have a remarkable impact on people's lives across several key therapeutic areas including immunology, oncology, neuroscience and eye care – and products and services in our Allergan Aesthetics portfolio. For more information about AbbVie, please visit us at . Follow @abbvie on LinkedIn, Facebook, Instagram, X (formerly Twitter), and YouTube.
Forward-Looking Statements
Some statements in this news release are, or may be considered, forward-looking statements for purposes of the Private Securities Litigation Reform Act of 1995. The words "believe," "expect," "anticipate," "project" and similar expressions and uses of future or conditional verbs, generally identify forward-looking statements. AbbVie cautions that these forward-looking statements are subject to risks and uncertainties that may cause actual results to differ materially from those expressed or implied in the forward-looking statements. Such risks and uncertainties include, but are not limited to, challenges to intellectual property, competition from other products, difficulties inherent in the research and development process, adverse litigation or government action, and changes to laws and regulations applicable to our industry. Additional information about the economic, competitive, governmental, technological and other factors that may affect AbbVie's operations is set forth in Item 1A, "Risk Factors," of AbbVie's 2024 Annual Report on Form 10-K, which has been filed with the Securities and Exchange Commission, as updated by its subsequent Quarterly Reports on Form 10-Q. AbbVie undertakes no obligation, and specifically declines, to release publicly any revisions to forward-looking statements as a result of subsequent events or developments, except as required by law.
References
Blockmans D, Penn SK, Setty AR, et al. A phase 3 trial of upadacitinib for giant-cell arteritis. N Engl J Med. Published online April 2, 2025; doi:10.1056/NEJMoa2413449.
RINVOQ. Summary of Product Characteristics. AbbVie; 2025.
Ameer MA, Peterfy RJ, Khazaeni B. Giant cell arteritis (temporal arteritis). Updated August 8, 2023.
Mohammad AJ, Englund M, Turesson C, et al. Rate of Comorbidities in Giant Cell Arteritis: A Population-based Study. J Rheumatol. 2017;44(1):84-90. doi:10.3899/jrheum.160249
Weyand CM, Goronzy JJ. Immunology of giant cell arteritis. Circ Res. 2023;132(2):238-250. doi:10.1161/CIRCRESAHA.122.322128
Giant cell arteritis. Arthritis Foundation. Accessed January 9, 2025.
AbbVie. Data on file: ABVRRTI78418.
Pipeline. AbbVie. 2023. Accessed January 9, 2025.
A study to evaluate the safety and efficacy of upadacitinib in participants with giant cell arteritis (SELECT-GCA). ClinicalTrials.gov identifier: NCT03725202. Accessed January 9, 2025.
A study to evaluate the efficacy and safety of upadacitinib in participants with Takaysu arteritis (TAK) (SELECT-TAK). ClinicalTrials.gov identifier: NCT04161898. Accessed January 9, 2025.
Program to assess adverse events and change in disease activity of oral upadacitinib in adult participants with moderate to severe systemic lupus erythematosus (SELECT-SLE). ClinicalTrials.gov identifier: NCT05843643. Accessed January 9, 2025.
A study to assess change in disease activity and adverse events of oral upadacitinib in adult and adolescent participants with moderate to severe hidradenitis suppurativa who have failed anti-TNF therapy (Step-Up HS). ClinicalTrials.gov identifier: NCT05889182. Accessed January 9, 2025.
A study to assess adverse events and effectiveness of upadacitinib oral tablets in adult and adolescent participants with vitiligo (Viti-Up). ClinicalTrials.gov identifier: NCT06118411. Accessed January 9, 2025.
A study to evaluate the safety and effectiveness of upadacitinib tablets in adult and adolescent participants with severe alopecia areata (UP-AA). ClinicalTrials.gov identifier: NCT06012240. Accessed January 9, 2025.
SOURCE AbbVie
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果临床3期上市批准细胞疗法
分析
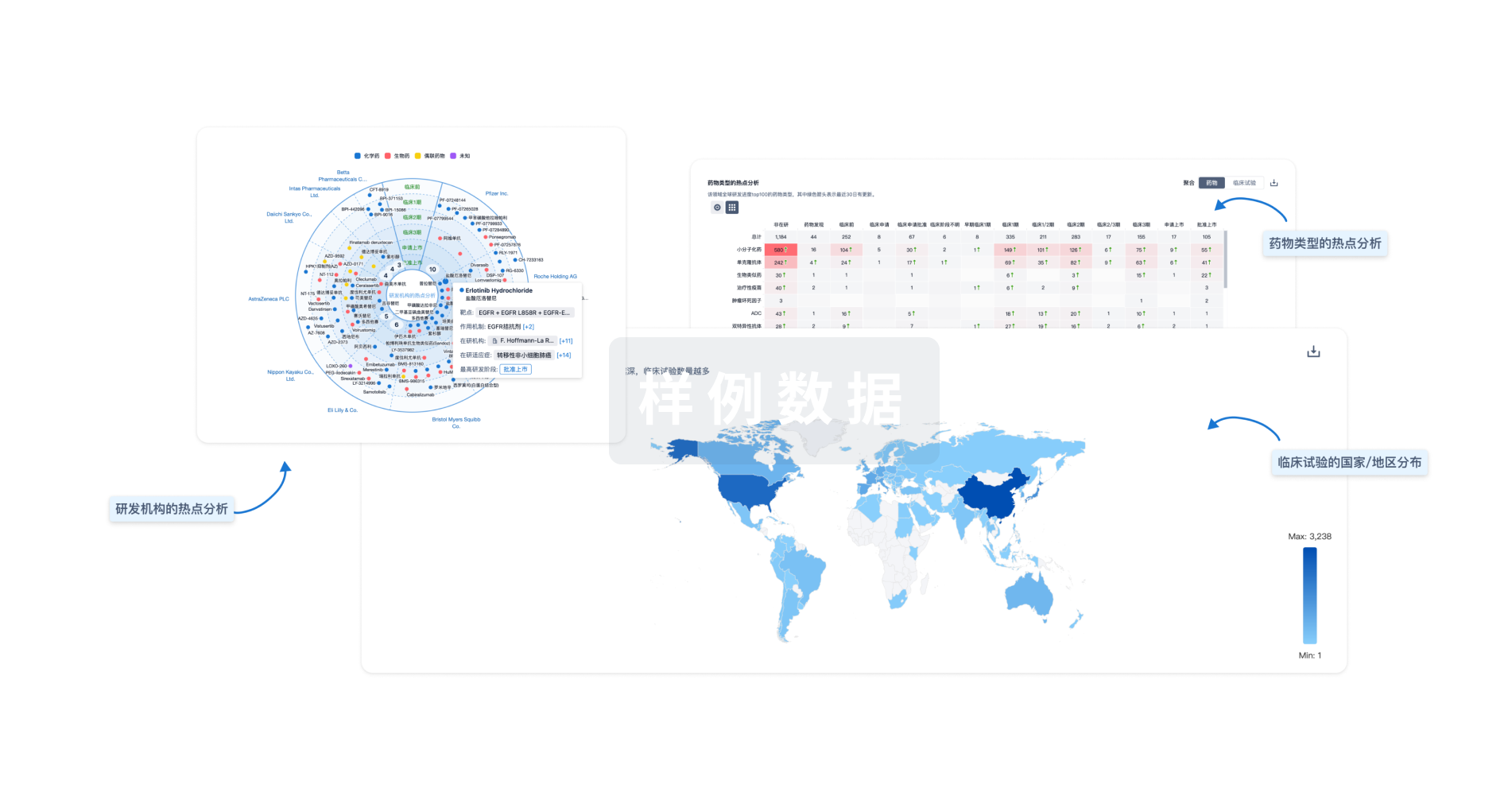
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用




