预约演示
更新于:2025-05-07
Prostatic Intraepithelial Neoplasia
前列腺上皮内瘤变
更新于:2025-05-07
基本信息
别名 Intraepithelial Neoplasia, Prostatic、Intraepithelial Neoplasm, Prostatic、Intraepithelial Neoplasms, Prostatic + [27] |
简介 A premalignant change arising in the prostatic epithelium, regarded as the most important and most likely precursor of prostatic adenocarcinoma. The neoplasia takes the form of an intra-acinar or ductal proliferation of secretory cells with unequivocal nuclear anaplasia, which corresponds to nuclear grade 2 and 3 invasive prostate cancer. |
关联
3
项与 前列腺上皮内瘤变 相关的药物靶点- |
作用机制 免疫刺激剂 |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
28
项与 前列腺上皮内瘤变 相关的临床试验NCT05463796
InAdvance: Surveillance, Prevention, and Interception in a Population at Risk For Cancer
This research study is creating a way to collect and store specimens and information from participants who may be at an increased risk of developing cancer, or has been diagnosed with an early phase of a cancer or a family member who has a family member with a precursor condition for cancer.
* The objective of this study is to identify exposures as well as clinical, molecular, and pathological changes that can be used to predict early development of cancer, malignant transformation, and risks of progression to symptomatic cancer that can ultimately be fatal.
* The ultimate goal is to identify novel markers of early detection and risk stratification to drive potential therapeutic approaches to intercept progression to cancer.
* The objective of this study is to identify exposures as well as clinical, molecular, and pathological changes that can be used to predict early development of cancer, malignant transformation, and risks of progression to symptomatic cancer that can ultimately be fatal.
* The ultimate goal is to identify novel markers of early detection and risk stratification to drive potential therapeutic approaches to intercept progression to cancer.
开始日期2023-04-25 |
CTR20223306
重组九价人乳头瘤病毒(6/11/16/18/31/33/45/52/58型)疫苗(大肠埃希菌)在中国18-45岁男性中的安全性、有效性和免疫原性的多中心、随机、双盲、安慰剂对照Ⅲ期临床试验
评价重组九价人乳头瘤病毒(6/11/16/18/31/33/45/52/58型)疫苗(大肠埃希菌)在中国18-45岁男性中的保护效力、免疫原性和安全性
开始日期2022-12-18 |
申办/合作机构 |
ChiCTR2200065900
Clinical study on huanglian ointment in preventing infection of kirschner wire in children
开始日期2022-12-01 |
申办/合作机构- |
100 项与 前列腺上皮内瘤变 相关的临床结果
登录后查看更多信息
100 项与 前列腺上皮内瘤变 相关的转化医学
登录后查看更多信息
0 项与 前列腺上皮内瘤变 相关的专利(医药)
登录后查看更多信息
4,208
项与 前列腺上皮内瘤变 相关的文献(医药)2025-05-01·Journal of Pediatric Orthopaedics B
Femoral shaft fractures in preschool children: external fixation and elastic intramedullary nail treatments in clinical practice
Article
作者: Song, Baojian ; Wang, Qiang ; Wen, Yuwei ; Feng, Wei ; Zhu, Danjiang ; Guo, Jiale
2025-05-01·American Journal of Surgical Pathology
Validation as a Marker of Unsampled Adverse Pathology in a Clinicopathologic Series of 142 New Patients
Article
作者: Bhattarai, Roshan ; Liu, Xuefeng ; Schwen, Zeyad ; Nguyen, Jane K. ; Cox, Roni M. ; Weight, Christopher J. ; Williamson, Sean R. ; Przybycin, Christopher G. ; Alaghehbandan, Reza ; McKenney, Jesse K. ; Myles, Jonathan L.
2025-04-01·Orthopedic Clinics of North America
Perioperative Risks Associated with the Use of External Fixators in Adult and Pediatric Patients with Trauma
Review
作者: Pretell-Mazzini, Juan A ; Mendez-Guerra, Carolina ; Inchaustegui, Maria L ; Gonzalez, Marcos R ; de la Blanca, Juan Carlos G
16
项与 前列腺上皮内瘤变 相关的新闻(医药)2025-04-05
文章探讨前列腺癌治疗现状及挑战,着重分析 mRNA 疫苗在前列腺癌治疗中的应用,涵盖抗原选择、临床试验、优化策略等方面,指出其虽面临挑战,但具有潜力。前列腺癌概述与治疗现状疾病特征与分期:在英国男性中,前列腺癌是常见癌症。其发展从前列腺上皮内瘤变(PIN)到高级别 PIN(HG - PIN),最终形成腺癌并转移。疾病分为局限性、局部晚期和转移性三个阶段,不同阶段的生存率差异显著,转移性前列腺癌 5 年生存率约 30%。现有治疗手段:治疗方法包括免疫疗法、放疗、激素疗法、手术和化疗。局限性或局部晚期前列腺癌的一线治疗是根治性前列腺切除术或放疗,转移性前列腺癌通常采用化疗。不同治疗方法各有优劣,如根治性前列腺切除术虽可治愈部分患者,但存在勃起功能障碍和尿失禁等副作用;化疗药物多西他赛可延长患者生存期,但也有一定不良反应 。前列腺癌中的抗原肿瘤相关抗原(TAA):TAA 在癌细胞中高表达,在正常细胞中低表达,是癌症疫苗的潜在靶点。常见的前列腺癌 TAA 包括 PSMA、PSCA、PSA 等。与单价疫苗相比,多价疫苗能引发更广泛的免疫反应,如 CV9103 疫苗编码多种抗原,在临床试验中展现出一定优势。其他抗原性基因:p53、PTEN 和 SPOP 等基因在前列腺癌中易发生突变。突变的 p53 在肿瘤细胞中常过表达,可作为选择性癌症治疗的靶点;PTEN 突变会导致 PI3K - AKT 通路激活,促进肿瘤生长;SPOP 也是前列腺癌中的高频突变基因。这些突变抗原相较于野生型抗原,在肿瘤细胞中特异性高,有望成为更有效的治疗靶点,但目前用于临床还面临诸多挑战。癌症抗原设计的未来方向:通过下一代测序(NGS)等技术可发现肿瘤特异性的新抗原。基于 MHC 多表位抗原构建疫苗,能提高免疫原性,利用生物信息学方法可预测 MHC 结合表位,设计更有效的表位疫苗。前列腺癌疫苗临床试验肽癌症疫苗:由 TSA/TAA 的氨基酸序列组成,能刺激免疫系统攻击癌细胞。但肽疫苗在激活 CD8 T 细胞免疫反应的同时,会激活大量 CD4 T 细胞,可能影响抗肿瘤效果。短肽半衰期短,合成长肽(SLPs)虽能诱导 CD4 和 CD8 T 细胞免疫反应,但临床效果不佳。目前可通过生物信息学方法设计 SLPs 疫苗以改善疗效。树突状细胞疫苗(DC 疫苗):DC 细胞是强大的抗原呈递细胞,DC 疫苗通过收集患者的未成熟 DC 细胞,加载肿瘤相关抗原后回输患者体内激活免疫反应。Sipuleucel - T 是首个获批的前列腺癌 DC 疫苗,可延长患者生存期。DC 疫苗与其他疗法联合使用,如与免疫检查点抑制剂联合,可能提高治疗效果 。mRNA 疫苗:与 DNA 疫苗相比,mRNA 疫苗具有蛋白表达速度快、安全性高、能触发强烈的体液和细胞免疫等优势。但部分前列腺癌 mRNA 疫苗临床试验结果不理想,如 CV9104 疫苗,可能与未修饰 mRNA 免疫原性不足、注射途径等因素有关。在 COVID - 19 疫苗中,mRNA 疫苗展现出高疗效和良好安全性,为其在癌症治疗中的应用提供了借鉴。mRNA 疫苗与其他传统疫苗比较:以 COVID - 19 疫苗为例,mRNA 疫苗(如 BNT162b2 和 mRNA - 1273)在预防 COVID - 19 方面疗效优于灭活疫苗(CoronaVac)、腺病毒疫苗(Ad26.COV2.S)和重组蛋白疫苗(Covovax),且安全性良好。mRNA 疫苗的未来前景:mRNA 疫苗可编码患者特异性基因,结合免疫检查点抑制剂等免疫疗法,有望提高疗效,目前多项相关临床试验正在进行中。提高 mRNA 疫苗效率的策略优化 5’ Cap 策略:5’ Cap 结构影响 mRNA 的翻译效率和免疫原性。Cap 1 和 Cap 2 结构(具有 2’ - O - 甲基化)能提高翻译效率、减少免疫激活。CleanCap 技术可直接生成 Cap 1 结构,提高 capping 效率,减少免疫反应,其中 CleanCap M6 可进一步提高蛋白表达。优化 5’和 3’ UTR 策略:5’ UTR 负责启动蛋白翻译,3’ UTR 调节 mRNA 稳定性。使用 α 和 β 珠蛋白序列作为 UTR,添加 Kozak 序列,可提高 mRNA 稳定性和翻译效率。优化 poly(A)策略:poly(A)位于 mRNA 3’端,影响 mRNA 半衰期和翻译效率。设计 DNA 模板序列时添加固定长度的 poly(A),可控制其长度和提高重复性。IVT - mRNA 纯化:纯化 IVT mRNA 可去除杂质,尤其是 dsRNA,避免激活先天免疫反应。常用的纯化方法有 HPLC、纤维素吸附和 Rnase III 酶降解等。未来展望:前列腺癌的治疗仍具挑战,常需联合疗法。开发 mRNA 疫苗需考虑抗原选择、mRNA 设计优化以及合适的递送途径。未来需进一步研究如何增强 mRNA 疫苗刺激 CTL 免疫反应的能力,以提高治疗效果。识别微信二维码,添加生物制品圈小编,符合条件者即可加入生物制品微信群!请注明:姓名+研究方向!版权声明本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观不本站。
疫苗信使RNA免疫疗法
2024-11-03
10月31日,奥地利维也纳医科大学与德国基尔大学研究人员合作在期刊《Molecular Cancer》上发表了研究论文,题为“Cell-autonomous IL6ST activation suppresses prostate cancer development via STAT3/ARF/p53-driven senescence and confers an immune-active tumor microenvironment”,本研究结果表明,IL6ST/STAT3在肿瘤发生过程中具有依赖于环境的特性,并且在前列腺癌进展中具有抑制肿瘤的功能,通过诱导细胞衰老和吸引免疫细胞。研究人员挑战了将阻断IL6ST/STAT3信号传递作为前列腺癌功能性治疗方法的普遍观念,并提出通过细胞自主激活IL6ST作为一种新的治疗策略。
https://molecular-cancer-biomedcentral-com.libproxy1.nus.edu.sg/articles/10.1186/s12943-024-02114-8#Sec21
背景信息
01
前列腺癌(PCa)是男性第二大常见的癌症类型,2020年全球新发病例达140万例,相关死亡病例达37.5万例。与PCa在临床和分子特征上的巨大异质性相对应,目前有多种治疗方法在使用。这些治疗方法的准确性往往受到缺乏可靠的生物标志物的限制,无法区分具有侵袭性的肿瘤和非侵袭性肿瘤。为了寻找这些生物标志物,人们发现,被称为IL6ST(也称为GP130)的细胞因子信号转导异常活动,以及IL6ST信号通路的关键下游调节因子STAT3,在炎症和癌变过程中扮演着关键角色。STAT3信号通路在PCa中异常活跃,在细胞增殖、细胞存活、血管生成和免疫逃避方面发挥着依赖于肿瘤微环境(TME)的作用。因此,进一步研究IL6ST和STAT3或其他潜在的下游靶标之间的轴或PCa中的其他潜在下游靶标,对于改善治疗策略至关重要。
其它由IL6ST激活的靶点包括SH2、SHP2、PI3K和 Hippo/YES-associated protein (YAP) 通路,这些通路本身已被与PCa相关联。同样,肿瘤抑制因子PTEN 在PCa中经常发生突变或缺失,从而导致异常的PI3K激活,促进前列腺癌发生并诱导p53依赖的细胞衰老。衰老是一种由p19ARF/p53或p16INK4A/RB途径介导的细胞周期停滞状态,已被证明可抑制PCa进展。衰老通常伴随着炎症细胞因子、趋化因子、生长因子和蛋白酶的释放,被称为衰老相关分泌表型 (SASP)。SASP 是一种双刃剑,具有肿瘤抑制和促进肿瘤生长的双重作用。调节抗肿瘤和促肿瘤衰老效应平衡的因子很可能是细胞类型特异性的,并且尚未完全理解。
IL6ST信号通路可降低体内Pten缺陷肿瘤生长
02
接下来,研究人员在19周龄的小鼠中检测了持续活跃的IL6ST信号传导的影响,发现野生型和L-gp130peKI/KI小鼠的前列腺在宏观上没有区别。正如预期的那样,PtenpeΔ/Δ小鼠出现了肉眼可见的PCa。有趣的是,同时激活IL6ST信号的小鼠(PtenpeΔ/Δ;L-gp130peKI/KI)比pten缺陷小鼠的前列腺肿瘤更小,导致PtenpeΔ/Δ;L-gp130peKI/KI比PtenpeΔ/Δ小鼠的前列腺重量显著降低。
HE染色结果显示,野生型和L-gp130peKI/KI小鼠的前列腺除1只L-gp130peKI/KI小鼠(占分析小鼠的11.1%)外,其余均无病理学特征。这只动物表现出前列腺上皮内瘤变(PIN),前列腺癌的前体。绝大多数(72.7%)PtenpeΔ/Δ小鼠发生PCa,而PtenpeΔ/Δ;L-gp130peKI/KI小鼠仅22.2%发生PCa。相反,77.8%的小鼠只表现出PIN,与PtenpeΔ/Δ小鼠相比,表现出更低的侵袭性形态学。这些发现支持IL6ST信号通路在体内前列腺癌中的肿瘤抑制作用。
IL6ST信号通路在PCa患者中促进STAT3活化、衰老上调、免疫评分升高和T细胞介导的细胞毒性
03
研究人员发现衰老和抗肿瘤免疫参与了IL6ST/STAT3信号通路的肿瘤抑制作用,为了解决研究结果与人类的相关性,研究人员根据IL6ST mRNA表达水平区分了IL6SThigh和IL6STlow组,从而细化了对TCGA-PRAD患者数据集的分析。HALLMARK基因集的fGSEA显示,与IL6STlow患者相比,“IL-6/JAK/STAT3信号传导”在IL6SThigh中上调,STAT3靶基因表达增加证明了这一点。
PCa患者中IL6ST信号通路激活STAT3信号通路,并上调衰老、免疫评分和细胞毒性
随着研究人员在体内小鼠模型中描述衰老和细胞周期调节因子的变化,研究人员进行了fGSEA,排除了任何有TP53突变的患者。对衰老相关基因集的分析表明,它们在IL6SThigh PCa患者中显著上调。为患者生存率提高提供了可能的解释。这些患者还表现出下调的细胞周期基因集和上调的p53信号。
使用ESTIMATE(一种预测肿瘤纯度的工具),以及基于基因表达数据的肿瘤组织中浸润的间质/免疫细胞,研究人员证实,由于免疫评分低,大多数PCa患者可被认为是免疫冷的。值得注意的是,较高的免疫评分与PCa患者较长的生存率相关。在患者队列中,IL6SThigh患者的免疫评分显著高于IL6STlow患者,这与免疫反应相关基因集的上调有关。此外,在TCGA-PRAD数据集中,与T细胞活化和细胞毒性,中性粒细胞和巨噬细胞相关的前20个GO-BP基因集在IL6SThigh中上调,与IL6STlow表达患者相比,强调了T细胞,中性粒细胞和巨噬细胞介导的肿瘤防御在IL6ST高表达的PCa患者中的相关性。综上所述,本研究数据表明,IL6ST高表达的PCa患者表现出衰老的增加,细胞周期活性的降低,免疫细胞浸润的增强,这可能是他们改善生存结局的原因。
结论
04
总之,本研究重新定义了IL6ST/STAT3信号通路在前列腺癌中的作用,揭示了其通过衰老和免疫细胞募集的肿瘤抑制作用。这对STAT3作为癌基因的传统观点提出了挑战,并对抑制该通路的前列腺癌治疗策略提出了质疑。研究人员提议将IL6ST激活作为一种新型治疗策略,为利用免疫系统参与对抗肿瘤的创新癌症疗法铺平道路。本研究结果将活性IL6ST信号作为开发更有效的PCa治疗的关键元素,突出了其改变PCa治疗的潜力。(转化医学网360zhyx.com)
【参考资料】
https://molecular-cancer-biomedcentral-com.libproxy1.nus.edu.sg/articles/10.1186/s12943-024-02114-8#Sec21
【关于投稿】
转化医学网(360zhyx.com)是转化医学核心门户,旨在推动基础研究、临床诊疗和产业的发展,核心内容涵盖组学、检验、免疫、肿瘤、心血管、糖尿病等。如您有最新的研究内容发表,欢迎联系我们进行免费报道(公众号菜单栏-在线客服联系),我们的理念:内容创造价值,转化铸就未来!
转化医学网(360zhyx.com)发布的文章旨在介绍前沿医学研究进展,不能作为治疗方案使用;如需获得健康指导,请至正规医院就诊。
临床1期
2024-10-31
点击上方蓝字 关注我们
编者按:近年来,去势抵抗性前列腺癌(CRPC)的治疗取得了显著进步;同时,前列腺特异性膜抗原(PSMA)作为前列腺癌分子成像和治疗靶点,也已经取得了突破性进展,如:PSMA-PET成像可显著提高前列腺癌定位精确程度,177Lu-PSMA-617为前列腺癌患者带来全新治疗策略等等。近期,Nature子刊发表了一篇综述,总结了当前PSMA表达、调控及其异质性的研究,并分析了临床应用前景。本刊特别整理,以期为精准治疗提供更多思路。
前列腺中的PSMA表达
前列腺是由上皮组织和纤维肌肉基质组成的外分泌腺(图1)。在微观层面上,PSMA主要在腔上皮的分泌细胞中表达,尤其是在AR阳性的腔上皮细胞中;而基质细胞和少量神经内分泌细胞几乎不表达PSMA。尽管PSMA不在正常血管的内皮细胞中表达,但在多种实体肿瘤的血管生成过程中可以上调,包括乳腺癌、肾癌和前列腺癌等。
图1 前列腺腔上皮中的PSMA表达
靶向PSMA的诊断和治疗方案
通过放射性标记,PSMA-PET/CT可将PSMA表达可视化。但应注意,PSMA假阳性可能出现于软组织病变、异常血管增生、创伤或胸腺瘤等。此外,良性前列腺病变中的PSMA,特别是良性前列腺增生和前列腺上皮内瘤变,需要进一步分析。而通过对PSMA-PET/CT成像进行仔细分析,可提高诊断精度。同时,目前也正在开发多种PSMA放射性配体疗法,如表1所示。
表1 基于GUL的PSMA放射性配体
明确PSMA阳性,改善肿瘤诊断与治疗
对PSMA阳性和同质性的界定,对于筛选合适患者进行PSMA靶向治疗至关重要。研究表明,超过95%的原发性前列腺癌具有中高水平的PSMA表达,但这种PSMA高表达情况仅存在于71%的CRPC患者,而神经内分泌型前列腺癌(NEPC)患者中的比例则下降至32%(图2)。
图2 前列腺癌发展过程中的PSMA表达抑制分析
目前尚无统一的免疫组织化学(IHC)评分系统,临床上主要依赖PSMA-PET成像确定PSMA阳性状态。PSMA-PET/CT图像基于miTNM分类系统中的miPSMA评分(图3),即按照与血液、肝脏和腮腺的摄取量对比进行分级,miPSMA评分为2和3的肿瘤被认为适合PSMA-RLT治疗。
图3 确定PSMA阳性对于选择合适患者至关重要
在PET成像领域,放射性示踪剂的摄取量使用标准摄取值(SUV)进行半定量评估,不同研究使用的SUV标准不同。此外,骨转移在前列腺癌中很常见,SUVmax比值大于2.2通常用于区分恶性和良性病灶。神经内分泌型前列腺癌(NEPC)通常PSMA表达较低,因此在成像中挑战较大,不同的前列腺癌组织学变异也可能影响成像特征。
PSMA影像筛选PSMA-RLT治疗人群
PSMA阴性病灶无法保留PSMA放射性配体,因此PSMA阴性或同时存在PSMA阳性和阴性病灶的患者通常被排除在PSMA-RLT试验之外。虽然基于PSMA-PET识别PSMA阴性病灶的概念较为简单,但实际操作较为复杂,miPSMA评分为0的病灶可能难以识别。为了增强检测,部分试验使用氟脱氧葡萄糖(FDG)PET作为辅助影像方法,因为其可进一步增强筛选精确程度。此外,也有试验数据表明,放射组学与转录组学结果相符,显示RNA-seq数据具有分析PSMA调控的潜力。
区分PSMA异质性与经典肿瘤异质性
最新数据显示,PSMA阳性患者且SUVmean高于10时,177Lu-PSMA-617治疗出现缓解的几率更高。SUVmean用于衡量PSMA异质性,包括细胞、肿瘤、患者个体、空间和时间维度差异(图4)。肿瘤异质性通常是指在原发或转移性肿瘤中存在不同的细胞群,这些细胞具有不同的遗传和表型特征。PSMA的异质性可以通过免疫染色和单细胞RNA测序显示,细胞和肿瘤层面均存在PSMA表达的范围差异。2023年一项研究对52例患者的339个CRPC样本的PSMA表达进行了分类,发现存在低/阴性、异质性和均匀高表达三种模式,部分NEPC亚群也存在PSMA高表达。PSMA在CRPC中表达的谱系内时间异质性也很明显,如雄激素剥夺疗法和AR抑制剂(如恩扎卢胺)可提高AR+肿瘤的PSMA表达水平,表明CRPC在不同时间PSMA异质性的细微差别。
图4 PSMA异质性的复杂性表明需要采用更细致的方案
PSMA异质性在PSMA诊疗中的表现
PSMA-PET/CT结合了核医学与CT影像,其空间分辨率极限通常在4~5 mm,这意味着限制了肿瘤内部PSMA阳性和阴性只有距离>4~5 mm才有可能进行明确区分。放射学结果称为“影像学层面的PSMA”,而免疫组织化学识别的PSMA称为“病理学层面的PSMA”,分辨率的差异可能导致二者异质性的产生。临床前研究显示,PSMA表达程度和PSMA+细胞比例,与肿瘤摄取与177Lu-/225Ac-PSMA-617相关的DNA损伤有关。因此,评估PSMA-PET放射配体摄取的均一性可能会改善纳入标准。
应承认,目前缺乏对“PSMA阴性”病灶的统一定义。为了提高前列腺癌转移的诊断准确性,PSMA-PET与相应的CT或MRI使用也至关重要,这会直接影响到纳入标准。未来的最佳患者选择可能会受到PSMA成像异质性及其强度的影响。结合其他生物标志物参数,如肿瘤特征、循环肿瘤细胞和循环肿瘤DNA,以及互补的PET成像数据和深度学习图像处理算法,可能有助于进一步改进。
PSMA低表达的分子特征
有研究评估了LuCaP系列PDX模型以及UW-TAN和SU2C-PCF患者队列,发现相比PSMA高表达患者,PSMA低表达患者具有显著的全局表达变化,患者的炎症反应、缺氧、上皮-间质转化以及代谢和糖酵解通路增加。
CRPC中PSMA抑制的出现凸显了寻找PSMA以外靶点的需求。目前已经开发了替代放射性配体以识别靶抗原或改进现有临床配体,包括18F-FDG、胆碱、GRPR、DHT放射性标记物和18F-fluciclovine,以及Zr-DFO-DLL3-scFv和Zr-DFO-MSTP2109A等。成纤维细胞活化蛋白(FAP)也因在CRPC基质中的过表达而成为潜在成像靶点。
PSMA相关的精准医疗未来方向
PSMA作为一种细胞表面蛋白,除了PSMA-RLT之外,还被用作其他治疗的靶点,如PSMA靶向T细胞激活剂、CAR-T细胞治疗和抗体偶联药物。为了优化这些治疗方案,需要深入研究PSMA表达水平和反应、耐药的生物标志物。结合PET成像和液体活检,可评估PSMA表达的动态变化,进行个性化治疗计划,并提前检测耐药。新兴技术如3D组织学、空间转录组学和人工智能,也有助于提高对PSMA在前列腺癌中的生物学理解,并推动更多疗法的开发。
结论
PSMA是前列腺癌的重要生物标志物和治疗靶点,广泛应用于癌症诊断和治疗。PSMA受多重基因组和表观遗传网络调控,尤其是雄激素受体(AR)的影响。然而,部分晚期前列腺癌患者因PSMA表达丧失,影响了PSMA-RLT的疗效。PSMA表达的异质性及其在转移部位以及耐药机制的复杂性,进一步增加了治疗挑战。应探索放射性同位素以外的PSMA靶向治疗途径,以提升前列腺癌治疗效果。
▌参考文献:
Bakht, Martin K., and Himisha Beltran. Biological determinants of PSMA expression, regulation and heterogeneity in prostate cancer. Nature Reviews Urology (2024): 1-20.
(来源:《肿瘤瞭望-泌尿时讯》编辑部)
声 明
凡署名原创的文章版权属《肿瘤瞭望》所有,欢迎分享、转载。本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
临床结果放射疗法
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
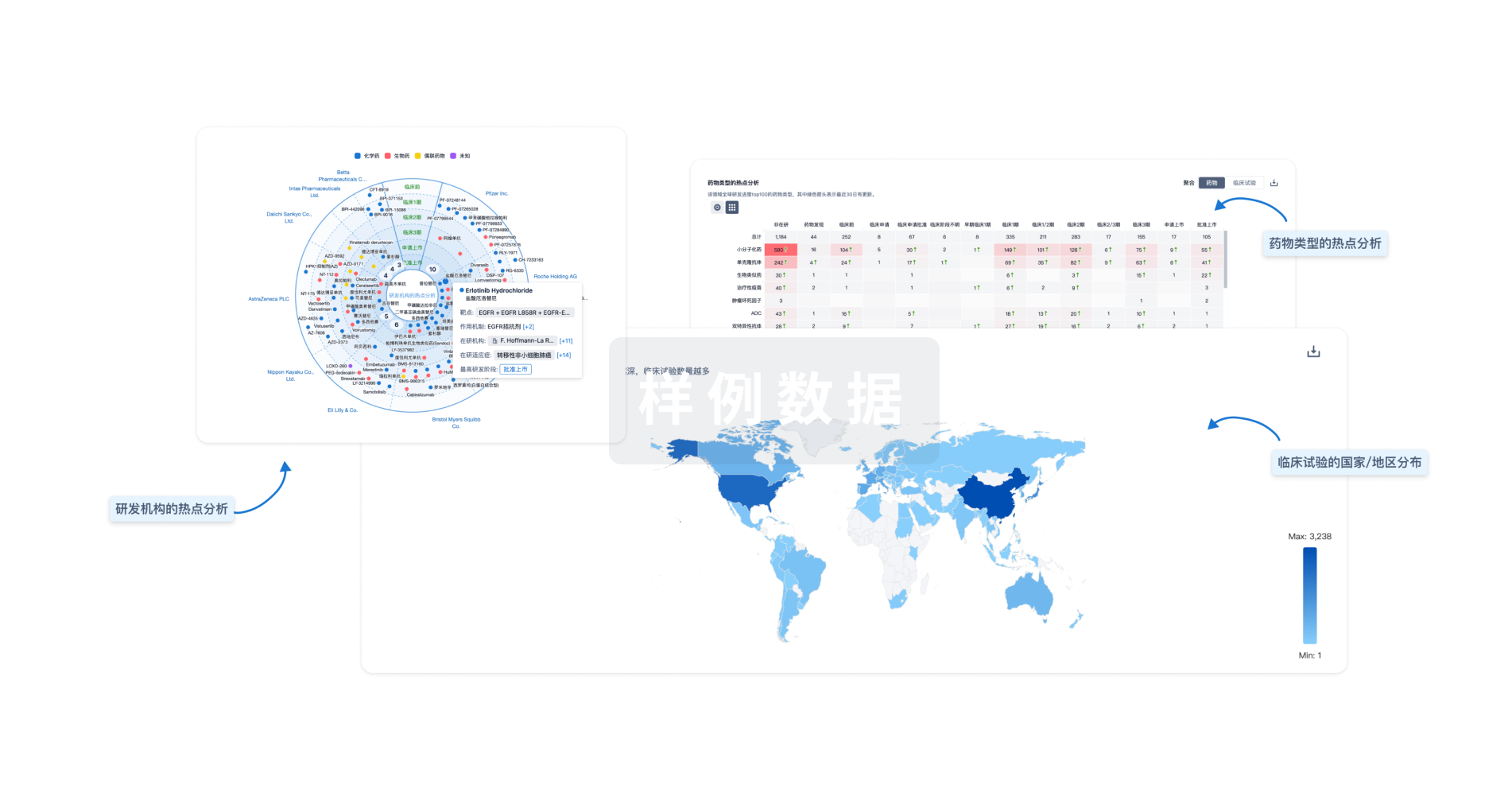
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


