预约演示
更新于:2025-05-07
Unresectable Solid Neoplasm
不可切除的实体瘤
更新于:2025-05-07
基本信息
别名 Unresectable Solid Neoplasm |
简介 A solid neoplasm that is not amenable to surgical resection. |
关联
74
项与 不可切除的实体瘤 相关的药物靶点 |
作用机制 PI3Kα抑制剂 |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-10-10 |
靶点 |
作用机制 CSF-1R拮抗剂 |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-08-14 |
靶点 |
作用机制 IL15R激动剂 [+1] |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-04-22 |
110
项与 不可切除的实体瘤 相关的临床试验NCT06911008
Phase I Trial of SCD I: A First in Human Dose Regimen-Finding Study to Evaluate the Safety, Tolerability, Pharmacokinetics, and Activity of MTI-301 in Patients With Advanced Malignancy
This phase I trial tests the safety, side effects, and best dose of MTI-301 in treating patients with solid cancers that have spread from where they first started (primary site) to other places in the body (metastatic) or that cannot be removed by surgery (unresectable) and that have not responded to previous treatment (refractory). MTI-301 is a drug that inhibits an enzyme called SCD1. SCD1 is an enzyme that promotes tumor growth and spread and is upregulated in some cancer types. MTI-301 may disrupt the activity of SCD1, which may lead to reduced tumor growth and/or spread.
开始日期2025-06-09 |
申办/合作机构  Mayo Clinic Mayo Clinic [+1] |
NCT06626256
A Phase 1 Safety and Efficacy Study of STIL101 for Injection in Locally Advanced, Unresectable, or Metastatic Pancreatic Ductal Adenocarcinoma, Colorectal Cancer, Renal Cell Carcinoma, Cervical Cancer, and Melanoma
This phase I trial tests the safety and side effects of STIL101 for injection and how well it works in treating patients with pancreatic cancer, colorectal cancer (CRC), renal cell cancer (RCC), cervical cancer (CC) and melanoma that has spread to nearby tissue or lymph nodes (locally advanced) or to other places in the body (metastatic) or that cannot be removed by surgery (unresectable). STIL101 for injection, an autologous (made from the patients own cells) cellular therapy, is made up of specialized white blood cells called lymphocytes or "T cells" collected from a piece of the patients tumor tissue. The T cells collected from the tumor are then grown in a laboratory to create STIL101 for injection. STIL101 for injection is then given to the patient where it may attack the tumor. Giving chemotherapy, such as cyclophosphamide and fludarabine, helps prepare the body to receive STIL101 for injection in a way that allows the T cells the best opportunity to attack the tumor. Aldesleukin is a form of interleukin-2, a cytokine made by leukocytes. Aldesleukin increases the activity and growth of white blood cells called T lymphocytes and B lymphocytes. Giving STIL101 for injection may be safe, tolerable and/or effective in treating patients with locally advanced, metastatic or unresectable pancreatic cancer, CRC, RCC, CC and melanoma.
开始日期2025-04-30 |
申办/合作机构 |
NCT06364410
Phase 1 Study of Trastuzumab Deruxtecan (DS-8201a) in Combination With Azenosertib (ZN-c3) in HER2-Expressing/Amplified Cyclin E-Amplified Gastric/Gastroesophageal Junction Cancer and Other Solid Tumors With HER2 Expression
This phase I trial tests the safety, side effects, and best dose of azenosertib in combination with trastuzumab deruxtecan in treating patients with HER2-positive and cyclin E amplified gastric or gastroesophageal junction cancer and other HER2-positive solid tumors that have spread to nearby tissue or lymph nodes (locally advanced), that have spread from where it first started (primary site) to other places in the body (metastatic), or that cannot be removed by surgery (unresectable). Azenosertib is in a class of medications called kinase inhibitors. It inhibits a protein called Wee1. Inhibition of the Wee1 protein can make tumor cells more vulnerable to chemotherapy drugs, leading to tumor cell death. Trastuzumab deruxtecan is in a class of medications called antibody-drug conjugates. It is composed of a monoclonal antibody, called trastuzumab, linked to a chemotherapy drug, called deruxtecan. Trastuzumab attaches to HER2 positive cancer cells in a targeted way and delivers deruxtecan to kill them. Giving azenosertib in combination with trastuzumab deruxtecan may be safe, tolerable, and/or more effective in treating patients with locally advanced, metastatic, or unresectable HER2-positive gastric, gastroesophageal junction, or other solid tumors, compared to just trastuzumab deruxtecan alone.
开始日期2025-02-03 |
申办/合作机构 |
100 项与 不可切除的实体瘤 相关的临床结果
登录后查看更多信息
100 项与 不可切除的实体瘤 相关的转化医学
登录后查看更多信息
0 项与 不可切除的实体瘤 相关的专利(医药)
登录后查看更多信息
555
项与 不可切除的实体瘤 相关的文献(医药)2025-06-01·Journal of Vascular Surgery Cases, Innovations and Techniques
Vascular segmental exclusion for recurrent vulvar squamous cell carcinoma invading the femoral vessels
Article
作者: Chaar, Cassius Iyad Ochoa ; Cardella, Jonathan ; Schwartz, Andrew W ; Azodi, Masoud
2025-03-01·Medical Dosimetry
Plan evaluation tool for spatially fractionated radiation therapy for unresectable large tumors via spatial biological effective dose modeling in combination therapy
Article
作者: Misa, Josh ; Knight, James ; Clair, William St ; Pokhrel, Damodar
2025-02-10·ACS Biomaterials Science & Engineering
Traditional Chinese Medicine-Based Nanoformulations for Enhanced Photothermal Therapy of Cancer
Review
作者: Liu, Jingjing ; Yu, Lin ; Qin, Xueying ; Liang, Bing
23
项与 不可切除的实体瘤 相关的新闻(医药)2025-04-28
– Complete response (CR) observed in 79% (26/33) of evaluable patients with low-grade upper tract urothelial cancer (UTUC) who completed the Induction Treatment Phase (ITP) of the ENLIGHTED Phase 3 trial evaluating Padeliporfin VTP in UTUC – – Padeliporfin VTP treatment continues to be safe and efficacious, establishing profile consistent with prior results alongside additional follow-up in Maintenance Treatment Phase (MTP) – – Additional podium presentation reinforces platform applicability across solid tumors and highlights robust, long-term durability of response out to 48 months post-treatment with Padeliporfin VTP in intermediate-risk prostate cancer – TEL AVIV, Israel, April 28, 2025 (GLOBE NEWSWIRE) -- ImPact Biotech, a clinical-stage biotechnology company focused on developing Padeliporfin vascular targeted photodynamic (VTP) therapy to treat a range of solid tumors, today announced updated preliminary results from ENLIGHTED, the Company’s ongoing Phase 3 study of Padeliporfin VTP treatment in patients with low-grade upper tract urothelial cancer (UTUC), as well as long-term follow up from the PCM-204 Phase 2b trial evaluating Padeliporfin VTP in men with intermediate risk of prostate cancer. These data were presented at the American Urological Association’s 2025 Annual Meeting (AUA) on April 27, 2025 in Las Vegas, Nevada. “Positive updates from the ENLIGHTED trial continue to reinforce Padeliporfin VTP’s potential to shift the treatment paradigm as a promising non-invasive option for patients with low-grade UTUC,” said Eyal Morag, M.D., Chief Medical Officer of ImPact Biotech. “We are highly encouraged by the robust complete response rate, which is in line with other minimally invasive interventions but without incurring risk of organ injury or loss. We also see potential for deepening of partial responses in a real-world setting, where retreatment may be possible beyond the number of inductions included in trial protocol. We look forward to sharing additional updates from the ENLIGHTED study, and anticipate reporting complete topline data within the year to support potential registration of Padeliporfin VTP in this indication.” Key updated preliminary results from the Phase 3 ENLIGHTED study of Padeliporfin VTP: As of November 4, 2024, the data cut-off for the poster presentation at AUA, 44 patients had begun treatment, of which 33 had completed ITP and were evaluable for efficacy. Clinical Profile: 26 of the 33 (79%) response-evaluable patients achieved a CR at the end of ITP.6 of the 33 (18%) response-evaluable patients achieved a partial response (PR) at the end of ITP. Safety and Tolerability Profile: Padeliporfin VTP was well-tolerated with a safety profile consistent with the previous data obtained from the Phase 1 study and previously announced preliminary Phase 3 results.Adverse events (AEs) observed were primarily Grade 1 or 2, most of which were related to the ureteroscopic procedure rather than VTP, and all resolved within two to seven days. Only one patient experienced a Grade 3 serious adverse event that was related to the VTP therapy, which resolved within two days, and there were no VTP related Grade 4 or 5 serious adverse events observed. ImPact continues to recruit for the ENLIGHTED study and expects to complete enrollment in mid-2025. Long-term follow-up from PCM-204 Phase 2b trial in intermediate-risk prostate cancer: In addition to updates from the ENLIGHTED study, the Company delivered an oral presentation on 48-month follow-up from the PCM-204 Phase 2b trial evaluating Padeliporfin VTP in men with intermediate risk prostate cancer. 46 of the 50 (92%) of patients included in the study were assessable at the 48-month follow-up interval. “We are further excited by the updates from longer-term evaluation in men with intermediate-risk prostate cancer, extending prior observations in low-risk prostate cancer for which Padeliporfin VTP has previously been approved,” Dr. Morag continued. “These data further underscore the potential of our technology’s applicability across solid tumors and, importantly, provide visibility into the durability of response to treatment with Padeliporfin VTP.” Efficacy Profile: 32 off the 46 (69%) of the evaluable men remained free from evidence of clinical disease progression at 48 months post-treatment. Functional Outcomes and Safety: Padeliporfin demonstrated minimal long-term toxicity including low impact on urinary and sexual function, consisted with the safety and tolerability profile established in the Phase 3 trial in low-risk disease. Functional outcomes at 48 months post-treatment included a non-significant mean decrease in IIEF-5 scores from baseline of -0.67 (standard deviation [SD] 4.4).IPSS demonstrated an average non-significant change of -0.34 (SD 5.1).All patients maintained pad-free urinary continence. Padeliporfin VTP (brand name Tookad) has previously been approved by the European Union, Israel, and Mexico as a treatment for low-risk prostate cancer, following demonstration of significant clinical benefit as a localized partial gland ablation (PGA) therapy when compared to active surveillance for low-risk prostate cancer. Podium and Poster Session Details: Poster Title: Efficacy and Safety of Padeliporfin Vascular Targeted Photodynamic Therapy (VTP) for Treatment of Low-grade Upper Tract Urothelial Cancer (LG UTUC): ENLIGHTED Phase 3 StudyPresenter: Vitaly Margulis, Professor of Urologic Oncology, University of Texas Southwestern Medical CenterPoster Number: IP-12-14Session Title: Bladder Cancer: Upper Tract Transitional Cell Carcinoma Podium Session Title: 48-Month Follow up of Results of the PCM-204 Phase 2b Trial of Partial-Gland Ablation for Men with Intermediate-Risk Prostate Cancer with Padeliporfin (WST11 or Tookad) Vascular-Targeted Photodynamic TherapyPresenter: Jonathan Fainberg, Urologic Surgeon, Memorial Sloan Kettering Cancer CenterPodium Session Number: PD19-06 About ENLIGHTEDThe Phase 3 ENLIGHTED study is a single arm, non-randomized, open-label, pivotal trial evaluating Padeliporfin VTP for the treatment of low-grade UTUC. Across 29 clinical sites globally, ImPact is targeting enrollment of up to 100 patients with new or recurrent low-grade, non-invasive UTUC of the kidney or ureter. The study consists of two parts – an Induction Treatment Phase (ITP) and Maintenance Treatment Phase (MTP) – across which Padeliporfin, a photosensitizing drug, is administered intravenously and VTP therapy is performed, via an outpatient endoscopy which applies a laser fiber illumination for 10 minutes in the proximity of the tumor, leading to local activation of Padeliporfin in the tumor. ITP consists of one-to-three treatments with VTP therapy at four-week intervals or until a complete response (CR) is achieved; MTP follows with standard-of-care treatment alongside VTP therapy administered every three months for up to 12 months. The study’s primary objective is to assess the response rate to Padeliporfin VTP treatment at the end of ITP, with secondary objectives evaluating safety, tolerability and duration of response. About ImPact BiotechImPact Biotech is an advanced clinical-stage oncology company focused on the development and commercialization of Padeliporfin Vascular Targeted Photodynamic (VTP) therapy, a minimally invasive drug-device combination for selective ablation of unresectable solid tumors. The novel VTP platform delivers non-thermal laser light via optical fibers to locally activate Padeliporfin in the tumor microenvironment. Padeliporfin VTP is currently being evaluated in a pivotal Phase 3 study in low-grade upper tract urothelial carcinoma (UTUC) with earlier stage studies ongoing or planned in high-grade UTUC, pancreatic ductal adenocarcinoma (PDAC) and non-small cell lung cancer (NSCLC). The Company has longstanding collaborations with the Weizmann Institute of Science and Memorial Sloan Kettering Cancer Center and operations in the EU, Israel and the US. For more on ImPact Biotech Ltd., visit: www.impactbiotech.com and the ENLIGHTED clinical trial website (for the US): https://www.enlighted-study.com. Contacts Global Head of Business DevelopmentGuy Schmidtguy.schmidt@impactbiotech.com Precision AQJosh Rappaportjosh.rappaport@precisionaq.com
临床结果临床3期临床2期
2024-12-04
-- Complete response (CR) observed in 85% (17/20) of evaluable patients with low-grade upper tract urothelial cancer (UTUC) who completed the Induction Treatment Phase -- -- Padeliporfin VTP treatment continues to be safe and efficacious, establishing profile consistent with prior results alongside additional follow-up in Maintenance Treatment Phase – TEL AVIV, Israel, Dec. 04, 2024 (GLOBE NEWSWIRE) -- ImPact Biotech, a clinical-stage biotechnology company focused on developing Padeliporfin vascular targeted photodynamic (VTP) therapy to treat a range of solid tumors, today announced updated interim results from ENLIGHTED, the Company’s ongoing Phase 3 study of Padeliporfin VTP treatment in patients with low-grade upper tract urothelial cancer (UTUC). These data will be presented at the 25th Annual Meeting of the Society of Urologic Oncology (SUO 2024) taking place December 4-6, 2024 in Dallas, Texas. “As data from the ENLIGHTED trial matures, we continue to be encouraged by compelling and sustained efficacy signals from treatment with Padeliporfin VTP,” said Eyal Morag, M.D., Chief Medical Officer of ImPact Biotech. “These results further underscore the potential for Padeliporfin VTP to transform the treatment paradigm in low-grade UTUC, offering efficacy in line with standard of care but without the associated risk of organ injury or loss. We look forward to sharing additional data from the ENLIGHTED trial and to progressing Padeliporfin VTP in other unresectable solid tumors in 2025.” As of July 22, 2024, the data cut-off for the poster presentation at SUO, 32 patients had begun treatment, of which 20 had completed ITP and were evaluable for efficacy.
Key updated preliminary results from the Phase 3 ENLIGHTED study of Padeliporfin VTP:
Clinical Profile:
17 of the 20 (85%) response-evaluable patients achieved a CR at the end of ITP. Safety and Tolerability Profile:
Padeliporfin VTP was well-tolerated with a safety profile consistent with the previous data obtained from the Phase 1 study and previously announced preliminary Phase 3 results. Adverse events (AEs) observed were primarily Grade 1 or 2, most of which were pain related, and all resolved within two to seven days. Only one patient experienced a Grade 3 serious adverse event that was related to the VTP therapy, which resolved within two days.There were no Grade 4 or 5 serious adverse events observed. ImPact continues to recruit for the ENLIGHTED study. As previously announced in September, the Company has exceeded 50% enrollment in the study and expects to complete enrollment by early 2025. Poster & Session Details:
Poster Title: Efficacy and Safety of Padeliporfin Vascular Targeted Photodynamic Therapy (VTP) for Treatment of Low-grade Upper Tract Urothelial Cancer (LG UTUC): ENLIGHTENED Phase 3 studyPresenter: Vitaly Margulis, M.D., Chair in Urology, UT Southwestern Medical CenterPoster Number: 244Session Title: SUO24 Networking and Abstract Discussion SessionSession Date & Time: December 6, 2024, 1:45 PM CST About ENLIGHTEDThe Phase 3 ENLIGHTED study is a single arm, non-randomized, open-label, pivotal trial evaluating Padeliporfin VTP for the treatment of low-grade UTUC. Across 29 clinical sites globally, ImPact is targeting enrollment of up to 100 patients with new or recurrent low-grade, non-invasive UTUC of the kidney or ureter. The study consists of two parts – an Induction Treatment Phase (ITP) and Maintenance Treatment Phase (MTP) – across which Padeliporfin, a photosensitizing drug, is administered intravenously and VTP therapy is performed, via an outpatient endoscopy which applies a laser fiber illumination for 10 minutes in the proximity of the tumor, leading to local activation of Padeliporfin in the tumor. ITP consists of one-to-three treatments with VTP therapy at four-week intervals or until a complete response (CR) is achieved; MTP follows with standard-of-care treatment alongside VTP therapy administered every three months for up to 12 months. The study’s primary objective is to assess the response rate to Padeliporfin VTP treatment at the end of ITP, with secondary objectives evaluating safety, tolerability and duration of response.
About ImPact Biotech ImPact Biotech is an advanced clinical-stage oncology company focused on the development and commercialization of Padeliporfin Vascular Targeted Photodynamic (VTP) therapy, a minimally invasive drug-device combination for selective ablation of unresectable solid tumors. The novel VTP platform delivers non-thermal laser light via optical fibers to locally activate Padeliporfin in the tumor microenvironment. Padeliporfin VTP is currently being evaluated in a pivotal Phase 3 study in low-grade upper tract urothelial carcinoma (UTUC) with earlier stage studies ongoing or planned in high-grade UTUC, pancreatic ductal adenocarcinoma (PDAC) and non-small cell lung cancer (NSCLC). The Company has longstanding collaborations with the Weizmann Institute of Science and Memorial Sloan Kettering Cancer Center and operations in the EU, Israel and the US. For more on ImPact Biotech Ltd., visit: www.impactbiotech.com and the ENLIGHTED clinical trial website (for the US): https://www.enlighted-study.com. Contacts Global Head of Business DevelopmentGuy Schmidtguy.schmidt@impactbiotech.com Precision AQJosh Rappaportjosh.rappaport@precisionaq.com
临床3期临床结果ASCO会议临床1期
2024-11-22
2024 年11月22日,和誉医药(港交所代码:02256)宣布,已完成“一项评估ABSK061和ABSK043联合或不联合化疗在FGFR2/3改变的转移性/不可切除的实体瘤患者中的安全性及有效性的开放性多中心II期临床研究(方案编号: ABSK061-201)”的首例胃癌患者给药。ABSK061是全球进度最快的靶向FGFR2和FGFR3的口服高选择性的强效抑制剂。ABSK043是一种靶向PD-L1的口服小分子抑制剂。两药在前期研究中均观察到了初步的抗肿瘤活性及良好的安全性,且联用产生药物相互作用的风险较小,支持在FGFR改变的晚期实体瘤患者中探索ABSK061联合ABSK043的有效性及安全性。
ABSK061-201是一项评估ABSK061和ABSK043联合或不联合化疗在FGFR2/3改变的转移性/不可切除的实体瘤患者中的安全性及有效性的开放性多中心II期临床研究。试验包括剂量递增和扩展期两个部分。剂量递增将评估ABSK061+ABSK043在FGFR2/3激活改变或过表达的转移性/不可切除的晚期实体瘤患者中的安全性、耐受性、初步疗效和PK特征,并推荐用于扩展期的给药剂量。
扩展期将在多个不同的实体瘤队列,入组包含特定FGFR2/3基因改变的肿瘤类型(包括HER2阴性胃/胃食管交界癌),评估ABSK061+ABSK043联合或不联合化疗的抗肿瘤疗效。
关于ABSK061
ABSK061是和誉医药独立自主研发并拥有全球知识产权的一款新一代口服、高活性、高选择性小分子FGFR2/3抑制剂,也是全球范围内第一款进入临床的FGFR2/3选择性抑制剂。首代泛FGFR抑制剂已在针对多种携带FGFR2/3变异的肿瘤中展现出临床疗效并在全球范围内逐步获批上市,但安全窗及药效均受限于FGFR1抑制相关副作用。通过降低对FGFR1的抑制以及保持对FGFR2/3的高活性,ABSK061作为第二代FGFR抑制剂有望在临床上取得更好的安全窗及疗效。除肿瘤以外,ABSK061还具备拓展用于治疗包括软骨发育不全在内的多种非肿瘤适应症的巨大潜力。
关于ABSK043
ABSK043为一款全新的具备优异活性及高度选择性的口服小分子PD-L1抑制剂。癌细胞可以利用PD-1及其配体PD-L1这些免疫检查点来逃避免疫监管和清除,抑制或限制T细胞应答。ABSK043可与PD-L1受体特异性结合并诱导其从细胞表面内吞,有效地抑制PD-1/PD-L1的相互作用,解除PD-L1介导的T细胞活化抑制作用。ABSK043在多个临床前模型中展现出与已获批PD-L1抗体相当的抗肿瘤功效。截止目前,全球已有多款PD-1/PD-L1抗体药物获批上市,但并无PD-1/PD-L1小分子药物获批。ABSK043目前正在澳大利亚和中国开展针对晚期实体肿瘤的I期临床试验。
First-Patient Dosed in Gastric Cancer in Phase II Clinical Study Evaluating ABSK043, an Oral PD-L1 Inhibitor, in Combination with ABSK061, an Oral FGFR2/3 Inhibitor, for Solid Tumors
22, November 2024, Shanghai – Abbisko Therapeutics Co., Ltd. (HKD:02256) today announced that the first gastric cancer patient has been dosed in “A Phase 2, Multicenter,Open-Label Clinical Study to Evaluate the Safety and Efficacy of ABSK061 and ABSK043 with or without Chemotherapy in Patients with Metastatic/Unresectable Solid Tumors with FGFR2/3 Alterations(Protocol No: ABSK061-201)”.
ABSK061 is the world's most clinically advanced orally bioavailable, potent and selective inhibitor of FGFR2 and FGFR3. ABSK043 is a leading orally bioavailable, potent and selective inhibitor of PD-L1. In previous studies, both drugs demonstrated robust anti-tumor activity, a favorable safety profile, and low-risk of drug interaction, supporting the exploration of efficacy and safety of ABSK061 in combination with ABSK043 in advanced solid tumors with FGFR alterations.
ABSK061-201 is an open-label, multicenter, phase II clinical study designed to evaluate the safety and efficacy of the combination of ABSK061 and ABSK043 with or without chemotherapy in patients with metastatic/unresectable solid tumors harboring FGFR2/3 alterations. The study consists of two parts, a dose escalation and expansion phase. The dose escalation portion will assess safety, tolerability, preliminary efficacy, and the PK profile of ABSK061 + ABSK043 in patients with metastatic/unresectable advanced solid tumors with altered FGFR2/3 activation or overexpression to identify the recommended dose for the expansion phase.
The expansion phase will enroll tumor types with specific FGFR2/3 gene alterations, including HER2 negative gastric/gastroesophageal junction carcinoma, in multiple distinct solid tumor cohorts to evaluate the anti-tumor efficacy of ABSK061+ABSK043 with or without chemotherapy.
About ABSK061
ABSK061 is a novel, orally bioavailable, highly potent and selective small molecule inhibitor of FGFR2 and FGFR3 independently discovered and wholly owned by Abbisko Therapeutics. It is the first FGFR2/3 inhibitor to enter clinical trials globally. First-generation pan-FGFR inhibitors demonstrated clinical efficacy in multiple tumors carrying FGFR2/3 variants and have steadily gained regulatory approval globally. However, the therapeutic window of pan-FGFRs and their clinical efficacy have been limited by side effects associated with FGFR1 inhibition. By reducing FGFR1 activity while maintaining potency against FGFR2 and FGFR3, ABSK061 is expected to achieve a wider therapeutic window with improved clinical efficacy as a new-generation of FGFR inhibitors. In addition, ABSK061 has shown great potential to expand its use to a variety of non-oncology indications, including achondroplasia.
About ABSK043
ABSK043 is a novel, orally administered small molecule PD-L1 inhibitor displaying exceptional activity and high selectivity wholly owned by Abbisko Therapeutics. Tumor cells can exploit immune checkpoints such as PD-1 and its ligand PD-L1 to evade immune detection and clearance, thereby suppressing or restricting T-cell responses. ABSK043 selectively binds to the PD-L1 receptor and induces its internalization from the cell surface, effectively inhibiting the PD-1/PD-L1 interaction and alleviating PD-L1-mediated suppression of T-cell activation. In preclinical models, ABSK043 has demonstrated anti-tumor efficacy comparable to approved PD-L1 antibodies. While several PD-1/PD-L1 monoclonal antibodies have been approved worldwide, there are currently no approved orally available PD-1/PD-L1 small molecule drugs. ABSK043 is currently being studied in an ongoing Phase I clinical trial for advanced solid tumors in Australia and China.
关于和誉
和誉医药(香港联交所代码:02256)是一家立足中国,着眼全球的创新药研发公司。公司的创始人和管理团队拥有多年顶尖跨国药企的研发和管理经验,并参与了多个临床及上市新药的研发。和誉医药专注于肿瘤新药研发,以小分子肿瘤精准治疗和小分子肿瘤免疫治疗药物为核心,着眼病患及医药市场的需求,秉承国际新药开发的理念和标准,致力于开发新颖及高潜力药物靶点的潜在first-in-class或best-in-class创新药物,用于改善中国及全球病人的生活质量。
自2016年成立以来,和誉医药已拥有由16种候选药物组成的产品管线,涵盖肿瘤精准治疗领域以及肿瘤免疫治疗领域。
更多信息,欢迎访问 www.abbisko.com。
临床1期临床2期
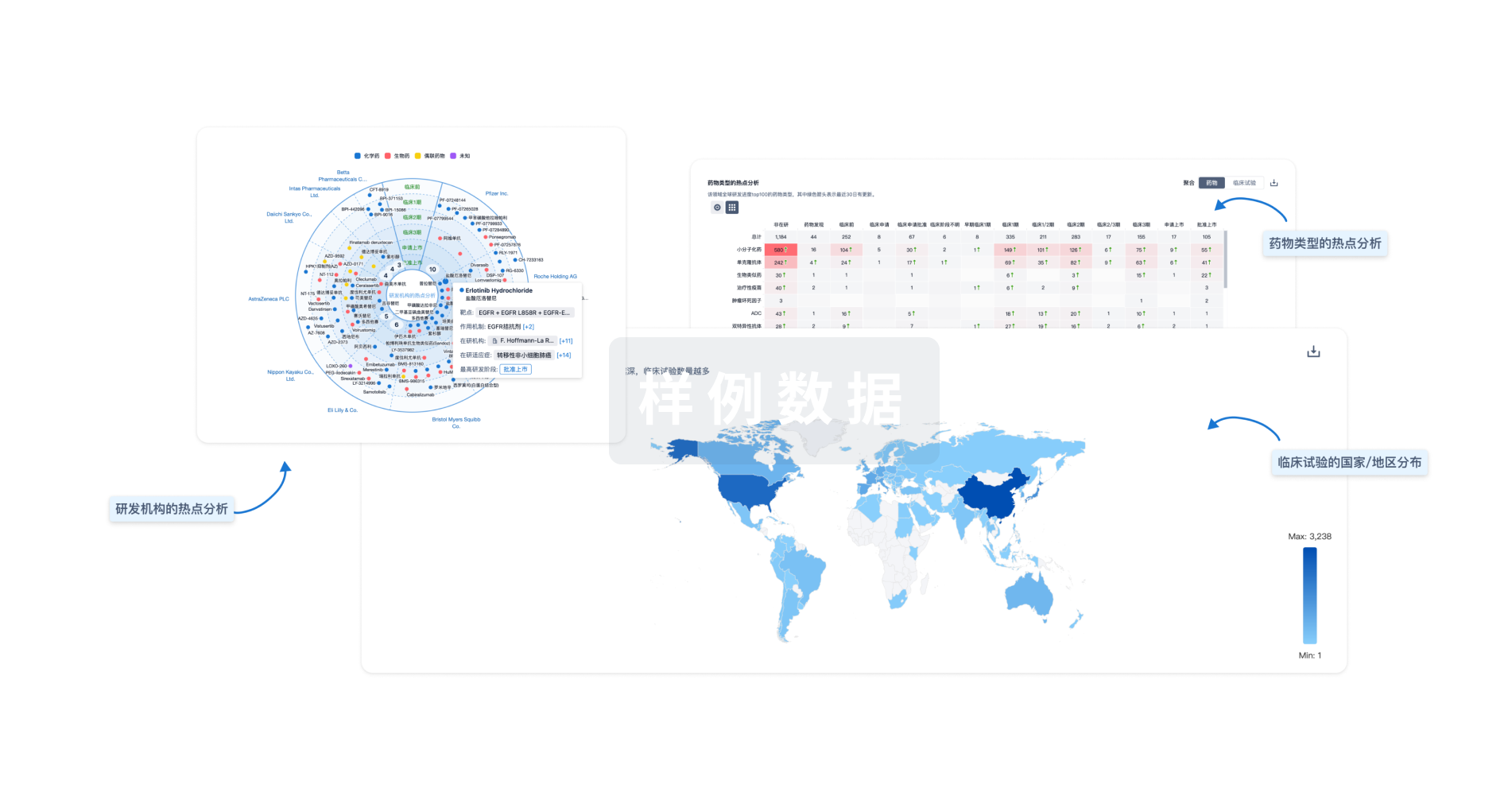
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用