预约演示
更新于:2025-05-07
Locally Advanced Bladder Carcinoma
局部晚期膀胱癌
更新于:2025-05-07
基本信息
别名 Locally Advanced Bladder Carcinoma |
简介 A bladder carcinoma that has spread from its original site of growth to nearby tissues or lymph nodes. |
关联
10
项与 局部晚期膀胱癌 相关的药物作用机制 微管蛋白抑制剂 [+1] |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2019-12-18 |
靶点 |
作用机制 PD-1抑制剂 |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期2014-07-04 |
29
项与 局部晚期膀胱癌 相关的临床试验NCT06434350
Enfortumab Vedotin with Radiation for Locally Advanced Bladder Cancer (CONSOLIDATE)
To learn if the combination of enfortumab vedotin plus radiation therapy could help to control the disease.
开始日期2024-10-10 |
NCT06414317
A Comprehensive Education and Navigational Support Program for Advanced Bladder Cancer
This clinical trial evaluates the impact of an education and navigation support tool (ENST) on patient and caregiver participation in care coordination for bladder cancer that has spread to nearby tissue or lymph nodes (locally advanced), to other places in the body (metastatic) or that cannot be removed by surgery (unresectable). Patients with advanced bladder cancer tend to be older, have multiple medical conditions and often have poor access to health care. An ENST may be an effective method to improve participation in treatment decision-making and care planning among patients with locally advanced, metastatic and unresectable bladder cancer and their caregivers.
开始日期2024-01-12 |
NCT05756569
Phase II Single-Arm Study of Enfortumab Vedotin (EV) Plus Pembrolizumab in the Treatment of Locally Advanced or Metastatic Bladder Cancer of Variant Histology
This phase II trial tests how well enfortumab vedotin (EV) and pembrolizumab works in treating patients with bladder cancer of variant histology (a group of less common types of bladder cancer) that have spread to nearby tissue or lymph nodes (locally advanced) or that has spread from where it first started (primary site) to other places in the body (metastatic). Enfortumab vedotin is a monoclonal antibody, enfortumab, linked to an anticancer drug called vedotin. Enfortumab attaches to a protein called nectin-4 on cancer cells in a targeted way and delivers vedotin to kill them. It is a type of antibody-drug conjugate. Immunotherapy with monoclonal antibodies, such as pembrolizumab, may help the body's immune system attack the cancer, and may interfere with the ability of tumor cells to grow and spread. Giving enfortumab vedotin and pembrolizumab may kill more tumor cells in patients with locally advanced or metastatic bladder cancer of variant histology.
开始日期2023-09-26 |
申办/合作机构  Emory University Emory University [+4] |
100 项与 局部晚期膀胱癌 相关的临床结果
登录后查看更多信息
100 项与 局部晚期膀胱癌 相关的转化医学
登录后查看更多信息
0 项与 局部晚期膀胱癌 相关的专利(医药)
登录后查看更多信息
516
项与 局部晚期膀胱癌 相关的文献(医药)2025-04-01·Cancer Medicine
Visceral Adipose Predicts Prognosis and Toxicities in Locally Advanced Bladder Cancer Patients Treated With Adjuvant Gemcitabine Plus Cisplatin Chemotherapy
Article
作者: Li, Zhen ; Li, Hailong ; Qin, Xu ; Gao, Zhimin ; Qi, Nienie ; Wang, Junqi ; Wang, Zewei ; Zhang, Lei
2025-03-01·Current Opinion in Urology
Is there a role for neoadjuvant therapies followed by radical cystectomy in oligometastatic bladder cancer?
Review
作者: Cadenar, Anna ; D'Andrea, David ; Mancon, Stefano ; Shariat, Shahrokh F
2025-03-01·International Journal of Radiation Oncology*Biology*Physics
Adjuvant Radiation Therapy for Locally Advanced Bladder Cancer: A Safe and Promising Emerging Treatment Option
作者: Baumann, Brian C ; Efstathiou, Jason A ; Baumann, Brian C. ; Efstathiou, Jason A.
4
项与 局部晚期膀胱癌 相关的新闻(医药)2025-04-08
当地时间2025年3月21日-3月24日,第40届欧洲泌尿外科协会(European Association of Urology,EAU)年会在西班牙马德里召开。EAU是全球泌尿外科领域极具影响力的专业组织,自 1972 年成立以来,始终坚守提升泌尿外科临床实践、科研与教育水平的使命。作为泌尿外科界的顶级盛会,为泌尿外科领域专业人士提供了交流最新研究成果、临床经验和技术创新的良好平台。本次年会上,中山大学肿瘤防治中心泌尿外科共有5项口头报告亮相,在国际舞台上充分展示了科室的科研实力与临床智慧,引发了参会专家们的广泛关注和热烈讨论。站在这个国际顶尖的学术舞台上,高质量的研究成果充分展现了中肿学者锐意进取的学术风貌。现在,就让我们一同探索这些新进展吧!01膀胱癌单病种团队标题:辅助性动脉内化疗可改善根治性膀胱切除术后III A-IIIB期膀胱尿路上皮癌患者的生存率:一项开放标签、前瞻性、随机临床试验英文标题:Adjuvant intraarterial chemotherapy improves the survival of patients with stage IIIA-IIIB bladder urothelial carcinoma after radical cystectomy: an open-label, prospective, randomized clinical trial研究概括:周朝晖博士代表膀胱癌单病种团队进行了此项研究的报告。这项多中心临床研究评估了局部晚期膀胱癌患者接受术后辅助动脉化疗的有效性和安全性。结果显示,术后辅助动脉化疗患者的无复发生存(RFS)显著优于对照组(5年RFS率:47.7% vs. 35.2%),并且3-4级不良反应发生率较低,患者耐受性良好。该研究为应用辅助动脉化疗改善局部晚期膀胱癌患者预后提供了证据支持,得到了在场专家的关注与交流。02前列腺癌单病种团队中文标题:帕米帕利治疗携带有害生殖系或体细胞BRCA1/2突变或同源重组缺陷的转移性去势抵抗性前列腺癌患者的Ⅱ期单臂、开放标签试验:疗效和安全性结果的更新中期分析英文标题:A Phase II Single-Arm, Open-Label Trial of Pamiparib in Metastatic Castration-Resistant Prostate Cancer (mCRPC) Patients with Deleterious Germline or Somatic BRCA1/2 Alterations or Homologous Recombination Deficiency (HRD): Updated Interim Analysis of Efficacy and Safety Result研究概括:前列腺癌团队在李永红教授的带领下积极参会,并在Expert Guided Poster Tour环节取得突出表现。赵迪威博士研究生代表团队此项研究进行报告。该研究旨在评估帕米帕利在携带BRCA1/2基因突变或HRD的mCRPC患者中的疗效和安全性。本次中期结果显示,帕米帕利在BRCA1/2突变患者中位无进展生存期(rPFS)达到7个月,客观缓解率(ORR)为33.3%,并且安全性良好。此次EAU大会的研究汇报突出了帕米帕利在携带BRCA1/2突变及HRD评分≥43分的mCRPC患者中的疗效,受到国际同行的高度关注。03肾癌单病种团队标题:卡度尼利单抗联合仑伐替尼用于早期肾细胞癌(需行部分肾切除但手术风险高)的新辅助治疗:一项前瞻性单臂Ⅱ期临床试验英文标题:Cadonilimab combined with lenvatinib for neoadjuvant therapy in early-stage renal cell carcinoma with indications for partial nephrectomy but high surgical risk: A prospective single-arm phase II clinical trial研究概括:彭毓璐博士代表肾癌癌单病种团队进行了此项研究的报告。结果显示,患者ORR达55.6%,10.5%的患者发生≥3级不良反应,无3级术后并发症发生。本研究中所有患者在术前均显示出肿瘤缩小,这提示联合治疗可显著降低肾透明细胞癌患者的肿瘤负荷,并且在缩瘤降期与安全性方面具有双重优势。该研究为高危早期肾透明细胞癌患者提供了全新的治疗选择,并有望使该类患者在“手术风险”和“治疗获益”中取得更好的平衡,获得了在场专家们的高度评价。标题:帕唑帕尼联合信迪利单抗用于部分肾切除术手术复杂性高的肾细胞癌患者的新辅助治疗:一项Ⅱ期试验英文标题:Efficacy and Safety of Neoadjuvant Pazopanib Plus Sintilimab in Renal Cell Carcinoma Patients with High Surgical Complexity of Partial Nephrectomy: A Phase II Trial研究概括:邹湘鹏博士研究生代表肾癌癌单病种团队进行了此项研究的报告。本研究评估了使用降低剂量的帕唑帕尼(200-600 mg/日)联合信迪利单抗新辅助治疗在适合保肾但手术难度较高的肾癌患者中的疗效和安全性。尽管本研究展现了初步的疗效,但≥3级不良反应发生率较高,主要表现为肝酶水平(AST、ALT)升高,分别为50%和60%。严重肝毒性限制了该联合方案的进一步应用,未来研究将进一步探索不同的剂量方案,或不同的免疫检查点抑制剂与TKI联合方案,以期在短期新辅助治疗过程中,为肾癌患者提供更安全且有效的治疗策略。报道引起了同场专家们的热烈讨论。04肾上腺肿瘤单病种团队标题:肾上腺转移灶的局部区域治疗:一项多中心回顾性队列比较研究英文标题:The New Sandwich Total Neoadjuvant Treatment (TNT) Strategy in Locally Advanced Rectal Cancer Patients: First Results of TESS Phase II Trial研究概括:介入科谢霖博士代表郭胜杰教授和范卫君教授团队进行了此项研究的报告。该研究是一项纳入496例肾上腺转移瘤患者的多中心真实世界研究,采用逆概率加权模型(IPTW)突破回顾性研究局限,首次系统对比了手术、消融、放疗三大局部疗法治疗肾上腺转移瘤的疗效及安全性。手术组3年总生存率53.2%,局部控制率超71%,尤其适合肿瘤≥5cm患者;消融组并发症率最低,是小肿瘤(<5cm)及不耐受手术者的理想选择;放疗组3年局部控制率达73.6%,且安全性突出,是重要的治疗手段。该研究为多学科诊疗治疗肾上腺转移瘤提供高质量证据,推动肾上腺转移瘤治疗个体化进程。本次报告获得了国际同行的充分肯定及热烈讨论,期待后续在前瞻性临床研究中的结果。中山大学肿瘤防治中心泌尿外科团队的积极参与和卓越表现,通过这次会议,不仅拓宽了专业视野,还结识了众多国内外同行,展示了团队其在泌尿肿瘤领域的专业实力,为今后的合作与交流奠定了基础。展望未来,中肿泌尿外科团队将把会议中的新理念、新方法运用到实际工作中,为患者的健康福祉贡献更多的力量,继续推动泌尿系肿瘤防治事业的进步,为人类健康事业做出更大贡献。(来源:中山大学肿瘤防治中心泌尿外科)声 明凡署名原创的文章版权属《肿瘤瞭望》所有,欢迎分享、转载。本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
临床2期临床结果临床3期临床失败
2024-05-09
The trial’s other primary endpoint, overall survival, was not formally tested because the Keytruda-chemo combo failed to reach superiority on the DFS metric, Merck said.
While Merck & Co.’s Keytruda already boasts a pair of approvals to treat certain forms of endometrial cancer, a recent effort to prove the PD-1 inhibitor’s worth as a post-surgery add-on therapy in newly diagnosed patients has fallen short.
Adjuvant treatment with Keytruda and chemotherapy—with or without radiotherapy—failed to hit the mark for disease-free survival (DFS) in newly diagnosed, high-risk endometrial cancer patients who received surgery with curative intent, according to an interim analysis of Merck’s late-stage KEYNOTE-B21 study. DFS refers to the length of time after a primary treatment ends that a patient survives without any signs or symptoms of their cancer.
The trial’s other primary endpoint, overall survival, was not formally tested because the Keytruda-chemo combo failed to reach statistical significance on the DFS metric, Merck said in a Thursday release.
Merck says it’s continuing a full evaluation of the data and is working with investigators to share the results at a later date.
Endometrial cancer is the sixth most common cancer in women and the most common type of cancer in the uterus, according to Merck. In the U.S. alone, the company estimates roughly 67,880 patients will be diagnosed with uterine body cancer this year. Merck also estimates there will be 13,250 patient deaths from the disease in 2024.
“While these results were not what we had hoped, we are focused on continuing to build on the established role of Keytruda in advanced endometrial carcinoma through our approved indications,” Gursel Aktan, M.D., Ph.D., vice president of global clinical development at Merck Research Laboratories, said in a statement.
Merck will continue to test Keytruda-based combinations—plus other treatment approaches like antibody-drug conjugates (ADC)—in endometrial and other types of gynecologic cancers, Aktan said.
Keytruda is already approved in patients with endometrial carcinoma that is microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR). The PD-1 inhibitor picked up that nod in 2022 following a 2017 approval that allowed the drug to cover previously treated MSI-H/dMMR tumors in patients without alternative treatment options.
Keytruda also boasts a second indication alongside Eisai-partnered Lenvima in previously treated endometrial cancer that’s not dMMR.
Over the past year, Merck’s Keytruda has been sparring with GSK’s PD-1 rival Jemperli over endometrial cancer dominance in the clinic.
Last February, just two months after Jemperli snagged a historic win for immunotherapy in first-line endometrial cancer, Keytruda plus standard chemotherapy beat chemotherapy alone at staving off tumor progression or death in advanced or recurrent disease.
The following month at the Society of Gynecologic Oncology 2023 annual meeting, both GSK and Merck provided a closer look at their meds’ late-stage performance in first-line endometrial cancer, with Keytruda appearing to edge out Jemperli in MMR proficient (pMMR) patients—a key subgroup that Merck says comprises roughly two-thirds of all endometrial cancer cases.
GSK ultimately beat Merck to the finish line for a PD-1 nod in newly diagnosed disease, with the company’s Jemperli in July snagging FDA clearance as an add-on to chemotherapy for patients with primary advanced or recurrent endometrial cancer but only for tumors that are mismatch repair deficient (dMMR) or microsatellite instability-high (MSI-H).
Meanwhile, Merck and Eisai’s Keytruda-Lenvima combo in December missed the mark in a phase 3 study as a potential first-line treatment in certain patients with advanced or recurrent endometrial carcinoma. The oncology cocktail failed to demonstrate an improvement in overall survival and progression-free survival over a regimen of platinum-based chemotherapy, missing both of its primary endpoints.
While Keytruda climbed to the top of pharma's sales charts in 2023, the drug has experienced a series of clinical ups and downs in 2024.
The PD-1 inhibitor started out the year by delivering a partial win in a phase 3 study pitting the drug against high-risk localized muscle-invasive bladder cancer and locally advanced bladder cancer. Around the same time, Keytruda bolstered its case as a postsurgical treatment for resectable kidney cancer with data showing it helped slash the risk of death by 38% versus placebo post-kidney removal in patients with clear cell renal carcinoma—the most common form of kidney cancer.
The drug also posted a win in cervical cancer in March. But that same month, Keytruda in combination with Lynparza failed to improve patients’ life expectancy or delay progression or death when subbed in for the chemotherapy pemetrexed during maintenance treatment of newly diagnosed metastatic nonsquamous non-small cell lunger cancer.

临床3期上市批准临床结果ASCO会议
2024-01-26
Merck's Keytruda already boasts approvals in certain patients with non-muscle invasive bladder cancer and in combination with Pfizer and Astellas' Padcev in first-line advanced bladder cancer.
The combination of Merck's Keytruda and Pfizer and Astellas' Padcev recently made waves in bladder cancer—and the broader oncology world—by delivering a massive life-extension benefit against chemotherapy. Now, Merck can claim another positive readout for Keytruda in bladder cancer, although this one is short of a home run.
This time, Keytruda showed its benefit when used after surgery in high-risk patients with localized muscle-invasive bladder cancer and locally advanced bladder cancer. The PD-1 inhibitor pared down the risk of disease recurrence or death by 31% compared with observation in the phase 3 AMBASSADOR trial, which was organized by the National Cancer Institute.
Keytruda more than doubled the median time that patients were alive and disease-free to 29 months, compared with the control arm’s 14 months. The data are being presented at the 2024 American Society of Clinical Oncology Genitourinary Cancers Symposium.
If the AMBASSADOR results eventually lead to an FDA approval, Keytruda would be able to cover an even broader spectrum of bladder cancer patients. In 2020, the drug won a go-ahead to treat certain patients with non-muscle invasive bladder cancer. More recently, the FDA endorsed the drug—alongside Padcev—as a first-line treatment for advanced bladder cancer.
But unlike the Padcev combo approval, which was backed by a 53% reduction in the risk of death versus chemotherapy, Keytruda can’t yet claim an overall survival win in AMBASSADOR.
At an interim analysis, Keytruda showed no benefit toward prolonging patients’ lives. The risk of death marginally favored Keytruda by 2%, but patients who took the PD-1 drug were alive for a median 50.9 months, which was worse than the 55.8 months for their counterparts in the control group.
Overall survival data remained immature, Marjorie Green, M.D., head of oncology global clinical development at Merck Research Laboratories, told Fierce Pharma. The current overall survival readout counts 257 deaths, and the final analysis will be triggered at about 320 deaths, she said. Disease-free survival and overall survival are dual primary endpoints of the AMBASSADOR trial.
Some factors may have put Keytruda at a disadvantage, Green noted. A higher percentage of patients in the control group dropped out mid-study compared with the Keytruda arm. The rates were 27.2% and 17.4%, respectively.
Green declined to comment on Merck’s regulatory plan because it’s confidential. Still, she argued that the disease-free survival data represent an important clinical endpoint, and that Keytruda holds a potential to be a new adjuvant therapy option for patients with earlier stages of resectable muscle-invasive bladder cancer.
Keytruda’s disease-free survival benefit looks consistent across patient subgroups. In patients who had or hadn’t received presurgical neoadjuvant therapy, Keytruda’s improvements were nearly identical. In patients whose tumors expressed PD-L1, Keytruda reduced the risk of recurrence or death by 23%, and in PD-L1-negative disease, the improvement was 39%.
Despite radical surgery, up to half of patients with muscle-invasive bladder cancer still experience high rates of cancer recurrence, Andrea Apolo, M.D., a principal investigator at the Center for Cancer Research of the National Cancer Institute, said in a statement. The current data show the promise of using Keytruda after surgery for certain high-risk patients with persistent muscle-invasive or locally advanced urothelial carcinoma, she said.
Keytruda has enjoyed much fanfare in bladder cancer following the high-profile success of its combination with the antibody-drug conjugate Padcev in previously untreated advanced patients. The Keynote-905 trial, also coded EV303, is now testing the same Keytruda-Padcev pairing—or Keytruda alone—for use both before and after surgery in patients who are ineligible for cisplatin or decline cisplatin with muscle-invasive bladder cancer. Separately, Keynote-866 is adding perioperative Keytruda to neoadjuvant chemo in cisplatin-eligible disease.
Editor's Note: The story now includes the most up to date patient withdrawal rates in the AMBASSADOR trial.

临床结果ASCO会议上市批准临床3期
分析
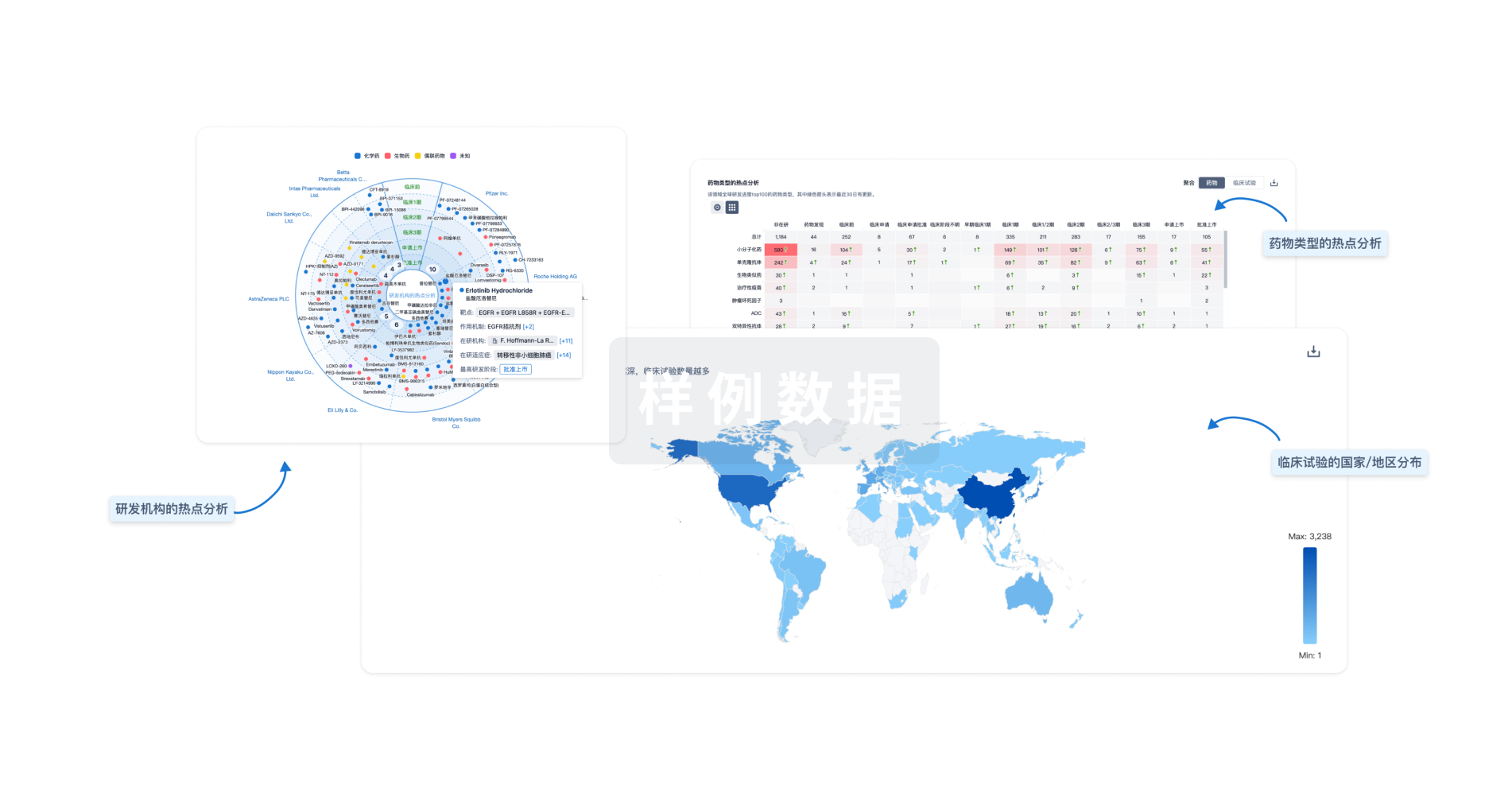
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用