预约演示
更新于:2025-05-07
Rhinitis, Allergic, Seasonal
季节性过敏性鼻炎
更新于:2025-05-07
基本信息
别名 ALLERGY SEASONAL、ALLERGY TO POLLEN、Allergic Rhinitides, Seasonal + [87] |
简介 Allergic rhinitis that occurs at the same time every year. It is characterized by acute CONJUNCTIVITIS with lacrimation and ITCHING, and regarded as an allergic condition triggered by specific ALLERGENS. |
关联
177
项与 季节性过敏性鼻炎 相关的药物靶点 |
作用机制 IL-4Rα抑制剂 |
在研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2024-09-10 |
靶点- |
作用机制 免疫刺激剂 |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2023-05-06 |
靶点- |
作用机制 免疫调节剂 |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2023-05-06 |
915
项与 季节性过敏性鼻炎 相关的临床试验NCT06817889
An Open-Label Study to Assess the Safety and Efficacy of Remdesivir for Treatment of Symptomatic Laboratory-Confirmed Respiratory Syncytial Virus Infection of the Upper Respiratory Tract in Patients Receiving Cellular or Bispecific Antibody Therapies
This phase II trial tests how well remdesivir works for treatment of respiratory syncytial virus (RSV) infection of the upper respiratory tract in patients receiving cellular or bispecific antibody therapy. Cellular or bispecific antibody therapies cause suppression of the immune system, making infections more frequent and reducing the body's ability to fight the infections. RSV infections are one of the most common respiratory infections in immunocompromised individuals and can cause significant pneumonia and even death. Remdesivir is in a class of medications called antivirals. It works by stopping viruses from spreading in the body.
开始日期2025-08-01 |
申办/合作机构 |
NCT06907680
A Randomized Placebo-controlled Crossover Trial Assessing the Efficacy and Safety of M-Gard Particulate EW in the Treatment of Seasonal Allergic Rhinitis
The goal of this clinical trial is to assess the efficacy and safety of M-Gard supplementation for alleviating the symptoms of allergic rhinitis.
开始日期2025-05-01 |
申办/合作机构 |
NCT06876506
Identification and Quantitation of Human B Regulatory Cells Via Flow Cytometry and Their Potential Role as a Treatment Efficacy Biomarker in Allergen-specific Immunotherapy
The goal of this laboratory and observational study is to develop a test to quantify B-regulatory cells in blood. This will be used to detect changes in B-regulatory cell populations in pollen and insect venom allergic patients who are receiving routine allergen immunotherapy treatment. The primary question this study aim to answer is;
1). Are changes in blood B-regulatory cells associated with successful allergen immunotherapy treatment, and therefore do these changes suggest patients have developed a suitable level of allergen tolerance and reduction in their allergic symptoms upon re-exposure to the causal allergen.
Patients will also be asked to complete quality of life questionnaire periodically throughout the study to determine if there are associations between variation in B-regulatory cell populations in blood and allergic symptoms experienced.
1). Are changes in blood B-regulatory cells associated with successful allergen immunotherapy treatment, and therefore do these changes suggest patients have developed a suitable level of allergen tolerance and reduction in their allergic symptoms upon re-exposure to the causal allergen.
Patients will also be asked to complete quality of life questionnaire periodically throughout the study to determine if there are associations between variation in B-regulatory cell populations in blood and allergic symptoms experienced.
开始日期2025-05-01 |
申办/合作机构 |
100 项与 季节性过敏性鼻炎 相关的临床结果
登录后查看更多信息
100 项与 季节性过敏性鼻炎 相关的转化医学
登录后查看更多信息
0 项与 季节性过敏性鼻炎 相关的专利(医药)
登录后查看更多信息
9,003
项与 季节性过敏性鼻炎 相关的文献(医药)2025-07-01·Environmental Research
Associations between agricultural use of pyrethroid insecticides and asthma: AGRICAN cohort results
Article
作者: Baldi, Isabelle ; Lebailly, Pierre ; Douwes, Jeroen ; de Graaf, Lucie ; Tual, Séverine ; Bureau, Mathilde
2025-05-01·Journal of Allergy and Clinical Immunology: Global
Alleviating effect of intranasal zinc on symptoms of allergic rhinitis
Article
作者: Kato, Masashi ; Fujieda, Shigeharu ; Xu, Huadong ; Gao, Yanjun ; Tazaki, Akira ; Sumiya, Shogo ; Nishadhi, Delgama A S M ; Kagawa, Takumi ; Sakashita, Masafumi ; Tong, Keming ; Harusato, Akihito ; Iwasaki, Shinichi ; Iwasaki, Naruhito ; Ohgami, Nobutaka ; Ogi, Kazuhiro
2025-05-01·Lin chuang er bi yan hou tou jing wai ke za zhi = Journal of clinical otorhinolaryngology head and neck surgery
[Clinical characteristics of allergic rhinitis induced by pollen in northern China].
Article
作者: Ming, Wenhua ; Wang, Xiaoyan ; Wang, Xueyan ; Chen, Lijia ; He, Sinan ; Wang, Hongtian
360
项与 季节性过敏性鼻炎 相关的新闻(医药)2025-05-02
NIH findings may lead to insights on pregnancy complications, adult health
BETHESDA, Md., May 2, 2025 /PRNewswire-HISPANIC PR WIRE/ --
What: The genes of male and female placentas have marked differences in how they are expressed, according to a study by researchers at the National Institutes of Health (NIH) and other institutions. These differences involve the presence or absence of tags on DNA known as methyl groups, which switch genes on or off without changing their structure. Understanding these DNA methylation patterns may inform future research on the higher risk for pregnancy complications involving male fetuses, such as stillbirth and prematurity, as well as later life health conditions that occur in adults who were born after a complicated pregnancy.
Researchers analyzed male and female placental samples from a larger study for differences in their methylation patterns, and found differences in gene activity between male and female placentas that may play a role in birthweight and adult diseases.
The study identified 2,497 previously unreported DNA sites that had different methylation patterns for males and females. Of these and more than 2,500 sites that had also been identified by previous studies, 66.9% of large increases in methylation occurred in DNA from male placentas and 33.1% from female placentas. Increases in methylation in male placentas was linked with greater neonatal size whereas those in females was linked with greater placental size.
Some increases in methylation found in male placentas were located near the CCDC6 gene. Lower activation of CCDC6 has been linked with preterm birth in previous studies.
Higher methylation near the FNDC5 gene was associated with lower expression of the gene in male placentas but not in female placentas. FNDC5 is involved with the manufacture of irisin, which protects the placenta from damage by reactive oxygen molecules and insulin resistance (cells' difficulty in using insulin to lower blood sugar.) Lower irisin levels have been associated with the pregnancy-related high blood pressure disorder, known as preeclampsia.
Variations in the genes ATP5MG and FAM83A, expressed in female placentas, have been associated with asthma, hay fever, eczema (dry, itchy, inflamed skin) and higher risk for breast cancer later in life.
Genetic factors influence the health differences between males and females, from before birth to later in life. Male fetuses grow faster than female fetuses and their pregnancies are more likely to be complicated by such conditions as preeclampsia (a hypertensive disorder of pregnancy), failure to grow at an adequate rate, and preterm birth. They also are more likely to die in the year after birth. Dysfunction of the placenta underlies many pregnancy complications and is thought to set the stage for male and female health differences that occur later in life. Variations in methylation patterns are thought to underlie many of these differences.
The study was conducted by Fasil Tekola-Ayele, Ph.D., of the NIH's Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and colleagues at other institutions. It appears in Nature Communications.
Who: Fasil Tekola-Ayele, Ph.D., is available for comment on this study.
Reference
Tekola-Ayele F, et al. Sex-differentiated placental methylation and gene expression regulation has implications for neonatal traits and adult diseases. Nature Communications. DOI: 10.1038/s41467-025-58128-3 (2025)
SOURCE Eunice Kennedy Shriver National Institute of Child Health and Human Development; National Institutes of Health (NIH)
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果
2025-04-23
ALK (ALKB.DC / OMX: ALK B) today announced that its European regulatory filing for ITULAZAX® (tree pollen sublingual allergy immunotherapy tablet) for treatment of young children and adolescents aged five to 17 has been approved by the health authorities in 17 EU countries via a type II variation procedure. First market introductions are expected to follow in the coming months ahead of the 2025/2026 initiation season for new patients starting treatment on pollen allergy tablets.
Executive Vice President of R&D, Henriette Mersebach (MD), says: “We are very pleased with the European health authorities' approval which allows us to provide this important treatment option to children and adolescents whose lives are impaired by uncontrolled tree pollen-induced respiratory allergy. Today’s approval marks another significant milestone in our continuous efforts to make our respiratory tablets available to all age groups in all relevant markets".
ALK’s regulatory filing was based on data from the TT-06 clinical trial. TT-06 was a randomised, placebo-controlled Phase 3 trial involving 952 children and adolescents aged five to 17 with a clinical history of moderate to severe allergic rhinitis and/or conjunctivitis induced by pollen from birch trees and other trees in the birch homologous group. The trial confirmed that the treatment was well tolerated and had a favourable safety profile. The peer-reviewed results were published in 2024 in the European Journal of Allergy and Clinical Immunology.
The tree tablet, branded ITULAZAX® in Europe and ITULATEK® in Canada, has, until now, been approved by 22 countries for adult patients aged 18 to 65. Corresponding paediatric regulatory reviews are currently ongoing in Canada, Switzerland, and the UK. These reviews are expected to complete in 2025.
The approval of ITULAZAX® for paediatric use marks the completion of ALK's decade-long development efforts, ensuring that five of the most common respiratory allergies (grass pollen, house dust mite, ragweed pollen, Japanese cedar pollen, and now tree pollen) are all covered by allergy immunotherapy tablets approved for children, adolescents, and adults in relevant markets.
The approval is not expected to affect ALK’s financial outlook for 2025.
ALK-Abelló A/S
For further information please contact:
Investor Relations: Per Plotnikof, tel. +45 4574 7527, mobile +45 2261 2525
Media: Maiken Riise Andersen, tel. +45 5054 1434
About ALKALK is a global specialty pharmaceutical company focused on allergy and allergic asthma. ALK manufactures and markets allergy immunotherapy (‘AIT’) treatments and other products and services for people with allergy and allergy doctors. Headquartered in Hørsholm, Denmark, ALK employs around 2,800 people worldwide and is listed on Nasdaq Copenhagen. Find more information at www.alk.net.
Attachment
Company release_08_25UK_230425_Itulazax_approval_children
临床3期免疫疗法上市批准临床结果
2025-04-16
·米内网
彩内容近日,成都市第七人民医院公告称,经审核,将引进9款新药(均为独家品种)以满足临床科室诊疗需求,“中化生”领域均有涉及。其中,不乏艾瑞昔布片等2023年在中国公立医疗机构终端销售额超9亿元的明星药,以及注射用磷丙泊酚二钠等2024上半年销售额增速达三位数的潜力品种。9款拟进院的新药均为独家品种(含独家剂型,下同),包括5款化学药、3款中成药和1款生物药;按治疗大类统计,神经系统药物、消化系统及代谢药在数量上占优,各有2个产品在列;从剂型上看,片剂和注射剂为主力军,分别占3个和2个席位。拟进院新药名单来源:成都市第七人民医院,米内网整理注射用磷丙泊酚二钠为全球唯一水溶性丙泊酚前体药物,用于成人全身麻醉的诱导,对高脂血症患者具有优势,是人福医药在2021年获批的1类新药。在中国城市公立医院、县级公立医院、城市社区中心及乡镇卫生院(简称中国公立医疗机构)终端,该产品2023-2024上半年的销售额增长率分别达68.22%和398.91%,市场潜力在持续释放。近年来中国公立医疗机构终端注射用磷丙泊酚二钠销售趋势(单位:万元)来源:米内网中国公立医疗机构药品终端竞争格局艾瑞昔布片为恒瑞医药首款独家1类创新药,用于缓解骨关节炎的疼痛症状。米内网数据显示,该新药最早于2011年获批上市,于2017年进入医保目录后迅速放量,2023年在中国公立医疗机构终端销售规模超过9亿元,2024上半年收获约4.7亿元,是抗炎和抗风湿口服化学药TOP3产品。2024H1中国公立医疗机构终端抗炎和抗风湿口服化学药产品TOP10注:增长率低于10%用*表示来源:米内网中国公立医疗机构药品终端竞争格局益气通窍丸为扬子江药业的独家1.1类中成药,具有益气固表、散风通窍的功效,用于治疗季节性过敏性鼻炎中医辨证属肺脾气虚证。在鼻炎中成药方面,扬子江药业还有散风通窍滴丸已获批上市,用于急性单纯性鼻炎外感风寒、郁肺化热证等,其2023年在中国公立医疗机构终端销售额超过2亿元,同比增长23.88%。扬子江药业已获批上市的鼻炎中成药来源:米内网中国申报进度(MED)数据库此外,拟新增进院的独家品种还包括:科伦药业的注射用芦康沙妥珠单抗(乳腺癌、非小细胞肺癌等)、海思科的考格列汀片(2型糖尿病)和苯磺酸克利加巴林胶囊(糖尿病周围神经痛、带状疱疹后神经痛)、卓和药业的九味止咳口服液(急性气管-支气管炎)等,涵盖抗肿瘤和免疫调节剂、消化系统及代谢药、神经系统药物、呼吸系统疾病用药等治疗大类,满足不同患者的临床用药需求。来源:米内网数据库、成都市第七人民医院注:米内网《中国公立医疗机构药品终端竞争格局》,统计范围是:中国城市公立医院、县级公立医院、城市社区中心以及乡镇卫生院,不含民营医院、私人诊所、村卫生室;上述销售额以产品在终端的平均零售价计算。数据统计截至4月16日,如有疏漏,欢迎指正!免责声明:本文仅作医药信息传播分享,并不构成投资或决策建议。本文为原创稿件,转载文章或引用数据请注明来源和作者,否则将追究侵权责任。投稿及报料请发邮件到872470254@qq.com稿件要求详询米内微信首页菜单栏商务及内容合作可联系QQ:412539092【分享、点赞、在看】点一点不失联哦
上市批准免疫疗法
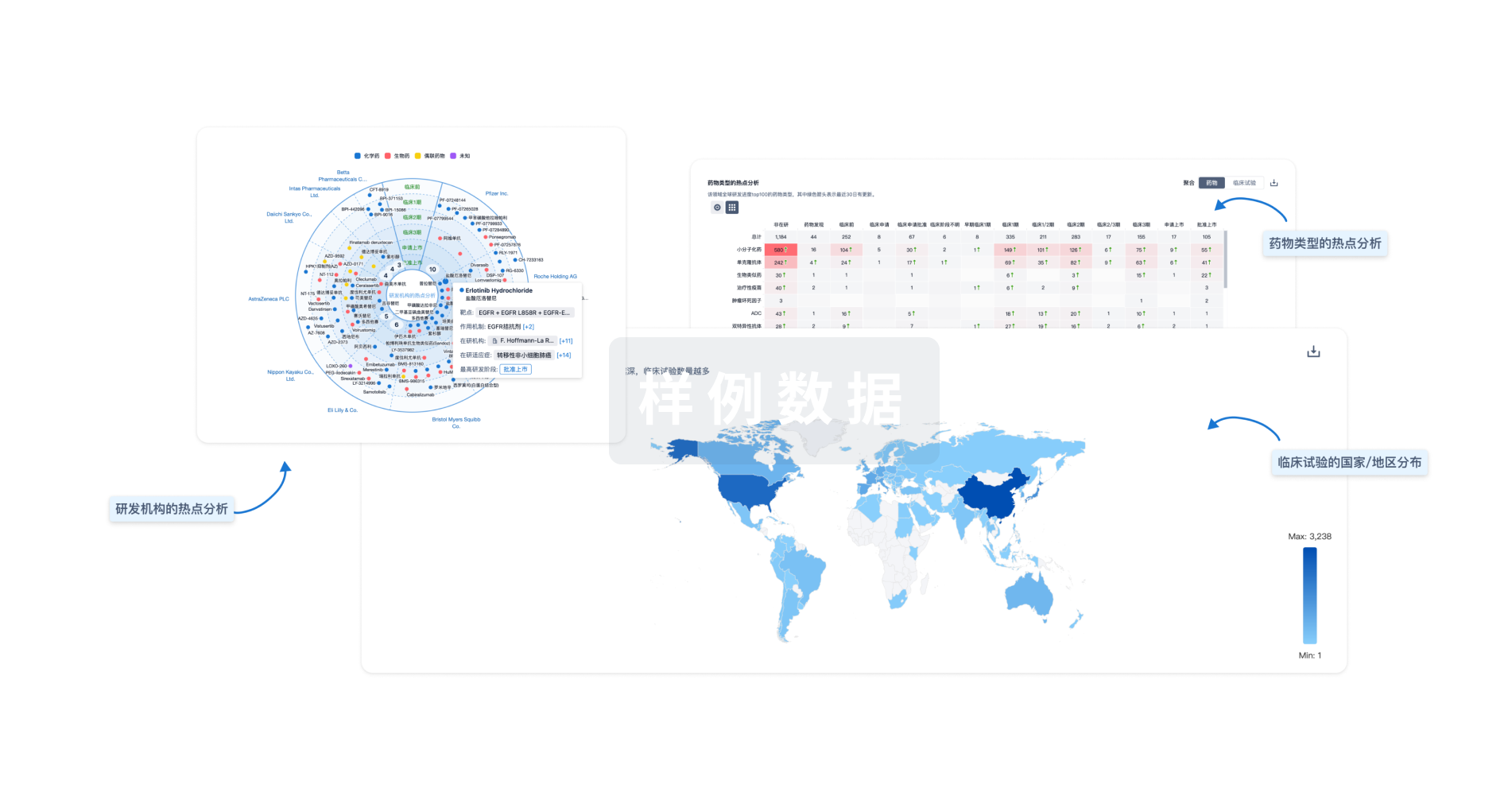
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用