预约演示
更新于:2025-05-07
VEGF-A x PGF
更新于:2025-05-07
关联
32
项与 VEGF-A x PGF 相关的药物作用机制 PGF抑制剂 [+1] |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-08-23 |
作用机制 PGF抑制剂 [+1] |
在研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-08-09 |
作用机制 PGF抑制剂 [+1] |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-06-28 |
47
项与 VEGF-A x PGF 相关的临床试验NCT06470373
A Phase 3 Clinical Trial to Compare Efficacy, Safety, Tolerability and Immunogenicity of RBS-001 to Eylea® in Subjects With Neovascular Age-Related Macular Degeneration
This clinical study is designed to demonstrate the equivalence of the two Investigational Products by comparing the efficacy, safety, tolerability and immunogenicity of RBS-001 and Eylea® in subjects with Neovascular age-related macular degeneration.
开始日期2025-07-01 |
申办/合作机构 |
NCT06864988
A Phase 3, Randomized, Double-Masked, Active-Controlled Trial of a Single Intravitreal Injection of 4D-150 in Adults With Macular Neovascularization Secondary to Age-Related Macular Degeneration
A Phase 3, Randomized, Double-Masked, Active-Controlled Trial in Adults with Macular Neovascularization Secondary to Age-Related Macular Degeneration
开始日期2025-03-03 |
100 项与 VEGF-A x PGF 相关的临床结果
登录后查看更多信息
100 项与 VEGF-A x PGF 相关的转化医学
登录后查看更多信息
0 项与 VEGF-A x PGF 相关的专利(医药)
登录后查看更多信息
480
项与 VEGF-A x PGF 相关的文献(医药)2025-06-01·Cytokine
Aqueous humor mediator levels as biomarkers of anti-VEGF response in age-related macular degeneration
Article
作者: Pace-Loscos, Tanguy ; Pagès, Gilles ; Baillif, Stéphanie ; Nahon-Esteve, Sacha ; Dufies, Maeva
2025-04-01·Journal of Cellular and Molecular Medicine
Unveiling the Angiogenic Potential and Functional Decline of Valve Interstitial Cells During Calcific Aortic Valve Stenosis Progression
Article
作者: Gendron, Nicolas ; Rancic, Jeanne ; Rossi, Elisa ; Cholley, Bernard ; Smadja, David M. ; Rosa, Mickael ; Philippe, Aurélien ; Bièche, Ivan ; Gaussem, Pascale ; Blandinières, Adeline ; Poitier, Bastien ; Susen, Sophie ; Idelcadi, Salim ; Dupont, Annabelle ; Vacher, Sophie
2025-02-01·Placenta
Sex-specific associations between feto-placental growth and maternal physical activity volume and sitting time: Findings from the Queensland Family Cohort study
Article
作者: Kubler, Jade M ; Steane, Sarah E ; Holland, Olivia J ; Rae, Kym M ; Kumar, Sailesh ; Borg, Danielle J ; Beetham, Kassia S ; Clifton, Vicki L
73
项与 VEGF-A x PGF 相关的新闻(医药)2025-04-13
·小药说药
-01-引言新血管的形成,是一个由各种促血管生成和抗血管生成分子调节的复杂而动态的过程,在肿瘤生长、侵袭和转移中起着至关重要的作用。随着分子生物学和细胞生物学的发展,参与肿瘤血管生成的各种生物分子,如生长因子、趋化因子和粘附因子已逐渐被阐明。基于这些分子的靶向治疗研究推动抗肿瘤血管生成治疗成为一种非常有前景的策略。最广泛使用的抗血管生成剂包括靶向血管内皮生长因子(VEGF)的单克隆抗体和酪氨酸激酶抑制剂(TKIs)。然而,由于不良反应、获得性耐药、肿瘤复发以及缺乏有效的生物标志物等缺陷,这种治疗模式的临床益处仍然有限,这促使人们进一步研究肿瘤血管生成的机制,开发多种新型药物和联合治疗,以提高疗效。-02-一、肿瘤血管生成的病理生理学血液循环是细胞代谢的基础,在正常组织中,紧密的周细胞覆盖和血管内皮细胞连接确保了正常的血液循环,形成了成熟的血管结构。然而,在肿瘤组织中,来自肿瘤组织的更多机械应力导致肿瘤血管的厚度不均和结构变形,它们以不规则的回旋方式表现出密集的出芽,这往往会阻碍血液流动。机械应力还会破坏淋巴管道,阻止多余间质液的淋巴引流。此外,脆弱且高渗透性的肿瘤血管,其内皮细胞和周细胞排列不规则,导致血液渗漏和灌注不连贯。这种空间异常结构表现为低血流量,减少了氧气和营养的供应,在肿瘤微环境中引起随后的酸性环境、缺氧以及高间质高压。所有这些因素都会导致肿瘤血管的混乱功能和异常结构,进一步加重酸性和缺氧的肿瘤微环境,从而促进肿瘤血管生成、侵袭和转移。肿瘤血管生成有多种模式。其中,血管出芽生成是生理和病理血管生成中最典型的过程,即在现有血管中形成新的血管分支,并通过尖端细胞的迁移和干细胞的增殖最终渗透到肿瘤组织中;套叠式血管生成涉及双腔的形成,双腔分裂成两条血管,渗透到肿瘤组织中;血管发生是指骨髓来源或血管壁固有的内皮祖细胞,这些细胞分化为内皮细胞形成新血管。除了上述三种模型外,肿瘤还可以通过血管选择、血管模拟、癌症干细胞分化模式来实现血管生成。血管选择指肿瘤细胞在预先存在的血管周围迁移或渗透到周围组织空间,最终包裹血管并引导它们进入肿瘤组织,为肿瘤细胞提供营养;血管模拟是肿瘤细胞延伸形成模拟血管腔,然后插入预先存在的血管,输送营养到肿瘤组织中的过程;最后,癌症肝细胞可以通过上皮-内皮转化转分化为内皮样细胞。-03- 二、肿瘤血管生成的关键分子和信号通路促进或抑制血管生成的各种生物分子构成了复杂而动态的血管生成系统,包括生长因子(如血管内皮生长因子、成纤维细胞生长因子、转化生长因子、肝细胞生长因子)、粘附因子(整合素、钙粘蛋白)、蛋白酶(如基质金属蛋白酶)、细胞外基质蛋白(纤连蛋白、胶原),转录因子(缺氧诱导因子、核因子)、血管生成素、血管抑素、内皮抑素和白细胞介素等。所有这些都通过跨膜受体激活基因表达并诱导内皮细胞增殖、存活和血管生成。VEGF/VEGFRVEGF-A是血管生成最重要的调节因子,在肿瘤生长、增殖、侵袭、转移、血管生成和耐药性中发挥着不可替代的作用。生理和病理血管生成中最关键的信号通路是VEGF-A/VEGFR-2,它刺激内皮细胞(EC)的有丝分裂、趋化和形态发生,并诱导实体瘤的增殖、迁移、侵袭和血管生成。PDGF/PDGFRs血小板衍生生长因子(PDGF)作为成纤维细胞、平滑肌细胞和神经胶质细胞等间充质细胞的主要有丝分裂原,PDGF通过旁分泌或自分泌参与细胞生长和分化、伤口愈合、血管生成、募集和周细胞和平滑肌细胞的分化。PDGF-BB是PDGF家族中研究最多的因子之一,过度表达的PDGF信号不仅增强组织纤维化,而且在肿瘤进展和抗VEGF治疗中激发血管生成和耐药性。EGF/EGFRs表皮生长因子(EGF)通过EGFR广泛参与细胞生长、增殖、分化、迁移、粘附、凋亡和肿瘤血管生成。作为启动分子,EGF通过激活下游信号通路(MAPK、PI3K/AKT/PKB、STAT和PLCγ/PKC)参与内皮细胞增殖和分化。此外,它促进有丝分裂,并通过Ang-2配体上调各种血管生成因子的合成、表达和分泌,如VEGF,间接促进肿瘤血管生成。FGF/FGFR作为促进伤口愈合的关键因素,成纤维细胞生长因子(FGF)家族是内皮细胞的有效有丝分裂原和驱动因子之一,也是最早发现的与血管生成相关的生长因子。主要由血管内皮细胞、干细胞和受损心肌细胞分泌。FGF家族中最具影响力的促血管生成因子是FGF-2(bFGF),它通过旁分泌调节心脏非肌细胞的功能分化,并刺激血管生成相关过程,如内皮细胞的迁移和侵袭以及纤溶酶原激活剂的产生。bFGF在乳腺癌(BC)、肺癌、膀胱癌和白血病中通常过度表达,与癌症转移和患者预后不良有关。HGF/c-MetHGF/c-Met是伤口愈合、组织再生和胚胎发生的关键信号通路。异常的HGF/c-Met信号,如c-Met基因的扩增或突变、转录失调以及HGF的异常分泌,促进癌组织的扩散、侵袭和血管生成。IGF/IGFR胰岛素样生长因子(IGF)是一种调节人类生长、发育和能量代谢的生长因子。高表达的IGF1和IGF2诱导VEGF合成并上调HIF-1α和VEGF的表达以促进血管生成。研究表明,IGF过表达会促进糖尿病视网膜病变(DR)、动脉粥样硬化和癌症的进展。TGF-βTGF-β是一种多效性的细胞因子,与身体稳态、组织修复、炎症和免疫反应有关,还参与细胞生长、分化、增殖、自噬、凋亡和肿瘤血管生成。在肿瘤中,TGF-β诱导内皮细胞迁移,促使血管出芽;其次,其通过EMT促进肿瘤的浸润和侵袭;此外,TGF-β诱导结缔组织生长因子(CTGF)、VEGF和bFGF的表达,它们对肿瘤血管生成至关重要。HIF-1缺氧诱导因子-1(HIF-1)调节细胞对缺氧的适应、能量代谢、红细胞生成和组织灌注平衡,并参与细胞存活、增殖,迁移、粘附、细胞凋亡、红细胞生成和葡萄糖代谢。在肿瘤进展中,HIF-1α可以上调所有VEGF亚型、PlGF、FGF、PDGF和Ang-1的相关基因的表达,以促进肿瘤血管生成或诱导耐药性。整合素整合素是细胞外基质中的主要粘附因子,通过调节细胞之间以及这些细胞与周围基质的信号转导,参与人体中的各种细胞过程。αvβ6是整合素中第一个发现具有血管生成作用的粘附因子,广泛表达于重塑和病理组织中活化的血管内皮细胞上。αvβ3是bFGF和TNF-α信号通路启动的血管生成中不可或缺的因子,而αvβ5是TGF-α和VEGF介导的血管生成所必需的。蛋白水解酶基质金属蛋白酶(MMPs)是一类由结缔组织和基质细胞分泌的锌和钙依赖性内肽酶家族。在各种血管生成中,MMPs是破坏ECM和重塑基底膜的主要介质。参与肿瘤血管生成的主要亚型是MMP-2、MMP-9和MMP-14。MMP-9是细胞外基质降解的中心蛋白酶,其增加VEGF的生物利用度并募集周细胞以维持肿瘤微环境中的稳态,触发内皮细胞的形态发生和出芽以刺激肿瘤血管生成。NF-κB核因子κB(NF-κB)是人体中的一种重要转录因子,参与细胞存活、氧化损伤、炎症、免疫反应和血管生成。作为一种间接介质,NF-κB通过调节血管生成因子的表达水平来调节各种癌症(如CRC、BC和黑色素瘤)的进展。血管生成素血管生成素维持静止的内皮细胞稳态和血管形态,并参与新血管的形成、胚胎发育和肿瘤血管生成。血管生成素由四个配体组成,Ang-1、Ang-2、Ang-3和Ang-4。Ang-1和Ang-2是参与血管稳态的主要因素。在肿瘤中,Ang-1和Ang-2的过表达促进血管生成和肿瘤生长。Notch通路Notch受体是一种特殊的非RTK蛋白,参与许多细胞过程,如形态发生、增殖、迁移、分化、凋亡、粘附、EMT和血管生成。在Notch家族中,Dll-4和Jag-1是肿瘤血管生成中最具代表性的配体。Ephrin/EphREphrin/EphR是一个独特的激酶家族,通过典型的双向信号转导调节相邻细胞之间的相互作用。在人体中,Ephrin/EphR信号通路在细胞形态发生、动静脉形成、神经系统发育、组织形成、组织稳态和各种血管生成过程中发挥着至关重要的作用。其中,最关键的通路是EphrinB2/EphB4,它能有效地促进发芽,肿瘤血管生成中的血管成熟和血运重建。-04-三、抗肿瘤血管生成药物的研究进展抗血管生成治疗是通过抗血管生成药物抑制肿瘤生长和转移,限制肿瘤组织的血液供应来实现的。尽管分子和机制研究表明,许多调节因子参与了肿瘤血管生成,但血管生成抑制剂的研究仍然集中在VEGF/VEGFR信号通路上。其中,单克隆抗体和小分子酪氨酸激酶抑制剂是抗血管生成治疗的主流药物。单克隆抗体最具代表性的抗肿瘤血管生成抗体是贝伐单抗(Avastin)。贝伐单抗是第一种获批的血管生成抑制剂,通过中和所有VEGF亚型来抑制肿瘤血管生成,从而阻断VEGF通路的转导。在CRC患者的III期临床试验中, PFS从中位数6.2个月增加到10.6个月,OS从34.8%增加到44.8%,中位反应持续时间增加了3.3个月。因此,贝伐单抗于2004年被FDA批准用于CRC患者。除了第一个适应症外,贝伐单抗已被批准用于多种其他癌症的单药治疗、手术辅助治疗或与化疗联合治疗,并且测试抗血管生成治疗的更多潜力。Ramucirumab(Cyramza)是一种靶向VEGFR-2的抗体,在三期REGARD临床试验中,Ramucirumab显著改善了不可切除胃和胃食管交界腺癌患者的中位OS(5.2个月vs 3.8个月)和PFS(2.1个月vs 1.3个月)。2014年,FDA批准ramucirmab用于先前治疗的晚期胃或胃食管交界处(GEJ)腺癌。Olaratumab(Lartruvo)是一种靶向PDGFRα的单克隆抗体,是FDA批准的治疗软组织肉瘤的一线药物。寡核苷酸衍生物Pegaptanib(Macugen)是一种VEGF-A靶向RNA适配体,于2004年12月被批准用于血管源性年龄相关性黄斑变性,通过玻璃体内注射,在AMD患者中具有良好的耐受性和治疗效果。重组融合蛋白Aflibercept(Eylea)是一种靶向VEGF的重组诱饵蛋白,它细胞外VEGFR结构域和人IgG1的Fc段融合而成。Aflibercept通过特异性阻断VEGF-A从而抑制内皮细胞的分裂和增殖,降低血管通透性,并用于AMD、DR和DME等非肿瘤性血管生成疾病。此外,它也被FDA批准用于治疗对含奥沙利铂耐药性或进展的转移性CRC患者。mTOR抑制剂Everolimus(RAD001)是mTOR的口服抑制剂,通过间接阻断mTOR抑制肿瘤细胞的增殖并诱导细胞凋亡和自噬。mTOR是一种丝氨酸/苏氨酸(Ser/Thr)激酶,通过与PI3K/AKT信号通路协同作用,在肿瘤细胞增殖和血管生成中发挥关键作用。在一项针对RCC患者的II期临床试验中,Everolimus取得了很好的结果,中位PFS为11.2个月,中位OS为22.1个Temsirolimus是另一种mTOR抑制剂,已被FDA批准用于晚期RCC。它还被欧盟批准用于复发或难治性套细胞淋巴瘤/非霍奇金淋巴瘤。小分子TKIssorafenib是一种多重靶向的血管生成抑制剂,通过阻断Raf和激酶受体(包括VEGFR、PDGFR、c-Kit和RET)的自磷酸化,抑制肿瘤的增殖、侵袭、转移和血管生成。2005年12月,FDA批准sorafenib用于晚期RCC患者。sorafenib作为首个抗血管生成小分子酪氨酸激酶抑制剂,显著促进了随后抗血管生成大分子药物的开发和临床研究。此外,其它的小分子血管生成抑制剂还包括Sunitinib、Pazopanib、Vandetanib、Regorafenib、Cabozantinib、Lenvatinib和Axitinib等。-05-四、抗血管生成治疗的局限性和挑战血管生成抑制剂用于癌症治疗,通过影响肿瘤中新血管的形成,为广泛的实体瘤治疗开辟了新的领域。然而,由于肿瘤血管生成机制复杂,研究有限,抗血管生成治疗仍存在一些不足,包括肿瘤复发、耐药性、缺乏生物标志物、短效疗效和一些严重不良事件。安全性和有效性最初认为,与其他化疗药物相比,抗血管生成疗法可能没有毒性。然而,事实证明这是一个误判。在许多不同的临床治疗中出现了常见的严重不良事件,如高血压、蛋白尿、淋巴细胞减少症、血小板减少症、白细胞减少症、中性粒细胞减少症和一些由不同药物引起的身体异常,这可能会影响患者的耐受性,甚至导致治疗终止。此外,血管生成抑制剂通过阻断血液供应在短期内控制肿瘤的生长和扩散,但长期结果可能是缺氧诱导的肿瘤局部侵袭和远处转移的风险增加,以及停止治疗后血运重建和肿瘤复发的可能性。耐药性耐药性是一个主要的挑战,它一直限制着靶向抗血管生成治疗的临床结果。可能的耐药机制包括:(a)肿瘤组织中代偿性促血管生成信号通路的上调;(b)肿瘤募集骨髓来源的内皮祖细胞、周细胞祖细胞、肿瘤相关巨噬细胞和未成熟单核细胞,其可以维持血管的形成;(c) 血管周细胞的募集,其可以覆盖未成熟的肿瘤血管,以防止抗血管生成药物的破坏;(d)非常规血管生成过程。此外,耐药性还涉及肿瘤组织和TME的高度异质性、内皮异质性、肿瘤细胞自噬、癌症干细胞分化、基质细胞浸润、肿瘤类型、肿瘤或靶点的基因突变以及患者的用药史等因素,都会影响患者对抗肿瘤治疗的反应和耐受性。缺乏有效的生物标志物生物标志物的应用是一种强大的辅助手段,对疾病识别、早期诊断和预防以及药物治疗监测至关重要。然而,尽管做出了相当大的努力,但很少有对血管生成有反应的生物标志物被批准用于临床应用。事实上,由于肿瘤血管生成的复杂性、肿瘤的异质性和可变性、反应或毒性的不可预测性以及临床前和临床试验的局限性等众多因素,生物标志物的开发将是一个巨大的挑战。-06-结语血管生成是肿瘤增殖、侵袭和转移的关键条件之一,以血管优化为标准的抗血管生成治疗已逐渐成为一种流行的抗肿瘤策略。但一些不可忽视的问题仍有待解决,如治疗效果不足、耐药性等。这些限制激励着研究人员开发新的血管生成抑制剂,探索更多靶点的药物以及可靠的生物标志物。相信随着对肿瘤血管生成、肿瘤微环境和耐药性的深入了解,这些问题可能在不久的将来得到解决。作为一种新兴的策略,抗血管生成治疗将为癌症患者和抗肿瘤治疗带来更多的临床益处。参考资料:1.Angiogenic signaling pathways and anti-angiogenic therapy for cancer. Signal Transduct Target Ther.2023 May 11;8(1):198公众号内回复“ADC”或扫描下方图片中的二维码免费下载《抗体偶联药物:从基础到临床》的PDF格式电子书!公众号已建立“小药说药专业交流群”微信行业交流群以及读者交流群,扫描下方小编二维码加入,入行业群请主动告知姓名、工作单位和职务。
2025-03-25
·抗体圈
在最近进行的两项关键临床试验中,Opthea的Sozinibercept和Unity的UBX1325均未能在疗效上击败或匹配再生元(Regeneron)的Eylea(阿柏西普)。这一结果对这两家公司来说无疑是巨大的挑战,尤其是在市场竞争日益激烈的眼科疾病治疗领域。
临床数据对比
1. Opthea的Sozinibercept:
Opthea的Sozinibercept是一种新型的VEGF受体融合蛋白,旨在通过靶向VEGF-A和PlGF来治疗湿性年龄相关性黄斑变性(wAMD)和其他视网膜疾病。具体数据显示,Sozinibercept在最佳矫正视力(BCVA)和中央视网膜厚度(CST)这两个关键指标上均未能显著优于Eylea。
• COAST III期研究招募了近1000名患者,这些患者接受了为期4周或8周的Sozinibercept治疗。一年后,在视力图表上测量的平均年龄变化分别为13.5和12.8个字母,而单独使用Eylea上的人则为13.7个字母。这相当于p值分别为0.86和0.42,这意味着与单独使用Eylea相比,联合治疗并没有显著改善视力。
2. Unity的UBX1325
UBX1325是一种靶向Bcl-xL的小分子抑制剂,用于治疗糖尿病性黄斑水肿(DME)。在II期临床试验中,UBX1325也未能在疗效上超越Eylea。
• 从基线到24周,ubx1325治疗的患者BCVA平均变化为+5.2 ETDRS字母,与阿非利西普组相比,差异为+0.4 ETDRS字母
• 从基线到36周,ubx1325治疗的患者BCVA平均变化为+5.5 ETDRS字母,与阿布利西普组相比,差异为+0.2 ETDRS字母
• 除了第20周和第24周的平均值外,UBX1325在36周的所有时间点都不逊于afliberept
• 使用UBX1325的患者在第16周和第20周时中心亚野厚度(CST)增加,这导致CST显著增加的患者补充抗vegf治疗
尽管UBX1325在一些次要终点上显示出一定的潜力,但在主要疗效指标上仍未达到预期目标。当天Unity股价下跌28.77%!
再生元公司的阿柏西普(Eylea)业务去年营收达 59 亿美元。该药物获批用于包括湿性年龄相关性黄斑变性和糖尿病性黄斑水肿在内的一系列病症。去年,阿柏西普的首个生物类似药已上市。
结束语:
再生元的Eylea自上市以来一直是眼科疾病治疗领域的主导药物之一,尤其是在湿性黄斑变性和糖尿病性黄斑水肿等适应症中。此次Opthea和Unity的试验结果进一步巩固了Eylea的市场地位。与此同时,Opthea和Unity面临着巨大的市场压力,需要重新评估其研发策略和产品管线。
识别微信二维码,添加抗体圈小编,符合条件者即可加入抗体圈微信群!
请注明:姓名+研究方向!
本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
临床结果生物类似药临床3期
2025-03-25
iStock, White Bear Studio
The Eylea franchise was in need of a win after an appellate court last week denied the pharma’s bid to block Amgen’s biosimilar from the U.S.
Two investigational eye therapies, from Opthea Limited and UNITY Biotechnology, were unable to unseat
Regeneron
’s blockbuster anti-VEGF therapy Eylea on Monday as the standard of care in two different ophthalmic indications.
The news comes as Regeneron last week
lost its court appeal
to prevent Amgen’s biosimilar Pavblu from entering the U.S. market. In a March 15 note to investors, BMO Capital Markets analysts said the failed appeal “reads as a modest negative to Regeneron” and compounds the existing risk to its Eylea franchise.
Presenting topline data from the Phase III COAST study, Australian biotech Opthea revealed that its investigational VEGF blocker sozinibercept
failed
to significantly outperform Eylea at improving vision in patients with wet age-related macular degeneration (AMD).
At 52 weeks, best-corrected visual acuity (BCVA) in those treated with sozinibercept improved by 12.8 letters on average from baseline, while mean improvement in Eylea counterparts was 13.7 letters.
Like Eylea, sozinibercept is designed to be injected into the eye and also works by binding VEGF, a protein involved in the formation of new blood vessels. Uniquely, however, sozinibercept targets the VEGF-C and VEGF-D subtypes (Eylea binds to VEGF-A and placental growth factor), which according to Opthea is
highly expressed
in patients receiving the standard VEGF-A therapies, in turn leading to leaky blood vessels that could ultimately also harm vision.
Sozinibercept is Opthea’s
only clinical candidate
, and wet AMD is its most advanced indication. Monday’s Phase III stumble thus presents a financial problem for the biotech, which in its news release revealed that it “has been assessing its rights and obligations” to investors. Opthea could be on the hook for certain payments that “would have a material adverse impact on the solvency of the company,” it wrote.
The biotech is in “active discussions” with its investors, trying to determine “whether there is a pathway that represents the best outcome for the company and its shareholders,” according to Monday’s release. Opthea has yet to reach a decision but is mulling over terminating the COAST trial or unmasking a separate wet AMD trial.
Also on Monday, California-based UNITY Biotechnology announced that its investigational eye injection UBX1325 likewise
fell to Eylea
in patients with diabetic macular edema. Topline data from the Phase IIb ASPIRE study showed that UBX1325 improved visual acuity by more than five letters at 24 and 36 weeks versus baseline.
These gains, according to UNITY, were “non-inferior” to Eylea at almost all time points through 36 weeks except at the average of weeks 20 and 24. At this time point, UBX1325 showed non-inferiority at an 88% confidence interval—just shy of the 90% prespecified threshold for the study’s primary endpoint.
Despite missing its target, UNITY CEO Anirvan Ghosh sang an optimistic tune in a statement on Monday, noting that UBX1325 “showed robust vision improvements in a difficult to treat patient population.” The biotech will continue to advance the candidate into late-stage studies.
临床结果临床3期临床2期
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
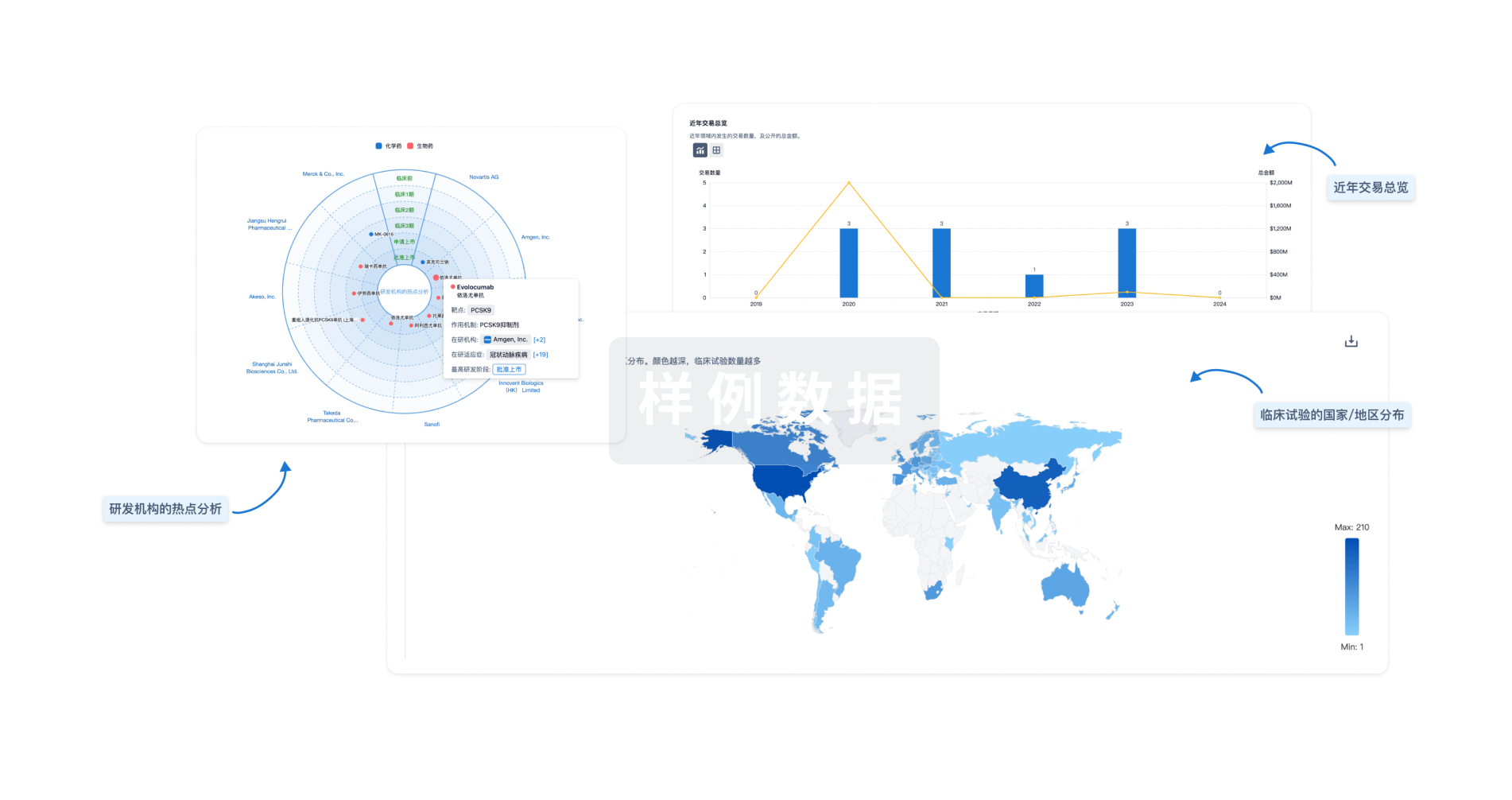
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用