预约演示
更新于:2025-07-06

The Salk Institute for Biological Studies
更新于:2025-07-06
概览
标签
神经系统疾病
肿瘤
其他疾病
小分子化药
间充质干细胞疗法
合成多肽
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 6 |
| 合成多肽 | 1 |
| CRISPR/Cas9 | 1 |
| 腺相关病毒基因治疗 | 1 |
| 间充质干细胞疗法 | 1 |
关联
11
项与 The Salk Institute for Biological Studies 相关的药物作用机制 Akt 抑制剂 [+1] |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 PCDH15 modulators |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
作用机制 CRHR1拮抗剂 [+1] |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
23
项与 The Salk Institute for Biological Studies 相关的临床试验NCT06891352
Optimization of Chrononutrition to Reduce the Risk of Disease in Shift Workers - The SHIFT Study
In this randomized controlled trial, the investigators will assess the health impacts of optimizing the timing of dietary consumption in nurses and nursing assistants who work night shifts, have a habitual eating window of 14 hours or more, and elevated weight. Participants will be randomized to one of three groups: (1) dietary monitoring, (2) dietary monitoring plus 10-hour daytime time-restricted eating (TRE), or (3) TRE with a low-glycemic snack during night shifts. The study includes a 2-week screening/baseline health assessment, with follow-up health assessments at 3-, 6- (primary outcome), and 12 months.
开始日期2025-06-02 |
申办/合作机构 |
NCT06884059
Impact of Time-Restricted Eating (TRE) on Kidney Health (The TREK Study)
This is a clinical trial to assess how time-restricted eating (TRE) may improve kidney health and filtration patients with type 2 diabetes and increased protein content in their urine. All participants will be participating in TRE in which they follow a consistent 8-10 hour eating window everyday.
开始日期2025-03-01 |
申办/合作机构 |
NCT06555406
Time-restricted Eating as an Adjunctive Intervention for Bipolar Disorder
The goal of this clinical trial is to understand how level of adherence with time-restricted eating (TRE) predicts change in diurnal rhythms (as measured using the amplitude of diurnal peripheral clock gene expression), and how those changes predict lower mania and depressive symptoms, and downstream improvements in quality of life. The effects of diurnal amplitude of clock gene expression is expected to remain significant when controlling for change in glucose tolerance and inflammation. Participants will be enrolled who are already receiving medication treatment for bipolar disorder. Participants will complete daily measures of eating, sleep and mood for two weeks, and then will be assigned to follow TRE for eight weeks. Symptoms and Quality of Life will be measured at baseline and during and after the food plan.
开始日期2024-11-22 |
申办/合作机构 |
100 项与 The Salk Institute for Biological Studies 相关的临床结果
登录后查看更多信息
0 项与 The Salk Institute for Biological Studies 相关的专利(医药)
登录后查看更多信息
11,108
项与 The Salk Institute for Biological Studies 相关的文献(医药)2025-09-01·Life Science Alliance
PSME3 regulates migration and differentiation of myoblasts
Article
作者: Cho, Ukrae H ; Kuhn, Kenneth D ; Hetzer, Martin W
The acquisition of cellular identity requires large-scale alterations in cellular state. The noncanonical proteasome activator PSME3 is known to regulate diverse cellular processes, but its importance for differentiation remains unclear. Here, we demonstrate that PSME3 binds dynamically to highly active promoters over the course of differentiation. However, loss of PSME3 does not globally affect mRNA transcription. We find instead that PSME3 influences the levels of several adhesion-related proteins and acts upstream of the HSP90 co-chaperone NUDC to regulate cell motility and myoblast differentiation in a proteasome-independent manner. Our findings reveal several new facets of PSME3 functionality and highlight its importance for the differentiation of myogenic cells.
2025-09-01·BIOORGANIC & MEDICINAL CHEMISTRY
Scaffold hopping and sidechain modification from a flavone scaffold lead to discovery of potent, selective CK2A2 inhibitors with favorable properties for CNS activity
Article
作者: Gage, Fred H ; Tucker, James K ; Da Silva, Ioana I N
The human protein kinase CK2 has long been of interest as a target in oncology, but new evidence is emerging of its role in central nervous system (CNS) disorders. The CK2 catalytic subunit paralog CK2A2 is enriched in the CNS relative to other tissues; however, the catalytic subunit paralog CK2A1 is expressed at similar levels across most tissues. Current treatment modalities centered on CK2 inhibition under clinical study lack evidence of CNS activity, kinome-wide selectivity, or CK2A2 paralog selectivity. Therefore, a brain-penetrant inhibitor selective for CK2A2 over CK2A1 may enable the further elucidation of the role of this paralog in CNS pathologies. In this work, we describe a series of flavone-inspired inhibitors of CK2A1 and CK2A2 designed and synthesized in a structure-based drug-design campaign. Multiple candidates demonstrating promising CK2A2 potency, kinome-wide selectivity, and CNS permeability/activity were identified, with compound 65 representing the best confluence of these properties. Although these lead candidates exhibited only up to three-fold preferential inhibition of CK2A2, they represent a starting point for the study of CK2A2 and the disorders it may mediate in the CNS.
2025-08-01·NEUROSCIENCE
Stable expression of voltage-gated calcium channel mRNA in α2δ (CACNA2D) knockout mouse brains
Article
作者: Geisler, Stefanie M ; Traxler, Larissa ; Obermair, Gerald J
Voltage-gated Ca2+ channels (VGCCs) regulate Ca2+ entry in healthy and diseased neurons, and their function is modulated by auxiliary α2δ subunits. Among the four α2δ isoforms, α2δ-1, α2δ-2, and α2δ-3 show overlapping expression in various brain regions, raising questions about their respective specific and redundant roles. Here, we investigated if the loss of α2δ isoforms affects mRNA expression of other VGCC α1, α2δ, and β subunits. Moreover, qPCR expression profiling in knockout conditions provides insights into potential compensatory mechanisms. To this end, we analyzed the expression of the high-VGCC complement, including seven α1, four β, and four α2δ subunit isoforms, in hippocampal and striatal tissues from α2δ single and α2δ-1/-3 double knockout mice. Our findings reveal that mRNA expression profiles of hippocampal and striatal tissues contain the entire set of neuronal high-VGCC subunits. Notably, α2δ-3 mRNA is the most abundant isoform in striatum and α2δ-1/-3 double knockout mice show increased amounts of mutant α2δ-3 mRNA reporter transcripts compared to α2δ-3 single knockout mice. These findings support a critical role of α2δ-3 in GABAergic striatal medium spiny neurons. Of note, mRNA expression levels of individual α1 and β isoforms were remarkably similar between α2δ single knockout and α2δ-1/-3 double knockout compared to control mice. Taken together, our study provides novel insights into the resilience of VGCC mRNA levels to disruptions of α2δ isoform expression, suggesting transcriptional stability of core calcium channel components comparable to housekeeping genes. However, this stability does not fully prevent physiological deficits, suggesting limited functional compensation at the transcript level.
162
项与 The Salk Institute for Biological Studies 相关的新闻(医药)2025-05-29
Scientists analyzed almost 200 cannabis genomes to create the most comprehensive, high-quality, detailed genetic atlas of the plant to date. The atlas reveals unprecedented diversity and complexity within the species, sets the stage for advances in cannabis-based agriculture, medicine, and industry, and builds on a 10,000-year long relationship between humans and cannabis, showing that cannabis can be as important as other crops like corn or wheat.
Cannabis has been a globally important crop for millennia. While best known today as marijuana for its psychoactive cannabinoid THC (tetrahydrocannabinol), historically, cannabis has been a cornerstone of human civilization, providing seed oil, textiles, and food for more than 10,000 years. Today, cannabis remains an understudied and underutilized resource, but United States legislation passed in 2014 and 2018 have re-energized cannabis crop development for medicinal, grain, and fiber applications.
Researchers from the Salk Institute have created the most comprehensive, high-quality, and detailed genetic atlas of cannabis to date. The team analyzed 193 different cannabis genomes (entire sets of genetic information), revealing an unprecedented diversity, complexity, and untapped opportunity within this foundational agricultural species. This landmark achievement was the result of a multi-year collaboration with Oregon CBD, Oregon State University, and the HudsonAlpha Institute of Biotechnology.
The findings, published in Nature on May 28, 2025, set the stage for transformative advances in cannabis-based agriculture, medicine, and industry.
"Cannabis is one of the most extraordinary plants on Earth. Despite its global importance as a source of medicine, food, seed oil, and fiber for at least the last 10,000 years, it remains one of the least developed major crops of modern times, largely due to a century of legal restrictions," says Todd Michael, senior author of the study and research professor at Salk. "Our team constructed the most complete genetic map, or pangenome, of the plant to date by analyzing nearly 200 diverse cannabis genomes, showing that we are just starting to see the full potential of this amazing plant. Those same legal restrictions spurred an underground breeding revolution, revealing cannabis's power as a chemical factory. With this new genomic blueprint, we can now apply modern breeding to unlock novel compounds and traits across agriculture, medicine, and biotechnology."
Background: Cannabis as a chemical powerhouse
Cannabis sativa, also known as hemp, is a flowering plant native to Asia. Cannabis has many unique features that have made it a prominent crop over the course of human history, like its ability to produce strong fibers for textiles or its medicinal qualities stemming from its being one of the few plants to make high quantities of cannabinoids. Innovators today suggest that cannabis oil could rival canola or soybean with the right breeding, or that cannabis derivatives could even be used as a sustainable alternative to jet fuel.
Cannabis is a chemical powerhouse. It can produce more than 30% by dry weight as terpenes and cannabinoids, small chemicals that the plant makes to protect against predators, yet humans leverage for mood-altering purposes. Terpenes create the exquisite aromas that attract us to fruits and flowers, while cannabinoids interact with the human body to provide many therapeutic properties. One cannabinoid, the non-psychedelic cannabidiol (CBD), expanded the public's view of cannabis when the "Charlotte's Web" strain was used to treat epileptic seizures. CBD, tetrahydrocannabinol (THC), and more than 100 other poorly studied cannabinoids have been used to treat a variety of ailments, including pain, arthritis, nausea, asthma, depression, and anxiety.
Importantly, the impact this selective breeding has had on cannabis's genomic diversity has remained a mystery. Solving this mystery has proven difficult since cannabis has a complicated genome. First, cannabis is among the less than 5% of plants to have distinct female and male sexes on separate plants. Second, cannabis genomes contain many transposable elements, which are repetitive stretches of DNA that can "jump" around the genome and are thus difficult to track.
Key discoveries: New, and surprisingly diverse, genetic patterns
Scientists use a technology called sequencing to determine the patterns of nucleic acids, which connect across DNA's double helix to form base pairs, along DNA strands. Traditional short-read sequencing methods chop up the DNA to investigate it piece by piece, just a few hundred base pairs at a time. Newer long-read sequencing techniques can capture thousands of base pairs at once.
"There are limits to what you can discover with short-read sequencing technologies, since those short genetic excerpts are impossible to stitch together in any meaningful way when looking at complex regions of the genome, especially repetitive DNA sequences," says co-first author Lillian Padgitt-Cobb, a postdoctoral researcher in Michael's lab. "We're among the first to harness this long-read technology at scale in the pangenome context, and with that comes all these insights into structural variation and gene ordering that can inform end-game decisions about breeding favorable traits into cannabis plants."
The study isn't the first to use long-read sequencing -- in fact, Michael himself was the first researcher to generate a chromosome-level genome of cannabis using long-read sequencing back in 2018, which revealed complex genetic architecture where cannabinoids are synthesized, and explained the breeding history behind anti-epileptic Charlotte's Web. Where this new study stands apart is its completeness. It contains the most genomes yet, and is the first to include sex chromosomes and, relatedly, the first to have haplotype resolution.
Cannabis is a diploid plant. This means that, like humans, it contains two sets of chromosomes, one set inherited from a male plant and the other from a female plant. While most genomes published to date have only been able to decode one chromosome, also known as haplotype resolution, the team resolved both sets of cannabis chromosomes. By looking at both chromosome sets, the researchers revealed an unprecedented amount of genetic variation -- possibly up to 20 times that of humans.
"With this haplotype resolution," Padgitt-Cobb explains, "we can look at what was inherited from just one of the parent plants and start to understand the breeding and background of that plant."
The team's study collected genomes from 144 different cannabis plants from around the world to assemble 193 total genomes -- 181 of which had never been catalogued before. The genome total is greater than the plant total owing to that haplotype resolution, since each plant that had both chromosome sets investigated produced two genome assemblies. Collectively, these many genomes make up the pangenome, which was analyzed to understand the full extent of genetic diversity within the cannabis species.
The high quality of the collected genomes allowed the researchers to resolve previously unseen genetic patterns, including the architecture of genes responsible for cannabinoid synthesis, and, by incorporating sex chromosomes, a first look at cannabis Y chromosomes.
Their first discovery was that there is unexpected diversity within the species. Across the pangenome, 23% of genes were found in every genome, 55% were nearly universal (seen in 95%-99% of genomes), 21% were in between 5% and 94% of genomes, and less than 1% were entirely unique. Some of the most universal genes were those that produce cannabinoids.
While cannabinoid genes were consistent across genomes, genes related to fatty acid metabolism, growth, and defense were not. These variable genes are an untapped breeding pool, and their selective breeding could also make cannabis more robust in the field or improve the nutritional content of hemp oil to make it a competitor among existing seed oils. Notably, the research team discovered that structural variation in the fatty acid biosynthetic pathway contributes to the production of tetrahydrocannabivarin (THCV), a rare varin-type cannabinoid gaining attention for its non-psychoactive, energizing effects.
Looking more closely at cannabinoid genes across the pangenome, the researchers concluded that two genes, THCAS and CBDAS, are likely under strong selective pressure from human-directed breeding for THC and CBD content. Importantly, they found that cannabinoid genes are located in transposable elements. Selectively breeding for genes inside these "jumping" transposable elements has, in turn, created immense diversity among cannabis plants.
Looking ahead: Optimizing plants for health and industry
The researchers also identified interesting targets for agricultural optimization. First, by looking at the differences between European and Asian genomes, they concluded there is likely an ancient cannabis relative somewhere in Asia waiting to be discovered. This wild relative will have novel genetic adaptations related to its unique environmental history, making it a wealth of information for breeding cannabis plants that are more resilient crops.
Finally, the novel insight into sex chromosomes revealed that there are genes only present in "father" plants that can be used to breed better-performing offspring. Modern marijuana breeding leverages "feminization," where farmers induce a female plant to make male flowers -- entirely bypassing the Y chromosome. These new findings suggest that breeding programs may be missing valuable genetic diversity and trait potential encoded in those bypassed male genomes. Incorporating true male plants into breeding strategies could unlock overlooked genetic gains and expand opportunities for crop improvement.
"Over the last 10 years, breeders have already done a decent job of getting yields up and making cannabis an economically viable crop," says co-first author Ryan Lynch, a postdoctoral researcher in Michael's lab. "Once there's market interest there, paired with these new insights into cannabis genomes that can guide breeding efforts, I can see hemp and hemp oils really booming in both human health and industry applications."
In the short term, the team hopes the pangenome will serve as a dynamic resource for researchers around the world to build upon and use to inform cultivation strategies, helping to realize the untapped potential of cannabis as a valuable multi-use crop grown for fiber, seed oil, and medicine.
2025-05-28
SAN DIEGO, May 28, 2025 /PRNewswire/ -- As federal funding for medical and life sciences research faces deep and destabilizing cuts, Prebys Foundation is stepping in with a rapid response package totaling $7 million to defend San Diego's biomedical research sector—one of the world's leading innovation hubs.
Federal grants have historically provided nearly half of all medical research funding in the United States. This support has enabled transformative advances in drug discovery, fueled job growth, and secured America's position as a global leader in the life sciences. In San Diego, the impact has been profound, home to internationally renowned research institutes, universities, and biotech startups that together make up a biomedical ecosystem unlike any other in the country.
But that ecosystem is now under severe strain. In confidential conversations with the Prebys Foundation, leaders across the medical research field shared frank and urgent concerns about the future of their work. These quotes are presented without attribution to protect the identities of those who spoke candidly under an agreement of anonymity:
"The suction of talent is real. People need to understand that the NIH and U.S. taxpayers have invested billions in training scientists, and now we're losing them—often for pennies on the dollar—to countries like Sweden and China that have the infrastructure to support robust research programs."
"As of now, few grants have been awarded in 2025 - the pipeline is dry and constricted. Most research spans five years and is funded on a rolling basis each quarter—but this year, even renewals that should have been routine are disappearing."
Executive orders and steep reductions in federal research investment are threatening critical local initiatives, halting active projects, and forcing early- and mid-career scientists to look abroad or leave the field altogether. Without swift and targeted action, the region risks an exodus of talent and a slowdown in the medical breakthroughs that improve lives and drive the economy.
"San Diego's biomedical research institutions aren't just world-class in reputation—they deliver real impact by tackling urgent problems and advancing the treatments and cures the world needs," said Grant Oliphant, CEO of the Prebys Foundation. "While we can't match the scale of federal investment, we can respond with urgency to help prevent the loss of extraordinary talent and critical momentum. This is a defining moment, and philanthropy must rise to meet it."
To address the immediate need, Prebys Foundation is awarding grants to seven anchor institutions:
La Jolla Institute for Immunology – $1,000,000
Rady Children's Hospital Foundation – $1,000,000
Salk Institute for Biological Studies – $1,000,000
San Diego State University – $1,000,000
Sanford Burnham Prebys Medical Discovery Institute – $1,000,000
Scripps Research – $1,000,000
University of California San Diego – $1,000,000
The grants will provide general operating support aimed at retaining early and mid-career scientists at risk of being lost to the field, as well as supporting key research programs.
"This is not just about science—it's about our economy, our global leadership, and the health of future generations," said Oliphant. "This funding was an emergency allocation above and beyond our planned giving for the year. We urge other funders and stakeholders to join us in going above traditional spending allocations to help preserve the excellence and impact of San Diego's life sciences community."
About Prebys Foundation
The Prebys Foundation—pronounced Preh-Biss—is a charitable foundation based in San Diego County. We are dedicated to advancing a vibrant, equitable, and resilient future for all San Diegans by investing in four key areas: health and well-being, medical research, arts and culture, and youth success.
While we operate under both Prebys Foundation and The Conrad Prebys Foundation as our DBAs, we use "Prebys Foundation" in our branding to keep things concise, accessible, and aligned with our forward-facing identity.
SOURCE The Conrad Prebys Foundation
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
2025-04-09
SEOUL, South Korea, April 9, 2025 /PRNewswire/ -- Darnatein, a wholly-owned subsidiary of OSR Holdings, Inc. (NASDAQ: OSRH), today announces that it has successfully secured an additional international patent for its protein-based osteoarthritis treatment technology, marking a significant step in its expansion into the global market.
Activin/BMP7 Chimera Protein Technology Registered in China
Darnatein has officially registered a patent with the China National Intellectual Property Administration (CNIPA) for the core technology behind its break-through disease-modifying osteoarthritis drug (DMOAD) lead drug candidate, DRT-101. Following the national registration of the patent in South Korea in November last year, this marks the company's first successful international patent registration as part of its efforts to secure global intellectual property rights through the PCT (Patent Cooperation Treaty) route in key regions such as the EU, the United States, and China.
The technology basis is an AI-enhanced innovative protein structure generator designed to provide therapeutics that overcome the current limitations of standard of care treatment in osteoarthritis—a condition for which only symptom management options currently exist. This technology represents a wholly new approach to protein design and is expected to address the underlying causes of disease. This treatment approach may significantly improve treatment outcomes not only for osteoarthritis but also for a wide range of other musculoskeletal disorders.
In particular, the DRT-101 chimeric protein, which recombines the natural BMP7 and Activin proteins into a wholly novel structure, has already been shown to enhance both therapeutic efficacy and safety in vivo, in studies conducted between 2020 and 2024 at the University of California, San Diego, School of Medicine.
Senyon Choe, Darnatein Chief Executive Officer, stated, "The protein design technology now also patented in China has been developed over years from a core platform strategy to the current technology with the potential to revolutionize the global OA treatment market. Securing intellectual property rights in China, one of the largest markets in the world, is a crucial stepping-stone for our global expansion."
Constance Höfer, Chief Scientific Officer of OSR Holdings, stated, "Darnatein's groundbreaking technology represents a wholly new, AI-enhanced approach to therapeutic protein design. The successful patent registration in China underscores the novelty and relevance of this technology to the development of better treatment options for OA patients worldwide."
Global Technological Competitiveness and Licensing Potential
The osteoarthritis treatment market continues to grow, due to globally aging populations. In 2023, the market size reached approximately USD 8.9 billion and is projected to grow at an average annual rate of about 7%, reaching approximately USD 16.1 billion by 2032. China is experiencing rapid population aging and a surge in osteoarthritis cases, making it a highly promising market.
Industry experts have remarked, "Darnatein's Activin/BMP7 chimera technology offers a superior profile to be developed into a potential DMOAD, or disease-modifying OA drug, compared to existing standard of care for osteoarthritis treatments," adding, "Big Pharma is looking for novel treatments that can slow, stop, or even reverse the cartilage degeneration and joint damage that occurs with OA. On this backdrop, Darnatein's chimeric protein approach represents a paradigm shift away from only symptom relief (e.g. painkillers and anti-inflammatories) to treatment options targeting the underlying pathobiology of OA"
Darnatein is currently completing preclinical studies with DRT-101, its degenerative OA treatment candidate, with the goal to initiate Phase 1 clinical trials later this year.
About Darnatein
Founded in 2012, Darnatein is a biotherapeutics company based in South Korea developing a pipeline of innovative treatments for osteoarthritis and bone fusion, including DRT-101 as a ground breaking disease-modifying OA drug (DMOAD) candidate. Darnatein was established by Dr. Senyon Choe, one of the co-founders of the structural protein laboratory of the prestigious Salk Institute for Biological Studies in La Jolla, CA, and a faculty member of UC San Diego since 1993. Darnatein operates as a wholly owned subsidiary of OSR Holdings, Inc. following its acquisition in 2023.
About OSR Holdings, Inc.
OSR Holdings, Inc. is a global healthcare company dedicated to advancing biomedical innovation. Through its subsidiaries, OSR is engaged in oncology immunotherapies, degenerative disease biologics, and medical device distribution. OSR's vision is to acquire and operate a portfolio of innovative healthcare companies, improving patient care through cutting-edge research and development. For more information, visit .
Contact
[email protected]
SOURCE OSR Holdings Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
并购
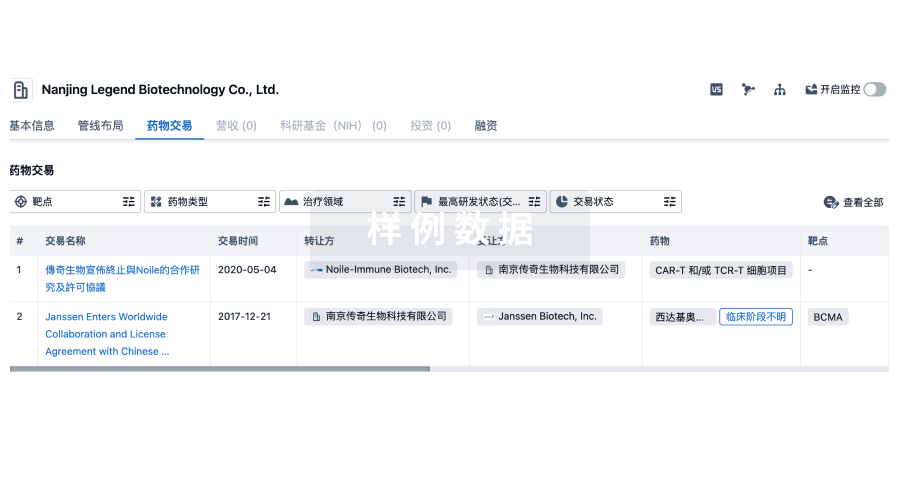
100 项与 The Salk Institute for Biological Studies 相关的药物交易
登录后查看更多信息
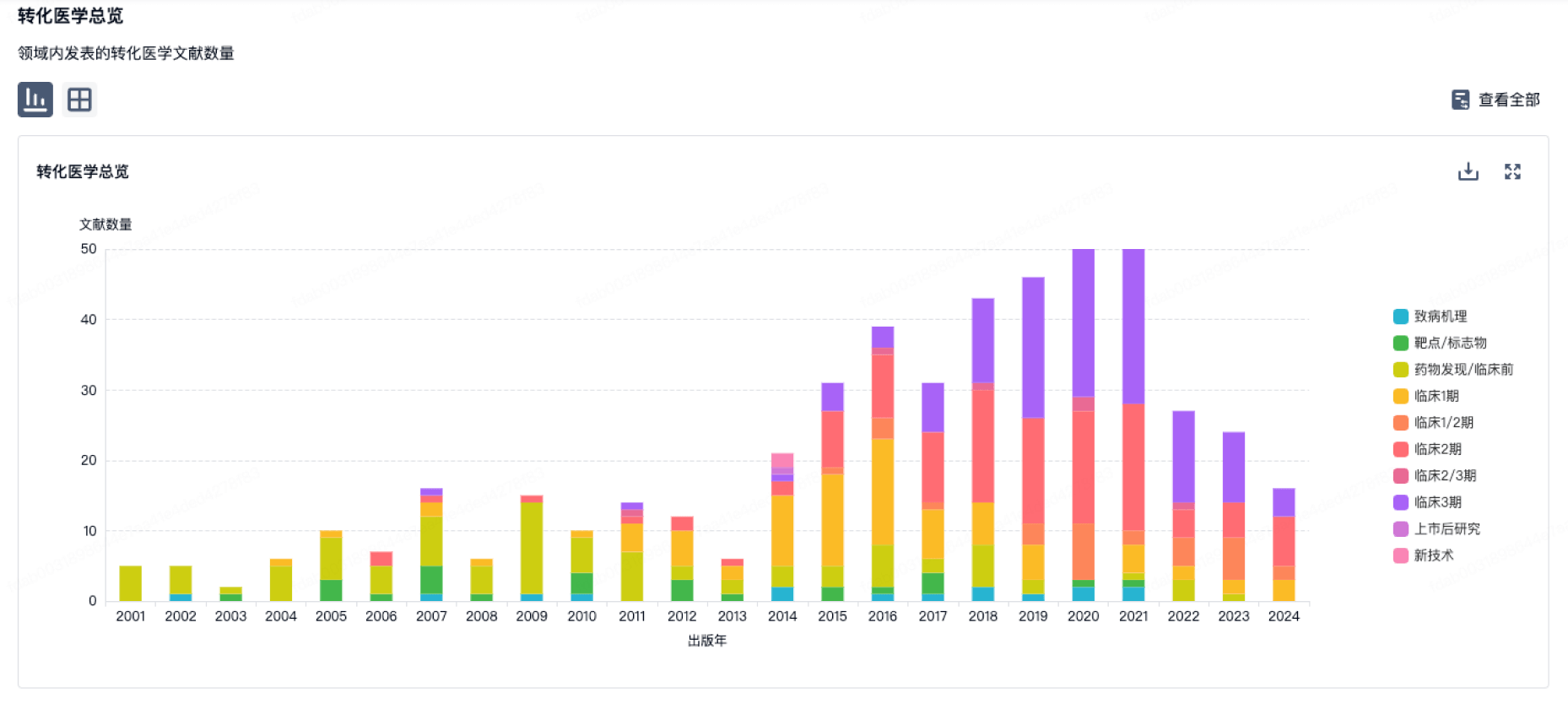
100 项与 The Salk Institute for Biological Studies 相关的转化医学
登录后查看更多信息
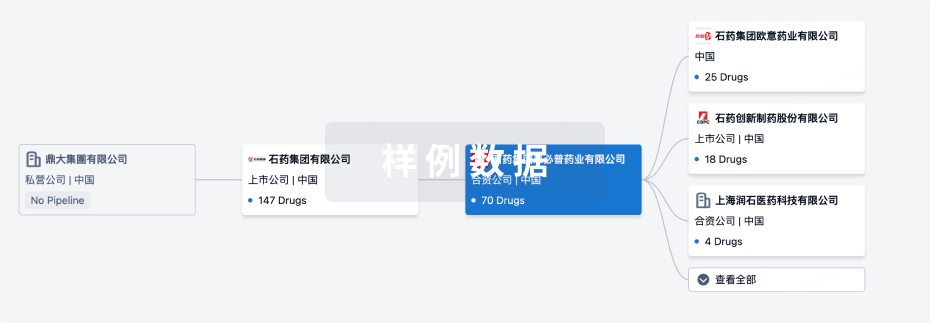
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月18日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
4
7
临床前
其他
9
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
CRISPR–Cas9 therapy(Salk Institute for Biological Studies) | 早衰 更多 | 临床前 |
SR9011 ( NR1D1 x NR1D2 ) | 肿瘤 更多 | 临床前 |
J-147 ( 5-LOX ) | 阿尔茨海默症 更多 | 临床前 |
NP-C86 | 炎症性肠病 更多 | 临床前 |
15d-PGJ2 ( Akt x PPARγ ) | 代谢性疾病 更多 | 临床前 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
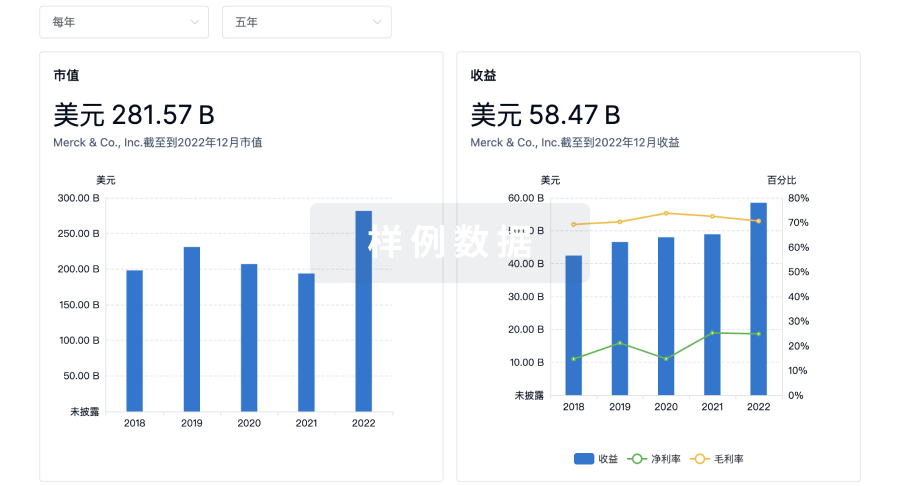
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



