预约演示
更新于:2025-09-09

Sanford Burnham Prebys Medical Discovery Institute
更新于:2025-09-09
概览
标签
肿瘤
感染
心血管疾病
小分子化药
化学药
siRNA
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 24 |
| 化学药 | 2 |
| 诊断用放射药物 | 1 |
| 治疗性疫苗 | 1 |
| 分子胶 | 1 |
关联
29
项与 Sanford Burnham Prebys Medical Discovery Institute 相关的药物靶点 |
作用机制 PSMA抑制剂 [+1] |
在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2021-05-26 |
靶点 |
作用机制 CSF-3R激动剂 |
在研适应症 |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 MYC调节剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
9
项与 Sanford Burnham Prebys Medical Discovery Institute 相关的临床试验NCT04199000
Clinical and Basic Investigations Into Congenital Disorders of Glycosylation
The purpose of this research is to study the natural history of congenital disorders of glycosylation and its causes and treatments.
开始日期2019-10-08 |
申办/合作机构 |
NCT03032627
Identifying Targets of Maladaptive Metabolic Responses in Heart Failure
The purpose of the research is to help researchers understand changes in metabolism in patients that develop heart failure.
开始日期2017-03-20 |
NCT02728635
Epigenetic Regulation of Human Adipose Tissue Distribution
The purpose of this study is to collect data to help researchers better understand the different ways that women or men store fat (apple shape versus pear shape).
开始日期2016-07-01 |
100 项与 Sanford Burnham Prebys Medical Discovery Institute 相关的临床结果
登录后查看更多信息
0 项与 Sanford Burnham Prebys Medical Discovery Institute 相关的专利(医药)
登录后查看更多信息
6,536
项与 Sanford Burnham Prebys Medical Discovery Institute 相关的文献(医药)2025-12-31·Gut Microbes
Article
作者: Murakami, Ryuta ; Katoh, Toshihiko ; Odamaki, Toshitaka ; Nakajima, Aruto ; Rodionov, Dmitry A. ; Nagao, Saeko ; Kozakai, Tomoya ; Yoshida, Keisuke ; Hirose, Junko ; Sakanaka, Mikiyasu ; Ojima, Miriam N. ; Katayama, Takane ; Xiao, Jin-Zhong ; Arzamasov, Aleksandr A.
Fortifying infant formula with human milk oligosaccharides, such as 2'-fucosyllactose (2'-FL), is a global trend. Previous studies have shown the inability of pathogenic gut microbes to utilize 2'-FL. However, the present study demonstrates that the type strain (JCM 1290T) of Clostridium perfringens, a pathobiont species often more prevalent and abundant in the feces of C-section-delivered infants, exhibits potentially pathogenic growth on 2'-FL. The expression of genes for α-toxin, an activator of NLRP3 inflammasome, and ethanolamine ammonia-lyase, a factor responsible for the progression of gas gangrene, was significantly upregulated during 2'-FL assimilation compared to growth on lactose. However, colony-forming unit of C. perfringens JCM 1290T markedly decreased when co-cultivated with selected strains of Bifidobacterium, a taxon frequently detected in the breastfed infant gut. Moreover, during co-cultivation, the expression of virulence-related genes, including the gene for perfringolysin O - another activator of NLRP3 inflammasome - were significantly downregulated, while the lactate oxidation genes were upregulated. This can occur through two different mechanisms: direct competition for 2'-FL between the two organisms, or cross-feeding of lactose, released from 2'-FL by C. perfringens JCM 1290T, to Bifidobacterium. Attenuation of α-toxin production by the selected Bifidobacterium strains was observed to varying extents in 2'-FL-utilizing C. perfringens strains clinically isolated from healthy infants. Our results warrant detailed in vivo studies using animal models with dysbiotic microbiota dominated by various types of C. perfringens strains to further validate the safety of 2'-FL for clinical interventions, particularly on vulnerable preterm infants.
2025-12-31·Gut Microbes
Human milk oligosaccharide metabolism and antibiotic resistance in early gut colonizers: insights from bifidobacteria and lactobacilli in the maternal-infant microbiome
Article
作者: Arzamasov, Aleksandr A ; Bode, Lars ; Martínez-Costa, Cecilia ; Cabrera-Rubio, Raul ; Acuna-Gonzalez, Antia ; Rodionov, Dmitry A ; Segata, Nicola ; Samarra, Anna ; Spann, Kennedy ; Osterman, Andrei L ; Renwick, Simone ; Hall, Lindsay ; Collado, MCarmen
Breast milk, rich in human milk oligosaccharides (HMOs), supports the early-life colonization of beneficial bacteria such as bifidobacteria and lactobacilli, potentially reducing early-life antibiotic resistance. However, antibiotic treatment may interfere with the beneficial functions of HMO-degrading bacteria. This study investigated the metabolism of HMOs by bifidobacteria and lactobacilli isolated from human milk and mother-infant paired fecal samples, along with their antibiotic resistance profiles. Understanding these species- and sample-type-specific interactions will provide valuable insights into how bioactive components in human milk may shape the infant resistome during early life. A total of 39 Bifidobacterium and 14 Lactobacillaceae strains were isolated from paired mother-infant fecal and breast milk samples. Whole genome sequencing (WGS) allowed functional predictions on the HMO metabolism abilities and the resistance genotype of each strain. In vitro HMO utilization was assessed using growth kinetics assays combined with HMO glycoprofiling in culture supernatant. The minimum inhibitory concentration (MIC) was also determined for each strain. HMO metabolism by the bifidobacteria was species-specific. Bifidobacterium bifidum (B. bifidum) and Bifidobacterium longum subsp. infantis (B. infantis) exhibited the highest capacity for HMO degradation, consistent with genomic predictions. In contrast, lactobacilli were unable to degrade HMOs in vitro but were predicted to metabolize the by-products of HMO degradation. Phenotypic analysis revealed that B. bifidum strains had the lowest levels of antibiotic resistance, while Bifidobacterium animalis subsp. lactis (B. lactis) strains were resistant to most tested antibiotics. Overall, B. bifidum demonstrated the strongest HMO-degrading ability while remaining the most antibiotic-susceptible species. Early-life colonizing bifidobacterial species possess the essential machinery required to degrade HMOs and are highly susceptible to antibiotics. A better understanding of these dynamics could inform clinical strategies to protect and restore the infant gut microbiome, particularly in neonates exposed to antibiotics.
2025-11-01·NEUROPHARMACOLOGY
Sex-dependent role of Neuropeptide-S on anxiety, fear conditioning, and alcohol seeking in alcohol preferring rats
Article
作者: Clark, Stewart ; Li, Min ; Runyon, Scott P ; Ciccocioppo, Roberto ; De Carlo, Sara ; Haass-Koffler, Carolina L ; Cannella, Nazzareno ; Soverchia, Laura ; Roberto, Marisa ; Sheffler, Douglas J
Alcohol Use Disorder (AUD) is a global health concern, with stress playing a crucial role in its development and persistence. Currently, no pharmacotherapies specifically targeting stress are approved for AUD treatment. Neuropeptide S (NPS) plays a dual role in stress regulation, exhibiting both anxiolytic and stress-enhancing effects. While NPS reduces alcohol self-administration (ASA) in alcohol preferring rats, its role in AUD-related stress and anxiety remains unclear. This study investigated the behavioral effects of NPS in male and female Marchigian Sardinian alcohol-preferring (msP) rats. To assess its impact on locomotion, anxiety, and fear memory, we conducted an open-field, an elevated plus maze (EPM), and a fear conditioning (FC) paradigm following intracerebroventricular administration of NPS. Furthermore, we examined the effects of NPS on ASA and yohimbine-induced reinstatement of alcohol-seeking in msP rats. Our results indicate that NPS administration increased locomotor activity in both sexes and selectively alleviated generalized anxiety levels in male rats in the EPM test. In the FC task, administration of NPS immediately after FC test facilitated the extinction of fear memories in females but not in males. Notably, NPS reduced ASA in both female and male rats but did not alter yohimbine-induced reinstatement of alcohol-seeking. In conclusion, NPS modulates anxiety in a sex-dependent manner. Since both alcohol and NPS alleviate anxiety and fear conditioning in msP rats, NPS may reduce alcohol intake by replacing the anxiolytic properties of alcohol. These effects appear to be sex-dependent, with NPS primarily alleviating generalized anxiety in males and facilitating fear extinction in females.
49
项与 Sanford Burnham Prebys Medical Discovery Institute 相关的新闻(医药)2025-08-12
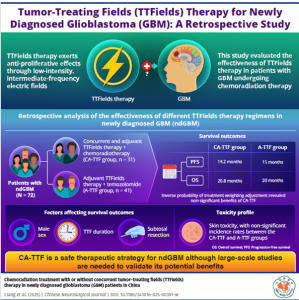
Researchers study the clinical outcomes of using tumor-treating fields therapy, with or without chemoradiation, in patients with newly diagnosed glioblastoma
BEIJING, BEIJING, CHINA, August 12, 2025 /
EINPresswire.com
/ -- The most prevalent malignant brain tumor in adults – glioblastoma (GBM) – is an aggressive cancer with a poor prognosis. Several preclinical studies suggest that the addition of tumor-treating fields (TTFields) to chemoradiation therapy (CRT) helps improve the progression-free survival (PFS) and overall survival (OS) in patients with GBM. TTFields therapy is a novel treatment strategy for cancer, in which tumors are exposed to low-intensity electrical fields of intermediate-frequency to inhibit cancer cell replication. According to previous reports, apart from an anti-mitotic effect, TTFields also increase cell permeability, activate autophagy, stimulate immune responses, and inhibit the DNA damage repair pathway of cancer cells. Increased cell permeability after TTFields therapy ensures better delivery of chemotherapeutic agents like temozolomide to glioma cells, improving response to the treatment. This provides a strong rationale for using concurrent TTFields with CRT for patients with newly diagnosed and recurrent GBM. An international phase 3 randomized clinical trial to examine the efficacy of this strategy is underway, but the real-world outcomes of this strategy are not well-studied.
To this end, Dr. Zhiyong Qin and Dr. Yang Wang from Fudan University, China, collaborated with researchers from Shanghai Gamma Hospital, China; Sidney Kimmel Cancer Center, USA; Fudan University Cancer Hospital, China; and Shanxi Academy of Medical Sciences, China, to conduct a retrospective study examining the clinical outcomes of concurrent TTFields therapy with CRT in patients with newly diagnosed GBM (ndGBM). Their findings were published in the
Chinese Neurosurgical Journal
on March 7, 2025.
This study included patients who underwent radiation therapy and TTFields at Huashan Hospital, China, between January 2020 and December 2021. “Patients were categorized into two groups: one group received adjuvant TTFields therapy after completing CRT (referred to as the A-TTF group), while the other received TTFields therapy concurrently with CRT and continued TTFields after treatment (referred to as the CA-TTF group),” explains Dr. Qin. Out of the 72 patients included in this retrospective study, 41 belonged to the CA-TTF group, and 31 were part of the A-TTF group.
The researchers compared the efficacy and toxicity of the treatment modalities between the CA-TTF and A-TTF groups. They found no significant difference in the median PFS and OS between the two treatment groups. The PFS and OS for the CA-TTF group were 14.2 months and 20.8 months, respectively, whereas for the A-TTF group, the PFS and OS were 15 months and 20 months, respectively. Dr. Wang explains, “After adjusting for baseline characteristics, the hazard ratios (HRs) for PFS and OS suggested a potential benefit for concurrent TTFields therapy, although the differences were not statistically significant,” suggesting that further investigations may be necessary to confirm the above observation. The researchers also studied the distribution of relevant molecular markers, like MGMT promoter methylation status and TERT promoter mutation status, between the two treatment groups. Earlier studies have shown that MGMT promoter methylation is associated with a better prognosis, whereas higher mutations in the TERT promoter can result in poorer prognosis. In this study, the survival outcomes for patients with methylations at the MGMT promoter was better in both CA-TTF and A-TTF groups. However, TERT promoter mutations were more prevalent in the CA-TTF group than in the A-TTF group. Despite this, these patients achieved comparable survival outcomes as the patients in the A-TTF group.
Skin-related adverse effects (AEs), such as dermatitis, pruritus, electric sensation, and skin burning sensation, were observed and graded along with the survival outcomes of patients. Mild scalp irritation was reported in 55 to 60% of the patients. Dermatitis was the most common skin-related AE, while pruritus was the second most common in this patient population. Electric sensation and burning sensation were rarely reported by these patients. Overall, the researchers found no significant difference in skin toxicity between the CA-TTF and A-TTF groups.
This study is the first real-world analysis of the advantages of concurrent TTFields therapy combined with CRT in patients with ndGBM. Dr. Qin and Dr. Wang conclude, “Our findings suggest that TTFields, when used concurrently with CRT, could maintain a favorable safety profile, with no significant differences observed in survival outcomes compared to adjuvant therapy (A-TTF group).”
To summarize, TTFields used concurrently with CRT has the potential to improve survival outcomes for patients with ndGBM.
About the University
Fudan University was established in 1905 as Fudan Public School. Fudan University is a comprehensive research-oriented university located in Shanghai, China. Fudan combines liberal education with cultivation of eminent talents through a proactive exploration of a new system that boasts of disciplinary intersection and integration and coordinates innovation and cultivation in scientific research. The University strives for a world-class undergraduate education and a postgraduate educational system with international influence, both of which inject continual vitality into the hundred-year-old institution.
Website:
https://www.fudan.edu.cn/en/
About Dr. Zhiyong Qin from Fudan University
Zhiyong Qin born in China, in 1969. He received the Ph.D. degree in neurosurgery from Fudan University, Shanghai, China, in 2000. He is currently a Professor with the Department of Neurosurgery, Huashan Hospital, Fudan University. His research focuses on developing comprehensive treatment plans for brain tumors, encompassing surgical intervention, individualized therapies, and physiotherapy approaches.
Funding information:
This study was supported by the Beijing Xisike Clinical Oncology Research Foundation (Approval Nos. Y-zai2021/qn-0204 and Y-zai2021/zd-0207).
***
Reference
Title of original paper: Chemoradiation treatment with or without concurrent tumor-treating fields (TTFields) therapy in newly diagnosed glioblastoma (GBM) patients in China
Journal: Chinese Neurosurgical Journal
DOI:
https://doi-org.libproxy1.nus.edu.sg/10.1186/s41016-025-00391-w
Yi Lu
Chinese Neurosurgical Journal
+861059978478 ext.
luyi617@sina.cn
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability
for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this
article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
临床结果临床3期放射疗法
2025-07-17
MADISON, Wis., July 17, 2025 /PRNewswire/ -- BrainXell, a leading producer of iPSC-derived human neurons and glia, is proud to announce the continued growth of its executive leadership team with the appointment of Paul Marcus as President, Chief Operating Officer, Chief Financial Officer and Board of Directors.
Continue Reading
Paul Marcus, BrainXell President, COO & CFO
Dr. Su-Chun Zhang, BrainXell's Advising CSO
The company also continues to benefit from the scientific leadership of its founder, Dr. Su-Chun Zhang, an internationally recognized expert in stem cell neuroscience whose groundbreaking work in human iPSC differentiation and CNS development underpins BrainXell's core technology platform. He now serves as Advising Chief Scientific Officer.
"We are incredibly fortunate to have Paul and Su-Chun guiding BrainXell at this pivotal time," said Katherine Vega Stultz, CEO of BrainXell. "Their leadership reflects the heart of BrainXell's work, combining scientific breakthroughs with operational strength to accelerate progress in both our research tools and therapeutics businesses."
Mr. Marcus has decades of institutional investment experience in life sciences and broader market sectors. Mr. Marcus began his career as an executive with Bank of America and then with Morgan Stanley, followed by serving as CEO of Winchester Capital and its successor companies. Concurrently, Mr. Marcus has served in executive/c-suite positions with several market leaders in China, including: VIPKID, AINemo, Digital Domain, and 01.ai. In addition, Mr. Marcus is an Emeritus Member of the St. Jude Children's Research Hospital Board of Directors and Governors and a Governing Trustee of the Board of Trustees of the Dana-Farber Cancer Institute.
Dr. Su-Chun Zhang's research laid the scientific foundation for BrainXell's proprietary iPSC technology, which enables the generation of high-purity, functionally mature CNS cells for research and drug discovery. As a faculty member at the Sanford Burnham Prebys Medical Discovery Institute, he continues to advance the field of regenerative neuroscience. Since its founding in 2015, BrainXell has grown into an industry leader, supporting biotech and pharma partners worldwide while advancing a therapeutic pipeline aimed at addressing complex neurological diseases.
About BrainXell
BrainXell was established to translate cutting-edge stem cell science into meaningful tools and therapies for neuroscience. Using its proprietary technology to guide human iPSCs into highly enriched CNS cell types, BrainXell supports discovery and therapeutic development through a dual-operating model. Learn more at .
SOURCE BrainXell, Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
高管变更
2025-07-10
NEW YORK, NY, USA & TOKYO, Japan I July 10, 2025 I
Pfizer Inc. (NYSE: PFE) and Astellas Pharma Inc. (TSE: 4503, President and CEO: Naoki Okamura, “Astellas”) today announced positive topline results from the overall survival (OS) analysis from the Phase 3 EMBARK study evaluating XTANDI
®
(enzalutamide), in combination with leuprolide and as a monotherapy, in men with non-metastatic hormone-sensitive prostate cancer (nmHSPC; also known as nonmetastatic castration-sensitive prostate cancer or nmCSPC) with biochemical recurrence (BCR) at high risk for metastasis.
For patients treated with XTANDI plus leuprolide versus placebo plus leuprolide, EMBARK met the key secondary endpoint with a statistically significant and clinically meaningful improvement in OS. Results also showed a favorable trend towards improved OS for patients treated with XTANDI monotherapy versus placebo plus leuprolide, however the difference did not reach statistical significance. No new safety signals were observed in the analysis, and the safety results were consistent with the demonstrated safety profile of XTANDI.
1
“These data demonstrate that treatment with XTANDI can extend life for men with nmHSPC and high-risk BCR who have relapsed after initial curative-intent therapy with prostatectomy, radiation therapy or both, further validating EMBARK’s metastasis-free survival (MFS) data,” said Neal Shore, M.D., F.A.C.S, START Carolinas/Carolina Urologic Research Center. “While men with nmHSPC with high-risk BCR now have expanded treatment choices, these results demonstrate a clear clinical benefit, including both MFS and OS, supporting the clinical practice of initiating XTANDI for these patients.”
Among men who have undergone definitive prostate cancer treatment, including radical prostatectomy, radiotherapy, or both, an estimated 20-40% will experience BCR within 10 years.
2
About nine out of 10 men with high-risk BCR will develop metastatic disease, and one in three will die as a result of their metastatic prostate cancer.
3
“XTANDI is the only androgen receptor inhibitor-based regimen to demonstrate a survival benefit in metastatic HSPC and nmHSPC with high-risk BCR, as well as castration-resistant prostate cancer, highlighting its significant patient impact in advanced prostate cancer,” said Johanna Bendell, M.D., Oncology Chief Development Officer, Pfizer. “These positive results add to the robust clinical support for the use of XTANDI and broaden clinical confidence, offering men with high-risk BCR evidence that they might live longer when they start XTANDI early.”
In the EMBARK study, patients were randomized to one of three study arms: XTANDI plus leuprolide, placebo plus leuprolide, or XTANDI monotherapy. An initial analysis was previously reported in
The New England Journal of Medicine
in 2023, demonstrating that the study met its primary endpoint with a statistically significant and clinically meaningful improvement in MFS for patients treated with XTANDI plus leuprolide versus placebo plus leuprolide.
4
The most common adverse events (occurring in ≥10% of patients) in the combination group and the leuprolide-alone group were hot flashes and fatigue. The most common adverse events in the monotherapy group were gynecomastia, hot flashes, and fatigue.
4
XTANDI is currently approved in more than 80 countries, including in the United States, European Union, and Japan.
“Over 1.5 million men with advanced prostate cancer around the world have benefited from treatment with XTANDI since its initial approval in 2012,”
5
said Shontelle Dodson, Executive Vice President, Head of Medical Affairs, Astellas. “The scope and rigor of the EMBARK trial exemplify Astellas’ and Pfizer’s longstanding commitment to the prostate cancer community, and we look forward to sharing detailed findings in a future scientific forum.”
Detailed OS results from EMBARK will be presented at a future medical meeting.
About EMBARK
4
The Phase 3, randomized, double-blind, placebo-controlled, multi-national trial enrolled 1,068 patients with non-metastatic hormone-sensitive prostate cancer (nmHSPC; also known as non-metastatic castration-sensitive prostate cancer or nmCSPC) with high-risk biochemical recurrence (BCR) at sites in the United States, Canada, Europe, South America, and the Asia-Pacific region. Patients who were considered high-risk BCR had a prostate-specific antigen (PSA) doubling time ≤ 9 months, serum testosterone ≥ 150 ng/dL (5.2 nmol/L), and screening PSA by the central laboratory ≥ 1 ng/mL if they had a radical prostatectomy (with or without radiotherapy) as primary treatment for prostate cancer or at least 2 ng/mL above the nadir if they had radiotherapy only as primary treatment for prostate cancer. Patients in the EMBARK trial were randomized to receive enzalutamide 160 mg daily plus leuprolide, enzalutamide 160 mg as monotherapy, or placebo plus leuprolide.
The primary results from the EMBARK trial were published in
The New England Journal of Medicine
in 2023. The primary endpoint of the trial was metastasis-free survival (MFS) for enzalutamide plus leuprolide versus placebo plus leuprolide. MFS is defined as the duration of time in months between randomization and the earliest objective evidence of radiographic progression by central imaging or death.
For more information on the EMBARK (
NCT02319837
) trial go to
www.clinicaltrials.gov
.
About Non-Metastatic Hormone-Sensitive Prostate Cancer with High-Risk Biochemical Recurrence
Non-metastatic hormone- (or castration-) sensitive prostate cancer (nmHSPC or nmCSPC) means there is no detectable evidence of the cancer spreading to distant parts of the body (metastases) with conventional radiological methods (CT/MRI) and the cancer still responds to medical or surgical treatment to lower testosterone levels.
6,7
Of men who have undergone definitive prostate cancer treatment, including radical prostatectomy, radiotherapy, or both, an estimated 20-40% will experience a biochemical recurrence (BCR) within 10 years.
8
About 9 out of 10 men with high-risk BCR will develop metastatic disease, and 1 in 3 will die as a result of the recurrence.
8
The EMBARK trial focused on men with high-risk BCR. Per the EMBARK protocol, patients with nmHSPC with high-risk BCR are those initially treated by radical prostatectomy or radiotherapy, or both, with a PSA doubling time ≤ 9 months. Patients with nmCSPC who experience BCR after local therapy may be at a higher risk of metastases and death if their PSA doubling time is ≤ 9 months.
9
About XTANDI
®
(enzalutamide)
XTANDI (enzalutamide) is an androgen receptor signaling inhibitor. XTANDI is a standard of care and has received regulatory approvals in one or more countries around the world for use in men with metastatic hormone-sensitive prostate cancer (mHSPC), metastatic castration-resistant prostate cancer (mCRPC), non-metastatic castration-resistant prostate cancer (nmCRPC) and non-metastatic hormone-sensitive prostate cancer (nmHSPC) with high-risk biochemical recurrence (BCR). XTANDI is currently approved for one or more of these indications in more than 80 countries, including in the United States, European Union and Japan. Over 1.5 million patients have been treated with XTANDI globally.
5
About XTANDI (enzalutamide) and U.S. Important Safety Information
XTANDI (enzalutamide) is indicated for the treatment of patients with:
Please see
Full Prescribing Information
for additional safety information.
About Astellas
Astellas Pharma Inc. is a pharmaceutical company conducting business in more than 70 countries around the world. We are promoting the Focus Area Approach that is designed to identify opportunities for the continuous creation of new drugs to address diseases with high unmet medical needs by focusing on Biology and Modality. Furthermore, we are also looking beyond our foundational Rx focus to create Rx+
®
healthcare solutions that combine our expertise and knowledge with cutting-edge technology in different fields of external partners. Through these efforts, Astellas stands at the forefront of healthcare change to turn innovative science into VALUE for patients. For more information, please visit our website at
https://www.astellas.com/en
.
About Pfizer Oncology
At Pfizer Oncology, we are at the forefront of a new era in cancer care. Our industry-leading portfolio and extensive pipeline includes three core mechanisms of action to attack cancer from multiple angles, including small molecules, antibody-drug conjugates (ADCs), and bispecific antibodies, including other immune-oncology biologics. We are focused on delivering transformative therapies in some of the world’s most common cancers, including breast cancer, genitourinary cancer, hematology-oncology, and thoracic cancers, which includes lung cancer. Driven by science, we are committed to accelerating breakthroughs to help people with cancer live better and longer lives.
About the Pfizer/Astellas Collaboration
In October 2009, Medivation, Inc., which is now part of Pfizer (NYSE: PFE), and Astellas (TSE: 4503) entered into a global agreement to jointly develop and commercialize XTANDI (enzalutamide). The companies jointly commercialize XTANDI in the United States, and Astellas has responsibility for manufacturing and all additional regulatory filings globally, as well as commercializing XTANDI outside the United States.
SOURCE:
Pfizer
临床结果临床3期引进/卖出上市批准
100 项与 Sanford Burnham Prebys Medical Discovery Institute 相关的药物交易
登录后查看更多信息
100 项与 Sanford Burnham Prebys Medical Discovery Institute 相关的转化医学
登录后查看更多信息
组织架构
使用我们的机构树数据加速您的研究。
登录
或

管线布局
2025年11月01日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
8
19
临床前
临床1期
1
1
临床2期
其他
43
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
K562/GM-CSF vaccine(The Johns Hopkins University) ( CSF-3R ) | 费城染色体阳性慢性粒细胞白血病 更多 | 临床2期 |
[18F]DCFPyL ( PSMA ) | 肾细胞癌 更多 | 临床1期 |
OT-717 ( caspase 9 ) | 视网膜静脉阻塞 更多 | 临床前 |
T-005 | 感染 更多 | 临床前 |
T-007 | 感染 更多 | 临床前 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

转化医学
使用我们的转化医学数据加速您的研究。
登录
或

营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或

科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或

融资
发掘融资趋势以验证和推进您的投资机会。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用




