预约演示
更新于:2025-01-23
南方医院
更新于:2025-01-23
概览
标签
免疫系统疾病
神经系统疾病
血液及淋巴系统疾病
小分子化药
CAR-T
关联
3
项与 南方医院 相关的药物靶点- |
作用机制- |
在研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 CGAS抑制剂 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
572
项与 南方医院 相关的临床试验NCT05414383
A Prospective Study to Evaluate the Diagnostic Accuracy of Computer-aided Diagnosis (CADx) System in Real-time Characterization of Colorectal Neoplasia
The investigators hypothesize that a newly developed CADx system will have a higher diagnostic accuracy in predicting histopathology of colorectal neoplasia than both expert and junior endoscopists.
开始日期2024-12-01 |
申办/合作机构  香港中文大学 香港中文大学 [+2] |
NCT06673459
Busulfan Plus Cyclophosphamide Vs. Total Body Irradiation Plus Cyclophosphamide for Allogeneic Hematopoietic Stem Cell Transplantation in Patients with Acute T Lymphoblastic Leukemia: a Randomized Controlled, Open-label, Multi-center Clinical Trial
T-cell acute lymphoblastic leukemia (T-ALL), a hematological malignant neoplasm of immature T cells, accounting for a morbidity of 10-15% among pediatric and 20-25% among adult patients of ALL. Despite the application of improved intensive therapies, the overall survival (OS) of T-ALL patients is still unsatisfactory, with a 5-year OS rate of less than 60% in adults and 85% in children. Over the past few decades, allogeneic hematopoietic stem-cell transplantation (allo-HSCT) has emerged as a potential and the most likely curative treatment for patients with high-risk hematological malignant neoplasms, and it has been proven that allo-HSCT could hold the potential to improve the prognosis of T-ALL patients and may even cure T-ALL.
The two most common myeloablative conditioning regimens for T-ALL patients with allo-HSCT were total body irradiation (TBI) plus cyclophosphamide (TBI-Cy) and busulfan (Bu) plus cyclophosphamide (BuCy). The most common use conditioning regimen for ALL patients is the TBI-Cy conditioning regimen over other hematological malignancy patients because TBI possess potent and distinct anti-leukemic effects, particularly in organs not easily affected by systemic chemotherapy and intense immunosuppressive effects. However, TBI-based conditioning regimens may cause a high risk of cataracts, interstitial pneumonitis (IP), engraftment failure and even subsequent malignant neoplasms (SMNs). To avoid these disadvantages, intravenous Bu replaced TBI as a part of conditioning.
Extensive studies have shown that allo-HSCT with conditioning regimens based on TBI could benefit survival compared with conditioning regimens based on chemotheraphy in treating ALL. We retrospectively analyzed post-10-year data from T-ALL patients from two transplant centers, and all the databases were used to eliminate confounding factors via PSM. We demonstrated that the TBI-Cy conditioning regimen had inferior efficacy to the BuCy conditioning regimen, especially for T-ALL patients who were children, refractory, had extramedullary disease before transplantation, had active disease or an MRD-positive status at allo-HSCT, or who received haplo-HSCT.
The two most common myeloablative conditioning regimens for T-ALL patients with allo-HSCT were total body irradiation (TBI) plus cyclophosphamide (TBI-Cy) and busulfan (Bu) plus cyclophosphamide (BuCy). The most common use conditioning regimen for ALL patients is the TBI-Cy conditioning regimen over other hematological malignancy patients because TBI possess potent and distinct anti-leukemic effects, particularly in organs not easily affected by systemic chemotherapy and intense immunosuppressive effects. However, TBI-based conditioning regimens may cause a high risk of cataracts, interstitial pneumonitis (IP), engraftment failure and even subsequent malignant neoplasms (SMNs). To avoid these disadvantages, intravenous Bu replaced TBI as a part of conditioning.
Extensive studies have shown that allo-HSCT with conditioning regimens based on TBI could benefit survival compared with conditioning regimens based on chemotheraphy in treating ALL. We retrospectively analyzed post-10-year data from T-ALL patients from two transplant centers, and all the databases were used to eliminate confounding factors via PSM. We demonstrated that the TBI-Cy conditioning regimen had inferior efficacy to the BuCy conditioning regimen, especially for T-ALL patients who were children, refractory, had extramedullary disease before transplantation, had active disease or an MRD-positive status at allo-HSCT, or who received haplo-HSCT.
开始日期2024-12-01 |
申办/合作机构  苏州大学附属第一医院 苏州大学附属第一医院 [+7] |
ITMCTR2024000633
Comparative study on clinical efficacy and safety of traditional decoction and formula granules of Buyang Huanwu decoction in the treatment of acute myocardial infarction with Qi deficiency and blood stasis syndrome after PCI
开始日期2024-11-15 |
申办/合作机构 |
100 项与 南方医院 相关的临床结果
登录后查看更多信息
0 项与 南方医院 相关的专利(医药)
登录后查看更多信息
1,294
项与 南方医院 相关的文献(医药)2024-12-31·Journal of Bone and Mineral Research
β-Hydroxybutyrate ameliorates osteoarthritis through activation of the ERBB3 signaling pathway in mice
Article
作者: Zhang, Kang ; Song, Qiancheng ; Cai, Zhiqing ; Bai, Xiaochun ; Deng, Yinghu ; Zhang, Zhimin ; Lai, Pinglin ; Zhang, Jingyi ; Xie, Mengyun ; Hu, Hongling ; Leng, Jiarong ; Zhang, Haiyan
2024-11-12·Circulation
Abstract 4142370: KDM2B Antagonizes Trimethylamine N-Oxide-Induced Calcific Aortic Valve Disease by Suppressing Nox4 via JunD Demethylation
作者: Xu, Dingli ; Zeng, Qingchun ; Li, Shunyi ; Duan, Xiaolin ; Xian, Gaopeng ; Li, Jiaying ; Lin, Ying-wen ; Xu, minhui
2024-11-12·Circulation
Abstract 4143725: Down-regulation Of Cardiomyocyte Isocitrate Dehydrogenase 2 Mediates Metabolic Reprogramming, Contributing To Heart Failure By Remodeling The Lactate Microenvironment.
作者: Duan, Xiaolin ; Liu, Pei ; Lin, Ying-wen ; Lin, Xiangjie ; Zhong, Guoheng ; Li, Juncong ; Wen, Liming ; Hu, Dongtu ; Zhang, hao ; Zeng, Qingchun ; Li, Shunyi
37
项与 南方医院 相关的新闻(医药)2024-12-23
12月21日,以“医企创新 数领未来”为主题的2024中国医药创新大会在深圳龙岗隆重举办!本次大会由中国医师协会指导,《中国医学人文》杂志社主办,深圳湾宝龙生物创新投资发展有限公司联合深圳市生物医药产业联盟、深圳国家高技术产业创新中心、市区医疗体系、行业组织、药械企业等共同举办。
本次大会旨在推进医药领域科技创新,实现“医智融合、医工结合”创新发展新模式、新范式的重要活动之一,美国医学与生物工程院院士、广东龙城医疗集团总院长蔡志明、中华出版促进会副会长陈垠做开幕式致辞,监管领导、行业专家、产业主管领导、全国头部PI以及药械企业、医院、高校、投资机构代表近500人出席大会。
致辞环节
活动现场30多家领军企业、新锐公司、上下游服务公司发布新技术、新场景、新应用及合作需求,50+全国知名PI发布最新临床需求,医院与企业将共同凝练科学问题,共同挖掘更多临床研究合作机遇,实现更合规、更高效的实施路径。
医药创新成果展
本次大会包含1个主论坛,4个专业分论坛,医药创新生态展及宝龙生物药创新发展先导区(以下简称“宝龙先导区”)现场参观,4个专业分论坛分别由深圳大学华南附属医院、深圳市龙岗中心医院、深圳市龙岗区第三人民医院、深圳市整形美容行业协会承办,内容涵盖人工智能、智慧医疗、精准治疗、未来医美等多个主题,汇聚来自全国各地200余位的主任医生参加,共同推动医企创新合作。
医学技术+人文关怀
建设健康中国
院企合作不仅体现在医学技术的发展合作,也体现在双方如何实现社会价值。2024年9月29日在国家卫生健康委员会办公厅联合多个部门印发的《医学人文关怀提升行动方案(2024-2027年)》中,明确提出要“深入推进健康中国建设,提升医学人文关怀”,本次大会由深圳市人民医院副院长杨超发布《医学人文质量控制标准》,该标准将医学人文精神这一“无形资产”具象化,倡导将人文服务理念融入诊疗全过程,提升医疗服务水平,推动人文医院的建设。
深圳市人民医院副院长 杨超
随后,中国医师协会报刊出版管理部主任王德发布了《医院人文指数发展报告》,通过量化指标的展示,指导医疗机构不仅要关注医疗技术的精湛,更要重视医疗服务中的人文关怀、患者体验及医患关系的和谐。
中国医师协会报刊出版管理部主任 王德
《深圳市生物医药产业白皮书
(2024年)》重磅发布,推动产业发展
会上,由深圳国家高技术产业创新中心(深圳发展改革研究院)生物所所长王春安重磅发布《深圳市生物医药产业发展白皮书(2024)》。白皮书编制团队由邓子新、李兰娟、陈有海院士等专家担任顾问,陈艳萍担任主编,王春安担任副主编,危紫翼、王海旭、罗茜等担任编委。白皮书编制内容分为产业定义特点、全球趋势展望、我国发展情况、深圳发展情况等六个章节。当前深圳生物医药产业处于国内第二梯队,规上医药制造业产值530亿元,规上企业131家,上市企业13家,在研药物92款,6家企业进入医药工业百强系列榜单。
深圳国家高技术产业创新中心
(深圳发展改革研究院)生物所所长 王春安
“AI+”医药创新引航
宝龙先导区助企发展新场景
深圳作为AI+的创新引领者和应用高地,在中国乃至全球的人工智能领域都占据着举足轻重的地位。龙岗区正在全力创建人工智能全域全时应用示范区,宝龙先导区获评深圳市“AI+”药械专业园区,现场由深圳市药械办副主任陈睿、龙岗区卫生健康局副局长李海涛、龙岗区科技创新局副局长崔殿鹏、深圳市产城融合促进会执行会长闫晋、深圳市大数据研究院万翔博士、深圳湾宝龙公司常务副总经理李建立、华为云深圳政企大企业业务部总监鲁祖训共同上台挂牌。
深圳市“AI+”药械专业园区挂牌仪式
宝龙先导区将继续聚焦生物技术与信息技术(BT+IT)融合创新,以创新转化为核心,携手亚辉龙、精锋医疗、深圳市线上工研院、钦源智能、科辉智药、无境创新、爱奥乐、瑞图生物、联池系统等一系列在细分应用领域内领先的AI+企业,共建“AI+”药械生态、AI+医疗、AI+药械服务平台,提供从药械研发、临床、生产、销售全过程、全领域数字智能化解决方案,是药械企业链接AI高效发展的首选载体。
“AI+”药械生态共建企业签约仪式
宝龙先导区预开园,
迎来首批企业入驻
好的园区不仅是一个载体,更是企业发展的长久伙伴,宝龙先导区作为深圳市重点打造的五大生物医药园区之一、首批四大“AI+”药械专业园区之一,也是生物医药产业的关键支撑平台和发展沃土。现场举行了预开园仪式,迎来了腾云医学、健新医疗、德益达美、洁菲灭菌、德森特、中科正德、诺诚海洋生物、医友天下、德尼生物、南方昶晟等首批企业入驻签约,标志着这一优质载体,可以正式开始招商运营为产业发展赋能。大会当天下午,宝龙先导区组织了20余家企业参观园区现场,专业园区得到了参观企业的高度认可。
宝龙生物药创新发展先导区一期项目
入驻企业签约仪式
企业参观园区
加速科技成果转化
搭建科技创新生态
为了更好的服务企业,加速推动深圳生物医药科技成果向实际应用转化,促进产业创新发展,会上,宝龙先导区联合龙岗区卫生健康局、龙岗区科技创新局、深圳市龙岗中心医院、石药集团、亚辉龙、蒲公英共同开启“生物医药创新成果转化中心”的启动仪式。这一转化中心致力于打造集科研、孵化、产业化于一体的综合性服务平台,作为连接科研机构、医疗机构与企业的桥梁,推动生物医药科技成果的产业化进程。
生物医药创新成果转化中心启动仪式
前沿趋势策略分析,
为产业发展提供新思路
如何加速医企合作,加快产品落地,大会邀请了蔡志明院士、原国家食品药品监督管理局药品安全监管司李国庆司长、西安交通大学医学部主任、第一附属医院院长吕毅、石药集团董事、执行总裁王振国分别围绕药物的研发逻辑与策略、健康产业发展新路径、医工交叉产教融合模式创新与实践、新药研发风险管控等进行主题演讲,为医企合作注入更多的智慧。为了让更多优质企业了解龙岗,为与会企业发展提供新的思路和选择,龙岗区科技创新局副局长崔殿鹏为大家介绍了《深圳市龙岗区生物医药营商环境及医疗资源》。
政产学研医融合发展观点碰撞
主论坛最后,由中华出版促进会副会长陈垠主持,与“政产学研医”代表:深圳市医药和医疗器械产业办公室副主任陈睿、业务一组组长袁帅,龙岗区卫生健康局副局长李海涛,深圳市龙岗中心医院院长于建渤,石药集团董事、执行总裁王振国,亚辉龙董事长胡鹍辉,江苏春帆生物总经理李天宇共同围绕医企合作与全链条创新发展,探讨如何打破传统医药行业的界限,促进产学研医全链条合作,整合医药、生物技术、信息技术、大数据等多领域的资源和优势,加速新药研发、医疗器械创新以及医疗服务模式的变革,给现场观众带来了精彩的观点分享。
圆桌对话
专业论坛精彩纷呈、百花齐放
◆专业论坛一:多成果发布,彰显医工融合新成效
12月21日下午,在深圳市龙岗中心医院主办的“精准诊疗医工融合前沿论坛”上,龙岗中心医院与浙江大学智慧医疗研究中心举行了“AI联合实验室”的签约及揭牌仪式。同时,16家医工合作企业、4项医工合作转化成果也顺利合作签约。更令人振奋的是,龙岗中心医院与企业合作研发的广东省第二类创新医疗器械成功上市。此次论坛不仅展示了龙岗中心医院在医工融合领域的丰硕成果,更为龙岗医疗产业创新发展开辟了新路径,彰显医院在推动医疗科技进步中的引领作用。未来,龙岗中心医院将继续深化医工合作,为人民群众提供更加精准、高效的医疗服务。
◆专业论坛二:智慧医疗与主动健康,带动产业转型升级
12月21日下午,由深圳大学附属华南医院承办的“智慧医疗与主动健康论坛”上,深圳大学附属华南医院智能医学机器人研究所团队发布了一项医学人工智能理论——医学人工智能松散具身理论(SongFlex-Embodied Theory)。同时,深圳大学附属华南医院吴松院长与深圳市海和科技股份有限公司代表曹鹏云董事长签署了战略合作协议,双方约定将携手共建“松散具身理论机器人应用实验室联合研发中心”,共同促进基于医学人工智能和大模型的具身智能应用平台建设。来自清华大学、浙大邵逸夫医院、中科院深圳先进院、兰州大学二院、江苏省人民医院、深大华南医院、华为云等特邀与会专家围绕智慧医疗创新发展,基于各方在智慧医疗实践和创新药械研究过程中积累的经验方法,共同探讨如何解决和攻克其发展面临的挑战和难题,与会专家群策群力,共谋医智、医工融合创新转化和发展新路径。
◆专业论坛三:多领域探索,医学影像AI+应用新场景
12月21日上午,由深圳市医院协会、龙岗区第三人民医院主办的“医学影像人工智能论坛”,汇聚首都医科大学、中山大学、中国科学院深圳先进技术研究院、中山大学附属第八医院、上海联影智能等等名校专家及医疗器械、科技公司等机构的医学影像AI+实践者。聚焦医学影像人工智能技术在医疗实践中的应用案例和经验、高端医疗设备国产化建设思路、医学影像人工智能技术的挑战、机遇和发展方向进行深入探讨,共同推动医学影像更多智能化应用场景的发现与发展。
◆专业论坛四:多维度融合,探索未来美学发展新轨迹
12月22日下午,由深圳市整形美容行业协会主办,艾尔建美学(艾伯维旗下公司)承办的“未来医美创新论坛”,汇聚辽宁省人民医院、武汉大学人民医院、北京大学深圳医院、南方医院、深圳非凡医疗美容医院、爱思特医疗美容集团等医疗机构专家主任,聚焦光影美学、光电仪器、再生材料等创新产品与技术在临床中的应用实践,共同探索企业与医院跨越合作的新路径,提升技术研发、产品创新及市场应用等方面的紧密合作,共同推动深圳医美行业向更高水平发展,打造全国领先、全球知名的“世界医美之都”。
关于湾区共创荟
共创荟作为蒲公英在大湾区助力生物医药行业全产业链发展的平台,实行会员制度,为会员单位提供区域商务窗口与共享空间,通过整合资源、互通项目、链接人脉,助力拓展区域项目业务。
蒲公英作为中国医药行业极具影响力的媒体,旗下微信公众号关注用户突破100万+,专业媒体矩阵日均阅读量超8万+。
蒲公英创投(OurVentures)是蒲公英旗下投资板块,专注生物医药领域早期投资,与数十家知名机构共同建立蒲公英创投生态圈,为创业企业加速赋能。
药搭QMS信息系统是国内第一家制药人研发的GMP软件,唯一一家内嵌2200+专业培训课程的软件系统,由蒲公英团队自主研发。目前全国已超过30家知名药企上线系统,并通过了药监局“无纸化”迎检。
市场合作:
Michelle 19928711912
投融资、孵化合作:
于总监 17614409884
信息化管理软件:
刘经理 17154825444
2024-12-19
中国创新药研发在过去十年取得长足进步,不论是申报临床试验数量还与获批上市的药品数量,都在快速提升。
截至2024年8月,中国新药批准上市数量持续增长,位列全球第二,仅次于美国。在研新药管线数量也达到了全球占比超过三分之一,这表明中国在新药研发方面的强劲势头。
然,创新药获批之路并非坦途,一方面,我国医药创新领域同质化竞争显著,导致研发资源浪费,商业化竞争加剧,回报难以支撑后续研发;另一方面,临床试验作为新药研发的必经之路,涉及数据收集、中心筛选、试验启动、患者招募、检查、临床数据报告递交及存档等多个环节,这些环节之间需要高度协同,且每个环节都面临严格的监管要求。
在全球医药创新浪潮澎湃、科技竞争白热化的时代背景下,中国医药产业临床试验机构作为创新驱动的关键引擎,正经历深刻变革,尤其是在如何通过新质生产力赋能于提升临床试验质量管理、以及人才的培养培育等方面砥砺前行、多点突破,重塑产业发展新格局。在日前召开的“‘新’ 质驱动,构建临研新势力——ClinChoice昆翎中青年论坛”期间,E药经理人与十余位来自全国各大知名医院临床试验机构的负责人、中青年专家,探讨临床试验领域的新趋势、新挑战与新机遇。
01
促创新成果转化
新质生产力给生物医药产业带来了新一轮变革:面对大环境、监管、市场的多重压力,产业各方都需要“进化式创新”,来重新定义更有价值的产品、服务、运营与价值链生态。
站在行业洞察的角度来看,波士顿咨询董事总经理、全球合伙人胡奇聪直言,中国生物医药产业的创新转型之路政策驱动显著,多技术领域成果丰硕、出海license-out 成大势。然,挑战并存,扎堆的成熟靶点,导致管线重复严重、商业化价值降低;创新药占国内市场仅10%左右,前沿技术布局滞后。
但胡奇聪也认为,机遇亦显。基础科研与转化医学进展斐然,近年来,我国医疗机构、临床试验研究机构的自主研究能力取得长足进步,研究效率不断提升,本土创新乃至“全球创新”不断涌现,中国临床试验成果的国际认可度越来越高,凝聚着中国研究者智慧的研究成果,越来越频繁地登上国际舞台。
新质生产力拓展中,医工企协同成关键引擎。北京积水潭医院临床试验机构办主任、I 期临床试验研究室负责人王美霞对此深有感触。她告诉E药经理人,北京积水潭医院智能骨科机器人创新成果斐然,天玑机器人通用多能、远程协同高效;医院充分发挥临床资源的溢出效应,通过丰富的临床资源和优质的专家资源“以床引企”,引进在智能骨科手术机器人研发领域顶尖的创新企业在北京落户,医院与企业优势互补,在柔性臂手术机器人、康复机器人等领域管线丰富、创新迭出。技术融合赋能临床转化,大数据与 AI 辅助诊断、手术规划、加速康复、优化诊疗流程、提效手术精准度。医院也在创新闯关转化方面持续挖潜,整合前沿技术、临床洞察与企业创新活力,借创新生态迭代升级催生新质生产力,引领骨科诊疗智能化变革、重塑医疗服务范式,提升医疗科技核心竞争力与行业辐射影响力,为患者福祉注入创新动能。
满足临床未解决的需求是成果转化的核心。浙江大学医学院附属第一医院血液科主任佟红艳直言,科研能力不应以发表学术报告或论文为终点,要转换成真正有临床价值的产品,才是终点。佟红艳认为,临床试验不仅仅是研发新药,还是探索多种治疗药物联合使用的优化。以浙江大学医学院附属第一医院血液科为例,在这方面探索了很多现有临床药物组合,对于治疗疾病都有很好的提升效果。这些成果在国际学术大会上都做了展示,亮出了中国品牌。
以新质生产力为创新引擎,华西医院也在“多点开花”。四川大学华西医院眼科主任张明表示,百卅华西医院的全链条转化平台、国重实验室、技术转移中心等协同联动,从基础研究到产业转化无缝对接。学科交叉融合赋能,多病种研究汇聚多学科智慧,精准诊疗创新、成果转化提速,借创新生态协同、前沿技术融合催生新质生产力,驱动临床研究高质量跨越、拓展医疗创新前沿边界,提升医院国际影响力与区域辐射带动力。
在这方面,江苏省人民医院的“新质生产力培育路径”也相对清晰,江苏省人民医院肿瘤科副主任医师梁艳介绍道,江苏省人民医院正在践行“新质生产力培育深植临床实践与创新协同”,肿瘤科、血液科、心血管内科、骨科、普外科等前沿探索成果丰硕,实体瘤、血液肿瘤精准诊疗突破,心血管器械药物创新迭代,驱动临床质效跃升。基础研究成果临床转化紧密衔接,创新技术、诊疗方案加速落地,借临床验证优化升级,催生新质生产力。青年人才创新思维活跃,于重点项目历练成长,融合前沿理念技术,为新质生产力注入创新动能,推动医院临床研究高质量发展、引领医疗创新前沿突破。
厦门大学附属第一医院药物临床试验机构办副主任罗茜表示,新质生产力培育要锚定本地的医药产业结构。以厦大一院的实践来看,契合厦门产业格局,医院牵手药企、诊断试剂企业,依临床洞察驱动仿制药BE与诊断试剂研发优化,实现产学研医深度融合,加速成果临床转化、反哺产业升级。以产业需求为导向、跨界合作为路径,激活创新要素融合聚变,催生新质生产力,提升医院区域创新辐射力、产业核心竞争力,拓展医疗创新服务边界与价值内涵。
在上海市胸科医院,临床研究从医院层面有了顶层设计。上海市胸科医院临床研究中心主任、机构办公室主任、呼吸内科主任医师储天晴表示,从企业发起的注册研究,到由医生发起的IIT研究,当前这两大类临床研究项目在该医院都在火热开展中。
上海市胸科医院肿瘤科主任李子明以“精准诊疗在肺癌中的进展与应用转化研究”为例,他表示,近年来肺癌领域的新药蓬勃发展,本土创新企业的涌现,助推了在本地开展早期新药、新疗法的临床研究规模,尤其是在当前“无药可医”的部分晚期肺癌患者更多的机会,能在临床试验项目中遇到了有潜力的新药、新疗法。一方面得益于本土企业的创新势头,带来更多的新疗法,另一方面也得益于医院、学科日益完善的临床研究团队,目前胸科医院在研临床试验项目达到过去难以想象的数量。
不过,在南方医科大学南方医院国家药物临床试验机构办主任、中国药学会药物临床评价研究专委会主委、CCHRPP创建者许重远看来,产学研医协同链条还存在科技成果转化“最后一公里、乃至最后五百米”难以走通的梗阻。
好的一面是,在国家持续推动科技创新体制机制建设的部署下,科研机构与企业实现协同研发,孵化、转化了一批高质量发展企业。但不能忽视在高价值成果供给、专业服务体系搭建、科技激励政策创新及执行等层面,仍然存在卡点未清除、转化土壤不够肥沃等难点与痛点,从而导致生物医药领域的科创资源潜力得不到充分发挥、科创资源创新活力得不到有效激发。
许重远强调,当产学研用协同创新生态中,成果转化机制日臻完善,当转化环境持续优化,在政策引导、资源倾斜、人才汇聚等几方驱动下,才能更好地激发创新潜能,催生新质生产力,引领医疗创新前沿突破,提升医院核心竞争力与行业影响力。
目前,在以国家全面深化改革为核心的全面创新改革试验文件精神指导下,国内医药类高等院校、科研院所、新型研发机构等各类试点单位,仍然要探索解决科研人员“不想转”“不敢转”的问题。
作为生物医药重要的创新源头之一,临床医生能够发现临床需求,但是在旧的职称审评、绩效考核等制度之下,研究者被迫更注重科技成果的产生而对成果的转移转化并未重视。因此,和海外地区很多先进医疗器械、新药的专利发明者大多为临床医生相比,国内临床研究成果转化之路任重道远。
02
临床试验管理提质增效
新质生产力该如何赋能临床试验机构提质增效?国内多家临床试验机构负责人都给出类似的解决方案:流程标准化的精耕细作、核查强化与风险预控,数字化、智能化转型成关键驱动力。
许重远结合南方医院在这方面的具体实践,向E药经理人介绍了临床试验机构质量管理进阶路径。他表示,南方医院正从多维度深耕临床试验质量管理。机构高度重视GCP及IIT研究,构建了数据集成平台革新管理。精准整合入组患者全量数据,借桌面系统实现项目级数据可视化,优化数据监测与分析流程,提升管理效能。积极拓展DCT应用,无缝集成院内外数据,肾病慢病管理项目成效初显,确保数据连贯性与完整性,强化远程受试者管理质量,以技术融合驱动质量管理数字化、智能化转型,提升临床试验质量管控精度与效率。
北京大学人民医院临床试验机构副主任医师牛素平则从临床试验机构质量管理精进策略方面,介绍了该院研究型病房在质量管理方面的严谨、高效。她表示,北京大学人民医院通过立足优势学科,构建一体化临床研究平台,提供 pre-IND至III期临床一站式服务,专业优势与服务协同提升质量。牛素平介绍道,在获创新药IND试点资质后高效运作,机构办速审缩时,保项目顺畅推进。从方案设计、受试者管理到数据统计全流程接轨国际,借信息化升级优化流程,实现化验单收费转账、数据电子化溯源、远程监察探索与 DCT 试点,全方位提升管理精度与效率,稳固质量管控体系。
在临床试验机构质量管理路径强化方面,湖南省肿瘤医院则紧扣创新与高质量核心,构建坚实质量管理架构。湖南省肿瘤医院国家药物临床试验机构办主任龚倩介绍道,从医院战略规划出发,协同学科、团队与平台建设,依循政策与行业趋势优化管理模式。于信息化建设发力,通过CTMS等系统为申办方打造项目全景视窗,贯通PI管理、CRC协调、数据溯源等模块,精准呈现进度与质量详情,以实时洞察驱策高效决策,化解成本管控难题,提升整体管理效能与质量透明度,确保临床试验稳健推进、品质卓越。
北京积水潭医院则建立了临床试验质量管理构建多元保障机制。医工企合作中,从智能骨科机器人研发至临床应用全程严格质控。王美霞表示,产品研发历经临床反复打磨、软硬件适配迭代优化;应用环节精准评估手术效果、降低医患风险;远程手术借助 5G +技术,形成一托多台手术同时开展,远程精准规划和手术指导的模式,保障指令传输稳定及时、术后效果良好。研究型病房建设依政策指引强化管理,研究立项、伦理审查、方案执行和质量管理协同发力,试点基于风险分层管理模式探索,动态评估,平衡创新的时效性与实施的合规规范性,提升质量管理效能与适应性,稳固临床试验品质基石。
四川大学华西医院临床试验中心王振磊副教授告诉E药经理人,华西医院是国内临床研究体量最大的医院,因此也催生出对临床研究的流程优化刚需。华西医院将智能化、数字化转型作为核心增质升效策略,借助人工智能等新技术、新方法重塑临床研究流程,并通过在国内率先构建创新医药临床研究人工智能大模型精准高效管理海量数据与复杂流程。通过临床研究的分级管理,为高质量创新项目提供全流程绿色通道服务,确保重点项目精准推进。此外,针对创新临床研究,华西医院还通过伦理与科学审查双轮驱动,为前沿创新研究筑牢安全防线、点亮科学灯塔,稳固质量管理核心优势,积极打造创新临床研究行业标杆。
山东省肿瘤医院在临床试验机构质量管理则围绕“速度与质量齐升”下功夫,山东省肿瘤医临床研究部副主任、GCP办公室主任李慧娟介绍,目前流程革新效果显著。具体来看,借CTMS系统实现立项线上审核,实现提效减负保质量;伦理审核分层优化,组长单位前置会审,分中心快审协同合同审核签署,依政策缩时保质;入组环节优势突显,临床研究纳入内科医生岗位聘任、工作考核指标,激励入组积极性,同时CTMS与HIS对接,精准匹配项目与患者,双向筛选加速入组,夯实研究根基,全方位提升临床试验效率与质量管控精度。
03
梯队建设激发新活力
人才是高质量发展的重要引擎。只有高度重视青年人才梯队建设,多维举措协同发力,才能更好地激发创新活力。
在人才培养体系创新架构方面,许重远认为,人才培育战略要多元协同。包括为临床5+3专硕定制临床研究课程,为药学专硕开设GCP课程,为行业举办“临研骨干研修班”等,理论要与实践技能,夯实专业基础。在青年医师提升路径中,借青年科学家论坛、主题研讨及案例研习驱动知识体系更新。医教研协同发力,依岗位需求定制成长路径,塑造出临床研究多面手,为行业输出优质人才,强化人才梯队创新驱动力与实践执行力。
同济大学附属东方医院临床研究管理办公室副主任、GCP办公室主任施燕表示,东方医院自上而下都高度重视临床研究,医院将临床试验纳入绩效考核,并力求多学科发展,开展MDT多学科建设,基础研究和临床研究相接。另外,医院还建立了专家学科的人才培养梯队,把临床研究和临床试验紧密结合起来,与众多企业和研发机构进行沟通交流,帮助有科研意愿的医生护士对接合适的平台。
江苏省人民医院则设立院内青年基金,为创新萌芽供养分、激发探索热情。梁艳介绍,国自然基金专项辅导精准赋能,邀专家提升申报技巧、增强竞争力,中标率攀升助力学术成长。“高层次人才培育计划”创新激励,稀缺名额激发斗志、点燃科研激情,驱动青年勇攀科研高峰、加速专业精进,为临床研究注入持久创新活力、厚植人才成长沃土。
张明认为人才培育要传承与创新并举。当跨学科合作成为常态,多领域专家协同破题,催生前沿成果,培育复合型人才。他告诉E药经理人,目前华西医院全员GCP培训铸专业根基,医护技全员资质认证,提升临床试验实操水准。“以质选项目、以研促发展”的导向鲜明,PI进阶激励卓越担当,从项目锤炼中成长,以临床需求牵引科研,借多学科融合厚植创新土壤,激发人才创新潜能,构筑人才成长进阶的阶梯,强化临床试验人才梯队创新实力与专业深度。
此外,中青年人才的培养过程中,精准扶持、资源倾斜等方式是能力提升的重要催化剂。
王美霞表示,积水潭医院聚焦内在驱动激发,依兴趣专长定向扶持,借院内基金助青年创新破题,育研究热忱与专长深度。同时,正视人才专职困境,借政策东风疏晋升堵点,纳临床研究于绩效晋升,增加职业引力将临床试验成果纳医护技晋升指标,激励青年勇担重任。科研基金青年专项扩容、职称晋升绿色通道开辟,设立专属考核晋升的标尺,多措并举强化临床试验人才梯队核心竞争力与创新续航力。
“真金白银”支持很重要。上海市胸科医院临床研究中心主任、机构办公室主任、呼吸内科主任医师储天晴表示,尤其是在医生发起的IIT研究方面,上海市胸科医院还在今年12月推行了面向45岁以下青年医生的临床研究专项孵育计划,涉及包括给予真金白银的第一桶金的支持,同步给予统计辅导、数据质量管理、服务跟进等,还以“创新俱乐部”等形式对接律师、知识产权、产业园区资源等,希望助推更多医生主导的临床研究落地、转化。
龚倩透露,目前湖南省肿瘤医院的资深PI通过领衔青年团队,采取资深专家“导师制”传承赋能,从方案设计、项目实施至成果发表全程指导,助其积累经验、拓展人脉、塑造科研品格;实践历练平台多元拓展,机构鼓励青年主持 IIT 研究、参与申办方项目核心环节。
罗茜介绍道,推进青年国际合作交流、搭建医企共建平台,于实战锤炼中提升创新与管理能力,塑青年人才为行业创新先锋,激活人才梯队创新潜能。
临床医生是临床研究的主力军。
东方医院肿瘤科副主任医师李玮作为肿瘤科主任周彩存教授团队的核心成员,他表示,近年来,医院对于临床研究的扶持力度很大,他们团队主导和参与的临床研究数量也在不断增长,好的政策、环境和平台可以让医生心无旁骛地做好临床研究工作,用研究成功的优质成果来服务广大患者。
在人才培养机制建设方面,北京大学人民医院的人才培育机制完善且多元。北京大学人民医院皮肤科副主任医师赵琰介绍,自新员工入职开启全程规划,院内基金扶持、课题申报引导助力科研起步。科室梯队建设成熟,资深专家引领青年医生入临床研究正轨,言传身教纠错成长。GCP培训课程定期赋能,核查经验全院共享强化规范意识。医院依个体差异与科室需求定制路径,临床、科研、手术、思维全方位雕琢,激发潜能、选拔精英,为临床研究筑牢人才梯队,注入创新活力,驱动持续发展。
南方医科大学南方医院感染内科副主任医师梁携儿则结合自身经验,她表示,临床试验是人才培养的熔炉,深度锤炼研究者综合素养,涵盖研究设计、方案执行、数据解析、质量把控等能力矩阵。历经了锤炼、汲取了经验、拓展了视野,才能成长为兼具专业深度与国际广度的复合型人才,为临床研究注入持久创新活力,同时强化人才梯队核心竞争力。
一审| 黄佳
二审| 李芳晨
三审| 李静芝
引进/卖出上市批准临床1期
2024-12-16
·同写意
乙肝功能治愈新时代,浪潮澎湃。
强家(JNJ)与罗家(Roche)选择退场,冀家(GSK)有望拔得头筹,“中国国家队”强势崛起!临床研究堪称百技之首,更能一锤定音!团队聚是一团火,散是满天星!
华山张文宏教授和谢青教授在上海疫情封控期间被隔离,吃住在办公室,他们对临床研究的执着和强烈的使命感,使得试验没有因为疫情受影响。我耳旁始终有谢姐这朵铿锵玫瑰说的十二个字,“绝对支持,要人有人,要血有血!”
好友愈哥说,侯哥,你知道吗,无论药物研发是基于怎样的战略思考或者商业考虑,此时又是谁家独占鳌头,最重要的是在这过程中培养的复合型研究型医师人才和不断夯实的临床试验平台!这是生命方舟!这是传承给人类的真正的财富!唯有紧跟时代、创新突破,方能在竞争中屹立。
感恩强家、罗家、冀家对“乙肝功能治愈”概念验证征途中的前赴后继的人力、财力和物力的巨大投入,使得乙肝治愈走出关键一步。下一段,siRNA与免疫调节药物携手以及siRNA序贯ASO的终极对决即将登场,必将在乙肝功能治愈新时代绽放出绚烂夺目的光彩。
2023年6月 南方医院肝病中心治愈研究执行团队
在南方医院某新药研究第一针镜头
在医药研发领域这片广袤无垠又充满挑战的领域,我有幸结识了一位独具慧眼、言辞犀利的愈哥。他对数十年来乙肝药物的研发如数家珍,宛如一部鲜活的乙肝功能治愈研发的宝典。令人称奇的是,他对于其中的许多细节皆能娓娓道来,且点评鲜辣,剖析精准,直击要害,因此我总是与其聊得不舍昼夜。
提及中国临床科研团队于2024年12月5日在《新英格兰医学杂志》上发表的乙肝功能治愈新药平台概念验证文章,他赞不绝口,鼓励中国的药物研发团队,要继续“以终为始”,坚定不移地沿着《新英格兰医学杂志》这篇具有重大概念验证意义的“雄文”所开辟的乙肝治愈光明大道,奋勇前行。正所谓:“披荆斩棘五十载,科学研究改写人类命运”。
2017年2月12日 广州和上海临床研究团队
第一章 强家之无奈
强家(JNJ),曾是乙肝功能治愈管线开发的先锋劲旅,一度风光无限。其在乙肝核苷(酸)类似物如日中天之时,就在功能治愈的漫漫征途中提前布局,全力以赴,恰似一位无畏的开拓者,最终第一个完成二期概念验证研究。
然而,命运却在此处悄然转折,尽管二期结果令人鼓舞,但强家仿佛陷入了重重迷雾笼罩的深谷,在长达两年的时光里,举棋不定。
彼时,外部市场环境波谲云诡,内部决策的权衡也如不见硝烟的战场,错综复杂。而曾经意气风发、踌躇满志的强家,在这混沌不清的局势中逐渐丧失了往昔的锐气与锋芒。
最终,或是出于公司整体战略的角度,考虑到乙肝是亚洲病,又适逢siRNA管线中国研发强势推进,强家在承受巨大压力的同时又无信心在乙肝功能治愈的商战上独占鳌头,做出了令人瞠目结舌的壮士断腕之举——毅然决然地斩断全部感染管线,并将凝聚无数心血、寄予厚望的成果,如弃敝履般转让给冀家(GSK)。
早期抗感染的研发团队的精英们只能无奈地一一作别。在愈哥的眼中,强家此举无疑是头号“愚者”行径,将大好的发展契机拱手相让,徒留壮志未酬的悲怆叹息在医药江湖久久回荡。
第二章 冀家之奋进
冀家(GSK),在乙肝医药研发的历史长河中,犹如一颗恒定闪耀的星辰,有着执着探索的光辉。虽然三十年几经蹉跎,但其在感染和乙肝领域开拓的信念,始终坚如磐石。冀家是乙肝核苷类似物的开山鼻祖,因拉米夫定剂量选择的一时保守而成为二线药物,痛心不已,后相继成功落地两个口服抗病毒药物,阿德福韦酯和替诺福韦酯,引领乙肝治疗市场10余年,之后一批国产仿制药上市,加上集采政策,市场一度萎缩。
但冀家坚韧的品质,继续支撑着他家研发团队砥砺前行。经历了漫长的寒冬后,在小核酸药物崭露微弱曙光之际,拿出了手中的孪生双子剑ASO:836和404,并罕见的开展了堪称“七伤拳”的优化自我比拼。最终404被淘汰,但这也成就了836成为了小核酸治疗领域领域的美玉——BPV。
凭借着这份过人的胆色,冀家势如破竹地率先踏入全球三期乙肝功能治愈全球注册临床阶段。中国临床研究牵头中心南方医院入组病人一骑绝尘,高质量完成入组。而冀家未雨绸缪的战略布局远不止于此,在稍纵即逝的机遇闪现之际,凭借着敏锐的洞察力与果敢的决断力,在世人一片“千金买骨”的议论中,他将强家舍弃的siRNA归于账下,谋划着一套“刀劈剑刺”的绝妙攻势。
这一落子堪称精妙绝伦。在此过程中,冀家研发团队如同精密无误的钟表高速运转,继续全身心投入新的概念验证临床工作:每一次临床研究方案的精心设定,每一回临床试验的严谨开展,皆似激昂嘹亮的冲锋号角,向着乙肝病魔发起一轮又一轮的猛烈强攻。未来十年,冀家希望为全球乙肝患者功能治愈开启一扇充满希望的光明之门。
第三章 罗家之憾事
罗家在制药领域久负盛名,威名远扬,在乙肝治疗领域,其聚乙二醇化技术将人类的天然抗病毒武器——干扰素进行了跨跃式的升级。该药物(派罗欣)虽然受制于不良反应,但依赖其广谱、免疫激活作用,成为了乙肝治疗历史最为悠久的一线药物之一,战功赫赫。
然而,罗家似乎总是痴迷于“一剑封喉”,后续研发中忽略了对该药物的持续探索,甚至转卖、关停了该药物,甚至其威名也日渐式微,自此,罗家策略上的举棋不定,使其在乙肝功能治愈领域的研发一度沉沦。
历史,在冥冥中皆有预兆,既往在丙肝治疗领域,罗家就曾因摇摆,遗憾地错失过千载难逢的重大机遇——抗丙肝之王索非布韦。早在2004年,罗家就与法莫赛特合作研发靶向NS5B聚合酶的丙肝新药PSI-6130。由于该研发路径与罗家的方向背道而驰,且早期疗效因大量异构体的存在而未达预期,PSI-6130被罗家早早放弃。
与此相反,吉家则黄雀在后,认识到了PSI-6130的升级异构体——索非布韦的惊世价值:在错过以2亿美元收购的机会后,在一片质疑中以104亿美金将索非布韦收入囊中,后续以创新的区域性举措,横扫全球丙肝药物市场。最终,罗家只能无奈地眼睁睁看着吉家在丙肝领域登顶封禅,铸就辉煌,自己唯有悔恨叹息,空余遗憾。
如今,历史似乎有再度重演的迹象。在乙肝管线舞台上,罗家似乎要再行那“卖儿卖女”、“自断臂膀”之事,近日获悉,罗家要重蹈强家覆辙,将目前乙肝治愈管线的半壁江山(进度最快的siRNA,打包免疫调节药物TLR7激动剂,独特的肝脏靶向锁核酸PD-L1,以及还在一期研发未公布机制的神秘药物)打包送上货架,停止相关开发。对此,愈爷只能一再的摇头苦笑,深深闷了一口茶水。
2017年上海瞻仰中国乙肝临床研究鼻祖姚光弼教授雕像
第四章 国家之幸事
我爱我家,我爱临床研究,临床研究堪称百技之首!中国乙肝临床研究团队经历国家重大专项的洗礼,打造了世界级的乙肝临床研究的综合平台。乙肝是人类之殇,亚洲之殇,消除病毒性肝炎危害,摘掉乙肝大国的帽子是我辈义不容辞的义务!在过去数十年,由于各种原因,中国乙肝临床研究团队始终未能稳固地站在世界舞台中央。
每每谈论至此,愈哥总是忍不住义愤填膺,喝点小酒后更是热泪盈眶。而进入乙肝治愈时代中国临床研究成果如雨后春笋般群雄并起。特别是疫情期间,整个乙肝临床研究团队,不顾新冠疫情的纷扰,披荆斩棘,张文宏教授和谢青教授甚至在上海封城期间被隔离,吃住在办公室,日理万机,仍保持对临床治愈平台概念验证项目病人的密切追踪,我耳旁始终有谢姐这朵临床研究的铿锵玫瑰说的十二个字,“绝对支持,要人有人,要血有血”!
他们的奋斗必将是乙肝治愈征途上浓墨重彩的一笔。他们对发表在《新英格兰医学杂志》的具有重大概念验证意义的文章的贡献在于,第一次让世界认识到中国科研团队能肩负重大的责任,即使面对世界级新冠大流行的灾难时,也不忘驾稳这艘乙肝治愈的诺亚方舟。
风雨过去之际,中国的科研力量继续厚积薄发,成果在今年2024年11月美国肝病年会群星闪闪,向世人宣誓我们治愈乙肝的决心:处于研发关键阶段的乙肝新药层出不穷,浩博的ASO——AHB137,凭借其卓越显著的治疗效果引人瞩目,而星曜坤泽的小干扰RNA,也凭借其高效卓越的基因沉默能力及良好的安全性和特宝聚乙二醇干扰素新数据引发了热烈的研讨与深入的交流。
世家变迁,愈哥如数家珍,他感叹药物研发风险之高,参与其中则多多煎熬,但回首这风云变幻却可谓精彩绝伦。说罢,愈哥却话锋一转,目光一定,握拳铿锵有力的说到:“你知道吗,无论药物研发是基于怎样的商业考虑,此时又是谁家独占鳌头,最重要的是在这过程中成长的复合型研究型临床医师人才和不断夯实的临床试验平台!这是留给人类的真正的财富!”
是的,十年树木,百年树人,作为乙肝大国,我们在这数十年奋斗中,无论负责的是药物化学结构、生物机制靶点、统计分析、研究设计、项目管理、政策沟通,还是日常的患者管理,这些奋斗在每一岗位的工作人员,聚是一团火,散作满天星,将成为实现乙肝治愈的核心力量。
愈哥感叹,此次乙肝治愈的研究论文在顶级医学期刊登顶,更像一声集结号,是召唤更多的力量加入其中,是引导中国药物研发试验发起冲锋。聊罢,作为参与其中的人员,我也相信,实现乙肝治愈的时代已经来临,让我们共聚于此,共同见证科技人才造福人类命运共同体,实现乙肝治愈的一天。
同写意媒体矩阵,欢迎关注↓↓↓
核酸药物寡核苷酸
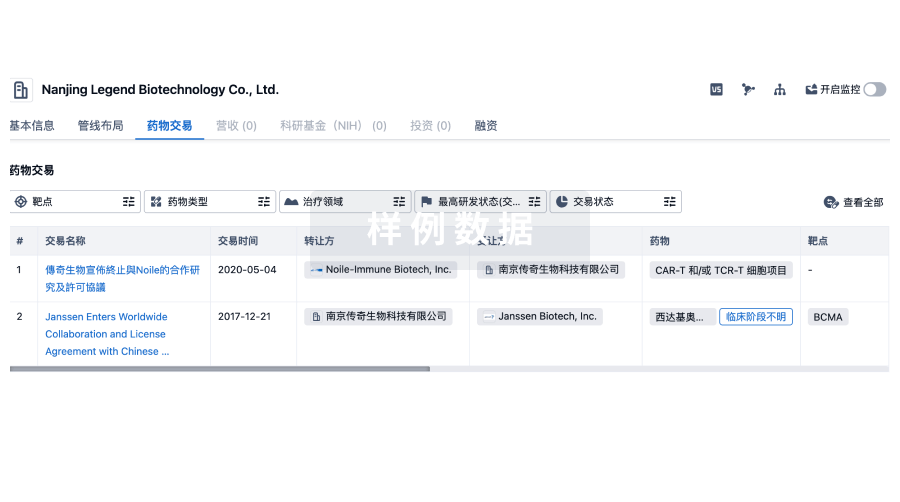
100 项与 南方医院 相关的药物交易
登录后查看更多信息
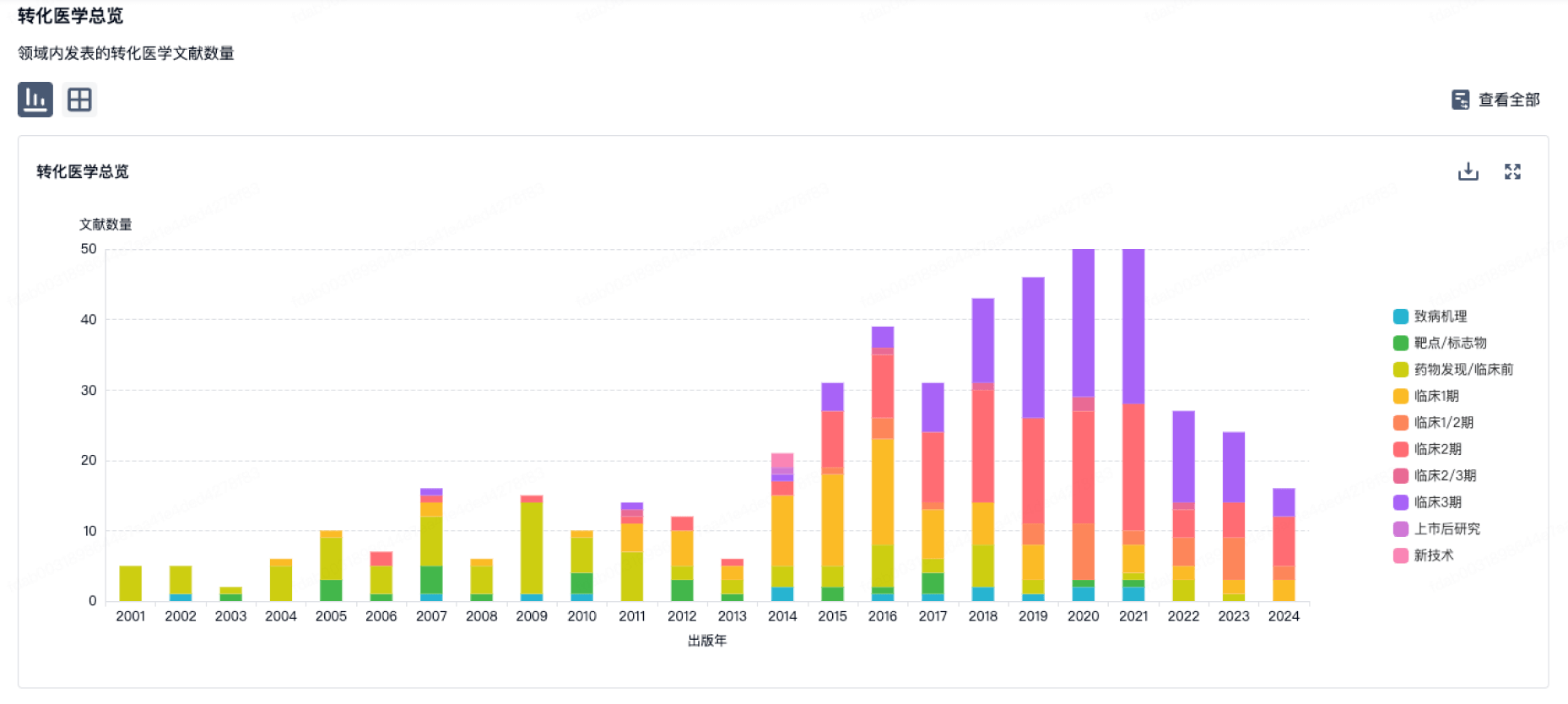
100 项与 南方医院 相关的转化医学
登录后查看更多信息
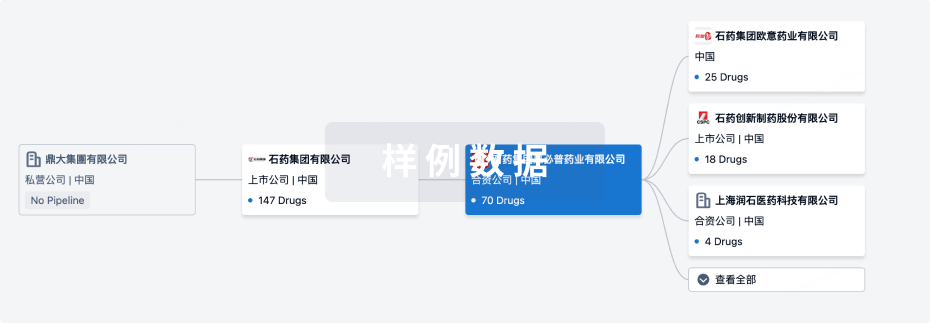
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年04月25日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
1
临床2期
其他
1
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
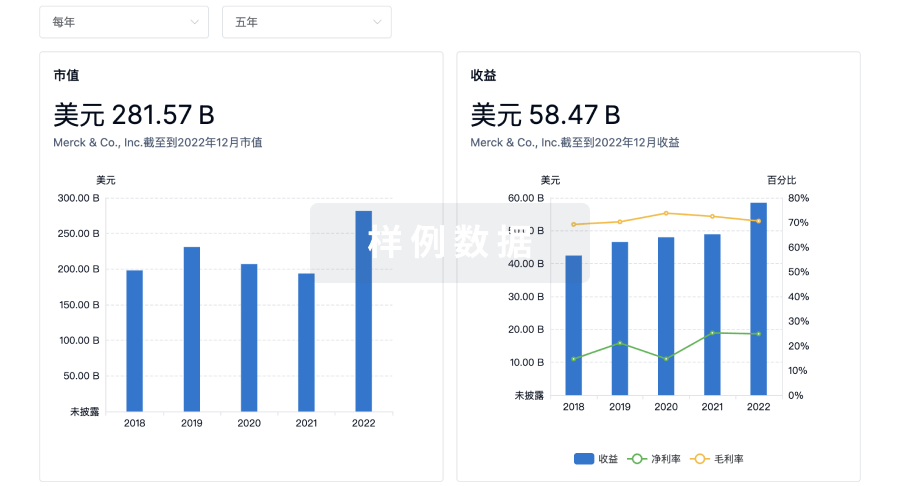
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
来和Eureka LS聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
