预约演示
更新于:2025-09-13

Intercept Pharmaceuticals, Inc.
更新于:2025-09-13
概览
标签
消化系统疾病
其他疾病
遗传病与畸形
小分子化药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 疾病领域 | 数量 |
|---|---|
| 内分泌与代谢疾病 | 2 |
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 6 |
| 排名前五的靶点 | 数量 |
|---|---|
| FXR(胆汁酸受体FXR) | 4 |
| FXR x PPARα | 1 |
| TGR5(G蛋白偶联胆汁酸受体1) | 1 |
关联
6
项与 Intercept Pharmaceuticals, Inc. 相关的药物靶点 |
作用机制 FXR激动剂 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2016-05-27 |
靶点 |
作用机制 FXR激动剂 [+1] |
在研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 日本 |
首次获批日期1983-05-27 |
作用机制 FXR激动剂 [+1] |
在研适应症 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
33
项与 Intercept Pharmaceuticals, Inc. 相关的临床试验CTIS2023-507771-22-01
A Phase 3, Open-Label, Long-Term Safety Extension Study Evaluating the Safety and Tolerability of the Fixed-Dose Combination of Obeticholic Acid and Bezafibrate in Subjects with Primary Biliary Cholangitis - 977-311
开始日期2025-04-09 |
NCT06121375
A Randomized, Double-blind, Placebo-controlled, Phase 2/3 Study to Assess the Efficacy, Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of Obeticholic Acid Compared to Placebo in Pediatric Subjects With Biliary Atresia, Post-hepatoportoenterostomy
This study will evaluate the efficacy, safety and tolerability, as well as PK/PD of OCA in eligible pediatric participants with biliary atresia with successful hepatoportoenterostomy (HPE, also known as a Kasai portoenterostomy). The double-blind period comprises of 2 phases: dose titration phase and age expansion treatment phase.
开始日期2024-09-02 |
NCT06488911
A Phase 3, Open-Label, Long-Term Safety Extension Study Evaluating the Safety and Tolerability of the Fixed-Dose Combination of Obeticholic Acid and Bezafibrate in Subjects With Primary Biliary Cholangitis
An Open Label Long-Term Study to Evaluate the Safety and Tolerability of the Fixed-Dose Combination (FDC) of Obeticholic Acid (OCA) and Bezafibrate (BZF) tablet in Subjects with Primary Biliary Cholangitis (PBC).
开始日期2024-07-01 |
100 项与 Intercept Pharmaceuticals, Inc. 相关的临床结果
登录后查看更多信息
0 项与 Intercept Pharmaceuticals, Inc. 相关的专利(医药)
登录后查看更多信息
107
项与 Intercept Pharmaceuticals, Inc. 相关的文献(医药)2025-08-01·AMERICAN JOURNAL OF PHYSIOLOGY-GASTROINTESTINAL AND LIVER PHYSIOLOGY
Farnesoid X receptor inhibits proinflammatory cytokine-induced epithelial necroptosis in vitro: implications for preservation of intestinal barrier function
Article
作者: Ní Chonghaile, Triona ; Adorini, Luciano ; Curley, Caitriona E. ; Keely, Stephen J. ; Lajczak-McGinley, Natalia K.
These studies demonstrate for the first time that FXR activation inhibits cytokine-induced necroptosis in vitro, an effect that may underlie protection against dysregulated barrier function in the setting of intestinal inflammation. These data support the potential for targeting FXR to promote epithelial barrier function in treatment of IBD.
2025-06-01·HEPATOLOGY
Hepatic real-world outcomes with obeticholic acid in primary biliary cholangitis (HEROES): A trial emulation study design
Article
作者: Mayne, Tracy J. ; Kareithi, Dorcas N. ; Smith, Rachel ; Kowdley, Kris V. ; Chu, Yucheng Julia ; Fried, Michael W. ; Breskin, Alexander ; Brookhart, M. Alan ; Ness, Erik ; Hiu, Shaun ; Jones, David ; Hansen, Bettina E. ; Li, Jing ; Seeger, John D. ; Bessonova, Leona ; Trivedi, Palak J. ; Mells, George ; Wason, James ; Coombs, Charles ; Hirschfield, Gideon M.
Background and Aims::
Primary biliary cholangitis is a rare, progressive liver disease. Obeticholic acid (OCA) received accelerated approval for treating patients with primary biliary cholangitis in whom ursodeoxycholic acid failed, based on a surrogate endpoint of reduction in ALP. Analysis of the long-term safety extension with 2 external control groups demonstrated a significant increase in event-free survival in OCA-treated patients. This fully real-world evidence study assessed the effect of OCA treatment on clinical outcomes.
Approach and Results::
This trial emulation used data from the Komodo Healthcare Map claims database linked to US national laboratory, transplant, and death databases. Patients with compensated primary biliary cholangitis and intolerance/inadequate response to ursodeoxycholic acid who initiated OCA therapy were compared with patients who were OCA-eligible but not OCA-treated. The primary endpoint was time to the first occurrence of death, liver transplant, or hospitalization for hepatic decompensation, analyzed using a propensity-score weighted Cox proportional hazards model. Baseline prognostic factors were balanced using standardized morbidity ratio weighting. For the primary analysis, 4174 patients contributed 11,246 control index dates, and 403 patients contributed OCA indexes. Weighted groups were well balanced. Median (95% CI) follow-up in the OCA and non-OCA arms was 9.3 (8.4–10.6) months and 17.5 (16.2–18.6) months (weighted population; censored at discontinuation). Eight events occurred in the OCA arm and 32 in the weighted control (HR = 0.37; 95% CI = 0.14–0.75; p < 0.001). Effects were consistent for each component of the composite endpoint.
Conclusions::
We identified a 63% reduced risk of hospitalization for hepatic decompensation, liver transplant, or death in OCA-treated versus non–OCA-treated individuals.
Trial Registration::
HEROES; ClinicalTrials.gov NCT05292872.
2025-05-01·CTS-Clinical and Translational Science
Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of INT ‐787, a Novel Farnesoid X Receptor Agonist, in Healthy Volunteers: A Phase 1 Trial
Article
作者: Van De Wetering, Jeroen ; Callahan, Jennifer ; Burkey, Jennifer ; Capozza, Thomas ; Erickson, Mary ; Kerb, Reinhold ; Kryzhanovskaya, Ludmila
ABSTRACT:
Aberrant farnesoid X receptor (FXR) signaling is implicated in cholestatic, inflammatory, and fibrotic liver diseases. In preclinical/clinical studies, semisynthetic bile acid‐derived FXR agonists markedly improved hepatic function in various conditions. INT‐787, a novel hydrophilic semisynthetic bile acid FXR agonist, has demonstrated a reduction in inflammatory and fibrotic markers and regulation of bile acid/lipid metabolism. This first‐in‐human, randomized, placebo‐controlled phase 1 study assessed the safety, tolerability, pharmacokinetics, and pharmacodynamics of INT‐787 and its equipotent metabolites in healthy volunteers by evaluating single ascending doses (SAD), multiple ascending doses (MAD), and food effect. Participants (n = 130) across all study portions were similar in age, race, and body mass index. In the SAD and MAD portions, the maximum plasma concentration (Cmax) and area under the curve (AUC) for total INT‐787 generally increased with dose. In the Food Effect portion, the mean Cmax of total INT‐787 was almost 2‐fold higher under fasted conditions compared with fed conditions; AUC0‐inf was unchanged. Steady state for total INT‐787 was reached by Day 7. In cohorts receiving ≥ 50 mg doses, the half‐life of total INT‐787 ranged from 21 to 55 h. INT‐787 metabolites exhibited increased concentrations after mealtimes despite morning dosing, consistent with endogenous bile acid behavior. Following single and multiple doses of INT‐787, decreases in C4 and increases in FGF‐19 levels were observed. Single and multiple oral doses were generally well tolerated; 4 adverse events of mild, transient pruritus not requiring interventions were reported at higher doses. These results warrant further investigation of INT‐787 in patients with liver‐related disorders.
449
项与 Intercept Pharmaceuticals, Inc. 相关的新闻(医药)2025-09-12
·氨基观察
氨基观察-创新药组原创出品
作者 | 黄恺
创新药改革继续深入。
9月12日,国家药监局发布实施《关于优化创新药临床试验审评审批有关事项的公告》(以下简称《公告》),贯彻落实《国务院办公厅关于全面深化药品医疗器械监管改革促进医药产业高质量发展的意见》,进一步优化创新药临床试验审评审批工作,在药物临床试验60日默示许可基础上增设创新药临床试验审评审批30日通道,以支持国家重点研发品种,鼓励全球早期同步研发和国际多中心临床试验。
奥贝胆酸在美国走到终点。
9月11日,Alfasigma全资子公司Intercept Pharmaceutical宣布决定自愿从美国市场撤出原发性胆汁性胆管炎(PBC)治疗药物Ocaliva(奥贝胆酸),这一决定是根据美国FDA的要求做出的。此外,FDA已要求暂停Intercept经美国IND批准开展的所有涉及奥贝胆酸的临床试验。
在过去的一天里,国内外医药市场还有哪些热点值得关注?让氨基君带你一探究竟。
/ 01 /
市场速递
1)创新药临床试验审评审批增设30日通道
9月12日,国家药监局发布实施《关于优化创新药临床试验审评审批有关事项的公告》(以下简称《公告》),创新药临床试验审评审批30日通道支持国家重点研发品种,鼓励全球早期同步研发和国际多中心临床试验,服务临床急需和国家医药产业发展。
根据《公告》,纳入30日通道的药物临床试验申请,应当为中药、化学药品、生物制品1类创新药临床试验,能够按要求提交申报资料,并需满足以下条件之一:(一)获国家全链条支持创新药发展政策体系支持的具有明显临床价值的重点创新药品种。(二)国家药监局药品审评中心公布的符合条件的儿童创新药、罕见病创新药,以及中药创新药品种。(三)全球同步研发品种。全球同步研发品种的Ⅰ期、Ⅱ期临床试验,我国药物临床试验机构的主要研究者牵头或共同牵头开展的Ⅲ期国际多中心临床试验。
/ 02 /
医药动态
1)亦诺微医药T3011疱疹病毒注射液获临床许可
9月12日,据CDE官网,亦诺微医药T3011疱疹病毒注射液获临床许可,拟开展治疗卡介苗无反应的高危非肌层浸润性膀胱癌的研究。
2)椎元医学异体人成纤维细胞注射液获临床许可
9月12日,据CDE官网,椎元医学异体人成纤维细胞注射液获临床许可,拟开展治疗中重度腰椎间盘退行性病变的研究。
3)艾立康ALK2401片获临床许可
9月12日,据CDE官网,艾立康ALK2401片获临床许可,拟开展治疗周围神经病理性疼痛的研究。
/ 03 /
海外药闻
1)阿斯利康司美替尼获批扩人群,覆盖1岁及以上患儿
9月10日,FDA官网显示,阿斯利康的司美替尼口服颗粒剂获批上市,可用于1岁及以上有症状且无法手术的1型神经纤维瘤病(NF1)相关丛状神经纤维瘤(PN)儿科患者。并且,此前已经获批的口服胶囊剂的适用人群也从2岁及以上儿科患者同步扩大至1岁及以上儿科患者。
2)奥贝胆酸将在美国撤市
9月11日,Alfasigma全资子公司Intercept Pharmaceutical宣布决定自愿从美国市场撤出原发性胆汁性胆管炎(PBC)治疗药物Ocaliva(奥贝胆酸),这一决定是根据美国FDA的要求做出的。此外,FDA已要求暂停Intercept经美国IND批准开展的所有涉及奥贝胆酸的临床试验。
PS:欢迎扫描下方二维码,添加氨基君微信号交流。
临床申请申请上市
2025-09-12
Bengaluru:
Intercept Pharmaceuticals
said on Thursday it is withdrawing its
liver disease drug
from the U.S. market following a request from the Food and Drug Administration.
This comes as another setback for the company after the U.S.
FDA
last year declined full approval for the drug,
Ocaliva
, and said it had identified cases of liver injury in patients who were on it.
Ocaliva, chemically known as
obeticholic acid
, got the FDA's accelerated approval in 2016 to treat patients with primary biliary cholangitis, a rare disease that causes inflammation of small bile ducts in the liver and can eventually destroy them.
Under the accelerated pathway, the FDA mandates additional post-market trials that verify the drug's benefits. If data from the trials do not show the drug's effectiveness, the regulator can ask the company to withdraw it from the market.
The FDA had said in December the drug was being studied for any injury to the organ in patients without severe scarring, based on its review of post-market clinical trial data.
In 2021, the regulator had restricted the use of Ocaliva in patients with advanced cirrhosis or scarring of the liver.
The FDA has also placed a clinical hold on all Intercept clinical trials conducted in the U.S. involving obeticholic acid, the company said on Thursday.
Intercept added that it will provide additional information to healthcare professionals and patients as it works with the FDA on the transition process. (Reporting by Sneha S K in Bengaluru; Editing by Shreya Biswas)
加速审批上市批准
2025-09-12
·药通社
2025年9月11日,Intercept Pharmaceuticals宣布:应美国FDA的要求,自愿将用于治疗原发性胆汁性胆管炎 (PBC) 的药物 OCALIVA® (奥贝胆酸) 从美国市场撤回。
同时,FDA还暂停了所有涉及奥贝胆酸临床试验。
对此,Intercept美国总裁Vivek Devaraj表示:“我们仍然相信,所有临床和真实世界证据都支持 OCALIVA 用于适当的患者,我们为OCALIVA在推进PBC患者护理方面做出的贡献感到自豪。虽然我们对OCALIVA的收益风险状况的看法与FDA不同,但我们尊重其要求,并做出了这一艰难的决定,为患者和处方者提供明确的指导。
↓ 扫码加入药通社交流群 ↓
奥贝胆酸,最早于2016年5月获美国FDA批准上市,成为20年来唯一获批的原发性胆汁性肝硬化的重磅药物。
7个月后,奥贝胆酸又获得了EMA附条件批准上市,成为欧洲市场首个PBC二线治疗药物。
带着明星肝药的Title,奥贝胆酸销售良好,2019年全球销售为2.5亿美元,2020年为3.1亿美元,后续几年一直稳定在3亿美元左右。
然而这款明星药物自上市以来,临床风险获益比却备受质疑。早在2017年,FDA 就曾发出警告,指出不正确的剂量可能增加严重肝损伤和死亡的风险,并于2018年将其列入黑框警告。
奥贝胆酸就这样一路伴随着光环与质疑,直到2023年10月,欧洲人用药委员会(CHMP)宣布着手重新评估奥贝胆酸的临床风险获益比,最终在审查四期临床数据后得出结论:现有数据无法证实奥贝胆酸临床获益,建议撤市。
一代“传奇”奥贝胆酸在欧洲的结局就此落定,最终于2024年11月27日正式在欧洲撤市。而在美国市场,奥贝胆酸也是一样饱受着非议,如上文所说,FDA早在2018年就给出过黑框警告。
根据 FDA 的数据,从2021年5月26日至2024年9月18日,共发现了20例与 OCALIVA 相关的严重肝损伤病例,其中包括7例肝移植、8例肝移植评估或列入名单,以及6例肝相关死亡。其中,至少有3例是发生在肝病已达晚期、本不应接受 OCALIVA 治疗的患者身上。
鉴于这些严重风险,OCALIVA 被明确禁用于:失代偿性肝硬化(如 Child-Pugh B 或 C 级)或有既往失代偿事件的 PBC 患者;它也禁用于伴有门脉高压证据(例如腹水、胃食管静脉曲张、持续性血小板减少症)的代偿性肝硬化患者,以及完全胆道阻塞的患者。除此之外,还有非常多不良反应。
而今随着原研宣告主动在美国撤市,一代明星肝药的结局也算注定了。
↓ 扫码加入药通社交流群 ↓
而看回国内,奥贝胆酸原研国内一直未上市。
2021年3月,奥贝胆酸片入选我国第二批鼓励仿制药品目录,面对如此市场自然有仿制企业跃跃欲试,随后多家企业进行了仿制研究及申报。
但结果看来并不好,就在上周,南京正大天晴的奥贝胆酸片才刚刚被下发通知件,至此正大天晴该品种的所有上市申请已全部失败。
相关文章:原研撤市,仿制再失败!
2020年,恒瑞曾仅做BE试验申报上市,被驳回。在此之后,正大天晴就着手进行III期临床,且进行了两次不同目的临床:
一次是奥贝胆酸片与熊去氧胆酸(UDCA)联合使用的有效性和安全性;另一次是奥贝胆酸片在胆管炎中的有效性和安全性。
然而前者于今年8月被驳回,后者于上周被驳回。III期临床费用不低,正大天晴还做了两次,可惜现如今全部失败告终。
奥贝胆酸原研的质疑,显然已经蔓延到了仿制药,原研撤市对国内仿制的影响很大。
目前提交上市申请的仅剩复旦张江一家,据摩熵医药显示:CDE于24年10月承办,并已于日前9月9日离开了新报任务,不知结果如何,估计很快会有答案了。
↓⭐关注药通社,洞见行业趋势↓
投稿/企业合作/内容沟通:
药通社总编—华籍美人(Ww_150525)
*添加请注明备注及来意
上市批准临床3期引进/卖出
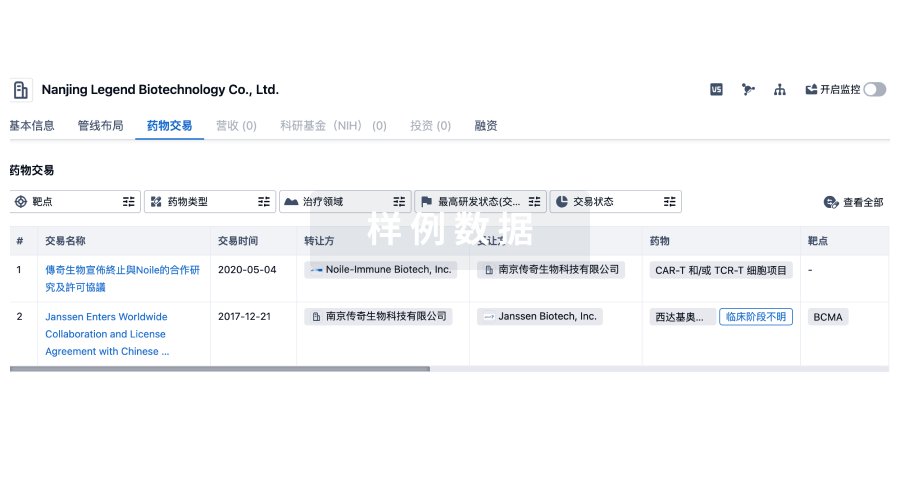
100 项与 Intercept Pharmaceuticals, Inc. 相关的药物交易
登录后查看更多信息
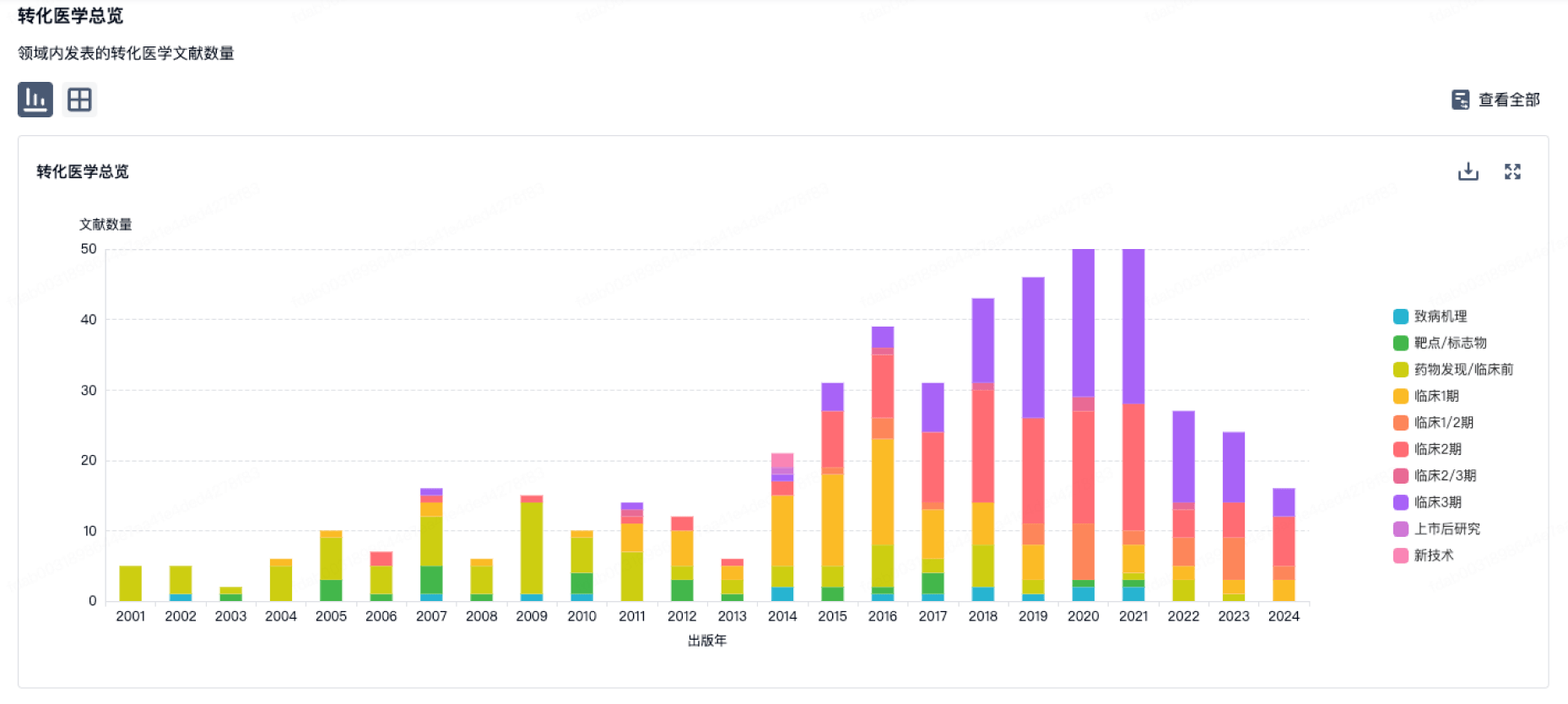
100 项与 Intercept Pharmaceuticals, Inc. 相关的转化医学
登录后查看更多信息
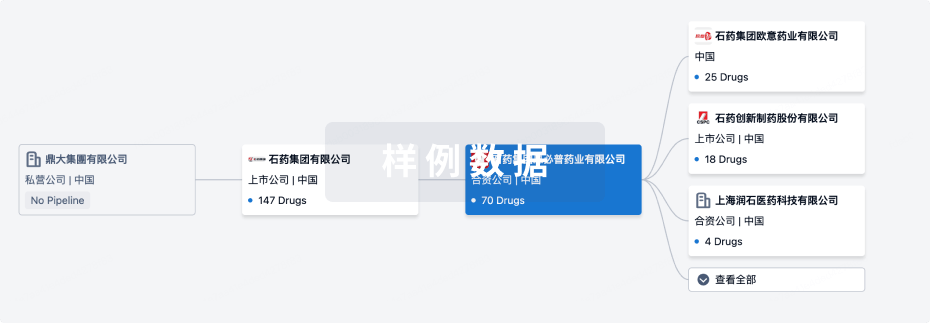
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年10月21日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
1
1
临床前
临床2期
1
1
临床3期
批准上市
2
2
其他
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
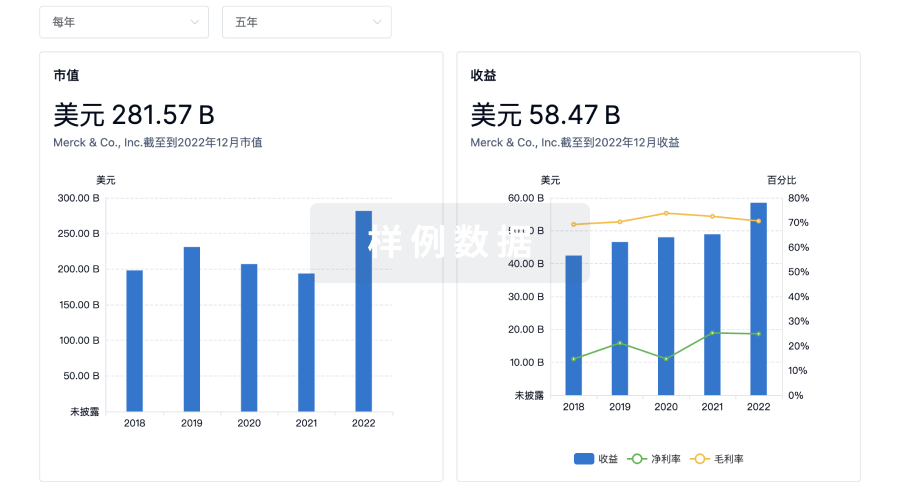
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
