预约演示
更新于:2025-05-16
Interferon alpha-2b (Beijing Kawin Technology)
人干扰素α2b (北京凯因)
更新于:2025-05-16
概要
基本信息
药物类型 干扰素 |
别名 Interferon alpha2b vaginal effervescent tablet Beijing Kawin technology、Recombinant human interferon alpha2b injection Beijing Kawin technology、Recombinant human interferon α2b(Beijing Kawin Technology) + [3] |
靶点 |
作用方式 激动剂、刺激剂、诱导剂 |
作用机制 IFNAR激动剂(干扰素α/β受体复合体激动剂)、免疫刺激剂、先天性抗病毒免疫应答诱导剂 |
在研适应症 |
非在研适应症 |
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
最高研发阶段(中国)批准上市 |
特殊审评- |
登录后查看时间轴
结构/序列
Sequence Code 167544

关联
4
项与 人干扰素α2b (北京凯因) 相关的临床试验CTR20241695
随机、双盲、安慰剂对照评价人干扰素α2b阴道泡腾片辅助治疗阴道/宫颈尖锐湿疣有效性和安全性的II期临床试验
主要目的:评价人干扰素α2b阴道泡腾片辅助治疗女性阴道/宫颈尖锐湿疣的有效性;
次要目的:评价人干扰素α2b阴道泡腾片辅助治疗女性阴道/宫颈尖锐湿疣的安全性。
开始日期2024-06-17 |
申办/合作机构 |
CTR20233836
评价人干扰素α2b喷雾剂治疗儿童疱疹性咽峡炎患儿的有效性和安全性的多中心、随机、双盲、安慰剂对照的II期临床试验
主要目的: 评价人干扰素α2b喷雾剂治疗儿童疱疹性咽峡炎的有效性。
次要目的: 评价人干扰素α2b喷雾剂治疗儿童疱疹性咽峡炎的安全性; 探索人干扰素α2b喷雾剂治疗儿童疱疹性咽峡炎的有效剂量。
开始日期2024-01-22 |
申办/合作机构 |
CTR20223324
一项在中国健康成年受试者中评价人干扰素α2b喷雾剂单次给药的安全性、耐受性、药代动力学和药效动力学的单中心、开放标签、剂量递增I期临床研究
主要目的:1)评价人干扰素α2b喷雾剂在中国健康成年受试者中单次用药的安全性和耐受性。
次要目的:1)评价人干扰素α2b喷雾剂在中国健康成年受试者中单次用药的药代动力学(PK)特征。2)评价人干扰素α2b喷雾剂在中国健康成年受试者中单次用药的药效动力学(PD)。3)评价人干扰素α2b喷雾剂的免疫原性。
开始日期2023-01-06 |
申办/合作机构 |
100 项与 人干扰素α2b (北京凯因) 相关的临床结果
登录后查看更多信息
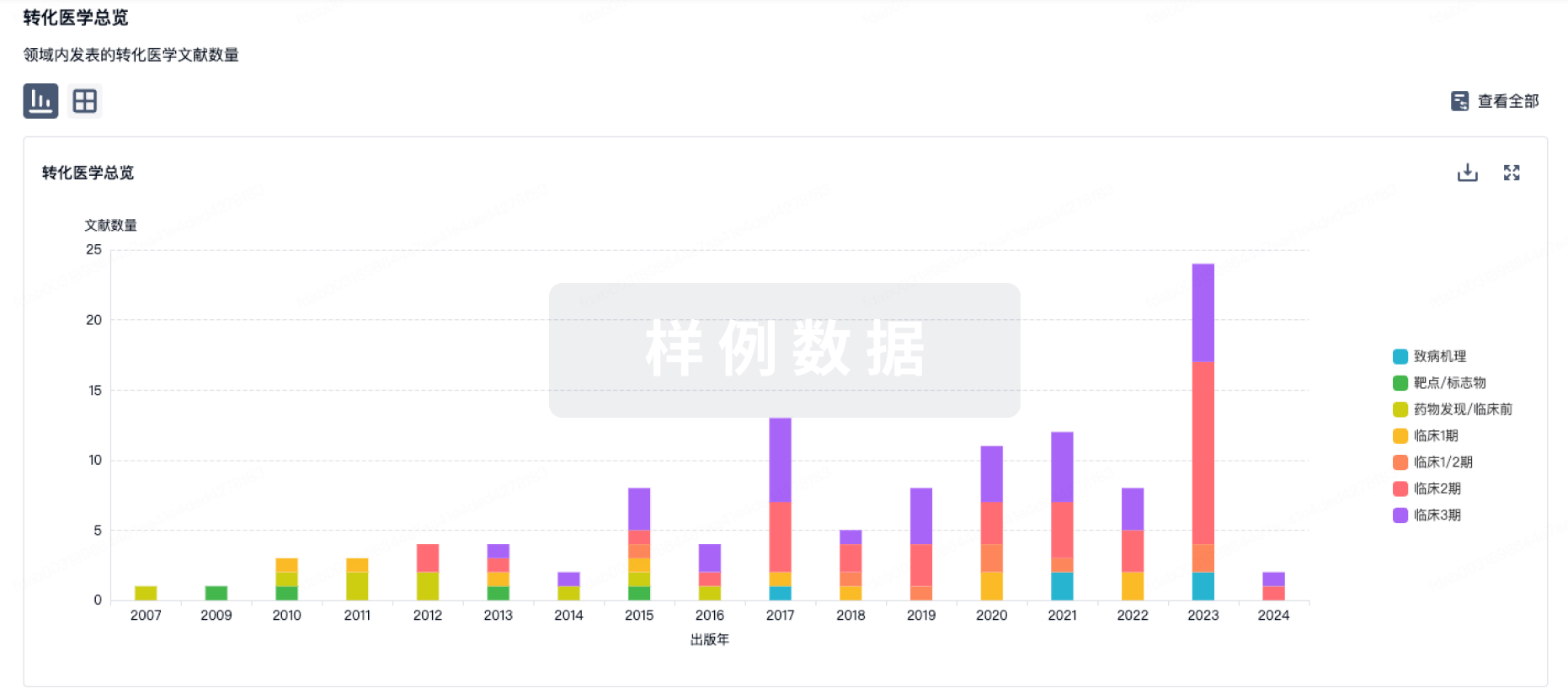
100 项与 人干扰素α2b (北京凯因) 相关的转化医学
登录后查看更多信息
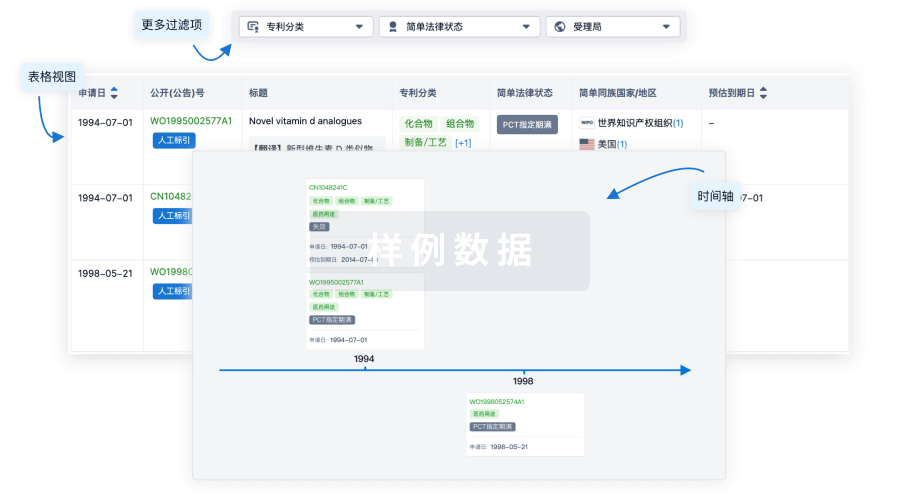
100 项与 人干扰素α2b (北京凯因) 相关的专利(医药)
登录后查看更多信息
39
项与 人干扰素α2b (北京凯因) 相关的文献(医药)2024-05-01·Oman journal of ophthalmology
Corneal ocular surface squamous neoplasia: Case series and review of literature
Article
作者: Kaliki, Swathi ; Agarwal, Ayushi ; Farhan, Marwan H. ; Mishra, Dilip K.
The authors present a retrospective analysis of three cases of isolated corneal ocular surface squamous neoplasia (C-OSSN) without limbal or conjunctival involvement and review the clinical and anterior segment optical coherence tomography (AS-OCT) features, along with treatment outcomes. The mean age at presentation was 51 years (range: 32–64 years). The mean tumor diameter was 5 mm (range: 3–6.5 mm). All lesions were placoid with <1 mm thickness. One case had surface keratin. AS-OCT revealed hyperreflective epithelium with abrupt transition in all cases, with mean thickness of 118 μm (range: 60–162 μm). One patient underwent alcohol-assisted keratoepitheliectomy (AKE) and two patients received topical Interferon alpha-2B followed by AKE. Histopathology revealed mild squamous dysplasia in all. No tumor residue or recurrence was noted at a mean follow-up period of 2 years (range: 1–4 years). Isolated C-OSSN is rare. AS-OCT serves as a useful noninvasive tool for supporting the diagnosis of AKE yielding long-term favorable outcomes.
2011-04-01·Pediatric blood & cancer3区 · 医学
Gorham's disease and diffuse lymphangiomatosis in children and adolescents
3区 · 医学
Article
作者: Marcio H. Malogolowkin ; Nina S. Ma ; Pisit Pitukcheewanont ; Leo Mascarenhas ; Rajkumar Venkatramani
Abstract:
Gorham's disease is a rare disorder of unknown etiology and variable clinical presentation that is characterized by proliferation of thin‐walled vascular channels resulting in destruction and resorption of osseous matrix. The condition is frequently under recognized or misdiagnosed. There is no standard treatment defined for this disease. Here we report on eight children diagnosed with Gorham's disease at our institution over a ten‐year period. Soft tissue lymphangioma was present in seven and six children had splenic involvement. Disease stabilization and improvement was observed on treatment with interferon alpha‐2b and bisphosphonate therapy. Pediatr Blood Cancer 2011;56:667–670. © 2010 Wiley‐Liss, Inc.
2009-12-01·Hematology (Amsterdam, Netherlands)4区 · 医学
Minimal residual disease and normalization of the bone marrow after long-term treatment with alpha-interferon2b in polycythemia vera. A report on molecular response patterns in seven patients in sustained complete hematological remission
4区 · 医学
ArticleOA
作者: Hasselbalch, Hans Carl ; de Stricker, Karin ; Andersen, Morten T. ; Møller, Michael Boe ; Samuelsson, Jan ; Nørgaard, Peter ; Marcher, Claus ; Larsen, Thomas Stauffer ; Bjerrum, Ole Weis
Polycythemia vera (PV) is characterized by the presence of the JAK2V617F mutation in virtually all patients. Several studies have shown that the JAK2V617F mutational load decreases during treatment with alpha-interferon 2. We report on molecular and histomorphological bone marrow responses in seven PV patients with profound molecular responses during and after long-term treatment with alpha-interferon 2b. All patients obtained a major molecular response (MMR). Subsequently all patients discontinued alpha-interferon and sustained complete hematological remission with a follow-up period of median 10 months (range 4-30 months). Complete normalization of the bone marrow was seen in three of five patients. Long term treatment with IFN2b is able to induce 'minimal residual disease' with very low JAK2 V617F allele burden and may induce profound, and in some patients total, regression of histomorphological bone marrow features of PV. Finally, hematological remissions and major molecular responses can be sustained after discontinuation of long-term treatment with IFN2b.
11
项与 人干扰素α2b (北京凯因) 相关的新闻(医药)2025-01-16
·赛柏蓝
作者 | 颜色
来源 | 赛柏蓝
01
安徽将牵头开展全国生物药联盟集采
1月14日,安徽省医保工作会议在合肥召开,会议从七个方面对2025年安徽省医保工作作出部署。其中第三条提到,牵头全国生物药品联盟集采。
安徽在生物药集采方面已经有一定的经验,2023年部分化药及生物制剂集采中,人免疫球蛋白注射剂等被纳入,2022年部分化药及生物制剂集采中,利妥昔单抗等被纳入。
全国范围的生物药集采,胰岛素是最先进入的品种。
2021年11月,国家组织胰岛素集中采购首次将生物药纳入集采范围,中选产品平均降价48%。与集采前相比,三代胰岛素使用量占比从58%提升至70%;2024年4月,胰岛素国采接续,共13家企业的53个产品参与本次接续采购,49个产品获得中选资格,中选率92%。
国家医保局曾多次提及生物药集采。
2020年10月,国家医保局在对“十三届全国人大三次会议第6450号建议的答复”中提出“生物类似药并非集中带量采购的禁区”,首次从官方层面明确“将生物类似药纳入集采”。
2023年3月,国家医保局发布《关于做好2023年医药集中采购和价格管理工作的通知》,鼓励省级药品集采从“填空”和“补缺”两个维度扩大集采覆盖范围,化学药、中成药、生物药均应有所覆盖。生物药逐渐进入药品集采覆盖范围和规则探索阶段。
本次全国生物药品联盟集采将会有哪些品种纳入?
米内网数据显示,国内生物药及生物类似药获批企业≥3家的品种有7个,包括贝伐珠单抗注射液、注射用曲妥珠单抗、利妥昔单抗注射液、阿达木单抗注射液、注射用英夫利西单抗、地舒单抗注射液以及托珠单抗注射液。
这些品种2022年在中国公立医疗机构终端销售规模分别超过77、65、46、15、10、6及2亿元。竞争充分、市场体量大,被纳入集采的可能性增加。
生物药集采一直备受市场关注,其价格相对较高且无法开展一致性评价,市场需求持续增长且研发火热。
02
规则几何?哪些省份可能参与?
国家医保局认为,和化学药相比,生物药无一致性评价作为支撑,命名复杂多样、产能爬坡提升较慢,因此对集采条件及中选规则作出相应调整显得尤为重要。
胰岛素集采规则是在化药集采基础上,充分考虑生物药的特点而精心制定。下一步,国家医保局会在现有集采成功经验基础上,结合生物药特点,不断完善生物药集采规则。
在第六批胰岛素专项集采中,国家医保局在保供的基础上,对中选规则做出修改,如参与的厂家全部有产品中选等,大幅降价不是其主要目的,重点是挤掉药品部分价格虚高以及为后续的生物药集采作试点。
赛柏蓝不完全统计,截至目前,胰岛素、血液制品、生长激素、单抗、肝素、干扰素等生物制品均出现在不同层级的集采之中。
截至目前地方已经开展的生物药集采包括——
2022年3月10日,广东等11省联盟双氯芬酸等药品带量采购拟中选/备选结果出炉,生物类似药利妥昔单抗、血液制品首次被纳入了集采名单;
2023年12月14日,江西牵头开展的29省干扰素省际联盟集采,共有13家干扰素医药企业参加现场投标,12个品种48个规格采购成功。3家以上企业报名的品种(人干扰素α2b注射剂)中选平均降幅47.79%,最高降幅54.58%;2家企业报名的品种(人干扰素α1b注射剂和人干扰素α1b滴眼液)中选平均降幅19.38%,最高降幅24.55%;独家企业报名的9个品种中选平均降幅20.91%,最高降幅27.19%。
2023年7月21日,江西省药品医用耗材集中采购联席会议办公室发布《关于干扰素省际联盟采购拟集采品种目录的公示》,14个干扰素品种纳入。
2023年8月17日,河北省医保局发布《河北牵头京津冀化学药品、生物制剂集中带量采购文件(HBYPJC-2023-01)》,纳入化药84种、生物药10种。
一旦全国生物药联盟集采启动,我国生物药千亿市场或将迎来洗牌,产能充足、竞争充分的产品或首当其冲。
END
内容沟通:郑瑶(13810174402)
左下角「关注账号」,右下角「在看」,防止失联
生物类似药带量采购
2024-05-13
来源:国家药典委 编辑:wangxinglai2004近日,国家药典委发布了6个标准公示,分别为人用疫苗总论国家药品标准、碘帕醇国家药品标准、23价肺炎球菌多糖疫苗国家药品标准、安立生坦国家药品标准等标准,其中23价肺炎球菌多糖疫苗国家药品标准和人用疫苗总论国家药品标准公示期为3个月,其余同为2个月。 01 人用疫苗总论国家药品标准我委拟修订人用疫苗总论国家药品标准,标准编号:《中国药典》2020年版三部。为确保标准的科学性、合理性和适用性,现将拟修订的人用疫苗总论国家药品标准公示征求社会各界意见(详见附件)。公示期自发布之日起三个月。请认真研核,若有异议,请及时在线反馈,并附相关说明、实验数据和联系方式。来函需打印后加盖公章,个人来函需打印后本人签名,并邮寄至我委通讯地址。 公示期满未回复意见即视为对公示标准草案无异议。 联系人:王晓娟王晓娟 电话:010-6707956367079563 通信地址:北京市东城区法华南里11号楼国家药典委员会办公室 邮编:100061 02 碘帕醇国家药品标准我委拟制定碘帕醇国家药品标准。为确保标准的科学性、合理性和适用性,现将拟制定的碘帕醇国家药品标准公示征求社会各界意见(详见附件)。公示期自发布之日起两个月。请认真研核,若有异议,请及时在线反馈,并附相关说明、实验数据和联系方式。来函需打印后加盖公章,个人来函需打印后本人签名,并邮寄至我委通讯地址。 公示期满未回复意见即视为对公示标准草案无异议。 联系人:程奇蕾 电话:010-67079557 通信地址:北京市东城区法华南里11号楼国家药典委员会办公室 邮编:100061 03 23价肺炎球菌多糖疫苗国家药品标准我委拟修订23价肺炎球菌多糖疫苗国家药品标准,标准编号:《中国药典》2020年版第一增补本。为确保标准的科学性、合理性和适用性,现将拟修订的23价肺炎球菌多糖疫苗国家药品标准公示征求社会各界意见(详见附件)。公示期自发布之日起三个月。请认真研核,若有异议,请及时在线反馈,并附相关说明、实验数据和联系方式。来函需打印后加盖公章,个人来函需打印后本人签名,并邮寄至我委通讯地址。公示期满未回复意见即视为对公示标准草案无异议。联系人:王晓娟电话:010-67079563通信地址:北京市东城区法华南里11号楼 国家药典委员会办公室邮编:100061 04 注射用人干扰素我委拟修订注射用人干扰素α1b、人干扰素α1b注射液、注射用人干扰素α2a、人干扰素α2a注射液、注射用人干扰素α2b、人干扰素α2b注射液和注射用人干扰素γ国家标准,标准编号均为《中国药典》2020年版三部。为确保标准的科学性、合理性和适用性,现将拟修订的相关品种国家标准公示征求社会各界意见(详见附件)。公示期自发布之日起两个月。请认真研核,若有异议,请及时在线反馈,并附相关说明、实验数据和联系方式。来函需打印后加盖公章,个人来函需打印后本人签名,并邮寄至我委通讯地址。 公示期满未回复意见即视为对公示标准草案无异议。 联系人:赵雄曹琰 电话:010-67079598 通信地址:北京市东城区法华南里11号楼国家药典委员会办公室 邮编:100061 05 安立生坦国家药品标准我委拟制定安立生坦国家药品标准。为确保标准的科学性、合理性和适用性,现将拟制定的安立生坦国家药品标准公示征求社会各界意见(详见附件)。公示期自发布之日起两个月。请认真研核,若有异议,请及时在线反馈,并附相关说明、实验数据和联系方式。来函需打印后加盖公章,个人来函需打印后本人签名,并邮寄至我委通讯地址。 公示期满未回复意见即视为对公示标准草案无异议。 联系人:周怡 电话:010-67079556 通信地址:北京市东城区法华南里11号楼国家药典委员会办公室 邮编:100061 06 安立生坦片国家药品标准我委拟制定安立生坦片国家药品标准。为确保标准的科学性、合理性和适用性,现将拟制定的安立生坦片国家药品标准公示征求社会各界意见(详见附件)。公示期自发布之日起两个月。请认真研核,若有异议,请及时在线反馈,并附相关说明、实验数据和联系方式。来函需打印后加盖公章,个人来函需打印后本人签名,并邮寄至我委通讯地址。 公示期满未回复意见即视为对公示标准草案无异议。 联系人:周怡 电话:010-67079556 通信地址:北京市东城区法华南里11号楼国家药典委员会办公室 邮编:100061
疫苗
2024-02-06
·赛柏蓝
作者 | 颜色来源 | 赛柏蓝近段时间,不少地方带量采购又有了新的进展,易短缺药和急抢救药联盟集中带量采购公布中选/备选结果、全国中成药联盟采购(湖北)执行公布最新进展、全国中成药联盟采购(湖北)非中选和流标药品议价结果公布......此前,全国医疗保障工作会议在北京召开。会议研究部署了2024年的医保工作,并明确提到今年医保工作的九大重点,其中第六点:推动集采“扩围提质”。开展新批次国家组织药品耗材集采,做好集采中选品种协议期满接续,实现国家和省级集采药品数合计至少达到500个。01易短缺和急抢救药联盟集中带量采购中选/备选结果公布2月5日,广州公共资源交易中心发布《关于公布易短缺和急抢救药联盟集中带量采购中选/备选结果的通知》。易短缺和急抢救药联盟集中带量采购针对国家基本医保药品目录内部分需稳价保供临床必需易短缺类、急抢救类等化学药品和治疗用生物制品药品剂型开展。药品集中带量采购周期原则上到2026年12月31日,自中选结果实际执行日起计。2023年12月,广州公共资源交易中心发布《易短缺和急抢救药联盟集中带量采购文件》,山西省、内蒙古自治区、辽宁省、黑龙江省、上海市、江苏省、浙江省、安徽省、福建省、江西省、河南省、湖北省、湖南省、广东省、广西壮族自治区、海南省、重庆市、四川省、贵州省、云南省、西藏自治区、陕西省、甘肃省、青海省、宁夏回族自治区、新疆维吾尔自治区和新疆生产建设兵团组成省际采购联盟开展易短缺和急抢救药品联盟集中带量采购工作。在拟中选或备选产品确定上,分类确定,一是单位可比价排序,二是对于非专项品种,同品种同组有效报价的企业仅有2家及以下的,有效报价企业均为拟中选企业,其申报价格为拟中选价格等;三是对于专项品种,有专项价格的产品,有效报价的相应企业为拟中选企业,其申报价格为拟中选价格等;四是采取复活机制等。中选和备选结果公布后,接下来就是落地执行的系列工作。02全国中成药联盟采购(湖北)非中选和流标药品议价结果公布日前,湖北省医保局发布《关于执行全国中成药联盟采购(湖北)非中选和流标药品议价结果的通知》,从2024年2月5日起,全省统一执行本次议价结果。执行要求主要在几个方面,一是挂网价格,对议价成功药品、议价未成功药品、其他非中选和流标药品;二是医保支付标准,如议价成功药品按规定以该药品议价价格或同采购组中选报价代表品日均费用最高值确定医保支付标准等。中成药集采逐渐常态化。全国开展的中成药集采包括湖北牵头的首轮中成药集采(平均降幅42.27%)、广东牵头的6省中成药集采(平均降幅55.9%)、山东中成药集采(平均降幅44.31%)、北京中成药集采(平均降幅23%)等。目前来看,不少省份的集采不仅包括化药,还有中成药和生物药等,三大领域一次性覆盖。03广东阿比特龙等药品集中带量采购续签1月12日,广东省医保局发布《关于做好阿比特龙等药品集中带量采购续签工作的通知》,对阿比特龙等药品集中采购第二采购年续签。本次续签的阿比特龙等药品集采的中选(入围)产品第二采购年的实施时间,自2024年1月1日起至2024年12月31日止。续签对于药品进院和供应十分重视,要求畅通进院渠道,即医疗机构要按照约定采购量所列品种,确保相关中选(入围)产品进入医院,并在采购周期内完成合同用量。同时,医疗机构要按采购合同与企业及时结清药款,结清时间不得超过交货验收合格后次月底,并履行承诺及承担相应违约责任。此前,广东省医保局组织开展了第二、四批国家组织药品集采协议期满的阿比特龙等66个药品的集中带量采购。04河南联盟药品集中带量采购中选结果执行(新疆地区)1月30日,新疆维吾尔自治区医保局发布《关于做好国家组织第九批、河南联盟药品集中带量采购中选结果执行工作的通知》。新疆维吾尔自治区医保局对第九批国采新疆(含兵团)中选品种、备供品种及第二备供品种,河南联盟十九省药品集中采购中选品种结果进行执行工作,从2024年3月20日起。本次国家组织第九批各品种采购周期自中选结果执行之日起至2027年12月31日;河南联盟十九省药品采购周期为1年,视情况可延长1年。根据新疆维吾尔自治区医保局相关工作安排,生产、经营(配送)企业注册、认证和信息维护工作截止时间为2024年2月23日;中选产品信息确认截止时间为2024年2月26日;生产、经营(配送)企业确认配送关系截止时间为2024年3月3日;自治区和兵团医药招采管理系统于3月20日起切换采购价格。同时,参与集中采购的医药机构于2024年3月4日-18日在网上完成第三方协议签订,配送(经营)企业要在3月19日前将中选产品配送入院。新疆维吾尔自治区医保局还发布了系列配套政策协同,包括落实贷款结算、推进梯度降价和医保支付政策有序衔接等。05胰岛素集中带量采购协议期满接续采购品种范围相关采购数据报送开始2月5日,湖南省医保局发布《关于报送胰岛素集中带量采购协议期满接续采购品种范围相关采购数据的通知》,本次接续采购品种范围与第六批国采药品相同,纳入人胰岛素和胰岛素类似物,包括餐食人胰岛素、基础人胰岛素、预混人胰岛素、餐食胰岛素类似物、基础胰岛素类似物、预混胰岛素类似物共6个采购组。根据时间安排,2月6日(周二)24:00前,导入管理用户账号和医疗机构账号,相关用户可通过账号进入系统进行报量操作测试;2月7日(周四)正式启动报量,导入2023年历史采购量数据供医疗机构参考,医疗机构填报时需对应到每个药品名称下的每个药品上市许可持有人/生产企业/分包装厂,并于3月1日(周五)24:00前提交数据;3月5日(周二)24:00前,需要各市州医保部门完成人胰岛素和胰岛素类似物采购需求量审核工作等。06江西干扰素省际联盟集采最新进展1月31日,江西省医保局发布《关于干扰素省际联盟集中带量采购拟中选结果申投诉意见采纳情况的公告》。本次共有4个申诉内容,均未采纳。2023年12月16日,江西牵头29省干扰素联盟集采产生拟中选结果。江西省干扰素集采共有13家干扰素医药企业参加现场投标,12个品种48个规格采购成功。3家以上企业报名的品种(人干扰素α2b注射剂)中选平均降幅47.79%,最高降幅54.58%;2家企业报名的品种(人干扰素α1b注射剂和人干扰素α1b滴眼液)中选平均降幅19.38%,最高降幅24.55%;独家企业报名的9个品种中选平均降幅20.91%,最高降幅27.19%。根据联盟省份约定采购量计算,相对最高有效申报价,预计可为联盟省份年节约采购资金3.07亿元。注:文中统计品种数未去重。附:易短缺和急抢救药联盟集中带量采购中选药品供应清单阿比特龙等药品集中带量采购续签干扰素省际联盟集中带量采购拟中选结果申投诉意见采纳情况END医药代表交流群扫描下方二维码加入医药代理商转型交流群扫描下方二维码加入
带量采购一致性评价
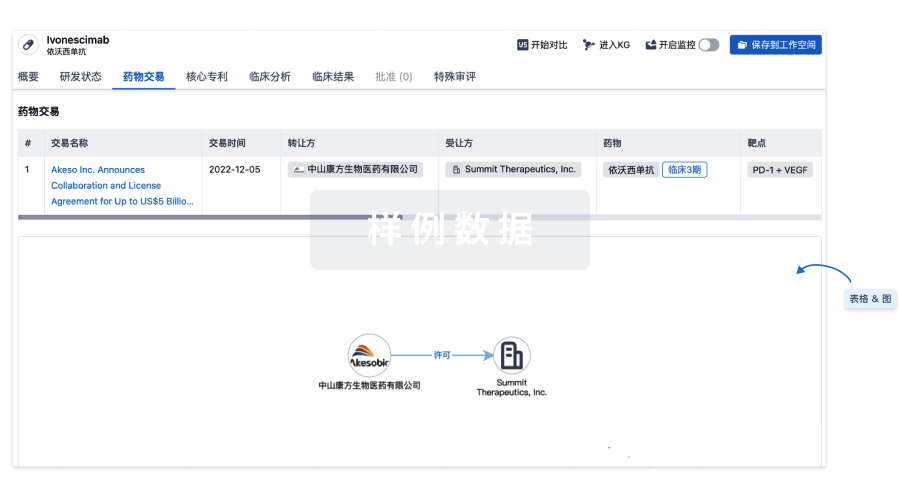
100 项与 人干扰素α2b (北京凯因) 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | - | - |
研发状态
批准上市
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 肾肿瘤 | 中国 | 2015-09-20 | |
| 毛细胞白血病 | 中国 | 2015-08-21 | |
| 费城染色体阳性慢性粒细胞白血病 | 中国 | 2015-08-18 | |
| 淋巴瘤 | 中国 | 2015-08-17 | |
| 尖锐湿疣 | 中国 | 2015-08-15 | |
| 丙型肝炎 | 中国 | 2015-08-15 | |
| 基底细胞癌 | 中国 | 2015-08-14 | |
| 卵巢上皮癌 | 中国 | 2015-08-13 | |
| 黑色素瘤 | 中国 | 2015-08-12 | |
| 卡波西肉瘤 | 中国 | 2015-08-11 | |
| 水痘 | 中国 | 2015-08-09 | |
| 多发性骨髓瘤 | 中国 | 2015-08-09 | |
| 乙型肝炎 | 中国 | 2015-08-06 | |
| 子宫疾病 | 中国 | 2012-12-15 | |
| 肿瘤 | 中国 | 2001-01-01 | |
| 病毒感染 | 中国 | 2001-01-01 |
未上市
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 疱疹性咽峡炎 | 临床2期 | 中国 | 2024-01-22 | |
| 生殖器疱疹 | 临床申请批准 | 中国 | 2024-03-19 | |
| 新型冠状病毒感染 | 临床前 | 中国 | 2022-07-07 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
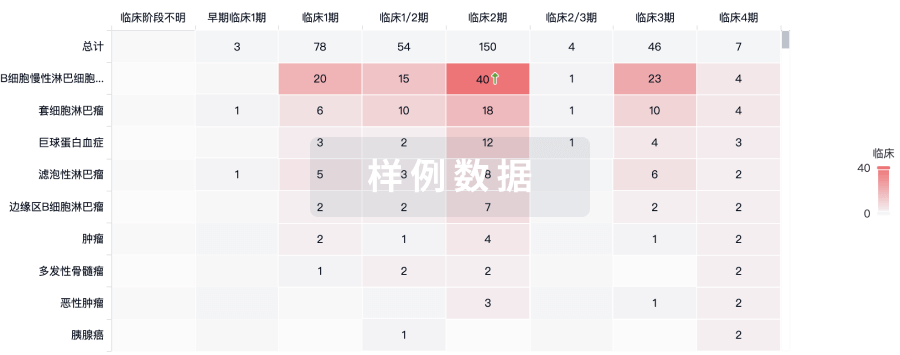
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
