预约演示
更新于:2025-05-07
Hyperinsulinism
高胰岛素血症
更新于:2025-05-07
基本信息
别名 Elevated insulin level、Elevated insulin levels、HYPERINSULINEMIA + [48] |
简介 A syndrome with excessively high INSULIN levels in the BLOOD. It may cause HYPOGLYCEMIA. Etiology of hyperinsulinism varies, including hypersecretion of a beta cell tumor (INSULINOMA); autoantibodies against insulin (INSULIN ANTIBODIES); defective insulin receptor (INSULIN RESISTANCE); or overuse of exogenous insulin or HYPOGLYCEMIC AGENTS. |
关联
220
项与 高胰岛素血症 相关的药物作用机制 PPARα激动剂 [+1] |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2024-06-10 |
靶点- |
作用机制 细菌替代物 [+1] |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期2022-11-30 |
作用机制 glucokinase激活剂 |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2022-09-30 |
4,463
项与 高胰岛素血症 相关的临床试验NCT06825143
Therapeutic Strategies to Reduce Endothelial Ischemia-reperfusion Injury with Metabolic Syndrome: a Combination Approach with Lactate Administration and Ischemic Preconditioning
The objective of this clinical trial is to better understand how lactate, a naturally occurring energy substance, can be used to lessen damage to the vascular system in adults with a high cardiovascular disease risk.
The main questions it aims to answer are:
1. Does giving lactate intravenously reduce injury to the vascular system?
2. Does giving lactate intravenously together with blood flow occlusion - known as ischemic preconditioning, reduce vascular injury better than blood flow occlusion by itself?
3. How does lactate help the vascular system?
Researchers will compare lactate to a placebo (a look-alike substance that contains no lactate) to see if lactate works to lessen vascular injury.
Researchers will also compare lactate to blood flow occlusion to see which one is better at preventing vascular injury.
Researchers will also compare lactate and blood flow occlusion together to see if combining them works better than either one alone.
In one visit to the laboratory, participants will:
Obtain a measurement of vascular health in an arm Be given liquid lactate, a liquid placebo, and/or arm blood flow occlusion Obtain a second measurement of vascular health in an arm.
The main questions it aims to answer are:
1. Does giving lactate intravenously reduce injury to the vascular system?
2. Does giving lactate intravenously together with blood flow occlusion - known as ischemic preconditioning, reduce vascular injury better than blood flow occlusion by itself?
3. How does lactate help the vascular system?
Researchers will compare lactate to a placebo (a look-alike substance that contains no lactate) to see if lactate works to lessen vascular injury.
Researchers will also compare lactate to blood flow occlusion to see which one is better at preventing vascular injury.
Researchers will also compare lactate and blood flow occlusion together to see if combining them works better than either one alone.
In one visit to the laboratory, participants will:
Obtain a measurement of vascular health in an arm Be given liquid lactate, a liquid placebo, and/or arm blood flow occlusion Obtain a second measurement of vascular health in an arm.
开始日期2026-10-01 |
申办/合作机构- |
NCT06765057
Effect of Probiotics "Psychobiotics" on Depression in Adults With Obesity and Metabolic Syndrome in Riyadh City
The goal of this clinical trial is to assess the effect of commercial multi-strains psychobiotics supplementation as an ad-on therapy on depressive symptoms and metabolic syndrome components (HDL-C, FPG, TGs, WC, BP) in adult depressed obese patients with metabolic syndrome. The second goal is to explore the effect of commercial multi-strains psychobiotics supplementation on the anthropometric measurement (weight, body mass index (BMI)) in adult depressed obese patients with metabolic syndrome. The main questions they aim to answer are:
* Will commercial multi-strains psychobiotics supplementation help to ease depressive symptoms as an ad-on therapy in patients with obesity and metabolic syndrome?
* Will commercial multi-strains psychobiotics supplementation improve anthropometric measurements and metabolic syndrome components (WC, FPG, BP, TGs, HDL-C) in obese depressed patients? Researchers will compare psychobiotics to a placebo (a look-alike substance that contains no drug) to see if psychobiotics work to improve depression and obesity comorbid with metabolic syndrome.
Participants will:
* Be examined for depression, anxiety, and metabolic syndrome components (waist circumference, diabetes, blood pressure, triglycerides, and high-density lipoprotein).
* Be asked to conduct laboratory tests to determine the inclusion and exclusion criteria.
* Be given probiotics/ placebo to consume every day for 3 months.
* Repeat the examination and laboratory tests to determine the results.
* Be followed up weekly for adverse events and to insure their compliance with the study instructions.
* Be followed up after 4 weeks as an end-visit and will conduct the examination and the laboratory blood tests.
* Will commercial multi-strains psychobiotics supplementation help to ease depressive symptoms as an ad-on therapy in patients with obesity and metabolic syndrome?
* Will commercial multi-strains psychobiotics supplementation improve anthropometric measurements and metabolic syndrome components (WC, FPG, BP, TGs, HDL-C) in obese depressed patients? Researchers will compare psychobiotics to a placebo (a look-alike substance that contains no drug) to see if psychobiotics work to improve depression and obesity comorbid with metabolic syndrome.
Participants will:
* Be examined for depression, anxiety, and metabolic syndrome components (waist circumference, diabetes, blood pressure, triglycerides, and high-density lipoprotein).
* Be asked to conduct laboratory tests to determine the inclusion and exclusion criteria.
* Be given probiotics/ placebo to consume every day for 3 months.
* Repeat the examination and laboratory tests to determine the results.
* Be followed up weekly for adverse events and to insure their compliance with the study instructions.
* Be followed up after 4 weeks as an end-visit and will conduct the examination and the laboratory blood tests.
开始日期2026-01-15 |
申办/合作机构 |
NCT06759740
An Exploratory Study of 68Ga-DOTA-SEMA in Preoperative Precise Imaging of Patients with Glucagon-Like Peptide-1 Receptor (GLP1R) Positive Insulinomas
Traditional imaging techniques for insulinomas have a low detection rate. This study aims to evaluate the safety, internal radiation dosimetry, and targeted imaging capability of the novel GLP1R imaging agent, 68Ga-DOTA-SEMA, in patients with GLP1R-positive insulinomas.
开始日期2026-01-01 |
申办/合作机构 |
100 项与 高胰岛素血症 相关的临床结果
登录后查看更多信息
100 项与 高胰岛素血症 相关的转化医学
登录后查看更多信息
0 项与 高胰岛素血症 相关的专利(医药)
登录后查看更多信息
180,121
项与 高胰岛素血症 相关的文献(医药)2026-01-01·Neural Regeneration Research
Adiponectin as a potential mediator of the pro-cognitive effects of physical exercise on Alzheimer’s disease
Article
作者: Tsang, Hector Wing Hong ; Rosa, Julia Macedo ; Yau, Suk-Yu ; Yu, Jia-Sui ; Ou, Hai-Ning ; Guo, Hui-Hui ; Formolo, Douglas Affonso ; Cheng, Tong
2025-12-31·Renal Failure
The role of endothelin receptor antagonists in kidney disease
Review
作者: Chen, Wenmin ; Ma, Xiaoting ; Liang, Yuyang ; Lin, Haishan ; Zheng, Lingqian ; Zhou, Tianbiao
2025-12-31·Annals of Medicine
The addition of alpha-ketoglutarate to NT-proBNP improves the prediction of long-term all-cause mortality in acute heart failure patients
Article
作者: Zhang, Hao ; Peng, Zhengliang ; Zeng, Xianghui ; Dong, Yugang ; Ma, Zhuang ; Zeng, Qingchun ; Liu, Chen ; Xu, Dingli ; Zhan, Qiong ; Huang, Yuli ; Xu, Tianyu
2,634
项与 高胰岛素血症 相关的新闻(医药)2025-05-05
点击“蓝字”关注我们编者按近年来,孤独和社交隔离越来越被认为是公共卫生领域的重大问题。据研究,全球约25%的人群面临社交隔离,约21.3%的人群感到孤独。这些状况不仅影响心理健康,还可能与一系列慢性疾病的发生风险相关,尤其是2型糖尿病(T2DM)。近期一项发表在Diabetes Research and Clinical Practice杂志的研究结果表明[1],社交隔离与孤独已被证实是T2DM的重要风险因素。加强社会联结有望成为糖尿病防控的有效策略,提示应将心理社会因素纳入公共卫生政策与干预体系中。孤独与社交隔离与多种慢性疾病风险增加密切相关孤独与社交隔离日益成为全球公共卫生关注的重要议题,孤独与社交隔离不仅是情感层面的主观体验,更是一种“慢性社会应激状态”,对多系统健康造成深远影响。尽管孤独和社交隔离在日常语境中常被混为一谈,但它们在定义上却存在显著差异。社交隔离是指个体在社会网络中的互动和联系不足,表现为缺乏社交活动、亲密关系和社会支持。而孤独感则源于个体对其社交关系的不满足,表现为即便身处社交环境,也可能感受到强烈的孤立或被排斥的情绪。社交隔离通常是客观存在的,基于个体的社交互动频率、社交网络的规模等因素,而孤独则是一种主观的情感体验,可能出现在社交活动频繁的个体中。尽管它们存在差异,却往往紧密相连,孤独与社交隔离相互作用,共同对个体的健康状态产生深远影响。大量研究已证实,孤独与多种慢性疾病风险增加密切相关,如痴呆、高血压、卒中及冠心病。同样,社交隔离也与心力衰竭所致住院或死亡风险增加、肺炎发病率上升以及全因死亡率升高有关。尽管这些关联已较明确,但社交关系与其他慢性病(如T2DM)之间的潜在因果关系仍研究不足。近年来,关于孤独、社交隔离与T2DM发病之间关系的研究逐渐增多。许多研究表明,社会支持不足、情感孤立的个体可能更容易患上糖尿病。然而,目前关于孤独和社交隔离如何在生物学层面影响糖尿病发病的具体机制尚未完全阐明。此前一项Meta分析结果,独居个体发生T2DM的风险显著高于非独居者。然而,独居并不必然意味着社交关系差,因为它并不能直接反映孤独感或社交隔离状态。因此,关于不良社交关系与T2DM发病风险之间的关联仍存在重要研究空白,迄今尚无Meta分析对此进行系统评估。深入理解这一关联,有助于推动社会健康因素融入标准医疗实践,从而改善整体健康结果,并潜在地减少医疗成本。关注社会健康决定因素不仅有助于改善心理健康,还可能降低T2DM的发生风险。为了解决这一问题,本文基于一项Meta分析,深入探讨了孤独和社交隔离与T2DM之间的关系,并讨论如何通过改善社交联系与心理健康来降低糖尿病的风险。孤独和社交隔离均显著增加T2DM的发生风险该Meta分析共纳入了9项研究,涉及1 112 887例受试者。在这些受试者中,60.5%为女性,平均年龄为57.1岁。在平均长达10.7年的随访期间,共记录到50 961例新发T2DM患者。研究评估了孤独感和社交隔离对糖尿病发生风险的影响,通过计算风险比(HR)来量化其关联度。此外,研究还对包括性别、年龄、社会经济状态等在内的潜在混杂因素进行了调整,以确保结果的准确性。研究结果显示,孤独和社交隔离均与T2DM的发生风险增加显著相关。Meta分析显示,孤独感人群的糖尿病风险增加了32%(HR=1.32,95%CI:1.11~1.57)。这一结果表明,长期孤独感可能是糖尿病的重要危险因素,尤其是当孤独感较为严重或持续存在时,糖尿病的发生风险显著增加。社交隔离同样与T2DM的发生风险增加相关,风险增加了20%(HR=1.20,95%CI:1.01~1.43)。研究还进行了敏感性分析,结果表明,无论是否排除个别研究,孤独和社交隔离与糖尿病风险之间的关系都保持稳定。此外,研究表明,孤独和社交隔离的影响并没有因为参与者的年龄、随访时长等因素而显著变化。这些结果表明,无论是孤独感还是社交隔离,均对糖尿病的发生具有不容忽视的影响。特别是孤独感,它对糖尿病的影响似乎比社交隔离更为显著,可能与孤独带来的情感压力和生理反应有关。孤独和社交隔离增加T2DM发生风险的可能机制孤独是一种主观的负性情绪体验,常源于个体对社会联系的缺失感,即便身处人群中也可能感到孤独。大量研究表明,孤独与抑郁、焦虑等心理障碍密切相关,这些情绪障碍可通过影响下丘脑-垂体-肾上腺轴(HPA轴)功能,诱发皮质醇等应激激素的持续升高,进而促进肝脏糖异生、血糖升高。此外,孤独还可降低胰岛素敏感性、促进系统性慢性炎症反应,诱发胰岛素抵抗。这类人群往往缺乏外界支持,更易形成不健康的生活方式,如缺乏锻炼、高热量饮食、作息紊乱和药物依从性差,进一步加剧了T2DM的发生风险。社交隔离体现在个体与家庭、朋友、社区或社会网络之间的联系显著减少或完全中断,是一种客观存在的社会互动缺失状态。它不仅与心理健康恶化相关,还能激活多条生理路径,例如交感神经系统过度激活、促炎因子水平升高和自主神经功能失调,从而打破体内代谢稳态。研究显示,长期社交隔离可诱发低度慢性炎症,影响胰岛β细胞功能和胰岛素信号通路。此外,社交隔离人群由于缺乏社会支持和外界监督,更易采取被动应对方式,维持不良的健康行为模式。这些因素共同作用,可能显著提升T2DM的发生率和进展风险。该Meta结果对临床实践的启示孤独和社交隔离是T2DM的重要危险因素。解决社会联系可能是预防糖尿病的一项有价值的战略,这强调了将社会心理因素纳入公共卫生举措的必要性。促进社交互动与支持:鉴于孤独和社交隔离对糖尿病发病的潜在影响,临床医生应当关注患者的社交状况。在糖尿病的预防和治疗过程中,增强患者的社交支持网络至关重要。通过家庭支持、社交活动或社区参与等方式,可以有效改善患者的情绪状态,减轻孤独感。心理健康干预:对于感到孤独或有社交隔离的糖尿病患者,心理健康干预应成为治疗的一部分。认知行为疗法、社交技能训练等心理干预方法可以有效减少孤独感和抑郁症状,提高患者的生活质量。“社会处方”的推广:“社会处方”是一种由医疗机构和社区组织为患者或需要帮助的人群开具的非药物性处方,它通过社区病友会、社区治疗和社区护理等干预措施,旨在解决医疗之外的社会、心理和情感问题,从而改善个体的健康和生活质量。“社会处方”的适用人群包括慢性疾病患者、独居老人、社会孤立人群、有抑郁和焦虑等心理健康问题的患者等。近年来,“社会处方”在一些国家得到了应用,医生通过将患者与社区服务和志愿活动相连接,帮助患者改善社会关系和减少孤独感。这种方法在糖尿病患者群体中具有很大的潜力,能够帮助患者减轻社交隔离感,改善他们的整体健康状况。结语孤独和社交隔离不仅是心理健康的隐患,更是T2DM的重要危险因素。在临床实践中,医生应当意识到社交因素对患者健康的深远影响,将其纳入糖尿病的预防和管理策略中。通过改善患者的社交支持和心理健康,可以有效降低糖尿病的发生率,并提高患者的生活质量。参考文献:1.Diabetes Res Clin Pract. 2025 May:223:112124. doi: 10.1016/j.diabres.2025.112124. Epub 2025 Mar 22.声明:本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。最新《国际糖尿病》读者专属微信交流群建好了,快快加入吧!扫描左边《国际糖尿病》小助手二维码(微信号:guojitnb),回复“国际糖尿病读者”,ta会尽快拉您入群滴!(来源:《国际糖尿病》编辑部)版权声明版权属《国际糖尿病》所有。欢迎个人转发分享。其他任何媒体、网站未经授权,禁止转载。
2025-05-05
题图 | Pixabay撰文 | 宋文法糖尿病前期,是指血糖水平高于正常,但尚未达到糖尿病诊断标准的状态。糖尿病前期是2型糖尿病和心血管疾病的已知风险因素,已成为全球日益严重的公共健康问题。根据美国糖尿病协会的定义,糖尿病前期的特征是空腹血糖在100-125 mg/dL之间,糖化血红蛋在5.7-6.4%之间,或口服葡萄糖耐量试验2小时血糖在140-199 mg/dL之间。富含多酚的浆果类食物已被证明有助于降低2型糖尿病和心血管疾病风险,但目前针对糖尿病前期的研究较少。2025年4月16日,内华达大学的研究人员在" The Journal of Nutrition "期刊上发表了一篇题为" Strawberries improve insulin resistance and related cardiometabolic markers in adults with prediabetes:a randomized controlled crossover trial "的研究论文。研究显示,仅3个月,每天摄入32克冻干草莓,可以显著改善糖尿病前期患者的血糖控制,降低炎症水平,并改善整体心脏代谢健康,对于预防2型糖尿病和心血管疾病具有重要意义。图:论文截图在这项随机、对照、交叉试验中,纳入了25名糖尿病前期成年人,进行了一项为期28周的研究,研究分为两个12周的周期,中间有4周的洗脱期,参与者被随机分配到草莓组或对照组,草莓组每天摄入32克冻干草莓(相当于2.5份新鲜草莓),在不同时间节点收集了参与者的临床数据以及血液样本,分析了草莓对糖尿病前期患者胰岛素抵抗和心脏代谢健康的影响。结果发现,草莓组患者显著改善了血糖控制,包括血清胰岛素、胰岛素抵抗、空腹血糖和糖化血红蛋白,与对照组相比,分别平均降低了6.9 μIU/mL、2.3、8.9 mg/dL和0.2%。此外,草莓组还降低了血清总胆固醇水平,平均降低7.0 mg/dL,然而,草莓对LDL胆固醇、HDL胆固醇和甘油三酯没有显著影响。草莓对血糖、血脂、血压等影响(图:论文截图)不仅如此,草莓还降低了患者的体重和腰围,与对照组相比,草莓组平均降低了3.4磅、0.4英寸。重要的是,草莓还降低了患者的炎症标志物,高敏C反应蛋白、IL-6平均降低0.8 mg/L和10.8 ng/mL。草莓对血清炎症标志物的影响(图:论文截图)对于安全性而言,参与者整体依从性较好,且副作用较少。对于其中潜在的机制,研究指出,草莓中的多酚类化合物,如花青素和鞣花酸,可能通过激活胰岛素受体的磷酸化、降低氧化应激和炎症,从而改善胰岛素抵抗,降低血糖水平。研究指出,这项研究首次证明了草莓摄入可以改善糖尿病前期患者的胰岛素抵抗和整体心脏代谢状况,表明草莓是一种可行的、可持续的非药物干预手段。此外,研究还强调了草莓在减少炎症和改善血脂方面的作用,这对于预防2型糖尿病和心血管疾病具有重要意义。综上,结果表明,每天摄入2.5份新鲜草莓,持续12周,可以改善成年人的糖尿病前期血糖控制以及促进整体心脏代谢健康。参考文献:https://doi-org.libproxy1.nus.edu.sg/10.1016/j.tjnut.2025.04.015
临床研究临床结果
2025-05-03
点击“蓝字”关注我们编者按糖尿病是目前最主要的慢性非传染性疾病之一,患病率达10.5%,其中约90%为2型糖尿病(T2DM)。T2DM从发病机制到临床表现均呈现出高度异质性,导致临床管理复杂化。目前国际糖尿病组织的分型体系均未对T2DM进一步区分亚型,因此探索其亚型对引领精准治疗具有重要意义。在近期召开的第二十届湘雅国际糖尿病免疫学论坛上,中南大学湘雅二医院、国家代谢性疾病临床医学研究中心周智广教授聚焦T2DM精准分型领域,通过对比国内外分型差异,解析国内T2DM三大分型体系,并探讨与临床结局关联,层层递进剖析关键问题,为糖尿病的精准化管理提供了新思路与实践方向。以下为核心观点与创新进展的详细报道。国际分型与我国异同2018年,瑞典ANDIS研究基于起病年龄、体重指数(BMI)、HbA1c、稳态模型2评估的β细胞功能指数(HOMA2-B)、稳态模型2评估的胰岛素抵抗指数(HOMA2-IR)及谷氨酸脱羧酶抗体(GADA)等六项指标,通过无监督聚类将成人糖尿病分为5类,其中T2DM亚型包括:严重胰岛素缺乏型(SIDD)、严重胰岛素抵抗型(SIRD)、轻度肥胖相关型(MOD)和轻度年龄相关型(MARD)。由中南大学湘雅二医院、国家代谢性疾病临床医学研究中心(长沙)牵头的中国ADCC队列研究在2014~2017年对全国19 054名新诊成人糖尿病患者进行了研究分析,验证了ANDIS分型的稳定性,但发现了显著的人群差异:(1)亚型分布差异:中国患者SIDD组比例更高(瑞典均数未落入中国95%CI,P<0.05),MARD组比例更低;(2)代谢特征差异:中国患者起病年龄更轻(平均早5.2岁)、BMI更低(-1.8 kg/m2)、HbA1c更高(+0.6%)、HOMA2-B(-12%)和HOMA2-IR(-18%)更低;(3)治疗差异:中国患者胰岛素使用率更高(+23%),二甲双胍使用率更低(-34%),糖尿病家族史比例低于瑞典人群。因此,为了更好地探究我国T2DM人群的亚型特征,基于ADCC队列,通过数据驱动的方法,研究团队从17项指标中筛选出BMI、HbA1c、HOMA2-B和总胆固醇(TC)四项核心代谢指标,将中国T2DM患者分为三种亚型:温和进展型(MP2D)、肥胖相关型(OR2D)和胰岛素缺乏型(ID2D)(表1)。与ANDIS分型对比:中国ID2D与SIDD大部分重叠(70.03%),但OR2D与SIRD代谢特征差异显著(TC和BMI分布偏离瑞典95%CI)。表1. 中国T2DM患者三种亚型划分随后,通过敏感性分析、外部队列验证及全病程队列验证等多项验证,均得到与上述相似的结果,证明了该分类模型的稳定性与可重复性。亚型与临床结局的关联为了进一步探索T2DM分型对于糖尿病精准管理的指导意义,研究团队进一步分析了不同亚型的糖尿病并发症、合并症和死亡结局的差异。通过广义线性混合模型(GLMM)和Cox风险模型分析发现:(1)并发症差异:ID2D:神经病变(HR=1.8)和视网膜病变(HR=2.1)风险最高;OR2D:肾病(HR=1.6)、冠心病(HR=1.9)、脑卒中(HR=2.3)及代谢相关脂肪性肝病(MAFLD,HR=2.5)风险突出;(2)死亡风险:OR2D未校正死亡风险升高(HR=1.4,P=0.06),校正后差异不显著;(3)中国分型优势:较ANDIS分型更精准识别神经病变(AUC+0.12)和脑卒中(AUC+0.09)高风险人群。临床应用与展望在该项研究的基础上,研究团队已经开发了在线T2DM亚型分类器(http://subtyping4t2dm.com),以期在未来的研究工作中,深化亚型代谢机制研究,探索靶向干预策略;在未来的临床实践中,探索根据不同亚型选择不同治疗药物的有效性。致谢:本研究由全国46家中心共同完成:在本届湘雅论坛上,国家代谢性疾病临床医学研究中心(长沙)重磅推出六大糖尿病临床研究项目,标志着我国糖尿病研究进入多维度协同攻关新阶段。该系列研究将联合国内顶尖科研力量,构建覆盖糖尿病全病程、全类型的科研网络体系。本次启动的研究计划包括:“中国1型糖尿病环境因素研究(T1DEPC)”探索环境与疾病关联“中国1型糖尿病甜胞对研究(STAND)”聚焦中国人群基因特点“中国1型糖尿病综合管理计划(GLITTER)”建立全病程管理体系“中国1型糖尿病早期筛查计划(CARED)”强化预防医学实践应用“DPCC全面推广计划(DPCC)”推动糖尿病基层防治规范化“中国未定型糖尿病研究(ICDC)”破解未定型类型糖尿病难题国家代谢性疾病临床医学研究中心主任周智广教授表示,此次六大项目的协同推进,将推动实现从早期筛查、精准分型到全程管理的闭环研究体系。通过整合全国30余家核心单位及200余个研究站点,预计将建立覆盖10万例糖尿病患者的前瞻性队列,为制定符合中国人群特征的糖尿病防治策略提供高级别循证依据。据悉,该系列研究已吸引国内60余位糖尿病领域权威专家参与,未来将通过多中心协作模式,在疾病机制探索、诊疗技术创新和转化医学研究等方面实现突破,助力“健康中国2030”慢性病防治目标实现。专家简介周智广 教授中南大学湘雅二医院 代谢内分泌科 教授、一级主任医师、博导,“湘雅名医”国家杰出医师国家代谢性疾病临床医学研究中心主任糖尿病免疫学教育部重点实验室主任糖尿病细胞治疗湖南省工程研究中心主任中国医师协会内分泌代谢科医师分会名誉会长国家心血管病专家委员会心血管代谢医学专业委员会主任委员湖南省医学会副会长、湖南省内分泌专业委员会主委《中国医师杂志》主编,《 Front Immunol 》 副主编主持国家科技支撑计划、重点研发计划、国自国合重点等项目50余项培养毕业研究生186名(博士94名)获国家科技进步奖3项(排名第1、4、7 ),发表SCI论文380余篇获中国青年科技奖、卫生部有突出贡献中青年专家、全国优秀科技工作者等享受国务院政府特殊津贴(1993年始)供稿:中南大学湘雅二医院代谢内分泌科 谢雨婷,郭瑞声明:本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。最新《国际糖尿病》读者专属微信交流群建好了,快快加入吧!扫描左边《国际糖尿病》小助手二维码(微信号:guojitnb),回复“国际糖尿病读者”,ta会尽快拉您入群滴!(来源:《国际糖尿病》编辑部)版权声明版权属《国际糖尿病》所有。欢迎个人转发分享。其他任何媒体、网站未经授权,禁止转载。
临床结果临床研究
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
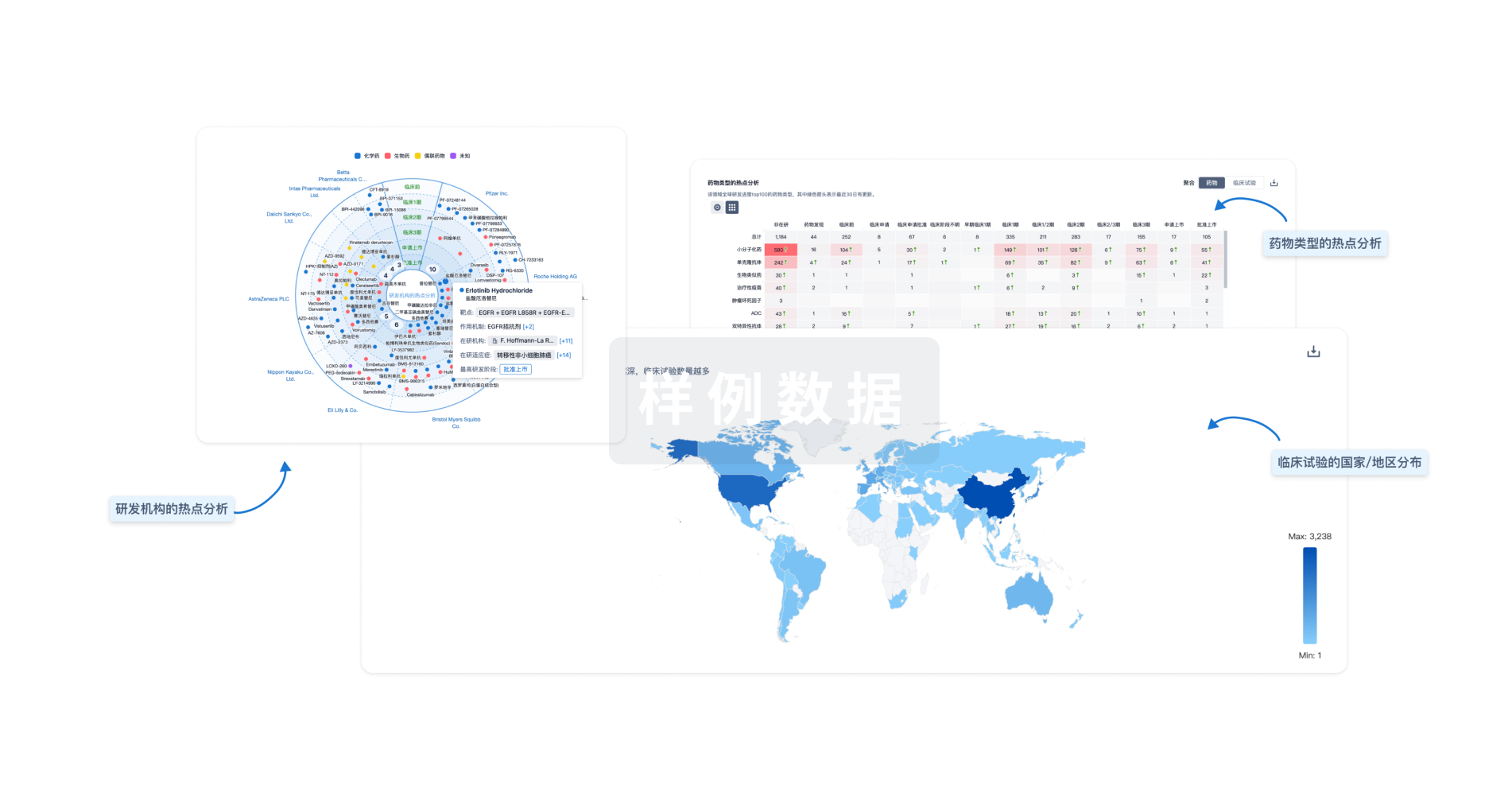
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用




