预约演示
更新于:2025-05-07
CCL19 x IL-7
更新于:2025-05-07
关联
4
项与 CCL19 x IL-7 相关的药物作用机制 CCL19 调节剂 [+2] |
在研适应症 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
作用机制 CCL19 调节剂 [+2] |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
作用机制 CCL19 调节剂 [+1] |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
1
项与 CCL19 x IL-7 相关的临床试验NCT04381741
CD19 CAR-T Expressing IL7 and CCL19 Combined With PD1 mAb for Relapsed or Refractory Diffuse Large B Cell Lymphoma
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin's lymphoma, accounting for 35% of lymphoma. Chimeric antigen receptor T cell (CAR-T) therapy is a new method to treat DLBCL. KTE-C19, published in the New England Medical Journal in December 2017, was used to treat relapsed and refractory B-cell lymphoma. One year of treatment for 111 patients, the total response rate was 82%, and the complete remission rate was 54%. However, a large number of clinical studies have shown that about 20% of patients with B-ALL and 50% of patients with B-NHL cannot achieve complete remission (CR) after CD19-CAR-T treatment. Targeting tumor microenvironment is an important new method to overcome the drug resistance of CAR-T cells. In this study, IL-7 and CCL19 were connected on the basis of traditional second generation CD19 CAR-T cells to construct novel fourth generation CAR-T cells, which can promote the infiltration, accumulation and survival of CAR-T cells in lymphoma tissue, and further enhance the anti-tumor effect of traditional CAR-T cells. At the same time, combined with four generations of CAR-T cells and PD1 monoclonal antibody, PD1 / PDL1 signal pathway was blocked, anti-tumor effect of CAR-T was improved, and immune response and long-term remission rate of DLBCL were improved.
开始日期2020-06-18 |
申办/合作机构 |
100 项与 CCL19 x IL-7 相关的临床结果
登录后查看更多信息
100 项与 CCL19 x IL-7 相关的转化医学
登录后查看更多信息
0 项与 CCL19 x IL-7 相关的专利(医药)
登录后查看更多信息
50
项与 CCL19 x IL-7 相关的文献(医药)2025-02-01·Clinical Lymphoma Myeloma and Leukemia
Plasma Cytokine and Chemokine Profiles Predict Efficacy and Toxicity of Anti-CD19 CAR-T Cell Therapy in Large B-Cell Lymphoma
Article
作者: Wang, Shuhua ; Koff, Jean L ; Waller, Edmund K ; Abousaud, Aseala I ; Zeng, Fanyuan ; O'Leary, Colin B ; Liu, Yuan ; Funk, Christopher R ; Wyman, Sarah ; Passang, Tenzin ; Rupji, Manali ; Zhang, Hanwen ; Li, Yiwen ; Dhodapkar, Kavita M
2024-09-01·Cancer Research Communications
Therapeutic Efficacy of IL7/CCL19-Expressing CAR-T Cells in Intractable Solid Tumor Models of Glioblastoma and Pancreatic Cancer
Article
作者: Adachi, Keishi ; Ohta, Keisuke ; Sakoda, Yukimi ; Nakajima, Masao ; Yasuda, Hiroyuki ; Tamada, Koji ; Shinozaki, Taro ; Nagano, Hiroaki
2024-09-01·Journal of Dental Research
The PerioGene North Study Uncovers Serum Proteins Related to Periodontitis
Article
作者: Holm, C.K. ; Lövgren, A. ; Betnér, S. ; Lerner, U.H. ; Isehed, C. ; Wänman, M. ; Hänström, L. ; Lindquist, S. ; Kindstedt, E. ; Palmqvist, P. ; Holmlund, A. ; Esberg, A. ; Lundberg, P.
24
项与 CCL19 x IL-7 相关的新闻(医药)2025-04-24
·同写意
近年来,嵌合抗原受体T细胞疗法(CAR-T)在恶性血液肿瘤中展现出的强大实力,使其逐渐成为最有前景的肿瘤免疫疗法,然而血液肿瘤(非实体瘤)仅仅是众多癌症中较小的一部分。根据2024年世界卫生组织国际癌症研究机构(IARC)在学术期刊CA: A Cancer Journal for Clinicians发布的2022年全球癌症负担数据显示,约90%的癌症发病率都是由实体瘤引起,全球癌症发病率和死亡率排名TOP5的癌症也均为实体肿瘤,而关于实体瘤的细胞治疗临床试验却相对较少,可见实体瘤未被满足的临床治疗需求巨大。2025年4月18日,聚焦于基因和细胞治疗的上海邦耀生物科技有限公司(以下简称“邦耀生物”)宣布,邦耀生物联合华东师范大学刘明耀教授、杜冰教授领衔的科研团队近日在国际顶级期刊Cancer Cell上发表了题为“CAR-T therapy in solid tumors”的综述文章,系统总结了CAR-T细胞疗法在实体瘤领域的突破性进展,深入剖析当前挑战,并提出多维度创新策略。该综述为全球实体瘤免疫治疗研究提供了重要方向,标志着CAR-T技术向实体瘤全面进军迈出关键一步。1突破性成果:从实验室到临床,实体瘤治疗曙光初现CAR-T疗法在血液肿瘤中已创造“治愈奇迹”,但在实体瘤中仍面临巨大挑战。在本综述中,研究团队首先汇总了全球多种实体瘤临床数据,并阐述了多项针对不同靶点的CAR-T细胞在治疗实体瘤中所取得的突破性进展:肺癌:相较于传统治疗手段,靶向EGFR的CAR-T细胞将患者的中位生存期提升至15.63个月。肝癌、胃癌:分别接受GPC3-CAR-T和CLDN18.2-CAR-T治疗后,实现了90%疾病控制率。前列腺癌:PSMA-CAR-T治疗后,可将患者前列腺特异性抗原(PSA)水平下降超95%以上。卵巢癌、脑胶质瘤:MSLN-CAR-T和GD2-CAR-T分别治疗后,实现70.2%(6个月生存率)和83.3%(12个月生存率)的显著疗效。尽管这些创新性CAR-T疗法在少数实体瘤患者中展示出了治疗潜力,但其整体的临床疗效仍有待提升。随后研究团队分析了CAR-T细胞治疗实体瘤面临的挑战,四大瓶颈亟待突破:(1)T细胞“疲劳”:长期对抗肿瘤导致CAR-T细胞活性下降。(2)误伤正常细胞:部分肿瘤靶点与正常组织相似,可能引发副作用。(3)免疫抑制的肿瘤环境:实体瘤微环境缺氧、营养匮乏,且充满抑制免疫的细胞和分子,如TGFβ等抑制CAR-T细胞的免疫反应。(4)CAR-T细胞难迁移并浸润:实体瘤具备纤维组织的物理屏障,加之趋化因子表达匮乏,不利于CAR-T细胞的定位和浸润。图1. CAR-T疗法在实体瘤中的挑战最后,研究团队对优化并提升CAR-T细胞治疗实体瘤的相关研究进展进行了归纳与总结,系统地提出了5大创新升级方案,让CAR-T疗法更精准、更安全:01智能设计CAR结构• 引入“双靶点”技术(如GD2+B7-H3),降低误伤风险。• 整合CAR-T和TCR-T技术,开发“STAR-T”新型受体,提升肿瘤识别灵敏度。02增强CAR-T细胞功能• 过表达IL-10、FOXO1等因子,增强细胞持久性和杀伤力。• 基因编辑技术敲除耗竭相关基因(如NR4A),延长CAR-T存活时间。03革新CAR-T细胞生产工艺• 现货通用型CAR-T可实现“即取即用”,大大缩短制备周期的同时,也有效降低了生产成本。• 非病毒定点整合技术改造细胞,提升安全性,避免基因插入错误风险。04瓦解肿瘤免疫微环境• 装载“定位信号”(如IL-7/CCL19),引导细胞深入肿瘤内部,增强对肿瘤细胞的杀伤。• 改造CAR-T分泌LIGHT、肝素酶,可实现破坏肿瘤外部屏障或重塑肿瘤异常的脉管系统。05提升CAR-T治疗安全性• 双靶点CAR-T细胞的设计与改造,以降低中靶脱瘤毒性。• 引入“安全开关”及时控制副作用,阻断细胞因子风暴(CRS)关键通路。图2. 克服实体瘤障碍的策略2从“可能”到“可行”,CAR-T开启实体瘤治疗新时代作为本篇综述共同作者,邦耀生物创始人&董事长刘明耀教授表示:“随着基因编辑、合成生物学与临床转化的深度融合,CAR-T完全有望成为实体瘤治疗的‘终极武器’。”邦耀生物作为全球领先的细胞基因药企,在细胞治疗实体瘤领域也实现了多项突破性进展,不但打造了具有自主知识产权的增强型T细胞平台(HyperTCell®),其主要通过T细胞的基因改造来攻克实体瘤治疗的世界难题。于2025年1月,邦耀生物科研团队还在Molecular Therapy杂志最新发文,开发出了一种创新型CAR-T细胞“GITRL-PSMA-CAR-T”不仅可以直接增强CAR-T细胞的抗肿瘤活性,还可以促进其在实体肿瘤微环境中的持久性,进一步提升了CAR-T对实体肿瘤的治疗效果,有望加速实现实体瘤CAR-T疗法的开发与应用。不得不说,近年来随着对肿瘤免疫微环境以及T细胞功能调控机制认识的不断深入,对于CAR-T细胞的改造也越来越系统化、多样化,使CAR-T细胞在实体肿瘤的临床治疗中不断取得突破性的进展,CAR-T治疗实体瘤的时代已经到来。未来,邦耀生物将不断加强技术开发,克服行业壁垒进行多管线战略布局和技术整合,力求解决基因和细胞治疗中遇到的核心问题和卡脖子的技术难题,从而为更多遗传疾病、肿瘤疾病(特别是实体肿瘤)及自身免疫疾病等患者带来福音。Cancer Cell综述原文链接:https://doi-org.libproxy1.nus.edu.sg/10.1016/j.ccell.2025.03.019关于邦耀生物上海邦耀生物科技有限公司致力于成为新商业文明时代全球领先的细胞基因药企,邦耀生物以“以基因编辑技术引领创新,开发突破性疗法,造福全人类”为使命,依托自主研发中心及与高校共建的“上海基因编辑与细胞治疗研究中心”,目前已产生100多项专利成果,有19个项目在20余家知名医院开展临床试验,5个项目已获批IND,正式进入注册临床试验阶段,还有多个项目进入IND申报阶段。其中,基因编辑治疗β-地中海贫血症、非病毒定点整合PD1-CAR-T、以及UCAR-T等项目已经取得优异临床效果,具有全球领先性,并在Nature、Cell、Nature Medicine、Nature biotechnology等知名学术期刊上发表多篇学术论文。邦耀生物已搭建基因编辑技术创新平台、造血干细胞平台、非病毒定点整合CAR-T平台、通用型细胞平台、增强型T细胞平台五大具有自主知识产权的技术平台,拥有7000平米GMP中试基地及近100人的运营团队,有力保障创新的研究成果能够快速转化与应用。邦耀生物通过患者需求和临床反馈不断推动研发产品快速更新迭代。并秉持开放、共享、共赢的态度,与全球创新生物医药生态链企业一起,加快推进创新药物的转化与落地,造福全球遗传疾病、恶性肿瘤及自身免疫系统疾病等患者!关于同写意 同写意论坛是中国新药研发行业权威的多元化交流平台,二十一年来共举办会议论坛百余期。“同写意新药英才俱乐部”基于同写意论坛而成立,早已成为众多新药英才的精神家园和中国新药思想的重要发源地之一。同写意在北京、苏州、深圳、成都设立多个管理中心负责同写意活动的运营。尊享多重企业/机构会员特权 ● 分享庞大新药生态圈资源库;● 同写意活动优享折扣;● 会员专属坐席及专家交流机会;● 同写意活动优先赞助权;● 机构品牌活动策划与全方位推广;● 秘书处一对一贴心服务。入会请联系同写意秘书处 同写意创新链盟机构 (上下滑动查看更多)三启生物 | 国通新药 | 通瑞生物 | 科济药业丨立迪生物 | 森西赛智 | 汇芯生物 | 申科生物 | 方拓生物 | 东抗生物 | 科盛达 | 依利特 | 翊曼生物丨锐拓生物丨复百澳生物丨圆因生物丨普洛斯丨华润三九丨皓阳生物丨人福医药丨广生堂药业丨澳宗生物丨妙顺生物 | 荣捷生物丨行诚生物 | 宜联生物 | 生命资本 | 恒诺康丨益诺思 | 深圳细胞谷丨佰诺达生物 | 沃臻生物 | 金仪盛世 | 朗信生物 | 亦笙科技 | 中健云康 | 九州通 | 劲帆医药 | 沙砾生物 | 裕策生物 | 同立海源 | 药明生基 | 奥浦迈 | 原启生物 | 百力司康 | 宁丹新药 | 上海细胞治疗集团 | 滨会生物 | FTA | 派真生物 | 希济生物 | 优睿赛思 | 血霁生物 | 优睿生物 | 邦耀生物 | 华大基因 | 银诺生物 | 百林科医药 | 纳微科技 | 可瑞生物 | 夏尔巴生物 | 金斯瑞蓬勃生物 | 健元医药 | 星眸生物 | 格兰科医药 | 莱羡科学仪器 | 明度智云 | 玮驰仪器 | 康源久远 | 易慕峰 | 茂行生物 | 济民可信 | 欣协生物 | 泰楚生物 | 泰澧生物 | 谱新生物 | 思鹏生物 | 领诺医药 | 宜明生物 | 爱科瑞思 | 阿思科力 | 博格隆生物 | 百吉生物 | 迈邦生物 | 多宁生物 | 万邦医药 | ASCT | 为度生物 | 比邻星创投 | 赛桥生物 | 吉美瑞生 | 荣泽生物 | 科金生物 | 汉超医药 | 康日百奥 | 汉腾生物 | 力品药业 | 安必生 | 博瑞策生物 | 中盛溯源 | 深研生物 | 东方略 | 赛赋医药 | 克睿基因 | 安润医药 | 镁伽科技 | 科锐迈德 | 和元生物 | 申基生物 |楷拓生物| 森松生命科技 | 凯理斯 | 尚德药缘 | 晟国医药 | 健新原力 | 纽福斯 | 华东医药 | 士泽生物 | 影研医疗科技 | 新格元生物 | 依生生物 | 腾迈医药 | 汉欣医药 | 恒驭生物 | 盛诺基 | 序祯达生物 | 乐纯生物 | 速石科技 | 耀海生物 | 新合生物 | 华龛生物 | 恺佧生物 | 成都凡微析 | 正帆科技 | 大橡科技 | 博雅辑因 | 因美纳 | 博雅控股集团 | 近岸蛋白 | 依科赛生物 | 利穗科技 | 东南科仪 | 倍谙基 | 辉诺医药 | 圣诺制药 | 埃格林医药 | 科镁信 | 爱思益普 | 复星医药 | 齐鲁制药 | 捷思英达丨荣昌生物丨泽璟制药丨奕安济世丨礼新医药丨维立志博丨派格生物丨赛生药业丨呈源生物丨启德医药丨双运生物丨宝船生物丨曙方医药丨澳斯康生物丨普莱医药丨维健医药丨海昶生物丨征祥医药丨智核生物丨望石智慧丨博生吉医药丨南京诺丹丨四星玻璃丨艾米能斯丨霁因生物丨普瑞康生物丨映恩生物丨康哲生物丨霍德生物丨海慈药业丨沃生生物丨睿健医药丨矩阵元丨斯微生物丨则正医药丨预立创投丨东立创新丨博安生物丨伟德杰生物丨星奕昂生物丨耀乘健康科技丨琅钰集团丨康德弘翼 | 原力生命科学丨上海科洲丨特瑞思丨药源丨健艾仕生物丨冠科美博丨微境生物丨天境生物丨合源生物丨泛生子丨创胜集团丨加科思药业丨丹诺医药丨凌科药业丨偶领生物丨凯斯艾生物丨成都圣诺丨松禾资本丨清普生物丨和其瑞丨开拓药业丨科兴制药丨玉森新药丨水木未来丨分享投资丨植德律所丨奥来恩丨乐明药业丨东曜药业丨君圣泰丨海创药业丨天汇资本丨再鼎医药丨济煜医药丨百英生物丨基石药业丨君实生物丨Sirnaomics,Inc.丨亦诺微丨博腾股份丨思路迪诊断丨艾博生物丨普瑞金生物丨未知君生物丨尚健生物丨阿诺医药丨有临医药丨赛业生物丨睿智医药丨博济医药丨晶泰科技丨药明康德丨创志科技丨奥星集团丨苏雅医药丨科贝源丨合全药业丨以岭药业丨科睿唯安丨DRG丨博瑞医药丨丽珠医药丨信立泰药业丨步长制药丨华素制药丨众生药业丨上海医药丨高博医疗集团丨药渡丨君联资本丨集萃药康丨诺思格丨精鼎医药丨百利药业丨Pfizer CentreOne丨默克中国创新中心丨奥来恩丨瑞博生物丨新通药物丨广东中润丨医普科诺丨诺唯赞丨康利华丨国信医药丨昆翎丨博纳西亚丨缔脉丨一品红丨和泽医药丨博志研新丨凯莱英医药丨汉佛莱丨英派药业丨京卫制药丨海思科药业丨宏韧医药丨开心生活科技丨哈三联丨Premier Research丨宣泰医药丨先声药业丨海金格丨普瑞盛医药丨Informa丨科特勒丨谋思医药丨HLT丨莱佛士丨辉瑞丨科林利康丨冠科生物丨科文斯丨卫信康丨龙沙(Lonza)丨美迪西丨阳光诺和丨润东医药丨勃林格殷格翰(中国)丨艾苏莱生物丨领晟医疗丨驯鹿医疗丨燃石医学丨中肽生化丨鸿运华宁丨泰格医药丨易迪希丨希麦迪丨百奥赛图丨迪纳利丨青云瑞晶丨鼎丰生科资本丨中源协和丨维亚生物丨青松医药丨中科谱研丨长风药业丨艾欣达伟丨鼎康生物丨中晟全肽丨海步医药丨勤浩医药丨奥萨医药丨太美医疗科技丨生特瑞丨东富龙丨Cytiva丨优辰实验室丨苏桥生物丨君达合创丨澎立生物丨南京澳健丨南京科默丨东阳光丨亚盛医药丨杰克森实验室丨上海科州丨三优生物丨三迭纪丨泰诺麦博丨Cell Signaling Technology丨PPC佳生丨澳斯康丨先为达丨智享生物丨锐得麦丨宜明昂科丨明济生物丨英百瑞丨六合宁远丨天津天诚丨百拓生物丨星药科技丨亓上生物丨真实生物丨引光医药丨方达医药丨高博医疗集团丨赞荣医药丨国投创新丨药明生物丨康哲药业丨高特佳投资丨普瑞基准丨臻格生物丨微谱医药丨和玉资本 | 倚锋资本
免疫疗法细胞疗法临床研究临床结果
2025-04-18
·生物世界
编辑丨王多鱼排版丨水成文尽管嵌合抗原受体(CAR)T 细胞疗法在血液系统恶性肿瘤中取得了巨大成功,但在占据癌症患者绝大多数的实体瘤中的疗效却因多种因素而受限,其中包括抗原异质性和肿瘤微环境(TME)的免疫抑制特性。2025 年 4 月 14 日,华东师范大学刘明耀教授、杜冰教授团队在 Cancer Cell 期刊发表了题为:CAR-T therapy in solid tumors 的综述论文,系统介绍了目前 CAR-T 细胞疗法在多种实体瘤临床研究中的突破性进展,探讨了 CAR-T 细胞疗法在实体瘤中面临的挑战,并对突破实体瘤治疗瓶颈的策略进行了全面总结。CAR-T 细胞疗法在实体瘤治疗中的临床进展:肺癌:EGFR-CAR-T 细胞疗法的中位无进展生存期(PFS)为 7.13 个月,总生存期(OS)达到了 15.63 个月;肝癌:GPC3-CAR-T 细胞疗法显示出 90.9% 的疾病控制率(DCR)和 50% 的客观缓解率(ORR);胃癌:CLDN18.2-CAR-T 细胞疗法显示出 91.8% 疾病控制率(DCR)和 38.8% 的客观缓解率(ORR);前列腺癌:PSMA-CAR-T 细胞疗法将患者前列腺特异性抗原(PSA)水平降低了 95% 以上;卵巢癌:MSLN-CAR-T 细胞疗法将患者的 6 个月总生存率提高到了 70.2%,无进展生存期为 5.8 个月;脑胶质瘤:鞘内给药 EGFR 和 IL13Rα2 靶向的双特异性 CAR-T 细胞,观察到短暂肿瘤消退;B7-H3-CAR-T 细胞疗法的 中位总生存期(OS)达 20.3 个月,12 个月总生存率为 83.3%;GD2-CAR-T 细胞疗法实现了 50% 的部分缓解率(PR)。尽管上述创新性 CAR-T 细胞疗法在少数实体瘤患者中展示出了治疗潜力,但其整体的临床疗效仍有待提升。随后作者分析了 CAR-T 细胞治疗实体瘤面临的挑战,四大瓶颈亟待突破:1、T 细胞耗竭:长期对抗肿瘤导致 CAR-T 细胞抗肿瘤活性下降;2、误伤正常细胞:部分肿瘤靶点在正常组织中也有表达,引起 On-target off-tumor 毒性;3、免疫抑制性的肿瘤微环境:实体瘤微环境缺氧、营养匮乏,且充满抑制免疫的细胞和分子,例如 TGFβ 等抑制 CAR-T 细胞的免疫反应;4、CAR-T 细胞难迁移并浸润:实体瘤具备纤维组织的物理屏障,加之趋化因子表达匮乏,不利于 CAR-T 细胞的定位和浸润。图1. CAR-T疗法在实体瘤中的挑战作者对优化并提升 CAR-T 细胞治疗实体瘤的相关研究进展进行了归纳与总结,系统地提出了 5 大创新升级方案,让 CAR-T 细胞疗法更精准、更安全:1、智能设计 CAR 结构引入“双靶点”技术(例如 GD2+B7-H3),降低误伤风险;整合 CAR-T 和 TCR-T 技术,开发“STAR-T”新型受体,提升肿瘤识别灵敏度。2、增强 CAR-T 细胞功能过表达 IL-10、FOXO1 等因子,增强细胞持久性和杀伤力;基因编辑技术敲除耗竭相关基因(例如 NR4A),延长 CAR-T 细胞存活时间。3、革新 CAR-T 细胞生产工艺现货通用型 CAR-T 可实现“即取即用”,大大缩短制备周期的同时,也有效降低了生产成本。非病毒定点整合技术改造细胞,提升安全性,避免基因插入错误风险。4、瓦解肿瘤免疫微环境装载“定位信号”(例如 IL-7/CCL19),引导细胞深入肿瘤内部,增强对肿瘤细胞的杀伤。改造 CAR-T 分泌 LIGHT、肝素酶,可实现破坏肿瘤外部屏障或重塑肿瘤异常的脉管系统。5、提升 CAR-T 治疗安全性双靶点 CAR-T 细胞的设计与改造,以降低中靶脱瘤毒性;引入“安全开关”及时控制副作用,阻断细胞因子风暴(CRS)关键通路。图2. 克服实体瘤障碍的策略总的来说,在这篇综述中,作者探讨了针对实体瘤的 CAR-T 细胞疗法在临床研究方面取得的进展以及所面临的挑战。为了提高 CAR-T 细胞在实体瘤中的疗效,研究人员探索了诸如增强 T 细胞持久性和细胞毒性、靶向多种抗原以及利用创新的同种异体 CAR-T 细胞制造等策略。此外,该综述还强调了将 CAR-T 细胞疗法与免疫检查点抑制剂及其他治疗手段相结合的潜在益处,以克服肿瘤微环境(TME)的限制。最后,作者表示,对于 CAR-T 细胞疗法在实体瘤中的未来持乐观态度,但还需要持续开展研究以优化治疗方案,并满足癌症患者的临床需求。原文链接:https://www-cell-com.libproxy1.nus.edu.sg/cancer-cell/abstract/S1535-6108(25)00120-5设置星标,不错过精彩推文开放转载欢迎转发到朋友圈和微信群 微信加群 为促进前沿研究的传播和交流,我们组建了多个专业交流群,长按下方二维码,即可添加小编微信进群,由于申请人数较多,添加微信时请备注:学校/专业/姓名,如果是PI/教授,还请注明。点在看,传递你的品味
细胞疗法免疫疗法临床结果临床研究
2025-04-18
近年来,嵌合抗原受体T细胞疗法(CAR-T)在恶性血液肿瘤中展现出的强大实力,使其逐渐成为最有前景的肿瘤免疫疗法,然而血液肿瘤(非实体瘤)仅仅是众多癌症中较小的一部分。根据2024年世界卫生组织国际癌症研究机构(IARC)在学术期刊CA: A Cancer Journal for Clinicians发布的2022年全球癌症负担数据显示,约90%的癌症发病率都是由实体瘤引起,全球癌症发病率和死亡率排名TOP5的癌症也均为实体肿瘤,而关于实体瘤的细胞治疗临床试验却相对较少,可见实体瘤未被满足的临床治疗需求巨大。
2025年4月18日,聚焦于基因和细胞治疗的上海邦耀生物科技有限公司(以下简称“邦耀生物”)宣布,邦耀生物联合华东师范大学刘明耀教授、杜冰教授领衔的科研团队近日在国际顶级期刊Cancer Cell上发表了题为“CAR-T therapy in solid tumors”的综述文章,系统总结了CAR-T细胞疗法在实体瘤领域的突破性进展,深入剖析当前挑战,并提出多维度创新策略。该综述为全球实体瘤免疫治疗研究提供了重要方向,标志着CAR-T技术向实体瘤全面进军迈出关键一步。
突破性成果:从实验室到临床,实体瘤治疗曙光初现
CAR-T疗法在血液肿瘤中已创造“治愈奇迹”,但在实体瘤中仍面临巨大挑战。在本综述中,研究团队首先汇总了全球多种实体瘤临床数据,并阐述了多项针对不同靶点的CAR-T细胞在治疗实体瘤中所取得的突破性进展:
肺癌:相较于传统治疗手段,靶向EGFR的CAR-T细胞将患者的中位生存期提升至15.63个月。 肝癌、胃癌:分别接受GPC3-CAR-T和CLDN18.2-CAR-T治疗后,实现了90%疾病控制率。 前列腺癌:PSMA-CAR-T治疗后,可将患者前列腺特异性抗原(PSA)水平下降超95%以上。 卵巢癌、脑胶质瘤:MSLN-CAR-T和GD2-CAR-T分别治疗后,实现70.2%(6个月生存率)和83.3%(12个月生存率)的显著疗效。
肺癌:相较于传统治疗手段,靶向EGFR的CAR-T细胞将患者的中位生存期提升至15.63个月。
肝癌、胃癌:分别接受GPC3-CAR-T和CLDN18.2-CAR-T治疗后,实现了90%疾病控制率。
前列腺癌:PSMA-CAR-T治疗后,可将患者前列腺特异性抗原(PSA)水平下降超95%以上。
卵巢癌、脑胶质瘤:MSLN-CAR-T和GD2-CAR-T分别治疗后,实现70.2%(6个月生存率)和83.3%(12个月生存率)的显著疗效。
尽管这些创新性CAR-T疗法在少数实体瘤患者中展示出了治疗潜力,但其整体的临床疗效仍有待提升。随后研究团队分析了CAR-T细胞治疗实体瘤面临的挑战,四大瓶颈亟待突破:
(1)T细胞“疲劳”:长期对抗肿瘤导致CAR-T细胞活性下降。
(2)误伤正常细胞:部分肿瘤靶点与正常组织相似,可能引发副作用。
(3)免疫抑制的肿瘤环境:实体瘤微环境缺氧、营养匮乏,且充满抑制免疫的细胞和分子,如TGFβ等抑制CAR-T细胞的免疫反应。
(4)CAR-T细胞难迁移并浸润:实体瘤具备纤维组织的物理屏障,加之趋化因子表达匮乏,不利于CAR-T细胞的定位和浸润。
图1. CAR-T疗法在实体瘤中的挑战
最后,研究团队对优化并提升CAR-T细胞治疗实体瘤的相关研究进展进行了归纳与总结,系统地提出了5大创新升级方案,让CAR-T疗法更精准、更安全:
智能设计CAR结构
引入“双靶点”技术(如GD2+B7-H3),降低误伤风险。 整合CAR-T和TCR-T技术,开发“STAR-T”新型受体,提升肿瘤识别灵敏度。
引入“双靶点”技术(如GD2+B7-H3),降低误伤风险。
整合CAR-T和TCR-T技术,开发“STAR-T”新型受体,提升肿瘤识别灵敏度。
增强CAR-T细胞功能
过表达IL-10、FOXO1等因子,增强细胞持久性和杀伤力。 基因编辑技术敲除耗竭相关基因(如NR4A),延长CAR-T存活时间。
过表达IL-10、FOXO1等因子,增强细胞持久性和杀伤力。
基因编辑技术敲除耗竭相关基因(如NR4A),延长CAR-T存活时间。
革新CAR-T细胞生产工艺
现货通用型CAR-T可实现“即取即用”,大大缩短制备周期的同时,也有效降低了生产成本。 非病毒定点整合技术改造细胞,提升安全性,避免基因插入错误风险。
现货通用型CAR-T可实现“即取即用”,大大缩短制备周期的同时,也有效降低了生产成本。
非病毒定点整合技术改造细胞,提升安全性,避免基因插入错误风险。
瓦解肿瘤免疫微环境
装载“定位信号”(如IL-7/CCL19),引导细胞深入肿瘤内部,增强对肿瘤细胞的杀伤。 改造CAR-T分泌LIGHT、肝素酶,可实现破坏肿瘤外部屏障或重塑肿瘤异常的脉管系统。
装载“定位信号”(如IL-7/CCL19),引导细胞深入肿瘤内部,增强对肿瘤细胞的杀伤。
改造CAR-T分泌LIGHT、肝素酶,可实现破坏肿瘤外部屏障或重塑肿瘤异常的脉管系统。
提升CAR-T治疗安全性
双靶点CAR-T细胞的设计与改造,以降低中靶脱瘤毒性。 引入“安全开关”及时控制副作用,阻断细胞因子风暴(CRS)关键通路。
双靶点CAR-T细胞的设计与改造,以降低中靶脱瘤毒性。
引入“安全开关”及时控制副作用,阻断细胞因子风暴(CRS)关键通路。
图2. 克服实体瘤障碍的策略
从“可能”到“可行”,CAR-T开启实体瘤治疗新时代
作为本篇综述共同作者,邦耀生物创始人&董事长刘明耀教授表示:“随着基因编辑、合成生物学与临床转化的深度融合,CAR-T完全有望成为实体瘤治疗的‘终极武器’。”
邦耀生物作为全球领先的细胞基因药企,在细胞治疗实体瘤领域也实现了多项突破性进展,不但打造了具有自主知识产权的增强型T细胞平台(HyperTCell®),其主要通过T细胞的基因改造来攻克实体瘤治疗的世界难题。于2025年1月,邦耀生物科研团队还在Molecular Therapy杂志最新发文,开发出了一种创新型CAR-T细胞“GITRL-PSMA-CAR-T”不仅可以直接增强CAR-T细胞的抗肿瘤活性,还可以促进其在实体肿瘤微环境中的持久性,进一步提升了CAR-T对实体肿瘤的治疗效果,有望加速实现实体瘤CAR-T疗法的开发与应用。不得不说,近年来随着对肿瘤免疫微环境以及T细胞功能调控机制认识的不断深入,对于CAR-T细胞的改造也越来越系统化、多样化,使CAR-T细胞在实体肿瘤的临床治疗中不断取得突破性的进展,CAR-T治疗实体瘤的时代已经到来。
未来,邦耀生物将不断加强技术开发,克服行业壁垒进行多管线战略布局和技术整合,力求解决基因和细胞治疗中遇到的核心问题和卡脖子的技术难题,从而为更多遗传疾病、肿瘤疾病(特别是实体肿瘤)及自身免疫疾病等患者带来福音。
Cancer Cell综述原文链接:https://doi-org.libproxy1.nus.edu.sg/10.1016/j.ccell.2025.03.019
免疫疗法细胞疗法临床研究临床结果
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
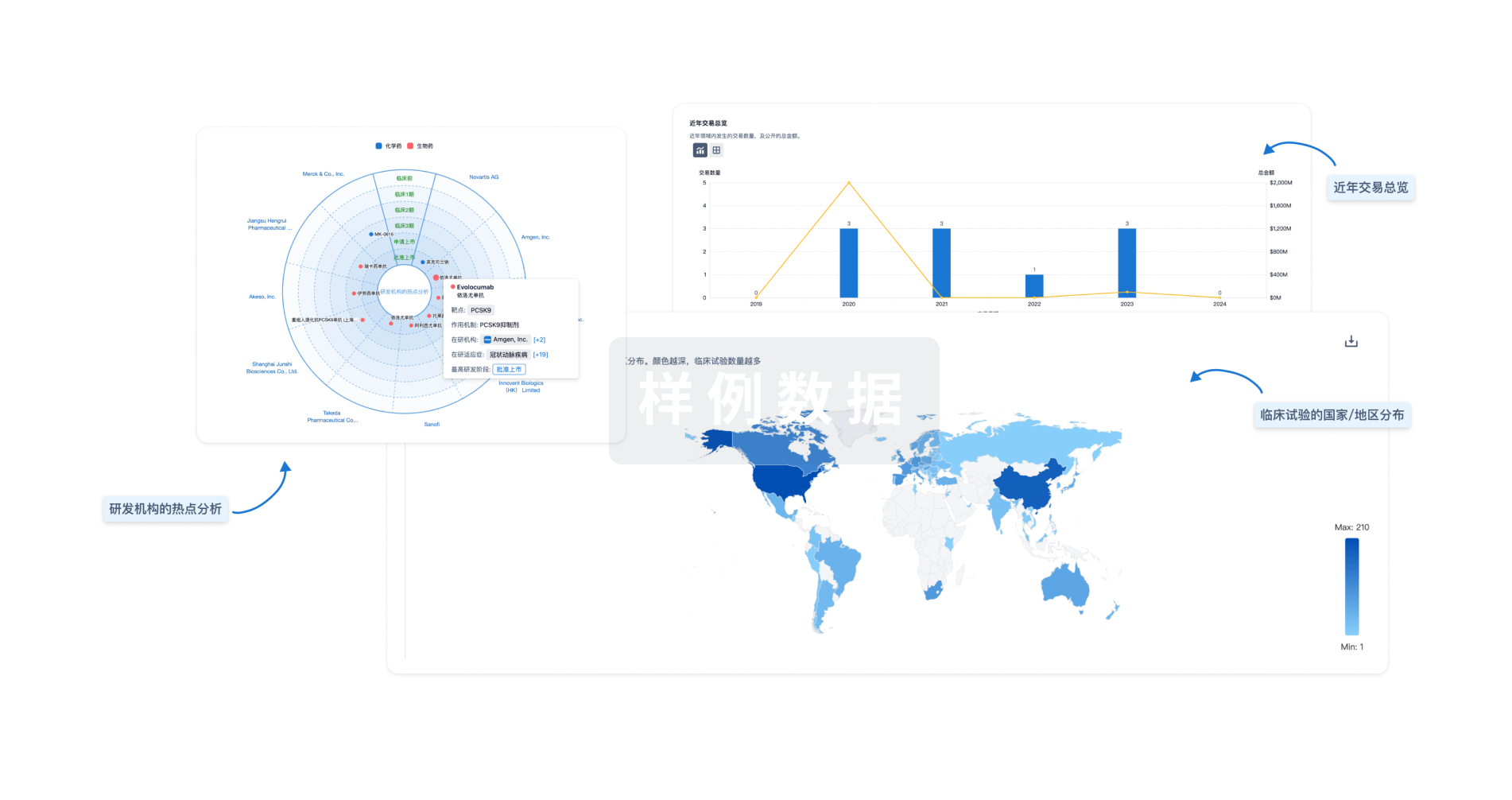
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

