预约演示
更新于:2025-05-07
NY-ESO-1
更新于:2025-05-07
基本信息
别名 Autoimmunogenic cancer/testis antigen NY-ESO-1、Cancer/testis antigen 1、Cancer/testis antigen 6.1 + [11] |
简介- |
关联
94
项与 NY-ESO-1 相关的药物靶点 |
作用机制 NY-ESO-1调节剂 |
在研机构 |
原研机构 |
最高研发阶段临床2/3期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点 |
作用机制 NY-ESO-1调节剂 |
在研适应症- |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点 |
作用机制 NY-ESO-1调节剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
127
项与 NY-ESO-1 相关的临床试验NCT06748872
EPITOME-1015-I: a Phase I Study to Investigate the Safety, Tolerability and Preliminary Efficacy of a Third Generation TCR-T Therapy, MDG1015, in Epithelial Ovarian Carcinoma, Gastroesophageal (Junction) Adenocarcinoma, Myxoid (Round Cell) Liposarcoma And/or Synovial Sarcoma Subjects with Advanced Disease Expressing NY-ESO-1 And/or LAGE-1a
MDG1015 is a third generation TCR-T therapy product targeting NY-ESO-1/LAGE-1a armored and enhanced by the PD1-41BB costimulatory switch protein (CSP). The study purpose is to establish the safety, tolerability and preliminary efficacy of MDG1015 in patients with epithelial ovarian cancer, gastroesophageal adenocarcinoma, round cell liposarcoma and/or synovial sarcoma that expresses NY-ESO-1 and/or LAGE-1a.
The main questions this clinical trial aims to answer are:
Can this TCR-T therapy MDG1015 be given to patients safely? What is the optimal dose of the TCR-T therapy MDG1015? If and what side effects do participants experience after receiving the TCR-T therapy MDG1015? Do participants experience a potential disease response after receiving the TCR-T therapy MDG1015?
Participants will:
Receive (in most cases) 1 single infusion of MDG1015 at a pre-defined dose level and will be followed up regularly up to 1 year. After one year, participants will enter the long term follow-up part up to 15 years after being treated. Any side effects and/or potential disease response will be documented during this period.
The main questions this clinical trial aims to answer are:
Can this TCR-T therapy MDG1015 be given to patients safely? What is the optimal dose of the TCR-T therapy MDG1015? If and what side effects do participants experience after receiving the TCR-T therapy MDG1015? Do participants experience a potential disease response after receiving the TCR-T therapy MDG1015?
Participants will:
Receive (in most cases) 1 single infusion of MDG1015 at a pre-defined dose level and will be followed up regularly up to 1 year. After one year, participants will enter the long term follow-up part up to 15 years after being treated. Any side effects and/or potential disease response will be documented during this period.
开始日期2025-07-01 |
申办/合作机构 |
NCT06942143
An Open-label, Phase I Clinical Trial of Autologous T Cells Transduced With NY-ESO-1 Antigen-specific High-affinity T Cell Receptors in NY-ESO-1-positive Patients With Advanced Solid Tumors
This study was a phase I safety and tolerability clinical trial conducted in a single-center, open-label, 3+3 design with dose escalation.
开始日期2025-04-23 |
申办/合作机构  广州泛恩生物科技有限公司 广州泛恩生物科技有限公司 [+1] |
NCT06552416
A Phase 1 Study of Allogenic Off-the-Shelf Multi-Tumor-Associated Antigen-Specific T Cell Products (MT-401-OTS) Administered to Patients with Relapsed Acute Myeloid Leukemia or Myelodysplastic Syndromes (RAPID)
This study is a Phase 1 multicenter, open-label study evaluating the safety and efficacy of escalating doses of MT-401-OTS in 2 participant populations: 1) Those with intermediate or high-risk AML per 2022 ELN criteria who have evidence of MRD and/or
开始日期2025-01-15 |
申办/合作机构 |
100 项与 NY-ESO-1 相关的临床结果
登录后查看更多信息
100 项与 NY-ESO-1 相关的转化医学
登录后查看更多信息
0 项与 NY-ESO-1 相关的专利(医药)
登录后查看更多信息
1,479
项与 NY-ESO-1 相关的文献(医药)2025-05-01·International Journal of Clinical Oncology
Treatment strategies for advanced synovial sarcoma: from chemotherapy to TCR-engineered T-cell therapy
Review
作者: Hasegawa, Masahiro ; Nakamura, Tomoki
2025-04-01·Cancer Medicine
Expression of Cancer‐Testis Antigens MAGE ‐A1 , MAGE ‐A4 , NY ‐ESO ‐1 and PRAME in Bone and Soft Tissue Sarcomas: The Experience From a Single Center in China
Article
作者: Wang, Xiaolu ; Li, Lin ; Yu, Lixia ; Yen, Ying‐Tzu ; Liu, Fangcen ; Wei, Zijian ; Wang, Chun ; Li, Rutian ; Chen, Anni ; Qiu, Yuling ; Li, Chunhua
2025-03-01·Journal for ImmunoTherapy of Cancer
mTOR inhibition modulates vaccine-induced immune responses to generate memory T cells in patients with solid tumors
Article
作者: Hutson, Alan ; Chodon, Thinle ; Keler, Tibor ; Long, Mark ; Lele, Shashikant B ; Liu, Song ; Yan, Li ; Shrikant, Protul ; Tsuji, Takemasa ; Odunsi, Kunle ; Matsuzaki, Junko ; Withers, Henry G ; Zsiros, Emese ; Bhardwaj, Nina ; Rosario, Spencer R ; Lugade, Amit ; Blank, Stephanie ; Koya, Richard ; Wang, Jianming
259
项与 NY-ESO-1 相关的新闻(医药)2025-04-30
·药学进展
“点击蓝字 关注我们潘国宇上海微知卓生物科技有限公司董事长,中国科学院上海药物研究所研究员,中国药科大学博士。曾在美国波士顿诺华研究院担任高级研究员,回国后就职于中国科学院上海药物研究所,从事药物肝脏代谢、毒性机制和细胞治疗等研究工作,发表SCI期刊学术论文50余篇。现为中国药物代谢委员会委员、中国细胞治疗研究与应用协会常任理事、国家“生物人工肝”重大专项首席科学家。创立微知卓公司后,主要进行肝脏疾病的细胞治疗、生物人工肝临床转化研究。人多能干细胞国际标准与国内团体标准的对比解析 PPS 王莹1,田娥1,周冰洁1,郭新颖1,潘国宇1,2*(1.上海微知卓生物科技有限公司,上海 200135;2.中国科学院上海药物研究所,上海 201203)[摘要]干细胞研究和产业化是当今生物医学基础研究和成果转化领域前沿方向之一,然而国内外研究和转化标准并不统一。介绍了多能干细胞的定义与研究概况,并对国际干细胞研究学会(ISSCR)发布的《人干细胞基础研究标准》以及中国细胞生物学学会发布的《人胚干细胞》与《人诱导多能干细胞》团体标准进行介绍和比较分析,旨在为我国干细胞基础研究和产品转化提供参考。1引言2023年6月,国际干细胞研究学会(ISSCR)发布了《人干细胞基础研究标准》(Standards for Human Stem Cell Use in Research)[1],该项国际学术团体标准为从事人类干细胞研究的相关人员制定了基础的研究标准;中国细胞生物学学会在2019年发布《人胚干细胞》团体标准[2](2020年修订),2021年发布了《人诱导多能干细胞》团体标准[3]。前者针对干细胞研究初步规划直至论文发表这一过程中应完成的研究活动进行了建议;后者对干细胞研究走向产业化的过程中生产和检测的重要考察指标进行了规范化建议。尽管国内外科研和产业化背景差异较大,标准的受众关注点却有交叉。例如,在美国,科研工作者完成研究工作后,往往以与公司合作的方式进行产业转化,其标准虽被标注为研究而设计,但也考虑了后续产业化的需求;而在我国,干细胞研究的产业化工作很多是由基础科研人员主导,因此我国现阶段制定的产业化干细胞研究标准往往有浓厚的科研痕迹。此外,ISSCR发布的《人干细胞基础研究标准》的制定有我国科技工作者的深度参与,该标准的基本逻辑和我国的两项团体标准具有相通之处。本文介绍了多能干细胞的基本定义,国内外临床研究进展,法规、伦理的演进和发展侧重点,并对上述3项干细胞标准的制定背景、主要内容和使用场景进行对比,分析异同产生的原因,旨在为我国干细胞研究工作提供参考。2多能干细胞的定义和研究概况多能干细胞主要包括诱导多能干细胞(iPSC)和胚胎干细胞(ESC)。iPSC是将多个转录因子导入到成熟体细胞中,并使其重编程为具有类似胚胎干细胞特征的细胞;ESC是从早期胚胎的内部细胞团(ICM)中分离出来的细胞。尽管人ESC(hESC)在临床上展现出比iPSC更好的效果,但由于hESC来源于人类胚胎,其应用受到了限制。相比之下,iPSC免疫原性较低,可降低免疫排斥风险,且减少了干细胞研究在伦理方面的争议,在再生医学、疾病建模、药物开发以及细胞治疗等领域应用广泛[4]。截至2024年3月,ClinicalTrials.gov上检索到的有关iPSC的临床试验有164项,主要集中在神经系统疾病[5]、心血管疾病[6]、代谢性疾病[7-10]、眼科疾病[11]和癌症等领域[12-14]。由CynataTherapeutics开发的用于治疗骨关节炎的CYP-004是全球首个进入Ⅲ期临床的iPSC衍生产品。目前共有48项注册的临床试验将源于hESC的细胞用于各类疾病的治疗,其中,有24项试验基于hESC来源的视网膜色素上皮细胞治疗黄斑变性;4项试验将hESC分化为间充质干细胞(MSC)或MSC样细胞并用于治疗多发性硬化症、间质性膀胱炎、原发性卵巢功能不全以及半月板损伤;4项试验将hESC分化为胰腺祖细胞或胰腺上皮细胞并用于1型糖尿病治疗;其余试验将hESC分化后的细胞用于治疗慢性缺血性左心室功能不全、脊髓损伤、帕金森病、缺血性脑卒中等。首个与hESC相关的临床试验注册于2002年。2012年以后,hESC相关临床试验注册数量显著上升。目前,注册数量最多的是美国,其次是中国。与眼科疾病相关的hESC临床试验占比最高,其次是神经系统疾病,以Ⅰ期或Ⅰ/Ⅱ期临床试验为主[15]。目前,多能干细胞治疗疾病的相关探索正在进行中。在临床前阶段,多能干细胞已经被成功分化为多种类型细胞,且其疗效已在动物模型中得到了验证。多项基于多能干细胞治疗疾病的临床试验已启动。尽管已取得显著进展,但多能干细胞仍存在一些问题。Yamanaka[16]在2020年的综述中提到了多能干细胞治疗面临的3个主要挑战:安全性、免疫原性和异质性。除了技术方面的挑战,干细胞研究还会面临伦理问题。hESC通常来自体外受精(IVF)程序捐赠的剩余胚胎。在符合人类利益如治疗疾病的情况下,我国支持对人类胚胎和hESC进行研究。因此2003年我国发布的《人胚胎干细胞研究伦理指导原则》明确规定研究人员在hESC及iPSC的获取、改造与应用过程中应认真对待捐献者的知情同意情况、福利和权利以及潜在风险和益处等,并严格按照伦理指导原则中的要求执行。除了道德伦理上的考虑,人类胚胎的法律地位可能也会影响胚胎和干细胞研究政策和法规。根据我国法律,人类胚胎不被视作一个人,但人的胚胎是介于人与物质之间的特殊物质,它应该比无生命的物体具有更高的道德伦理地位,应该得到特殊的尊重和保护。《人胚胎干细胞研究伦理指导原则》自发布施行至今已有20年未更新,若干细胞伦理政策导向在未来有所变化,将会对该研究领域相关法律法规产生深远影响。此外,在2019年之前,我国对胚胎干细胞相关研究不予专利保护。直到2019年4月,国家知识产权局对外公布了《专利审查指南修改草案(征求意见稿)》,其中修改了人胚胎干细胞相关规定,不再对“未经过体内发育的受精14天以内的人类胚胎分离或者获取干细胞技术”的专利保护以专利法第5条为由完全排除,同时明确人胚干细胞不属于处于各个发育阶段的人体。随着干细胞研究领域的发展,国内外均对干细胞专利适用性做出调整,《专利审查指南》的修改体现了我国鼓励再生医疗技术领域发展、支持干细胞技术专利保护的政策动向,旨在激励干细胞研究的创新。3国际干细胞研究学会标准与国内干细胞团体标准的比较我国细胞治疗技术发展迅速,在这一过程中需要制定统一标准并对产品进行监督管理。2019年中国细胞生物学学会发布了《人胚胎干细胞》团体标准[17],2020年修订了该团体标准,更名为《人胚干细胞》[2]。2021年中国细胞生物学学会发布《人诱导多能干细胞》团体标准[3]。以上两项标准规定了人多能干细胞的技术要求、检测方法、使用说明、标签、包装、存储、运输和废弃物处理要求,适用于人多能干细胞的生产和检测。2023年6月,ISSCR发布了《人干细胞基础研究标准》。该标准主要确定了成体干细胞和多能干细胞的实验室使用的质量标准,内容共分为5个部分:第一部分介绍了人类干细胞获取/生成、保存和早期表征的关键原则;第二部分介绍如何定义和表征人类多能干细胞;第三部分提倡监测干细胞在储存和培养过程中是否发生了遗传变化;第四部分主要阐述提高模型系统在基础研究中的实用性的方式;第五部分重点强调了涉及多能干细胞或组织干细胞的论文中应报告的必要细节。以下将对ISSCR标准与国内干细胞团体标准进行比较。3.1 国际干细胞研究学会标准与国内干细胞团体标准的相同点ISSCR标准与国内干细胞团体标准对多能干细胞研究与生产过程中涉及的多个关键步骤以及质量属性提出了类似的建议。3.1.1 细胞原材料获取 3项标准均要求对细胞原材料进行人类病毒病原体[包括Ⅰ型人免疫缺陷病毒(HIV-Ⅰ)、Ⅱ型人免疫缺陷病毒(HIV-Ⅱ)、乙型肝炎病毒(HBV)和丙型肝炎病毒(HCV)等]筛查。多能干细胞构建成功后也需进行微生物检测,包括真菌、细菌、支原体、HIV-Ⅰ、HIV-Ⅱ、HBV、HCV、人类T细胞白血病病毒(HTLV)、爱泼斯坦-巴尔病毒(EBV)、人类巨细胞病毒(HCMV)和梅毒螺旋体(TP),这些病原体均应为阴性。国内干细胞团体标准规定在获取细胞原材料并进行研究时应遵守《T/CSCB0001干细胞通用要求》[19]。另外,研究人员构建及使用人胚干细胞时还应遵守2003年发布的《人胚胎干细胞研究伦理指导原则》[18]。ISSCR标准强烈建议原材料获取时必须遵守国内法律法规,但理想情况下,还应验证是否符合ISSCR等相关机构提出的国际原则《ISSCR干细胞研究和临床转化指南:2021年更新》(ISSCR Guidelines for Stem Cell Research and Clinical Translation: The 2021 update)。国内干细胞通用标准要求干细胞的来源应符合研究者所在国认可的伦理和当地的法律法规,材料获取前应严格审查。干细胞材料供者应签署书面合法有效的知情同意书,以保护受试者的隐私等。并且,国际以及国内干细胞指导原则均明确规定:1)研究者禁止进行生殖性克隆人任何研究;2)用于研究的人胚胎干细胞只能来源于体外受精时多余的配子或囊胚,自然或自愿选择流产得到的胎儿细胞,体细胞核移植技术所获得的囊胚和单性分裂囊胚,自愿捐献的生殖细胞;3)利用体外受精、体细胞核移植、单倍体复制技术或遗传修饰获得的囊胚,其体外培养期限自受精或核移植开始不得超过14天;4)不得将人的生殖细胞与其他物种的生殖细胞结合。3.1.2 定义和表征人类多能干细胞 3项标准均建议检测未分化多能干细胞表达的细胞表面标记物,如阶段特异性胚胎抗原(SSEA)3、SSEA4、TRA-1-60、TRA-1-81等。ISSCR标准强烈建议进行短串联重复序列(STR)分析来鉴定染色体核型。国内干细胞团体标准也明确规定细胞产品STR检测结果应与供者细胞保持一致,外源重编程基因检测结果应为阴性。3.1.3 细胞存储 ISSCR标准建议使用双生物库系统并在场外保护部分具有特征的主细胞库(MCB),以防止当地灾难性事件造成的损失。国内干细胞团体标准及其相关参考标准同样提议,为防止不可抗性因素所导致的损坏或丢失,应将同一来源的细胞进行“镜像保存”(即分成若干份,分放不同区域的不同容器中长期保存)。3.1.4 其他方面 ISSCR发布的《人干细胞基础研究标准》对使用干细胞构建细胞疾病模型提出相关建议,包括:应尽早表征材料的来源组织或细胞;在当地法规允许的情况下,应考虑捐赠者的性别、年龄、种族和遗传背景、健康状况、风险因素以及任何其他临床体征或症状;在将疾病模型与健康对照进行比较时,应明确界定“健康”的含义等。另外,在涉及多能干细胞或组织干细胞的论文中应报告的必要细节,包括细胞系的来源或其衍生的细胞系、干细胞维持和保存的方法以及传代次数的注册号等。论文中应彻底描述细胞多能性和未分化状态的测试,包括测定方法、试剂来源、数据、定量和统计分析,并应指出细胞系培养过程中进行测定的时间点。3.2国际干细胞研究学会标准与国内干细胞团体标准 的主要不同点ISSCR标准与国内干细胞团体标准在人类多能干细胞原材料获取、人类多能干细胞的定义和表征、细胞标签内容的规范,以及废弃物处理方面均有所不同,表1对此进行了初步梳理和分析。4讨论ISSCR的《人干细胞基础研究标准》主要针对干细胞研究活动提供了建议和指导,内容涵盖获取干细胞要求、干细胞培养时的监测以及最终论文发表等方面。《人诱导多能干细胞》团体标准和《人胚干细胞》团体标准较为相似,主要对产业化过程中干细胞产品的生产和检测重要考察指标进行规范化建议。这种差异和两类标准的制定目的有关。ISSCR的《人干细胞基础研究标准》主要针对欧美干细胞工作者提供科研方面的基础指导。在欧美国家,尤其是美国,科研工作者完成研究工作后,也会进行产业转化,但是产品后期开发主要以公司形式完成,因此产业化初期阶段只要考虑产业化的基本需求即可。而在我国,许多干细胞研究由基础科研人员主导,一旦有所突破,往往是由基础科学家直接开展临床研究,尤其是医疗机构的科研人员会独立开展“前店后厂”式的科研服务(参考国家卫生健康委员会于2015年颁布的《干细胞临床研究管理办法(试行)》),产业化进程和科研进程是同步进行的。因此我国现阶段制定的干细胞研究标准规范基于对科研工作者的研究要求,同时又包含产业化的许多具体要求。建议科研人员根据自己的实际需求,在工作中灵活运用不同标准来指导工作。国际方面,以Fatetherapeutics产品——iPSC来源T细胞的研究为例。产品从获取供体细胞开始构建完整的动态药品生产管理规范(current Good Manufacture Practices,cGMP)iPSC细胞系,获取时遵循相关的ISSCR指南,包括请供体签署书面和合法有效的知情同意书。为确保iPSC主产物的质量(如无菌性和遗传稳定性等),需按ISSCR标准建立质量控制测试和放行标准[22]。国内方面,以中盛溯源研制的iPSC来源自然杀伤细胞(NK)产品为例。该产品使用的干细胞库的构建,以及生产质量控制均须按国内干细胞团体标准规定执行,包括染色体核型、STR分析、细胞标志物检测、无菌检测、支原体检测、内毒素检测、病原体检测、畸胎瘤形成以及三胚层分化检测等。需要指出的是,国内外标准仅为相关从业人员提供最基础的必须遵守的标准,以确保研究和应用的安全性和有效性。ISSCR发布的《人干细胞基础研究标准》其基本逻辑与我国的两项团体标准具有许多相通之处,这是因为此标准的制定有我国科技工作者的深度参与。我国两项干细胞团体标准的前期经验,为该标准的制定提供了宝贵经验。这充分说明,我国科学研究与世界联系已非常紧密,随着我国科研的迅速发展,我国科技工作者在世界上的声音会越来越响亮。根据《“健康中国2030”规划纲要》,干细胞技术被视为医学前沿技术的重点发展方向之一。未来干细胞技术将在技术研发和转化方面取得更多突破,推动临床应用的进展。随着技术进步和市场需求的增长,干细胞治疗产业链的各个环节都将得到进一步的发展和完善。国家高度重视干细胞行业的发展,并多次提出大力发展干细胞技术,预计未来将有更多的政策支持,包括资金投入、税收优惠等,以促进干细胞技术的研究和产业化。目前,干细胞产品按药品进行管理,形成了药品监管部门、卫生健康管理部门“双重监管”的管理体系。许多企业在进行药品临床试验注册申请前,已与医疗机构合作开展了临床研究。药品审评中心(CDE)于2017年发布《细胞治疗产品研究与评价技术指导原则(试行)》,对细胞治疗产品按照药品管理相关法律法规进行研发时的技术要求进行了总体阐述。CDE于2023年发布了《人源干细胞产品药学研究与评价技术指导原则(试行)》《人源性干细胞及其衍生细胞治疗产品临床试验技术指导原则(试行)》,2024年发布了《人源干细胞产品非临床研究技术指导原则》,上述指导原则的发布表明我国干细胞产品监管标准逐步完善,也为企业后续按照药品注册路径申报临床试验所涉及的研究活动提供了政策依据以及指引。附录:中国干细胞相关标准的发展历程近年来,我国科研技术不断创新突破,国家政策逐渐深入引导,我国干细胞技术快速发展,深受国际的认可。我国研究者是国际科技研究和转化应用领域第一阵营的主要力量之一,参与制定的指导原则、标准以及法规为从事干细胞研究的国内外同行规定了多能干细胞的建系培养、生物学特性鉴定、质量控制、信息管理、分发和运输等方面的要求。科技部和卫生部于2003年联合发布《人胚胎干细胞研究伦理指导原则》[18],中国细胞生物学会于2017年8月发布《干细胞通用要求》团体标准[19],2020年发布《人胚干细胞》团体标准修订版[2],2021年1月发布《人诱导多能干细胞》团体标准[3],2022年8月发布《人干细胞研究伦理审查技术规范》团体标准[21],这些标准为国内从事多能干细胞研究的全体成员提供了生产、检测和质量控制以及伦理审查的标准,推动了我国干细胞领域标准化与规范化发展。2022年10月,我国研究者牵头制定了国际标准《人和小鼠多能性干细胞通用要求(ISO24603)》[21],这是国际标准化组织生物技术委员会的第一个干细胞标准,也是全球首个干细胞国际标准,标志着我国干细胞基础和转化研究以及标准建设走在国际前列。致谢:特别感谢中国科学院上海生命科学院上海生物化学和细胞研究所惠利健教授,中国科学院动物研究所赵同标教授、郝捷教授等提出的宝贵意见。参考文献:[1] International Society for Stem Cell Research. Standards for Human Stem Cell Use in Research[EB/OL]. (2023-06-06)[2023-08-10]. https://www.isscr.org/basic-research-standards.[2] 中国细胞生物学学会 . T/CSCB 0002—2020《人胚干细胞》团体 标准 [S]. 北京 : 中国标准出版社, 2020.[3] 中国细胞生物学学会 . T/CSCB 0005—2021《人诱导多能干细胞》 团体标准 [S]. 北京 : 中国标准出版社, 2021.[4] Karagiannis P, Takahashi K, Saito M, et al. Induced pluripotent stem cells and their use in human models of disease and development[J]. Physiol Rev, 2019, 99(1): 79-114.[5] Bassil R, Shields K, Granger K, et al. Improved modeling of human AD with an automated culturing platform for iPSC neurons, astrocytes and microglia[J]. Nat Commun, 2021, 12(1): 5220. DOI:10.1038/s41467-021-25344-6.[6] Zimmermann W H, Tissue engineered heart repair from preclinical models to first-in-patient studies[J]. Curr Opin Physiol, 2020, 14: 70- 77.[7] Csobonyeiova M, Polak S, Danisovic L. Generation of pancreatic β-cells from iPSCs and their potential for type 1 diabetes mellitus replacement therapy and modelling[J]. Exp Clin Endocrinol Diabetes, 2020, 128(5): 339-346.[8] Zhang D, Jiang W, Liu M, et al. Highly efficient differentiation of human ES cells and iPS cells into mature pancreatic insulin-producing cells[J]. Cell Res, 2009, 19(4): 429-438.[9] Ogawa M, Ogawa S, Bear C E, et al. Directed differentiation of cholangiocytes from human pluripotent stem cells[J]. Nat Biotechnol, 2015, 33(8): 853-861.[10] Sampaziotis F, de Brito M C, Madrigal P, et al. Cholangiocytes derived from human induced pluripotent stem cells for disease modeling and drug validation[J]. Nat Biotechnol, 2015, 33(8): 845- 852.[11] Mandai M, Watanabe A, KurimotoY, et al. Autologous induced stem- cell-derived retinal cells for macular degeneration[J]. N Engl J Med, 2017, 376(11): 1038-1046.[12] Zhang L, Tian L, Dai X Y, et al. Pluripotent stem cell-derived CAR- macrophage cells with antigen-dependent anti-cancer cell functions[J]. J Hematol Oncol, 2020, 13(1): 153. DOI:10.1186/s13045-020-00983- 2.[13] Lin X T, Sun Y, Dong X, et al. IPSC-derived CAR-NK cells for cancer immunotherapy[J]. BiomedPharmacother, 2023, 165: 115123. DOI:10.1016/j.biopha.2023.115123.[14] Ueda T, Shiina S, Iriguchi S, et al. Optimization of the proliferation and persistency of CAR T cells derived from human induced pluripotent stem cells[J]. Nat BiomedEng, 2023, 7(1): 24-37.[15] Park S J, Kim YY, Han JY, et al. Advancements in human embryonic stem cell research: clinical applications and ethical issues[J]. Tissue Eng Regen Med, 2024, 21(3): 379-394.[16] Yamanaka S. Pluripotent stem cell-based cell therapy-promise and challenges[J]. Cell Stem Cell, 2020, 27(4): 523-531.[17] 中国细胞生物学学会 . T/CSSCR002—2019《人胚胎干细胞》团体标准 [S]. 北京 : 中国标准出版社, 2019.[18] 中华人民共和国科技部和卫生部 . 人胚胎干细胞研究伦理指导原则 [J]. 中国生育健康杂志, 2004, 15(2): 71.[19] 中国细胞生物学学会 . T/CSCB 0001—2020《干细胞通用要求》团体标准 [S]. 北京 : 中国标准出版社, 2020.[20] 中国细胞生物学学会 . T/CSCB 0001—2022《人干细胞研究伦理 审查技术规范》团体标准 [S]. 北京 : 中国标准出版社, 2022.[21] ISO. Requirements for human and mouse pluripotent stem cells[EB/OL].(2022-08-03)[2023-08-30]. https://www.iso.org/obp/ ui#iso:std:iso:24603:ed-1:v1:en.[22] Netsrithong R, Garcia-Perez L, Themeli M. Engineered T cells from induced pluripotent stem cells: from research towards clinical implementation[J]. Front Immunol, 2024, 14: 1325209. DOI:10.3389/ fimmu.2023.1325209.美编排版:张苗苗感谢您阅读《药学进展》微信平台原创好文,也欢迎各位读者转载、引用。本文选自《药学进展》2025年第 3 期。《药学进展》杂志由教育部主管、中国药科大学和中国药学会共同主办,中国科技核心期刊(中国科技论文统计源期刊)。刊物以反映药学科研领域的新方法、新成果、新进展、新趋势为宗旨,以综述、评述、行业发展报告为特色,以药学学科进展、技术进展、新药研发各环节技术信息为重点,是一本专注于医药科技前沿与产业动态的专业媒体。《药学进展》注重内容策划、加强组稿约稿、深度挖掘、分析药学信息资源、在药学学科进展、科研思路方法、靶点机制探讨、新药研发报告、临床用药分析、国际医药前沿等方面初具特色;特别是医药信息内容以科学前沿与国家战略需求相合,更加突出前瞻性、权威性、时效性、新颖性、系统性、实战性。根据最新统计数据,刊物篇均下载率连续三年蝉联我国医药期刊榜首,复合影响因子1.216,具有较高的影响力。《药学进展》编委会由国家重大专项化学药总师陈凯先院士担任主编,编委由新药研发技术链政府监管部门、高校科研院所、制药企业、临床医院、CRO、金融资本及知识产权相关机构近两百位极具影响力的专家组成。联系《药学进展》↓↓↓编辑部官网:pps.cpu.edu.cn;邮箱:yxjz@163.com;电话:025-83271227。欢迎投稿、订阅!往期推荐聚焦“兴药为民·2023生物医药创新融合发展大会”“兴药为民·2023生物医药创新融合发展大会”盛大启幕!院士专家齐聚杭城,绘就生物医药前沿赛道新蓝图“兴药强刊”青年学者论坛暨《药学进展》第二届青年编委会议成功召开“兴药为民·2023生物医药创新融合发展大会”路演专场圆满收官!校企合作新旅程已启航我知道你在看哟
细胞疗法
2025-04-26
·今日头条
在免疫细胞疗法的创新探索中,TCR-T细胞疗法因在实体瘤治疗中的独特潜力备受关注,目前多项临床研究已进入关键验证阶段。从实验室到临床的跨越中,TCR-T疗法正用科学实证改写“癌转移不可战胜”的固有认知。
那么这项疗法在临床实践中的真实效果如何?是否有权威数据支撑呢?以下通过国际权威期刊《Nature Medicine》发布的IMA203(TCR-T)首次I期临床研究展开分析:在40例入组患者中,治疗总缓解率高达52.5%,而高剂量治疗组总缓解率更是高达70%!
这组数据不仅为实体瘤免疫治疗奠定重要临床基石,更以直观的疗效改写患者命运:影像学报告上缩小的肿瘤病灶、持续延长的生存曲线,每一个数字背后都是重燃的生命希望!
▲截图源自“nature medicine”
一、IMA203 TCR-T疗法震撼数据:实体瘤总缓解率52.5%,高剂量组达70%!难治性黑色素瘤患者治疗15个月完全缓解,持续获益超2年!
近年来,原发性肿瘤及转移性肿瘤的治疗取得显著进展,早期筛查技术与新型疗法的普及提升了多种癌症的总体生存率。然而对癌症幸存者而言,初次治疗成功后仍需警惕癌症复发转移的潜在风险。尽管手术、放化疗等传统疗法显著延长了生存周期,但在遏制肿瘤转移复发、降低治疗副作用等方面仍有局限,探索更精准高效的治疗手段成为临床迫切需求。
IMA203是一种靶向自体黑色素瘤优先表达抗原(PRAME)的TCR-T细胞疗法,靶向由HLA-A02:01呈递的PRAME衍生肽,适用于治疗HLA-A02⁺且携带PRAME⁺的复发性和/或难治性实体瘤患者(包括黑色素瘤、肉瘤等)。
《Nature Medicine》报道的首次人体剂量递增试验(NCT03686124)分为两个阶段:1a期剂量递增阶段(27例患者,总剂量中位数为0.409×109TCR-T细胞)、1b期剂量扩展阶段(总剂量中位数为4.16×109TCRT细胞)。结果显示如下:
1、
全队列
:全部40例接受IMA203治疗的患者(覆盖黑色素瘤、肉瘤等)中,
总缓解率(含未确认/已确认缓解)高达52.5%
(21/40),
确认缓解率(cORR)为28.9%
(11/38),
中位缓解持续时间为4.4个月
(范围:2.4-23.0个月)。
2、
1a期队列(27例)
:
总缓解率(u/cORR)为48.1%
(13/27),
cORR为18.5%
(5/27),
中位缓解持续时间(mDOR)为4.4个月,中位无进展生存期(PFS)为2.8个月,中位总生存期(OS)为7.5个月
。
3、
1b期队列(13例)
:
总缓解率提升至61.5%
(8/13),
cORR达54.5%
(6/11),8例缓解患者中
4例持续缓解
,其中
2例在治疗1年后仍维持部分缓解
;中位随访11.5个月,
中位缓解持续时间8.1个月,中位PFS为5.7个月
,中位OS未达到。
4、
黑色素瘤高剂量亚组(10例)
:对1a期和1b期队列中接受DL4/DL5治疗的黑色素瘤患者(n=10)分析显示,
au/cORR高达70%
(7/10;95%CI:34.8–93.3),
cORR为50%
(5/10;95%CI:18.7–81.3)。
其中3例患者在治疗9个月(1例)和12个月(2例)后仍持续缓解
,mDOR尚未达到。
▲图源“nature medicine”,版权归原作者所有,如无意中侵犯了知识产权,请联系我们删除
综上,IMA203在多种实体瘤(包括难治性黑色素瘤)中展现良好抗肿瘤活性,且高剂量给药、基线肿瘤负荷较低的患者中,确认缓解率显著更高。
一例复发性黑色素瘤患者治疗15个月实现完全缓解,持续缓解超2年!
此前,在2024年黑色素瘤研究学会大会上,公布了IMA203 TCR-T疗法针对黑色素瘤的1b期临床更新数据。其中一名51岁男性皮肤黑色素瘤患者(编号A-DL4-03)在接受IMA203治疗15个月后,成功实现完全缓解(CR)。
该患者有13年的皮肤黑色素瘤病史,曾先后接受达拉非尼+曲美替尼、帕博利珠单抗、恩拉菲尼+比美替尼等5种系统治疗方案,但病情持续进展。入组前,其颈部淋巴结存在23mm的目标病灶,盆腔骨骼和肺部亦有非目标病灶。
接受IMA203 TCR-T细胞治疗后,根据RECIST1.1标准评估,
输注后24个月内持续无进展,病灶缩小78.3%
。研究者通过正电子发射断层扫描(PET)成像发现,
输注后第15个月已达到代谢完全缓解(CR)
(详见下图)。尤为令人振奋的是,
截至数据截止时,该患者持续缓解已超过两年。
▲图源“Immatics”,版权归原作者所有,如无意中侵犯了知识产权,请联系我们删除
二、TCR-T横扫宫颈癌、食管癌、尿路上皮癌、骨肉瘤,一例患者转移灶完全缓解持续29个月
《临床肿瘤学杂志》报道了一项TCR-T细胞治疗转移性癌症的临床研究,结果振奋人心:1例转移性宫颈癌患者经治疗后实现持续≥29个月的客观完全缓解,另有3例不同癌种患者(食管癌、尿路上皮癌、骨肉瘤)在最高剂量治疗中出现持续4-19个月的客观部分缓解。
本次研究共纳入17例转移性癌症患者,接受TCR转导的CD4⁺T细胞治疗,其中8例在剂量递增期接受低剂量治疗,9例在最高剂量组接受高剂量治疗。
结果显示:TCR转导CD4⁺T细胞疗法在转移性宫颈癌中展现持久完全缓解潜力,在食管癌、尿路上皮癌、骨肉瘤中亦能诱导短期至中期的部分缓解,为多种实体瘤的免疫治疗提供了新方向。其中有几例患者的情况值得广泛关注:
6号宫颈癌患者
其中6号宫颈癌患者:曾接受放疗及6个周期的顺铂治疗,后出现锁骨上淋巴结复发(PET阳性+活检证实)。遂入组接受2.7×10⁹个TCR转导CD4⁺T细胞治疗。结果显示:
治疗后锁骨上淋巴结转移灶完全消失,且该缓解持续29个月
。PET复查显示,该患者
剩余的淋巴结呈阴性且缩小至<1cm
(详见下图)。
▼转移性宫颈癌患者(患者6)在接受TCR-T细胞治疗前(左图)与治疗后29个月(右图)的颈部计算机断层扫描(CT)对比
▲图源“JCO”,版权归原作者所有,如无意中侵犯了知识产权,请联系我们删除
9号食管癌患者
9号食管癌患者:既往接受放疗、FOLFOX方案(亚叶酸-氟尿嘧啶-奥沙利铂)及卡培他滨治疗后,
纵隔及食管旁淋巴结出现部分缓解(PR)
。
11号尿路上皮癌患者
11号尿路上皮癌患者:原发肿瘤累及左输尿管,并伴肝及腹腔淋巴结转移,经手术和化疗后进展,遂接受TCR-T治疗。结果显示:治疗后,
主动脉周围淋巴结及肝转移灶持续19个月部分缓解,仅残留少量病灶
(详见下图)。
▼转移性尿路上皮癌患者(患者11)在接受TCR-T细胞治疗前(左图)与治疗后18个月(右图)的MRI对比
▲图源“JCO”,版权归原作者所有,如无意中侵犯了知识产权,请联系我们删除
16号骨肉瘤患者
16号骨肉瘤患者:历经手术、化疗、靶向治疗(索拉非尼)等多线治疗后,又入组接受TCR-T治疗,结果显示:
肺转移灶部分缓解持续4个月
(详见下图)。
▼转移性转移性骨肉瘤患者(患者16)在接受TCR-T细胞治疗前(左图)与治疗后4个月(右图)的胸部CT对比
▲图源“JCO”,版权归原作者所有,如无意中侵犯了知识产权,请联系我们删除
三、NY-ESO-1 TCR-T疗法疗法改写肺癌治疗困局:多线治疗失败患者获部分缓解,肺癌转移灶缩小76%,生活质量大幅提升
NY-ESO-1作为癌症免疫治疗中极具潜力的靶点,在11.8%-21%的非小细胞肺癌中均有表达,其安全性与有效性已得到广泛关注。
近期,《Oncology Letters》报道了一则NYESO1特异性TCR-T细胞疗法治疗晚期非小细胞肺癌(NSCLC)的振奋案例(NCT02457650),成功使肿瘤明显缩小至部分缓解。
该研究纳入4例HLA-A2阳性、NY-ESO-1表达的转移性非小细胞肺癌患者,入组后,先接受淋巴细胞清除化疗,随后进行NY-ESO-1TCR-T细胞的过继转移,并配合全身性IL-2治疗。
结果显示:
2例取得临床反应
。其中,
患者1在NY-ESO-1TCR-T细胞后近3个月,达病情稳定(SD);患者2在治疗4个月后,达到部分缓解(PR)
。
值得一提的是,患者2的疗效尤为显著:这是一位44岁,HLA-A2阳性且携带EGFR突变的NY-ESO-1晚期肺腺癌(LADC)的女性,卡氏功能状态评分(KPS)仅50分,存在咯血、胸痛等症状。既往曾先后接受6周期多西他赛+卡铂化疗、吉非替尼+厄洛替尼靶向治疗,均告失败。2015年9月CT显示:右肺门、纵隔、右胸膜、右肝叶及肝包膜广泛转移,此时临床上已无更合适的治疗方案。但天无绝人之路,该患者右肺肿瘤活检证实NY-ESO-1强阳性,符合TCR-T治疗条件,遂得以入组接受NY-ESO-1 TCR-T细胞治疗。
令人振奋的是,首次TCR-T细胞输注后43天CT显示:
肺原发灶从95×86×54mm缩小至64×44×54mm(体积减少约56%)
;
肝转移灶由19.8×19.6×20mm缩小至10×10×10mm(体积减少约76%)
;
胸水吸收,肺复张
,依据RECIST1.1标准
达到部分缓解(PR)
。同时,患者的
卡氏功能状态评分(KPS)从50分提升至90分
,
咯血、胸痛症状显著缓解,生活质量大幅提升。
▲图源“Oncology Letters”,版权归原作者所有,如无意中侵犯了知识产权,请联系我们删除
四、小编寄语
TCR-T治疗创新性地开创了“抗癌+抗病毒”双效合一的治疗范式。近年来,科研团队正加速探索其在病毒相关性实体瘤领域的应用,尤其是乙肝病毒引发的肝细胞癌,以及人乳头瘤病毒(HPV)相关的宫颈癌值得振奋的是,随着首款TCR-T细胞治疗产品成功获批上市,标志着这一前沿技术正式迈入临床应用阶段!我们期待未来有更多突破性抗癌治疗获批,助力实体瘤患者实现长期带瘤生存的希望。
五、参考资料
[1]Wermke M,et al.Autologous T cell therapy for PRAME+ advanced solid tumors in HLA-A* 02+ patients: a phase 1 trial[J]. Nature Medicine, 2025: 1-10.
https://www-nature-com.libproxy1.nus.edu.sg/articles/s41591-025-03650-6
[2]Lu Y C,et al.Treatment of patients with metastatic cancer using a major histocompatibility complex class II–restricted T-cell receptor targeting the cancer germline antigen MAGE-A3[J]. Journal of Clinical Oncology, 2017, 35(29): 3322-3329.
https://ascopubs-org.libproxy1.nus.edu.sg/doi/10.1200/JCO.2017.74.5463?url_ver=Z39.882003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
[3]Xia Y,et al.Treatment of metastatic nonsmall cell lung cancer with NYESO1 specific TCR engineeredT cells in a phase I clinical trial: A case report[J]. Oncology letters, 2018, 16(6): 6998-7007.
https://www-spandidos-publications-com.libproxy1.nus.edu.sg/10.3892/ol.2018.9534
[4]https://www.globenewswire.com/news-release/2024/10/10/2961129/0/en/Immatics-Announces-Updated-Phase-1b-Clinical-Data-on-ACTengine-IMA203-TCR-T-Targeting-PRAME-in-Melanoma-Patients-and-Provides-Update-on-Upcoming-SUPRAME-Phase-3-Trial.html
本文为全球肿瘤医生网原创,未经授权严禁转载
细胞疗法临床结果免疫疗法临床1期
2025-04-24
·今日头条
TCR-T疗法凭借NY-ESO-1靶点,精准暴击黑色素瘤、滑膜肉瘤等
TCR-T疗法利用NY-ESO-1靶点,在黑色素瘤和滑膜肉瘤治疗中显示出显著疗效,为晚期癌症患者带来新希望。
1. NY-ESO-1蛋白的表达特点
NY-ESO-1蛋白在多种肿瘤中高表达,而在正常组织中低表达或不表达,因此它可以作为一个理想的肿瘤治疗靶点。
2. TCR-T细胞疗法的优势
TCR-T细胞疗法具有长效抗肿瘤效应,能精准识别肿瘤细胞特异性抗原,对难治性肿瘤有潜在治疗效果。
3. TCR-T疗法的临床应用
TCR-T疗法已应用于宫颈癌、乙肝病毒相关肝细胞癌等癌种的治疗,并取得显著成效。
细胞疗法
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
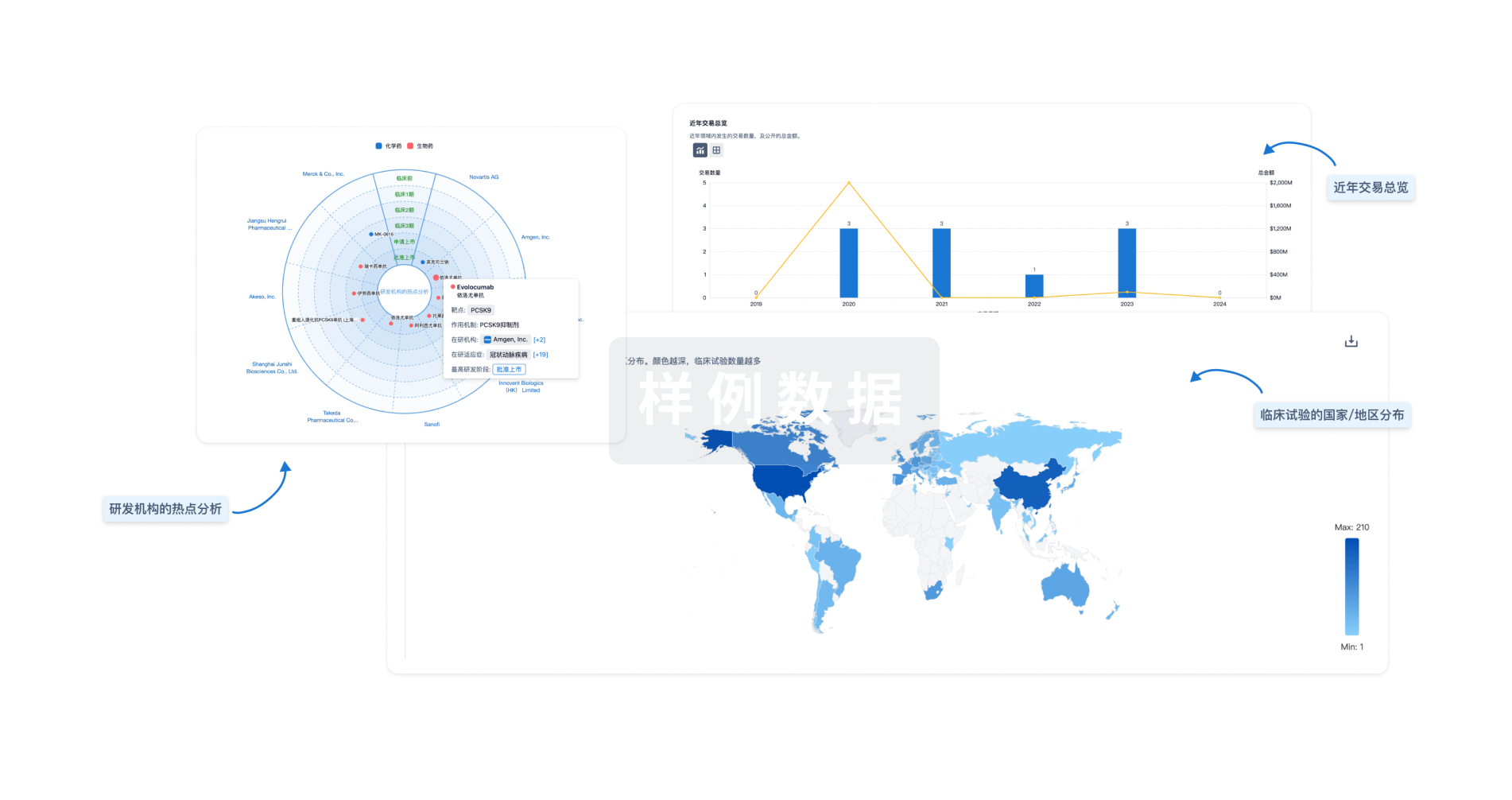
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用