预约演示
更新于:2025-05-07
IL-23
更新于:2025-05-07
基本信息
别名 白细胞介素-23 |
简介- |
关联
82
项与 IL-23 相关的药物作用机制 IL-12p40抑制剂 [+1] |
在研机构 |
原研机构 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2025-04-15 |
作用机制 IL-12抑制剂 [+1] |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 澳大利亚 |
首次获批日期2025-02-11 |
545
项与 IL-23 相关的临床试验NCT06916390
Guselkumab Intervention and Diet Evaluation for Pouchitis
Restorative proctocolectomy (RPC) with ileal pouch-anal anastomosis (IPAA) is considered the procedure of choice in patients with ulcerative colitis (UC) refractory to medical therapy or with neoplasia. The most common complication after IPAA is the development of pouchitis. Pouchitis is clinically characterized by variable symptoms including increased stool frequency, altered consistency, bloody stools, abdominal cramping, urgency, and incontinence. Symptomatic pouchitis longer than four weeks is considered chronic pouchitis.
The conventional treatment for acute and chronic pouchitis is antibiotics, such as metronidazole and ciprofloxacin. The disease course of antibiotic responsive pouchitis may evolve into antibiotic dependent (requiring antibiotic maintenance therapy) pouchitis and then antibiotic refractory (no response to antibiotic treatment) pouchitis. Although many patients respond to antibiotic therapy, there is also evidence that suggest that aberrant regulation of the mucosal immune system might play a part in the pathogenesis of pouchitis arising from an abnormal mucosal immune response to a dysbiosis of the pouch microbiota. If individuals fail to respond to antibiotics, anti-tumor necrosis factor (anti-TNF) agents and vedolizumab have been proposed for the treatment of chronic pouchitis.
Guselkumab, an interleukin-23 (IL-23) p19 subunit antagonist monoclonal antibody, is proven to be efficacious in patients with moderately-to-severely active UC. Efficacy of guselkumab in treating UC has been shown in multiple large clinical trials. However, patients with pouchitis were never the targeted population and were even often excluded from the trials.
Pouchitis becomes a chronic problem with a huge impact in the quality of life of these patients. The incidence of pouchitis has been rising in the last decades. This increase might be explained by a change in dietary habits of this population.
This open label single center trial at UZ Leuven aims to evaluate the efficacy and safety of guselkumab in the treatment of chronic antibiotic refractory pouchitis during a 48-week treatment period, with or without a dietary intervention. Twenty subjects with a proctocolectomy and IPAA for UC who have developed chronic or relapsing pouchitis will be enrolled.
The conventional treatment for acute and chronic pouchitis is antibiotics, such as metronidazole and ciprofloxacin. The disease course of antibiotic responsive pouchitis may evolve into antibiotic dependent (requiring antibiotic maintenance therapy) pouchitis and then antibiotic refractory (no response to antibiotic treatment) pouchitis. Although many patients respond to antibiotic therapy, there is also evidence that suggest that aberrant regulation of the mucosal immune system might play a part in the pathogenesis of pouchitis arising from an abnormal mucosal immune response to a dysbiosis of the pouch microbiota. If individuals fail to respond to antibiotics, anti-tumor necrosis factor (anti-TNF) agents and vedolizumab have been proposed for the treatment of chronic pouchitis.
Guselkumab, an interleukin-23 (IL-23) p19 subunit antagonist monoclonal antibody, is proven to be efficacious in patients with moderately-to-severely active UC. Efficacy of guselkumab in treating UC has been shown in multiple large clinical trials. However, patients with pouchitis were never the targeted population and were even often excluded from the trials.
Pouchitis becomes a chronic problem with a huge impact in the quality of life of these patients. The incidence of pouchitis has been rising in the last decades. This increase might be explained by a change in dietary habits of this population.
This open label single center trial at UZ Leuven aims to evaluate the efficacy and safety of guselkumab in the treatment of chronic antibiotic refractory pouchitis during a 48-week treatment period, with or without a dietary intervention. Twenty subjects with a proctocolectomy and IPAA for UC who have developed chronic or relapsing pouchitis will be enrolled.
开始日期2025-09-30 |
申办/合作机构- |
NCT06807593
Treatment of Immune Checkpoint Inhibitor-related Diarrhea and/ or Colitis With Ustekinumab in Cancer Patients
The goal of this clinical research study is to learn if ustekinumab can help to control immune-related diarrhea and/or colitis in cancer patients.
开始日期2025-06-30 |
NCT06880744
Phase 3b, Multicenter, Randomized, Open-Label Study of Risankizumab Compared to Vedolizumab for the Treatment of Adult Subjects With Moderate to Severe Ulcerative Colitis Who Are Naïve to Targeted Therapies
Ulcerative colitis (UC) is a type of inflammatory bowel disease that causes inflammation and bleeding from the lining of the rectum and colon (large intestine).This study will evaluate how safe and effective risankizumab is compared to vedolizumab in treating adult participants with moderate to severe UC who are naive to targeted therapies (TaTs).
Risankizumab and vedolizumab are approved medications for moderate to severe UC in multiple countries. Participants who meet the eligibility criteria will be randomized in a 1:1 ratio to receive open label risankizumab or vedolizumab. Approximately 530 adult participants with moderate to severe UC who are naïve to targeted therapies (TaTs) will be enrolled at 285 sites worldwide.
For participants randomized to risankizumab, drug will be administered intravenous(IV) during the induction period followed by subcutaneous injection during the maintenance period. Participants randomized to vedolizumab will receive drug IV throughout the study.
The duration of the study is approximately 69 weeks for participants randomized to risankizumab and 71 weeks for participants randomized to vedolizumab. This includes up to a 35-day screening period followed by a treatment period of 44 weeks for risankizumab and 46 weeks for vedolizumab.
There may be higher treatment burden for participants in this trial compared to their standard of care. Participants will attend regular outpatient visits during the study. The effect and safety of the treatment will be checked by medical assessments, evaluation of side effects and completing questionnaires.
Risankizumab and vedolizumab are approved medications for moderate to severe UC in multiple countries. Participants who meet the eligibility criteria will be randomized in a 1:1 ratio to receive open label risankizumab or vedolizumab. Approximately 530 adult participants with moderate to severe UC who are naïve to targeted therapies (TaTs) will be enrolled at 285 sites worldwide.
For participants randomized to risankizumab, drug will be administered intravenous(IV) during the induction period followed by subcutaneous injection during the maintenance period. Participants randomized to vedolizumab will receive drug IV throughout the study.
The duration of the study is approximately 69 weeks for participants randomized to risankizumab and 71 weeks for participants randomized to vedolizumab. This includes up to a 35-day screening period followed by a treatment period of 44 weeks for risankizumab and 46 weeks for vedolizumab.
There may be higher treatment burden for participants in this trial compared to their standard of care. Participants will attend regular outpatient visits during the study. The effect and safety of the treatment will be checked by medical assessments, evaluation of side effects and completing questionnaires.
开始日期2025-06-26 |
申办/合作机构 |
100 项与 IL-23 相关的临床结果
登录后查看更多信息
100 项与 IL-23 相关的转化医学
登录后查看更多信息
0 项与 IL-23 相关的专利(医药)
登录后查看更多信息
13,372
项与 IL-23 相关的文献(医药)2025-12-31·OncoImmunology
Circulating cytokine associations with clinical outcomes in melanoma patients treated with combination nivolumab plus ipilimumab
Article
作者: Baginska, Joanna ; Weirather, Jason L. ; Manos, Michael ; Hathaway, Emma ; Liu, David ; Huang, Amy Y. ; Tarantino, Giuseppe ; Chen, Jiajia ; Rodig, Scott J. ; Nazzaro, Matthew ; Brennick, Ryan ; Pfaff, Kathleen L. ; Russell, Janice D. ; Hodi, F. Stephen ; Manuszak, Claire ; Ranasinghe, Srinika ; Holovatska, Marta ; Giobbie-Hurder, Anita ; Severgnini, Mariano
2025-12-31·Gut Microbes
Anti-interleukin-23 treatment linked to improved
Clostridioides difficile
infection survival
Article
作者: Madden, Gregory R. ; Preissner, Robert ; Preissner, Saskia ; Petri, William A.
2025-12-31·Cancer Biology & Therapy
Identification of endoplasmic reticulum stress-related genes as prognostic markers in colon cancer
Article
作者: Li, Wei ; Liu, Xian ; Sun, Wei ; Li, Yaqiang ; Xu, Wenjing ; Xu, Baohong ; Kuai, Dayu
1,731
项与 IL-23 相关的新闻(医药)2025-05-05
Data from the QUASAR long-term extension study demonstrate more than 70% of patients were in clinical remission and more than 40% of patients were in endoscopic remission at Week 92
SAN DIEGO, Calif., May 5, 2025 /PRNewswire/ -- Johnson & Johnson (NYSE: JNJ) today announced new data from the TREMFYA® (guselkumab) Phase 3 QUASAR long-term extension (LTE) study in adults with moderately-to-severely active ulcerative colitis (UC). These data are among 24 abstracts highlighting the Company's research being presented at Digestive Disease Week (DDW) 2025.
Data from the QUASAR LTE study demonstrate patients treated with TREMFYA® sustained clinical and endoscopic efficacy at Week 92: a, 1
72% of patients were in clinical remissionb with 99% of those patients remaining corticosteroid free for 8 or more weeks through Week 92.
43% of patients were in endoscopic remission.c
Among patients achieving endoscopic improvementd at Week 44, 84% maintained endoscopic improvement through Week 92.
Patients treated with TREMFYA® sustained clinical and endoscopic remission regardless of prior biologic and/or JAK inhibitor treatment history.
"People living with ulcerative colitis seek treatments that both address the challenging symptoms of the disease and provide durable results," said Gary R. Lichtenstein, Vice Chief, Division of Gastroenterology and Hepatology, Development and Philanthropy at the University of Pennsylvania.e "These new data show TREMFYA delivers long-term, sustained clinical and endoscopic remission, marking important progress in UC care."
Safety data were consistent with the well-established safety profile of TREMFYA® in inflammatory bowel disease (IBD) with no new safety concerns identified.
"With these findings, TREMFYA shows the powerful impact it can have in achieving longer term remission in patients," said Esi Lamousé-Smith, MD, PhD, Vice President, Gastroenterology Disease Area Lead, Immunology, Johnson & Johnson Innovative Medicine. "This is a significant step forward in our mission to reshape the standard of care in inflammatory bowel disease."
TREMFYA® is the first and only approved, dual-acting monoclonal antibody that blocks IL-23 while also binding to CD64, a receptor on cells that produce IL-23. IL-23 is a cytokine secreted by activated monocyte/macrophages and dendritic cells that is known to be a driver of immune-mediated diseases including UC.2,3,4,5,6
TREMFYA® received FDA approval in September 2024 for the treatment of adult patients with moderately to severely active UC and is currently administered via an IV induction regimen, followed by a SC maintenance regimen. In November 2024, a supplemental Biologics License Application (sBLA) was submitted to the FDA seeking approval of a SC induction regimen of TREMFYA® for the treatment of adults with moderately to severely active UC. TREMFYA® was also approved by the FDA in March 2025 for SC and IV induction options for the treatment of adults with moderately to severely active Crohn's disease (CD).
For a full list of all data being presented at DDW visit:
Editor's Notes:
a. Nonresponder imputation results. Data were analyzed using 2 methods: 'nonresponder imputation' (NRI) accounting for patients with treatment failure or missing data, and 'as observed'. NRI results were consistent with as observed.
b. Clinical remission was defined as a Mayo stool frequency subscore of 0 or 1 and not increased from induction baseline, a Mayo rectal bleeding subscore of 0, and a Mayo endoscopic subscore (MES) of 0 or 1.
c. Endoscopic remission (normalization) was defined as a MES of 0.
d. Endoscopic improvement was defined as a MES of 0 or 1.
e. Dr. Lichtenstein has received honorarium for his role as a consultant to Johnson & Johnson. He has not been compensated for any media work.
ABOUT THE QUASAR PROGRAM (NCT04033445)
QUASAR is a randomized, double-blind, placebo-controlled, parallel group, multicenter, Phase 2b/3 program designed to evaluate the efficacy and safety of TREMFYA® in adults with moderately to severely active ulcerative colitis who had an inadequate response or intolerance to conventional therapy (e.g., thiopurines or corticosteroids), prior biologics (TNF antagonists or vedolizumab) and/or JAK inhibitors (tofacitinib). QUASAR included a Phase 2b dose-ranging induction study, a confirmatory Phase 3 induction study, and a Phase 3 randomized withdrawal maintenance study. In the Phase 3 induction study, patients received either TREMFYA® 200 mg or placebo by IV infusion at Weeks 0, 4, and 8. In the Phase 3 maintenance study, patients received a SC maintenance regimen of either TREMFYA® 200 mg q4w, TREMFYA® 100 mg q8w, or placebo.7 The ongoing long-term extension study provides an additional 4 years of treatment. Efficacy, safety, pharmacokinetics, immunogenicity, and biomarkers are assessed at specified time points.
ABOUT ULCERATIVE COLITIS
Ulcerative colitis (UC) is a chronic disease of the large intestine, also known as the colon, in which the lining of the colon becomes inflamed and develops tiny open sores, or ulcers, that produce pus and mucus. It is the result of the immune system's overactive response. Symptoms vary but may typically include loose and more urgent bowel movements, rectal bleeding or bloody stool, persistent diarrhea, abdominal pain, loss of appetite, weight loss, and fatigue.8
ABOUT TREMFYA® (guselkumab)
Developed by Johnson & Johnson, TREMFYA® is the first approved fully-human, dual-acting monoclonal antibody designed to neutralize inflammation at the cellular source by blocking IL-23 and binding to CD64 (a receptor on cells that produce IL-23). Findings for dual-acting are limited to in vitro studies that demonstrate guselkumab binds to CD64, which is expressed on the surface of IL-23 producing cells in an inflammatory monocyte model. The clinical significance of this finding is not known.
TREMFYA® is a prescription medicine approved in the U.S. to treat:
adults with moderate to severe plaque psoriasis who may benefit from taking injections or pills (systemic therapy) or phototherapy (treatment using ultraviolet or UV light).
adults with active psoriatic arthritis.
adults with moderately to severely active ulcerative colitis.
adults with moderately to severely active Crohn's disease.4
TREMFYA® is approved in Europe, Canada, Japan, and a number of other countries for the treatment of adults with moderate-to-severe plaque psoriasis and for the treatment of adults with active psoriatic arthritis. In addition, TREMFYA ® is approved in Europe, Japan and Brazil for the treatment of adult patients with moderately to severely active UC and in Brazil and China for the treatment of adults with moderately to severely active CD.
Johnson & Johnson maintains exclusive worldwide marketing rights to TREMFYA®. For more information, visit: .
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about TREMFYA®?
TREMFYA® is a prescription medicine that may cause serious side effects, including:
Serious Allergic Reactions. Stop using TREMFYA® and get emergency medical help right away if you develop any of the following symptoms of a serious allergic reaction:
Infections. TREMFYA® may lower the ability of your immune system to fight infections and may increase your risk of infections. Your healthcare provider should check you for infections and tuberculosis (TB) before starting treatment with TREMFYA® and may treat you for TB before you begin treatment with TREMFYA® if you have a history of TB or have active TB. Your healthcare provider should watch you closely for signs and symptoms of TB during and after treatment with TREMFYA®.
Tell your healthcare provider right away if you have an infection or have symptoms of an infection, including:
Liver problems. With the treatment of Crohn's disease or ulcerative colitis, your healthcare provider will do blood tests to check your liver before and during treatment with TREMFYA®. Your healthcare provider may stop treatment with TREMFYA® if you develop liver problems. Tell your healthcare provider right away if you notice any of the following symptoms:
Do not use TREMFYA® if you have had a serious allergic reaction to guselkumab or any of the ingredients in TREMFYA®.
Before using TREMFYA®, tell your healthcare provider about all of your medical conditions, including if you:
have any of the conditions or symptoms listed in the section
"What is the most important information I should know about TREMFYA®?"
have an infection that does not go away or that keeps coming back.
have TB or have been in close contact with someone with TB.
have recently received or are scheduled to receive an immunization (vaccine). You should avoid receiving live vaccines during treatment with TREMFYA®.
are pregnant or plan to become pregnant. It is not known if TREMFYA® can harm your unborn baby.
Pregnancy Registry: If you become pregnant during treatment with TREMFYA®, talk to your healthcare provider about registering in the pregnancy exposure registry for TREMFYA®. You can enroll by visiting , by calling 1-877-311-8972, or emailing [email protected]. The purpose of this registry is to collect information about the safety of TREMFYA® during pregnancy.
are breastfeeding or plan to breastfeed. It is not known if TREMFYA® passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side effects of TREMFYA®?
TREMFYA® may cause serious side effects. See "What is the most important information I should know about TREMFYA®?"
The most common side effects of TREMFYA® include: respiratory tract infections, headache, injection site reactions, joint pain (arthralgia), diarrhea, stomach flu (gastroenteritis), fungal skin infections, herpes simplex infections, stomach pain, and bronchitis.
These are not all the possible side effects of TREMFYA®. Call your doctor for medical advice about side effects.
Use TREMFYA® exactly as your healthcare provider tells you to use it.
Please read the full Prescribing Information, including Medication Guide, for TREMFYA® and discuss any questions that you have with your doctor.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit , or call 1-800-FDA-1088.
Dosage Forms and Strengths: TREMFYA® is available as 100 mg/mL and 200 mg/2mL for subcutaneous injection and as a 200 mg/20 mL (10 mg/mL) single dose vial for intravenous infusion.
ABOUT JOHNSON & JOHNSON
At Johnson & Johnson, we believe health is everything. Our strength in healthcare innovation empowers us to build a world where complex diseases are prevented, treated, and cured, where treatments are smarter and less invasive, and solutions are personal. Through our expertise in Innovative Medicine and MedTech, we are uniquely positioned to innovate across the full spectrum of healthcare solutions today to deliver the breakthroughs of tomorrow, and profoundly impact health for humanity.
Learn more at or at
Follow us at @JNJInnovMed.
Janssen Research & Development, LLC and Janssen Biotech, Inc. are Johnson & Johnson companies.
Cautions Concerning Forward-Looking Statements
This press release contains "forward-looking statements" as defined in the Private Securities Litigation Reform Act of 1995 regarding TREMFYA®. The reader is cautioned not to rely on these forward-looking statements. These statements are based on current expectations of future events. If underlying assumptions prove inaccurate or known or unknown risks or uncertainties materialize, actual results could vary materially from the expectations and projections of Johnson & Johnson. Risks and uncertainties include, but are not limited to: challenges and uncertainties inherent in product research and development, including the uncertainty of clinical success and of obtaining regulatory approvals; uncertainty of commercial success; manufacturing difficulties and delays; competition, including technological advances, new products and patents attained by competitors; challenges to patents; product efficacy or safety concerns resulting in product recalls or regulatory action; changes in behavior and spending patterns of purchasers of health care products and services; changes to applicable laws and regulations, including global health care reforms; and trends toward health care cost containment. A further list and descriptions of these risks, uncertainties and other factors can be found in Johnson & Johnson's most recent Annual Report on Form 10-K, including in the sections captioned "Cautionary Note Regarding Forward-Looking Statements" and "Item 1A. Risk Factors," and in Johnson & Johnson's subsequent Quarterly Reports on Form 10-Q and other filings with the Securities and Exchange Commission. Copies of these filings are available online at , or on request from Johnson & Johnson. Johnson & Johnson does not undertake to update any forward-looking statement as a result of new information or future events or developments.
References:
1 Lichtenstein GR, et al. Efficacy And Safety Of Guselkumab For Ulcerative Colitis Through Week 92 Of The Quasar Long-Term Extension Study. Poster presentation (#4241842) at Digestive Disease Week 2025. May 2025.
2 Atreya R, Abreu MT, Krueger JG, et al. Guselkumab, an IL-23p19 subunit-specific monoclonal antibody, binds CD64+ myeloid cells and potentially neutralizes IL-23 produced from the same cells. Poster presented at: 18th Congress of the European Crohn's and Colitis Organization (ECCO); March 1-4, 2023; Copenhagen, Denmark. Poster P504
3 Kreuger JG, Eyerich K, Kuchroo VK. Il-23 past, present, and future: a roadmap to advancing IL-23 science and therapy. Front Immunol. 2024; 15:1331217. doi:10.3389/fimmu.2024.1331217.
4 TREMFYA® [Prescribing Information]. Horsham, PA: Janssen Biotech, Inc.
5 Skyrizi® [Prescribing Information]. North Chicago, IL: AbbVie, Inc.
6 Omvoh™ [Prescribing Information]. Indianapolis, IN: Eli Lilly and Company.
7 National Institutes of Health: Clinicaltrials.gov. A Study of Guselkumab in Participants With Moderately to Severely Active Ulcerative Colitis (QUASAR). Identifier: NCT04033445. . Accessed March 2025.
8 Crohn's & Colitis Foundation. What is ulcerative colitis? Available at: . Accessed March 2025
SOURCE Johnson & Johnson
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果临床3期上市批准
2025-05-05
TREMFYA® subcutaneous induction demonstrates significant rates of clinical remission and endoscopic improvement at Week 24 in ulcerative colitis
Findings build on recent FDA-approval of both routes of administration for induction therapy with TREMFYA® in Crohn's disease
SAN DIEGO, May 5, 2025 /PRNewswire/ -- Johnson & Johnson (NYSE: JNJ) today announced new data from the Phase 3 ASTRO study evaluating TREMFYA® (guselkumab) subcutaneous (SC) induction therapy in adults with moderately to severely active ulcerative colitis (UC). The ASTRO Week 24 data build on the Week 12 SC induction data that showed statistically significant and clinically meaningful improvements compared to placebo across all clinical and endoscopic measures consistent with the U.S. Food and Drug Administration (FDA)-approved intravenous (IV) induction regimen evaluated in this population, in the Phase 3 QUASAR study.1,2 TREMFYA® is the first and only IL-23 inhibitor to demonstrate robust results with a fully SC regimen. These findings are among 24 abstracts highlighting the Company's research being presented at Digestive Disease Week (DDW) 2025.
Data at Week 24 show patients treated with TREMFYA® 400 mg SC induction followed by SC maintenance dose regimens of either 100 mg every eight weeks (q8w) or 200 mg every four weeks (q4w) demonstrated statistically significant and clinically meaningful improvements across all clinical and endoscopic measures compared with patients receiving placebo.1
"Data from the ASTRO study demonstrate that subcutaneous induction treatment with TREMFYA provides clinically meaningful remission in patients with ulcerative colitis, similar to the effects seen with intravenous induction," said Millie Long, M.D., MPH, Professor of Gastroenterology and Hepatology at the University of North Carolina at Chapel Hill and study investigator.e "The availability of both subcutaneous and intravenous induction options would offer physicians and patients greater flexibility in their treatment approach."
Furthermore, at Week 24, in prespecified analyses of subpopulations defined by prior advanced therapy treatment status, TREMFYA® demonstrated statistically significant results across endpoints in both biologic and JAK inhibitor-naïve and biologic and JAK inhibitor-refractory patients. Safety data from the ASTRO study were consistent with the well-established safety profile of TREMFYA®.1
"These results highlight the potential of TREMFYA to redefine ulcerative colitis care with a fully subcutaneous induction and maintenance regimen that offers a convenient option with meaningful clinical and endoscopic improvements," said Esi Lamousé-Smith, MD, PhD, Vice President, Gastroenterology Disease Area Lead, Immunology, Johnson & Johnson Innovative Medicine. "Our goal is to reshape UC care and empower prescribers with a differentiated and effective treatment that offers the option of patient self-administration from day one."
TREMFYA® is the first and only approved, dual-acting monoclonal antibody that blocks IL-23 while also binding to CD64, a receptor on cells that produce IL-23. IL-23 is a cytokine secreted by activated monocyte/macrophages and dendritic cells that is known to be a driver of immune-mediated diseases including UC.3,4,5,6,7
TREMFYA® received FDA approval in September 2024 for the treatment of adult patients with moderately to severely active UC and is currently administered via an IV induction regimen, followed by a SC maintenance regimen. In November 2024, a supplemental Biologics License Application (sBLA) was submitted to the FDA seeking approval of a SC induction regimen of TREMFYA® for the treatment of adults with moderately to severely active UC. TREMFYA® was also approved by the FDA in March 2025 for SC and IV induction options for the treatment of adults with moderately to severely active Crohn's disease (CD).
For a full list of all data being presented at DDW visit:
Editor's Notes:
a. Clinical remission was defined as a Mayo stool frequency subscore of 0 or 1 and not increased from baseline, a Mayo rectal bleeding subscore of 0, and a Mayo endoscopic subscore of 0, or 1 with no friability present on the endoscopy.
b. Symptomatic remission per Mayo score is defined as a stool frequency subscore of 0 (normal number of stools) or 1 (1 to 2 stools more than normal) and a rectal bleeding subscore of 0 (no blood seen).
c. Endoscopic improvement was defined as an endoscopy subscore of 0 or 1 with no friability present on the endoscopy.
d. Clinical response is defined as decrease from baseline in the modified Mayo score by greater than or equal to (>=) 30 percent (%) and >=2 points, with either a >=1-point decrease from baseline in the rectal bleeding subscore or a rectal bleeding subscore of 0 or 1.
e. Dr. Long is a paid consultant for Johnson & Johnson. She has not been compensated for any media work.
ABOUT THE ASTRO STUDY (NCT05528510)
ASTRO is a randomized, double-blind, placebo-controlled, parallel-group, multicenter, treat-through Phase 3 study designed to evaluate the efficacy and safety of TREMFYA® SC induction therapy (400 mg at Weeks 0, 4, and 8) in adults with moderately to severely active ulcerative colitis who had an inadequate response or intolerance to conventional therapy (e.g., thiopurines or corticosteroids), prior biologics (TNF antagonists or vedolizumab) and/or ozanimod or approved JAK inhibitors. Patients (n = 418) were randomized 1:1:1 to receive TREMFYA® 400 mg SC induction at Weeks 0, 4 and 8 followed by TREMFYA® 200 mg SC every 4 weeks (q4w); or TREMFYA® 400 mg SC induction at Weeks 0, 4 and 8, followed by TREMFYA® 100 mg SC every 8 weeks (q8w); or placebo. The maintenance dose regimens in ASTRO (200 mg SC q4w and 100 mg SC q8w) are the same as those evaluated in the Phase 3 QUASAR program which established the efficacy and safety profile of IV induction followed by SC maintenance therapy in patients with moderate to severely active UC.8
ABOUT ULCERATIVE COLITIS
Ulcerative colitis (UC) is a chronic disease of the large intestine, also known as the colon, in which the lining of the colon becomes inflamed and develops tiny open sores, or ulcers, that produce pus and mucus. It is the result of the immune system's overactive response. Symptoms vary but may typically include loose and more urgent bowel movements, rectal bleeding or bloody stool, persistent diarrhea, abdominal pain, loss of appetite, weight loss, and fatigue.9
ABOUT TREMFYA® (guselkumab)
Developed by Johnson & Johnson, TREMFYA® is the first approved fully-human, dual-acting monoclonal antibody designed to neutralize inflammation at the cellular source by blocking IL-23 and binding to CD64 (a receptor on cells that produce IL-23). Findings for dual-acting are limited to in vitro studies that demonstrate guselkumab binds to CD64, which is expressed on the surface of IL-23 producing cells in an inflammatory monocyte model. The clinical significance of this finding is not known.
TREMFYA® is a prescription medicine approved in the U.S. to treat:
adults with moderate to severe plaque psoriasis who may benefit from taking injections or pills (systemic therapy) or phototherapy (treatment using ultraviolet or UV light).
adults with active psoriatic arthritis.
adults with moderately to severely active ulcerative colitis.
adults with moderately to severely active Crohn's disease.5
TREMFYA® is approved in Europe, Canada, Japan, and a number of other countries for the treatment of adults with moderate-to-severe plaque psoriasis and for the treatment of adults with active psoriatic arthritis. In addition, TREMFYA ® is approved in Europe, Japan and Brazil for the treatment of adult patients with moderately to severely active UC and in Brazil and China for the treatment of adults with moderately to severely active CD.
Johnson & Johnson maintains exclusive worldwide marketing rights to TREMFYA®. For more information, visit: .
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about TREMFYA®?
TREMFYA® is a prescription medicine that may cause serious side effects, including:
Serious Allergic Reactions. Stop using TREMFYA® and get emergency medical help right away if you develop any of the following symptoms of a serious allergic reaction:
Infections. TREMFYA® may lower the ability of your immune system to fight infections and may increase your risk of infections. Your healthcare provider should check you for infections and tuberculosis (TB) before starting treatment with TREMFYA® and may treat you for TB before you begin treatment with TREMFYA® if you have a history of TB or have active TB. Your healthcare provider should watch you closely for signs and symptoms of TB during and after treatment with TREMFYA®.
Tell your healthcare provider right away if you have an infection or have symptoms of an infection, including:
Liver problems. With the treatment of Crohn's disease or ulcerative colitis, your healthcare provider will do blood tests to check your liver before and during treatment with TREMFYA®. Your healthcare provider may stop treatment with TREMFYA® if you develop liver problems. Tell your healthcare provider right away if you notice any of the following symptoms:
Do not use TREMFYA® if you have had a serious allergic reaction to guselkumab or any of the ingredients in TREMFYA®.
Before using TREMFYA®, tell your healthcare provider about all of your medical conditions, including if you:
have any of the conditions or symptoms listed in the section
"What is the most important information I should know about TREMFYA®?"
have an infection that does not go away or that keeps coming back.
have TB or have been in close contact with someone with TB.
have recently received or are scheduled to receive an immunization (vaccine). You should avoid receiving live vaccines during treatment with TREMFYA®.
are pregnant or plan to become pregnant. It is not known if TREMFYA® can harm your unborn baby.
Pregnancy Registry: If you become pregnant during treatment with TREMFYA®, talk to your healthcare provider about registering in the pregnancy exposure registry for TREMFYA®. You can enroll by visiting , by calling 1-877-311-8972, or emailing [email protected]. The purpose of this registry is to collect information about the safety of TREMFYA® during pregnancy.
are breastfeeding or plan to breastfeed. It is not known if TREMFYA® passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side effects of TREMFYA®?
TREMFYA® may cause serious side effects. See "What is the most important information I should know about TREMFYA®?"
The most common side effects of TREMFYA® include: respiratory tract infections, headache, injection site reactions, joint pain (arthralgia), diarrhea, stomach flu (gastroenteritis), fungal skin infections, herpes simplex infections, stomach pain, and bronchitis.
These are not all the possible side effects of TREMFYA®. Call your doctor for medical advice about side effects.
Use TREMFYA® exactly as your healthcare provider tells you to use it.
Please read the full Prescribing Information, including Medication Guide, for TREMFYA® and discuss any questions that you have with your doctor.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit , or call 1-800-FDA-1088.
Dosage Forms and Strengths: TREMFYA® is available as 100 mg/mL and 200 mg/2mL for subcutaneous injection and as a 200 mg/20 mL (10 mg/mL) single dose vial for intravenous infusion.
ABOUT JOHNSON & JOHNSON
At Johnson & Johnson, we believe health is everything. Our strength in healthcare innovation empowers us to build a world where complex diseases are prevented, treated, and cured, where treatments are smarter and less invasive, and solutions are personal. Through our expertise in Innovative Medicine and MedTech, we are uniquely positioned to innovate across the full spectrum of healthcare solutions today to deliver the breakthroughs of tomorrow, and profoundly impact health for humanity.
Learn more at or at
Follow us at @JNJInnovMed.
Janssen Research & Development, LLC and Janssen Biotech, Inc. are Johnson & Johnson companies.
Cautions Concerning Forward-Looking Statements
This press release contains "forward-looking statements" as defined in the Private Securities Litigation Reform Act of 1995 regarding TREMFYA®. The reader is cautioned not to rely on these forward-looking statements. These statements are based on current expectations of future events. If underlying assumptions prove inaccurate or known or unknown risks or uncertainties materialize, actual results could vary materially from the expectations and projections of Johnson & Johnson. Risks and uncertainties include, but are not limited to: challenges and uncertainties inherent in product research and development, including the uncertainty of clinical success and of obtaining regulatory approvals; uncertainty of commercial success; manufacturing difficulties and delays; competition, including technological advances, new products and patents attained by competitors; challenges to patents; product efficacy or safety concerns resulting in product recalls or regulatory action; changes in behavior and spending patterns of purchasers of health care products and services; changes to applicable laws and regulations, including global health care reforms; and trends toward health care cost containment. A further list and descriptions of these risks, uncertainties and other factors can be found in Johnson & Johnson's most recent Annual Report on Form 10-K, including in the sections captioned "Cautionary Note Regarding Forward-Looking Statements" and "Item 1A. Risk Factors," and in Johnson & Johnson's subsequent Quarterly Reports on Form 10-Q and other filings with the Securities and Exchange Commission. Copies of these filings are available online at , or on request from Johnson & Johnson. Johnson & Johnson does not undertake to update any forward-looking statement as a result of new information or future events or developments.
References:
1 Peyrin-Biroulet, et al. Efficacy and safety of subcutaneous guselkumab induction therapy in patients with Ulcerative Colitis: Results through week 12 from the phase 3 ASTRO study. Results from the Phase 3 ASTRO study. Oral presentation (#OP10) at the 20th Congress of the European Crohn's and Colitis Organization (ECCO). February 2025.
2 Long M, et al. Efficacy And Safety Of Subcutaneous Guselkumab Induction Therapy In Patients With Ulcerative Colitis: Results Through Week 24 From The Phase 3 Astro Study. Oral presentation (#4241895) at Digestive Disease Week 2025. May 2025.
3 Atreya R, Abreu MT, Krueger JG, et al. Guselkumab, an IL-23p19 subunit-specific monoclonal antibody, binds CD64+ myeloid cells and potentially neutralizes IL-23 produced from the same cells. Poster presented at: 18th Congress of the European Crohn's and Colitis Organization (ECCO); March 1-4, 2023; Copenhagen, Denmark. Poster P504.
4 Kreuger JG, Eyerich K, Kuchroo VK. Il-23 past, present, and future: a roadmap to advancing IL-23 science and therapy. Front Immunol. 2024; 15:1331217. doi:10.3389/fimmu.2024.1331217.
5 TREMFYA® [Prescribing Information]. Horsham, PA: Janssen Biotech, Inc.
6 Skyrizi® [Prescribing Information]. North Chicago, IL: AbbVie, Inc.
7 Omvoh™ [Prescribing Information]. Indianapolis, IN: Eli Lilly and Company.
8 National Institutes of Health: Clinicaltrials.gov. A Study of Guselkumab Therapy in Participants With Moderately to Severely Active Ulcerative Colitis (ASTRO). Identifier: NCT05528510. . Accessed March 2025.
9 Crohn's & Colitis Foundation. What is ulcerative colitis? Available at: . Accessed March 2025
SOURCE Johnson & Johnson
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果临床3期上市批准
2025-05-05
SPY001 is a novel, half-life extended α4β7 antibody in development for the treatment of Inflammatory Bowel Disease (IBD)
SPY001 pharmacokinetic (PK) data up to eight months continues to support a potential best-in-class profile, including a half-life more than three times that of vedolizumab
SPY001 pharmacodynamic (PD) data up to eight months showed that a single dose of SPY001 resulted in rapid and sustained saturation of α4β7 receptors at expected Phase 2 trough concentrations
Spyre remains on track to initiate its planned platform Phase 2 trial in mid-2025 that includes SPY001, followed by SPY002 (TL1A), SPY003 (IL-23), and combinations thereof, with initial monotherapy data expected in 2026
WALTHAM, Mass., May 5, 2025 /PRNewswire/ -- Spyre Therapeutics, Inc. (NASDAQ: SYRE) (the "Company" or "Spyre"), a clinical-stage biotechnology company advancing best-in-class antibody engineering, dose optimization, and rational therapeutic combinations for the treatment of Inflammatory Bowel Disease ("IBD") and other immune-mediated diseases, today announced two poster presentations at Digestive Disease Week (DDW) 2025, being held May 3-6, 2025, in San Diego, California.
Spyre presented results out to eight months of follow up from its SPY001 Phase 1 program. Updated results from our ongoing Phase 1 trial of SPY001, our novel half-life extended α4β7 antibody for the treatment of IBD, continues to show that SPY001 is well tolerated, has a half-life of more than three-fold compared to vedolizumab based on population PK modeling, and sustains target engagement at expected Phase 2 trough concentrations. This longer follow-up data strengthens the potential for SPY001 to demonstrate improved induction responses with greater exposures as well as durable responses with quarterly or biannual maintenance dosing.
Spyre presented expanded preclinical data on combined inhibition of α4β7 integrin and TL1A cytokine in murine colitis models. Data presented demonstrate that combined inhibition of α4β7 integrin and TL1A cytokine is superior to either monotherapy in mouse models of colitis.
"Extended follow-up data continue to show that SPY001 is well tolerated and has a PK and PD profile that supports potential best-in-class quarterly or biannual dosing for patients with IBD," said Deanna Nguyen, MD, SVP of Clinical Development at Spyre. "We look forward to testing SPY001 as a monotherapy and as a backbone for combinations in our Phase 2 platform trial in ulcerative colitis patients, which remains on-track to begin mid-year."
The poster will be available for viewing during the DDW exhibition, and details are as follows:
Title: Interim PK Data for SPY001, a Novel Half-Life Extended Monoclonal Antibody Targeting α4β7, Suggest a Potential for Q3M or Q6M Maintenance Dosing for Inflammatory Bowel Disease
Authors: D Nguyen, L Yan, K Hew, P Patel, R McLean, R Himes, T Das, M Huyghe, B Connolly, J Friedman
Title: Combined inhibition of TL1A and integrin β7 is superior to either monotherapy in mouse models of colitis and coadministration of SPY001 and SPY002 demonstrates no drug-drug effects on exposure in non-human primates
Authors: M Siegel, J Friedman, D Nguyen, J McNally, M Kennedy, O Ballew, M Rose, A Spencer
Full session details can be accessed via the DDW Program.
About SPY001
SPY001 is an investigational novel, extended half-life monoclonal antibody targeting α4β7 for the treatment of IBD. IBD is a chronic condition characterized by inflammation in the gastrointestinal tract and encompasses two main disorders: ulcerative colitis and Crohn's disease. In the United States, it is estimated that approximately 2.4 million individuals currently have IBD. SPY001 targets the same epitope as vedolizumab and demonstrates equivalent potency and selectivity as vedolizumab in head-to-head preclinical studies. Interim data from a Phase 1 trial demonstrated that SPY001 was well tolerated and exhibited a human half-life of ~80 days, approximately three-fold greater than vedolizumab. This half-life supports potential quarterly or biannual SC maintenance dosing in a single autoinjector compared to vedolizumab's Q2W SC profile. Based on initial Phase 1 clinical data, the company plans to initiate a Phase 2 platform trial in ulcerative colitis in mid-2025.
About Spyre Therapeutics
Spyre Therapeutics is a biotechnology company that aims to create next-generation inflammatory bowel disease (IBD) and other immune-mediated disease products by combining best-in-class antibody engineering, dose optimization, and rational therapeutic combinations. Spyre's pipeline includes extended half-life antibodies targeting α4β7, TL1A, and IL-23. For more information, visit Spyre's website at .
Forward-Looking
Statements
Certain statements in this press release, other than purely historical information, may constitute "forward-looking statements" within the meaning of the federal securities laws, including for purposes of the safe harbor provisions under the United States Private Securities Litigation Reform Act of 1995, concerning Spyre and other matters. These forward-looking statements include, but are not limited to, express or implied statements relating to Spyre's management team's expectations, hopes, beliefs, intentions or strategies regarding the future including, without limitation, Spyre's ability to achieve the expected benefits or opportunities with respect to its pipeline of product candidates such as potential best-in-class dosing regimen and safety profile of SPY001 in humans; expectations regarding the drug delivery of SPY001, including in the form of a single autoinjector; Spyre's future clinical development activities, including the expected design and timing of the planned platform Phase 2 trial of SPY001, SPY002, SPY003 and combinations thereof and timing of each cohort and data readouts; the potential therapeutic benefits of Spyre's product candidates as monotherapies or in combinations and their extended half-life, including the expected duration of half-life in comparison to competitor products and the potential efficacy, durability and exposure of induction responses for SPY001; and the timing and results of clinical trials. In addition, any statements that refer to projections, forecasts or other characterizations of future events or circumstances, including any underlying assumptions, are forward-looking statements. The words "opportunity," "potential," "milestones," "pipeline," "can," "goal," "aim," "strategy," "target," "seek," "anticipate," "achieve," "believe," "contemplate," "continue," "could," "estimate," "expect," "intends," "may," "might," "plan," "possible," "predict," "project," "should," "will," "would," and similar expressions (including the negatives of these terms or variations of them) may identify forward-looking statements, but the absence of these words does not mean that a statement is not forward-looking. These forward-looking statements are based on current expectations and beliefs concerning future developments and their potential effects. There can be no assurance that future developments affecting Spyre will be those that have been anticipated. These forward-looking statements involve a number of risks, uncertainties (some of which are beyond Spyre's control) or other assumptions that may cause actual results or performance to be materially different from those expressed or implied by these forward-looking statements. These risks and uncertainties include, but are not limited those uncertainties and factors described under the heading "Risk Factors" and "Note about Forward-Looking Statements" in Spyre's most recent Annual Report on From 10-K filed with the SEC, as well as discussions of potential risks, uncertainties, and other important factors included in other filings by Spyre from time to time. Should one or more of these risks or uncertainties materialize, or should any of Spyre's assumptions prove incorrect, actual results may vary in material respects from those projected in these forward-looking statements. Nothing in this press release should be regarded as a representation by any person that the forward-looking statements set forth therein will be achieved or that any of the contemplated results of such forward-looking statements will be achieved. You should not place undue reliance on forward-looking statements in this press release, which speak only as of the date they are made and are qualified in their entirety by reference to the cautionary statements herein. Spyre does not undertake or accept any duty to make any updates or revisions to any forward-looking statements. This press release does not purport to summarize all of the conditions, risks and other attributes of an investment in Spyre.
SOURCE Spyre Therapeutics, Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床1期临床2期免疫疗法临床结果抗体药物偶联物
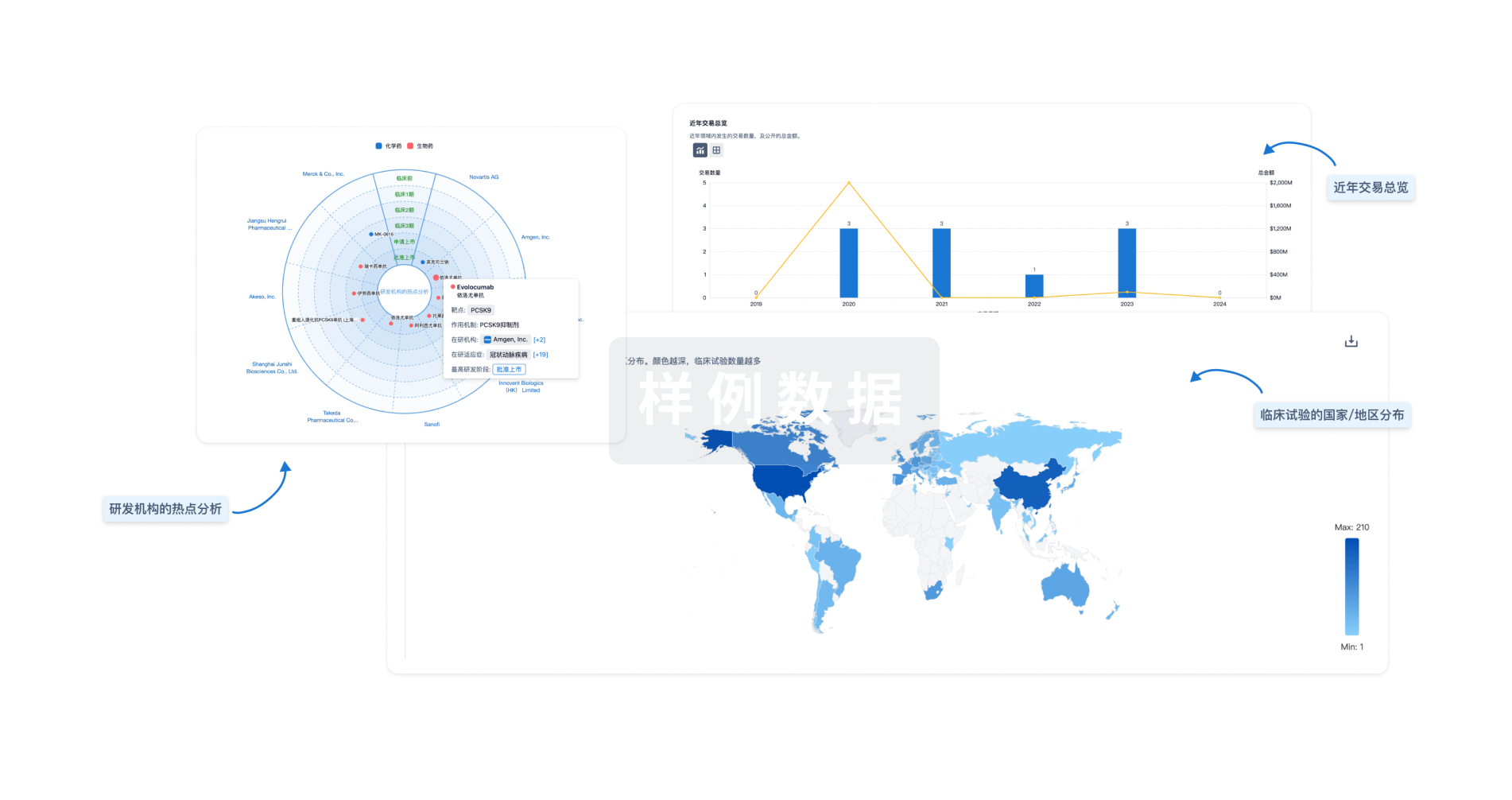
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

