预约演示
更新于:2025-05-07
IL-23 x VEGI
更新于:2025-05-07
关联
7
项与 IL-23 x VEGI 相关的药物作用机制 IL-12p40抑制剂 [+1] |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
作用机制 IL-23抑制剂 [+1] |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
作用机制 IL-23调节剂 [+1] |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
1
项与 IL-23 x VEGI 相关的临床试验NCT05536440
A PHASE 1, RANDOMIZED, DOUBLE-BLIND, SPONSOR OPEN, PLACEBO CONTROLLED, DOSE ESCALATING STUDY TO EVALUATE THE SAFETY, TOLERABILITY, PHARMACOKINETICS, AND PHARMACODYNAMICS OF SINGLE INTRAVENOUS AND MULTIPLE SUBCUTANEOUS AND INTRAVENOUS DOSES OF PF-07261271 IN HEALTHY PARTICIPANTS
The purpose of this clinical trial is to learn about the safety and effects of the study medicine PF-07261271 for the potential treatment of Inflammatory Bowel Disease.
开始日期2022-10-17 |
申办/合作机构 |
100 项与 IL-23 x VEGI 相关的临床结果
登录后查看更多信息
100 项与 IL-23 x VEGI 相关的转化医学
登录后查看更多信息
0 项与 IL-23 x VEGI 相关的专利(医药)
登录后查看更多信息
27
项与 IL-23 x VEGI 相关的文献(医药)2024-09-25·Cureus
Shared Pathophysiology of Inflammatory Bowel Disease and Psoriasis: Unraveling the Connection
Review
作者: Ali Ahmed, Aaliya ; Pino, Nohelia ; Sulaiman, Hakam ; Marepalli, Nitheesha Reddy ; Abraham Suárez Álvarez, José ; Rajeev Joshi, Megha ; Tabbarah, Shadi ; Ansah Owusu, Frank ; Saleem Azam, Samra
2024-01-01·Therapeutic Advances in Gastroenterology
Advancing therapeutic frontiers: a pipeline of novel drugs for luminal and perianal Crohn's disease management
Review
作者: Angriman, Imerio ; Bonazzi, Erica ; Savarino, Edoardo Vincenzo ; de Barba, Caterina ; Lorenzon, Greta ; Facchin, Sonia ; Zingone, Fabiana ; Scarpa, Marco ; Buda, Andrea ; Barberio, Brigida ; Zanconato, Miriana ; Ruffolo, Cesare ; Crepaldi, Martina ; Bertin, Luisa ; Maniero, Daria
2022-11-10·Human Molecular Genetics2区 · 生物学
Identification of shared loci associated with both Crohn’s disease and leprosy in East Asians
2区 · 生物学
Article
作者: Park, Dohoon ; Jung, Seulgi ; Ye, Byong Duk ; Han, Buhm ; Yang, Suk-Kyun ; Liu, Jianjun ; Lee, Ho-Su ; Song, Kyuyoung ; Kim, Yongjae ; Baek, Jiwon ; Sun, Yonghu ; Liu, Hong ; Zhang, Furen ; Park, Sang Hyoung ; Hwang, Sung Wook
114
项与 IL-23 x VEGI 相关的新闻(医药)2025-05-05
SPY001 is a novel, half-life extended α4β7 antibody in development for the treatment of Inflammatory Bowel Disease (IBD)
SPY001 pharmacokinetic (PK) data up to eight months continues to support a potential best-in-class profile, including a half-life more than three times that of vedolizumab
SPY001 pharmacodynamic (PD) data up to eight months showed that a single dose of SPY001 resulted in rapid and sustained saturation of α4β7 receptors at expected Phase 2 trough concentrations
Spyre remains on track to initiate its planned platform Phase 2 trial in mid-2025 that includes SPY001, followed by SPY002 (TL1A), SPY003 (IL-23), and combinations thereof, with initial monotherapy data expected in 2026
WALTHAM, Mass., May 5, 2025 /PRNewswire/ -- Spyre Therapeutics, Inc. (NASDAQ: SYRE) (the "Company" or "Spyre"), a clinical-stage biotechnology company advancing best-in-class antibody engineering, dose optimization, and rational therapeutic combinations for the treatment of Inflammatory Bowel Disease ("IBD") and other immune-mediated diseases, today announced two poster presentations at Digestive Disease Week (DDW) 2025, being held May 3-6, 2025, in San Diego, California.
Spyre presented results out to eight months of follow up from its SPY001 Phase 1 program. Updated results from our ongoing Phase 1 trial of SPY001, our novel half-life extended α4β7 antibody for the treatment of IBD, continues to show that SPY001 is well tolerated, has a half-life of more than three-fold compared to vedolizumab based on population PK modeling, and sustains target engagement at expected Phase 2 trough concentrations. This longer follow-up data strengthens the potential for SPY001 to demonstrate improved induction responses with greater exposures as well as durable responses with quarterly or biannual maintenance dosing.
Spyre presented expanded preclinical data on combined inhibition of α4β7 integrin and TL1A cytokine in murine colitis models. Data presented demonstrate that combined inhibition of α4β7 integrin and TL1A cytokine is superior to either monotherapy in mouse models of colitis.
"Extended follow-up data continue to show that SPY001 is well tolerated and has a PK and PD profile that supports potential best-in-class quarterly or biannual dosing for patients with IBD," said Deanna Nguyen, MD, SVP of Clinical Development at Spyre. "We look forward to testing SPY001 as a monotherapy and as a backbone for combinations in our Phase 2 platform trial in ulcerative colitis patients, which remains on-track to begin mid-year."
The poster will be available for viewing during the DDW exhibition, and details are as follows:
Title: Interim PK Data for SPY001, a Novel Half-Life Extended Monoclonal Antibody Targeting α4β7, Suggest a Potential for Q3M or Q6M Maintenance Dosing for Inflammatory Bowel Disease
Authors: D Nguyen, L Yan, K Hew, P Patel, R McLean, R Himes, T Das, M Huyghe, B Connolly, J Friedman
Title: Combined inhibition of TL1A and integrin β7 is superior to either monotherapy in mouse models of colitis and coadministration of SPY001 and SPY002 demonstrates no drug-drug effects on exposure in non-human primates
Authors: M Siegel, J Friedman, D Nguyen, J McNally, M Kennedy, O Ballew, M Rose, A Spencer
Full session details can be accessed via the DDW Program.
About SPY001
SPY001 is an investigational novel, extended half-life monoclonal antibody targeting α4β7 for the treatment of IBD. IBD is a chronic condition characterized by inflammation in the gastrointestinal tract and encompasses two main disorders: ulcerative colitis and Crohn's disease. In the United States, it is estimated that approximately 2.4 million individuals currently have IBD. SPY001 targets the same epitope as vedolizumab and demonstrates equivalent potency and selectivity as vedolizumab in head-to-head preclinical studies. Interim data from a Phase 1 trial demonstrated that SPY001 was well tolerated and exhibited a human half-life of ~80 days, approximately three-fold greater than vedolizumab. This half-life supports potential quarterly or biannual SC maintenance dosing in a single autoinjector compared to vedolizumab's Q2W SC profile. Based on initial Phase 1 clinical data, the company plans to initiate a Phase 2 platform trial in ulcerative colitis in mid-2025.
About Spyre Therapeutics
Spyre Therapeutics is a biotechnology company that aims to create next-generation inflammatory bowel disease (IBD) and other immune-mediated disease products by combining best-in-class antibody engineering, dose optimization, and rational therapeutic combinations. Spyre's pipeline includes extended half-life antibodies targeting α4β7, TL1A, and IL-23. For more information, visit Spyre's website at .
Forward-Looking
Statements
Certain statements in this press release, other than purely historical information, may constitute "forward-looking statements" within the meaning of the federal securities laws, including for purposes of the safe harbor provisions under the United States Private Securities Litigation Reform Act of 1995, concerning Spyre and other matters. These forward-looking statements include, but are not limited to, express or implied statements relating to Spyre's management team's expectations, hopes, beliefs, intentions or strategies regarding the future including, without limitation, Spyre's ability to achieve the expected benefits or opportunities with respect to its pipeline of product candidates such as potential best-in-class dosing regimen and safety profile of SPY001 in humans; expectations regarding the drug delivery of SPY001, including in the form of a single autoinjector; Spyre's future clinical development activities, including the expected design and timing of the planned platform Phase 2 trial of SPY001, SPY002, SPY003 and combinations thereof and timing of each cohort and data readouts; the potential therapeutic benefits of Spyre's product candidates as monotherapies or in combinations and their extended half-life, including the expected duration of half-life in comparison to competitor products and the potential efficacy, durability and exposure of induction responses for SPY001; and the timing and results of clinical trials. In addition, any statements that refer to projections, forecasts or other characterizations of future events or circumstances, including any underlying assumptions, are forward-looking statements. The words "opportunity," "potential," "milestones," "pipeline," "can," "goal," "aim," "strategy," "target," "seek," "anticipate," "achieve," "believe," "contemplate," "continue," "could," "estimate," "expect," "intends," "may," "might," "plan," "possible," "predict," "project," "should," "will," "would," and similar expressions (including the negatives of these terms or variations of them) may identify forward-looking statements, but the absence of these words does not mean that a statement is not forward-looking. These forward-looking statements are based on current expectations and beliefs concerning future developments and their potential effects. There can be no assurance that future developments affecting Spyre will be those that have been anticipated. These forward-looking statements involve a number of risks, uncertainties (some of which are beyond Spyre's control) or other assumptions that may cause actual results or performance to be materially different from those expressed or implied by these forward-looking statements. These risks and uncertainties include, but are not limited those uncertainties and factors described under the heading "Risk Factors" and "Note about Forward-Looking Statements" in Spyre's most recent Annual Report on From 10-K filed with the SEC, as well as discussions of potential risks, uncertainties, and other important factors included in other filings by Spyre from time to time. Should one or more of these risks or uncertainties materialize, or should any of Spyre's assumptions prove incorrect, actual results may vary in material respects from those projected in these forward-looking statements. Nothing in this press release should be regarded as a representation by any person that the forward-looking statements set forth therein will be achieved or that any of the contemplated results of such forward-looking statements will be achieved. You should not place undue reliance on forward-looking statements in this press release, which speak only as of the date they are made and are qualified in their entirety by reference to the cautionary statements herein. Spyre does not undertake or accept any duty to make any updates or revisions to any forward-looking statements. This press release does not purport to summarize all of the conditions, risks and other attributes of an investment in Spyre.
SOURCE Spyre Therapeutics, Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床1期临床2期免疫疗法临床结果抗体药物偶联物
2025-04-30
·小药说药
-01-引言炎症性肠病(IBD)由溃疡性结肠炎(UC)和克罗恩病(CD)组成,全球约有600万至800万人受到影响。作为一种慢性、进行性和复发性的肠道疾病,IBD严重影响患者的生活质量和日常生活,增加医疗负担。虽然目前普遍认为IBD是由遗传易感个体对微生物的异常免疫反应引起的,但其确切的发病机制在很大程度上尚不清楚。目前可用的IBD治疗包括非靶向治疗(如氨基水杨酸、糖皮质激素和免疫调节剂)和靶向治疗(如抗TNF、抗IL-12/IL-23和抗α4β7整合素)。虽然生物靶向疗法对许多患者有效,但依然有高达30%的患者对初始治疗没有反应,高达50%的患者随着时间的推移反应消失。因此,深刻理解肠免疫系统的运行机制和IBD的免疫发病机制,将有助于我们开发针对IBD的免疫治疗药物,并为IBD提供了新的免疫治疗手段。-02-一、肠道免疫系统肠道微生物群人类肠道微生物群由数万亿种微生物组成,包括真菌、单细胞动物、病毒、古生菌和占绝大多数的细菌。肠道微生物群通过调节固有免疫系统的激活,影响宿主能量代谢、免疫稳态和成熟,以及维持粘膜完整性,在IBD的发病机制中发挥着至关重要的作用。越来越多的证据表明IBD患者肠道微生物群的组成发生了改变。例如,大肠杆菌作为病原菌在肠道中增加,具有在巨噬细胞中生存和复制的能力,并诱导IBD中TNF-α的分泌和炎症反应。此外,作为益生菌的prausnitzii粪杆菌可以刺激DC分泌抗炎细胞因子IL-10,并抑制肠道中IL-12和INF-γ的产生,而IBD患者的肠道中这些细胞因子显著减少。此外,IBD患者肠道微生物群的代谢产物也会发生改变,例如胆汁酸代谢中断、色氨酸代谢水平降低、SCFA减少以及烟酸、牛磺酸和酰基卡尼汀水平升高。这些代谢物在肠道炎症过程中的丢失可能是IBD发病的驱动力。肠上皮细胞(IECs)肠上皮是人体最大的粘膜表面,充当管腔内容物和潜在免疫系统之间的物理和生化屏障。它由单层不同亚型的特异性内皮细胞组成,主要包括柱状上皮、杯状细胞和Paneth细胞。杯状细胞作为肠上皮的分泌细胞,可以在肠粘膜的管腔表面分泌粘液,粘液层提供了第一道防线。Paneth细胞是一种特殊的含有颗粒的细胞,存在于小肠的上皮隐窝中,在先天性肠道防御和保护附近干细胞中起着至关重要的作用。它们可以产生抗菌肽(AMP),如α-防御素、溶菌酶C、磷脂酶和C型凝集素等,这些抗菌肽可以对抗侵入的管腔病原体。已经证明,AMP在CD患者中存在缺陷。肠上皮的另一个重要组成部分是顶端连接复合体,由紧密连接(TJ)、粘附连接(AJ)和桥粒组成,紧密密封肠上皮细胞,以防止病原体进入,并调节对水、离子和营养素的渗透性。编码TJ的基因突变和TJ功能障碍已被阐明为IBD的关键致病因素。肠道免疫细胞肠道免疫细胞可分为天然免疫细胞和适应性免疫细胞,这两种细胞对IBD的免疫反应都有很大贡献。固有免疫细胞,如巨噬细胞、树突状细胞(DC)、中性粒细胞、自然杀伤(NK)细胞和固有淋巴细胞(ILC),相互作用并产生细胞因子、趋化因子和抗菌素,以触发炎症,导致吞噬、抗原提呈和适应性免疫系统的激活。巨噬细胞、树突状细胞、中性粒细胞、NKT细胞和ILC构成粘膜固有免疫系统的第一道防线。这些固有免疫系统的免疫细胞通过病原体相关分子模式(PAMP),导致多种信号通路的激活,并产生促炎细胞因子、趋化因子和抗菌肽。与天然免疫细胞相比,适应性免疫细胞具有高度的特异性和免疫记忆能力,它们相互补充,消除入侵病原体。适应性免疫反应的关键参与者是T细胞,在肠道相关淋巴组织(GALT)或肠系膜淋巴结中的抗原刺激下,原始T细胞被激活并分化为不同的亚群,在趋化因子受体(如CCR9和CCR10)和整合素等细胞粘附分子作用下迁移到肠道的炎症部位。如今,许多针对这些受体的药物已成功用于临床实践,以阻止T细胞向肠道迁移,以预防IBD患者的炎症。-03- 二、IBD的免疫学发病机制IL-22和IL-6IL-22是一种多效性细胞因子,由Th22、Th17和Th1细胞分泌,激活STAT3以促进肠组织修复并抑制肠道病原体。在IBD中,IL-22受微生物群的信号诱导在小肠中广泛表达。此外,IL-22还促进IBD易感基因如fut2、sec1、bcl2115和PTPN22的表达。IL-6主要由固有层中的巨噬细胞和树突状细胞产生。研究发现,CD患者血清和肠道中IL-6水平升高,并与临床疾病活动、复发频率和炎症严重程度相关。与受体结合后,IL-6激活gp130阳性T细胞,导致STAT-3信号转导和转录激活,随后激活抗凋亡基因Bcl-2和Bcl-xl的转录。目前,人源化抗IL-6R单克隆抗体tocilizumab已经用于治疗IBD。IL-12/IL-23由树突状细胞产生的IL-12和IL-23均属于IL-12家族,在慢性炎症性疾病的发病机制中发挥重要作用。在几种结肠炎模型中,致病性T细胞反应由IL-12和IL-23驱动。IL-12可以促进原始CD4+T细胞分化为产生IFN-γ的Th1细胞,并促进NK细胞、NKT细胞和细胞毒性T细胞的增殖和效应功能。IL-23通过加强和影响Th17细胞反应来发挥其生物学功能,同时它还拮抗抗炎Foxp3+Treg细胞反应从而促进肠道炎症。IL-17IL-17细胞因子,包括IL-17A和IL-17F,也在IBD的发病机制中发挥重要作用。全基因组关联研究(GWAS)已确定了许多与Th17相关的IBD易感基因,包括JAK2、STAT3、IL-23R、IL-12B和CCR6。临床研究发现,与健康对照组相比,IBD患者的肠粘膜和固有层中含有更高水平的Th17细胞、IL-17和IL-23。在小鼠模型中,IL-17A和IL-17F的缺陷显示对结肠炎具有保护作用。Il-10IL-10是抑制免疫系统促炎反应的最重要细胞因子,可由大量不同类型的细胞产生,包括Treg、巨噬细胞、树突状细胞等。在IBD患者的早期发病过程中,IL-10R亚单位基因的突变与肠道炎症免疫反应有关。事实上,IL-10和IL-10R缺陷小鼠都可以发生自发性结肠炎。此外,Treg细胞中c-MAF失活也会导致IL-10产生功能障碍,从而发展为自发性结肠炎。IL-1β家族细胞因子IL-1β是一种由巨噬细胞分泌的促炎细胞因子,与其他促炎细胞因子(如TNF-α和IL-6)协同作用,以诱导IBD炎症。研究发现,IL-10缺陷小鼠在自发性结肠炎发病前IL-1β分泌增加。此外,IL-1β和IL-18信号的遗传缺陷或抑制可缓解实验性结肠炎。TNF和TNF样配体1A(TL1A)TNF被认为是IBD发病机制中的促炎细胞因子,可刺激急性期时的反应,促进IL-1和IL-6的分泌,增加粘附分子的表达。研究发现,活动期IBD患者的血液、上皮组织和粪便中TNF-α显著升高,其水平与CD患者的临床疾病活动性相关。通过抗TNF-α单克隆抗体阻断TNF-α信号已成为中重度难治性IBD患者的重要治疗方法。TNF家族成员TL1A也被发现是肠道炎症的关键介质,在IBD患者中水平也升高。TL1A主要通过结合死亡受体3(DR3)发挥其功能,TL1A还可以协同促进IL-4、IL-12和IL-23的产生,并通过Th1、Th2和Th17细胞增加DR3的表达,以促进炎症。免疫细胞迁移免疫细胞迁移到肠道以启动和维持免疫反应是IBD的关键发病机制,其中T细胞迁移是最重要的一个。免疫细胞迁移的完整过程包括栓系、滚动、激活、粘附和外渗,涉及各种整合素、选择素、趋化因子及其配体或受体,例如促进迁移到小肠的整合素α4β7、α4β1、β2整合素和CCR9。针对免疫细胞迁移不同阶段的多种治疗方法已经应用于临床。-04-三、IBD的免疫治疗目前,7种生物制剂已被美国食品和药物管理局(FDA)正式批准用于治疗IBD,许多治疗IBD的创新候选药物的临床试验也正在进行中。靶向TNF-α抗TNF的抗体已广泛使用约25年。目前,四种TNF-α抑制剂已被批准用于临床,包括infliximab、adalimumab、golimumab和certolizumab pegol。infliximab可诱导粘膜溃疡愈合,这是第一种被批准用于CD肛周瘘的治疗方法,并被证明对CD和UC都有效。Adalimumab被证明可诱导CD的粘膜愈合,它对CD和UC以及对infliximab失去反应的CD患者也有效。此外,golimumab和certolizumab pegol也在美国被批准用于治疗UC。虽然抗肿瘤坏死因子治疗显示出临床疗效,但10-30%的IBD患者没有响应,20-40%的患者随着时间的推移失去响应。靶向IL-12/IL-23Ustekinumab是针对IL-12和IL-23的p40亚单位的单克隆抗体,在治疗IBD中显示出积极作用,它是目前FDA批准的唯一一种抗IL-23疗法。另一个靶点是针对IL-23的p19亚单位,也显示出了临床疗效,包括risankizumab、brazikumab、guselkumab和Mirikizumab。然而,这些抗体仍处于临床试验阶段。靶向JAKJanus激酶(JAK)家族包含四种细胞内酪氨酸激酶:JAK1、JAK2、JAK3和非受体酪氨酸蛋白激酶2,它们激活STAT通路并在IBD的发病机制中发挥关键作用。目前,已经评估了10种JAK抑制剂对IBD的临床疗效,而Tofacitinib是唯一具有临床疗效的抑制剂,并被批准用于UC的临床治疗。靶向细胞粘附分子作为T细胞募集和肠道炎症的重要介质,细胞粘附分子是IBD的潜在靶点。例如,抗α4β7整合素抗体vedolizumab和抗a4整合素单克隆抗体natalizumab在治疗IBD方面显示出了很好的疗效,目前已被批准并广泛应用于临床。此外,Etrolizumab(一种选择性结合β7亚单位的单克隆抗体)、abrilumab(一种阻断α4β7整合素的单克隆抗体)和ontamalimab(一种靶向MAdCAM-1的人源化抗体)在临床前数据中也显示出疗效,目前仍在进行临床试验。靶向NLRP3炎症小体NLRP3炎症小体和促炎细胞因子水平升高是IBD的主要病理机制。已经观察到CD患者具有高水平的NLRP3炎症小体。此外,活化的NLRP3炎性小体可促进过量IL-1β的产生,并改变结肠上皮中TJ的表达,从而加速疾病进展。因此,靶向NLRP3炎症小体为IBD治疗提供了一种有前景的策略。-05-结语在过去的几十年里,IBD的免疫学机制取得了很大进展,为IBD的治疗提供了新的策略和新的思路。在未来,特定基因位点的改变可能是IBD很有希望的治疗方法。此外,新型抗体或抑制剂、联合治疗方案和多因子阻断剂也有望打破IBD治疗的瓶颈,为IBD的患者的疾病改善带来福音。参考资料:1.Immunology of Inflammatory Bowel Disease: Molecular Mechanisms and Therapeutics. J Inflamm Res.2022; 15: 1825–1844.
免疫疗法微生物疗法
2025-04-30
— XENITH-UC, a Phase 2b study of XmAb942 in participants with ulcerative colitis, to begin in the second half of 2025 —
— Single and multiple doses of XmAb942 are well tolerated and safety profile is consistent with the anti-TL1A drug class —
— XmAb942 half-life supports a 12-week maintenance dosing interval in XENITH-UC —
— Lead selection for XmAb TL1A x IL23p19 program on track for first-in-human study start in 2026 —
— Management hosting webcast and conference call at 5:00 p.m. ET / 2:00 p.m. PT today —
PASADENA, CA, USA I April 29, 2025 I
Xencor, Inc. (NASDAQ:XNCR), a clinical-stage biopharmaceutical company developing engineered antibodies for the treatment of cancer and autoimmune diseases, today announced positive interim results from its first-in-human study of XmAb942, a high-potency, extended half-life, investigational anti-TL1A antibody in clinical development for patients with inflammatory bowel disease (IBD), such as ulcerative colitis (UC) and Crohn’s disease (CD). Interim results from the healthy volunteer dose-escalation study indicate that XmAb942 is well tolerated at single and multiple doses. Pharmacokinetic analysis of the single dose cohorts estimates a human half-life of greater than 71 days for XmAb942, which supports a 12-week dosing interval during maintenance treatment.
Based on these positive interim results, Xencor is initiating the XENITH clinical program, advancing XmAb942 into a Phase 2b study in patients with moderate-to-severely active UC (XENITH-UC), with the expected study start in the second half of 2025.
Lead selection for Xencor’s XmAb TL1A x IL23p19 bispecific antibody continues to advance. New
in vitro
studies show that several lead candidates match the target inhibition potency of commercial monospecific antibodies, but in a simple bispecific immunoglobulin G (IgG) format. Currently, these candidates are in final lead selection studies and manufacturing, in parallel, to prepare for the first-in-human study planned for 2026.
“Our Phase 1 data for XmAb942 validate our design goals for a best-in-class anti-TL1A therapy, combining high potency with less frequent dosing to potentially improve clinical outcomes and convenience for patients living with inflammatory bowel disease,” said Bassil Dahiyat, Ph.D., president and chief executive officer at Xencor. “We are excited to start our Phase 2b XENITH-UC trial later this year to efficiently support dose selection for pivotal studies, and we are poised to select our TL1A x IL23p19 bispecific lead candidate for an anticipated Phase 1 start in 2026. These and other milestones across our clinical portfolio are supported by our strong cash position.”
Key Highlights From Phase 1 Study Interim Results
The Phase 1 study of XmAb942 in healthy volunteers is a randomized, double-blind, placebo-controlled, dose-escalation trial, exploring intravenous (IV) and subcutaneous (SC) dose administration, at three escalating dose levels. The interim results reflect analyses with subjects in single dose cohorts (IV, n=24; SC, n=24) and in multiple dose cohorts (IV, n=16).
XENITH-UC: Phase 2b Study in Ulcerative Colitis (UC)
The Phase 2b study of XmAb942 in UC (XENITH-UC) will be a randomized, double-blind, placebo-controlled trial in patients with moderate-to-severely active UC, whose disease has progressed after at least one conventional or advanced therapy. XmAb942 will be administered intravenously during the 12-week induction period and subcutaneously every 12 weeks during the maintenance period. The primary endpoint of the study will be clinical remission based on the modified Mayo score at week 12. The study is designed to enroll approximately 220 patients across three induction dose levels and powered to enable Phase 3 dose selection. XENITH-UC is expected to start in the second half of 2025.
Conference Call and Webcast
Xencor will host a conference call and webcast today at 5:00 p.m. ET (2:00 p.m. PT) to review the interim results outlined in this news release. The live webcast of the conference call may be accessed through
this link
and through “Events & Presentations” in the Investors section of the Company’s website, located at
investors.xencor.com
. A recording will be available for at least 30 days.
About XmAb942
XmAb942 is a high-potency, extended half-life, investigational anti-TL1A antibody in clinical development for patients with inflammatory bowel disease (IBD), such as ulcerative colitis (UC) and Crohn’s disease (CD). The first generation of anti-TL1A antibodies, designed to block the interaction between the DR3 receptor and its ligand TL1A, have reduced disease activity in patients with UC and CD in multiple clinical studies. Interim results from a Phase 1 dose-escalation study in healthy volunteers indicate that XmAb942 is well tolerated at single and multiple doses. Pharmacokinetic analysis of the single dose cohorts estimates a human half-life of greater than 71 days for XmAb942, which supports a 12-week dosing interval during maintenance treatment.
About Xencor
Xencor is a clinical-stage biopharmaceutical company developing engineered antibodies for the treatment of patients with cancer and autoimmune diseases. More than 20 candidates engineered with Xencor’s XmAb® technology are in clinical development, and multiple XmAb medicines are marketed by partners. Xencor’s XmAb engineering technology enables small changes to a protein’s structure that result in new mechanisms of therapeutic action. For more information, please visit
www.xencor.com
.
SOURCE:
Xencor
临床1期临床2期临床结果免疫疗法
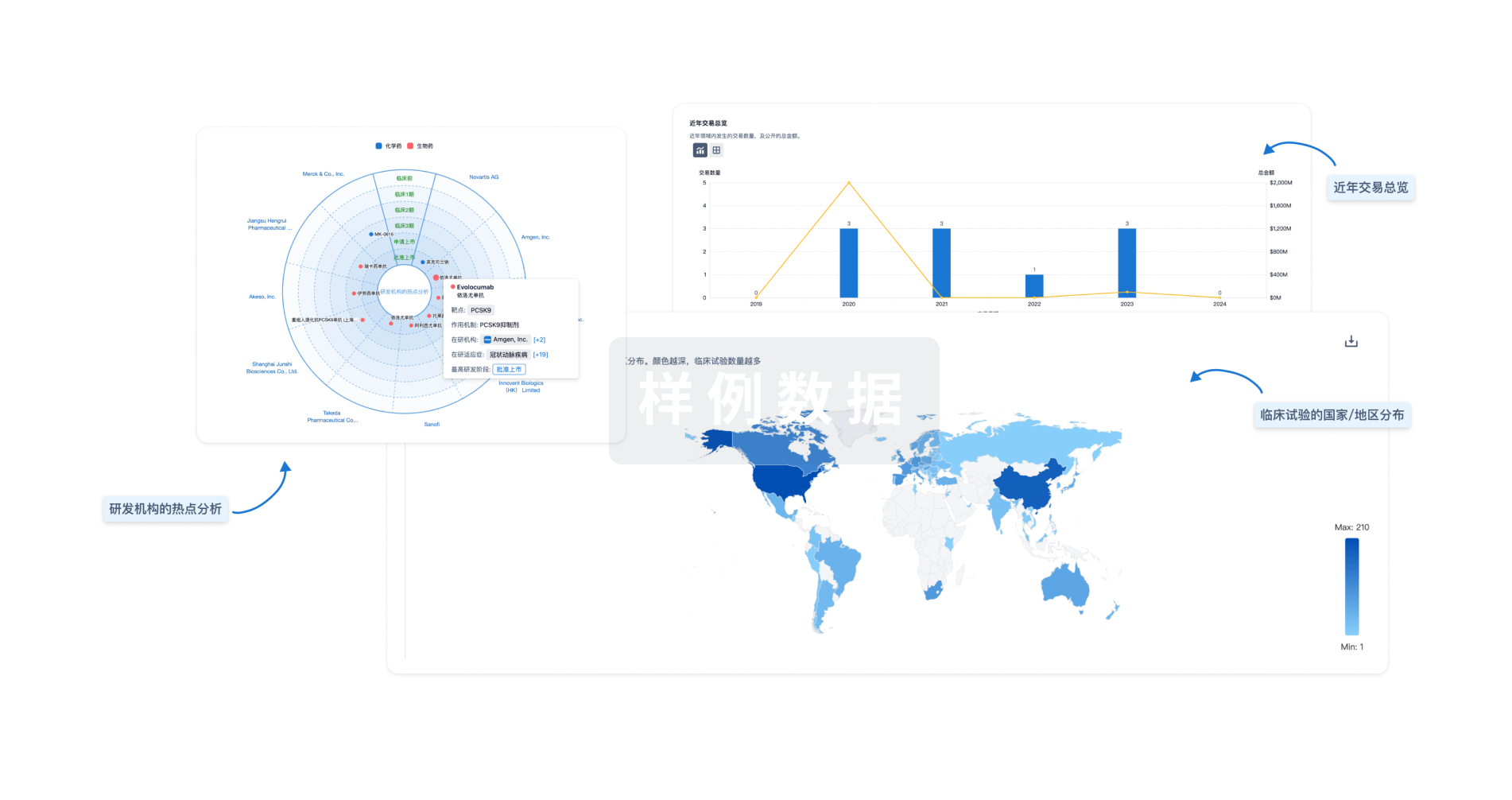
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


