预约演示
更新于:2025-05-07

Shenzhen Children's Hospital
更新于:2025-05-07
概览
关联
125
项与 深圳市儿童医院 相关的临床试验ChiCTR2500099839
A prospective study on the analgesic effect of PECS ? after lateral thoracotomy in children with congenital heart disease
开始日期2025-03-31 |
申办/合作机构 |
NCT06822400
A Multi-center, Randomized, Controlled Investigation of Tetralogy of Fallot in Neonates
Child health serves as the foundation for overall public health, with neonatal mortality recognized globally as a comprehensive indicator of national health standards and societal advancement. The Healthy Children Action Improvement Plan (2021-2025) sets a national target to reduce neonatal mortality in China to below 3.1‰. Congenital heart disease (CHD), the most prevalent congenital defect among neonates, constitutes a significant cause of disability and premature death in the Chinese population. Annually, approximately 70,000-80,000 neonates are born with CHD, among whom nearly 10,000 present with critical congenital heart disease (CCHD). Postnatal manifestations of CCHD often include cyanosis, hypoperfusion, and respiratory distress, with untreated cases resulting in approximately 50% mortality. CCHD is one of the leading causes of infant death.
Tetralogy of Fallot (TOF), the most common form of CCHD, accounts for a substantial proportion of cyanotic congenital heart diseases. It is characterized by four anatomical abnormalities: ventricular septal defect, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy. These structural defects disrupt intracardiac blood flow, reduce arterial oxygen saturation, and result in cyanosis and other related symptoms. Untreated TOF leads to significant health issues early in life, including growth retardation, recurrent hypoxic episodes, heart failure, and increased susceptibility to infections. Long-term survival is markedly reduced, with only a small proportion surviving into adulthood. Thus, surgical intervention is pivotal for improving outcomes in TOF(Tetralogy of Fallot) patients.
Despite advances in medical technology yielding satisfactory early outcomes, long-term prognosis following TOF correction remains a challenge. Historically, surgical strategies emphasized complete relief of right ventricular outflow tract obstruction, often at the expense of pulmonary valve function. Recent studies, however, highlight the critical role of preserving pulmonary valve function in improving long-term outcomes, as pulmonary valve dysfunction is a leading cause of late right ventricular failure and reintervention. Additionally, surgical approaches, whether via atrial or ventricular access, have inherent advantages and limitations, but neither can fully eliminate the risk of postoperative arrhythmias associated with TOF's anatomical complexity and surgical impact. These issues underscore the necessity for further advancements in long-term management strategies.
Surgical correction of TOF in a single-stage procedure has become standard practice, with the timing of surgery progressively shifting to earlier ages-from school age in the 1990s to the current standard of 3-6 months of age. This timing ensures sufficient weight and organ maturity to withstand the complexities of cardiac surgery. However, in clinical practice, significant challenges persist, including: (1) Deterioration during the waiting period, during which patients may experience recurrent hypoxic episodes, inadequate weight gain, and exacerbated pulmonary vascular underdevelopment, thereby complicating definitive surgery and increasing perioperative risk. (2) Developmental delays due to chronic hypoxemia and heart failure, potentially leading to neurological deficits and pulmonary hypertension, adversely affecting cognitive and motor development. Neonatal repair, performed within 28 days of life, may mitigate these challenges by restoring normal circulatory physiology at the earliest possible stage.
International guidelines endorse neonatal TOF repair for capable centers, citing the potential for enhanced clinical benefits and superior prognoses. Clinical observations at our center indicate several advantages of neonatal TOF repair, including reduced intraoperative bleeding, cleaner surgical fields, and better pulmonary vascular development. These benefits may be attributed to the regenerative potential of neonatal myocardial cells and the absence of prolonged pathological circulatory states, which otherwise exacerbate anatomical abnormalities. Early intervention may reduce right ventricular fibrosis and pulmonary vascular pathology, thereby improving long-term outcomes.
With advancements in surgical techniques and perioperative care, neonatal TOF repair has become a routine practice at our center, with over 100 cases performed annually for two consecutive years. This success is supported by an integrated prenatal-to-postnatal care model, establishing a comprehensive treatment framework.
Given this context, the investigators propose a multicenter, randomized controlled trial (RCT) to compare the safety and efficacy of neonatal and infant TOF repair. This study aims to provide high-quality evidence for clinical practice, determine optimal surgical timing, and enhance overall survival rates and quality of life for TOF patients.
Tetralogy of Fallot (TOF), the most common form of CCHD, accounts for a substantial proportion of cyanotic congenital heart diseases. It is characterized by four anatomical abnormalities: ventricular septal defect, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy. These structural defects disrupt intracardiac blood flow, reduce arterial oxygen saturation, and result in cyanosis and other related symptoms. Untreated TOF leads to significant health issues early in life, including growth retardation, recurrent hypoxic episodes, heart failure, and increased susceptibility to infections. Long-term survival is markedly reduced, with only a small proportion surviving into adulthood. Thus, surgical intervention is pivotal for improving outcomes in TOF(Tetralogy of Fallot) patients.
Despite advances in medical technology yielding satisfactory early outcomes, long-term prognosis following TOF correction remains a challenge. Historically, surgical strategies emphasized complete relief of right ventricular outflow tract obstruction, often at the expense of pulmonary valve function. Recent studies, however, highlight the critical role of preserving pulmonary valve function in improving long-term outcomes, as pulmonary valve dysfunction is a leading cause of late right ventricular failure and reintervention. Additionally, surgical approaches, whether via atrial or ventricular access, have inherent advantages and limitations, but neither can fully eliminate the risk of postoperative arrhythmias associated with TOF's anatomical complexity and surgical impact. These issues underscore the necessity for further advancements in long-term management strategies.
Surgical correction of TOF in a single-stage procedure has become standard practice, with the timing of surgery progressively shifting to earlier ages-from school age in the 1990s to the current standard of 3-6 months of age. This timing ensures sufficient weight and organ maturity to withstand the complexities of cardiac surgery. However, in clinical practice, significant challenges persist, including: (1) Deterioration during the waiting period, during which patients may experience recurrent hypoxic episodes, inadequate weight gain, and exacerbated pulmonary vascular underdevelopment, thereby complicating definitive surgery and increasing perioperative risk. (2) Developmental delays due to chronic hypoxemia and heart failure, potentially leading to neurological deficits and pulmonary hypertension, adversely affecting cognitive and motor development. Neonatal repair, performed within 28 days of life, may mitigate these challenges by restoring normal circulatory physiology at the earliest possible stage.
International guidelines endorse neonatal TOF repair for capable centers, citing the potential for enhanced clinical benefits and superior prognoses. Clinical observations at our center indicate several advantages of neonatal TOF repair, including reduced intraoperative bleeding, cleaner surgical fields, and better pulmonary vascular development. These benefits may be attributed to the regenerative potential of neonatal myocardial cells and the absence of prolonged pathological circulatory states, which otherwise exacerbate anatomical abnormalities. Early intervention may reduce right ventricular fibrosis and pulmonary vascular pathology, thereby improving long-term outcomes.
With advancements in surgical techniques and perioperative care, neonatal TOF repair has become a routine practice at our center, with over 100 cases performed annually for two consecutive years. This success is supported by an integrated prenatal-to-postnatal care model, establishing a comprehensive treatment framework.
Given this context, the investigators propose a multicenter, randomized controlled trial (RCT) to compare the safety and efficacy of neonatal and infant TOF repair. This study aims to provide high-quality evidence for clinical practice, determine optimal surgical timing, and enhance overall survival rates and quality of life for TOF patients.
开始日期2025-03-01 |
申办/合作机构 首都医科大学附属北京安贞医院 [+3] |
ChiCTR2500096065
Based on the Rasch model, a measurement reference standard was constructed to evaluate the functional impairment of patients with autism spectrum disorder
开始日期2025-02-01 |
申办/合作机构 |
100 项与 深圳市儿童医院 相关的临床结果
登录后查看更多信息
0 项与 深圳市儿童医院 相关的专利(医药)
登录后查看更多信息
2,136
项与 深圳市儿童医院 相关的文献(医药)2025-12-31·Emerging Microbes & Infections
Influenza vaccine effectiveness among primary and secondary school students in Shenzhen during the 2023/24 influenza season
Article
作者: Chen, Xiaozhen ; Wang, Xin ; Lu, Quan ; Wu, Xiaoliang ; Fang, Shisong ; Shu, Yuelong ; Sun, Jiatong ; Jiang, Yawen ; Xie, Xu ; Lu, Jianhua ; Liu, Hui ; Huang, Fang ; Gu, Huiqiao ; Jiang, Min ; Sun, Ying ; Feng, Tiejian
2025-12-01·Acta Epileptologica
Exploring physiological beta-hydroxybutyrate level in children treated with the classical ketogenic diet for drug-resistant epilepsy
Article
作者: Scheffer, Ingrid E ; Qiao, Xiaoying ; Zou, Dongfang ; Wen, Jialun ; Chen, Zhibin ; Chen, Li ; Cao, Dezhi ; Ye, Zimeng ; Liao, Jianxiang ; Zou, Huafang ; Kwan, Patrick ; Zhang, Man ; Lin, Sufang ; Qin, Jiong
2025-12-01·Child's Nervous System
Relationship between the volume of ventricles, brain parenchyma and neurocognition in children after hydrocephalus treatment
Article
作者: Zhao, Cailei ; Huang, Kun ; Yang, Qinzhu ; Li, Xianjun ; Zhang, Gongwei ; Gao, Yi
9
项与 深圳市儿童医院 相关的新闻(医药)2024-12-25
·卫医荟
2024年第四届
癫痫高峰精彩回顾
“携手克癫,共创未来”!
前言
2024年12月21日,由中国抗癫痫协会(CAAE)与卫材药业共同主办的“第四届癫痫高峰论坛”在北京隆重举办。作为癫痫领域最盛大的聚会,本届高峰论坛汇聚了国内癫痫领域的顶尖专家与临床学者,现场参会人数超过150人。本次论坛旨在共同探讨癫痫疾病的最前沿研究成果、临床诊疗进展及与吡仑帕奈相关研究及活动启动规划。让我们重温盛会,一起见证中国癫痫学者在会上的精彩瞬间!
开场视频
EES
大会以一段精心制作的开场视频拉开帷幕,带领参会者回顾过去五年中癫痫研究领域的主要工作及重要成就,现场气氛热烈而温情。
大会主席致辞
EES
大会主席由中国抗癫痫协会会长周东教授、中国抗癫痫协会副会长姜玉武教授共同担任,2位教授在致辞中提到“癫痫作为一种影响广泛的神经系统疾病,不仅给患者带来了极大的身心痛苦,也对其家庭乃至整个社会造成了深远的影响。期望全国的专家同道、包括相关企业组织,一起携手合作,共同推动癫痫领域的科学研究发展,改善患者的生活质量。”希望通过此次会议中各位专家的学术分享与交流碰撞出创新的火花,共同为癫痫事业的发展贡献力量。
Pathwys to Progress
Progress
EES
该环节由重庆医科大学附属第一医院王学峰教授、中山大学附属第七医院周列民教授担任主持;北京大学第一医院刘晓燕教授、宣武医院王玉平教授、北京大学第一医院姜玉武教授分别对于癫痫在脑电质控、睡眠、遗传学研究进展上进行了主题分享。刘晓燕教授分享了脑电质控方向在癫痫领域的诊断新进展;同时也提及不同ASM对脑电的影响需要引起临床重视。王玉平教授分享的关于睡眠的内容,从AMPA机制层面提示FYC对于伴睡眠障碍癫痫患者的用药优势。姜玉武教授分享的话题中明确提及:对于NR2F1相关的婴儿痉挛症,PER单独或者联合托吡酯很可能是比ACTH、氨己烯酸更合适的首选治疗方案。
Bridging Research to Practice
EES
本场会议的第二环节由浙江大学医学院附属第二医院丁美萍教授和广州医科大学附属第二医院廖卫平教授主持。该环节中有4位专家分享临床科研工作,在科研内容分享前,首都医科大学三博脑科医院王梦阳教授代表中国抗癫痫协会药物治疗专业委员会分享了2024年的学术成果《吡仑帕奈治疗成人局灶性癫痫的中国专家共识》,该共识从临床实践出发,为第三代ASM吡仑帕奈在中国人群中的使用提出了切实可行的指导意见。山东省立医院刘学伍教授分享主题《吡仑帕奈治疗卒中后癫痫的有效性和安全性:一项多中心、真实世界研究》。本次会议还特别邀请到药学专家参与和分享,浙江儿童医院药剂科主任缪静教授带来了药学研究课题《年龄、联合药物及CYP3A4/5多态性对中国癫痫患儿吡仑帕奈暴露的影响》,从临床药学角度给癫痫治疗提出了新的思考思路。两位儿科教授分享了主题;深圳市儿童医院操德智教授分享《吡仑帕奈单药治疗儿童癫痫真实世界研究》,浙江大学医学院附属第二医院冯建华教授分享《吡仑帕奈对遗传病因的儿童癫痫疗效》内容。
MDT疑难病例讨论会
MDT讨论会环节由由复旦儿科周渊峰教授分享复杂且罕见的癫痫病例诊治经历,此环节由华中科技大学同济医学院附属同济医院朱遂强教授主持,由重庆医科大学附属儿童医院蔡方成教授、中山大学附属第一医院陈子怡教授、首都医科大学附属北京天坛医院邵晓秋教授进行病例讨论。现场讨论热烈,与会专家围绕着该病例展开了深入的交流。
吡仑帕奈作为机制独特的抗癫痫发作药物,进入中国市场后也越来越被临床广泛接受。伴随着吡仑帕奈口服混悬液的快速上市,为让临床医生充分了解混悬液的给药优势、更好的用于癫痫患者的治疗,本场会议中,由全国25家儿童医院专家共同开启了《吡仑帕奈用于低龄癫痫患儿的中国专家共识》撰写启动;也期待未来该“共识”可以帮助到更多患者。
会中也同步筹备了《病例来了-走进中抗直播间》项目启动会:中国抗癫痫协会秘书处段立嵘秘书长与卫材药业市场经理宋家慧经理共同讲解了项目进程,同时也明确了卫材药业将持续与中国抗癫痫协会深度合作的愿景,敬请期待!
总结
本次大会在周东教授的总结中圆满结束,周教授特别提到期待未来所有癫痫领域的专家同道仍能继续相聚在EES这样高水准的学术活动中。
2024-12-06
·药智网
广东药学会发布新版儿科超说明书用药目录,更多药有望在更多临床实践中运用。
01
广东再发超说明书用药目录(儿科版)
最新版共计87条用药信息
近日,广东省药学会发布《超药品说明书用药目录(儿科2024年版)》。截至目前,广东省药学会已经发布了两版关于儿科的超说明书用药目录。
图片来源:赛柏蓝
笔者梳理发现,《超药品说明书用药目录(儿科2024年版)》纳入了87条用药信息,包括泼尼松(5mg)、吗替麦考酚酯(①0.25g②0.5g)、他克莫司(①0.5mg②1mg)等,其中有20多条用药信息后备注“2024年新增”。《超药品说明书用药目录(儿科2023年版)》于2023年11月7日发布,共有51条用药信息。
值得注意的是,自2015年起,广东省药学会已经连续多年发布超药品说明书用药目录,仅在今年就发布了《罕见病超药品说明书用药专家共识(血液系统•2024年版)》《超药品说明书用药目录(2024年版)》,还发布了《放射性药品超药品说明书用药专家共识》以及关于面向全国征集《超药品说明书用药目录(2025年版)》用法的通知。
超说明书用药现象在国内外临床实践中普遍存在。欧盟16国的统计结果显示,整个门诊数据中超说明书用药占7%~95%,其中抗肿瘤药物超说明书用药的比例在30.0%以上;儿科患者超说明书用药情况最为严重,儿科门诊患者超说明书用药比例为53.0%~82.7%,住院患者高达46.9%~95.0%。
儿科超说明书用药管理是各医院面临的重要课题。本次《目录》由中山大学孙逸仙纪念医院和深圳市儿童医院共同执笔,参与起草的医疗机构超过40多家,入选药品满足以下条件之一(均为最新版),并需在证据等级、临床需求等基础上进行评估筛选:
图片来源:赛柏蓝
一直以来,超说明书用药存在一定争议。目前在我国,超说明书用药有了法律依据——2022年3月1日起,新版《中华人民共和国医师法》正式落地实施,首次将诊疗指南和循证医学下的超说明书用药写入法条。
上述法规规定:医师应当坚持安全有效、经济合理的用药原则,遵循药品临床应用指导原则、临床诊疗指南和药品说明书等合理用药。在尚无有效或者更好治疗手段等特殊情况下,医师取得患者明确知情同意后,可以采用药品说明书中未明确但具有循证医学证据的药品用法实施治疗。
广东省在其发布的多版超说明书用药中均已说明,“目录仅作为证据罗列,不作为推荐目录,超说明书用药在临床应用中仍需按正规流程规范管理”。
02
超说明书用药
如何监管、报销...是关键
超说明书用药后,如何报销以及能否报销,一直是业内热议的重点。
超医保限制范围用药是大数据监管下医疗机构最常见的违规行为之一。在各地公布的超医保限制用药范围支付的情况中,出现过某医院将“肾型过敏性紫癜”患者使用“麦考酚钠肠溶片”的费用纳入医保报销、某医院将“子宫肌瘤”患者使用“益母草注射液”的费用纳入医保报销等违规情况。
2024年国家医保目录中仍存在600多个药品有支付限制,药品的支付限制包括多种类型,如限定医疗机构级别、限定适应症、限定二线用药、限定支付天数、限定工伤保险支付、限定生育保险支付、限定儿童使用等。
根据相关规定,医疗保险统筹基金支付《药品目录》内药品所发生的费用,必须由医生开具处方或住院医嘱,参保患者自行购买药品发生的费用,由个人账户支付或个人自付。
所以,只有在限制范围内使用医保药品才能报销。
同时《基本医疗保险用药管理暂行办法》第二十三条规定,参保人使用《药品目录》内药品发生的费用,符合:以疾病诊断或治疗为目的;诊断、治疗与病情相符,符合药品法定适应症及医保限定支付范围;由符合规定的定点医药机构提供,急救、抢救的除外;由统筹基金支付的药品费用,应当凭医生处方或住院医嘱;按规定程序经过药师或执业药师的审查这五个条件,可由基本医疗保险基金支付。
上述“符合药品法定适应症及医保限定支付范围”即“药品说明书适应症”,如果药品说明书上没有提到某个适应症,报销则无法进行。
截至目前,山东、辽宁、吉林、黑龙江都已经发布过超说明书用药目录。不过,这些超说明书用药目录在具体的实践中仍仅作为证据罗列,并非为推荐目录。
超说明书用药的监管越发严格,国家医保局公布的地方案例中,如山东淄博市中心医院在加强用药审核中,即会建立超说明书范围用药、超适应症用药等31个预审核模块并嵌入医保规则,医生开用药医嘱时,“审方干预系统”会自动对门诊和住院处方进行审核。
在超说明书用药下,药品根据临床实际情况有机会运用到更多场景,不过报销仍然需在药品支付限制范围内进行。
附:
图片来源:赛柏蓝
友情推荐:医药行业深度技术内容,点击“博药”查看详情~
来源 | 赛柏蓝(药智网获取授权转载)
撰稿 | 颜色
责任编辑 | 八角
声明:本文系药智网转载内容,图片、文字版权归原作者所有,转载目的在于传递更多信息,并不代表本平台观点。如涉及作品内容、版权和其它问题,请在本平台留言,我们将在第一时间删除。
商务合作 | 王存星 19922864877(同微信)
阅读原文,是受欢迎的文章哦
放射疗法
2024-08-18
·生物探索
引言
异染性脑白质营养不良症(MLD)是一种遗传性罕见病,因芳基硫酸酯酶A(ARSA)活性降低导致神经系统中硫脂质的积累,引起脱髓鞘、神经炎症和神经变性,表现出进展迅速的神经退行性疾病临床症状,目前没有特效药。现有的治疗策略包括ARSA酶替代疗法、腺相关病毒基因疗法和同种异体造血干细胞移植等,但疗效有限。2024年4月,Orchard Therapeutics的一款造血干细胞基因治疗产品(HSCGT)Lenmeldy(Atidarsagene Autotemcel)获得FDA批准。但是该疗法仅适用于治疗患者症状前晚婴型、症状前或者症状早期的青少年型 MLD 患者,获益人群十分有限。由于缺乏对MLD的认识,大多数MLD患者在诊断时已进展到症状后阶段。不同于快速退化的晚婴型MLD,晚发型如青少年型和成人型MLD通常神经症状退行性进展速度较慢些,为潜在的干预提供了治疗时间窗口的可能机会。因此,迫切需要评估HSCGT对该患者人群在症状发生后的治疗安全性和有效性。
近日,深圳理工大学/中国科学院深圳先进技术研究院教授连祺周团队联合广州医科大学附属妇女儿童医疗中心、深圳市第二人民医院、深圳市儿童医院及香港大学等医疗机构,在Protein & Cell杂志在线发表了题为Lentivirus-modified hematopoietic stem cell gene therapy for advanced symptomatic juvenile metachromatic leukodystrophy: A long-term follow-up pilot study 的最新研究成果,报告了一项自体造血干细胞基因治疗已发病的青少年型异染性脑白质营养不良(MLD)患者将近10年的安全性和有效性随访研究。
早在2014年,连祺周团队开创了亚洲首个造血干细胞基因疗法应用于有症状的青少年型MLD患者,并进行了一项多中心、单臂、开放临床试验(ClinicalTrials.gov ID: NCT02559830),通过分析治疗后短期和长期随访期间发生的不良事件以评估该疗法的长期安全性,通过ARSA活性检测、MRI评分及神经功能评分等评估临床获益。
图1 慢病毒修饰的造血干细胞基因治疗发病后青少年型MLD患者的疗法概念图(Credit: Protein & Cell)
该项研究已经筛选了6例患者,并在持续开放入组。研究论文报道了入组前3名患者的临床特征以及分别随访了4.5、6.9及9.6年的安全性及有效性数据。安全性数据分析结果显示,患者接受治疗后的两个月内发生的不良事件主要为中性粒细胞减少症,与化疗清髓有关,经常规治疗在短期内好转。在长期随访中没有观察到HSCGT相关的不良事件,安全性良好。另外基因组整合效率评估结果显示,患者的造血干细胞以及外周血单个核细胞中均已整合正常功能的ARSA基因。研究团队特别关注了因慢病毒载体随机插入而诱发的突变以及致癌基因激活的风险。通过全基因组分析以及PCR检测,所有890个插入位点均分布在染色体上,没有聚集插入倾向,且大部分插入位点分布在基因内含子序列,只有12个插入位点分布在外显子、启动子以及3’UTR区域,致癌基因上没有发现任何插入位点。
有效性评估显示患者血清ARSA酶活性在接受HSCGT后明显提升并维持高于正常水平;与未接受HSCGT患者的自然病程相比,该研究患者在接受HSCGT后,颅脑核磁共振(MRI)评分有所改善且持续稳定,提示神经退行性变疾病的进展得以缓解;神经功能评分GMFC-MLD及FIM评分在治疗后得到改善,提示HSCGT治疗可改善患者日常生活自理能力。该项研究数据显示,研究团队采取的HSCGT疗法可提高已发病青少年型MLD患者的ARSA酶活性,缓解神经退行性疾病进展,提高患者日常生活自理能力,且安全性良好。该项研究在基因治疗遗传代谢性脑病领域实现了一个重要的里程碑,有力推动了我国细胞治疗和基因治疗技术的临床转化。
参考文献
https://academic-oup-com.libproxy1.nus.edu.sg/proteincell/advance-article/doi/10.1093/procel/pwae037/7698288?login=false
责编|探索君
排版|探索君
文章来源|“BioArt”
End
往期精选
围观
一文读透细胞死亡(Cell Death) | 24年Cell重磅综述(长文收藏版)
热文
Cell | 是什么决定了细胞的大小?
热文
Nature | 2024年值得关注的七项技术
热文
Nature | 自身免疫性疾病能被治愈吗?科学家们终于看到了希望
热文
CRISPR技术进化史 | 24年Cell综述
基因疗法临床结果临床研究细胞疗法
100 项与 深圳市儿童医院 相关的药物交易
登录后查看更多信息
100 项与 深圳市儿童医院 相关的转化医学
登录后查看更多信息
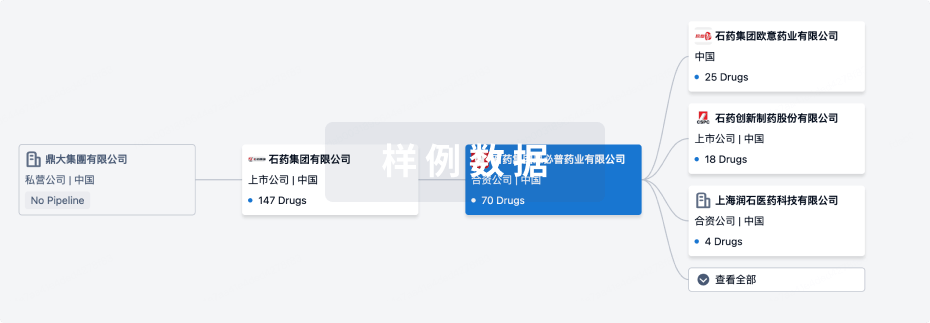
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月11日管线快照
无数据报导
登录后保持更新
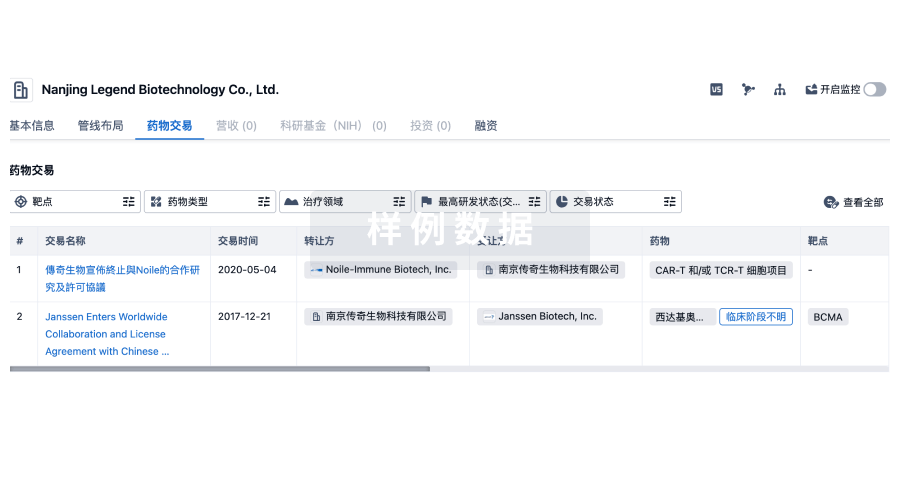
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
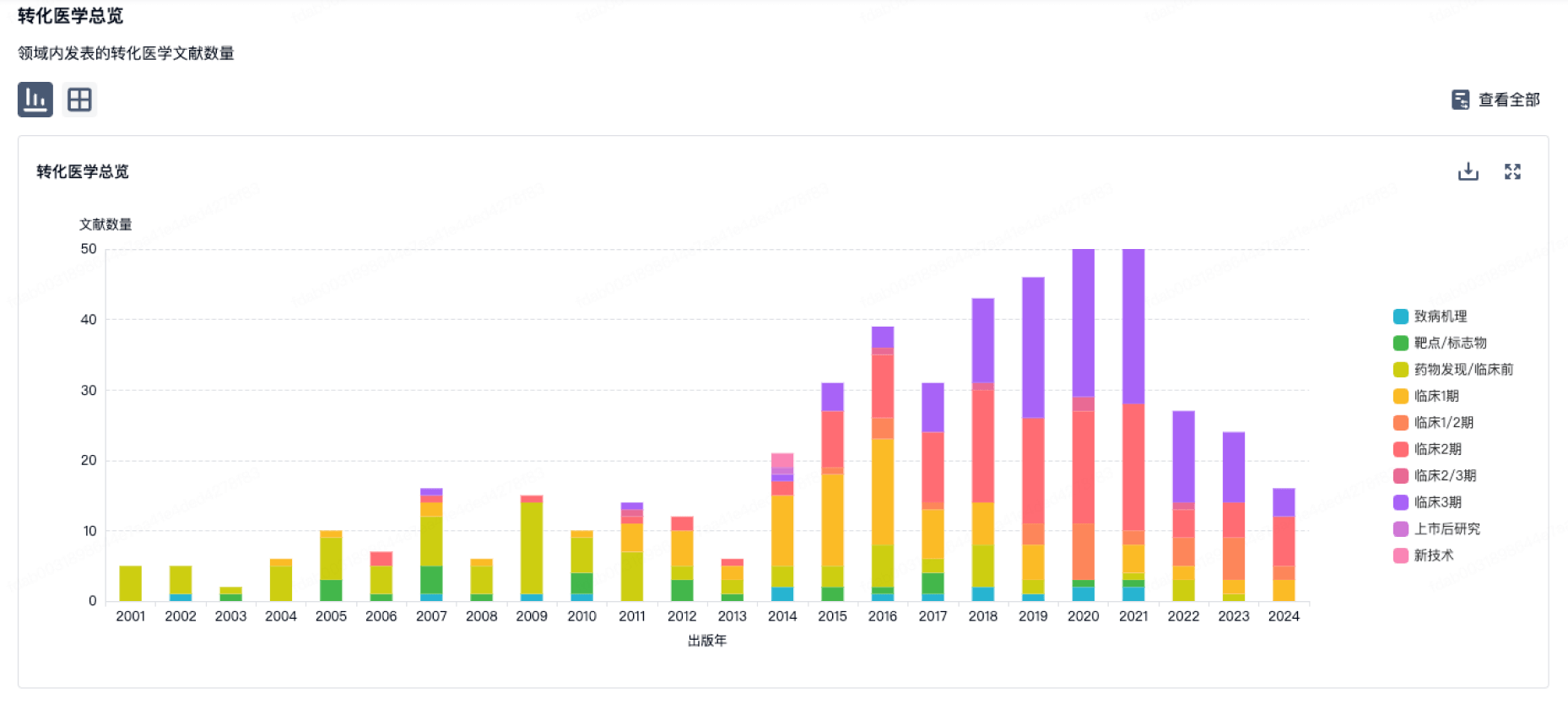
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
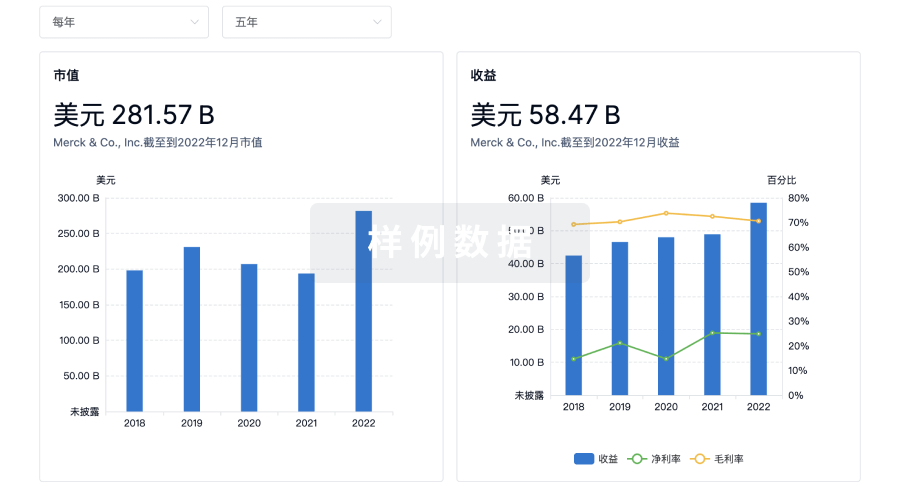
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用