预约演示
更新于:2025-05-07
The Christie Hospital Nhs Foundation Trust
更新于:2025-05-07
概览
关联
2
项与 The Christie Hospital Nhs Foundation Trust 相关的药物靶点 |
作用机制 CEACAM5调节剂 [+1] |
在研机构- |
在研适应症- |
最高研发阶段终止 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构- |
在研适应症- |
非在研适应症 |
最高研发阶段终止 |
首次获批国家/地区- |
首次获批日期- |
23
项与 The Christie Hospital Nhs Foundation Trust 相关的临床试验NCT06470880
Circulating Tumour DNA Guided Adaptive BRAF and MEK Inhibitor Therapy
The goal of this clinical trial is to investigate adaptive therapy in late-stage cutaneous melanoma. The main question it aims to answer are:
If the patient having breaks in their treatment allows the less resistant cells to continue to grow, this would result in a tumour with a lower proportion of resistant cells, making the tumour less resistant to the treatment, an increasing the time it takes for the disease to progress?
Participants will
Receive their allocated treatment regimen until their cancer progresses, they or their doctor withdraw them from the study, or until the study ends, whichever happens first.
Attend fortnightly visits to hospital.
Complete EORTC QLQ-C30 and PRO-CTCAE questionnaires, prior to treatment, every 12 weeks and at the point of cancer progression, to assess quality of life.
Researchers will compare the adaptive therapy participant arm with a standard of care arm to answer the research question described above.
If the patient having breaks in their treatment allows the less resistant cells to continue to grow, this would result in a tumour with a lower proportion of resistant cells, making the tumour less resistant to the treatment, an increasing the time it takes for the disease to progress?
Participants will
Receive their allocated treatment regimen until their cancer progresses, they or their doctor withdraw them from the study, or until the study ends, whichever happens first.
Attend fortnightly visits to hospital.
Complete EORTC QLQ-C30 and PRO-CTCAE questionnaires, prior to treatment, every 12 weeks and at the point of cancer progression, to assess quality of life.
Researchers will compare the adaptive therapy participant arm with a standard of care arm to answer the research question described above.
开始日期2024-06-01 |
申办/合作机构 |
NCT04901988
Circulating Tumour DNA guidEd Therapy for Stage IIB/C mElanoma After surgiCal resecTION (DETECTION)
The trial is looking for new and better ways to treat melanoma, an aggressive type of skin cancer. Having surgery to remove the melanoma will cure the majority of patients with early stage disease. However, a small percentage of these patients will go on to develop further disease, which may spread to other places in their body.
Currently, patients who have been cured of melanoma will have appointments in clinic to check that further disease has not developed or returned and some may also receive regular scans.
The trial team has developed a blood test that tells us whether cancer cells are still present or is becoming active after a patient has been 'cured' of melanoma, even if a scan looks normal. The test looks for pieces of DNA in the blood that are known to have come from the cancer, which we call 'circulating tumour DNA', or ctDNA. Patients who have ctDNA in their blood have an extremely high chance of the cancer returning.
By using the blood test that we have developed we think that we can identify patients earlier than normal. We think that some of the treatments that are used when melanoma cancer has spread may benefit patients at this earlier stage.
We want to see if these patients with ctDNA in their blood, who have a higher risk of their cancer returning or spreading, and receive treatment early have a better response to their cancer compared to those patients who receive treatment when their cancer has returned and it can be seen on a scan. This could mean we would be able to offer patients earlier treatment in the future using just a blood test rather than a scan, while also providing reassurance to those patients that do not have ctDNA in their blood that they do not need treatment and their cancer is not returning.
Currently, patients who have been cured of melanoma will have appointments in clinic to check that further disease has not developed or returned and some may also receive regular scans.
The trial team has developed a blood test that tells us whether cancer cells are still present or is becoming active after a patient has been 'cured' of melanoma, even if a scan looks normal. The test looks for pieces of DNA in the blood that are known to have come from the cancer, which we call 'circulating tumour DNA', or ctDNA. Patients who have ctDNA in their blood have an extremely high chance of the cancer returning.
By using the blood test that we have developed we think that we can identify patients earlier than normal. We think that some of the treatments that are used when melanoma cancer has spread may benefit patients at this earlier stage.
We want to see if these patients with ctDNA in their blood, who have a higher risk of their cancer returning or spreading, and receive treatment early have a better response to their cancer compared to those patients who receive treatment when their cancer has returned and it can be seen on a scan. This could mean we would be able to offer patients earlier treatment in the future using just a blood test rather than a scan, while also providing reassurance to those patients that do not have ctDNA in their blood that they do not need treatment and their cancer is not returning.
开始日期2021-11-08 |
申办/合作机构 |
NCT03794596
A Proof of Concept, Window Trial of the IMmunological Effects of AveLumab and Aspirin in Triple-Negative Breast Cancer
This research is being done because the investigators are looking for new and better ways to treat a type of breast cancer called triple negative breast cancer. This type of breast cancer can be more difficult to treat than other types of breast cancer as it does not respond to drugs such as hormonal therapies. One type of treatment that looks promising is immunotherapy using new drugs called immune checkpoint inhibitors.
Immune checkpoints help to regulate the immune system and can stop the immune system from attacking cancer cells. Immune checkpoint inhibitors block this 'off-switch' and aim to help the immune system control the cancer. These drugs have been very effective in other cancers such as melanoma and are now being tested in breast cancer.
In this study patients will receive an immune checkpoint inhibitor called avelumab. Half the patients on the study will also receive aspirin tablets for approximately 18 days as the investigators wish to compare the effects of avelumab alone versus in combination with aspirin.
Patients will attend hospital approximately five times in order to complete all necessary study assessments. The first visit screens patients for suitability, after which a baseline visit will collect the first of two breast tissue biopsies. At the third visit a single dose of Avelumab will be given via an infusion (a drip in the forearm). Patients will then return approximately two weeks later for a second breast tissue biopsy before having a final follow up visit another two weeks later. Blood and urine samples will be taken at various visits throughout the study to help us learn more about the effects these treatments may have on the immune system and on breast cancer cells.
Immune checkpoints help to regulate the immune system and can stop the immune system from attacking cancer cells. Immune checkpoint inhibitors block this 'off-switch' and aim to help the immune system control the cancer. These drugs have been very effective in other cancers such as melanoma and are now being tested in breast cancer.
In this study patients will receive an immune checkpoint inhibitor called avelumab. Half the patients on the study will also receive aspirin tablets for approximately 18 days as the investigators wish to compare the effects of avelumab alone versus in combination with aspirin.
Patients will attend hospital approximately five times in order to complete all necessary study assessments. The first visit screens patients for suitability, after which a baseline visit will collect the first of two breast tissue biopsies. At the third visit a single dose of Avelumab will be given via an infusion (a drip in the forearm). Patients will then return approximately two weeks later for a second breast tissue biopsy before having a final follow up visit another two weeks later. Blood and urine samples will be taken at various visits throughout the study to help us learn more about the effects these treatments may have on the immune system and on breast cancer cells.
开始日期2019-09-01 |
申办/合作机构 |
100 项与 The Christie Hospital Nhs Foundation Trust 相关的临床结果
登录后查看更多信息
0 项与 The Christie Hospital Nhs Foundation Trust 相关的专利(医药)
登录后查看更多信息
514
项与 The Christie Hospital Nhs Foundation Trust 相关的文献(医药)2025-04-03·Medical Teacher
Inter-school variations in the standard of examiners’ graduation-level OSCE judgements
Article
作者: O’Neill, Vikki ; Chung, Ching-Wa ; McCray, Gareth ; Goodfellow, Rhian ; Vallender, Rebecca ; Chung, Ching-wa ; Kinston, Ruth ; Yeates, Peter ; Cope, Natalie ; Maluf, Adriano ; McKinley, Robert ; Ensaff, Sue ; Goddard-Fuller, Rikki ; Cole, Aidan ; O'Neill, Vikki ; Cullen, Kathy
2025-03-04·Medical Teacher
A realist evaluation of how, why and when objective structured clinical exams (OSCEs) are experienced as an authentic assessment of clinical preparedness
Article
作者: O’Neill, Vikki ; Cope, Natalie ; Cole, Aidan ; Ensaff, Sue ; Goddard-Fuller, Rikki ; Goodfellow, Rhian ; Vallender, Rebecca ; Chung, Ching-wa ; Cullen, Kathy ; Yeates, Peter ; McKinley, Robert ; Maluf, Adriano ; Kinston, Ruth ; Wong, Geoff
2025-03-01·Leukemia
Multi-omic analysis of chronic myelomonocytic leukemia monocytes reveals metabolic and immune dysregulation leading to altered macrophage polarization
Article
作者: Addinsell, Hasse M ; Somervaille, Tim C P ; Wang, Yu-Hung ; Wiseman, Daniel H ; Batta, Kiran ; Cant, Rachel ; Hull, Nathan J
1
项与 The Christie Hospital Nhs Foundation Trust 相关的新闻(医药)2025-03-11
– VERITAC-2 achieved its primary endpoint in the estrogen receptor 1-mutant population, demonstrating statistically significant and clinically meaningful improvement in progression-free survival –
– Vepdegestrant is the first PROTAC degrader to demonstrate clinical benefit in a Phase 3 trial –
NEW HAVEN, Conn. and NEW YORK, March 11, 2025 – Arvinas, Inc. (Nasdaq: ARVN) and Pfizer Inc. (NYSE: PFE) today announced positive topline results from the Phase 3 VERITAC-2 clinical trial (NCT05654623) evaluating vepdegestrant monotherapy versus fulvestrant in adults with estrogen receptor-positive, human epidermal growth factor receptor 2-negative (ER+/HER2-) advanced or metastatic breast cancer whose disease progressed following prior treatment with cyclin-dependent kinase (CDK) 4/6 inhibitors and endocrine therapy. These are the first pivotal data for vepdegestrant, a potential first-in-class investigational oral PROteolysis TArgeting Chimera (PROTAC) ER degrader.
The trial met its primary endpoint in the estrogen receptor 1-mutant (ESR1m) population, demonstrating a statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to fulvestrant. The results exceeded the pre-specified target hazard ratio of 0.60 in the ESR1m population. The trial did not reach statistical significance in improvement in PFS in the intent-to-treat (ITT) population.
“The first Phase 3 data readout for a PROTAC degrader represents a significant achievement and these data show that vepdegestrant has the potential to provide clinically meaningful outcomes for thousands of patients with metastatic breast cancer whose tumors harbor estrogen receptor 1 mutations,” said John Houston, Ph.D., Chairperson, Chief Executive Officer and President at Arvinas. “We want to thank the patients and investigators who participated in this trial, and we look forward to sharing these data with health authorities as well as at a medical conference in 2025.”
Overall survival was not mature at the time of the analysis, with less than a quarter of the required number of events having occurred. The trial will continue to assess overall survival as a key secondary endpoint. In the trial, vepdegestrant was generally well tolerated and its safety profile was consistent with what has been observed in previous studies. Detailed results from VERITAC-2 will be submitted for presentation at a medical meeting later this year, and these data will be shared with global regulatory authorities to potentially support regulatory filings.
“Patients with advanced ER+/HER2- metastatic breast cancer face significant clinical challenges, with limited treatment options following disease progression and the development of resistance to available endocrine therapies,” said Megan O’Meara, M.D., Interim Chief Development Officer, Pfizer Oncology. “These data from VERITAC-2 support the potential of vepdegestrant to give patients whose tumors harbor ESR1 mutations additional time without disease progression, compared to fulvestrant."
Vepdegestrant is an investigational oral PROTAC ER degrader for ER+/HER2- breast cancer being jointly developed by Arvinas and Pfizer and is designed to harness the body’s natural protein disposal system to specifically target and degrade the ER. In February 2024, the companies announced that the U.S. Food and Drug Administration (FDA) granted Fast Track designation for the investigation of vepdegestrant for monotherapy in the treatment of adults with ER+/HER2- advanced or metastatic breast cancer previously treated with endocrine-based therapy.
About Metastatic Breast CancerAbout 2.3 million new breast cancer diagnoses were reported globally in 2022,1 and it is estimated there will be nearly 320,000 people diagnosed with breast cancer in the U.S. in 2025.2 Estrogen receptor-positive, human epidermal growth factor receptor 2-negative (ER+/HER2-) breast cancer accounts for approximately 70% of all cases.3
Nearly 30% of women initially diagnosed with early-stage breast cancer will ultimately develop metastatic breast cancer (MBC),4 the most advanced stage in which the disease has spread beyond the breast to other parts of the body. Treatment advances have helped those with MBC better manage symptoms, slow tumor growth, and may allow them to live longer, but most patients ultimately develop resistance to current standard-of-care treatments in the first-line setting and experience disease progression. ESR1 mutations are a common cause of acquired resistance and are found in approximately 40% of patients in the second-line setting.5 6 7
About the VERITAC-2 Clinical TrialThe Phase 3 VERITAC-2 clinical trial (NCT05654623) is a global randomized study evaluating the efficacy and safety of vepdegestrant (ARV-471) as a monotherapy compared to fulvestrant in patients with ER+/HER2- advanced or metastatic breast cancer. The trial enrolled 624 patients at sites in 26 countries who had previously received treatment with a CDK4/6 inhibitor plus endocrine therapy.
Patients were randomized to receive either vepdegestrant once daily, orally on a 28-day continuous dosing schedule, or fulvestrant, administered intramuscularly on Days 1 and 15 of Cycle 1 and then on Day 1 of each 28-day cycle starting from Day 1 of Cycle 2. The primary endpoint was progression-free survival (PFS) in the intent-to-treat and ESR1m populations as determined by blinded independent central review. Overall survival is a key secondary endpoint.
About VepdegestrantVepdegestrant is an investigational, orally bioavailable PROTAC (PROteolysis TArgeting Chimera) protein degrader designed to specifically target and degrade the estrogen receptor (ER) for the treatment of patients with ER-positive (ER+)/human epidermal growth factor receptor 2 (HER2)-negative (ER+/HER2-) breast cancer. Vepdegestrant is being developed as a potential monotherapy and as part of combination therapy across multiple treatment settings for ER+/HER2- metastatic breast cancer.
In July 2021, Arvinas announced a global collaboration with Pfizer for the co-development and co-commercialization of vepdegestrant; Arvinas and Pfizer will share worldwide development costs, commercialization expenses, and profits.
The U.S. Food and Drug Administration (FDA) has granted vepdegestrant Fast Track designation as a monotherapy in the treatment of adults with ER+/HER2- advanced or metastatic breast cancer previously treated with endocrine-based therapy.
About ArvinasArvinas (Nasdaq: ARVN) is a clinical-stage biotechnology company dedicated to improving the lives of patients suffering from debilitating and life-threatening diseases. Through its PROTAC (PROteolysis TArgeting Chimera) protein degrader platform, the Company is pioneering the development of protein degradation therapies designed to harness the body’s natural protein disposal system to selectively and efficiently degrade and remove disease-causing proteins. Arvinas is currently progressing multiple investigational drugs through clinical development programs, including vepdegestrant, targeting the estrogen receptor for patients with locally advanced or metastatic ER+/HER2- breast cancer; ARV-393, targeting BCL6 for relapsed/refractory non-Hodgkin Lymphoma; and ARV-102, targeting LRRK2 for neurodegenerative disorders. Arvinas is headquartered in New Haven, Connecticut. For more information about Arvinas, visit www.arvinas.com and connect on LinkedIn and X.
About Pfizer OncologyAt Pfizer Oncology, we are at the forefront of a new era in cancer care. Our industry-leading portfolio and extensive pipeline includes three core mechanisms of action to attack cancer from multiple angles, including small molecules, antibody-drug conjugates (ADCs), and bispecific antibodies, including other immune-oncology biologics. We are focused on delivering transformative therapies in some of the world’s most common cancers, including breast cancer, genitourinary cancer, hematology-oncology, and thoracic cancers, which includes lung cancer. Driven by science, we are committed to accelerating breakthroughs to help people with cancer live better and longer lives.
About Pfizer: Breakthroughs That Change Patients’ LivesAt Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world's premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For 175 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.pfizer.com. In addition, to learn more, please visit us on www.pfizer.com and follow us on X at @Pfizer and @Pfizer_News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
Arvinas Forward-Looking StatementsThis press release contains forward-looking statements within the meaning of The Private Securities Litigation Reform Act of 1995 that involve substantial risks and uncertainties, including statements regarding: vepdegestrant having the potential to provide clinically meaningful outcomes for thousands of patients with metastatic breast cancer whose tumors harbor estrogen receptor 1 mutations; Arvinas’ and Pfizer’s plans to share data from the Phase 3 VERITAC-2 clinical trial with health authorities, including to potentially support regulatory filings, as well as at a medical conference in 2025; and vepdegestrant’s development as a potential monotherapy and as part of combination therapy across multiple treatment settings for estrogen receptor positive, human epidermal growth factor receptor 2 negative metastatic breast cancer. All statements, other than statements of historical fact, contained in this press release, including statements regarding Arvinas’ strategy, future operations, future financial position, future revenues, projected costs, prospects, plans and objectives of management, are forward-looking statements. The words “anticipate,” “believe,” “estimate,” “expect,” “intend,” “may,” “plan,” “target,” “goal,” “potential,” “will,” “would,” “could,” “should,” “look forward,” “continue,” and similar expressions are intended to identify forward-looking statements, although not all forward-looking statements contain these identifying words.
Arvinas may not actually achieve the plans, intentions or expectations disclosed in these forward-looking statements, and you should not place undue reliance on such forward-looking statements. Actual results or events could differ materially from the plans, intentions and expectations disclosed in the forward-looking statements Arvinas makes as a result of various risks and uncertainties, including but not limited to: whether Arvinas and Pfizer will successfully perform their respective obligations under the collaboration between Arvinas and Pfizer; whether Arvinas and Pfizer will be able to successfully conduct and complete clinical development for vepdegestrant as a monotherapy and as part of combination therapy; whether Arvinas will be able to successfully conduct and complete development for its other product candidates, including ARV-393 and ARV-102; whether Arvinas and Pfizer, as appropriate, will be able to obtain marketing approval for and commercialize vepdegestrant and other product candidates on current timelines or at all; Arvinas’ ability to protect its intellectual property portfolio; Arvinas’ reliance on third parties; whether Arvinas will be able to raise capital when needed; whether Arvinas’ cash and cash equivalent resources will be sufficient to fund its foreseeable and unforeseeable operating expenses and capital expenditure requirements; and other important factors discussed in the “Risk Factors” section of Arvinas’ Annual Report on Form 10-K for the year ended December 31, 2024 and subsequent other reports on file with the U.S. Securities and Exchange Commission. The forward-looking statements contained in this press release reflect Arvinas’ current views with respect to future events, and Arvinas assumes no obligation to update any forward-looking statements, except as required by applicable law. These forward-looking statements should not be relied upon as representing Arvinas’ views as of any date subsequent to the date of this release.
Pfizer Disclosure Notice:The information contained in this release is as of March 11, 2025. Pfizer assumes no obligation to update forward-looking statements contained in this release as the result of new information or future events or developments.
This release contains forward-looking information about Pfizer Oncology and vepdegestrant, including its potential benefits, vepdegestrant’s potential for adults with ER+/HER2- advanced or metastatic breast cancer whose disease progressed following prior treatment with CDK 4/6 inhibitors and endocrine-based therapy and plans to share these data with global regulatory authorities to potentially support regulatory filings, that involve substantial risks and uncertainties that could cause actual results to differ materially from those expressed or implied by such statements.
Risks and uncertainties include, among other things, the uncertainties inherent in research and development, including the ability to meet anticipated clinical endpoints, commencement and/or completion dates for our clinical trials, regulatory submission dates, regulatory approval dates and/or launch dates, as well as the possibility of unfavorable new clinical data and further analyses of existing clinical data; whether the VERITAC-2 trial will meet the secondary endpoint for overall survival; the risk that clinical trial data are subject to differing interpretations and assessments by regulatory authorities; whether regulatory authorities will be satisfied with the design of and results from our clinical studies; whether and when drug applications may be filed in any jurisdictions for any potential indication for vepdegestrant; whether and when any such applications that may be filed for vepdegestrant may be approved by regulatory authorities, which will depend on myriad factors, including making a determination as to whether the product's benefits outweigh its known risks and determination of the product's efficacy, and, if approved, whether vepdegestrant will be commercially successful; decisions by regulatory authorities impacting labeling, manufacturing processes, safety and/or other matters that could affect the availability or commercial potential of vepdegestrant; whether the collaboration between Pfizer and Arvinas will be successful; uncertainties regarding the impact of COVID-19 on our business, operations and financial results; and competitive developments.
A further description of risks and uncertainties can be found in Pfizer’s Annual Report on Form 10-K for the fiscal year ended December 31, 2024, and in its subsequent reports on Form 10-Q, including in the sections thereof captioned “Risk Factors” and “Forward-Looking Information and Factors That May Affect Future Results”, as well as in its subsequent reports on Form 8-K, all of which are filed with the U.S. Securities and Exchange Commission and available at www.sec.gov and www.pfizer.com.
1 World Health Organization. (2024, March 13). Breast cancer. World Health Organization. https://www-who-int.libproxy1.nus.edu.sg/news-room/fact-sheets/detail/breast-cancer2 Siegel RL, Kratzer TB, Giaquinto AN, Sung H, Jemal A. Cancer statistics, 2025. CA Cancer J Clin. 2025 Jan-Feb;75(1):10-45. doi: 10.3322/caac.21871. Epub 2025 Jan 16. PMID: 39817679; PMCID: PMC11745215.3 Surveillance, Epidemiology, and End Results Program Data, https://seer.cancer.gov/statfacts/html/breast-subtypes.html.4 Redig AJ, McAllister SS. Breast cancer as a systemic disease: a view of metastasis. J Intern Med. 2013;274(2):113-126. doi:10.1111/joim.12084.5 Bidard F-C, et al. Elacestrant (oral selective estrogen receptor degrader) Versus Standard Endocrine Therapy for Estrogen Receptor–Positive, Human Epidermal Growth Factor Receptor 2–Negative Advanced Breast Cancer: Results From the Randomized Phase III EMERALD Trial. Journal of Clinical Onoclogy. 2022 May https://doi-org.libproxy1.nus.edu.sg/10.1200/JCO.22.00338.6 Kalinsky, K. Abemaciclib Plus Fulvestrant in Advanced Breast Cancer After Progression on CDK4/6 Inhibition: Results From the Phase III postMONARCH Trial. Journal of Clinical Oncology. 2024 Dec. https://doi-org.libproxy1.nus.edu.sg/10.1200/JCO-24-0208.7 Tolaney, S. et al. AMEERA-3: Randomized Phase II Study of Amcenestrant (Oral Selective Estrogen Receptor Degrader) Versus Standard Endocrine Monotherapy in Estrogen Receptor–Positive, Human Epidermal Growth Factor Receptor 2–Negative Advanced Breast Cancer. Journal of Clinical Oncology. https://ascopubs-org.libproxy1.nus.edu.sg/doi/full/10.1200/JCO.22.02746.
Media Contact:
+1 (212) 733-1225PfizerMediaRelations@Pfizer.com
Investor Contact:
+1 (212) 733-4848IR@Pfizer.com
Arvinas Media Contact:
Kirsten Owens+1 (203) 586-0307Kirsten.Owens@Arvinas.com
Arvinas Investor Contact:
Jeff Boyle+1 (347) 247-5089Jeff.Boyle@Arvinas.com
临床结果临床3期快速通道
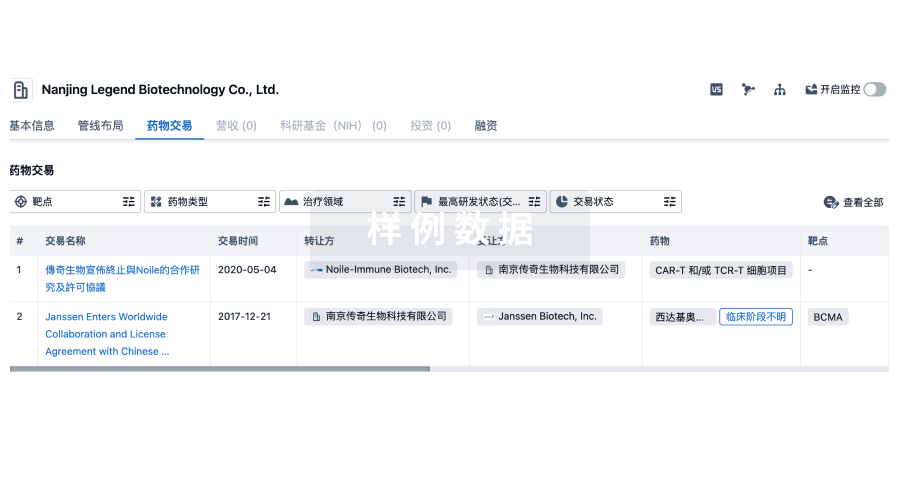
100 项与 The Christie Hospital Nhs Foundation Trust 相关的药物交易
登录后查看更多信息
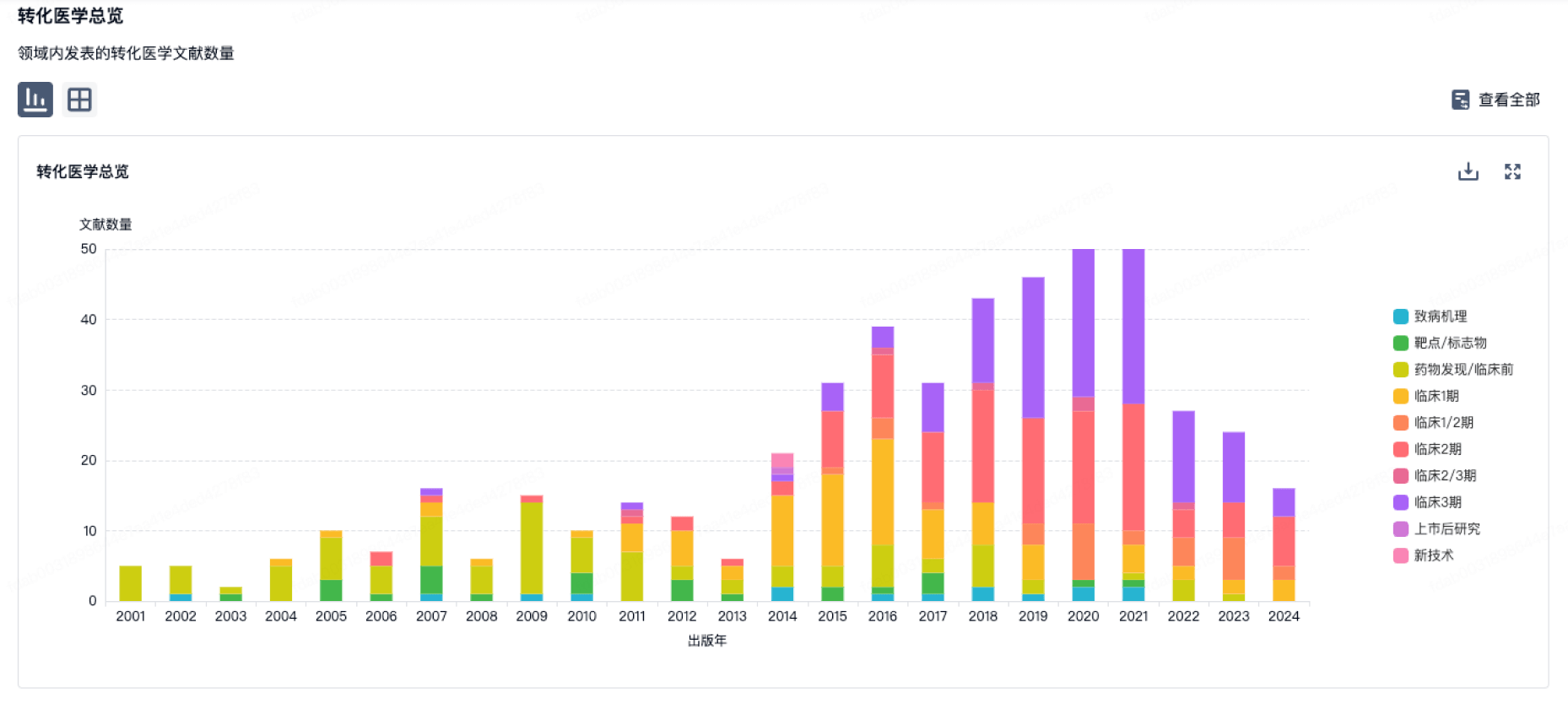
100 项与 The Christie Hospital Nhs Foundation Trust 相关的转化医学
登录后查看更多信息
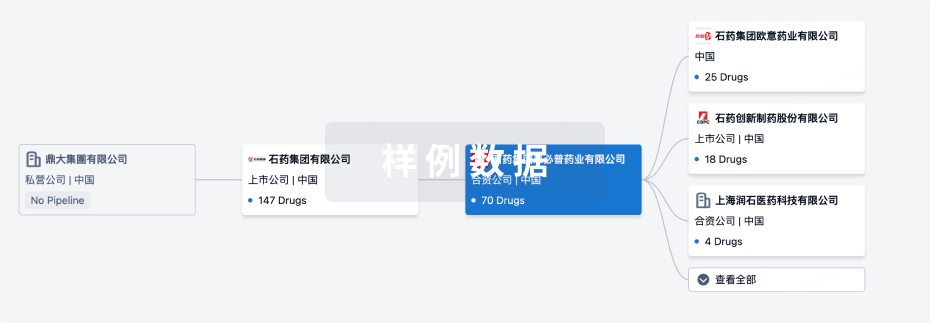
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月07日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
2
登录后查看更多信息
当前项目
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
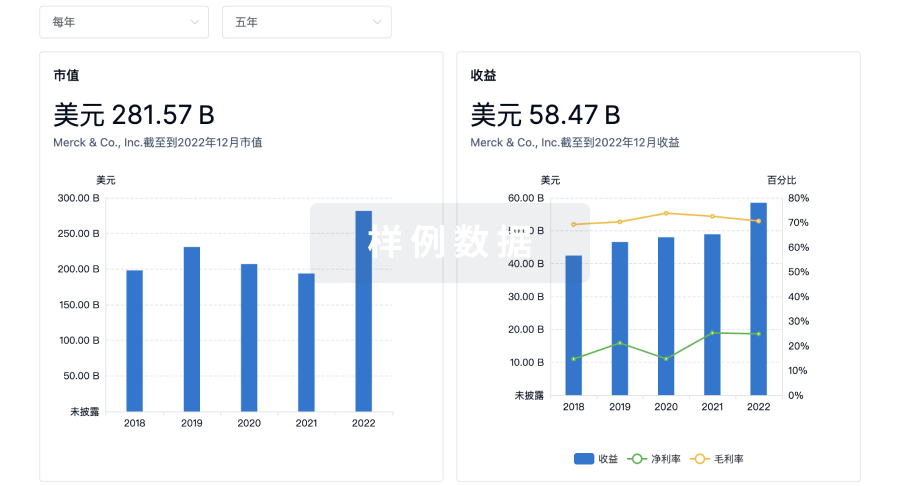
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用