预约演示
更新于:2025-08-14

ICGEB
更新于:2025-08-14
概览
标签
神经系统疾病
口颌疾病
消化系统疾病
生物药
治疗性疫苗
腺相关病毒基因治疗
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 生物药 | 1 |
| 治疗性疫苗 | 1 |
| 腺相关病毒基因治疗 | 1 |
| 生长因子 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| SMN2(运动神经元存活蛋白) | 1 |
| EGFR(表皮生长因子受体erbB1) | 1 |
关联
4
项与 ICGEB 相关的药物靶点- |
作用机制 免疫刺激剂 |
在研机构 |
在研适应症 |
非在研适应症 |
最高研发阶段批准上市 |
首次获批国家/地区 古巴 |
首次获批日期2015-01-01 |
靶点 |
作用机制 EGFR调节剂 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 古巴 |
首次获批日期2007-09-01 |
2
项与 ICGEB 相关的临床试验CTRI/2020/03/023739
A Phase I, randomized, controlled, dose escalating, single blind, clinical trial to assess the safety, tolerability and immunogenicity of Bivalent (JAIVAC-2: PfMSPFu24 +PfF2/ Alhydrogel) P. falciparum malaria vaccine in malaria naive healthy Indian adult males
开始日期2020-03-06 |
申办/合作机构  ICGEB ICGEB [+1] |
CTR20140502
评价注射用rhEGF治疗晚期DFU的有效性和安全性的随机双盲多中心安慰剂平行对照的III期临床研究
评估局部注射用重组人表皮生长因子用于晚期糖尿病足溃疡(Wagner分级3、4级)和有重度截肢风险的患者病灶内和病灶周围给药的疗效和安全性。
开始日期- |
申办/合作机构 华科医药科技有限公司 [+1] |
100 项与 ICGEB 相关的临床结果
登录后查看更多信息
0 项与 ICGEB 相关的专利(医药)
登录后查看更多信息
4,406
项与 ICGEB 相关的文献(医药)2025-12-31·Plant Signaling & Behavior
Putrescine mitigates NaCl-induced stress by modulating gene expression, antioxidants, and ethylene level in tomato
Article
作者: Yadav, Priya ; Brajendra ; Tuteja, Narendra ; Ansari, Mohammad Wahid ; Gill, Ritu ; Muley, Devayani ; Sahoo, Ranjan Kumar ; Rama Rao, Yalaga ; Singh Gill, Sarvajeet ; Bhushan Kumar, Shashi ; Rani, Varsha
Plant development and productivity are significantly hindered by salt stress, leading to substantial financial losses in the agriculture sector. Salinity stress negatively impacts the overall growth, physiology, and metabolism of plants. Specifically, NaCl stress is particularly harmful to tomato plants, causing suppression of seedling growth, accumulation of sodium (Na+) and chloride (Cl-) ions, disrupted ion homeostasis, reduced proline and chlorophyll content, and impairment of antioxidant enzyme systems. This research aimed to investigate the role of exogenous putrescine (PUT) application on tomato (Solanum lycopersicum L.) seedlings under NaCl stress (250 mm) to determine its potential protective effects. Various physio-biochemical attributes were estimated using precise protocols for NaCl-treated, PUT-treated, and untreated controlled tomato seedlings also analyzed for the expression of ACS1, NHX1, HKT1;2, and SOS1 genes. Additionally, ACC synthase activity, ethylene content, electrolyte leakage, proline content, Na+ and potassium (K+) ion content, lycopene content, and antioxidant enzyme activities were examined. Results indicated that PUT application enhanced the expression of ACS1, NHX1, HKT1;2, and SOS1 genes increase the ACC synthase activity, ethylene content, proline content, and Na+ and K+ ion content, while reducing electrolyte leakage. Furthermore, PUT application significantly increased the activity of superoxide dismutase (SOD), catalase (CAT), ascorbate peroxidase (APX), and glutathione reductase (GR), as well as other morphological parameters. Overall, our research demonstrated the potential benefits of PUT applications for enhancing crop growth and improving salt stress tolerance, which are crucial for agronomy.
2025-12-01·ENDOCRINE PATHOLOGY
A Novel Three-Stage AI-Assisted Approach for Accurate Differential Diagnosis and Classification of NIFTP and Thyroid Neoplasms
Article
作者: Tiwari, Nimisha ; Agarwal, Shipra ; Sharma, Arundhati ; Birla, Shweta ; Khatri, Abhishek ; Shyamal, Pragati ; Bandaru, Divya ; Gupta, Dinesh
The recent introduction of the term non-invasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) marked a pivotal shift in the classification of encapsulated follicular variant of papillary thyroid carcinoma (EFVPTC) lacking invasive features. While its reclassification from the "malignant" to "low-risk neoplasm" category significantly reduced overtreatment, its histopathological diagnosis remains challenging due to overlapping features with other thyroid lesions and inter-observer variability. Artificial intelligence (AI) overcomes such key limitations of histopathological evaluation, ensuring a robust and efficient diagnostic process. While preliminary studies are promising, AI models capable of efficiently distinguishing NIFTP from other benign and malignant thyroid entities are yet to be developed. We devised an innovative AI-based three-stage hierarchical pipeline that systematically evaluates architectural patterns and nuclear features. The prioritized models were trained using 154,498 patches, derived from 134 sections prepared from 125 thyroid nodules, representing follicular nodular disease (FND), follicular adenoma, dominant nodule in FND, invasive EFVPTC (IEFVPTC), and classic and infiltrative follicular subtypes of PTC. External validation revealed good accuracy at the overall, patient-wise, and class-wise levels. However, it showed limitations in the differential diagnosis of NIFTP from IEFVPTC-an expected challenge due to overlapping nuclear features and the absence of incorporating the assessment of the tumor capsule for invasive characteristics. While the novel approach and the algorithm show promise in transforming histopathological NIFTP diagnostics, further improvements and rigorous validations are necessary before considering its application in real-world clinical settings.
2025-12-01·JOURNAL OF VIROLOGICAL METHODS
Comparison of plant- and mammalian cell-produced human papillomavirus pseudovirions
Article
作者: Rybicki, Edward P ; Hitzeroth, Inga I ; Lindsay, Sarah ; van Zyl, Albertha R ; Schäfer, Georgia
High-risk human papillomaviruses (HPVs) are the primary etiological agents of cervical, anal and oropharyngeal cancers. While existing vaccines are effective in preventing infection, their impact in low-and middle-income countries (LMICs) is limited by type coverage, high costs and uptake. To address this gap, there is a critical need for next-generation vaccines that are both regionally tailored and cost-effective, along with efficient and accessible tools for evaluating their efficacy. HPV pseudovirions (PsVs), which encapsidate a reporter plasmid, are widely used in pseudovirion-based neutralisation assays (PBNAs) and in vivo murine models to assess vaccine-induced immunity - and have potential for use as DNA vaccine delivery systems. Traditionally, PsVs are produced in mammalian cells, which remain the gold standard due to their high infectivity and structural fidelity. However, recent studies have demonstrated the feasibility of producing PsVs in plants, a platform that offers lower infrastructure and reagent costs, scalability, and biosafety advantages. Although plant-derived PsVs have shown promise in PBNAs, their performance in in vivo models had not been evaluated prior to this study. Here, we compared mammalian cell-derived PsVs encapsidating either Gaussia or firefly luciferase reporter plasmids and found that firefly luciferase provided more consistent and robust signals in both in vitro and in vivo assays. Building on this, we generated PsVs encapsidating the firefly luciferase gene using both mammalian and plant expression systems, and assessed their infectivity. While plant-derived PsVs were capable of infecting HeLa cells and mice in a cervicovaginal challenge model, mammalian-derived PsVs exhibited significantly higher infectivity overall. These findings represent the first demonstration of in vivo infectivity of plant-produced HPV PsVs and highlight their potential as a cost-effective alternative for immunogenicity testing and potentially as vaccines. Although further optimization is needed, particularly in capsid assembly and purification, plant-based PsV production holds promise for expanding access to HPV research tools and supporting vaccine development in resource-limited settings.
6
项与 ICGEB 相关的新闻(医药)2023-10-12
药·械 追踪Products NewsNo.1 /阿斯利康AKT抑制剂在华申报上市近日,中国国家药监局药品审评中心(CDE)官网公示,阿斯利康旗下1 类创新药物、AKT抑制剂Capivasertib片的上市申请已获受理。Capivasertib是一款口服的first-in-class的AKT1/2/3高效选择性抑制剂,通过靶向PIK3/AKT 信号通路减少癌细胞的生长和扩散。PI3K/AKT通路在三阴性乳腺癌(TNBC) 中异常表达,并且被认为与化疗耐药性有关。GBI既往报道,Capivasertib在美国提交的上市申请已于2023年6月获FDA优先审评。III期临床试验数据显示,与安慰剂加氟维司群相比,capivasertib联合氟维司群治疗内分泌方案治疗后复发或进展的荷尔蒙受体(HR)阳性,人表皮生长因子受体2(HER2)阴性局部晚期或转移性乳腺癌,可将疾病进展或死亡风险降低40%,且安全性良好。->点击阅读原文,解锁完整双语新闻No.2 /罗氏双抗疗法Forimtamig在中国获批临床近日,据国家药监局药审中心数据,罗氏旗下治疗性1类生物制品Forimtamig获临床默示许可,用于多发性骨髓瘤。Forimtamig(RG6234)是一款可同时靶向GPRC5D和CD3的双特异性抗体,此前已在针对重度预处理的复发/难治性多发性骨髓瘤患者的Ⅰ期临床试验中,取得良好的疗效和可控的安全性。->点击阅读原文,解锁完整双语新闻No.3 /微创心律管理公司两款除颤产品在日获批上市近日,微创心律管理宣布,其ULYS植入式心律转复除颤器(ICDs)和INVICTA除颤电极导线在日本获批上市。INVICTA的安全性和有效性已在其上市前临床研究项目Apollo临床研究中得到证实。该研究结果显示:在3个月的主要临床终点,INVICTA具有100%的植入成功率和97.4%的无并发症发生率。->点击阅读原文,解锁完整双语新闻企业动态Companies NewsNo.1 /百图生科携手赛诺菲,大模型加持药物研发近日,百图生科(BioMap)宣布与赛诺菲达成一项具有突破性意义的战略合作,双方将基于百图生科生命科学大模型,共同开发用于生物治疗药物发现的领先模型。此次合作,是生命科学领域首次基于大模型的商业合作,并提出以模型开发而不是药物研发进展作为里程碑,为大模型时代中独特的MaaS(Model as a Service)商业模式带来新的案例。据协议,百图生科将获得1000万美元的预付款和多项近期的模型开发付款。根据达到临床前开发、临床开发、监管和商业里程碑付款等回报,百图生科将获得超过10亿美元的总交易金额。->点击阅读原文,解锁完整双语新闻No.2 /中国生物制药出售正大通用84.2%股权近日,中国生物制药发布公告称,集团以约人民币3.5亿元的估值出售附属公司上海正大通用药业股份有限公司约84.2%的股权,出售所得金额约人民币2.9亿元。出售事项完成后,集团将不再持有正大通用的任何股权。正大通用2022年度收入约人民币8900万元,净亏损约人民币3500万元,剥离正大通用有利于集团净利润率的提升。通过出售事项,集团将进一步聚焦四大核心治疗领域,即肿瘤、肝病、呼吸、外科/镇痛,提升四大核心治疗领域的研发投入。->点击阅读原文,解锁完整双语新闻No.3 /瑞科生物与津巴布韦、ICGEB达成三方合作,助力非洲疫苗产研近日,瑞科生物宣布与津巴布韦国家生物技术管理局、国际遗传工程和生物技术中心签署三方战略合作协议。协议约定瑞科生物将与ICGEB中国区域研究中心合作向津巴布韦提供疫苗生产相关技术支持,包括人员培训,厂房设计,临床试验,分包装技术转移以及原液技术转移等,以新冠疫苗为切入点,逐步扩展到其它疫苗品种,为津巴布韦和非洲实现本地化疫苗生产贡献力量。->点击阅读原文,解锁完整双语新闻行业政策Industry PoliciesNo.1 /博鳌乐城医疗先行区细化特许进口药械带离管理方法近日,海南省药监局、省卫健委联合发布《海南自由贸易港博鳌乐城国际医疗旅游先行区临床急需进口药品医疗器械带离使用管理办法》。《管理办法》规定,患者离院时,根据治疗需要,可将仅供自用、合理量、风险可控,且可自行完成操作的监测类、康复类和家用治疗类特许医疗器械带离医疗机构使用。->点击阅读原文,解锁完整双语新闻全球医疗情报领导者解锁隐藏在数据中的商业潜力 关于 G B I”自从2002年成立以来,GBI始终以技术为驱动,为药企、器械及行业相关服务商提供贯穿生命周期的全球药品市场竞争数据、全球行业资讯、HCPs洞察、全国医疗器械数据等商业信息与洞察,助力企业在进行战略布局和决策时,脱颖而出。历经20愈年的深耕细作GBI已成为95%以上跨国药企、国内头部药企、咨询与投资机构等医疗圈灯塔用户值得信赖的长期合作伙伴。联系我们投稿 | 发稿 | 媒体合作▶ sylvia.hua@generalbiologic.com数据库 | 咨询服务 | 资讯追踪▶ 点击左下“阅读原文”完成表单填写点击阅读原文,解锁完整双语新闻
引进/卖出临床3期优先审批申请上市临床2期
2023-10-10
·美通社
泰州
2023年10月10日
/美通社/ -- 2023年10月8日,津巴布韦国家生物技术管理局CEO萨瓦迪博士及国际遗传工程和生物技术中心(ICGEB)中国区域研究中心杨义力博士一行到访瑞科生物,在前期多轮洽谈的基础上,萨瓦迪博士一行对瑞科生物新冠/带状疱疹疫苗及HPV疫苗生产设施进行了实地考察。在泰州医药高新技术产业园区领导的见证下,三方共同签署战略合作协议。
协议约定瑞科生物将与ICGEB中国区域研究中心合作向津巴布韦提供疫苗生产相关技术支持,包括人员培训,厂房设计,临床试验,分包装技术转移以及原液技术转移等,以新冠疫苗为切入点,逐步扩展到其它疫苗品种,为津巴布韦和非洲实现本地化疫苗生产贡献力量。
此次签约,标志着瑞科生物疫苗研发和生产技术平台及产品得到了更多国际组织和国家的认可。瑞科生物将积极践行国家"一带一路"倡议,抢抓疫苗海外市场布局。
津巴布韦国家生物技术管理局是于2006年立法成立的津巴布韦政府部门,致力于在医药、农业等领域推广应用传统和前沿的生物技术。
国际遗传工程和生物技术中心(ICGEB)属政府间国际科技组织,在联合国工业发展组织(UNIDO)的支持下于1983年创立。截至目前已与超过65个会员国建立了互动网络,在科研、培训和技术向产业转移等方面取得了突出成就。
关于瑞科生物
江苏瑞科生物技术股份有限公司(股票代码:02179.HK)始创于2012年,是一家以自主研发技术为核心驱动力的创新型疫苗公司,致力于打造覆盖研发、生产及商业化的创新型疫苗。长期以来,公司始终秉持"创制一流疫苗,守护人类健康"的使命,凭借由新型佐剂、蛋白工程、免疫评价、mRNA疫苗等核心技术平台组成的强大研发引擎,公司已建立由10余款高度差异化组成的高价值创新型疫苗组合,覆盖宫颈癌、带状疱疹、新冠肺炎、肺结核等具有重大负担的疾病领域。核心产品重组HPV九价疫苗REC603,临床进度领先。此外,重组新冠病毒疫苗ReCOV已成为全球最具竞争力的第二代新
冠疫苗之一
。新佐剂重组带状疱疹疫苗REC610具有较好的免疫原性,其表现非劣于
国际主流疫苗
,目前已进入临床阶段。瑞科生物已制定明确清晰的商业化策略,旨在于全球范围内进一步渗透多元化疫苗市场。十年磨剑,厚积薄发,瑞科生物即将进入产品商业化的爆发期。
前瞻性说明
本新闻稿可能包含与本集团财务状况、经营业绩、资本状况、战略和业务有关的预测、估计、预测、目标、意见、前景、结果、回报和前瞻性陈述,这些可以由使用前瞻性术语,例如"可能"、"将"、"应该"、"预期"、"预期"、"项目"、"计划"、"估计"、"寻求"、"打算"、"目标" 、"相信"、"潜在"和"合理可能"或其否定词或其他变体或类似术语(统称为"前瞻性陈述"),包括战略重点、研发项目和任何财务、投资和资本目标以及本演示文稿内书面或口头描述的任何其他目标、承诺和抱负。任何此类前瞻性陈述都不是未来业绩的可靠指标,因为它们可能涉及重要的陈述或暗示假设和主观判断,这些假设和主观判断可能会或可能不会被证明是正确、准确或完整的。无法保证前瞻性陈述中列出的任何事项是可以实现的、将实际发生或将实现的或完整或准确的。这些假设和判断可能被证明是不正确、不准确或不完整的,并涉及已知及未知的风险、不确定性、或有事项和其他重要因素,其中许多不在本集团的控制范围内。亦无法保证本集团可以成功开发或销售其核心产品或其他候选产品。由于各种风险、不确定性和其他因素(包括但不限于一般市场状况、监管变化、地缘政治紧张局势或数据限制和变化)。任何此类前瞻性陈述均基于本集团在作出陈述之日的信念、期望和意见而作出,若情况或管理层的信念、期望或意见有所改变,本集团不承担并在此声明其不承担任何更新、修改或补充这些陈述的责任或义务。出于这些原因,阁下不应依赖任何前瞻性陈述并明确警惕阁下不应依赖任何前瞻性陈述。本集团或其代表不就本演示文稿所载任何预测、估计、预测、目标、承诺、前景或回报的实现或合理性作出任何明示或暗示的陈述或保证。
投资者问询:
Email:
ir@recbio.cn
Tel: +86-0523-86818860
媒体问询:
Email:
media@recbio.cn
Tel: +86-0523-86818860

疫苗信使RNA
2023-08-28
·生物谷
肺纤维化是一种进行性疾病,正常肺组织的疤痕会导致呼吸衰竭死亡。目前可用的两种药物,吡非尼酮和尼达尼布,对存活率只有轻微的影响。
肺纤维化是一种进行性疾病,正常肺组织的疤痕会导致呼吸衰竭死亡。目前可用的两种药物,吡非尼酮和尼达尼布,对存活率只有轻微的影响。缺乏有效的治疗很可能是由于对触发疾病发生和发展的致病机制缺乏了解,特别是其特发性形式(特发性肺纤维化,IPF)。
图片来源:https://doi-org.libproxy1.nus.edu.sg/10.1038/s41419-023-05962-2
近日,来自意大利的国际遗传工程和生物技术中心的研究者们在Cell Death and Disease杂志上发表了题为“Flt1 produced by lung endothelial cells impairs ATII cell transdifferentiation and repair in pulmonary fibrosis”的文章,该研究揭示了肺内皮细胞产生Flt1影响肺纤维化ATII细胞转分化和修复。
肺纤维化是一种破坏性疾病,纤维化组织逐渐取代肺泡结构,导致慢性呼吸衰竭。肺泡II型细胞作为上皮干细胞,能够转分化为I型肺泡型细胞,介导气体交换,从而促进肺内环境的稳定和损伤后的修复。上皮细胞转分化受损是导致肺纤维化发生和发展的主要致病机制。
在本研究中,研究者展示了肺内皮细胞分泌调节肺泡细胞分化的血管分泌因子。具体地说,我们基于我们之前关于抗纤维化microRNA-200C的数据,并确定血管内皮生长因子受体1,也称为Flt1,是其在内皮细胞中的主要功能靶点。
内皮特异的Flt1基因敲除复制了microRNA-200C抗肺纤维化的抗纤维化作用,并导致一系列可溶性因子和基质成分的分泌,能够以旁分泌方式促进上皮细胞转分化。总之,这些数据表明在体外和体内存在复杂的内皮-上皮旁分泌串扰,并将肺内皮细胞定位为对抗肺纤维化的相关治疗靶点。
Flt1 KO内皮细胞分泌的蛋白质调控上皮细胞转分化
图片来源:https://doi-org.libproxy1.nus.edu.sg/10.1038/s41419-023-05962-2
总而言之,本研究结果首次表明,内皮-上皮串扰通过促进ATII向ATI细胞的分化而显著调节肺修复。这将内皮细胞定位为治疗肺纤维化的创新靶点,更广泛地说,治疗任何可以从增强的上皮再生中受益的疾病。(生物谷 Bioon.com)
参考文献
Maria Concetta Volpe et al. Flt1 produced by lung endothelial cells impairs ATII cell transdifferentiation and repair in pulmonary fibrosis. Cell Death Dis. 2023 Jul 15;14(7):437. doi: 10.1038/s41419-023-05962-2.
临床研究
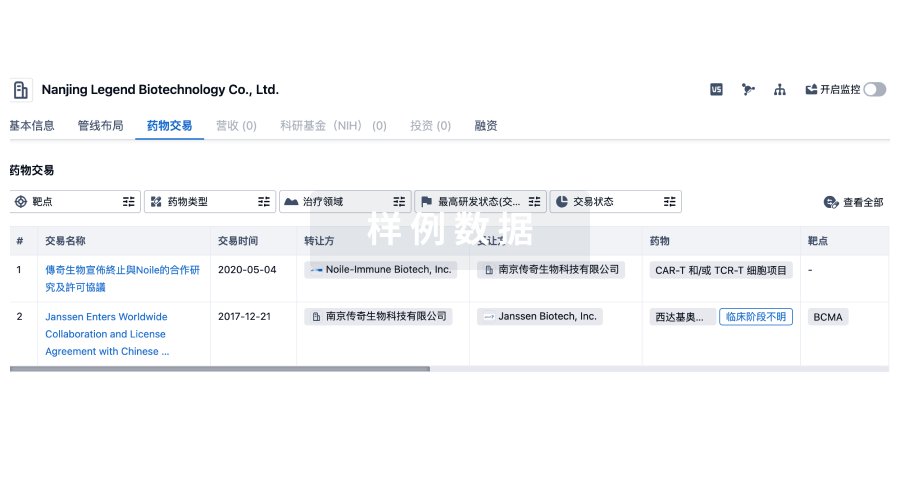
100 项与 ICGEB 相关的药物交易
登录后查看更多信息
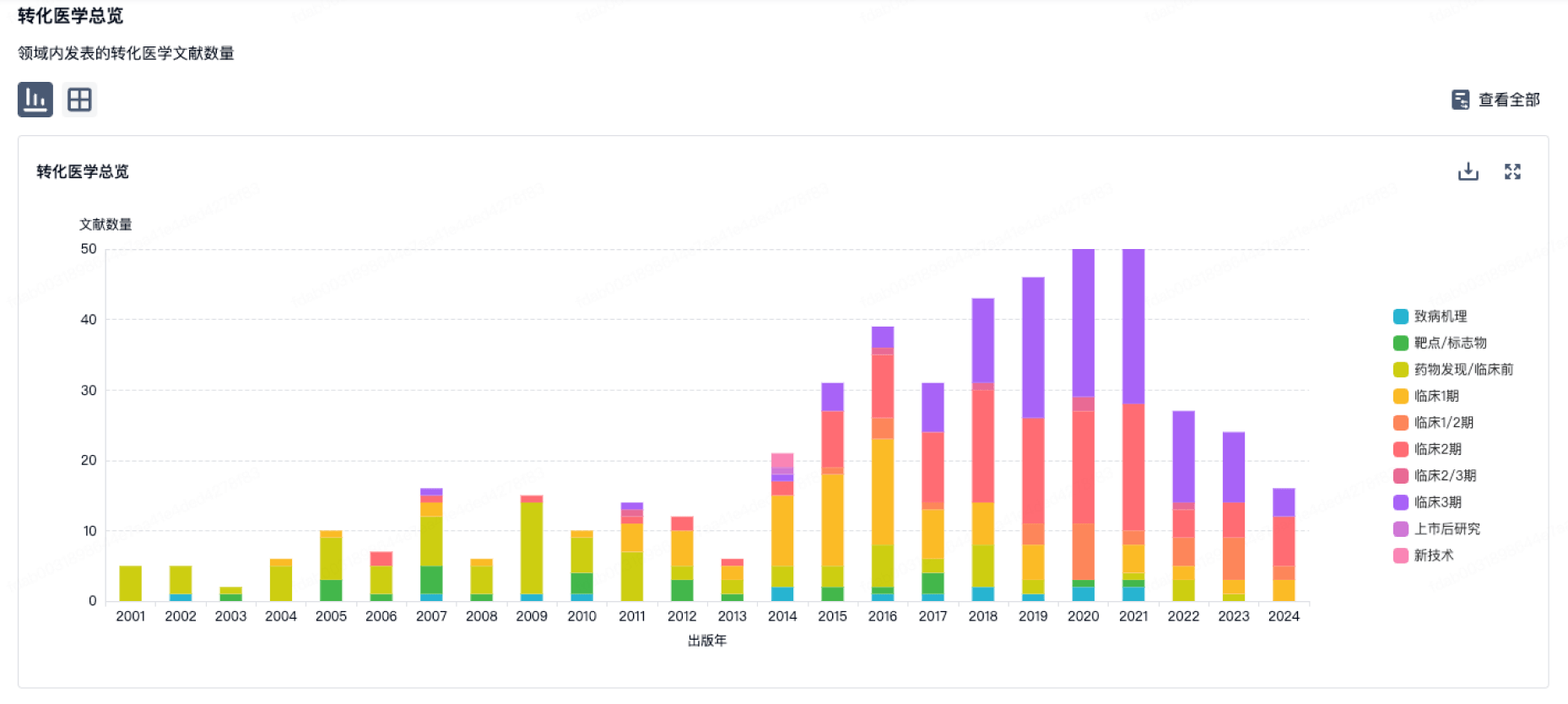
100 项与 ICGEB 相关的转化医学
登录后查看更多信息
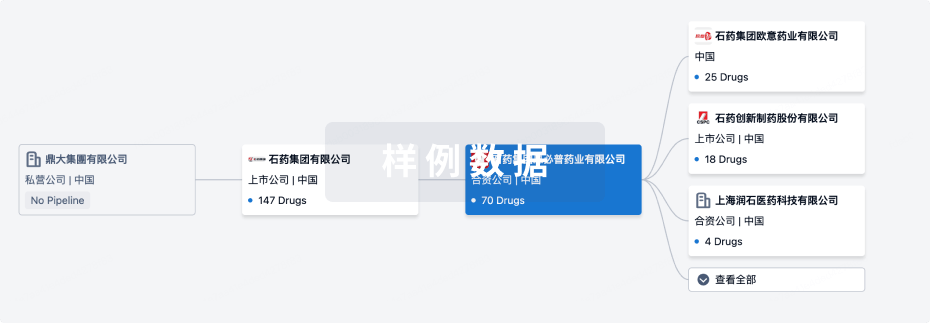
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年09月08日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
2
1
临床3期
批准上市
1
7
其他
登录后查看更多信息
当前项目
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
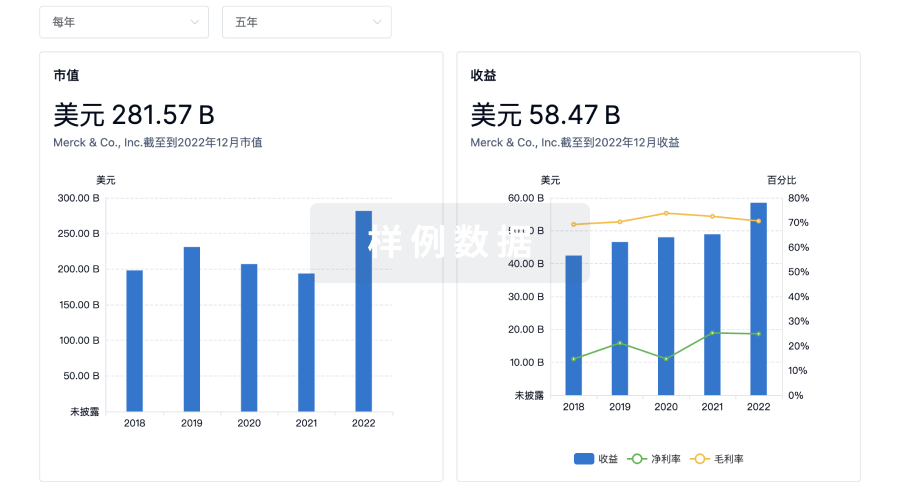
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

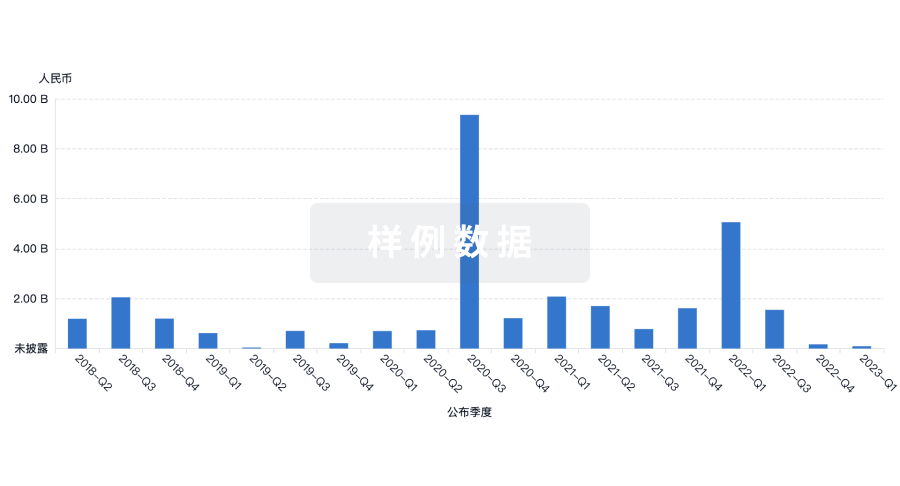
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
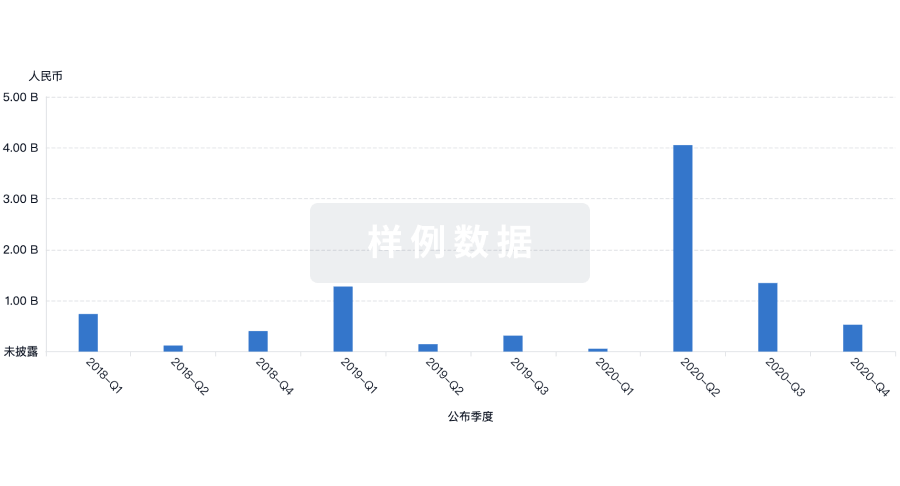
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用