预约演示
更新于:2025-08-29

CarThera SAS
更新于:2025-08-29
概览
标签
神经系统疾病
肿瘤
其他疾病
小分子化药
关联
1
项与 CarThera SAS 相关的药物靶点 |
作用机制 DNA抑制剂 |
在研机构 |
最高研发阶段批准上市 |
首次获批国家/地区 美国 |
首次获批日期1989-03-03 |
6
项与 CarThera SAS 相关的临床试验NCT05864534
A Phase 2a Trial of Immune Modulation in Combination With Ultrasound-mediated Blood Brain Barrier Opening in Patients With Newly Diagnosed Glioblastoma
Brain tumor treatment is hampered by the blood-brain barrier (BBB). This barrier prevents drugs carried in the bloodstream from getting into the brain. If the BBB can be opened, making it temporarily more permeable, drugs may able to better reach the brain tumor. In this trial we will implant a novel device with 9 ultrasound emitters, allowing temporary and reversible opening of the BBB to maximize brain penetration of drugs that modulate the immune system. The device will be implanted after radiation is completed. Immune modulating drugs will be given every 3 weeks in conjunction with activation of the device to open the BBB.
The objectives of this trial are to establish whether it is safe and feasible to administer immune modulating drugs in this manner, and identify whether the treatment is effective in treating glioblastoma.
The objectives of this trial are to establish whether it is safe and feasible to administer immune modulating drugs in this manner, and identify whether the treatment is effective in treating glioblastoma.
开始日期2024-01-31 |
申办/合作机构 |
NCT05902169
A Randomized, Open-label, Multicentric, Two-arm Pivotal Trial of SonoCloud-9 Combined With Carboplatin (CBDCA) vs Standard of Care Lomustine (CCNU) or Temozolomide (TMZ) in Patients Undergoing Planned Resection for First Recurrence Glioblastoma.
The brain is protected from any toxic or inflammatory molecule by the blood-brain barrier (BBB). This physical barrier is located at the level of the blood vessel walls. Because of these barrier properties, the blood vessels are also impermeable to the passage of therapeutic molecules from the blood to the brain. The development of effective treatments against glioblastoma is thus limited due to the BBB that prevents most drugs injected in the bloodstream from getting into brain tissue where the tumour is seated. The SonoCloud-9 (SC9) is an investigational device using ultrasound technology and specially developed to open the BBB in the area of and surrounding the tumour. The transient opening of the BBB allows more drugs to reach the brain tumour tissue. Carboplatin is a chemotherapy that is approved to treat different cancer types alone or in combination with other drugs, and has been used in the treatment of glioblastoma. Despite its proven efficacy in the laboratory on glioblastoma cells, carboplatin does not readily cross the BBB in humans. A clinical trial has shown that in combination with the SonoCloud-9, more carboplatin can reach the brain tumour tissue. The objective of the proposed trial is to show that the association - carboplatin with the SonoCloud-9 - will increase efficacy of the drug in patients with recurrent glioblastoma.
开始日期2024-01-29 |
申办/合作机构 |
NCT05293197
Phase I Trial Assessing the Safety of the Repeated Ultrasound-induced Opening of the Blood-brain Barrier in Pediatric Patients With Refractory Supra-tentorial Malignant Brain Tumors Before Chemotherapy Administration
Purpose : the aim of this study is to assess the feasibility and safety of ultrasound-induced opening of the blood-brain barrier (BBB) with the SonoCloud-9 implantable ultrasound device in pediatric patients treated for a recurrent malignant supra-tentorial brain tumor treated with carboplatin.
Study hypothesis : the blood-brain barrier can be transiently and safely opened with pulsed low intensity ultrasound immediately prior to intravenously delivered chemotherapy. The opening of the BBB with the SonoCloud-9 system will increase the tumor exposure to carboplatin and increase progression-free and overall survival in pediatric patients treated for a recurrent malignant supra-tentorial brain tumor.
Study hypothesis : the blood-brain barrier can be transiently and safely opened with pulsed low intensity ultrasound immediately prior to intravenously delivered chemotherapy. The opening of the BBB with the SonoCloud-9 system will increase the tumor exposure to carboplatin and increase progression-free and overall survival in pediatric patients treated for a recurrent malignant supra-tentorial brain tumor.
开始日期2023-02-06 |
申办/合作机构 |
100 项与 CarThera SAS 相关的临床结果
登录后查看更多信息
0 项与 CarThera SAS 相关的专利(医药)
登录后查看更多信息
8
项与 CarThera SAS 相关的新闻(医药)2025-04-22
PARIS--(BUSINESS WIRE)--Carthera, developer of the revolutionary SonoCloud® medical device, today announces it has enrolled the first 100 patients in its SONOBIRD pivotal trial for the treatment of recurrent glioblastoma. A spin-off of Sorbonne University founded by noted neurosurgeon Prof. Alexandre Carpentier, Carthera reaches this milestone as it prepares to conduct the largest clinical trial ever using ultrasound for the temporary opening of the blood-brain-barrier (BBB) in patients with recurrent glioblastoma.
Nearly all 40 participating sites across Europe and the U.S. are now active. Carthera anticipates that recruitment will continue swiftly to reach the 560 patients planned for the study.
The trial (NCT05902169) is the world’s first randomized, multicentric, two-arm pivotal trial of BBB opening prior to chemotherapy injection in recurrent glioblastoma patients. Notably, the trial makes use of the SonoCloud, an innovative ultrasound-based medical device developed by Carthera to treat a wide range of brain disorders. Specifically, the trial compares the use of SonoCloud combined with carboplatin versus standard therapies in patients with a first recurrence of glioblastoma.
“It has been a privilege to offer this trial to patients with recurrent glioblastoma. The underlying concept is highly promising, device implantation has proceeded smoothly and patients have shown strong interest in participating,” said Dr. Brian Gill, assistant professor of neurosurgery at Columbia University Irving Medical Center in New York.
“We desperately need new treatments for patients with recurrent glioblastoma. SonoCloud has the potential to transform our ability to deliver a high dose of therapeutics to the brain,” said Dr. Marjolein Geurts, neuro‐oncologist at Erasmus Medical Center Cancer Institute in Rotterdam, the Netherlands.
To date, more than 550 SonoCloud treatments have been performed worldwide, confirming Carthera’s position as a leader in the field of ultrasound-based BBB opening, as well as the growing interest in SonoCloud as a potentially viable new treatment option for patients with recurrent glioblastoma.
“Our progress in recruiting patients reflects the engagement and strong support from our clinical sites, and from the neuro-oncology and surgery community, in advancing innovative therapies,” said Carole Desseaux, chief clinical officer at Carthera. “We are very grateful for the commitment and enthusiasm of the patients and clinicians who are taking part in this trial.”
“Achieving this milestone is an important step in introducing our SonoCloud device to the large patient population urgently in need of solutions to improve treatment outcomes,” said Frederic Sottilini, CEO of Carthera. “With its breakthrough device and orphan drug designations, Carthera remains committed to transforming glioblastoma treatment and to acquiring market access for its groundbreaking technology.”
Initiated in February 2024, the registrational study aims to enroll a total of 560 US and EU patients within two years, with a view to obtaining marketing authorization. The first interim analysis of the clinical data will be available soon.
About the SONOBIRD trial
The open-label, comparative, randomized, multicenter, two-arm clinical trial with a 1:1 ratio aims to evaluate overall survival in patients undergoing carboplatin chemotherapy and treated with the SonoCloud system to open the Blood-Brain Barrier (BBB). This is compared to the medical consensus recommended regimens (lomustine or temozolomide). The trial also evaluates the effectiveness of the SonoCloud and carboplatin treatment in delaying or slowing tumor growth.
The SONOBIRD trial follows on from the SC9-GBM-01 trial, which demonstrated the feasibility and the safety profile of SonoCloud, as well as the potential of carboplatin tested as a monotherapy in combination with BBB opening.
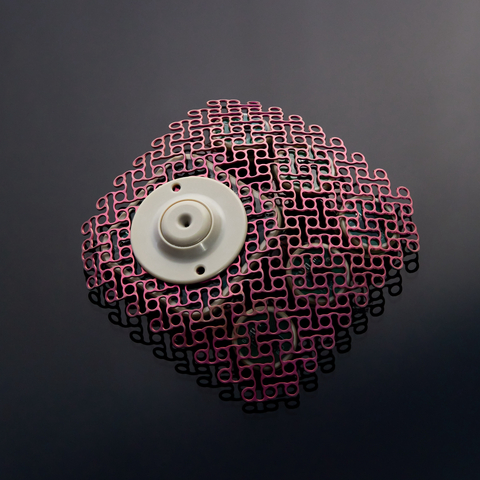
About SonoCloud
SonoCloud® is an innovative medical device developed by Carthera. It emits ultrasound to temporarily increase the permeability of the blood vessels in the brain to improve the delivery of therapeutic molecules. Invented by Prof. Alexandre Carpentier and developed in collaboration with the Laboratory of Therapeutic Applications of Ultrasound (Laboratoire Thérapie et Applications Ultrasonores, LabTAU, INSERM) in Lyon, France, SonoCloud is an implant inserted into the skull and activated prior to injection of a therapeutic agent. Several minutes of low-intensity ultrasound opens the blood-brain barrier for six hours and increases the concentration of therapeutic molecules in the brain. This ultrasound-induced opening of the blood-brain barrier is a world-first. It offers a new treatment option for a wide range of indications, including brain tumors and Alzheimer’s disease.
SonoCloud is an investigational product, the device has not yet received EMA or FDA approval.
About Carthera
Carthera is a clinical-stage medtech company focused on developing innovative ultrasound-based medical devices to treat a wide range of brain disorders. The company is a spin-off from AP-HP Paris and Sorbonne University. Carthera leverages the inventions of Prof. Alexandre Carpentier, head neurosurgeon at AP-HP Sorbonne university, who has achieved worldwide recognition for his innovative developments in treating brain disorders. Carthera is developing SonoCloud®, an intracranial implant that temporarily opens the blood-brain barrier. The device is currently in clinical trials in Europe and the United States. It received FDA Breakthrough Device Designation in 2022, and FDA/EMA Orphan Drug Designation in 2023 for carboplatin when used with SonoCloud.
Founded in 2010 by Prof. Alexandre Carpentier, run by CEO Frederic Sottilini and chaired by Oern Stuge, MD, Carthera has offices in France (Lyon and Paris) and a subsidiary in Boston, Massachusetts. Since its inception, the technical and clinical development of SonoCloud has received support from the National Research Agency (ANR), the French public investment bank (Bpifrance), the National Institutes of Health (NIH) and the European Innovation Council (EIC). Additional information is available at www.carthera.eu.
临床研究孤儿药
2025-01-28
Neurotechnology company, Grey Matter Neurosciences, announced it secured $14 million in seed financing, which will be used to develop an ultrasound headset for individuals with Alzheimer's disease and test that device in clinical trials.
The financing was led by the Wittington Innovation Fund, with participation from Toronto Innovation Acceleration Partners, Ontario Brain Institute and Ontario's Life Sciences Innovation Fund.
The company also announced that it has licensed advanced focused ultrasound technology developed at Sunnybrook Research Institute.
WHAT IT DOES
Grey Matter Neurosciences develops portable ultrasound helmet technology aimed at empowering seniors to restore brain function.
The company offers focused ultrasound technology for neuromodulation, with the aim of allowing seniors with Alzheimer's disease to experience enhanced brain-function recovery.
In a statement, the company said its offerings are based on transcranial focused-ultrasound technology, which was invented by Kullervo Hynynen at Sunnybrook Research Institute.
The seed funding will support advanced research on focused ultrasound neuromodulation. The company will construct an ultrasound headset for Alzheimer's patients and perform clinical trials to demonstrate the safety and feasibility of the technology.
Investigators will also analyze the ability of the transcranial focused-ultrasound device to sustainably improve cognitive performance, including memory.
"Generally speaking, there are no marketed therapies that can significantly and sustainably enhance cognitive function in individuals with dementia," Jeffrey Coull, founder and CEO of Grey Matter, said in a statement.
"I believe that our technology, which can reach the deepest recesses of the brain that control memory and learning, holds massive potential to boost cognition and, more generally, revolutionize how Alzheimer's and other diseases of the brain are treated."
The company also announced that Jim Orlando, managing partner of Wittington Ventures; Lara O'Donnell, executive director of the Weston Family Foundation; and Andy Smith, president and CEO of Sunnybrook Health Sciences Centre would join the company's board of directors.
In addition, Parimal Nathwani, president and CEO of Toronto Innovation Acceleration Partners, will serve as a board observer.
MARKET SNAPSHOT
Other companies in this space include Soterix Medical, which offers stimulation and synergistic monitoring technologies. In 2024, the company received 510(k) clearance from the FDA for its Intraoperative Neurophysiologic Monitoring (IOM) system.
MEGA-IOM provides integrated control of the central and peripheral nervous systems to reduce postoperative risk and improve surgical outcomes.
Also in 2024, CNS disease-focused NaviFUS entered into an agreement with Bracco, a company that markets ultrasound imaging agents, to enhance the NaviFUS system's capability to open the blood-brain barrier for the treatment of brain cancers and neurological diseases.
That same year, Sonic Concepts, a noninvasive therapeutic ultrasound platform, acquired the exclusive worldwide perpetual license for ultrasound neuromodulation patents from private neurotechnology company IST. The portfolio contains inventions and patents from Arizona State University that include discoveries of using low-intensity ultrasound for neuromodulation.
Carthera, a clinical-stage medtech company, focuses on developing innovative ultrasound-based medical devices to treat a wide range of brain disorders. SonoCloud is a medical device developed by Carthera that emits ultrasound to temporarily increase the permeability of the blood vessels in the brain to improve the delivery of therapeutic molecules.
In 2024, Carthera launched a Phase 2a clinical trial. The Northwestern University-sponsored trial used Carthera’s SonoCloud-9 device with Agenus’ checkpoint inhibitors balstilimab and botensilimab in patients with newly diagnosed glioblastoma (GBM) who have completed radiotherapy.
临床2期引进/卖出
2023-07-07
·动脉网
脑胶质瘤是最常见的原发性恶性脑肿瘤,胶质母细胞瘤(GBM)是最高级别以及恶性程度最高的脑胶质瘤,占颅内原发性恶性肿瘤的45%,术后极易复发,患者五年生存率不足5%。GBM是神经外科治疗中最棘手的难治性肿瘤之一。治疗脑胶质瘤的一个主要障碍是血脑屏障(BBB)。血脑屏障是一种微观结构,可以保护大脑免受绝大多数循环药物的侵害,但同时血脑屏障也阻断了95%以上的小分子和100%的大分子药物在大脑中的渗透,连最有效的化疗药物也无法渗透血脑屏障抵达脑肿瘤。因此,如何穿透血脑屏障,将诊断或治疗性化合物递送到大脑是神经系统疾病治疗中主要的技术障碍。CarThera成立于2010年,是法国的一家创新医疗器械公司,专注于研发基于超声治疗脑肿瘤的医疗设备。公司旗下的SonoCloud是一种植入颅内的超声设备,原则上可用于治疗原发性脑肿瘤(神经胶质瘤,胶质母细胞瘤,星形细胞瘤等)以及继发性脑肿瘤。动脉网获悉,2023年6月27日,Carthera完成3750万欧元B轮融资,这笔新的资金将用于启动植入式设备SonoCloud的多中心试验。此前,Carthera已进行过6轮融资,融资总金额超6680万欧元。Carthera融资历史 数据来源:crunchbase 基于超声打开血脑屏障,设备已获FDA突破性设备认定2015年,来自加拿大多伦多桑尼布鲁克研究所的科学家们宣布,他们利用充气微泡和超声波成功打开了一位脑癌患者的血脑屏障。患者服药并注射微泡后,在聚焦超声装置的作用下,微泡会产生振动,迫使构成血脑屏障的内皮细胞分开,血液中的化疗药物便可从间隙中穿过,到达肿瘤细胞附近。CarThera团队的研究也有着类似的原理,利用低强度脉冲超声结合静脉注射微泡(LIPU-MB)打开血脑屏障,但他们的研究相对桑尼布鲁克研究所存在新突破。一、CarThera使用了新研发的可植入颅内的1MHz超声设备SonoCloud;二、参与研究的患者共15名,获得的实验数据会更充分;三、在脑肿瘤治疗的每个治疗周期会重复打开血脑屏障,但未对人体造成伤害,证明此技术的安全性;四、相对于桑尼布鲁克研究所的精准定向于未扩散的肿瘤,CarThera研究使用的超声更发散,对GBM这样侵入周边组织的肿瘤更有效。在CarThera的研究中,患者首先服用化疗药物,医生向患者血管中注射充气微泡,然后将SonoCloud植入脑部区域的颅骨窗口,该窗口是医生在手术切除复发性GBM时创造的。然后在每个治疗周期,使用一次性无菌透皮针头和电缆将植入物通过经皮通道连接到脉冲发生器,SonoCloud得到激活并释放低强度超声,引起微泡振动,从而增加大脑中血管的通透性,药物可以以更高、更有效的浓度到达大脑。2022年6月22日,SonoCloud已获美国FDA突破性设备认定。SonoCloud 图源:CarThera官网 完成复发性GBM Ⅰ/Ⅱ期试验,扩展AD、脑转移瘤等适应症● 针对治疗复发性GBM,增加4~6倍药物浓度紫杉醇是一种“抗癌神药”,广泛应用于乳腺癌、卵巢癌、非小细胞肺癌、胰腺癌、食管癌及胃癌等恶性肿瘤的治疗。但紫杉醇无法跨越血脑屏障到达脑肿瘤,在系统给药治疗恶性神经胶质瘤的Ⅰ/Ⅱ期试验中也没有显示出疗效。而SonoCloud可以协助紫杉醇抵达脑肿瘤。2020年,为了进一步验证SonoCloud协助紫杉醇治疗复发性GBM的安全性和有效性,CarThera与西北大学合作开展人体复发性GBMⅠ/Ⅱ期试验。2023年5月2日,西北大学的科研人员发表在《柳叶刀·肿瘤学》的首个人体临床试验结果表明,SonoCloud释放4分钟的低强度脉冲超声可使血脑屏障开放1个小时,让进入人脑中的紫杉醇和卡铂等化疗药物浓度增加约4~6倍。● 减少β-淀粉样蛋白含量,适应症扩展到AD据《2021年世界阿尔茨海默病报告》显示,全球阿尔茨海默症(老年痴呆症,AD)患者数量超5500万。随着老年化社会的加速到来,AD患者数量还会急剧上升,预计2050年会上升到1.39亿。AD一般伴随着两种特征,一是细胞产生的细胞外异常沉积形成老年斑(β-淀粉样蛋白堆积形成),二是AD患者脑内神经元纤维会形成缠绕影响大脑功能。因此β-淀粉样蛋白逐渐被认为是引发AD的元凶之一。使用Sonocloud设备治疗脑肿瘤的过程中,Carthera团队发现在没有任何施药的情况下,人体内的β-淀粉样蛋白和Tau蛋白减少。因此Carthera团队决定将Sonocloud适应症扩张到AD,开始着手准备针对AD患者的临床试验。在局部麻醉下,将Sonocloud植入到轻度AD患者的脑部左侧边缘上。每个月对AD患者进行两次超声检查,每次大约持续10分钟以暂时破坏血脑屏障。在这个过程中,用PET(正电子发射计算机断层扫描技术)监测经4、8个月治疗后患者的大脑代谢和β-淀粉样蛋白水平。临床研究结果证明,尽管治疗和观察期较短,但经Sonocloud打开血脑屏障后,大多数患者的β-淀粉样蛋白水平下降,AD患者的症状可以有效延缓或者改善。目前CarThera已完成AD治疗的Ⅰ/Ⅱ期临床试验,Sonocloud治疗AD的有效性和安全性得到验证。接下来CarThera将与制药企业合作,探究如何将Sonocloud与新的药物疗法相结合,以获得更好的疗效。同时,CarThera已经验证了SonoCloud技术可以增强CAR-T免疫疗法治疗脑肿瘤的疗效;CarThera还在研究Sonocloud单独使用或结合其他化疗药物治疗脑转移瘤、早期GBM等脑疾病的有效性。临床试验进度 图源:CarThera官网治疗方案不断更新,电场、超声为脑肿瘤治疗带来新选择近些年来,科学家不断研究,在经历传统的放疗、化疗,以及靶向药物之后,免疫疗法堪称癌症治疗的第三次革命,而新兴的电场治疗、超声治疗为治疗脑肿瘤带来了新的选择。由于普通化疗的治疗指数低、副作用强,科学家一直在寻找特异性杀死肿瘤细胞而不影响正常细胞的治疗手段。靶向治疗就是他们找到的第一个替代化疗的治疗方案,其原理是根据肿瘤细胞的基因突变进行精准打击。但是一旦靶点基因发生突变,靶向药物就会失去作用;一些癌症患者在经过靶向治疗几年后,还会出现耐药情况。肿瘤免疫治疗起源于19世纪末期,但在近30年才得以快速发展。其作用原理是通过激活人体免疫系统,调动机体免疫细胞活性,让失活的免疫细胞再次活跃起来间接消灭肿瘤细胞,这个过程往往较为漫长。CAR-T技术与PD-1和PD-L1抗体药物是免疫疗法中具有代表性的突破。肿瘤电场治疗(TTFields) 是一种新的癌症治疗方式,利用敷贴于头皮的无创传感器电极阵列,产生中低频肿瘤治疗场,通过抑制肿瘤细胞有丝分裂发挥抗肿瘤作用。2011和2015年,TTFields先后被美国FDA批准应用于复发性和新诊断GBM的治疗,目前已经在美国、中国、欧洲、日本相继进入临床应用。超声作为一种经济、有效、无创、实时和安全的治疗方式,除用于分子水平诊断和病理过程监测外,能通过机械效应和热效应深入机体内部定位组织和细胞,已逐渐用于药物和基因的靶向递送。低强度脉冲超声技术打开血脑屏障的研究已经持续了二十多年,但目前还没有产品真正走到临床应用。近期推荐声明:动脉网所刊载内容之知识产权为动脉网及相关权利人专属所有或持有。未经许可,禁止进行转载、摘编、复制及建立镜像等任何使用。动脉网,未来医疗服务平台
突破性疗法细胞疗法临床研究免疫疗法微生物疗法
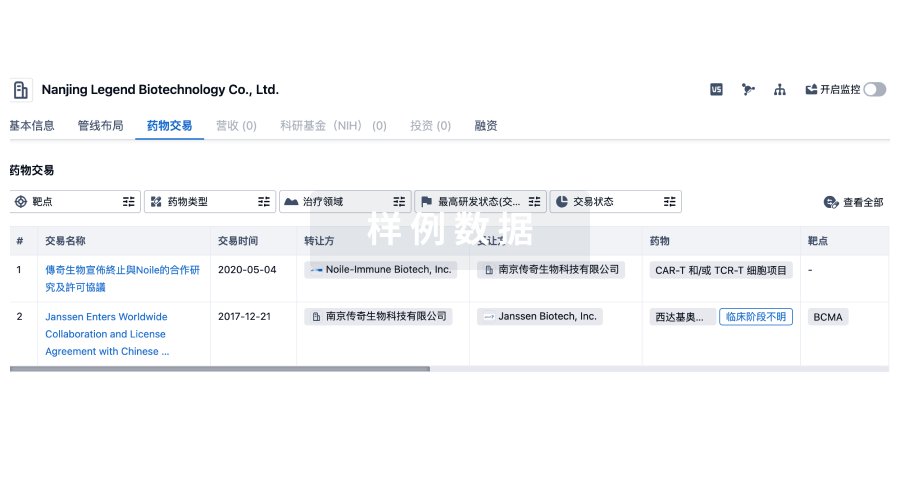
100 项与 CarThera SAS 相关的药物交易
登录后查看更多信息
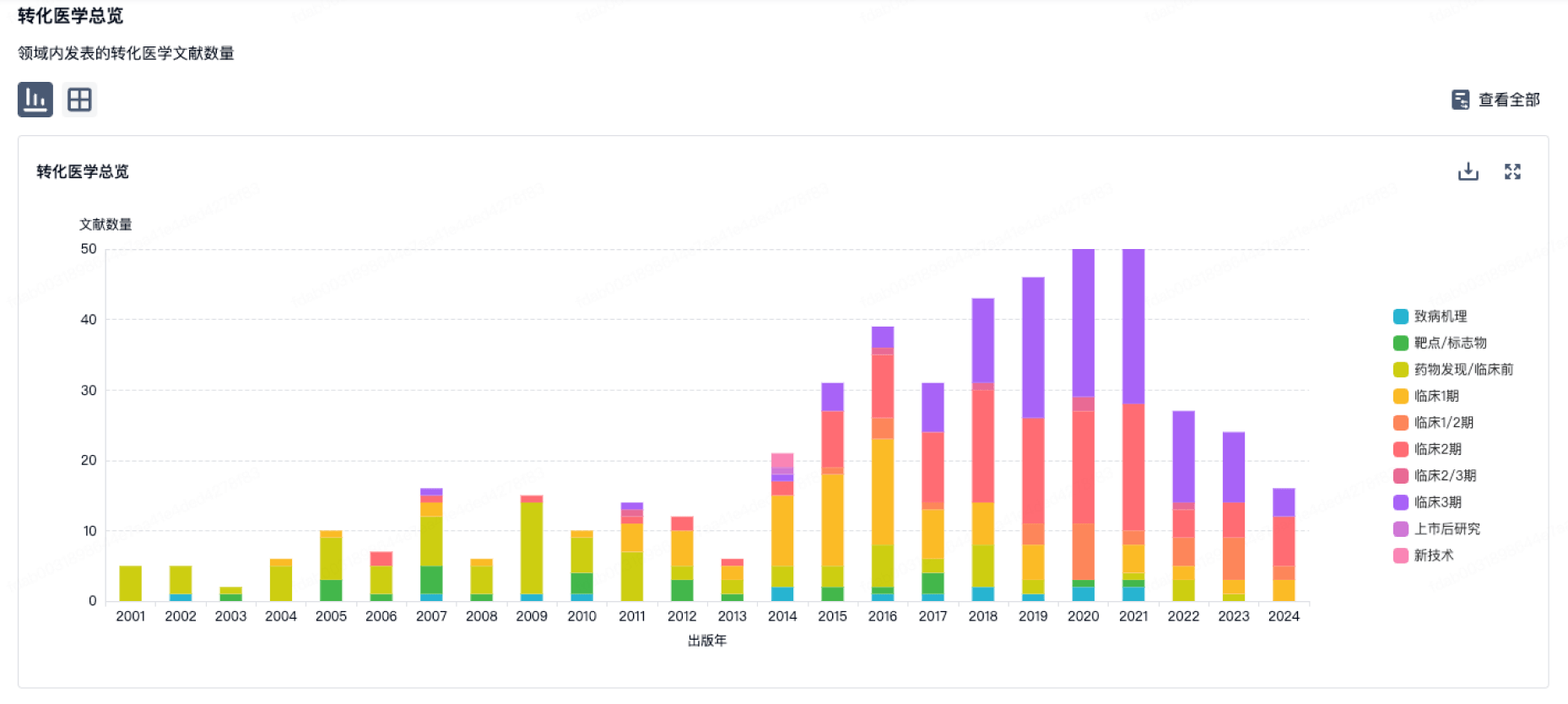
100 项与 CarThera SAS 相关的转化医学
登录后查看更多信息
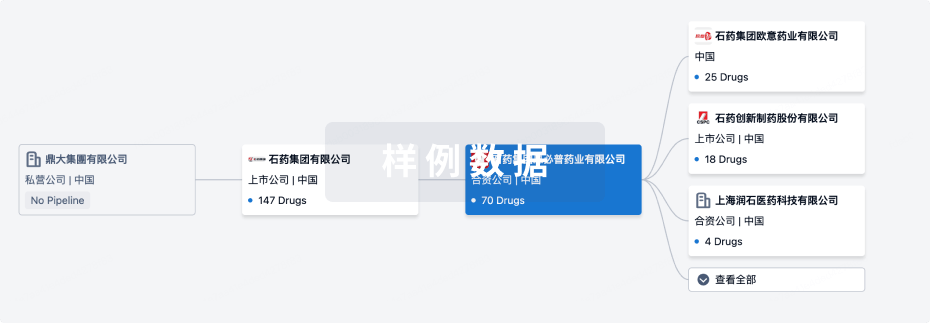
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年10月20日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床3期
1
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
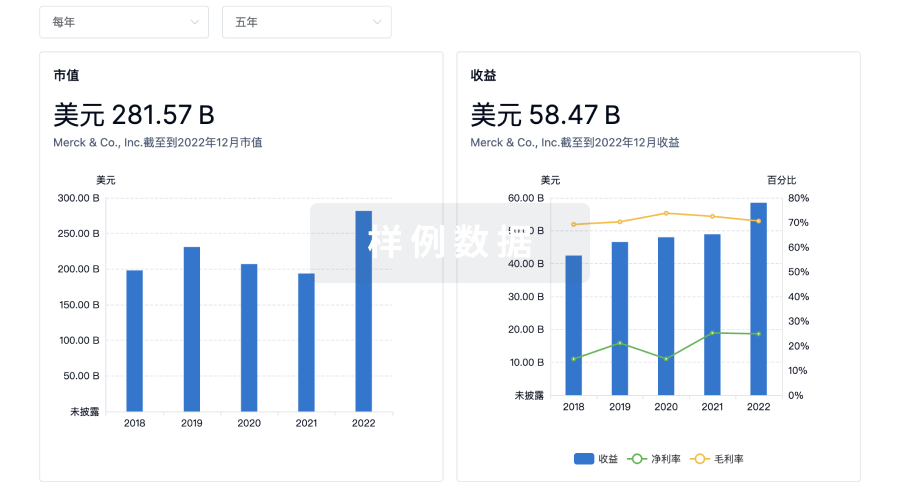
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

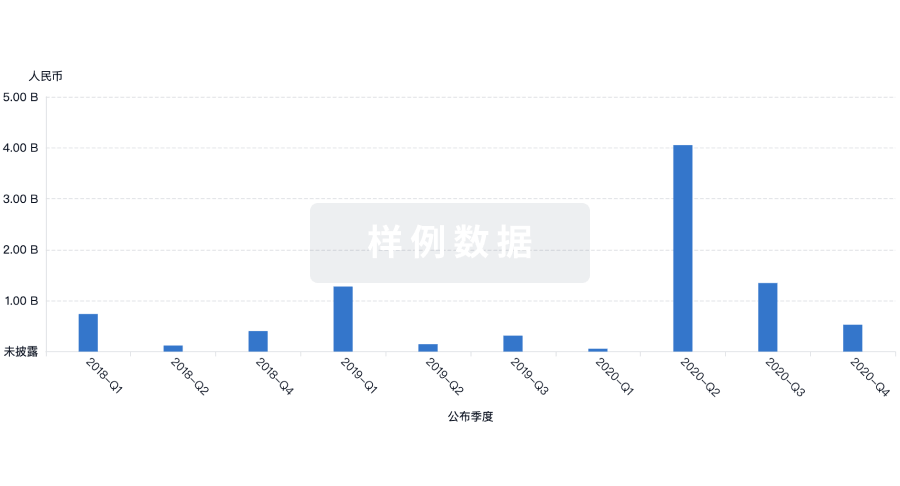
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
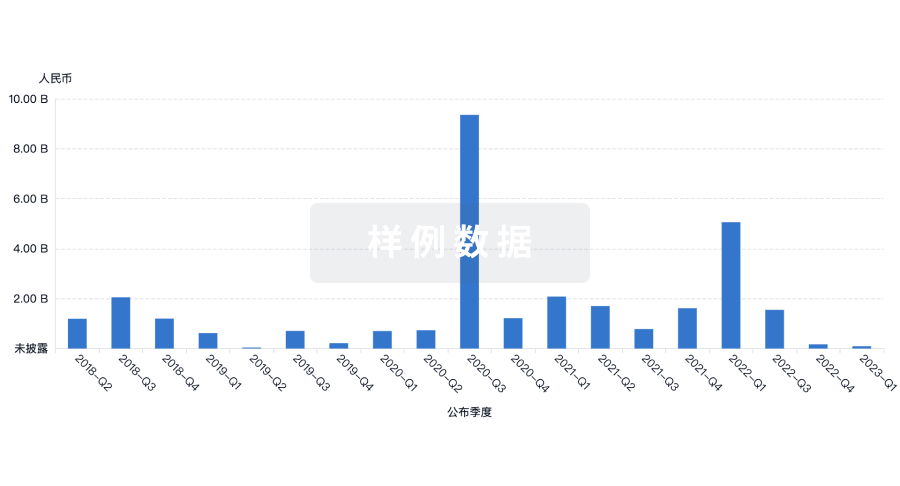
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


