预约演示
更新于:2025-09-09
Chang Gung Memorial Hospital
更新于:2025-09-09
概览
标签
其他疾病
消化系统疾病
肿瘤
小分子化药
腺相关病毒基因治疗
生长因子
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 6 |
| 腺相关病毒基因治疗 | 1 |
| 生长因子 | 1 |
关联
8
项与 长庚纪念医院 相关的药物1,241
项与 长庚纪念医院 相关的临床试验NCT04052191
Intra-Coronary Administration of MCRcI® (Myo-Cardial Regenerative Cellular Injection) Improves Left Ventricular Function in Patients With Diffuse Coronary Artery Disease
Safety evaluation of Intra-Coronary Administration of MCRcI® stem cells in Patients with Diffuse Coronary Artery Disease.
开始日期2025-12-01 |
申办/合作机构 鸿曜医学股份有限公司 [+1] |
NCT07087951
Development and Validation of an Innovative Gamma Auditory Stimulation System for Older Adults With Cognitive Decline: A Randomized, Double-blind, Placebo-controlled Study (Study 1)
Animal studies have shown that 40 Hz auditory stimulation alone can improve spatial memory and reduce Aβ deposition. However, human studies using 40 Hz auditory stimulation alone remain limited. Therefore, this study will use a randomized, double-blind, placebo-controlled design to investigate the effects of 40 Hz auditory stimulation on cognitive function, EEG activity, sleep quality, and quality of life in older adults with mild cognitive impairment (MCI) or mild dementia.
开始日期2025-09-01 |
申办/合作机构 |
NCT07122882
Integrated Genomics in Oncogene-driven Non-small Cell Lung Cancer With Acquired Resistance to Tyrosine Kinase Inhibitors
Currently, tyrosine kinase inhibitor (TKI) remains the standard of care for oncogene-driven non-small cell lung cancer (NSCLC). However, almost all oncogene-driven NSCLCs would develop acquired resistance against TKI in clinical practice. Therefore, understanding the molecular mechanisms underlying the acquired resistance is a critical issue in lung cancer. Based on the literature, acquired resistance mechanism against EGFR TKI includes EGFR secondary mutation (T790M, C797X, L792X, G796X, L718Q, and exon 20 insertions), MET amplification, HER2 amplification, acquired gene fusions, and other complex alterations.
From the perspective of mutagenesis, the acquired resistance against TKI may be associated with APOBEC mutational processes, kataegis, chromothripsis, extrachromosomal DNA (ecDNA), and the interaction among them. However, still 30% to 50% of oncogene-driven NSCLCs had no identified mechanism attributed to the acquired resistance. Previous studies mostly used targeted-gene sequencing, which may overlook some structural variation and the transcriptomic dynamics. This study aims to investigate the genomic alterations, mutational processes, and the transcriptomic landscape underlying the acquired resistance using integrated genomics.
From the perspective of mutagenesis, the acquired resistance against TKI may be associated with APOBEC mutational processes, kataegis, chromothripsis, extrachromosomal DNA (ecDNA), and the interaction among them. However, still 30% to 50% of oncogene-driven NSCLCs had no identified mechanism attributed to the acquired resistance. Previous studies mostly used targeted-gene sequencing, which may overlook some structural variation and the transcriptomic dynamics. This study aims to investigate the genomic alterations, mutational processes, and the transcriptomic landscape underlying the acquired resistance using integrated genomics.
开始日期2025-09-01 |
申办/合作机构 |
100 项与 长庚纪念医院 相关的临床结果
登录后查看更多信息
0 项与 长庚纪念医院 相关的专利(医药)
登录后查看更多信息
14,394
项与 长庚纪念医院 相关的文献(医药)2026-01-01·ULTRASONICS
Utilizing QUS envelope statistics imaging to predict the risk of vertebral fractures in postmenopausal women
Article
作者: Wang, Chiao-Yin ; Lin, Yu-Ching ; Tang, Ya-Chun ; Tsui, Po-Hsiang
This study aims to evaluate the clinical utility of quantitative ultrasound (QUS) envelope statistics imaging in predicting the risk of vertebral fractures (VFs) in postmenopausal women, compared to conventional dual-energy X-ray absorptiometry (DXA) measurements, including bone mineral density (BMD) and T-score. A total of 63 postmenopausal women were enrolled. QUS envelope statistics imaging was performed on the L3 vertebra, analyzing parameters including the Nakagami parameter (m), scatterer clustering parameter (α), coherent to diffuse signal ratio (k), and entropy (H) for comparisons with DXA. The data were divided into three tertiles: reference, early VF risk, and high-risk groups. Odds ratios (ORs) were calculated to evaluate the predictive abilities of each parameter for VF risk. Intraclass correlation coefficients (ICCs) and Bland-Altman plots were utilized to evaluate consistency both within subjects and across different operators. There were no significant differences in QUS parameters between subjects with and without VFs overall (p > 0.05). However, compared to DXA, the Nakagami parameter and entropy demonstrated a significant association with early VF risk, as subjects in the second tertile exhibited higher risks of VFs compared to those in the first tertile (ORs: 3.02 for m and 3.30 for H). Bland-Altman analysis indicated mean differences close to zero and ICCs exceeding 0.90 for all QUS parameters. QUS envelope statistics imaging could complement DXA in predicting VFs, particularly in detecting early fracture risk, offering a non-invasive, radiation-free alternative for osteoporosis screening.
2025-12-31·OncoImmunology
Mixed cryoglobulinemia decelerates hepatocellular carcinoma development in hepatitis C patients with SVR by downregulating regulatory B cells: a 12-year prospective cohort study
Article
作者: Cheng, Jur-Shan ; Shen, Yi-Jyun ; Chien, Rong-Nan ; Chen, Wei-Ting ; Chang, Ming-Ling ; Kuo, Chia-Jung
How mixed cryoglobulinemia (MC) affects cancer risk in chronic hepatitis C patients with sustained virologic response (SVR) remains unclear. In a 12-year prospective study, post-SVR MC was assessed every 3‒6 months. Among the 891 SVR patients, 265 (29.7%) had baseline (24 weeks after completing anti-HCV therapy) MC, and the 12-year cancer cumulative incidence was 19.7%. Among the 73 patients who developed cancer, 37 (50.7%) had hepatocellular carcinoma (HCC), with the following associated baseline variables: for cancer, male sex, age and alanine aminotransferase (ALT) levels; for HCC, male sex, age, and cirrhosis; and for non-HCC cancer, rheumatoid factor levels. Among patients with post-SVR HCC, the mean time to HCC was longer in those with than in those without baseline MC (1545.4 ± 276.5 vs. 856.9 ± 115.2 days, p = 0.014). Patients with baseline MC had decreased circulating interleukin-10 (IL-10)-positive B cell (CD19+IL-10+cells/CD19+cells) (31.24 ± 16.14 vs. 40.08 ± 15.42%, p = 0.031), regulatory B cell (Breg) (CD19+CD24hi CD27+cells/CD19+cells) (10.45 ± 7.10 vs. 15.76 ± 9.14%, p = 0.035), IL-10-positive Breg (CD19+CD24hiCD27+IL-10+cells/CD19+cells) (5.06 ± 4.68 vs. 8.83 ± 5.46%, p = 0.015) and HCC-infiltrating Breg (18.6 ± 10 vs. 33.51 ± 6.8%, p = 0.022) ratios but comparable circulating and HCC-infiltrating regulatory T cell ratios relative to patients without baseline MC. In conclusion, old male SVR patients with elevated ALT levels or cirrhosis require intensive monitoring for cancer development, especially HCC. Tailored HCC follow-up is needed for SVR patients according to their baseline MC, which might downregulate Bregs to decelerate HCC development for almost 2 years.
2025-12-31·VETERINARY QUARTERLY
Multiplexed immunoassay for a serum autoantibody biomarker panel in diagnostic and prognostic prediction of canine mammary tumors
Article
作者: Chan, Xiu-Ya ; Huang, Chun-Chueh ; Wu, Chih-Ching ; Liu, Hao-Ping ; Chou, Pei-Yi ; Yang, Youngsen ; Chang, Chia-Yu
Canine mammary tumor (CMT) is a prevalent and destructive disease often diagnosed at an advanced stage, leading to poor outcomes. Currently, there is a lack of effective biomarkers for early detection and prognostic prediction of CMT. To improve CMT detection, we established a multiplexed immunoassay using a fluorescence bead-based suspension array system to measure serum levels of autoantibodies against four CMT-associated proteins (AGR2, HAPLN1, IGFBP5, and TYMS) in CMT patients. Our data revealed that serum levels of the four autoantibodies (anti-AGR2, anti-HAPLN1, anti-IGFBP5, and anti-TYMS) were significantly elevated in CMT patients (n = 158) compared to healthy individuals (n = 39). Notably, serum levels of anti-AGR2, anti-HAPLN1, and anti-TYMS in the dogs with stage I CMT (n = 56) were higher than those in the healthy group. Using a marker panel consisting of the four autoantibodies for detecting malignant CMT (n = 125) achieved a sensitivity of 50.4% and a specificity of 90%. Furthermore, higher levels of anti-AGR2, anti-HAPLN1, anti-IGFBP5, and anti-TYMS were associated with poorer survival in CMT patients. Collectively, we established a multiplexed immunoassay platform to detect serum autoantibodies and demonstrated that a tailored autoantibody marker panel shows potential clinical applicability for the diagnosis and prognosis of CMT.
57
项与 长庚纪念医院 相关的新闻(医药)2025-09-02
September 2, 2025 6:45 am ET
Enlicitide is the first oral PCSK9 inhibitor to demonstrate statistically significant and clinically meaningful reductions in LDL-C compared to placebo in Phase 3 trials
Enlicitide had a favorable safety profile, with comparable rates of discontinuation between treatment groups
RAHWAY, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced positive topline results from the Phase 3 CORALreef Lipids trial evaluating the safety and efficacy of enlicitide decanoate, an investigational, once-daily oral proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor being evaluated for the treatment of adults with hypercholesterolemia on a moderate or high intensity statin (or with documented statin intolerance).
The CORALreef Lipids trial successfully met all primary and key secondary endpoints. Treatment with enlicitide resulted in statistically significant and clinically meaningful reduction in low-density lipoprotein cholesterol (LDL-C) compared to placebo at Week 24. Statistically and clinically significant reductions were also seen for enlicitide versus placebo across all key secondary endpoints including in non-high-density lipoprotein cholesterol (non-HDL-C), apolipoprotein B (ApoB), and lipoprotein(a) [Lp(a)]. There were no clinically meaningful differences in proportions of participants with adverse events (AE), including serious adverse events (SAE), between treatment groups. Discontinuations due to adverse events were low and comparable between treatment groups.
CORALreef Lipids represents the largest completed Phase 3 study evaluating enlicitide in a broad range of participants with elevated LDL-C and a history of or increased risk for major atherosclerotic cardiovascular disease events despite treatment with at least a moderate or high intensity statin (or with documented statin intolerance). Merck plans to share these results with regulatory authorities worldwide and will present the data at a future scientific congress.
“This is the third Phase 3 trial to demonstrate clinically meaningful and statistically significant LDL-C lowering for enlicitide,” said Dr. Dean Y. Li, president, Merck Research Laboratories. "The advent of injectable PCSK9 inhibitors has enabled a new approach to controlling LDL-C and reducing the risk of atherogenic cardiovascular events. Enlicitide, designed to deliver antibody-like efficacy, is the first oral macrocyclic peptide PCSK9 inhibitor with clinically meaningful and statistically significant LDL-C lowering in Phase 3 trials. If approved, it has the potential to change the way we think about managing LDL levels, giving patients the possibility of a new option to help them meet their treatment goals.”
“These data add to the growing body of evidence supporting the safety and efficacy profile of enlicitide to lower LDL cholesterol and other key atherogenic lipids including ApoB and Lp(a),” said Dr. Ann Marie Navar, a lead trial investigator of the study and Associate Professor of Medicine in the Division of Cardiology at UT Southwestern Medical Center. “Enlicitide has the potential to help more patients achieve guideline-recommended lipid goals and ultimately reduce atherosclerotic cardiovascular risk, which is currently being evaluated in an ongoing cardiovascular outcomes trial.”
About CORALreef Lipids
CORALreef Lipids (NCT05952856) was a Phase 3 randomized, double-blind, placebo-controlled study designed to evaluate the efficacy, safety and tolerability of enlicitide decanoate in adults with hypercholesterolemia and a history of a major atherosclerotic cardiovascular disease (ASCVD) event or increased risk for a first event. Participants were required to be treated with stable lipid lowering therapies including at least a statin (or have documented statin intolerance). The study’s primary objective was to assess whether enlicitide decanoate was superior to placebo in reducing LDL-C, as measured by mean percent change from baseline at Week 24. Key secondary efficacy endpoints included: change from baseline in LDL-C at week 52 and change from baseline in other key atherogenic lipids at week 24 (non-HDL-C, apolipoprotein B, lipoprotein(a) [Lp(a)]).
The efficacy and safety of enlicitide are being evaluated through the comprehensive CORALreef Clinical Trial program, including the large cardiovascular outcomes trial, CORALreef Outcomes, which has completed enrollment with over 14,500 participants. As previously announced, enlicitide demonstrated statistically significant and clinically meaningful reductions in LDL-C in both the Phase 3 CORALreef HeFH and CORALreef AddOn trials. The CORALreef program reflects Merck’s commitment to advancing research to help address the global burden of atherosclerotic cardiovascular disease.
About enlicitide and PCSK9
Enlicitide is an investigational, potentially first oral PCSK9 inhibitor designed to lower LDL-C via the same biological mechanism as currently approved monoclonal antibody, injectable PCSK9 inhibitors but in a daily pill form. Enlicitide is a novel small molecule macrocyclic peptide that binds to PCSK9 and inhibits the interaction of PCSK9 with LDL receptors.
PCSK9 plays a key role in cholesterol homeostasis by regulating levels of the LDL receptor, which is responsible for the uptake of cholesterol into cells. Inhibition of PCSK9 is designed to prevent the interaction of PCSK9 with LDL receptors. This results in greater numbers of LDL receptors available on the cell surface to remove LDL cholesterol from the blood.
About hypercholesterolemia
Hypercholesterolemia, a type of hyperlipidemia, is a disorder in which there are elevated LDL cholesterol levels in the blood. It affects approximately 86 million adults in the U.S and is a major risk driver for ASCVD, accounting for 85% of cardiovascular deaths. Nearly 70% of people with ASCVD who are treated with lipid lowering therapies do not reach target low-density lipoprotein cholesterol. High LDL-C, if left untreated, can lead to ASCVD events such as heart attacks and strokes.
Merck’s focus on cardiovascular disease
Merck has a long history of developing treatments for cardiovascular disease. More than 60 years ago, we introduced our first cardiovascular therapy—and our scientific efforts to understand and treat cardiovascular-related disorders have continued. Cardiovascular disease continues to be one of the most serious health challenges of the 21st century and is the leading cause of death worldwide. Approximately 18 million people across the globe die from cardiovascular disease every year; in the United States, one person dies every 36 seconds from cardiovascular disease.
Advancements in the treatment of cardiovascular disease can make a critical difference for patients and health systems around the world. At Merck, we strive for scientific excellence and innovation in all stages of research, from discovery through approval and life cycle management. We work with experts throughout the cardiovascular and pulmonary community to advance research that can help improve the lives of patients globally.
Information for other currently enrolling cardiovascular studies can be found by visiting: https://www.merckclinicaltrials.com/cardiovascular.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world—and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable, and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on X (formerly Twitter), Facebook, Instagram, YouTube and LinkedIn.
Forward-Looking statement of Merck & Co., Inc., Rahway, N.J., USA
This news release of Merck & Co., Inc., Rahway, N.J., USA (the “company”) includes “forward-looking statements” within the meaning of the safe harbor provisions of the U.S. Private Securities Litigation Reform Act of 1995. These statements are based upon the current beliefs and expectations of the company’s management and are subject to significant risks and uncertainties. There can be no guarantees with respect to pipeline candidates that the candidates will receive the necessary regulatory approvals or that they will prove to be commercially successful. If underlying assumptions prove inaccurate or risks or uncertainties materialize, actual results may differ materially from those set forth in the forward-looking statements.
Risks and uncertainties include but are not limited to, general industry conditions and competition; general economic factors, including interest rate and currency exchange rate fluctuations; the impact of pharmaceutical industry regulation and health care legislation in the United States and internationally; global trends toward health care cost containment; technological advances, new products and patents attained by competitors; challenges inherent in new product development, including obtaining regulatory approval; the company’s ability to accurately predict future market conditions; manufacturing difficulties or delays; financial instability of international economies and sovereign risk; dependence on the effectiveness of the company’s patents and other protections for innovative products; and the exposure to litigation, including patent litigation, and/or regulatory actions.
The company undertakes no obligation to publicly update any forward-looking statement, whether as a result of new information, future events or otherwise. Additional factors that could cause results to differ materially from those described in the forward-looking statements can be found in the company’s Annual Report on Form 10-K for the year ended December 31, 2024 and the company’s other filings with the Securities and Exchange Commission (SEC) available at the SEC’s Internet site (www.sec.gov).
Media: Julie Cunningham (617) 519-6264 Elizabeth Sell (484) 689-9978 Investors: Peter Dannenbaum (732) 594-1579 Ayn Wisler (917) 691-6218
临床3期临床结果AHA会议
2025-09-01
Cemdisiran monotherapy, dosed subcutaneously every three months, met the primary and key secondary endpoints, showing a 2.3-point placebo-adjusted improvement in Myasthenia Gravis Activities of Daily Living (MG-ADL) total score
U.S. regulatory submission for cemdisiran monotherapy is planned for the first quarter of 2026, pending discussions with the FDA
TARRYTOWN, N.Y. , Aug. 26, 2025 (GLOBE NEWSWIRE) -- Regeneron Pharmaceuticals, Inc. (NASDAQ: REGN) today announced that the primary and key secondary endpoints were met in the Phase 3 NIMBLE trial assessing investigational cemdisiran monotherapy in adults with generalized myasthenia gravis (gMG). Cemdisiran is an siRNA that reduces circulating levels of complement factor 5 (C5) and, as monotherapy in this trial, was associated with an average of 74% inhibition of complement activity. The trial also assessed a combination of cemdisiran and pozelimab, a C5 antibody; this combination (“cemdi-poze”), which resulted in nearly 99% inhibition of complement activity, also met the primary and key secondary endpoints, though cemdisiran monotherapy was numerically better across these endpoints.
“Our pipeline approach to treating complement-mediated diseases allows us to tailor treatment to the underlying disease biology,” said L. Andres Sirulnik , M.D., Ph.D., Senior Vice President and Hematology Clinical Development Unit Head at Regeneron . “The results of the NIMBLE trial confirm that, in myasthenia gravis, robust efficacy can be achieved without complete complement blockade, whereas in other diseases such as paroxysmal nocturnal hemoglobinuria (PNH), complete inhibition is likely to be necessary. We have previously released data from the lead-in portion of our PNH Phase 3 trial, supporting the potential for the cemdi-poze combination to deliver best-in-class efficacy in PNH. We are also investigating systemic administration of both cemdisiran monotherapy and the cemdi-poze combination in our Phase 3 program for geographic atrophy secondary to age-related macular degeneration.”
“The NIMBLE trial results underscore the potential for cemdisiran to offer a best-in-class profile for those suffering with myasthenia gravis, providing for robust efficacy with a convenient quarterly subcutaneous administration,” said George D. Yancopoulos , M.D., Ph.D., Board co-Chair, President and Chief Scientific Officer at Regeneron . “The potential for best-in-class efficacy with less than complete complement blockade with cemdisiran monotherapy may also provide for a more favorable safety profile. These exciting results highlight the transformative potential of our siRNA and genetic medicines pipeline to deliver paradigm-changing therapies for patients.”
The NIMBLE trial evaluated adults with symptomatic gMG who have antibodies to the acetylcholine receptor (anti-AChR) and may be receiving standard of care immunosuppressants based on the investigator’s discretion. Patients were randomized to receive subcutaneous administrations of: cemdisiran (600 mg) every 12 weeks, cemdi-poze (cemdisiran 200 mg and pozelimab 200 mg) every 4 weeks, or placebo every 4 weeks. The primary endpoint assessed total score changes from baseline to week 24 in the Myasthenia Gravis Activities of Daily Living (MG-ADL) total score, a patient-reported questionnaire that measures daily functions impacted by gMG, such as talking, eating, breathing, vision and mobility. The key secondary endpoint assessed total score changes from baseline in the Quantitative Myasthenia Gravis (QMG) total score, a physician-administered assessment evaluating vision, speaking/swallowing, breathing and limb function.
Historical clinical trial data report that currently approved C5 inhibitor therapies have shown a placebo-adjusted treatment difference in MG-ADL total scores ranging from -1.6 to -2.1 at 12 to 26 weeks.
Both cemdisiran and cemdi-poze demonstrated improvements in activities of daily functioning at week 24, with cemdisiran showing numerically better results across all gMG-specific outcomes. In the MG-ADL and QMG, greater reductions in total scores indicate greater improvement in disease symptoms and better treatment effect.
†Means and relative risks were adjusted per the amount immunosuppressant treatment and the Myasthenia Gravis Foundation of America Clinical Classification determined at screening. Means were also adjusted for baseline MG-ADL or QMG score.
There were no meningococcal infections in any patient. There were no treatment discontinuations due to adverse events through week 24 in the cemdisiran arm.
Across all arms, treatment-emergent adverse events (TEAEs) occurred in 69% of patients treated with cemdisiran, 81% with cemdi-poze, and 77% with placebo. Serious TEAEs occurred in 3% of patients treated with cemdisiran, 9% with cemdi-poze and 14% with placebo. The most common TEAEs observed in ≥5% of patients receiving cemdisiran, cemdi-poze or placebo were: worsening of MG (1%, 5%, 17%), upper respiratory tract infection (12%, 8%, 11%), urinary tract infection (5%, 6%, 3%), nasopharyngitis (5%, 3%, 4%), headache (5%, 11%, 10%), rash (5%, 3%, 1%), injection site reaction (4%, 8%, 1%), diarrhea (3%, 14%, 7%), arthralgia (1%, 6%, 1%), pain in extremity (1%, 5%, 1%), cough (1%, 5%, 1%), and pruritus (0%, 5%, 0%). There were no deaths during the 24-week placebo-controlled portion of the trial. During the extension period, one death due to pneumonia occurred in the cemdisiran arm, and one death due to septic shock occurred in the combination arm; both deaths occurred in patients who were on concomitant immuno-suppressive therapies.
Detailed results from the NIMBLE trial will be presented at an upcoming medical meeting. The U.S. regulatory application for cemdisiran is planned for the first quarter of 2026, pending discussions with the FDA.
The potential use of cemdisiran and/or pozelimab for the treatment of gMG is investigational and has not been approved by any regulatory authority. In the U.S. , pozelimab monotherapy is approved as Veopoz® (pozelimab-bbfg) for adult and pediatric patients 1 year of age and older with CHAPLE disease, also known as CD55-deficient protein-losing enteropathy, which includes a Boxed Warning for life-threatening and fatal meningococcal infections.
About Myasthenia Gravis (MG)MG is a rare and chronic autoimmune disease where abnormal antibodies activate the complement system including C5, disrupting communication between nerves and muscles that results in debilitating and potentially life-threatening muscle weakness. In the U.S. , the disease impacts approximately 85,000 people. Initial manifestations are usually ocular, but approximately 85% of MG patients experience additional advancements to the disease manifestations, which is known as generalized myasthenia gravis (gMG). For these patients, the disease affects muscles throughout the body, resulting in extreme fatigue and difficulties with facial expression, speech, swallowing and mobility. Treatment-related challenges – which include frequent hospital visits, inconsistent symptom control, and lack of durable treatment effects – can further affect quality of life and long-term disease management.
About the Complement Factor 5 (C5) Clinical ProgramNIMBLE is a randomized, double-blind, placebo-controlled trial evaluating cemdisiran and cemdi-poze in patients with gMG who have antibodies for AChR. The primary endpoint assessed changes in the MG-ADL total score from baseline to week 24. The MG-ADL scale is an eight-question patient-reported tool that measures how gMG affects aspects of daily life and provides a total score ranging from 0 to 24. The key secondary endpoint was the change from baseline in QMG total score at week 24. The QMG is a physician-administered 13-item standardized assessment evaluating muscle function that provides a total score ranging from 0 to 39. In both MG-ADL and QMG, a higher total score indicates greater disease severity, and a larger reduction in total score indicates greater improvement in disease symptoms and better treatment effect.
Cemdisiran and pozelimab are also being evaluated in separate Phase 3 trials as both monotherapy and combination therapy for additional complement-mediated disorders, including PNH and geographic atrophy secondary to age-related macular degeneration. For more information, visit the Regeneron clinical trials website, or contact clinicaltrials@regeneron.com or +1 844-734-6643.
Cemdisiran as a monotherapy and in combination with pozelimab was being developed under an initial agreement with Alnylam Pharmaceuticals, Inc. In June 2024 , Regeneron and Alnylam entered into an amended and restated C5 License Agreement, which granted Regeneron a worldwide license to cemdisiran as a monotherapy in addition to a license to cemdisiran in combination with C5 antibodies. Regeneron is solely responsible for development, manufacturing, and commercialization of cemdisiran as a monotherapy and in combination with C5 antibodies. For cemdisiran as a monotherapy, Alnylam is entitled to receive certain regulatory milestone payments as well as tiered, double-digit royalties (up to 15%) on calendar-year net sales. If cemdisiran is used as part of a combination product, Alnylam is entitled to receive a flat, low double-digit royalty on calendar-year net sales as well as commercial milestones of up to $325.0 million .
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about VEOPOZ?VEOPOZ is a medicine that affects your immune system and can lower the ability of your immune system to fight infections.
VEOPOZ increases your chance of getting serious and life-threatening meningococcal infections that may quickly become life-threatening and cause death if not recognized and treated early.
headache with nausea or vomiting headache with a stiff neck or stiff back fever and a rash muscle aches with flu-like symptoms headache and fever fever confusion eyes sensitive to light
Your healthcare provider will give you a Patient Safety Card about the symptoms of meningococcal, or other infection. Carry it with you at all times during treatment and for 3 months after your last VEOPOZ dose. Your risk of meningococcal infection may continue for several weeks after your last dose of VEOPOZ. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly.
VEOPOZ may also increase the risk of other types of serious bacterial infections.
People who take VEOPOZ may have an increased risk of getting infections caused by Streptococcus pneumoniae and Haemophilus influenzae. Certain people may also have an increased risk of bacterial infection including gonorrhea infection. Talk to your healthcare provider to find out if you are at risk of gonorrhea infection, about gonorrhea prevention, and regular testing.
Call your healthcare provider right away if you have any new signs or symptoms of infection.
Do not receive VEOPOZ if you have a meningococcal infection.
Before you receive VEOPOZ, tell your healthcare provider about all of your medical conditions, including if you: have an infection or fever, are pregnant or plan to become pregnant, and are breastfeeding or plan to breastfeed. It is not known if VEOPOZ will harm your unborn baby or if it passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with VEOPOZ.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. It is important that you have all recommended vaccinations before you start VEOPOZ, receive antibiotics if you start VEOPOZ within 2 weeks of receiving meningococcal vaccination, and stay up to date with all recommended vaccinations during treatment with VEOPOZ.
VEOPOZ and other medicines may affect each other, causing side effects. VEOPOZ may affect the way other medicines work, and other medicines may affect how VEOPOZ works.Especially tell your healthcare provider if you take Intravenous Immunoglobulin (IVIg).Know the medicines you take and the vaccines you receive. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
What are the possible side effects of VEOPOZ?VEOPOZ can cause serious side effects including allergic (hypersensitivity) reactions including infusion-related reactions, which may happen during your treatment. Tell your healthcare provider right away if you develop any of these symptoms or any other symptom during your VEOPOZ treatment that may mean you are having a serious allergic reaction: chest pain, trouble breathing or shortness of breath, swelling of your face, tongue, or throat, and feel faint or pass out.
The most common side effects of VEOPOZ are upper respiratory tract infection, fracture, raised, red patches of skin that are often very itchy (hives), and hair loss (alopecia).
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of VEOPOZ. Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see the full Prescribing Information, including Boxed WARNING, and Medication Guide for VEOPOZ.
About Regeneron 's VelocImmune® Technology Regeneron 's VelocImmune technology utilizes a proprietary genetically engineered mouse platform endowed with a genetically humanized immune system to produce optimized fully human antibodies. When Regeneron 's co-Founder, President and Chief Scientific Officer George D. Yancopoulos was a graduate student with his mentor Frederick W. Alt in 1985, they were the first to envision making such a genetically humanized mouse, and Regeneron has spent decades inventing and developing VelocImmune and related VelociSuite® technologies. Dr. Yancopoulos and his team have used VelocImmune technology to create a substantial proportion of all original, FDA-approved or authorized fully human monoclonal antibodies. This includes REGEN-COV® (casirivimab and imdevimab), Dupixent® (dupilumab), Libtayo® (cemiplimab-rwlc), Praluent® (alirocumab), Kevzara® (sarilumab), Evkeeza® (evinacumab-dgnb), Inmazeb® (atoltivimab, maftivimab and odesivimab-ebgn) and Veopoz® (pozelimab).
About Regeneron Regeneron (NASDAQ: REGN) is a leading biotechnology company that invents, develops and commercializes life-transforming medicines for people with serious diseases. Founded and led by physician-scientists, our unique ability to repeatedly and consistently translate science into medicine has led to numerous approved treatments and product candidates in development, most of which were homegrown in our laboratories. Our medicines and pipeline are designed to help patients with eye diseases, allergic and inflammatory diseases, cancer, cardiovascular and metabolic diseases, neurological diseases, hematologic conditions, infectious diseases, and rare diseases.
Regeneron pushes the boundaries of scientific discovery and accelerates drug development using our proprietary technologies, such as VelociSuite, which produces optimized fully human antibodies and new classes of bispecific antibodies. We are shaping the next frontier of medicine with data-powered insights from the Regeneron Genetics Center® and pioneering genetic medicine platforms, enabling us to identify innovative targets and complementary approaches to potentially treat or cure diseases.
For more information, please visit www.Regeneron.com or follow Regeneron on LinkedIn, Instagram, Facebook or X.
Forward-Looking Statements and Use of Digital Media This press release includes forward-looking statements that involve risks and uncertainties relating to future events and the future performance of Regeneron Pharmaceuticals, Inc. (“Regeneron” or the “Company”), and actual events or results may differ materially from these forward-looking statements. Words such as “anticipate,” “expect,” “intend,” “plan,” “believe,” “seek,” “estimate,” variations of such words, and similar expressions are intended to identify such forward-looking statements, although not all forward-looking statements contain these identifying words. These statements concern, and these risks and uncertainties include, among others, the nature, timing, and possible success and therapeutic applications of products marketed or otherwise commercialized by Regeneron and/or its collaborators or licensees (collectively, “Regeneron’s Products”) and product candidates being developed by Regeneron and/or its collaborators or licensees (collectively, “Regeneron’s Product Candidates”) and research and clinical programs now underway or planned, including without limitation cemdisiran (an investigational siRNA therapeutic targeting C5) as a monotherapy and in combination with pozelimab (a fully human monoclonal antibody designed to block the activity of C5) (collectively, “Regeneron’s C5 Product Candidates”); the likelihood, timing, and scope of possible regulatory approval and commercial launch of Regeneron’s Product Candidates and new indications for Regeneron’s Products, such as any of Regeneron’s C5 Product Candidates for the treatment of generalized myasthenia gravis as discussed in this press release as well as other complement-mediated conditions (including paroxysmal nocturnal hemoglobinuria and/or geographic atrophy); uncertainty of the utilization, market acceptance, and commercial success of Regeneron’s Products and Regeneron’s Product Candidates and the impact of studies (whether conducted by Regeneron or others and whether mandated or voluntary), including the studies discussed or referenced in this press release, on any of the foregoing or any potential regulatory approval of Regeneron’s Products and Regeneron’s Product Candidates (such as Regeneron’s C5 Product Candidates); the ability of Regeneron’s collaborators, licensees, suppliers, or other third parties (as applicable) to perform manufacturing, filling, finishing, packaging, labeling, distribution, and other steps related to Regeneron’s Products and Regeneron’s Product Candidates; the ability of Regeneron to manage supply chains for multiple products and product candidates and risks associated with tariffs and other trade restrictions; safety issues resulting from the administration of Regeneron’s Products and Regeneron’s Product Candidates (such as Regeneron’s C5 Product Candidates) in patients, including serious complications or side effects in connection with the use of Regeneron’s Products and Regeneron’s Product Candidates in clinical trials; determinations by regulatory and administrative governmental authorities which may delay or restrict Regeneron’s ability to continue to develop or commercialize Regeneron’s Products and Regeneron’s Product Candidates; ongoing regulatory obligations and oversight impacting Regeneron’s Products, research and clinical programs, and business, including those relating to patient privacy; the availability and extent of reimbursement or copay assistance for Regeneron’s Products from third-party payors and other third parties, including private payor healthcare and insurance programs, health maintenance organizations, pharmacy benefit management companies, and government programs such as Medicare and Medicaid; coverage and reimbursement determinations by such payors and other third parties and new policies and procedures adopted by such payors and other third parties; changes in laws, regulations, and policies affecting the healthcare industry; competing drugs and product candidates that may be superior to, or more cost effective than, Regeneron’s Products and Regeneron’s Product Candidates (including biosimilar versions of Regeneron’s Products); the extent to which the results from the research and development programs conducted by Regeneron and/or its collaborators or licensees may be replicated in other studies and/or lead to advancement of product candidates to clinical trials, therapeutic applications, or regulatory approval; unanticipated expenses; the costs of developing, producing, and selling products; the ability of Regeneron to meet any of its financial projections or guidance and changes to the assumptions underlying those projections or guidance; the potential for any license, collaboration, or supply agreement, including Regeneron’s agreements with Sanofi and Bayer (or their respective affiliated companies, as applicable) and the agreement with Alnylam Pharmaceuticals, Inc. referenced in this press release, to be cancelled or terminated; the impact of public health outbreaks, epidemics, or pandemics on Regeneron 's business; and risks associated with litigation and other proceedings and government investigations relating to the Company and/or its operations (including the pending civil proceedings initiated or joined by the U.S. Department of Justice and the U.S. Attorney's Office for the District of Massachusetts ), risks associated with intellectual property of other parties and pending or future litigation relating thereto (including without limitation the patent litigation and other related proceedings relating to EYLEA® (aflibercept) Injection), the ultimate outcome of any such proceedings and investigations, and the impact any of the foregoing may have on Regeneron’s business, prospects, operating results, and financial condition. A more complete description of these and other material risks can be found in Regeneron’s filings with the U.S. Securities and Exchange Commission , including its Form 10-K for the year ended December 31, 2024 and its Form 10-Q for the quarterly period ended June 30, 2025 . Any forward-looking statements are made based on management’s current beliefs and judgment, and the reader is cautioned not to rely on any forward-looking statements made by Regeneron . Regeneron does not undertake any obligation to update (publicly or otherwise) any forward-looking statement, including without limitation any financial projection or guidance, whether as a result of new information, future events, or otherwise.
Regeneron uses its media and investor relations website and social media outlets to publish important information about the Company, including information that may be deemed material to investors. Financial and other information about Regeneron is routinely posted and is accessible on Regeneron 's media and investor relations website (https://investor.regeneron.com) and its LinkedIn page (https://www.linkedin.com/company/regeneron-pharmaceuticals).
Source: Regeneron Pharmaceuticals, Inc.
临床结果临床3期引进/卖出上市批准
2025-08-27
Treatment with Verzenio plus endocrine therapy demonstrated a statistically significant and clinically meaningful improvement in overall survival compared to endocrine therapy alone
In the seven-year landmark analysis of monarchE, treatment with Verzenio also resulted in sustained invasive disease-free survival and distant relapse-free survival benefit
Results reinforce two years of Verzenio plus endocrine therapy as the standard of care in HR+, HER2-, node-positive, early breast cancer at a high risk of recurrence
INDIANAPOLIS, Aug. 27, 2025 /PRNewswire/ -- Eli Lilly and Company (NYSE: LLY) today announced positive topline results from the primary overall survival (OS) analysis of the Phase 3 monarchE trial. Treatment with two years of Verzenio plus endocrine therapy (ET) demonstrated a statistically significant and clinically meaningful improvement in OS compared to ET alone in patients with hormone receptor positive (HR+), HER2-, node-positive, high-risk early breast cancer.
The seven-year landmark analysis also demonstrated sustained benefit in invasive disease-free survival (IDFS) and distant relapse-free survival (DRFS), reinforcing the consistency and durability of treatment effect across endpoints.
"Preventing disease relapse and helping patients live longer is the ultimate goal and a high bar in the adjuvant setting. Achieving a statistically significant OS benefit with just two years of Verzenio therapy reinforces its differentiated profile in high-risk HR+, HER2- early breast cancer," said Jacob Van Naarden, executive vice president and president of Lilly Oncology. "These data validate Verzenio as the standard-of-care for patients with node-positive, high-risk disease and increase the urgency to ensure all eligible patients are treated."
With all patients having completed or discontinued the two-year course of Verzenio, the overall safety profile of Verzenio was unchanged and consistent with previous reports.
Detailed results will be presented at a future medical meeting, submitted for publication in a peer-reviewed journal and discussed with regulatory bodies.
About the monarchE Study
monarchE was a global, randomized, open-label, two cohort, multicenter Phase 3 clinical trial that enrolled 5,637 adults with HR+, HER2-, node-positive EBC at high risk of recurrence. The study enrolled patients across more than 600 sites in 38 countries and is the only adjuvant study designed to investigate a CDK4/6 inhibitor specifically in a node-positive, high risk EBC population. To be enrolled in Cohort 1 (n=5,120), which is the FDA-approved population, patients had to have 4+ positive nodes or 1-3 positive nodes and at least one of the following: tumors that were ≥5 cm or Grade 3. Patients enrolled in Cohort 2 could not have met the eligibility criteria for Cohort 1. To be enrolled in Cohort 2 (n=517), patients had to have 1-3 positive nodes and Ki-67 score ≥20%. Patients in each cohort were randomized 1:1 to receive either Verzenio 150 mg twice daily plus standard-of-care adjuvant ET (Cohort 1, n=2,555; Cohort 2, n=253) or standard-of-care adjuvant ET alone (Cohort 1, n=2,565; Cohort 2, n=264) for 2 years. ET continued for at least 5 years if deemed medically appropriate. The primary endpoint was IDFS. Consistent with expert guidelines, IDFS was defined as the length of time before breast cancer comes back, any new cancer develops, or death. OS was a key secondary endpoint in monarchE. The OS analysis plan was amended after the primary analysis of IDFS, following consultation with regulators, to increase the number of required OS events from 390 to 650 to ensure a minimum follow-up of at least 5 years and enable a more mature survival dataset.1,2
About Early Breast Cancer and Risk of Recurrence
It is estimated that 90% of all breast cancers are detected at an early stage.3 Approximately 70% of all breast cancer cases are the HR+, HER2- subtype.4 Although the prognosis for HR+, HER2- EBC is generally favorable, high risk patients are three times more likely than those with low risk characteristics to experience recurrence – with the majority being incurable metastatic disease.5 These patients have an increased risk of recurrence during the first two years of endocrine therapy.
Factors associated with high risk of recurrence in HR+, HER2- early breast cancer include: positive nodal status, the number of positive nodes, large tumor size (≥5 cm), and high tumor grade (Grade 3). Node-positive means that cancer cells from the tumor in the breast have been found in the lymph nodes near the breast. Although breast cancer is removed through surgery, the presence of cancer cells in the lymph nodes signifies that there is a higher chance of developing recurrence and distant metastatic disease.
About Breast Cancer
Breast cancer is the second most commonly diagnosed cancer worldwide (following lung cancer), according to GLOBOCAN. The estimated 2.3 million new cases indicate that close to 1 in every 4 cancers diagnosed in 2022 is breast cancer. With approximately 666,000 deaths in 2022, breast cancer is the fourth-leading cause of cancer death worldwide.6 In the U.S., it is estimated that there will be more than 310,000 new cases of breast cancer diagnosed in 2024. Breast cancer is the second leading cause of cancer death in women in the U.S.7
About Verzenio® (abemaciclib)
Verzenio® (abemaciclib) is approved to treat people with certain HR+, HER2- breast cancers in the adjuvant and advanced or metastatic setting. Verzenio is the first CDK4/6 inhibitor approved to treat node-positive, high risk early breast cancer (EBC) patients.8 For HR+, HER2- breast cancer, The National Comprehensive Cancer Network® (NCCN®) recommends consideration of two years of abemaciclib (Verzenio) added to endocrine therapy as a Category 1 treatment option in the adjuvant setting.9 NCCN® also includes Verzenio plus endocrine therapy as a preferred treatment option for HR+, HER2- metastatic breast cancer.9
The collective results of Lilly's clinical development program continue to differentiate Verzenio as a CDK4/6 inhibitor. In high risk EBC, Verzenio has shown a persistent and deepening benefit beyond the two-year treatment period in the monarchE trial, an adjuvant study designed specifically to investigate a CDK4/6 inhibitor in a node-positive, high risk EBC population. 10 In metastatic breast cancer, Verzenio has demonstrated statistically significant OS in the Phase 3 MONARCH 2 study.11 Verzenio has shown a consistent and generally manageable safety profile across clinical trials.
Verzenio is an oral tablet taken twice daily and available in strengths of 50 mg, 100 mg, 150 mg, and 200 mg. Discovered and developed by Lilly researchers, Verzenio was first approved in 2017 and is currently authorized for use in more than 90 counties around the world. For full details on indicated uses of Verzenio in HR+, HER2- breast cancer, please see full Prescribing Information, available at .
INDICATIONS FOR VERZENIO®
VERZENIO® is a kinase inhibitor indicated:
in combination with endocrine therapy (tamoxifen or an aromatase inhibitor) for the adjuvant treatment of adult patients with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative, node-positive, early breast cancer at high risk of recurrence.
in combination with an aromatase inhibitor as initial endocrine-based therapy for the treatment of adult patients with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced or metastatic breast cancer.
in combination with fulvestrant for the treatment of adult patients with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced or metastatic breast cancer with disease progression following endocrine therapy.
as monotherapy for the treatment of adult patients with HR-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy and prior chemotherapy in the metastatic setting.
IMPORTANT SAFETY INFORMATION FOR VERZENIO (abemaciclib)
Severe
diarrhea associated with dehydration and infection occurred in patients treated with Verzenio. Across four clinical trials in 3691 patients, diarrhea occurred in 81 to 90% of patients who received Verzenio. Grade 3 diarrhea occurred in 8 to 20% of patients receiving Verzenio. Most patients experienced diarrhea during the first month of Verzenio treatment. The median time to onset of the first diarrhea event ranged from 6 to 8 days; and the median duration of Grade 2 and Grade 3 diarrhea ranged from 6 to 11 days and 5 to 8 days, respectively. Across trials, 19 to 26% of patients with diarrhea required a Verzenio dose interruption and 13 to 23% required a dose reduction.
Instruct patients to start antidiarrheal therapy, such as loperamide, at the first sign of loose stools, increase oral fluids, and notify their healthcare provider for further instructions and appropriate follow-up. For Grade 3 or 4 diarrhea, or diarrhea that requires hospitalization, discontinue Verzenio until toxicity resolves to ≤Grade 1, and then resume Verzenio at the next lower dose.
Neutropenia, including febrile neutropenia and fatal neutropenic sepsis, occurred in patients treated with Verzenio. Across four clinical trials in 3691 patients, neutropenia occurred in 37 to 46% of patients receiving Verzenio. A Grade ≥3 decrease in neutrophil count (based on laboratory findings) occurred in 19 to 32% of patients receiving Verzenio. Across trials, the median time to first episode of Grade ≥3 neutropenia ranged from 29 to 33 days, and the median duration of Grade ≥3 neutropenia ranged from 11 to 16 days. Febrile neutropenia has been reported in <1% of patients exposed to Verzenio across trials. Two deaths due to neutropenic sepsis were observed in MONARCH 2. Inform patients to promptly report any episodes of fever to their healthcare provider.
Monitor complete blood counts prior to the start of Verzenio therapy, every 2 weeks for the first 2 months, monthly for the next 2 months, and as clinically indicated. Dose interruption, dose reduction, or delay in starting treatment cycles is recommended for patients who develop Grade 3 or 4 neutropenia.
Severe, life-threatening, or
fatal interstitial lung disease (ILD) or pneumonitis can occur in patients treated with Verzenio and other CDK4/6 inhibitors. In Verzenio-treated patients in EBC (monarchE), 3% of patients experienced ILD or pneumonitis of any grade: 0.4% were Grade 3 or 4 and there was one fatality (0.1%). In Verzenio-treated patients in MBC (MONARCH 1, MONARCH 2, MONARCH 3), 3.3% of Verzenio-treated patients had ILD or pneumonitis of any grade: 0.6% had Grade 3 or 4, and 0.4% had fatal outcomes. Additional cases of ILD or pneumonitis have been observed in the postmarketing setting, with fatalities reported.
Monitor patients for pulmonary symptoms indicative of ILD or pneumonitis. Symptoms may include hypoxia, cough, dyspnea, or interstitial infiltrates on radiologic exams. Infectious, neoplastic, and other causes for such symptoms should be excluded by means of appropriate investigations. Dose interruption or dose reduction is recommended in patients who develop persistent or recurrent Grade 2 ILD or pneumonitis. Permanently discontinue Verzenio in all patients with Grade 3 or 4 ILD or pneumonitis.
Grade
≥
3 increases in alanine aminotransferase (ALT) (2 to 6%) and
aspartate aminotransferase (AST) (2 to 3%) were reported in patients receiving Verzenio. Across three clinical trials in 3559 patients (monarchE, MONARCH 2, MONARCH 3), the median time to onset of Grade ≥3 ALT increases ranged from 57 to 87 days and the median time to resolution to Grade <3 was 13 to 14 days. The median time to onset of Grade ≥3 AST increases ranged from 71 to 185 days and the median time to resolution to Grade <3 ranged from 11 to 15 days.
Monitor liver function tests (LFTs) prior to the start of Verzenio therapy, every 2 weeks for the first 2 months, monthly for the next 2 months, and as clinically indicated. Dose interruption, dose reduction, dose discontinuation, or delay in starting treatment cycles is recommended for patients who develop persistent or recurrent Grade 2, or any Grade 3 or 4 hepatic transaminase elevation.
Venous thromboembolic events (VTE) were reported in 2 to 5% of patients across three clinical trials in 3559 patients treated with Verzenio (monarchE, MONARCH 2, MONARCH 3). VTE included deep vein thrombosis, pulmonary embolism, pelvic venous thrombosis, cerebral venous sinus thrombosis, subclavian and axillary vein thrombosis, and inferior vena cava thrombosis. In clinical trials, deaths due to VTE have been reported in patients treated with Verzenio.
Verzenio has not been studied in patients with early breast cancer who had a history of VTE. Monitor patients for signs and symptoms of venous thrombosis and pulmonary embolism and treat as medically appropriate. Dose interruption is recommended for EBC patients with any grade VTE and for MBC patients with a Grade 3 or 4 VTE.
Verzenio can cause
fetal harm when administered to a pregnant woman, based on findings from animal studies and the mechanism of action. In animal reproduction studies, administration of abemaciclib to pregnant rats during the period of organogenesis caused teratogenicity and decreased fetal weight at maternal exposures that were similar to the human clinical exposure based on area under the curve (AUC) at the maximum recommended human dose. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with Verzenio and for 3 weeks after the last dose. Based on findings in animals, Verzenio may impair fertility in males of reproductive potential. There are no data on the presence of Verzenio in human milk or its effects on the breastfed child or on milk production. Advise lactating women not to breastfeed during Verzenio treatment and for at least 3 weeks after the last dose because of the potential for serious adverse reactions in breastfed infants.
The most
common adverse reactions (all grades,
≥
10%) observed in
monarchE for
Verzenio plus tamoxifen or an aromatase inhibitor vs tamoxifen or an aromatase inhibitor, with a difference between arms of
≥
2%, were diarrhea (84% vs 9%), infections (51% vs 39%), neutropenia (46% vs 6%), fatigue (41% vs 18%), leukopenia (38% vs 7%), nausea (30% vs 9%), anemia (24% vs 4%), headache (20% vs 15%), vomiting (18% vs 4.6%), stomatitis (14% vs 5%), lymphopenia (14% vs 3%), thrombocytopenia (13% vs 2%), decreased appetite (12% vs 2.4%), ALT increased (12% vs 6%), AST increased (12% vs 5%), dizziness (11% vs 7%), rash (11% vs 4.5%), and alopecia (11% vs 2.7 %).
The
most frequently reported
≥
5% Grade 3 or 4 adverse reaction that occurred in the Verzenio arm vs the tamoxifen or an aromatase inhibitor arm of monarchE were neutropenia (19.6% vs 1%), leukopenia (11% vs <1%), diarrhea (8% vs 0.2%), and lymphopenia (5% vs <1%).
Lab abnormalities (all grades; Grade 3 or 4) for
monarchE in
≥
10% for Verzenio plus tamoxifen or an aromatase inhibitor with a difference between arms of
≥
2% were increased serum creatinine (99% vs 91%; .5% vs <.1%), decreased white blood cells (89% vs 28%; 19.1% vs 1.1%), decreased neutrophil count (84% vs 23%; 18.7% vs 1.9%), anemia (68% vs 17%; 1% vs .1%), decreased lymphocyte count (59% vs 24%; 13.2 % vs 2.5%), decreased platelet count (37% vs 10%; .9% vs .2%), increased ALT (37% vs 24%; 2.6% vs 1.2%), increased AST (31% vs 18%; 1.6% vs .9%), and hypokalemia (11% vs 3.8%; 1.3% vs 0.2%).
The
most common adverse reactions (all grades,
≥
10%) observed in
MONARCH 3 for Verzenio plus anastrozole or letrozole vs anastrozole or letrozole, with a difference between arms of
≥
2%, were diarrhea (81% vs 30%), fatigue (40% vs 32%), neutropenia (41% vs 2%), infections (39% vs 29%), nausea (39% vs 20%), abdominal pain (29% vs 12%), vomiting (28% vs 12%), anemia (28% vs 5%), alopecia (27% vs 11%), decreased appetite (24% vs 9%), leukopenia (21% vs 2%), creatinine increased (19% vs 4%), constipation (16% vs 12%), ALT increased (16% vs 7%), AST increased (15% vs 7%), rash (14% vs 5%), pruritus (13% vs 9%), cough (13% vs 9%), dyspnea (12% vs 6%), dizziness (11% vs 9%), weight decreased (10% vs 3.1%), influenza-like illness (10% vs 8%), and thrombocytopenia (10% vs 2%).
The
most frequently reported
≥
5% Grade 3 or 4 adverse reactions that occurred in the Verzenio arm vs the placebo arm of
MONARCH 3 were neutropenia (22% vs 1%), diarrhea (9% vs 1.2%), leukopenia (7% vs <1%)), increased ALT (6% vs 2%), and anemia (6% vs 1%).
Lab abnormalities (all grades; Grade 3 or 4) for
MONARCH 3 in
≥
10% for Verzenio plus anastrozole or letrozole with a difference between arms of
≥
2% were increased serum creatinine (98% vs 84%; 2.2% vs 0%), decreased white blood cells (82% vs 27%; 13% vs 0.6%), anemia (82% vs 28%; 1.6% vs 0%), decreased neutrophil count (80% vs 21%; 21.9% vs 2.6%), decreased lymphocyte count (53% vs 26%; 7.6% vs 1.9%), decreased platelet count (36% vs 12%; 1.9% vs 0.6%), increased ALT (48% vs 25%; 6.6% vs 1.9%), and increased AST (37% vs 23%; 3.8% vs 0.6%).
The
most common adverse reactions (all grades,
≥
10%) observed in
MONARCH 2 for Verzenio plus fulvestrant vs fulvestrant, with a difference between arms of
≥
2%, were diarrhea (86% vs 25%), neutropenia (46% vs 4%), fatigue (46% vs 32%), nausea (45% vs 23%), infections (43% vs 25%), abdominal pain (35% vs 16%), anemia (29% vs 4%), leukopenia (28% vs 2%), decreased appetite (27% vs 12%), vomiting (26% vs 10%), headache (20% vs 15%), dysgeusia (18% vs 2.7%), thrombocytopenia (16% vs 3%), alopecia (16% vs 1.8%), stomatitis (15% vs 10%), ALT increased (13% vs 5%), pruritus (13% vs 6%), cough (13% vs 11%), dizziness (12% vs 6%), AST increased (12% vs 7%), peripheral edema (12% vs 7%), creatinine increased (12% vs <1%), rash (11% vs 4.5%), pyrexia (11% vs 6%), and weight decreased (10% vs 2.2%).
The
most frequently reported
≥
5% Grade 3 or 4 adverse reactions that occurred in the Verzenio arm vs the placebo arm of
MONARCH 2 were neutropenia (25% vs 1%), diarrhea (13% vs 0.4%), leukopenia (9% vs 0%), anemia (7% vs 1%), and infections (5.7% vs 3.5%).
Lab abnormalities (all grades; Grade 3 or 4) for
MONARCH 2 in
≥
10% for Verzenio plus fulvestrant with a difference between arms of
≥
2% were increased serum creatinine (98% vs 74%; 1.2% vs 0%), decreased white blood cells (90% vs 33%; 23.7% vs .9%), decreased neutrophil count (87% vs 30%; 32.5% vs 4.2%), anemia (84% vs 34%; 2.6% vs .5%), decreased lymphocyte count (63% vs 32%; 12.2% vs 1.8%), decreased platelet count (53% vs 15%; 2.1% vs 0%), increased ALT (41% vs 32%; 4.6% vs 1.4%), and increased AST (37% vs 25%; 3.9% vs 4.2%).
The
most common adverse reactions (all grades,
≥
10%) observed in
MONARCH 1 with Verzenio were diarrhea (90%), fatigue (65%), nausea (64%), decreased appetite (45%), abdominal pain (39%), neutropenia (37%), vomiting (35%), infections (31%), anemia (25%), thrombocytopenia (20%), headache (20%), cough (19%), constipation (17%), leukopenia (17%), arthralgia (15%), dry mouth (14%), weight decreased (14%), stomatitis (14%), creatinine increased (13%), alopecia (12%), dysgeusia (12%), pyrexia (11%), dizziness (11%), and dehydration (10%).
The
most frequently reported
≥
5% Grade 3 or 4 adverse reactions from
MONARCH 1 with Verzenio were diarrhea (20%), neutropenia (24%), fatigue (13%), and leukopenia (5%).
Lab abnormalities (all grades; Grade 3 or 4) for MONARCH 1 with Verzenio were increased serum creatinine (99%; .8%), decreased white blood cells (91%; 28%), decreased neutrophil count (88%; 26.6%), anemia (69%; 0%), decreased lymphocyte count (42%; 13.8%), decreased platelet count (41%; 2.3%), increased ALT (31%; 3.1%), and increased AST (30%; 3.8%).
Strong and moderate CYP3A inhibitors increased the exposure of abemaciclib plus its active metabolites to a clinically meaningful extent and may lead to increased toxicity. Avoid concomitant use of ketoconazole. Ketoconazole is predicted to increase the AUC of abemaciclib by up to 16-fold. In patients with recommended starting doses of 200 mg twice daily or 150 mg twice daily, reduce the Verzenio dose to 100 mg twice daily with concomitant use of strong CYP3A inhibitors other than ketoconazole. In patients who have had a dose reduction to 100 mg twice daily due to adverse reactions, further reduce the Verzenio dose to 50 mg twice daily with concomitant use of strong CYP3A inhibitors. If a patient taking Verzenio discontinues a strong CYP3A inhibitor, increase the Verzenio dose (after 3 to 5 half-lives of the inhibitor) to the dose that was used before starting the inhibitor. With concomitant use of moderate CYP3A inhibitors, monitor for adverse reactions and consider reducing the Verzenio dose in 50 mg decrements. Patients should avoid grapefruit products.
Avoid concomitant use of strong or moderate CYP3A inducers and consider alternative agents. Coadministration of strong or moderate CYP3A inducers decreased the plasma concentrations of abemaciclib plus its active metabolites and may lead to reduced activity.
With severe hepatic impairment (Child-Pugh C), reduce the Verzenio dosing frequency to once daily. The pharmacokinetics of Verzenio in patients with
severe renal impairment (CLcr <30 mL/min), end stage renal disease, or in patients on dialysis is unknown. No dosage adjustments are necessary in patients with mild or moderate hepatic (Child-Pugh A or B) and/or renal impairment (CLcr ≥30-89 mL/min).
Please see full Prescribing Information and Patient Information for Verzenio.
AL HCP ISI 12OCT2021
About Lilly
Lilly is a medicine company turning science into healing to make life better for people around the world. We've been pioneering life-changing discoveries for nearly 150 years, and today our medicines help tens of millions of people across the globe. Harnessing the power of biotechnology, chemistry and genetic medicine, our scientists are urgently advancing new discoveries to solve some of the world's most significant health challenges: redefining diabetes care; treating obesity and curtailing its most devastating long-term effects; advancing the fight against Alzheimer's disease; providing solutions to some of the most debilitating immune system disorders; and transforming the most difficult-to-treat cancers into manageable diseases. With each step toward a healthier world, we're motivated by one thing: making life better for millions more people. That includes delivering innovative clinical trials that reflect the diversity of our world and working to ensure our medicines are accessible and affordable. To learn more, visit Lilly.com and Lilly.com/news, or follow us on Facebook, Instagram, and LinkedIn. P-LLY
Trademarks and Trade Names
All trademarks or trade names referred to in this press release are the property of the company, or, to the extent trademarks or trade names belonging to other companies are references in this press release, the property of their respective owners. Solely for convenience, the trademarks and trade names in this press release are referred to without the ® and ™ symbols, but such references should not be construed as any indicator that the company or, to the extent applicable, their respective owners will not assert, to the fullest extent under applicable law, the company's or their rights thereto. We do not intend the use or display of other companies' trademarks and trade names to imply a relationship with, or endorsement or sponsorship of us by, any other companies.
© Lilly USA, LLC 2025. ALL RIGHTS RESERVED.
Cautionary Statement Regarding Forward-Looking Statements
This press release contains forward-looking statements (as that term is defined in the Private Securities Litigation Reform Act of 1995) about Verzenio as a treatment for people with certain types of breast cancer and imlunestrant as a potential treatment for people with certain types of breast cancer and reflects Lilly's current beliefs and expectations. However, as with any pharmaceutical product, there are substantial risks and uncertainties in the process of drug research, development, and commercialization. Among other things, there is no guarantee that planned or ongoing studies will be completed as planned, that future study results will be consistent with study results to date, that Verzenio will receive additional regulatory approvals, or that imlunestrant will prove to be a safe and effective treatment for certain types of breast cancer or receive regulatory approval. For further discussion of these and other risks and uncertainties that could cause actual results to differ from Lilly's expectations, see Lilly's Form 10-K and Form 10-Q filings with the United States Securities and Exchange Commission. Except as required by law, Lilly undertakes no duty to update forward-looking statements to reflect events after the date of this release.
Endnotes and References
Johnston SRD, Harbeck N, Hegg R, et al; monarchE Committee Members and Investigators. Abemaciclib combined with endocrine therapy for the adjuvant treatment of HR+, HER2-, node-positive, high-risk, early breast cancer (monarchE) [published online ahead of print, September 20, 2020]. J Clin Oncol. doi:10.1200/JCO.20.02514.
Verzenio [package insert]. Indianapolis, IN: Eli Lilly and Company.
National Cancer Institute, SEER. Cancer Stat Facts: Female Breast Cancer. . Accessed August 21, 2025.
National Cancer Institute, SEER. Cancer Stat Facts: Female Breast Cancer Subtypes. . Accessed August 21, 2025.National Cancer Institute, SEER. Cancer Stat Facts: Female Breast Cancer Subtypes. . Accessed August 21, 2025.
Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687-1717. doi:10.1016/S0140-6736(05)66544-0.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229-263.
American Cancer Society. Cancer Statistics Center. . Accessed August 21, 2025.
Verzenio. Prescribing information. Lilly USA, LLC.
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Breast Cancer V.2.2024. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed May 9, 2024. To view the most recent and complete version of the guidelines, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Johnston SRD, Toi M, O'Shaughnessy J, Rastogi P, et al. Abemaciclib plus endocrine therapy for hormone receptor-positive, HER2-negative, node-positive, high-risk early breast cancer (monarchE): results from a preplanned interim analysis of a randomized, open-label, phase 3 trial. Lancet Oncol. 2023 Jan;24(1):77-90.
Sledge GW Jr, Toi M, Neven P, et al. The effect of abemaciclib plus fulvestrant on overall survival in hormone receptor-positive, ERBB2–negative breast cancer that progressed on endocrine therapy—MONARCH 2: a randomized clinical trial. JAMA Oncol. 2020;6(1):116-124. doi:10.1001/jamaoncol. 2019.4782
SOURCE Eli Lilly and Company
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果上市批准临床3期
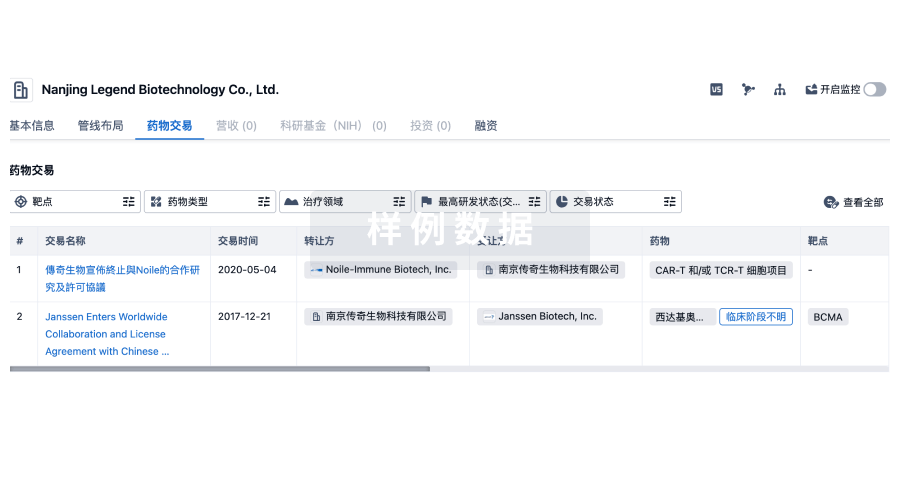
100 项与 长庚纪念医院 相关的药物交易
登录后查看更多信息
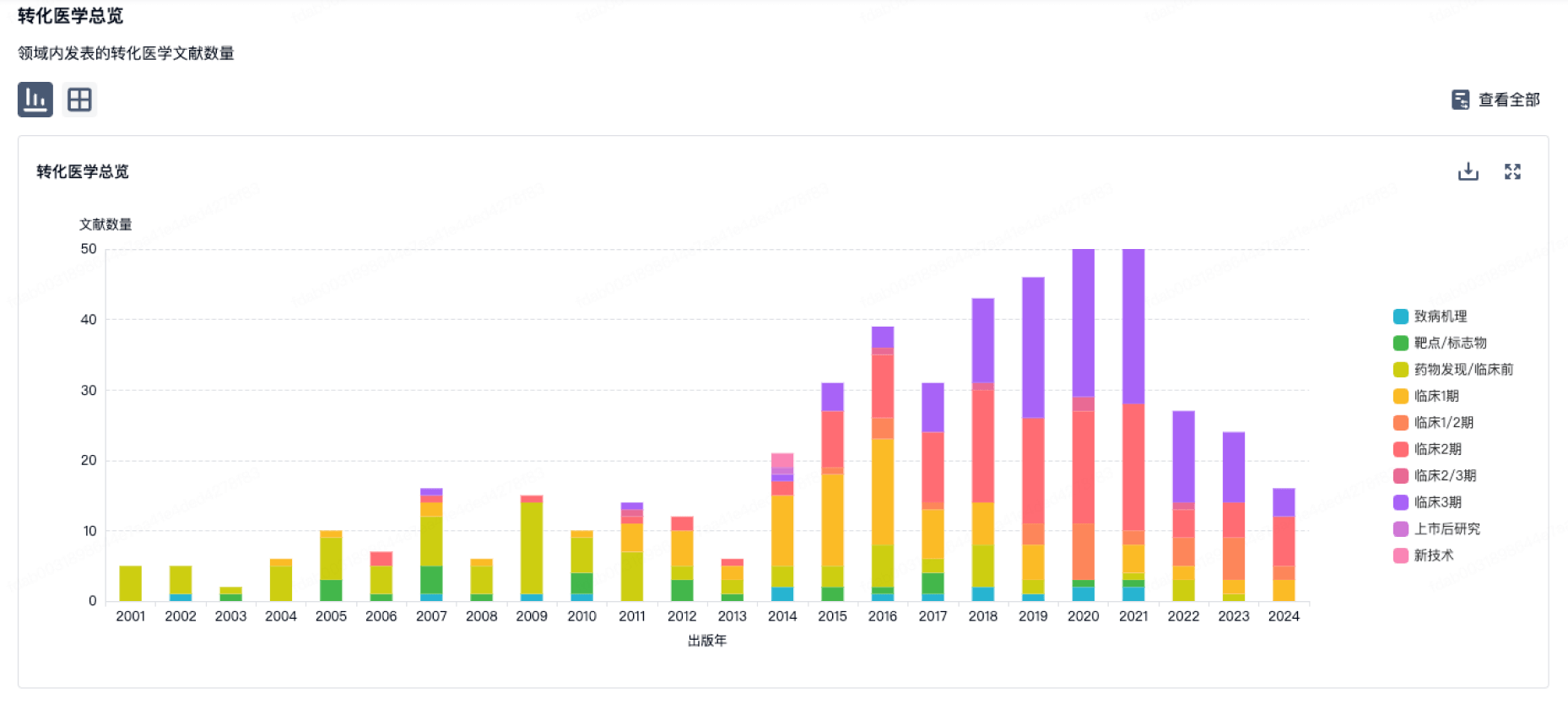
100 项与 长庚纪念医院 相关的转化医学
登录后查看更多信息
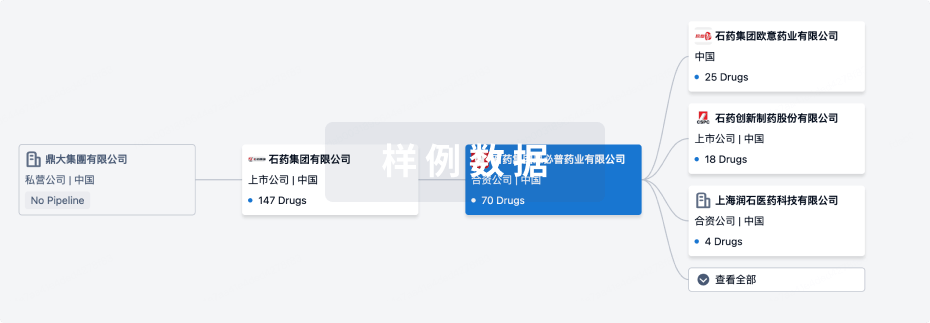
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月03日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
6
1
临床2期
其他
12
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
DAOIB ( NMDA receptor ) | 轻度认知障碍 更多 | 临床2期 |
Epidermal growth factor(Chang Gung Memorial Hospital) | 粘膜炎 更多 | 临床阶段不明 |
Small molecules 734(Chang Gung University) ( ANAPC1 ) | 乳腺癌 更多 | 临床前 |
茶黄素 ( RdRp ) | 新型冠状病毒感染 更多 | 临床前 |
Licochalcone D | 非酒精性脂肪性肝炎 更多 | 临床前 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
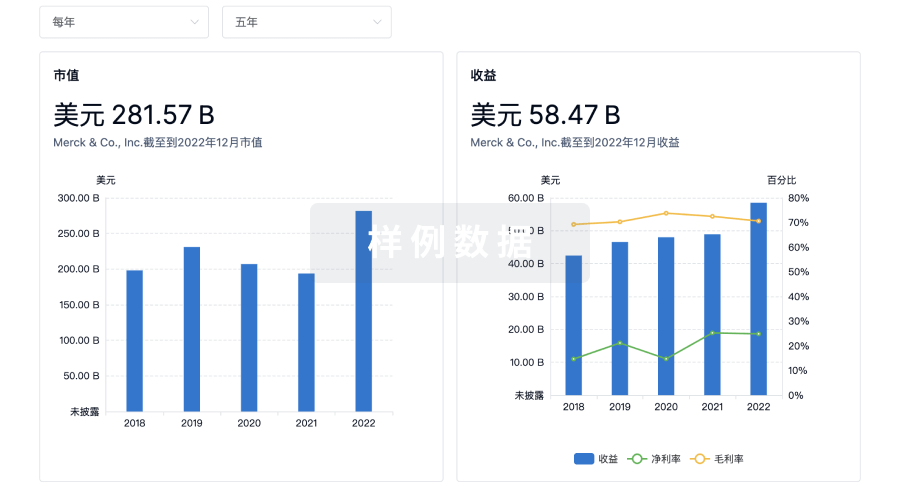
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
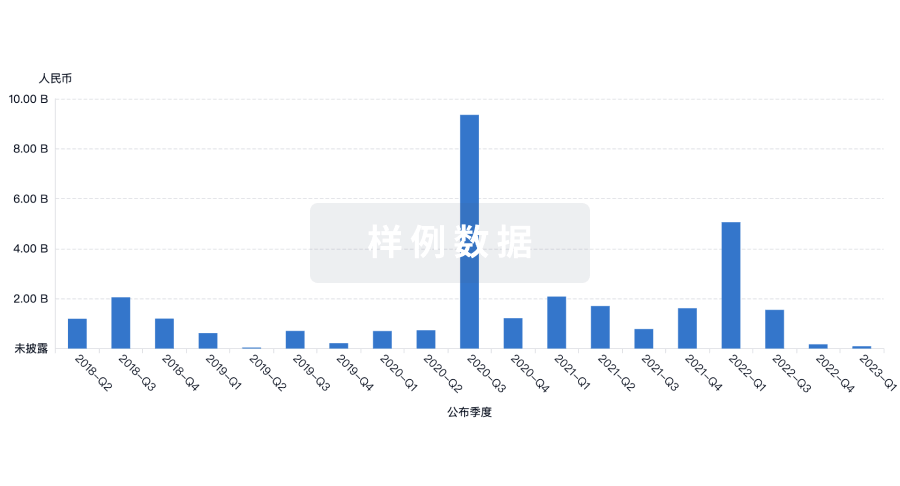
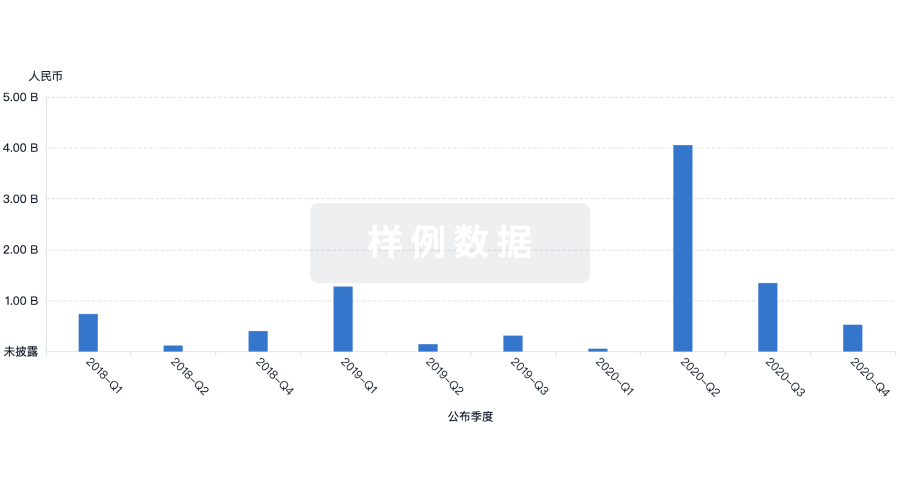
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
