更新于:2024-11-01
Guangzhou Institute Of Respiratory Health
更新于:2024-11-01
概览
标签
呼吸系统疾病
感染
干细胞疗法
外泌体药物
关联
2
项与 Guangzhou Institute Of Respiratory Health 相关的药物靶点- |
作用机制- |
在研适应症 |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
3
项与 Guangzhou Institute Of Respiratory Health 相关的临床试验Investigation of the Clinical, Radiological and Biological Factors Associated With Disease Progression, Phenotypes and Endotypes of COPD in China
This is a non-drug interventional cohort study, which aims to investigate the clinical, radiological and biological factors associated with disease progression in COPD in China. Participants will be recruited from multiple hospitals across Guangdong province categorized as Type A hospitals (those at prefecture-level and above) and Type B hospitals (those below prefecture-level).
开始日期2020-04-22 |
申办/合作机构  GSK Plc GSK Plc [+1] |
Clinical characteristics, predisposing factors and immune mechanism of Talaromyces marneffei in Chinese HIV-negative patients: A multicenter clinical study using bidirectional cohort
开始日期2019-06-01 |
Investigating the clinical features, airway inflammation and prognosis of atypical asthma patients in China: A Multi-centre, Prospective, Observational Cohort Study
开始日期2017-12-07 |
100 项与 Guangzhou Institute Of Respiratory Health 相关的临床结果
登录后查看更多信息
0 项与 Guangzhou Institute Of Respiratory Health 相关的专利(医药)
登录后查看更多信息
122
项与 Guangzhou Institute Of Respiratory Health 相关的文献(医药)2024-09-01·European Journal of Nuclear Medicine and Molecular Imaging
The impact of PET/CT and brain MRI for metastasis detection among patients with clinical T1-category lung cancer: Findings from a large-scale cohort study
Article
作者: Chen, Peiling ; Ye, Wenjun ; Chen, Zhuxing ; Xiang, Yang ; Fu, Xiuxia ; He, Jianxing ; Fu, Wenhai ; Liu, Haiping ; Wang, Huiting ; Cheng, Bo ; Wang, Qixia ; Feng, Yi ; Hu, Guodong ; Wang, Runchen ; Wang, Zixun ; Liang, Wenhua ; Li, Jianfu ; Zhan, Shuting ; Zhu, Feng ; Zheng, Xin ; Huang, Xiaoyan
2024-08-01·The Veterinary Journal
Development of a P30 protein-based indirect ELISA for detecting African swine fever antibodies utilizing the HEK293F expression system
Article
作者: Sunkang, Yongjie ; Cheng, Yuanyi ; Gao, Fei ; Jian, Weijun ; Huang, Lihong ; Niu, Xuefeng ; Chen, Huahan ; Qi, Wenbao ; Zhu, Junhai
2024-08-01·The Clinical Respiratory Journal
A Nomogram for Predicting Cancer‐Specific Survival in Young Patients With Advanced Lung Cancer Based on Competing Risk Model
Article
作者: Pan, Bolin ; Liu, Ming ; Li, Jiaxin ; Zhou, Chengzhi ; Lin, Xinqin ; Zhan, Chulan ; Huang, Qiying ; Wang, Liqiang ; Qiu, Yangzhi ; Xie, Xiaohong ; Zhang, Honglang ; Lin, Tong
26
项与 Guangzhou Institute Of Respiratory Health 相关的新闻(医药)2024-10-21
·动脉网
呼吸系统疾病的治疗一直是医疗领域研究的热点和难点。
作为全球四大类慢性病之一,呼吸系统疾病在我国患者总数超过1.5亿。但当前呼吸系统疾病的有效治疗方案相对有限,常规药物治疗对于晚期患者而言效果欠佳,已难以满足其治疗需求。因此,治疗效果良好的介入治疗方式成为现阶段临床研究重点,并快速发展。
其中,冷冻技术在早期临床呼吸系统疾病诊断及治疗中应用效果显著,自1994年可弯曲冷冻探头问世以来便在国内外的呼吸介入领域得到广泛应用,积累下一定临床经验。如今,层出不穷的技术创新,更是为临床提供了疗效更佳的解决方案:康沣生物另辟蹊径,采用液氮作为冷冻介质源,柔性导管作为输送器械,打造冷冻治疗呼吸疾病全面的产品组合。
值得一提的是,除持续优化迭代产品外,今年以来康沣生物还通过合作不断拓宽市场边界,深化产业布局。不仅在行业内积极拓展合作,与波士顿科学达成战略合作,利用双方在呼吸介入领域的业务布局、专业知识及资源,为创造呼吸介入领域的协同效应打下基础。近日,企业全资子公司宁波胜杰康生物科技有限公司(“宁波胜杰康”)还宣布将与广州医科大学附属第一医院共同参与广州国家实验室立项并管理的研究项目,以探索肺癌冷冻消融产品于临床实践的应用,加速此项创新疗法的落地,并惠及广大有需要的患者。
据了解,广州国家实验室是呼吸系统疾病及其防控领域的新型科研机构,是呼吸系统疾病领域的核心科技力量。广州医科大学附属第一医院是广州呼吸健康研究院、国家呼吸系统疾病临床医学研究中心以及呼吸疾病全国重点实验室所在医院。
根据科研合作协议,宁波胜杰康与广州医科大学附属第一医院将共同参与并完成基于液氮超低温冷冻系统研发及在肺癌消融的球囊冷冻研究,结合订约方资源共同推进开发完成基于液氮超低温冷冻系统的专用于周围性肺癌的创新冷冻球囊消融产品。
此次双方的合作不仅显示了业内对康沣生物冷冻技术满足临床需求及先进性的高度认可,同时也标志着双方将携手深入挖掘冷冻技术在肺周肿瘤治疗的潜力,通过学术交流、临床科研以及创新技术转化等途径,康沣也将加速冷冻技术在呼吸介入领域的研发及应用进程,为肺周肿瘤这一复杂疾病的治疗带来新突破。
重大创新!
突破液氮冷冻消融及柔性导管技术
冷冻技术是在支气管镜下经可弯曲冷冻探头在支气管腔内实施的一系列操作,包括冷冻消融和冷冻切除技术。该技术具有效果确切、操作安全简便、并发症少、费用低等特点,在气道良、恶性病变以及腔内少见病的诊治中发挥着热消融等方法无可替代的作用。
其中,冷冻消融不仅可用于治疗疼痛及与异常组织扩散相关的其他症状,而且在肿瘤手术风险过高时,也可作为独立疗法来缓解癌症症状。同时,冷冻消融无需开放手术即可进行,能够作为大型综合治疗方案的一部分,为无法进行手术摘除肿瘤的患者提供支持。与其他消融技术相比,具有局部麻醉、疼痛较轻及能保留肿瘤免疫抗原性等多重优势,且医生操作时间更短。此外,冷冻消融形成的冻结部位界线清晰、温度均匀,便于监控消融区域。
在人口老龄化加速、慢性病患病率上升以及政策支持等多重因素推动下,中国冷冻介入治疗器械市场近年来展现出强劲的增长势头。
尽管冷冻消融技术优势明显,但冷冻速度、复温速度、最低温度、重复次数以及冷冻持续时间等因素均会影响冷冻治疗效果。要最大化发挥冷冻消融技术的价值,设备厂商仍面临不小考验。
从技术研发的角度来看,仅实现冷冻消融设备的精准控制就是一项严峻挑战。这要求精确控制冷冻探头的温度,以确保既能有效破坏目标组织,同时又不损伤周围的健康组织。为此,设备厂商需要开发高精度的温度控制系统,并确保稳定的能源供应。此外,使用液氮等冷冻剂时,还需有效且准确地控制汽化过程中的体积膨胀,避免液氮通过细小通道泵发生大量体积膨胀,导致阻碍冷冻剂进一步流动等严重后果。
同时,冷冻消融探头的设计与制造也是一道关键突破口。探头唯有具备良好的柔韧性和硬度、耐高压性及耐温性等特性,才能够顺利深入肺部狭窄、弯曲的气道。而探头的材质和结构设计也需要不断优化,以提高冷冻效率并减少潜在的副作用。
在面临极高技术细节要求的情况下,康沣生物成功突破液氮冷冻消融技术和柔性导管技术,并将核心技术延伸至呼吸介入领域。
其液氮冷冻消融技术平台可保留液氮消融效率高及可控的优点,同时解决汽化相关的体积变化过大的问题,降低器械的工作压力及增加手术安全性。在此基础上,康沣生物还研发有精准温度场控制技术和实时真空技术等底层和配套技术,以提高产品的有效性和安全性,推进冷冻治疗系统的临床应用。
其柔性导管技术则具有易于弯曲的特点,能在到达目标位置后快速扩张,不仅能够使冷冻治疗导管内的球囊与靶向组织形成较宽的接触面,在相对较大的区域内进行冷冻消融,而且还可达到较深的深度。
近年来,由于空气污染严重、吸烟人口众多和重大急性呼吸传染疾病频发等因素,慢性呼吸疾病的患者人数仍在持续攀升,中国已成为呼吸疾病高发国家。数据表明,中国呼吸类疾病的患者数量已超过1.5亿人。
这不仅为呼吸科及相关科室的疾病防治工作带来了压力,也对呼吸学科与呼吸系统疾病治疗方式的创新发展提出了更高要求:临床需要更为高效、精准的治疗方式。
面对这一挑战,康沣生物基于底层技术,针对呼吸系统疾病临床需求,以微创介入(经人体自然腔道)的形式为呼吸系统的多种疾病提供更有效安全的解决方案,以冷冻消融产品为核心,布局涵盖哮喘、慢阻肺、气道狭窄、慢性咳嗽、肺周肿瘤疾病治疗等多个领域,实现多个产品“首创”,并计划于2024~2026年陆续将产品推向市场。
● 全球首个支气管冷冻去神经方案
哮喘作为一种肺气道长期发炎的疾病,特点是症状反复无常、可逆性气道受阻及容易触发的支气管痉挛。在我国20岁及以上人群哮喘患病率为4.2%,总数达4570万。
吸入剂或白三烯受体拮抗剂等药物控制是目前主要的控制方法。然而,药物控制对重度哮喘的疗效有限。在所有成人哮喘患者中,有3.6%被诊断为严重难治性哮喘。尽管药物对重度哮喘的疗效有限,但大部分重度哮喘患者(>99%)仍然使用药物控制症状(弗若斯特沙利文资料)。
对于重度哮喘患者而言,非药物治疗(如冷冻消融及支气管热成形术)可缓解症状。正是因此,康沣生物首创哮喘冷冻消融系统,通过冷冻靶向消融呼吸道迷走神经,阻断呼吸道迷走神经信号传递并减少乙酰胆碱释放,同时降低气道平滑肌张力并减少气道黏液的产生,进而减轻整个肺部的气道阻塞,达到治疗哮喘的作用。相较于射频消融该疗法更安全、疼痛感低、恢复快。
冷冻靶向去神经术
● 中国首个COPD喷雾冷冻系统,液氮喷雾精准消融黏膜病变细胞
慢阻肺(COPD)是一种常见的呼吸系统疾病,特点是持续的呼吸系统症状及气道受阻。临床上,慢性支气管炎和肺气肿与慢阻肺的发生密切相关。据最新《中国慢性阻塞性肺疾病分级诊疗报告》显示,中国慢阻肺患者数近1亿人,占总人口的近1/14。
根据不同症状及恶化病史的程度,慢阻肺药物治疗可分为四类,即支气管扩张剂、长效交感神经刺激剂、长效抗胆碱能药物及吸入式类固醇。迄今为止,尚未有确凿临床试验证据证明现有药物可调整肺功能的长期退化。冷冻消融作为其中一种介入疗法,具有并发症出现率低及存活率高等优势,有望成为治疗慢阻肺的有效疗法。
在此基础上,康沣生物研发出国内首款应用于慢性阻塞性肺疾病的冷冻消融器械。该系统能够在气道内实现环周、定量、可控地喷洒冷冻介质,对气道黏膜上皮进行冷冻替换,进而重塑黏膜上皮从而实现治疗效果,实现高效快速的非接触治疗。
液氮喷雾治疗COPD
● 首款用于支气管镜介入治疗良恶性气道狭窄的球囊冷冻产品
气道狭窄是由肿瘤或非肿瘤过程引起的气道缩窄。
恶性气道狭窄主要通过肿瘤切除及气管镜介入进行治疗,良性气道狭窄的传统治疗方式主要包括手术切除及手术重建。然而,由于手术创伤、高风险或健康状况不佳,外科手术的适应症十分有限,而术后吻合瘢痕的形成还可能引起再狭窄。在良性气道狭窄治疗过程中,通过对经热消融或球囊扩张后的残留病变部位进行冷冻消融,可降低瘢痕再狭窄的比率及程度。此外,冷冻治疗造成软骨损伤及穿孔的可能性较热消融低,出现气道软化及塌陷的并发症较少。
如今随着消融等介入疗法获得专业人士认可,有望为患者提供更多生存机会及延长寿命,并为后续治疗提供机会。正因如此,康沣生物首创冷冻消融系统,用于良、恶性气道狭窄的治疗。
在手术过程中,恶性气道狭窄冷冻消融系统利用冷冻消融系统产生的超低温消融气管腔内及腔壁的肿瘤细胞或治疗过程中的组织增生,然后通过复温进一步破坏残余细胞。冷冻消融球囊能在较大范围内对恶性肿瘤进行更彻底的消融,并延缓再狭窄的时间。良性狭窄冷冻消融系统在产品结构及操作程序上与恶性狭窄冷冻消融系统基本相同。
不同于传统用于气道组织冷冻失活的器械,该款产品冷冻温度更低,降温速率更快,可以短时间、大范围覆盖狭窄组织,进一步延缓患者再狭窄时间,降低患者再狭窄率,预计将是首款用于支气管镜介入治疗良恶性气道狭窄的球囊冷冻产品,是气道狭窄治疗的一种更优的解决方案。
● 全球首个经支气管球囊冷冻消融肺周肿瘤系统,超低温实现肿瘤完全消融覆盖
据最新发布的《2022年中国恶性肿瘤疾病负担情况》数据显示,肺癌已成为我国发病率和死亡率均位居首位的恶性肿瘤,且在男性和女性的恶性肿瘤发病率及死亡率排名中均高居榜首。
随着肺癌等呼吸系统疾病的发病率逐年攀升,以及现代医疗模式日益倾向于微创与精准治疗,患者对微创治疗的需求日益增长。创新技术的涌现,使得冷冻消融技术在呼吸介入领域的应用范围进一步扩大。
针对肺癌的高发病率及死亡率,康沣生物全球首创经支气管球囊冷冻消融治疗肺外周肿瘤的冷冻消融器械。利用球囊产生的超低温(-120℃~-150℃)实现对肿瘤的完全消融覆盖,达到原位灭活。通过柔性导管、经气道方式入路治疗,大大减少气胸、咯血等并发症的产生。同时利用冷冻消融诱导较强免疫反应的特点,通过冷冻消融与免疫治疗相结合,为肺癌的治疗提供更多的治疗机会及方案,更好地改善患者的生存质量,提高患者的生存时间,降低肺癌的病死率,缩短住院时间,减轻医疗负担。
冷冻消融肺周肿瘤
左:术前规划,中:柔性导管冷冻,右:消融范围覆盖肿瘤
● 国际首创,应用冷冻技术治疗慢性咳嗽
慢性咳嗽是在咳嗽变异性哮喘及慢阻肺等各种疾病期间出现的症状。我国的慢性咳嗽患病率为24.04%。由于其病因复杂,加上过去临床医生缺乏对慢性咳嗽的认识,临床误诊及不当治疗十分常见。
就有确实病因的慢性咳嗽而言,治疗通常根据病因对症下药。冷冻消融能通过药物治疗无法达成的方式,对准并消融病变气道,对慢性咳嗽进行治疗。
康沣生物自主研发的咳嗽冷冻喷雾治疗系统是国际首创应用冷冻技术治疗慢性咳嗽的医疗器械。该系统通过冷冻消融气道内过多和高敏感度的咳嗽感受器,恢复咳嗽阈值,从而达到治疗效果,有望成为全球首款针对慢性咳嗽的喷雾冷冻消融系统。
呼吸介入市场方兴未艾,
康沣生物持续拓宽市场布局
介入呼吸病学作为近二十年来逐步发展起来的一门新兴学科,随着新材料、新技术、新理念的不断涌现而快速发展,在呼吸系统疾病的诊断和治疗方面发挥着越来越重要的作用,其适应证也随之扩展。
球囊扩张、电烧蚀、冷冻、激光作为千禧年前后才进入中国的技术,近年来也逐渐在呼吸疾病的治疗中崭露头角,成为不可或缺的治疗技术。但由于冷冻介入治疗器械准入门槛高,研发者不仅需具备涵盖机械工程、先进材料及电磁兼容性等开发有源医疗器械的多学科专业知识,面临冷冻治疗器械的技术挑战,还需突破精确控制冷冻剂汽化过程中的体积膨胀,以及设计并制造能到达目标位置同时具备耐温性能的细长柔性导管等技术难关。
正因如此,国内成功研发呼吸系统介入冷冻治疗产品的企业仅是寥寥。
康沣生物作为中国首批开发利用喷雾及冷冻球囊消融技术治疗呼吸系统疾病的冷冻治疗产品市场参与者之一,已有11年冷冻技术及数年呼吸介入冷冻治疗产品研发经验。公司不仅实现了多项关键技术突破,还基于长时间的技术积累与迭代成功打造全面的冷冻治疗呼吸疾病产品组合。
此外,康沣生物不断与外部建立交流与合作,积累了丰富的临床资源和专家资源,临床中心覆盖全国大部分省市。这也将有助于企业围绕临床痛点与需求,打造满足不同适应症需求的产品组合,推动冷冻技术更好地在呼吸介入领域发挥价值。
今年以来,康沣生物分别与波士顿科学和广州呼吸健康研究院达成合作,更是在拓宽市场边界、深化产业布局及产品研发优化迭代上发力。目前,康沣生物围绕呼吸介入领域打造的8款产品中,已有1款拿证,其余产品也将陆续获批并商业化。
无疑,在呼吸介入领域,康沣生物还拥有更为广阔的想象空间。
如果您想对接文章中提到的项目,或您的项目想被动脉网报道,或者发布融资新闻,请与我们联系;也可加入动脉网行业社群,结交更多志同道合的好友。
近
期
推
荐
声明:动脉网所刊载内容之知识产权为动脉网及相关权利人专属所有或持有。未经许可,禁止进行转载、摘编、复制及建立镜像等任何使用。
动脉网,未来医疗服务平台
2024-06-09
·药事纵横
声明:因水平有限,错误不可避免,或有些信息非最及时,欢迎留言指出。本文仅作医疗健康相关药物介绍,非治疗方案推荐(若涉及);本文不构成任何投资建议。
2023年,匈牙利科学家Katalin Karikó和美国科学家Drew Weissman因在mRNA疫苗领域贡献突出,获得诺贝尔生理医学奖。
放眼全球,Moderna、BioNTech和CureVac已成为“mRNA三大巨头”,且肿瘤疫苗研发已进展至Ⅱ期临床甚至Ⅲ期临床阶段,其中Moderna和默沙东研发的mRNA-4157癌症疫苗进展最快,已进入Ⅲ期临床阶段。
5月31日,美国FDA批准Moderna的呼吸道合胞病毒(RSV)mRNA疫苗 mRESVIA(mRNA-1345)上市,用于保护60岁及以上成年人免受RSV感染引起的下呼吸道疾病,这是Moderna第2项获批的mRNA疫苗。
放眼国内,有手握mRNA新冠疫苗商业化产品的三大中国公司——石药集团、沃森生物、斯微生物,但是它们却“从未”享受到“新冠红利”。而艾博生物、斯微生物和丽凡达生物被称为“国产mRNA疫苗三剑客”。目前,国内mRNA技术的发展还处于早期阶段。据不完全统计,国内布局该领域的公司至少有55家,具体如下:
来源:细胞基因治疗前沿整理
由上表可见,受新冠疫情的影响,国内众多药企纷纷入局mRNA新冠疫苗研发。从2019年开始,国内mRNA公司快速增长。2018年仅有3家mRNA公司成立,2019年猛增至11家,2020年6家公司成立,2021年12家公司成立。
来源:细胞基因治疗前沿整理
由上图可见,55家mRNA公司主要集中在东部地区,主要分布在北上广、江苏。
接下来将列举部分药企及管线进度或最新研发进展情况。
1
沃森生物
沃森生物成立于2001年,是专业从事人用疫苗等生物技术药集研发、生产、销售于一体的高科技生物制药企业。于2010年在创业板上市,是云南省首家在创业板上市的企业。公司拥有全球两大重磅疫苗品种13价肺炎结合疫苗和HPV疫苗,并构建了国内领先的疫苗研发和产业化技术平台, 作为国内单体拥有已上市疫苗品种数量最多,且独家拥有两大全球最畅销疫苗品种的企业。
2023年12月初,沃森生物新冠病毒变异株mRNA疫苗(Omicron XBB.1.5)获批上市,成为我国首个基于完整III期安全性和有效性数据通过免疫原性桥接临床获批紧急使用的针对XBB等当前变异株的新冠mRNA疫苗。
研发管线
2
石药集团
石药集团作为老牌药企入局mRNA疫苗,优势显著。石药集团高效搭建起核酸药物平台,推进针对Delta和Omicron等多种毒株在内的mRNA疫苗项目,除了研发新冠疫苗,还研发针对慢性遗传基因相关重大疾病的药物。
2023年3月22日,其新冠病毒二价mRNA疫苗(SYS6006.32)在中国纳入紧急使用,用于预防新型冠状病毒感染引起的疾病。这是中国首个自主研发、获得紧急授权使用的新冠疫苗,证明了石药集团核酸平台的研发实力。而其mRNA RSV疫苗临床试验(IND)申请已获得CDE受理。
3
斯微生物
斯微生物曾被誉为“国产mRNA疫苗三剑客”之一,如今却深陷泥潭。2023年,斯微生物出现资金链紧张,旗下天慈工厂暂停运行,李航文被限制高消费。
而早在2021年1月,其新冠mRNA疫苗获得临床试验批件,成为了国内第二款进入临床阶段的国产新冠mRNA疫苗。
2022年12月8日,其自主研发的新型冠状病毒mRNA疫苗(商品名:斯维尔克®)获得老挝人民民主共和国卫生部食品药品监督管理局授予的紧急使用授权,用于18周岁及以上人群通过主动免疫来预防新冠病毒肺炎。这是第一个在老挝获批的国产新型冠状病毒mRNA疫苗,也是中国第一个获得紧急使用授权的新型冠状病毒变异株mRNA疫苗。
其自主研发的SWP1001是世界范围内首个获得临床批件的国产自主研发编码新抗原mRNA个性化肿瘤疫苗,也是国内首家进入临床研究公司。
4
艾博生物
艾博生物成立于2019年初,被誉为“国产mRNA疫苗三剑客”之一,掌握 LNP 核心技术,是国内自主研发 mRNA 疫苗进展最快的企业,拥有业界领先并具有自主知识产权的mRNA和纳米递送技术平台,建立了丰富的产品管线,涵盖传染病防治和肿瘤免疫等领域。
2023年4月,艾博生物与广州呼吸健康研究院联合启动自主研发肺癌新抗原mRNA疫苗临床研究项目。2023年11月17日,艾博生物与臻知医学合作的全球首创编码近20种肝癌抗原的mRNA疫苗完成首次人体给药,该疫苗经肌肉注射后可诱导患者自身免疫系统恢复抗肿瘤能力。
2024年3月,军科院/艾博生物开发组合型双打击mRNA编码抗体疗法,针对正痘病毒。
研发管线
5
丽凡达生物
丽凡达生物成立于2019年,是“国产mRNA疫苗三剑客”之一。该公司拥有自主mRNA生产和药物递送平台,主要聚焦传染病疫苗、肿瘤、肝脏疾病、罕见病等创新型生物药的开发,也可以应用于美容及抗衰老等领域。
2021年3月,丽凡达生物研制的mRNA新冠疫苗已在中国获批临床,成为继艾博生物、斯微生物之后的国产第3款mRNA新冠疫苗。但可惜的是直到疫情结束,该mRNA疫苗也未成功上市,
2021年5月,公司被艾美疫苗收购。
6
威斯津生物
威斯津生物成立于2021年,由四川大学华西院士团队创立,其主要的创始人之一宋相容教授曾在哈佛医学院从事mRNA疫苗相关的研究,拥有以人工智能突破mRNA序列和递送系统两大核心技术。
目前,威斯津生物在mRNA药物和新型纳米佐剂领域布局的产品管线超过20个,全面覆盖了mRNA肿瘤治疗性疫苗、针对传染病的mRNA预防性疫苗,以及针对其他疾病如肥胖、衰老的治疗性药物等领域。
肿瘤治疗疫苗研发管线
5月7日,威斯津生物EB病毒相关肿瘤mRNA疫苗“WGc-043 注射液”,获得美国FDA的IND批件,获准开展临床试验。这也是全球首个获批IND的EB病毒相关肿瘤mRNA治疗性疫苗。
7
深信生物
深信生物成立于2019年,主要专注于mRNA技术及LNP递送技术,从事预防性和治疗性新型疫苗及药物的开发。它是国际范围内少数掌握核心脂质体底层设计技术的公司之一。
深信生物在mRNA药物的设计、合成及修饰成方面亦拥有独特的技术优势,围绕mRNA及LNP技术平台申请了多项具有重要应用价值的专利,完成了多条研发管线的布局,部分管线即将完成临床前试验工作。
2020年12月,智飞生物认购深信生物10%股权,后退出,由Innorna接盘。
今年6月初,深信生物二价呼吸道合胞病毒(RSV)mRNA 疫苗 IN006获批进入临床,用于主动免疫,以预防 60 周岁及以上人群呼吸道合胞病毒(RSV)所致下呼吸道疾病。IN006成为首款获得中国临床试验许可的国产 RSV 疫苗产品。
8
嘉晨西海
嘉晨西海致力于开发基于mRNA平台的创新型药物,其基于自复制mRNA核心平台技术处于国际领先水平,可应用于包括肿瘤治疗药物、个性化肿瘤疫苗、传染病疫苗、罕见病治疗、医学美容等领域。
嘉晨西海特有的mRNA构建和成熟的通用化工艺平台,同时适合于自复制mRNA和传统非复制型mRNA产品的开发,便于根据疾病领域来选择更佳的mRNA形式。鉴于此,欧林生物、天境生物、君实生物、民海生物都与嘉晨西海进行了合作。
研发管线
嘉晨西海的JCXH-211是全球首款表达细胞因子的自复制mRNA癌症治疗药物,标准治疗后进展或对标准治疗不耐受的实体瘤患者(目前仅入组头颈癌和黑色素瘤),目前在中美同步进行临床试验。自复制mRNA癌症疫苗JCXH-212也已进入2期临床试验。
9
康希诺
康希诺生物成立于2009年,主营业务是研发、生产和商业化符合中国及国际标准的创新型疫苗,主要产品为埃博拉病毒病疫苗、脑膜炎疫苗、百白破疫苗、肺炎疫苗、结核病疫苗、带状疱疹疫苗、新冠肺炎疫苗、腺病毒疫苗、脊髓灰质炎疫苗。
2024年3月,康希诺与凯莱英生物宣布在在质粒、mRNA、LNP类的生物药大分子领域实现创新协作、优势互补,共同促进mRNA技术的研发和产业化。
研发管线
10
艾美疫苗
作为中国大型全产业链疫苗公司,艾美疫苗涵盖了从研发到制造再到商业化整个价值链。公司拥有5种经过验证的人用疫苗平台技术:细菌疫苗平台技术、病毒疫苗平台技术、基因工程疫苗平台技术、联合疫苗平台技术及mRNA疫苗平台技术。公司经营荣安生物、艾美诚信、艾美康淮及艾美卫信四个工厂。产品覆盖了31个省、自治区、直辖市,在售产品主要包括重组乙型肝炎疫苗、冻干人用狂犬病疫苗(Vero细胞)、甲型肝炎减活疫苗(人二倍细胞)等。
今年3月,艾美疫苗(06660.HK)发布公告:其研发的13价肺炎结合疫苗、无血清迭代狂犬疫苗及23价肺炎多糖疫苗均已完成III期临床试验,预计2024年完成申报并上市。
研发管线
参考资料:
公开资料
信使RNA疫苗临床3期上市批准基因疗法
2024-05-13
·信达生物
转载自:南山呼吸近日,广州医科大学附属第一医院何建行/梁文华教授团队,在国际顶级期刊Nature子刊Signal Transduction and Targeted Therapy(中国科学院/ JCR一区,IF=39.3)在线发表研究“The activity and immune dynamics of PD-1 inhibition on high-risk pulmonary ground glass opacity lesions: insights from a single-arm, phase II trial”[1]。广州医科大学附属第一医院、广州呼吸健康研究院、国家呼吸医学中心何建行教授、梁文华教授为共同通讯作者,团队程博博士,黎才琛博士,李坚福博士,梁鹏博士以及臻和科技巩龙龙博士为本文主要第一作者。该研究首次证实,PD-1抑制剂对多原发肺癌(MPLC)患者的早期磨玻璃病灶具有一定疗效,且安全性良好,并展示了PD-1阻断在超早期肺癌治疗中的免疫动态变化。研究背景随着抗PD-1/PD-L1抗体等免疫检查点抑制剂的广泛应用,晚期NSCLC患者的总生存期得到显著延长。此外,新辅助免疫治疗在I-IIIA期可切除NSCLC患者中的疗效同样显著。但关于免疫治疗对极早期肺癌患者的疗效,目前尚不明确。近年来,MPLC患者的检出率逐渐升高,在CT中通常表现为多发磨玻璃结节,这些结节大多是处于肺癌早期的微浸润性甚至浸润前病灶。在MPLC患者接受主要病灶的手术后,如何处理其未切除且有较高进展风险的剩余病灶当前尚无共识。研究表明,免疫逃逸在肺癌的浸润前阶段就已经发生。因此,免疫治疗在肺部高危磨玻璃结节患者中的应用值得探索。对此,何建行教授团队开展了一项单臂、II期临床研究(NCT04026841),旨在评估信迪利单抗治疗MPLC患者高危磨玻璃病灶的有效性和安全性,并观察了这些早期肺癌患者在用药治疗期间的免疫动态。研究设计这是一项前瞻性、单臂、II期临床试验。所有入组患者均具有两个或两个以上无法同时切除的肺结节,其中至少一个经病理检查(手术切除或穿刺活检)证实为NSCLC;且存在未切除的磨玻璃病灶,CTR≤0.5,直径1-3 cm,持续存在≥1年,经MDT一致评估为高危肺结节(Lung-RADs 4级或6个月内曾出现进展),高度怀疑为原发恶性病灶。图1. 研究设计及检测项目所有患者均接受共4个周期的信迪利单抗治疗(200mg,q3w),旨在评估信迪利单抗治疗MPLC患者高危磨玻璃病灶的有效性和安全性,主要终点为客观缓解率(ORR)。对于入组患者,目标病灶定义为符合入选标准的纯磨玻璃病灶或磨玻璃成分主的病灶(CTR≤0.5),非目标病灶定义为纯实性病灶或实性成分为主的病灶(CTR>0.5); 以上病灶均经MDT评估为恶性。研究结果研究共纳入36例患者,中位年龄为59.5岁(IQR, 53.5-69)。其中,66.7%(24/36)为女性,19.4%(7/36)的患者具有吸烟史;所有患者切除(或活检)的主病灶均为腺癌,其中88.9%(32/36)为I期或原位腺癌,52.8%(19/36)为EGFR突变阳性。有效性及安全性患者接受信迪利单抗治疗的ORR为5.6%(2/36),有2例患者的目标病灶(CTR≤0.5)获得缓解,包括1例完全缓解和1例部分缓解。此外,有3例患者的3个非目标病灶(CTR>0.5)在治疗后出现缓解。将非目标病灶考虑在内,则患者的总缓解率为13.9%(5/36),其余31例患者的病灶未见明显变化,所有入组患者在用药期间均未发生疾病进展。入组患者中有26例(72%)出现了不良事件(AE),其中17例(47%)为I级,9例(25%)为II级,随访过程中无患者发生3-5级AE。疲劳(36%,13/36)和皮疹(36%,13/36)是最常见的AE,无患者因AE退出试验。图2. 有效患者目标病灶的影像学变化在5例有效患者中,1例接受了手术治疗,4例继续随访观察;31例无效患者中,11例接受了手术治疗,20例继续随访观察。在治疗完成后的随访中,未观察到有患者出现疾病进展。多重荧光免疫组化(mIHC)治疗完成后,基于患者的手术切除肿瘤组织,进行了多重荧光免疫组化检测。结果显示,相比于无效患者,有效患者的肿瘤被更多的CD8+ T细胞浸润,而CD4+ T细胞,CD19+ B细胞,以及CD163+ M2型巨噬细胞更少。图3. mIHC检测结果T/B/NK细胞研究在每个周期用药前抽取血液样本(T1-T4),对有效患者和无效患者的T/B/NK细胞、T细胞受体(TCR)、细胞因子、和外泌体RNA等生物标志物进行了监测和比较。结果表明,有效患者(用药前)基线外周血中的CD8+ T细胞比例(平均值:36.6% vs 24.6%,P<0.001),以及CD8+/CD4+ T细胞比值(平均值:1.09 vs 0.64, P<0.001)均显著高于无效患者,并随着治疗进程逐渐降低。图4. 基线血T/B/NK细胞的检测结果及其变化趋势T细胞受体(TCR)比较两组患者基线外周血中TCR的克隆性和多样性发现,与无效患者相比,有效患者具有显著更高的TCR克隆性(平均值:0.319 vs 0.129,P<0.01),以及更低的Shannon指数(平均值:8.565 vs 11.504,P<0.01)和均匀性(平均值:0.681 vs 0.872, P<0.01)。此外,在治疗期间,有效患者的TCR克隆性呈下降趋势,而Shannon指数和均匀性呈上升趋势。图5. 基线血TCR的检测结果及其变化趋势细胞因子研究检测了患者外周血中的45种细胞因子和14个免疫检查点,发现有效患者在T2时的EGF(P=0.027)和T4时的CTLA-4(P=0.046)浓度显著高于无效患者。此外,观察细胞因子在患者治疗期间的变化情况,除两组患者的PD-1水平在用药后显著降低外,其余各种细胞因子均无明显变化。图6. 外周血细胞因子检测结果外泌体RNA基于患者的外泌体RNA进行GSEA富集分析。结果显示,相比于无效患者,有效患者中Myc targets_v2基因集上调,脂肪酸代谢、氧化磷酸化和蛋白质分泌相关基因集下调。研究者又采用时间序列聚类分析观察两组患者在治疗期间的基因表达趋势,发现有效患者中的部分基因通路发生了显著调控(上调或下调)。进一步采用KEGG和GO富集分析表明,在有效患者中,氧化磷酸化和非酒精性脂肪肝病等通路下调,以及与NADH脱氢酶和氧化还原酶活性相关的基因表达下调。图7. GSEA富集分析图8. KEGG及GO富集分析该研究首次证实,免疫治疗对MPLC患者的早期磨玻璃病灶具有一定疗效,且药物毒性可控,安全性较好。其治疗效果与特异性T细胞的重分布、EGF/CTLA-4等细胞因子的调节、和相关代谢通路的调控有关。总结&展望此前,何建行/梁文华教授团队发文,在国际上首次证明了EGFR-TKIs对MPLC患者早期磨玻璃样病灶具有治疗作用,而确认磨病灶的基因突变状态,是制定用药决策的关键环节[2, 3]。对此,该团队建立了预测肺腺癌患者磨玻璃病灶EGFR突变状态的影像组学模型,并开发出可即时使用的软件,作为一项无创、且准确快捷的诊断工具,能够有效筛选EGFR突变阳性病灶,显著提高了MPLC患者(磨玻璃病灶)接受EGFR-TKIs治疗的有效率[4]。本次研究证实,PD-1抑制剂对肺癌早期磨玻璃病灶具有一定的治疗效果。对于EGFR突变阴性或不适于EGFR-TKIs治疗的MPLC患者,免疫治疗可以作为潜在的治疗选择,其获益人群有待通过生物标志物进一步筛选。依据患者的EGFR突变状态(阳性或阴性),筛选识别用药受益人群,进行精准治疗,对于MPLC的临床实践具有重要意义。近年来,何建行/梁文华教授团队致力于探索早期肺癌以及MPLC的有效诊治策略,并针对靶向治疗与免疫治疗在MPLC患者中的应用开展了系列研究,致力于实现免创的肺结节/早期肺癌药物治疗模式。参考文献:[1] Cheng B, Li C, Li J, et al. The activity and immune dynamics of PD-1 inhibition on high-risk pulmonary ground glass opacity lesions: insights from a single-arm, phase II trial [J]. Signal Transduction and Targeted Therapy, 2024, 9(1): 93.[2] Cheng B, Li C, Zhao Y, et al. The impact of postoperative EGFR-TKIs treatment on residual GGO lesions after resection for lung cancer [J]. Signal Transduct Target Ther, 2021, 6(1): 73.[3] Cheng B, Deng H, Zhao Y, et al. Management for Residual Ground-Glass Opacity Lesions After Resection of Main Tumor in Multifocal Lung Cancer: A Case Report and Literature Review [J]. Cancer Management and Research, 2021, 13: 977-85.[4] Cheng B, Deng H, Zhao Y, et al. Predicting EGFR mutation status in lung adenocarcinoma presenting as ground-glass opacity: utilizing radiomics model in clinical translation [J]. European Radiology, 2022, 32(9): 5869-79.声明:本文旨在为医疗卫生专业人士传递更多医学信息,不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,信达不推荐任何未获批的药品/适应症使用。
临床结果免疫疗法上市后研究
100 项与 Guangzhou Institute Of Respiratory Health 相关的药物交易
登录后查看更多信息
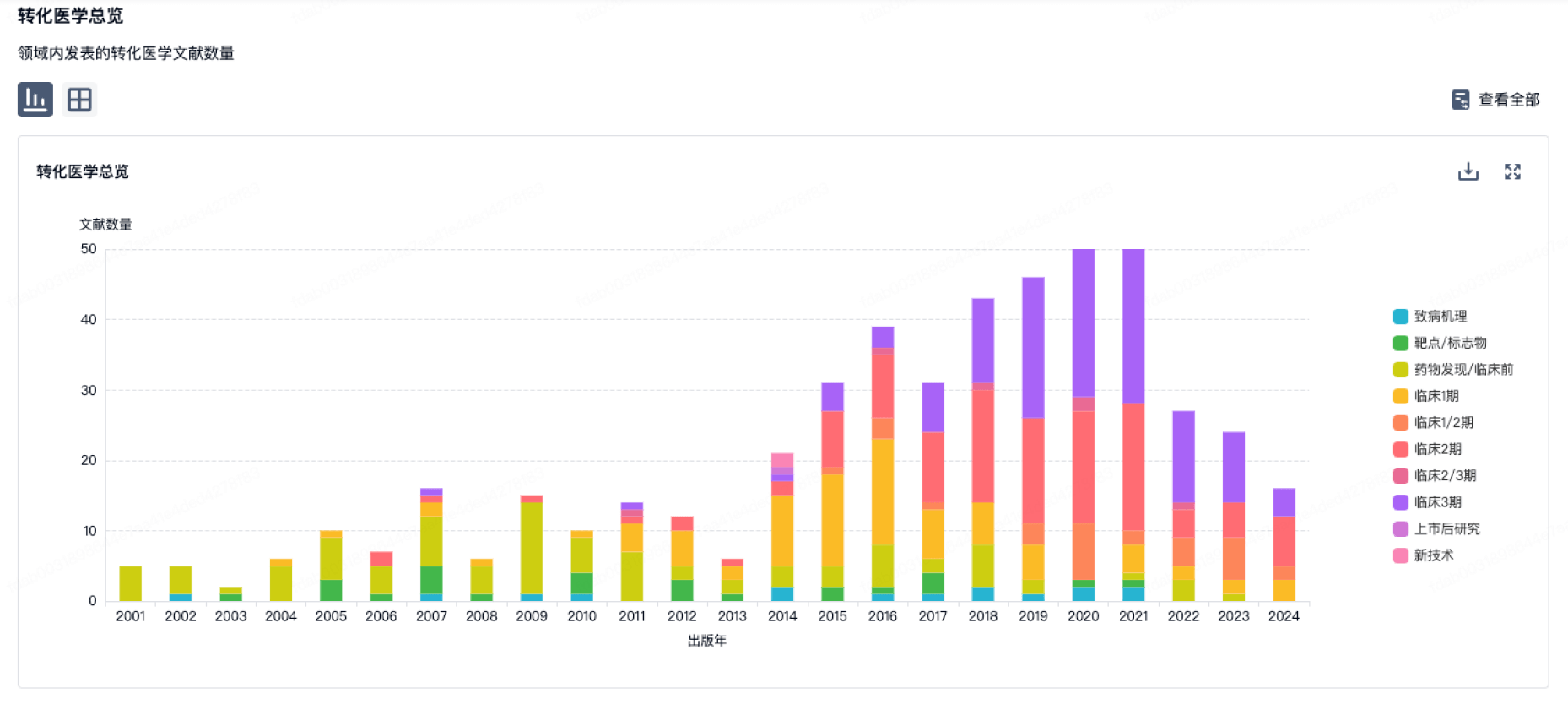
100 项与 Guangzhou Institute Of Respiratory Health 相关的转化医学
登录后查看更多信息
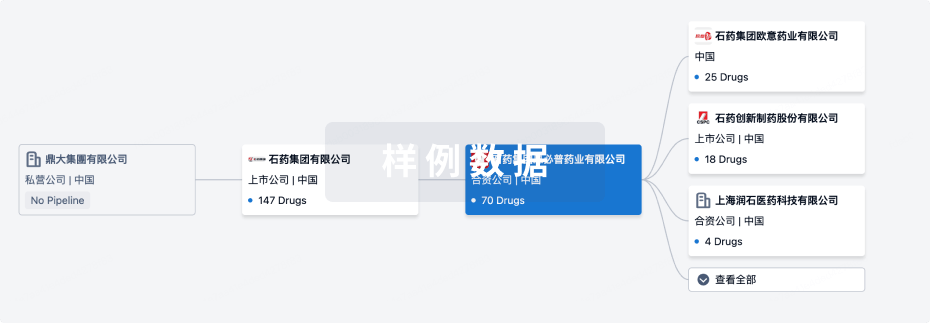
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2024年11月17日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
1
临床2期
登录后查看更多信息
当前项目
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

转化医学
使用我们的转化医学数据加速您的研究。
登录
或
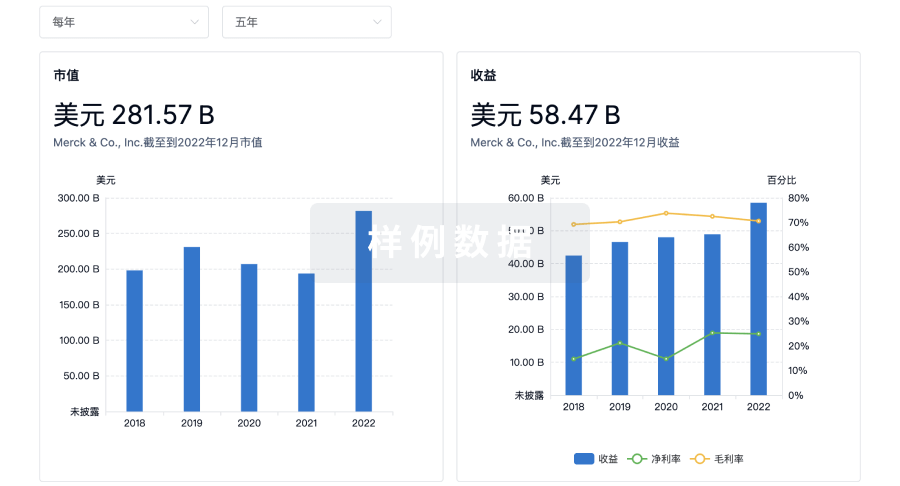
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或

融资
发掘融资趋势以验证和推进您的投资机会。
登录
或

标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用