预约演示
更新于:2025-08-29

Arog Pharmaceuticals, Inc.
更新于:2025-08-29
概览
标签
血液及淋巴系统疾病
肿瘤
小分子化药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| FLT3 x PDGFRs x c-Kit | 1 |
关联
1
项与 Arog Pharmaceuticals, Inc. 相关的药物作用机制 FLT3抑制剂 [+2] |
原研机构 |
在研适应症 |
非在研适应症 |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
18
项与 Arog Pharmaceuticals, Inc. 相关的临床试验NCT03258931
Phase III Randomized Study of Crenolanib Versus Midostaurin Administered Following Induction Chemotherapy and Consolidation Therapy in Newly Diagnosed Subjects With FLT3 Mutated Acute Myeloid Leukemia
A phase III randomized multi-center study designed to compare the efficacy of crenolanib with that of midostaurin when administered following induction chemotherapy, consolidation chemotherapy and bone marrow transplantation in newly diagnosed AML subjects with FLT3 mutation. About 510 subjects will be randomized in a 1:1 ratio to receive either crenolanib in addition to standard first line treatment of AML (chemotherapy and if eligible, transplantation) (arm A) or midostaurin and standard treatment (arm B). Potentially eligible subjects will be registered and tested for the presence of FLT3 mutation. Once the FLT3 mutation status is confirmed and additional eligibility is established, subject will be randomized and enter into the treatment phase.
开始日期2018-08-15 |
申办/合作机构 |
NCT03324243
A Phase II Study of Crenolanib With Fludarabine and Cytarabine in Pediatric Patients With Relapsed/Refractory FLT3-Mutated Acute Myeloid Leukemia
This is a phase II, multicenter, single-arm study to assess the safety and feasibility of combining crenolanib with fludarabine and cytarabine chemotherapy in pediatric patients with relapsed/refractory FLT3-mutated AML. Patients will receive up to two courses of salvage chemotherapy with fludarabine, cytarabine, and crenolanib. Response will be assessed between day 29-43 of each course.
开始日期2018-01-01 |
申办/合作机构 |
NCT03193918
Phase I/Ib Study of Crenolanib With Ramucirumab and Paclitaxel as Second Line Therapy for Advanced Esophagogastric Adenocarcinoma
This is a single-arm phase I/Ib study of crenolanib combined with ramucirumab/paclitaxel as second line therapy for patients with advanced/metastatic adenocarcinoma of the esophagus, GEJ or stomach. Patients will be enrolled in two phases; dose escalation phase and dose expansion phase.
开始日期2017-04-14 |
申办/合作机构 |
100 项与 Arog Pharmaceuticals, Inc. 相关的临床结果
登录后查看更多信息
0 项与 Arog Pharmaceuticals, Inc. 相关的专利(医药)
登录后查看更多信息
5
项与 Arog Pharmaceuticals, Inc. 相关的文献(医药)2021-01-01·Neuro-oncology advances
Phase I study using crenolanib to target PDGFR kinase in children and young adults with newly diagnosed DIPG or recurrent high-grade glioma, including DIPG
Article
作者: Patay, Zoltan ; Li, Xiaoyu ; Stewart, Clinton F ; Onar-Thomas, Arzu ; Zhang, Jinghui ; Gajjar, Amar ; Campagne, Olivia ; Wetmore, Cynthia ; Jain, Vinay ; Merchant, Thomas E ; Broniscer, Alberto ; Chiang, Jason ; Tinkle, Christopher L ; Orr, Brent A ; Baker, Suzanne J ; Huang, Jie
Abstract:
Background:
Platelet-derived growth factor receptor (PDGFR) signaling has been directly implicated in pediatric high-grade gliomagenesis. This study evaluated the safety and tolerability of crenolanib, a potent, selective inhibitor of PDGFR-mediated phosphorylation, in pediatric patients with high-grade glioma (HGG).
Methods:
We used a rolling-6 design to study the maximum tolerated dose (MTD) of once-daily crenolanib administered during and after focal radiation therapy in children with newly diagnosed diffuse intrinsic pontine glioma (DIPG) (stratum A) or with recurrent/progressive HGG (stratum B). Pharmacokinetics were studied during the first cycle at the first dose and at steady state (day 28). Alterations in PDGFRA were assessed by Sanger or exome sequencing and interphase fluorescence in situ hybridization or single nucleotide polymorphism arrays.
Results:
Fifty evaluable patients were enrolled in the 2 strata, and an MTD of 170 mg/m2 was established for both. Dose-limiting toxicities were primarily liver enzyme elevations and hematologic count suppression in both strata. Crenolanib AUC0–48h and CMAX did not differ significantly for crushed versus whole-tablet administration. Overall, PDGFRA alterations were observed in 25% and 30% of patients in stratum A and B, respectively. Neither crenolanib therapy duration nor survival outcomes differed significantly by PDGFRA status, and overall survival of stratum A was similar to that of historical controls.
Conclusions:
Children tolerate crenolanib well at doses slightly higher than the established MTD in adults, with a toxicity spectrum generally similar to that in adults. Studies evaluating intratumoral PDGFR pathway inhibition in biomarker-enriched patients are needed to evaluate further the clinical utility of crenolanib in this population.
2017-10-10·Oncotarget
Crenolanib is a type I tyrosine kinase inhibitor that inhibits mutant KIT D816 isoforms prevalent in systemic mastocytosis and core binding factor leukemia
Article
作者: Haeusser, Lara A. ; Illing, Barbara ; Kampa-Schittenhelm, Kerstin Maria ; Schittenhelm, Marcus Matthias ; Blumenstock, Gunnar ; Pavlovsky, Ashly A. ; Frey, Julia
Activating D816 mutations of the class III receptor tyrosine kinase KIT are associated with the majority of patients with systemic mastocytosis (SM), but also core binding factor (CBF) AML, making KIT mutations attractive therapeutic targets for the treatment of these cancers. Crenolanib is a potent and selective inhibitor of wild-type as well as mutant isoforms of the class III receptor tyrosine kinases FLT3 and PDGFRα/β. Notably, crenolanib inhibits constitutively active mutant-FLT3 isoforms resulting from amino acid substitutions of aspartic acid at codon 835, which is homologous to codon 816 in the KIT gene - suggesting sensitivity against mutant-KIT D816 isoforms as well. Here we demonstrate that crenolanib targets KIT D816 in SM and CBF AML models: crenolanib inhibits cellular proliferation and initiates apoptosis of mastocytosis cell lines expressing these mutations. Target-specificity was confirmed using an isogenic cell model. In addition, we demonstrate that KIT D816 mutations are targetable with clinically achievable doses of crenolanib. Further, a rationale to combine cladribine (2-CDA), the therapeutic standard in SM, with crenolanib is provided. In conclusion, we demonstrate that crenolanib is an inhibitor of mutant-KIT D816 isoforms at clinically achievable concentrations, and thus may be a potential treatment for SM and CBF AML as a monotherapy or in combination approaches.
2015-08-01·Gastroenterology1区 · 医学
Platelet-Derived Growth Factor Receptor-α Regulates Proliferation of Gastrointestinal Stromal Tumor Cells With Mutations in KIT by Stabilizing ETV1
1区 · 医学
Article
作者: Bardsley, Michael R ; Ordog, Tamas ; Ramachandran, Abhijit ; Gajdos, Gabriella B ; Tang, Chih-Min ; Hayashi, Yujiro ; Gibbons, Simon J ; Milosavljevic, Srdjan ; Farrugia, Gianrico ; Bingener-Casey, Juliane ; Fletcher, Jonathan A ; Sicklick, Jason K ; Reid-Lombardo, K Marie ; Rubin, Brian P ; Choi, Kyoung Moo ; Taguchi, Takahiro ; Toyomasu, Yoshitaka ; Kendrick, Michael L ; Gupta, Anu
BACKGROUND & AIMS:
In gastrointestinal muscles, v-kit Hardy-Zuckerman 4 feline sarcoma viral oncogene homolog (KIT) is predominantly expressed by interstitial cells of Cajal (ICC) and platelet-derived growth factor receptor-α (PDGFRA) polypeptide is expressed by so-called fibroblast-like cells. KIT and PDGFRA have been reported to be coexpressed in ICC precursors and gastrointestinal stromal tumors (GISTs), which originate from the ICC lineage. PDGFRA signaling has been proposed to stimulate growth of GISTs that express mutant KIT, but the effects and mechanisms of selective blockade of PDGFRA are unclear. We investigated whether inhibiting PDGFRA could reduce proliferation of GIST cells with mutant KIT via effects on the KIT-dependent transcription factor ETV1.
METHODS:
We studied 53 gastric, small intestinal, rectal, or abdominal GISTs collected immediately after surgery or archived as fixed blocks at the Mayo Clinic and University of California, San Diego. In human GIST cells carrying imatinib-sensitive and imatinib-resistant mutations in KIT, PDGFRA was reduced by RNA interference (knockdown) or inhibited with crenolanib besylate (a selective inhibitor of PDGFRA and PDGFRB). Mouse ICC precursors were retrovirally transduced to overexpress wild-type Kit. Cell proliferation was analyzed by methyltetrazolium, 5-ethynyl-2'-deoxyuridine incorporation, and Ki-67 immunofluorescence assays; we also analyzed growth of xenograft tumors in mice. Gastric ICC and ICC precursors, and their PDGFRA(+) subsets, were analyzed by flow cytometry and immunohistochemistry in wild-type, Kit(+/copGFP), Pdgfra(+/eGFP), and NOD/ShiLtJ mice. Immunoblots were used to quantify protein expression and phosphorylation.
RESULTS:
KIT and PDGFRA were coexpressed in 3%-5% of mouse ICC, 35%-44% of ICC precursors, and most human GIST samples and cell lines. PDGFRA knockdown or inhibition with crenolanib efficiently reduced proliferation of imatinib-sensitive and imatinib-resistant KIT(+)ETV1(+)PDGFRA(+) GIST cells (50% maximal inhibitory concentration = 5-32 nM), but not of cells lacking KIT, ETV1, or PDGFRA (50% maximal inhibitory concentration >230 nM). Crenolanib inhibited phosphorylation of PDGFRA and PDGFRB, but not KIT. However, Kit overexpression sensitized mouse ICC precursors to crenolanib. ETV1 knockdown reduced KIT expression and GIST proliferation. Crenolanib down-regulated ETV1 by inhibiting extracellular-signal-regulated kinase (ERK)-dependent stabilization of ETV1 protein and also reduced expression of KIT and PDGFRA.
CONCLUSIONS:
In KIT-mutant GIST, inhibition of PDGFRA disrupts a KIT-ERK-ETV1-KIT signaling loop by inhibiting ERK activation. The PDGFRA inhibitor crenolanib might be used to treat patients with imatinib-resistant, KIT-mutant GIST.
5
项与 Arog Pharmaceuticals, Inc. 相关的新闻(医药)2025-04-08
With its ability to specifically inhibit the mutant IDH1 enzyme, TIBSOVO addresses an unmet need in personalized cancer treatment, offering new hope for patients with limited options. As clinical evidence continues to support its efficacy and safety, TIBSOVO is positioned for strong growth in the oncology market, especially with expanding indications and global market penetration.
LAS VEGAS, April 8, 2025 /PRNewswire/ -- DelveInsight's "
TIBSOVO Market Size, Forecast, and Market Insight Report" highlights the details around TIBSOVO, the first and only targeted therapy approved for patients with previously treated IDH1-mutated cholangiocarcinoma. The report provides product descriptions, patent details, and competitor products (marketed and emerging therapies) of TIBSOVO. The report also highlights the historical and forecasted sales from 2020 to 2034 segmented into 7MM [the United States, the EU4 (Germany, France, Italy, and Spain), the United Kingdom, and Japan].
Servier's TIBSOVO (ivosidenib) Overview
TIBSOVO (ivosidenib) is a small molecule developed by Servier, acts as an isocitrate dehydrogenase-1 (IDH1) inhibitor. It is indicated for patients with a susceptible IDH1 mutation, which is identified through an FDA-approved test.
Currently, TIBSOVO is approved for the treatment of newly diagnosed acute myeloid leukemia (AML), relapsed or refractory AML, relapsed or refractory myelodysplastic syndromes (MDS), and locally advanced or metastatic cholangiocarcinoma.
According to Servier's pipeline, TIBSOVO is also being actively investigated for a range of additional indications, with key areas of exploration including solid tumors and hematological malignancies.
Learn more about TIBSOVO projected market size for AML, cholangiocarcinoma, and MDS @
TIBSOVO Market Potential
The oncology market has experienced significant growth in recent years, driven by advances in cancer research, the development of targeted therapies, and the increasing global prevalence of cancer. As the second-leading cause of death worldwide, cancer continues to pose a major public health challenge, creating a substantial demand for innovative treatments. The market is marked by a shift toward personalized medicine, where therapies are tailored to an individual's genetic profile, allowing for more effective and less toxic treatments. Immunotherapies, such as checkpoint inhibitors, CAR-T cell therapies, and oncolytic virus therapies, are at the forefront of these advancements, offering new hope to patients with previously untreatable cancers.
Moreover, the oncology market is expanding due to the growing adoption of precision oncology and molecular diagnostics, which enable earlier and more accurate detection of cancer. This has led to increased investments in research and development, especially in areas like liquid biopsies, companion diagnostics, and next-generation sequencing. The demand for more effective and accessible cancer treatments is fueling innovation in both the pharmaceutical and biotechnology sectors, with numerous new drugs and therapies entering clinical trials and moving toward commercialization. As a result, the oncology market is poised to continue growing, with significant opportunities for breakthrough therapies in immuno-oncology, targeted treatments, and gene therapies.
DelveInsight has expertise in the oncology market with an experienced team handling the oncology domain proficiently. DelveInsight has released a series of epidemiology-based market reports on
Acute Myeloid Leukemia, Cholangiocarcinoma, and Myelodysplastic Syndrome. These reports include a comprehensive understanding of current treatment practices, emerging drugs, market share of individual therapies, and current and forecasted market size from 2020 to 2034, segmented into 7MM [the United States, the EU4 (Germany, France, Italy, and Spain), the United Kingdom, and Japan].
Gain deeper insights into these diseases with a customized report tailored to your needs.
Connect with us today—our experts are ready to assist you!
Emerging Competitors of TIBSOVO
TIBSOVO faces significant competition in the newly diagnosed AML market from several alternative treatments. Oral therapies like
VENCLEXTA (venetoclax), which inhibits BCL-2, and
DAURISMO (glasdegib), which targets the hedgehog pathway, present strong contenders. Additionally, emerging therapies such as
Lisaftoclax (Ascentage Pharma), another BCL-2 inhibitor, and
gilteritinib (Astellas), a kinase inhibitor, are expected to further challenge TIBSOVO in the newly diagnosed AML space.
In the R/R AML market, TIBSOVO competes with several therapies, including
XOSPATA (gilteritinib),
IDHIFA (enasidenib), and others. Emerging therapies such as
Ziftomenib (Kura Oncology) and RVU-120 (Ryvu Therapeutics) are also expected to compete with TIBSOVO upon their approval. Ziftomenib, a small molecule developed by Kura Oncology, is currently in Phase I/II trials.
In the relapsed/refractory (R/R) MDS market, TIBSOVO faces competition from therapies such as
RYTELO (Imetelstat), an IV injection that inhibits oligonucleotide telomerase, and
REBLOZYL (Luspatercept), a subcutaneous injection, among other treatment options.
In the metastatic cholangiocarcinoma market, TIBSOVO faces relatively less competition, as there are few approved therapies. One such competitor is
PEMAZYRE (pemigatinib), a kinase inhibitor that was approved in the US in 2020 and in Europe in 2021. Whereas, Tyra Biosciences' TYRA-200, an FGFR1/2/3 inhibitor, is in phase I stage of development that might be a threat to TIBSOVO one approved.
To know more about the number of competing drugs in development, visit @
TIBSOVO Market Positioning Compared to Other Drugs
Key Developmental Activities of TIBSOVO
In
October 2023,
Servier announced that the FDA has approved TIBSOVO (ivosidenib tablets) for the treatment of IDH1-mutated R/R MDS.
In
May 2023, Servier announced that the European Commission has approved TIBSOVO as a targeted therapy in two indications: in combination with azacitidine for the treatment of adult patients with newly diagnosed AML with an isocitrate dehydrogenase-1 R132 mutation who are not eligible to receive standard induction chemotherapy; as well as in monotherapy for the treatment of adult patients with locally advanced or metastatic cholangiocarcinoma with an IDH1 R132 mutation who were previously treated by at least one prior line of systemic therapy.
In
May 2022, Servier announced FDA approval of TIBSOVO (ivosidenib tablets) in combination with azacitidine for patients with newly diagnosed IDH1-mutated acute myeloid leukemia.
In
August 2021, Servier announced FDA approval for TIBSOVO (ivosidenib tablets) for the treatment of adult patients with previously treated, locally advanced, or metastatic cholangiocarcinoma with an IDH1 mutation as detected by an FDA-approved test. TIBSOVO is the first and only targeted therapy approved for patients with previously treated IDH1-mutated cholangiocarcinoma.
In
May 2019, Agios announced FDA approval of TIBSOVO (ivosidenib tablets) as monotherapy for newly diagnosed adult patients with IDH1 mutant acute myeloid leukemia not eligible for intensive chemotherapy.
In
July 2018, the FDA approved TIBSOVO (ivosidenib) for relapsed or refractory acute myeloid leukemia with an idh1 mutation.
In
February 2018, the FDA accepted a new drug application and granted priority review for ivosidenib in relapsed or refractory AML with an IDH1 mutation.
In
December 2017, Agios submitted an NDA to the FDA for ivosidenib for the treatment of patients with relapsed/refractory aml and an IDH1 mutation.
TIBSOVO Patent Details
TIBSOVO is a drug owned by Servier Pharmaceuticals. Currently, it is protected by 10 Orange book-listed patents filed from 2018 to 2023, out of which none have expired yet. It is also protected by ODE exclusivity for various indications.
Discover how TIBSOVO is shaping the blood cancer treatment landscape @
TIBSOVO Side Effects
TIBSOVO Market Dynamics
In recent years, the therapeutic landscape has undergone significant changes, with promising approaches including
immunotherapy, chemotherapy combined with targeted treatments, and the regulation of immune checkpoint-mediated signaling pathways. One such treatment,
Ivosidenib, works by inducing the bone marrow to develop normal blood cells, helping to reduce the frequency of blood transfusions.
Investment in the
research and development of drugs has surged, contributing to a rich pipeline and forecasting promising opportunities in the treatment markets for AML and cholangiocarcinomas. Therapies like TIBSOVO have the potential to capture market attention due to their
efficacy and innovation.
As
healthcare spending continues to rise globally, the pharmaceutical market is expected to expand, providing greater opportunities for
market penetration by manufacturers and facilitating the development and distribution of new treatments.
Despite progress in cancer treatment,
significant gaps remain in understanding the full process that governs carcinogenesis and resistance to treatments, particularly in cancers like acute myeloid leukemia (AML). This highlights the
need for more advanced research to address these challenges. Additionally, the
limited biomarker testing for patients with the IDH1 mutation restricts the targeted patient pool, posing a challenge for therapies like TIBSOVO to achieve their expected market share.
The
increasing competition from emerging therapies, such as KEYTRUDA (pembrolizumab), IMFINZI (durvalumab), and the combination of Azacitidine + Venetoclax, further intensifies the pressure on TIBSOVO. Moreover, the
difficulty in obtaining sufficient patient pools and
diagnostic samples during disease recurrence presents significant hurdles to the effective development of translational research, potentially slowing progress in optimizing treatments.
Dive deeper to get more insight into TIBSOVO's strengths & weaknesses relative to competitors @
TIBSOVO Market Drug Report
Table of Contents
Related Reports
Acute Myeloid Leukemia Market
Acute Myeloid Leukemia Market Insights, Epidemiology, and Market Forecast – 2034 report deliver an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key AML companies including
Agios Pharmaceuticals, Abbvie, Jazz Pharmaceuticals, Astellas Pharma, Pfizer, Novartis Oncology, Daiichi Sankyo, AstraZeneca, Astex Pharmaceuticals, Inc., Chimerix, Takeda, Rafael Pharmaceuticals Inc., Delta-Fly Pharma, GlycoMimetics Incorporated, BerGenBio ASA, MacroGenics, Syndax Pharmaceuticals, Arog Pharmaceuticals, Forma Therapeutics, Sellas Life Sciences Group, Actinium Pharmaceuticals, Clear Creek Bio Inc., CellCentric Ltd., Biosight Ltd., Astex Pharmaceuticals, Inc., Curis, Inc., NexImmune Inc., Immunomedics, Inc., Sumitomo Dainippon Pharma Co., Ltd., Incyte Corporation, Aprea Therapeutics, Immunicum, DCPrime BV, GT Biopharma, Inc., Hanmi Pharmaceutical Company Limited, Cardiff Oncology, Bio-Path Holdings, Actinium Pharmaceuticals, Aptevo Therapeutics, Synimmune GmbH, GEMoaB Monoclonals, ImmunoGen, Inc., AGC Biologics S.p.A., Precigen, Inc., Novartis Pharmaceuticals, Xencor, Inc., Novartis, Celgene, Bristol Myers Squibb, among others.
Relapsed/Refractory Acute Myeloid Leukemia Market
Relapsed/Refractory Acute Myeloid Leukemia Market Insights, Epidemiology, and Market Forecast – 2034 report deliver an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key R/R AML companies including
Agios Pharmaceuticals, Abbvie, Jazz Pharmaceuticals, Astellas Pharma, Pfizer, Novartis Oncology, Daiichi Sankyo, AstraZeneca, Astex Pharmaceuticals, Inc., Chimerix, Takeda, Rafael Pharmaceuticals Inc., Delta-Fly Pharma, GlycoMimetics Incorporated, BerGenBio ASA, MacroGenics, Syndax Pharmaceuticals, Arog Pharmaceuticals, Forma Therapeutics, Sellas Life Sciences Group, Actinium Pharmaceuticals, Clear Creek Bio Inc., CellCentric Ltd., Biosight Ltd., Astex Pharmaceuticals, Inc., Curis, Inc., NexImmune Inc., Immunomedics, Inc., Sumitomo Dainippon Pharma Co., Ltd., Incyte Corporation, Aprea Therapeutics, Immunicum, DCPrime BV, GT Biopharma, Inc., Hanmi Pharmaceutical Company Limited, Cardiff Oncology, Bio-Path Holdings, Actinium Pharmaceuticals, Aptevo Therapeutics, Synimmune GmbH, GEMoaB Monoclonals, ImmunoGen, Inc., AGC Biologics S.p.A., Precigen, Inc., Novartis Pharmaceuticals, Xencor, Inc., Novartis, Celgene, Bristol Myers Squibb, among others.
Myelodysplastic Syndrome Market
Myelodysplastic Syndrome Market Insight, Epidemiology, and Market Forecast – 2034 report delivers an in-depth understanding of market trends, market drivers, market barriers, and key MDS companies such as
Bristol-Myers Squibb, Astex Pharmaceutical, Taiho Oncology, Fibrogen, AbbVie, Gilead Sciences, Novartis, Syros Pharmaceuticals, Takeda, Pfizer, Geron Corporation, Karyopharm Therapeutics, Antengene Corporation, BerGenBio ASA, Jazz Pharmaceuticals, Aprea Therapeutics, Sanofi, Medac, among others.
Cholangiocarcinoma Market
Cholangiocarcinoma Market Insight, Epidemiology, and Market Forecast – 2034 report delivers an in-depth understanding of market trends, market drivers, market barriers, and key cholangiocarcinoma companies such as
AstraZeneca, Decalth Systems, Basilea Pharmaceutica, Taiho Oncology, Eisai Pharmaceuticals, TransThera Sciences, Incyte Corporation, Roche, Agios Pharmaceuticals, Servier Pharma, among others.
About DelveInsight
DelveInsight is a leading Business Consultant and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve
.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
上市批准免疫疗法临床1期优先审批
2024-12-04
A case study on how a leading pharma company in hematology turned to DelveInsight for long-term competitive intelligence support. DelveInsight provided an in-depth analysis of competitive activity in key hematological malignancies, helping the company stay ahead of the competition.
LAS VEGAS, Dec. 4, 2024 /PRNewswire/ -- DelveInsight, a leader in healthcare competitive intelligence and consulting, released a case study on Competitive Intelligence in the Hematology Domain. A Europe-based client approached DelveInsight to evaluate a long-term partnership for insights supporting their clinical, commercial, and launch strategies for a novel oncology product targeting
acute myeloid leukemia (AML),
multiple myeloma, and
acute lymphoblastic leukemia (ALL). The client sought detailed intelligence on competitive activity, class-wise market trends, launch estimates in countries of interest, and regulatory landscapes to inform their development and commercialization plans. An additional request for the segregation of mutation/protein expression-specific therapies was also taken into consideration.
DelveInsight provided timely, in-depth analysis of the competitive landscape, emerging therapies, and regulatory situations across multiple countries. This enabled the client to make informed decisions on clinical development, market positioning, and commercialization, helping them stay ahead of the competition in the hematology space.
With hundreds of thousands of new cases diagnosed annually, hematologic cancers, such as
acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML), and multiple myeloma, among others present a serious global health challenge while also opening doors for breakthroughs in targeted and personalized treatments. These cancers affect the blood, bone marrow, and lymphatic system, and often require aggressive therapies due to their rapid progression and complex nature. AML and ALL are particularly aggressive, with AML being one of the most common forms of leukemia in adults and ALL affecting both children and adults.
Innovations in precision medicine and immunotherapy are transforming hematology, with CAR-T therapies showing promise for leukemias and CELMODs, like Iberdomide, emerging as potential successors to REVLIMID for multiple myeloma. Bristol Myers Squibb's collaboration with Karyopharm on mezigdomide highlights the growing focus on CELMODs. Additionally, FDA-approved therapies like CARVYKTI and TECVAYLI, along with ongoing advancements in bispecific antibodies and proteasome inhibitors, are reshaping the multiple myeloma treatment landscape, despite safety, cost, and manufacturing challenges. The market is rapidly evolving, with new therapies continually entering the pipeline.
Several companies, including
Bristol Myers Squibb, Celgene, Arcellx, Novartis, Regeneron Pharmaceuticals, Cartesian Therapeutics, Heidelberg Pharma, BeiGene, CARsgen Therapeutics, C4 Therapeutics, AbbVie (TeneoOne), Roche (Genentech), Pfizer, Agios Pharmaceuticals, Jazz Pharmaceuticals, Astellas Pharma, Novartis Oncology, Daiichi Sankyo, AstraZeneca/Astex Pharmaceuticals, Chimerix, Takeda, Rafael Pharmaceuticals Inc., Delta-Fly Pharma, GlycoMimetics Incorporated, BerGenBio ASA, MacroGenics, Syndax Pharmaceuticals, Arog Pharmaceuticals, Forma Therapeutics, Sellas Life Sciences Group, Autolus Therapeutics, Cellectis, Wugen, Servier, Allogene, and
Precision BioSciences, are currently advancing the therapeutic landscape for hematological disorders.
As research and innovation progress, there is renewed hope for improving survival rates and enhancing the quality of life for those affected by these challenging diagnoses.
DelveInsight's Methodology for Competitive Intelligence in the Hematology Domain helped the client by:
Comparative Analyses: Evaluating competitor products to identify strengths, weaknesses, and market positioning, enabling the client to understand where their product stands relative to competitors along with identifying the patient segment with high unmet need
KOL Insights: Gathering opinions from Key Opinion Leaders (KOLs) on clinical development strategies, client's product acceptability scenarios, data presentation, probable uptake of their asset,, providing valuable perspectives to refine the client's approach.
Current Treatment Paradigms: Analyzing existing treatment approaches to identify market trends, gaps, and unmet needs, helping the client position their product effectively in the market.
In-depth Competitive Benchmarking: Assessing competitors' commercial launch preparedness, patient awareness campaigns, and pricing strategies to inform the client's product's market entry and competitive strategy.
Market Intelligence: Providing insights into competitors' marketing, sales, and patient engagement approaches, guiding the client's commercialization and go-to-market strategies.
Clinical Development Trends: Evaluating clinical trial timelines and strategies, tracking phase shifts in terms of probability of their entry into the higher phase, and analyzing trial data to anticipate future market shifts and inform strategic decision-making.
Pricing and Access Strategies: Analyzing competitor pricing models and access strategies, allowing the client to make informed decisions on pricing and reimbursement for their product.
Request a proposal to see how
DelveInsight's Competitive Intelligence services
can support your long-term strategic insights.
How DelveInsight's In-Depth Competitive Intelligence in Hematology Helped Clients Stay Ahead in the Market
Periodic Competitive Inputs: Provided regular updates on competitor activities, keeping the client informed of market shifts.
Enhanced Market Awareness: Delivered ongoing insights into competitor strategies, enabling quick adaptation to market changes.
Short-Term Strategies: Developed actionable strategies for immediate response to competitor moves.
Counter-Messaging Design: Assisted in crafting counter-messaging strategies to address competitor claims and strengthen brand positioning.
Positioning Refinement: Helped refine product positioning to gain a competitive advantage.
Promotional Strategy Support: Offered recommendations on promotional tactics to boost market presence and attract key audiences.
Why Choose DelveInsight?
DelveInsight offers tailored, comprehensive competitive intelligence to keep your hematology product developmental and commercial strategy a step ahead. With expertise in AML, Multiple Myeloma, ALL, and other hematology domains, we support your clinical, commercial, and launch strategies with insights that matter.
What Sets Us Apart:
Timely Intelligence: Consistent, real-time updates on competitor activities, clinical shifts, and regulatory changes, ensuring you're never caught off-guard.
Expert Analysis: From comparative assessments to pricing benchmarks, we provide actionable data that sharpens your positioning.
Strategic Edge: We don't just offer data—we deliver strategic recommendations for counter-messaging, promotional tactics, and market adaptation.
Choosing DelveInsight means partnering with a team dedicated to turning competitive intelligence into growth and success for your business.
Transform your business with our case study.
Schedule a call
with our DelveInsight Business Development expert today!
Conference Coverage Services
: DelveInsight's Conference Coverage Services offer a thorough analysis of outcomes from major events like ASH, EHA, AACR, ESMO, ASCO, and others. This detailed examination provides businesses with essential insights for competitive intelligence and market trend forecasting, supporting the formulation of future strategies.
Competitive Intelligence Services: DelveInsight's competitive intelligence services provide real-time, accurate insights across the pharmaceutical, life sciences, and medical diagnostics sectors, helping clients stay ahead in a dynamic market. With over 100 years of combined experience, our experts deliver actionable strategic insights, backed by robust research methodologies, to support critical business decisions and create a competitive advantage for our clients.
Hematology Pipeline Assessment: Our hematology pipeline evaluation offers a comprehensive overview of cancer treatment options, clinical trials, and key areas within the hematological disorders field, all summarized in an accessible report format. The hematology-focused reports, available in our Report Store, provide in-depth insights into treatment strategies, mechanisms of action (MoAs), drug components, and launch plans for therapies in the late stages of development. This assessment enhances understanding of their launch timelines and strategic initiatives.
R&D Analysis: Our skilled research and development analyst specializes in the complexities of hematology, offering essential insights and advice to clients aiming to advance in hematological research and development. They utilize a methodical assessment approach, aligned with industry norms, to track the progress of each hematology drug in both pre-clinical and clinical stages. DelveInsight's comprehensive hematological reports are crafted to reduce uncertainties and highlight overlooked areas, providing organizations with timely and strategic intelligence.
About DelveInsight
DelveInsight is a leading Business Consultant and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve
.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED

免疫疗法ASH会议
2023-06-27
Ruxolitinib extinguished arrhythmias in three different types of mouse models, including one condition that's often resistant to treatment.
Biotechs have been investigating the therapeutic potential of drugs called calcium/calmodulin-dependent protein kinase II inhibitors, or CaMKII inhibitors, for at least a decade. But while the drugs have shown some promise in preclinical and early-stage clinical trials, questions remain about whether they have deleterious off-target effects on the brain.
Now, the results of a new study published June 21 in Science Translational Medicine by researchers from the University of Chicago and Johns Hopkins University may begin to put some of those concerns to rest. They also suggest that the cancer drug ruxolitinib, a JAK1/2 inhibitor commercialized by Novartis as Jakavi, could be a viable treatment against atrial fibrillation and a dangerous pediatric cardiac arrhythmia called catecholaminergic polymorphic ventricular tachycardia (CPVT).
“Our study was able to show for the first time that you can actually block the ‘bad’ CaMKII in the heart and completely spare the brain version of CaMKII with a small molecule, so you get the benefits without the side effects,” first author Oscar Reyes Gaido, an M.D.-Ph.D. student in the Johns Hopkins lab of Mark Anderson, M.D., Ph.D., told Fierce Biotech Research in an interview. “And we found that ruxolitinib behaves that way—it doesn’t cross into the brain very well, so this could be a really good repurposing candidate.”
While CaMKII, an enzyme, has some functions in the heart, experiments in animals have shown that it isn’t essential, Reyes Gaido and his team noted in their paper. On top of that, there’s increasingly abundant evidence that excessive CaMKII activity contributes to heart disease and arrhythmias, as the team explained in a January 2023 review article.
There have been but a handful of attempts to develop a CaMKII inhibitor for heart disease, and so far, such drugs have failed to translate from preclinical models to humans. Scientists are only just learning how many different conditions may be precipitated by excess CaMKII activity, so it makes sense that innovation on the front hasn’t yet picked up. But there’s another reason for stifled progress, too: There are four different isoforms, or types, of CaMKII found throughout the body. Hitting the wrong one—or all of them—could cause serious harm.
“They basically look identical, so it’s really challenging to inhibit one version without inhibiting all four,” Reyes Gaido explained. “That’s kept a lot of people from even trying.”
Given the inherent difficulty of developing a new CaMKII inhibitor, the Anderson lab wondered whether any drugs already approved by the U.S. FDA might have activity against the molecule. Their proven safety profile would mean the toxicity hurdle had already been surmounted, and they could potentially be fast-tracked to clinical trials.
“If we start with only molecules that are safe for humans, then you’ve completely eliminated that one deal breaker that all these other molecules have fallen to,” Reyes Gaido said.
But first, the researchers would need a better way to visualize the effects of the drugs on the enzyme’s activity. To that end, Reyes Gaido developed what’s known as a reporter molecule that could enable the researchers to monitor CaMKII levels in cells. Using a jellyfish-derived protein called green fluorescent protein—one that emits green light, just as it sounds—he created CaMKII Activity Reporter, or CaMKAR. The reporter molecule is injected into the tissue being studied, where it glows bright green whenever CaMKII is activated.
The team’s experiments showed CaMKAR to be far more sensitive to CaMKII levels than other biosensors used by the industry. It could detect CaMKII activity directly, rather than relying on proxy signals. That would be vital for figuring out which drugs were truly efficacious against CaMKII itself and weren’t instead targeting similar molecules, a problem that might explain why earlier inhibitors that seemed promising in preclinical studies failed to pan out in clinical trials. It would also lower the cost of high-throughput screening, as the researchers could draw conclusions from a smaller number of cells.
Using CaMKAR, the researchers analyzed how 4,475 different FDA-approved drugs affected CaMKII levels in human heart cells. They found five: baricitinib, a JAK1/2 inhibitor commercialized by Lilly for rheumatoid arthritis as Olumiant; the CK2 inhibitor silmitasertib, from Senhwa Biosciences, which has orphan-drug status for biliary tract cancer; crenolanib, a tyrosine kinase inhibitor by Arog Pharmaceuticals that was fast-tracked by the FDA in 2017 for acute myeloid leukemia; Lilly’s breast cancer drug abemaciclib, trade name Verzenio; and ruxolitinib.
Out of the five hits, ruxolitinib was the most potent CaMKII inhibitor. To see whether it had efficacy in the context of arrhythmia, the team first looked at whether it could hinder the enzyme in cells with a genetic mutation that caused CPVT. Seeing positive results, they moved to testing the drug in a mouse model of the same condition. Ten minutes after injecting the mice with ruxolitinib, CaMKII levels plunged and the arrhythmia was extinguished.
“It was surprising how well this drug worked,” Reyes Gaido said. “We could see CaMKII activity go to basically zero in 10 minutes, which was quite striking.”
The researchers saw similar results in two mouse models of acquired afib. Hyperglycemic mice with different forms of arrhythmia were given the same dose of ruxolitinib as the CPVT models. Ten minutes later, the arrhythmia could no longer be induced in one model and its frequency had fallen from 95% to 33% of heartbeats in the other.
But did the benefits come at the cost of cognition? To find out, the researchers ran mice through various types of learning and memory tests after giving them a single dose of ruxolitinib. They also ran longer studies where mice received daily doses of the drug before being trained on how to get through a maze, which would show any impacts on long-term spatial memory formation. The treated mice performed just as well as the control animals.
One concern going forward is that while ruxolitinib may not damage the brain, it does have known side effects including thrombocytopenia, a condition where blood platelets are too low. But for patients with conditions like CPVT—where as many as 30% of patients are resistant to treatment, and a full 31% die before reaching age 30—the benefits may outweigh the downsides.
Editor's note: This story has been updated to clarify a comment from Oscar Reyes Gaido.
孤儿药
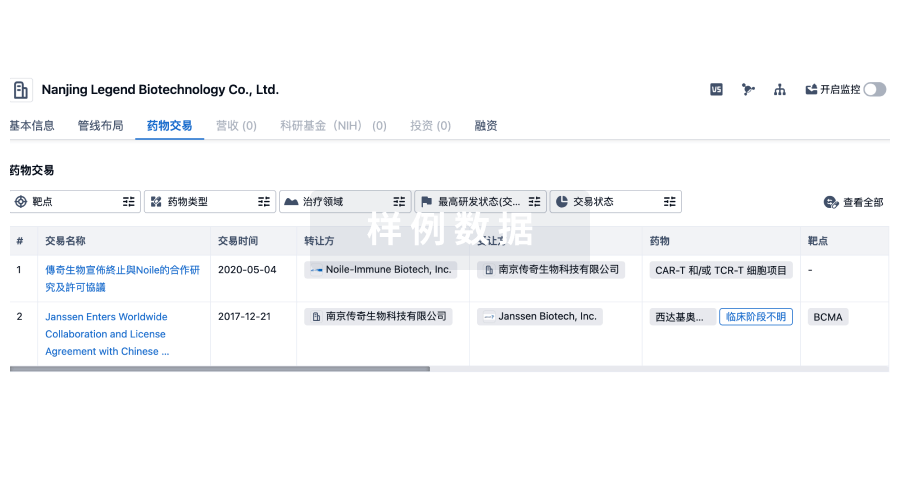
100 项与 Arog Pharmaceuticals, Inc. 相关的药物交易
登录后查看更多信息
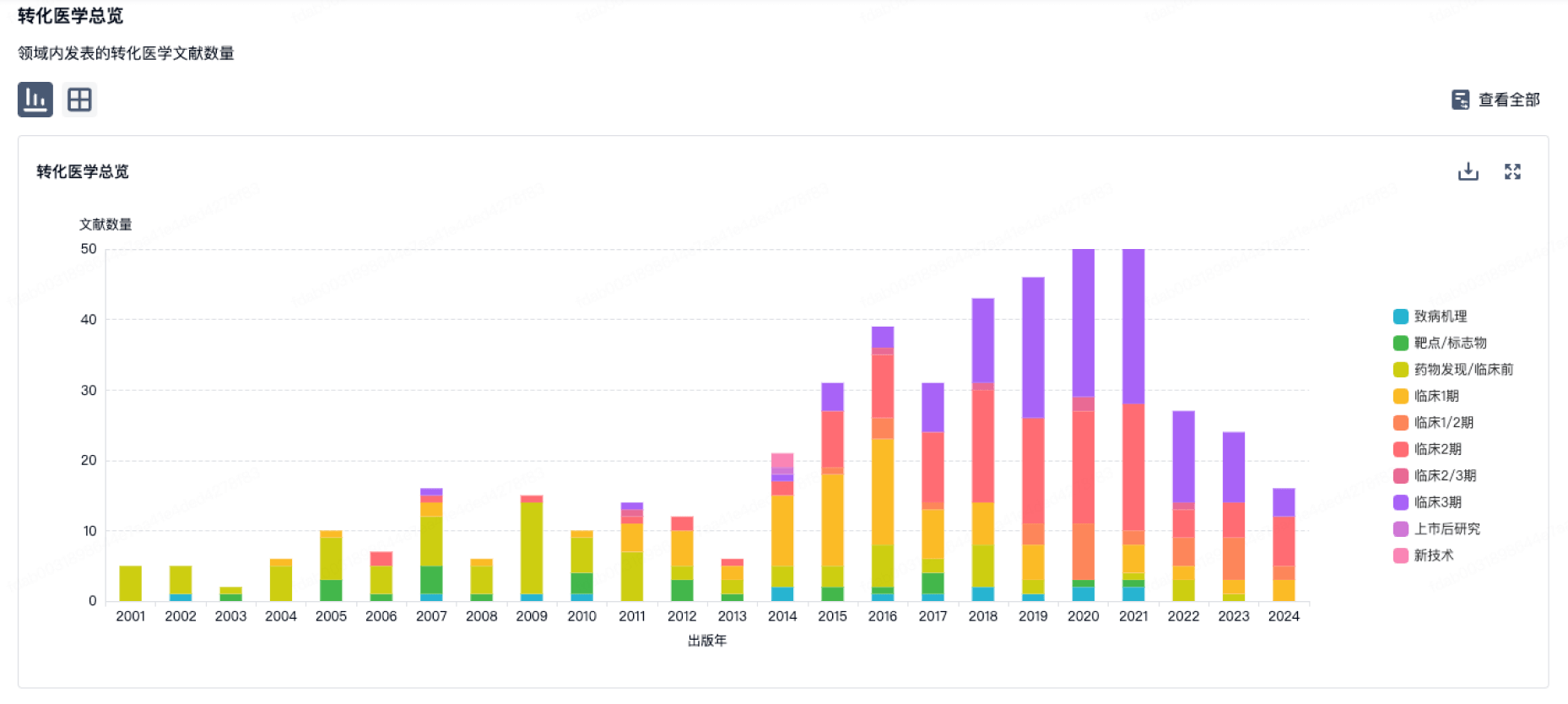
100 项与 Arog Pharmaceuticals, Inc. 相关的转化医学
登录后查看更多信息
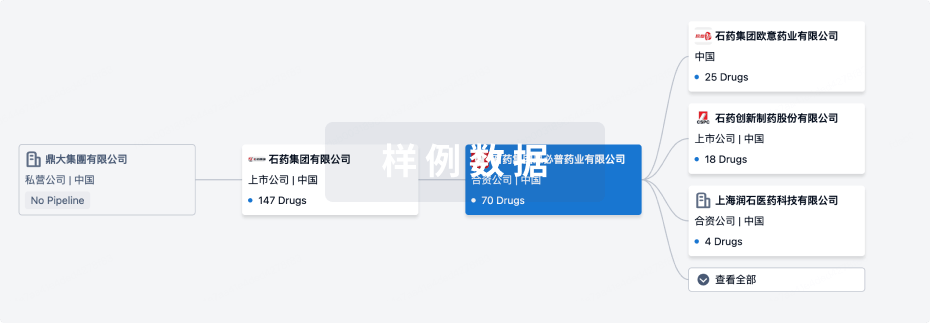
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年09月01日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床3期
1
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
苯磺酸克莱拉尼 ( FLT3 x PDGFRs x c-Kit ) | PDGFRA D842V突变胃肠道间质瘤 更多 | 无进展 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
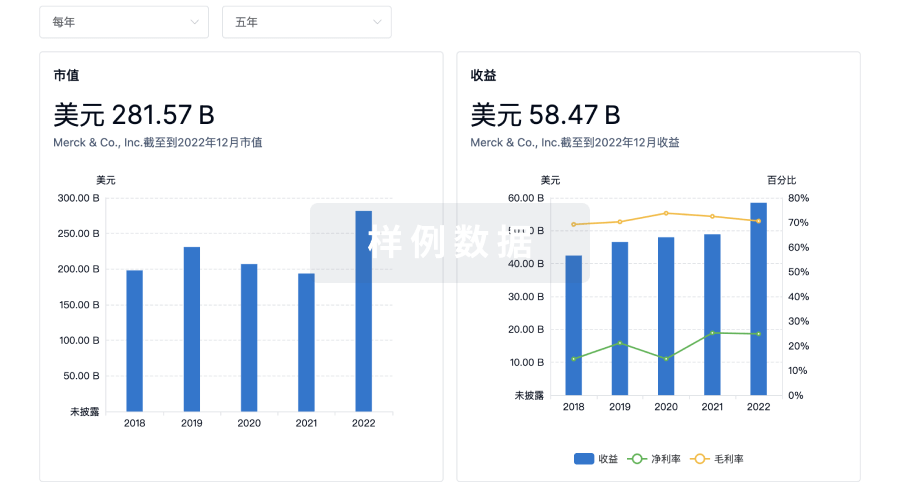
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
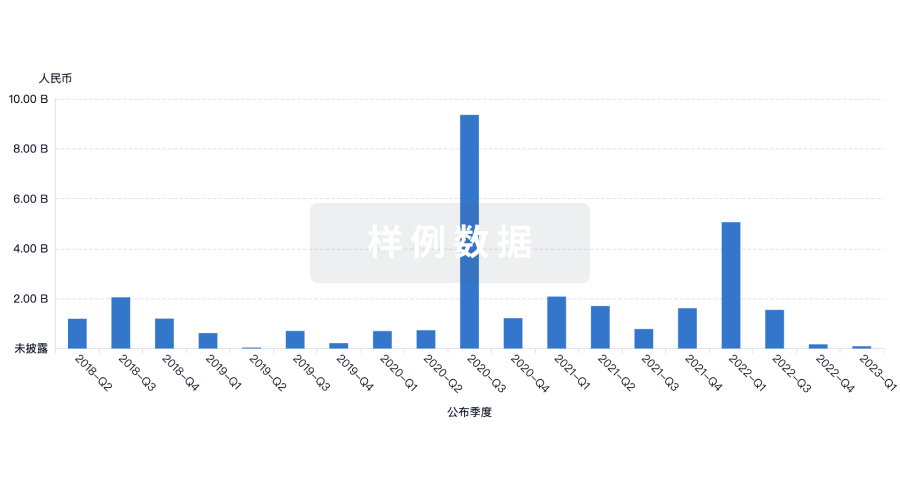
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
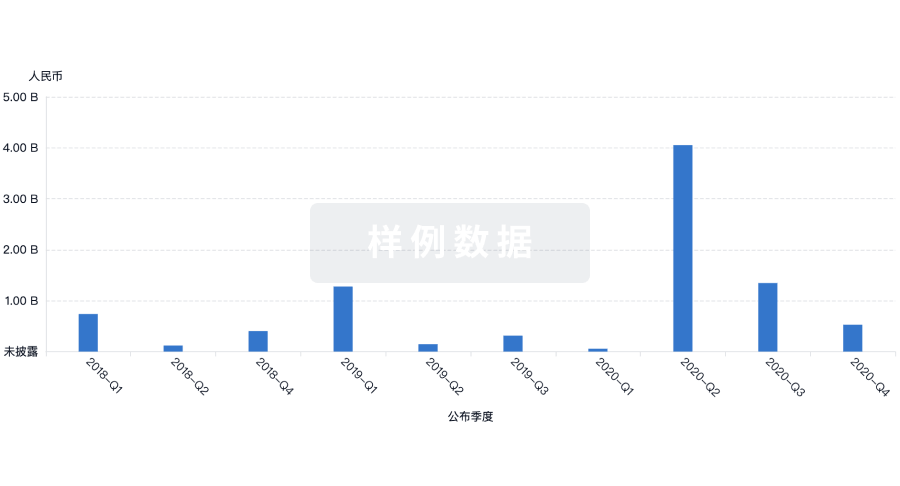
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
