预约演示
更新于:2025-08-29

ImmuneMed, Inc.
更新于:2025-08-29
概览
标签
免疫系统疾病
皮肤和肌肉骨骼疾病
内分泌与代谢疾病
单克隆抗体
化学药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 化学药 | 2 |
| 单克隆抗体 | 2 |
| 排名前五的靶点 | 数量 |
|---|---|
| vimentin(波形蛋白) | 2 |
关联
4
项与 ImmuneMed, Inc. 相关的药物靶点 |
作用机制 vimentin抑制剂 [+1] |
在研机构 |
原研机构 |
在研适应症 |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
8
项与 ImmuneMed, Inc. 相关的临床试验NCT06306339
A Phase 2a Multi-center, Randomized, Double-blind, Placebo-controlled Study to Evaluate the Efficacy and Safety of Burfiralimab(hzVSF-v13) Added to Disease-modifying Antirheumatic Drugs in Participants With Moderate to Severe RA
The goal of this clinical trial is to evaluate the efficacy and safety of intravenous infusions of burfiralimab (hzVSF-v13) when added to Disease-Modifying Antirheumatic Drug (DMARD) treatment as Standard of Care (SOC) in participants with moderate to severe Rheumatoid Arthritis (RA).
开始日期2024-03-01 |
申办/合作机构 |
NCT05808335
A Phase IIa Multi-center, Randomized, Double-blind, Placebo-controlled Study to Evaluate the Efficacy and Safety of Oral Antiviral Agents/hzVSF-v13 Combination Therapy vs Oral Antiviral Monotherapy in Chronic Hepatitis B Patients
This is a multicenter, randomized, double-blind, parallel group, 48-week follow-up, Phase IIa clinical study. This study has been designed to evaluate the change in HBsAg (log10 IU/mL) after administration of hzVSF-v13 50 mg/dose and hzVSF-v13 200 mg/dose in combination with an oral antiviral agent (Tenofovir or entecavir, including salt-free or salt-modifying drugs) compared to an oral antiviral agent in combination with a placebo (normal saline) in patients with chronic hepatitis B who are stably receiving an oral antiviral agent (Tenofovir or entecavir, including salt-free or salt-modifying drugs) for at least 24 weeks.
开始日期2022-01-11 |
申办/合作机构 |
NCT04679350
A Multi Center, Randomized, Double-blind, Parallel Design, Phase 2 Study to Evaluate the Efficacy and Safety of hzVSFv13 Compared to Standard of Care After Intravenous(IV) Administration With Add-on Standard of Care in COVID-19 Moderate to Severe Patients
To explore the efficacy and confirm the safety of the concomitant administration of the standard of care and hzVSF-v13 in patients with COVID-19 infection
开始日期2021-03-18 |
申办/合作机构 |
100 项与 ImmuneMed, Inc. 相关的临床结果
登录后查看更多信息
0 项与 ImmuneMed, Inc. 相关的专利(医药)
登录后查看更多信息
3
项与 ImmuneMed, Inc. 相关的文献(医药)PLoS One
Baculovirus entire ORF1629 is not essential for viral replication
Article
作者: Lee, See Nae ; Bae, Sung Min ; Gwak, Won Seok ; Kim, Hyun Soo ; Woo, Soo Dong ; Choi, Jae Bang ; Je, Yeon Ho ; Han, Beom Ku
It is generally accepted that ORF1629 is essential for baculovirus replication, which has enabled isolation of recombinant viruses in a baculovirus expression system using linearized viral DNA. ORF1629-defective viruses cannot replicate in insect cells; only recombinant virus with complete ORF1629 restoration by recombination can propagate, allowing for pure isolation and the development of bacmids for easy selection of recombinant viruses. We inadvertently found proliferation in insect cells of a bacmid lacking a complete ORF1629. PCR indicated no other viruses but a lack of complete ORF1629 in the proliferated bacmid, suggesting that the baculovirus propagated without a complete ORF1629. Lack of ORF1629 decreased the virus growth rate and yield; it also increased the occlusion body (OB) size but decreased its yield. These results were confirmed for Autographa californica multicapsid nucleopolyhedrovirus (AcMNPV) and Bombyx mori NPV (BmNPV). Thus, entire ORF1629 is not essential for viral replication, though it does affect the virus growth rate, yield, and size and OB production.
Viruses3区 · 医学
Enhanced Production of Recombinant Protein by Fusion Expression with Ssp DnaB Mini-Intein in the Baculovirus Expression System
3区 · 医学
ArticleOA
作者: Bae, Sung Min ; Gwak, Won Seok ; Han, Beom Ku ; Choi, Jae Bang ; Woo, Soo Dong
The baculovirus expression system (BES) is considered to be a very powerful tool for the expression of numerous difficult to express vertebrate proteins. Ssp DnaB mini-intein is a useful fusion partner for the production of recombinant proteins because it can be self-cleaved by controlling the pH and temperature, without additional treatment. To evaluate the utility of Ssp DnaB mini-intein in the BES, recombinant viruses were generated to express the enhanced green fluorescent protein, the VP2 protein of porcine parvovirus, and the E2 protein of classical swine fever virus fused to a mini-intein. As expected, intracellular self-cleavage of the mini-intein occurred during virus infection, but the cleavage initiation time varied depending on the target protein. Significantly enhanced protein production was observed for all of the target proteins that were fused to the mini-intein. This increase was enough to overcome the decrease in the fusion protein due to intracellular self-cleavage. The mini-intein in all of the recombinant fusion proteins was successfully cleaved by controlling the pH and temperature. These results suggest that the Ssp DnaB mini-intein is a useful fusion partner in the BES for easy purification and enhanced production of target proteins.
Cells3区 · 生物学
Combination Treatment with the Vimentin-Targeting Antibody hzVSF and Tenofovir Suppresses Woodchuck Hepatitis Virus Infection in Woodchucks
3区 · 生物学
ArticleOA
作者: Lee, Kyoung-pil ; Li, Bin ; Suresh, Manasa ; Kallakury, Bhaskar V. ; Park, Sungman ; Yon, Changsuek ; Menne, Stephan ; Kim, Yoon-Won ; Huang, Xu ; Korolowicz, Kyle E.
Current treatment options for patients infected with hepatitis B virus (HBV) are suboptimal, because the approved drugs rarely induce cure due to the persistence of the viral DNA genome in the nucleus of infected hepatocytes, and are associated with either severe side effects (pegylated interferon-alpha) or require life-long administration (nucleos(t)ide analogs). We report here the evaluation of the safety and therapeutic efficacy of a novel, humanized antibody (hzVSF) in the woodchuck model of HBV infection. hzVSF has been shown to act as a viral entry inhibitor, most likely by suppressing vimentin-mediated endocytosis of virions. Targeting the increased vimentin expression on liver cells by hzVSF after infection with HBV or woodchuck hepatitis virus (WHV) was demonstrated initially. Thereafter, hzVSF safety was assessed in eight woodchucks naïve for WHV infection. Antiviral efficacy of hzVSF was evaluated subsequently in 24 chronic WHV carrier woodchucks by monotreatment with three ascending doses and in combination with tenofovir alafenamide fumarate (TAF). Consistent with the proposed blocking of WHV reinfection, intravenous hzVSF administration for 12 weeks resulted in a modest but transient reduction of viral replication and associated liver inflammation. In combination with oral TAF dosing, the antiviral effect of hzVSF was enhanced and sustained in half of the woodchucks with an antibody response to viral proteins. Thus, hzVSF safely but modestly alters chronic WHV infection in woodchucks; however, as a combination partner to TAF, its antiviral efficacy is markedly increased. The results of this preclinical study support future evaluation of this novel anti-HBV drug in patients.
1
项与 ImmuneMed, Inc. 相关的新闻(医药)2025-03-31
·药智网
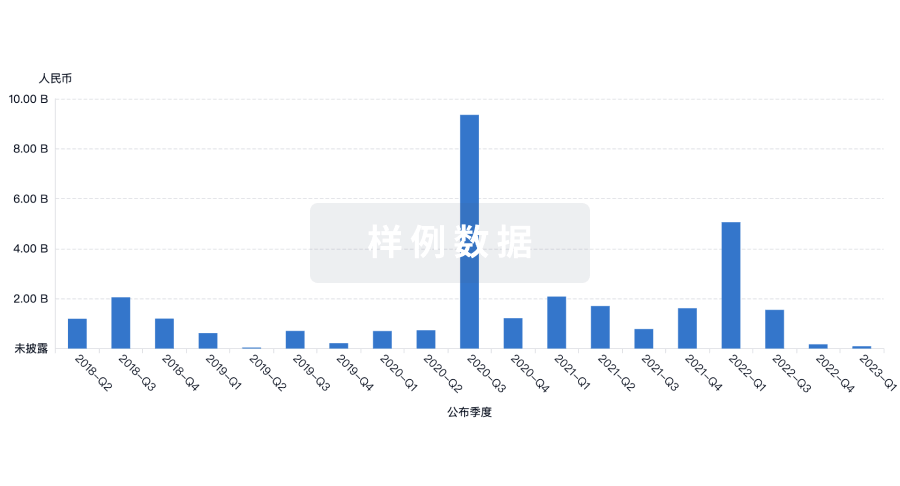
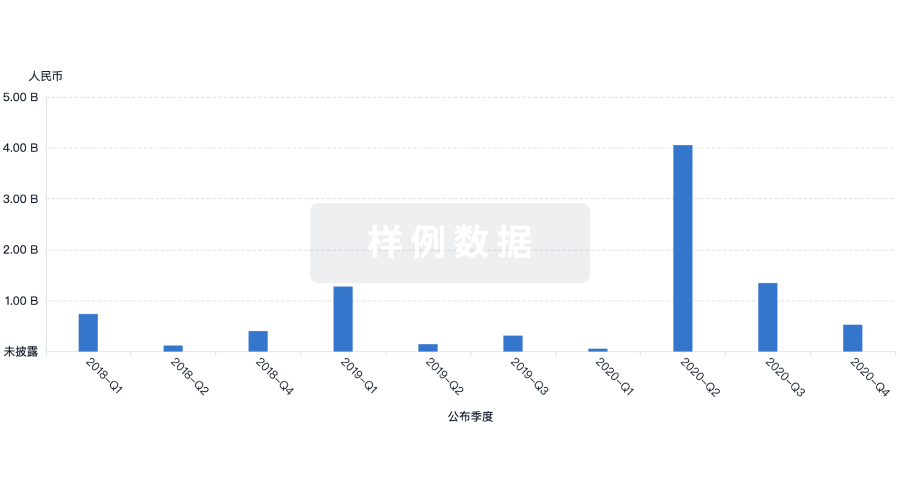
2013年,索非布韦获得美国食品与药品监督管理局(FDA)批准,在美国上市,该药显示了强大的疗效,对丙肝的治愈率达到 95% 左右。2025年,CROI会议上,RIO和FRESH两项研究公布了关于bnAb在HIV治疗中的重要成果,为HIV功能性治愈带来新曙光。同是令人谈之色变的病毒疾病,随着新药研究的深入,HCV与HIV均已迎来治愈曙光,而更常见的乙型肝炎(HBV)的新药研究却还处于怎样的阶段?乙肝:病毒领域致病机制最复杂的疾病原则上来讲,病毒领域致病机制最负责的疾病,既不是RSV也不是HIV,反而是更常见的乙肝,从最初发现至今的60余年里仍难以治愈,甚至其新药研究的推进也相对困难,这是为何?这主要是因为,乙肝病毒双链DNA能在细胞核中形成cccDNA,除了在常规“中心原则”下可以顺势转录为RNA、形成病毒蛋白,还能通过前体RNA“逆转录”形成双链DNA,最后双链DNA与病毒蛋白再次组成新的病毒颗粒,开始新一轮的感染,这就导致病毒源源不断,最终让免疫细胞疲于应付,压制免疫系统,使得人体难以形成有效的抗体。乙肝作为一种严重威胁人类公共健康的疾病,全球约有3亿人携带乙肝病毒,中国作为乙肝高发区,乙肝患者基数庞大。长期的乙肝病毒感染不仅会导致慢性肝炎,还可能进一步发展为肝硬化和肝癌,给患者的健康和生活带来沉重负担。图片来源:盖德视界而对于乙肝的治疗,根据体内HBeAg情况,可分为未治疗阶段、病毒抑制阶段、功能性治愈阶段、完全治愈阶段阶段,而以目前的医疗环境,则多处于第二、第三阶段之间,如恩替卡韦、替诺福韦等药物虽能有效控制病情,但一方面需要患者终身用药,另一方面其也难以彻底清除肝细胞内的病毒“储备库”。因此,研发一种能够实现乙肝功能性治愈的药物,成为全球医药领域的重要目标。乙肝治疗的百年历程纵观乙肝治疗的百年历史,从1963年巴鲁克-布隆伯格(Baruch S. Blumberg)和他的同事们在澳大利亚土著人血清中发现了“澳抗(乙肝表面抗原)”,乙肝的神秘面纱开始被揭开,之后历经数年,乙肝病病毒的结构才最终被人类完全破解。但尽管病毒研究顺利,临床上药物来得却比较晚,直至上世纪90年代真正意义上的临床治疗才算开始,并在之后30余年里迅速发展,其整体可分为四个主要阶段,即短效干扰素时代、核苷酸类似物时代、联用时代与新型抗病毒时代。数据来源:公开数据整理(点击查看大图)阶段一:短效干扰素时代1990年,第一款用来治疗乙型肝炎的药物诞生,先灵葆雅的干扰素α被美国FDA正式批准用于治疗慢性乙型肝炎,是乙肝治疗的一个重要里程碑。干扰素α不仅具有一定的抗病毒作用,且由于具备免疫调节剂特性,导致其抗病毒的同时还能提高患者免疫调节能力,增加NK细胞的杀伤力,具有双重抗病毒机制,并且还具备减轻肝纤维化、降低肝硬化和肝癌的发生率等诸多正向作用。但同时,干扰素也并非完美,其在治疗乙肝方面也同样存在较大的局限性,比如:抗病毒效果弱:对于乙肝病毒载量较高的患者,干扰素α的抗病毒效果较差,难以有效抑制病毒复制。患者顺应性不佳:干扰素α需要注射给药,且由于早期短效制剂特点,往往需要更频繁的注射给药,同时药品还需冷冻保存,极大地增加了患者的使用难度和不便。副作用明显:干扰素α伴随较大的副作用,如肝功能损害、甲状腺功能异常、流感样症状、骨髓抑制等。适用范围受限:干扰素α不适用于失代偿肝病患者(如肝硬化、伴有黄疸的慢性乙型肝炎患者)以及有甲状腺疾病或精神疾病史的患者。其中,副作用与频繁注射最令乙肝患者所不能接受,也是导致欧美接受干扰素治疗的患者比例不超过10%的主要原因。为此,开发一款副作用低或能够口服的乙肝抗病毒新药成为彼时最主要的临床需求。阶段二:核苷酸类似物时代1998年,GSK研发出了第一款“口服”抗病毒药物—拉米夫定,这也是历史第一款用于乙肝治疗的核苷酸类似物疗法。图片来源:贝杰医药其治疗上贯彻“病毒欺骗”概念,即通过对脱氧核糖核酸聚合酶产生竞争性抑制,抑制有逆转录活性的乙型肝炎病毒DNA聚合酶,干扰乙型肝炎病毒DNA的合成,从而实现阻止乙型肝炎病毒复制的目的。在其临床数据中,短期治疗阶段(4-12周),即可显著降低血清HBV DNA水平,部分患者达到病毒学应答(VR),而长期治疗(1~5年)则可进一步提高HBeAg血清学转换率,分别为16%(1年)、17%(2年)、23%(3年)、28%(4年)和35%(5年),且副作用与不良反应发生率在可接受范围内。因此拉米夫定一经上市,其“口服特性”就直接导致其卖爆,也因此成功挽救了无数乙肝患者的生命,减少了肝硬化、肝癌的发生率。不过,也正是由于核苷酸类似物的治疗理念是“欺骗病毒”,因此其只能缓解症状、延缓病情,却注定无法根治乙肝。通常情况下患者需要终生服药。但随着用药时间的逐渐拉长,拉米夫定最大的问题开始出现,即病毒对药物的敏感性降低,俗称耐药。这对于患者而言无疑于毁灭性打击,因为乙肝治疗一旦耐药也就意味着病毒的迅速反扑,一切也就回到了原点。因此,在该阶段之下,如何应对乙肝药物耐药成为最主要思想,方法也很简单,即一方面积极开发全新种类的核苷酸类似物药物,另一方面则想方设法延缓抗病毒疗法的耐药进展。阶段三:药物联用时代随着拉米夫定的耐药患者越来越多,越来越多全新类型的核苷酸类似物疗法因此诞生:2002年,阿德福韦酯(ADV)问世,其与拉米夫定不发生交叉耐药,因此其成为“拉米夫定”耐药后的最佳替代者,为拉米夫定分担了巨大的压力,但其部分患者出现肾性低血磷性骨软化症或低磷血症等副作用,也限制了其发展。2005年,恩替卡韦(ETV)问世,其在抗病毒效果、耐药性和不良反应这些方面均优于前两代产品,很大程度上缓解了核苷类药物耐药后无药可医的窘境(治疗5年的累计耐药发生率为1.2%),但缺点在于,其不适宜妊娠期妇女,所以恩替卡韦仍不够完美。2006年,替比夫定(LDT)上市,虽其抗病毒、耐药性,不良反应等虽均不及恩替卡韦,但其却具备两大核心优势,一者是对胎儿安全,可以用于孕妇的抗病毒治疗;二者是有利于肾功能恢复,可应用于伴有肾脏问题的乙肝患者。2008年,替诺福韦酯(TDF)在欧美上市,其在前几代核苷类药物基础上,具有强效抑制病毒复制的作用,耐药发生率低。采用替诺福韦长期治疗还能显著改善肝脏组织学,降低HCC发生率,然而,替诺福韦具有一定肾毒性,长期使用会产生轻微肾损伤和降低骨密度风险。2016年,丙酚替诺福韦(TAF)上市,除去强效抑制病毒复制、耐药率极低优点外,还避免了肾损害,具有更好的骨骼安全性,降低了患骨质疏松症的风险。2021年,艾米替诺福韦(TMF)上市,是我国自主研发的第一款抗乙肝病毒核苷(酸)类药物,艾米替诺福韦通过创新的ProTide(磷酰胺酯化前药)技术,实现了替诺福韦(TFV)向肝细胞的靶向输送,在提高肝细胞内活性代谢物TFV-DP浓度的同时,大幅降低血浆中TFV的暴露量,从而在高效抑制HBV复制的同时,降低了长期使用的安全性风险。当然,随着不同类型的药物逐渐上市,下一步就需要思考如何延缓患者耐药进程,也是这个阶段,药物联用逐渐成为了主流。据研究人员发现,经过核苷和聚乙二醇干扰素α联合治疗的患者,不仅会出现HBsAg的清除,核苷经治优势患者加用聚乙二醇干扰素临床治愈率可达30%~80%,而且耐药性也得到有效缓解。因此,核苷酸类似物+核苷酸类似物、核苷酸类似物+干扰素的治疗逐渐成为彼时乙肝治疗的主要策略,尤其是后者。而药物联用阶段的开始,也标志着临床上要求的“临床治愈”概念有了落实之处,也为后续的创新研究指明了最终方向。阶段四:创新疗法时代2020年之后,乙肝抗病毒的治疗与新药研究手段爆发,除核苷类似物与长效干扰素之外,一系列新型潜在抗病毒创新疗法开始进入临床。截止目前,粗略估计全球在研乙肝新药已超200款,其中绝大部分创新疗法均处于临床前期阶段,临床I期或临床前研究阶段的管线占比66.4%;临床Ⅱ期管线占比31.5%;临床Ⅲ期管线仅2.1%。数据来源:公开数据整理从根据不同乙肝新药的研发策略,临床上的新药在研也分为了两大类,即“靶向HBV生命周期的直接抗病毒药物”与“靶向宿主免疫系统的间接抗病毒药物”。前者包括衣壳抑制剂、进入抑制剂、RNA干扰(siRNA)、反义寡核苷酸(ASO)等;后者包括治疗性疫苗、单克隆抗体、凋亡诱导剂、先天免疫激活剂、PD-1抑制剂与T细胞免疫调节剂等。数据来源:药智数据、公开数据整理(点击查看大图)从新药数量上看,由于直接抗病毒药物对病毒抑制作用更直接、症状缓解作用更大,故其在新药数量上占主要地位(44.6%),而细分新药类型上,直接抗病毒疗法中新药数量从高到底依次是衣壳抑制剂、siRNA、进入抑制剂、HBsAg抑制剂、ASO与基因疗法。部分乙肝创新疗法数据对比分类聚乙二醇干扰素α+核苷衣壳抑制剂(AB-729)HBsAg抑制剂(REP2139/REP2165)ASO(GSK836)siRNAVIR-2218临床方案临床方案联用核苷+干扰素联用核苷+干扰素联用Peg-IFN联用干扰素优势患者群体HBsAg低水平HBsAg高水平HBsAg高水平HBsAg低水平HBsAg低水平HBsAg清除率40.98%(48周)35%(48周)40%(48周)35%(24周)30%~40%(24周)HBV DNA的抑制情况无优势显著无优势显著显著耐药性应对弱良良优优注:非头对头对比,入组患者群体、临床时间、HBsAg基线等有所不同,仅作为参考数据来源:公开数据整理在临床优势上,由于各种疗法间的优势目标存在较大差距,比如HBsAg抑制剂联用核苷与干扰素情况下,对于耐药与HBsAg高水平患者的有效性更高,而ASO与siRNA除了可观的HBsAg清除能力外,对HBV-DNA水平降低能力却更强,因此,原则上并不能说ASO、siRNA能完全替代传统疗法,多数只能是选择性替代或直接联用。1. 衣壳抑制剂衣壳抑制剂是近年来乙肝治疗领域的一个重要研究方向,目前全球范围内尚无任何一款衣壳抑制剂获批治疗乙肝。其机制上是通过诱导核心蛋白的异构变化来抑制HBV衣壳,从而导致非感染性病毒颗粒(空核衣壳)形成,继而无法完成后续的逆转录和复制环节,同时其还可以增强核心蛋白二聚体结合力,干扰病毒在肝细胞核的脱壳过程,可以从源头阻断共价闭合环状DNA(cccDNA)的形成。某种层面可以将其简单地看作核苷类药物的补充版,其在降低病毒DNA的同时,还能降低RNA。但同时,衣壳抑制剂也同样存在明显的局限性,比如无法有效清除共价闭合环状DNA(cccDNA)、耐药性问题仍在、HBV(DNA/RNA)减少效果有限等,因此其从原理上无法实现乙肝的完全治愈、只能作为联合疗法的一部分使用。数据显示,全球已有近50款用于乙肝治疗的衣壳抑制剂在研(另一集中适应症为HIV)。其中临床阶段最靠前的为东阳光药业的甲磺酸莫非赛定,目前已进入临床Ⅲ期;其次是8款处于临床Ⅱ期的创新疗法,如广生堂的奈瑞可韦、正大天晴的TQA-3605、Novira的AL-3778等;之后则是18款处于临床I期的管线,包括科伦博泰的KL-060332、西安新通的XT-1061、维申医药的VD-1219、恒瑞医药的HRS5091等。全球最高阶段药品名称原研单位管线状态临床III期甲磺酸莫非赛定 Morphothiadine Mesylate广东东阳光药业股份有限公司临床III期临床Ⅱ期奈瑞可韦 Neracorvir上海药明康德新药开发有限公司;福建广生堂药业股份有限公司活跃TQA-3605正大天晴药业集团股份有限公司活跃HEC-121120广东东阳光药业股份有限公司临床III期ABI-H2158Assembly Biosciences Inc百济神州(合作单位)临床III期JNJ-56136379(突破性治疗)强生创新制药临床III期AL-3778Novira Therapeutics Inc活跃乌赞色替 VebicorvirAssembly Biosciences Inc百济神州(合作单位)临床III期canocapavir-ZM-H1505R(突破性治疗)上海挚盟医药科技有限公司活跃临床Ⅰ期KL-060332四川科伦博泰生物医药股份有限公司临床III期福瑞赛定 Freethiadine广东东阳光药业股份有限公司活跃XT-1061西安新通药物研究股份有限公司活跃VD-1219维申医药科技(上海)有限公司活跃XTYW-001西安新通药物研究股份有限公司活跃ABI-4334Assembly Biosciences Inc吉利德科学(合作单位)活跃LW-231上海长森药业有限公司活跃VNRX-9945Venatorx Pharmaceuticals Inc临床III期AB-836Arbutus Biopharma Corp活跃ALG-000184Aligos Therapeutics Inc活跃HRS5091江苏恒瑞医药股份有限公司临床III期ABI-H3733Assembly Biosciences Inc百济神州(合作单位)活跃EDP-514Enanta Pharmaceuticals Inc临床III期AB-506(终止)Arbutus Biopharma Corp临床III期AB-423Arbutus Biopharma Corp临床III期JNJ-440Alios BioPharma Inc临床III期QL-007齐鲁制药有限公司临床III期RO6889678罗氏临床III期数据来源:药智数据2. 进入抑制剂所谓进入抑制剂,又称为NTCP抑制剂,其主要是通过抑制乙肝病毒进入肝细胞来阻止病毒的复制和传播。这种抑制剂通常通过与乙肝病毒的包膜蛋白结合,阻止病毒与肝细胞表面的受体结合,从而抑制病毒感染细胞。在临床上,乙肝进入抑制剂的开发已取得一定进展。例如,myrcludex b是一种人工合成的多肽,由乙肝病毒的pre S1蛋白的2-48残基组成,它可以与钠离子牛磺胆酸共转运蛋白(NTCP)竞争性结合,从而抑制HBV进入细胞。总体来讲,进入抑制剂在乙肝治疗中具有以下优势:源头阻断病毒复制:通过阻止病毒进入肝细胞,从源头抑制病毒复制,减少病毒载量。联合治疗潜力:与现有抗病毒药物(如核苷类似物)联合使用,可增强治疗效果,降低耐药风险。针对合并感染:对乙肝合并丁肝感染患者具有显著疗效,填补了现有治疗手段的空白。乙肝进入抑制剂的开发和研究为乙肝治疗提供了新的思路和方法,有助于减少病毒对人体的侵害,但目前这类药物仍在研究和开发阶段,尚未广泛应用于临床。药品名称药品类别靶点原研单位全球最高阶段管线状态布乐韦肽 Bulevirtide生物制品;脂肽NTCPMYR GmbH批准上市(丙肝)注册申请:乙肝活跃Hepalatide化药;蛋白/多肽NTCP上海贺普药业股份有限公司临床Ⅱ期活跃布雷利单抗 Burfiralimab单抗VimentinImmuneMed Inc临床Ⅱ期活跃A-2342化药NTCPAlbireo AB;益普生临床Ⅰ期活跃HH-1270暂无NTCP华辉安健(北京)生物科技有限公司临床前活跃OT-1301多肽CYP;NTCP欧康维视生物医药(香港)有限公司临床前活跃SCY995化药NTCPSCYNEXIS Inc临床前活跃SCY450化药NTCPSCYNEXIS Inc临床前活跃N6HB426-20单抗NTCPRiken Corp临床前活跃SCY446化药NTCPSCYNEXIS Inc临床前活跃数据来源:药智数据当让,无论是新药数量还是研发热度,进入抑制剂都远逊于衣壳抑制剂与miRNA等热门方向,全球仅有10余款管线布局,且进入临床阶段的产品极少,其中MYR GmbH(吉利德收购)的Bulevirtide在丙肝适应症获批上市的前提下,其乙肝适应症也是全球进入抑制剂领域最靠前的新药产品,目前已处于注册申请阶段;其次是贺普药业的Hepalatide、ImmuneMed的Burfiralimab进度也相对靠前,处于临床II期间。3. HBsAg抑制剂HBsAg抑制剂是一类专门针对乙型肝炎表面抗原(HBsAg)的药物,旨在阻断HBsAg和亚病毒颗粒的释放以控制HBV的复制和感染过程。目前,HBsAg抑制剂的研究和开发相对较少,并非乙肝抗病毒治疗的主力方向,仅有少数几款新药管线的研究推进顺利。管线名称技术分类靶点类型原研企业临床阶段REP-2139核酸聚合物HBsAgHBSAg抑制剂REPLICor Inc临床Ⅱ期REP-2165核酸聚合物HBsAgHBSAg抑制剂REPLICor Inc临床Ⅱ期GST-HG131化药TENT4A;TENT4BHBSAg抑制剂上海药明康德新药开发有限公司;福建广生堂药业股份有限公司临床Ⅱ期LP-128化药HBsAgHBSAg抑制剂广州麓鹏制药有限公司临床Ⅰ期GST-HG121化药HBsAgHBSAg抑制剂上海药明康德新药开发有限公司;福建广生堂药业股份有限公司临床Ⅰ期数据来源:药智数据4. ASOASO(反义寡核苷酸)治疗乙肝的作用机制主要基于其对病毒基因表达的精准调控,通过序列互补性与HBV mRNA结合,形成稳定的DNA双链结构,直接阻断核糖体对病毒mRNA的识别,抑制HBsAg、HBeAg等关键病毒蛋白的翻译过程。简单来说,将乙肝病毒的mRNA比作制作HBsAg和HBeAg等抗原的“模版”,ASO疗法针对目标不再选择致病抗原,而是这些“模版”,从源头层面试图减少乙肝病毒抗原的产生。相较其他抗病毒疗法,ASO与siRNA被认为是目前最能实现乙肝“功能治愈”的疗法,其不仅具备诸多特异性优势,且临床上也取得了一些可喜的结果,显示了研发活跃的积极状态。针对性强:ASO药物能够特异性地针对HBV的关键mRNA进行降解,减少非特异性副作用。潜在疗效显著:临床试验显示,ASO药物能够显著降低HBsAg和HBV-DNA水平,有望实现CHB的功能性治愈。安全性良好:多数ASO药物在临床试验中表现出良好的安全性和耐受性。药品名称靶点原研单位全球最高阶段中国最高阶段管线状态GSK836(突破性疗法)HBVIonis Pharmaceuticals Inc;葛兰素史克临床Ⅲ期临床Ⅲ期活跃AHB-137(突破性疗法)HBV杭州浩博医药有限公司临床Ⅱ期临床Ⅱ期活跃GSK4388067-葛兰素史克临床Ⅱ期临床Ⅲ期活跃GSK3389404ASGPR;HBsAg葛兰素史克临床Ⅱ期临床Ⅱ期活跃ALG-020572HBsAgAligos Therapeutics Inc临床Ⅰ期临床Ⅲ期活跃SB 539HBVF-star Therapeutics Inc临床前临床Ⅲ期活跃SB-527HBVF-star Therapeutics Inc临床前临床Ⅲ期活跃数据来源:药智数据其中,GSK的GSK836作为全球ASO乙肝疗法中进展最快的管线,目前已处于临床Ⅲ期阶段,GSK更是在其2024年财报中重点提及该药将于2026年敲定上市,同时公布比较完整的Phase Ⅲ期临床数据。图片来源:肝博士之后,浩博医药的AHB-137、GSK的GSK4388067与GSK3389404也已进入临床Ⅱ期,也是ASO乙肝疗法中备受期待的管线。5. RNA干扰(siRNA)相较衣壳抑制剂等小分子抗病毒疗法而言,RNAi药物在作用机制上则存在较为明显的优势,其高效靶向和降解HBV转录的本质,可以抑制HBV抗原表达,阻断病毒复制,减轻免疫耐受,虽然对cccDNA或整合病毒DNA无直接作用,但却可以抑制来自整合HBV-DNA和cccDNA的HBsAg。同时由于其在作用机制上,与ASO具有相似的药物设计理念,两者均为靶向HBV mRNA降解,不过较ASO疗法,siRNA理论上还具有诸多显著优势:作用机制更高效:siRNA通过RNA干扰(RNAi)机制,直接降解病毒mRNA,显著降低HBsAg和HBV DNA水平,且对cccDNA转录的pgRNA也有抑制作用。而ASO主要通过结合mRNA并依赖RNase H降解病毒RNA,但其对cccDNA的直接影响有限。靶向范围更广:siRNA可同时靶向多个HBV转录本,包括HBsAg、HBeAg和HBV DNA,实现更全面的病毒抑制,ASO通常针对特定mRNA序列,作用范围相对较窄。临床疗效更显著:临床试验显示,siRNA药物(如Xalnesiran)在联合或不联合免疫调节剂的情况下,显著提高HBsAg转阴率,部分患者实现功能性治愈。ASO(如Bepirovirsen)虽能降低HBsAg水平,但其功能性治愈率相对较低,且需长期治疗。免疫调节潜力更强:siRNA可通过激活TLR7等免疫受体,增强先天免疫反应,促进病毒清除;ASO的免疫调节作用较弱,主要通过直接抑制病毒RNA发挥作用。给药频率更低:siRNA药物通常每4周给药一次,患者依从性更高。ASO需更频繁给药,可能增加治疗负担。而在临床研究层面,siRNA疗法同时也是现阶段乙肝抗病毒新药数量中仅次于衣壳抑制剂的存在,全球约有超20款重点管线涉及,且大部分管线均已进入临床Ⅱ期阶段,比如星曜坤泽生物的HT-101、正大天晴的TQA-3038、腾盛博药的VIR-2218、Arrowhead的JNJ-3989、罗氏的RO-7445482等。药品名称药品类别靶点原研单位全球最高阶段中国最高阶段管线状态HT-101化药;核酸偶联药物;siRNAHBsAg苏州星曜坤泽生物制药有限公司临床Ⅱ期临床Ⅱ期活跃TQA-3038化药;核酸偶联药物;siRNAASGPR正大天晴药业集团股份有限公司临床Ⅱ期临床Ⅱ期活跃Imdusiran化药;siRNAHBsAgArbutus Biopharma Corp;齐鲁制药(合作)临床Ⅱ期临床申请活跃BW-20507化药;siRNA-ARGO Biopharma Australia Pty Ltd临床Ⅱ期临床Ⅰ期活跃VIR-2218(突破性疗法)化药;核酸偶联药物;siRNAASGPRAlnylam Pharmaceuticals Inc;Vir Biotechnology Inc腾盛博药(合作)临床Ⅱ期临床Ⅱ期活跃JNJ-3989(突破性疗法)化药;核酸偶联药物;siRNAASGPRArrowhead Pharmaceuticals Inc;强生创新制药;葛兰素史克临床Ⅱ期临床Ⅱ期活跃ARC-520生物制品;核酸偶联药物;siRNAHBV;siRNAArrowhead Pharmaceuticals Inc临床Ⅱ期暂无研发进展活跃ALN-HBV生物制品;核酸偶联药物;siRNAASGPRAlnylam Pharmaceuticals Inc临床Ⅱ期暂无研发进展活跃ARB-1467生物制品;脂质纳米颗粒;siRNAHBV;siRNAArbutus Biopharma Corp临床Ⅱ期暂无研发进展活跃RO-7445482化药;siRNA-Dicerna Pharmaceuticals Inc;罗氏临床Ⅱ期临床申请活跃BW-03生物制品;siRNA-上海舶望制药有限公司临床Ⅰ期临床Ⅰ期活跃ALG-125755生物制品;核酸偶联药物;siRNAHBsAgAligos Therapeutics Inc临床Ⅰ期暂无研发进展活跃ARB-1740生物制品;脂质纳米颗粒;siRNAHBVArbutus Biopharma Corp临床Ⅰ期暂无研发进展活跃ALG-072571生物制品;siRNAPD-L1Aligos Therapeutics Inc临床前暂无研发进展活跃托立司兰 Tomligisiran生物制品;siRNA-强生创新制药临床前暂无研发进展活跃KW-040生物制品;siRNA-北京凯因科技股份有限公司;北京安龙生物医药有限公司临床前暂无研发进展活跃OLX-703A生物制品;siRNAHBVOliX Pharmaceuticals Inc临床前暂无研发进展活跃STP-155G生物制品;siRNAHBV圣诺生物临床前暂无研发进展活跃CG2021V生物制品;siRNA-上海柯君医药科技有限公司临床前暂无研发进展活跃ALG-125097生物制品;siRNAHBVAligos Therapeutics Inc临床前暂无研发进展活跃HPG6198生物制品;siRNAsiRNA雅创医药技术(上海)有限公司临床前暂无研发进展活跃数据来源:药智数据、公开数据整理从siRNA的开发历程来看,目前该领域主要有两代产品构成,第一代产品以Arrowhead的ARC-520和ARC-521为代表,但由于其HBsAg降低的有效性数据不明显,且有较大的肝脏损伤可能,故最终搁浅;第二代产品则是目前主流的siRNA类型,比如知名的VIR-2218、JNJ-3989等,这些新药不仅临床有效性较好,且安全性数据也不错,往往效果还能持续数月。综合评判之下,腾盛博药的VIR-2218是目前最具潜力的新药管线,其靶向乙型肝炎病毒(HBV)基因组的 X 区域(该区域是所有HBV病毒RNA转录本的共同区域),联合PegIFN的组别显著提高了HBsAg下降幅度。在其联合PEG-IFNα治疗乙肝的Ⅱ期研究数据中其中队列5(VIR-2218 × ≤ 13 + PEG IFNα × ≤ 44)在治疗结束时的HBsAg清除率可达30.8%,且队列4与队列五中15%~16%的患者在治疗结束后至少持续24周,有助于实现“功能性治愈”。而总体而言,虽然siRNA治疗乙肝领域仍有不少问题需要解决,比如长期有效性数据,长期安全性数据以及各类抗病毒药物的用药规划等都尚不明确,不过以其在治疗慢性乙型肝炎上显示出的潜力而言,其仍不失为乙肝治疗领域最受期待的创新疗法之一,尤其是未来与其他抗病毒药物联用方向。乙肝治疗的未来对于目前乙肝治疗的临床需求,以及乙肝新药的整体研发格局,如今仅靠单药疗法应对如此多复杂的需求明显不现实,无论是有效性、安全性、耐药性都很难取得质的突破,因此“联合治疗”或是未来实现功能性治愈的最佳研究方向。目前来看,乙肝联合治疗模式一般是围绕三大策略模式进行:抑制HBV复制(进入抑制剂、核苷(酸)类似物、衣壳抑制剂、siRNA/反义寡核苷酸)。抑制HBsAg产生(SiRNA/反义寡核苷酸、NAP、pegIFNa)。激活对HBV的免疫反应(检查点抑制剂、TLR激动剂或pegIFNa、治疗性疫苗)。目前各类型药物组合方式与方法尚没有明确定义,但多数新药均在以联用的方式推进产品有效性数据突破,比如过去常见的聚乙二醇干扰素α+核苷、衣壳抑制剂+核苷、ASO+干扰素、siRNA+核苷等。图片来源:医脉通小结其实,从短效干扰素到核苷酸类似物疗法,再到如今比较火热的衣壳抑制剂、ASO与siRNA疗法,不仅乙肝药物治疗的基础策略方案有了诸多变化,比如从“病毒欺骗”到“模版抑制”、比如从部分治愈到临床治愈,而且新时代下,单药治疗不再是唯一选项,反而是不同作用机制的创新疗法联用成为趋势。如今,随着衣壳抑制剂、HBsAg抑制剂、ASO与siRNA等创新疗法的临床进展,未来或许也面临着多款新药接踵而至,但从整体却仍难以改变长效干扰素与核苷酸类似物疗法的临床地位。在很多时候,医药创新都是在逐渐满足临床需求的过程中不断推进,至少现阶段而言,乙肝的完全治愈还并非现有哪种新药能办到的,道阻且长,还需努力。来源 | 博药(药智网获取授权转载)撰稿 | 博药内容中心责任编辑 | 八角声明:本文系药智网转载内容,图片、文字版权归原作者所有,转载目的在于传递更多信息,并不代表本平台观点。如涉及作品内容、版权和其它问题,请在本平台留言,我们将在第一时间删除。合作、投稿 | 马老师 18323856316(同微信) 阅读原文,是受欢迎的文章哦
临床研究上市批准
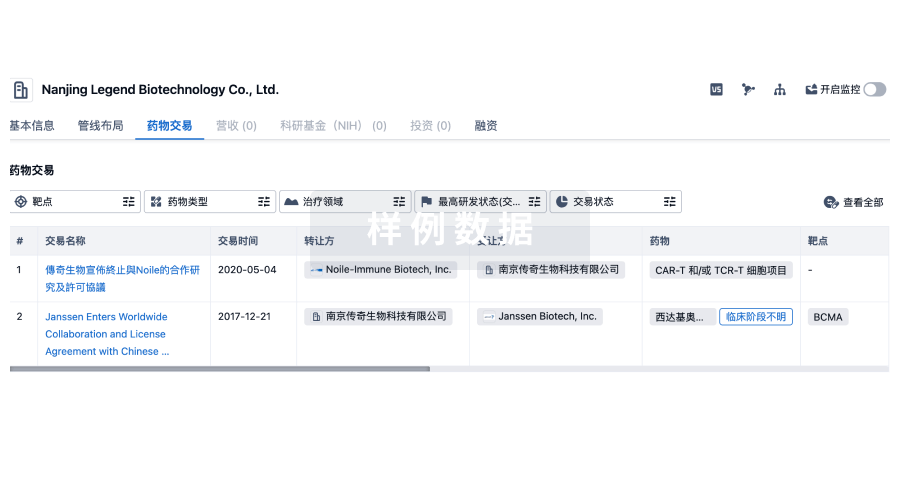
100 项与 ImmuneMed, Inc. 相关的药物交易
登录后查看更多信息
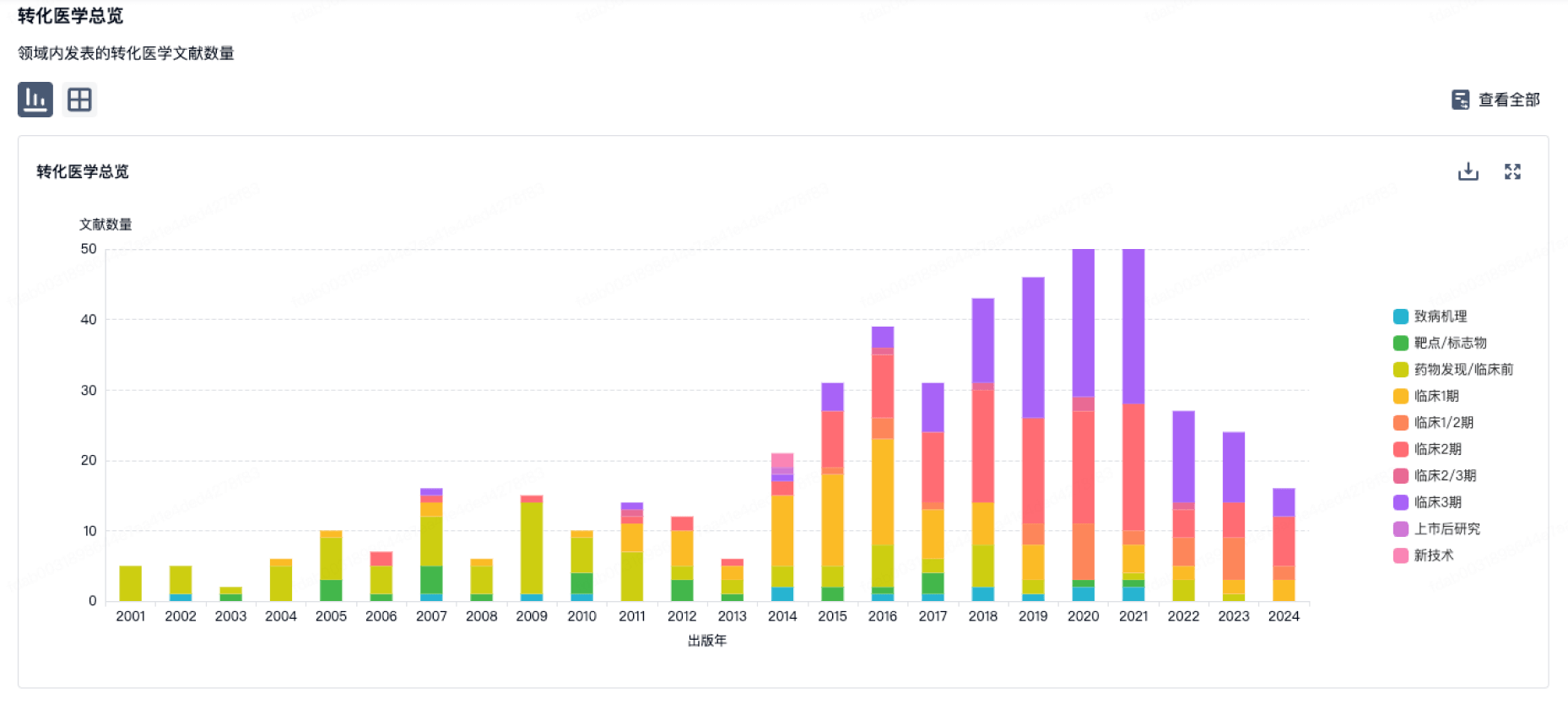
100 项与 ImmuneMed, Inc. 相关的转化医学
登录后查看更多信息
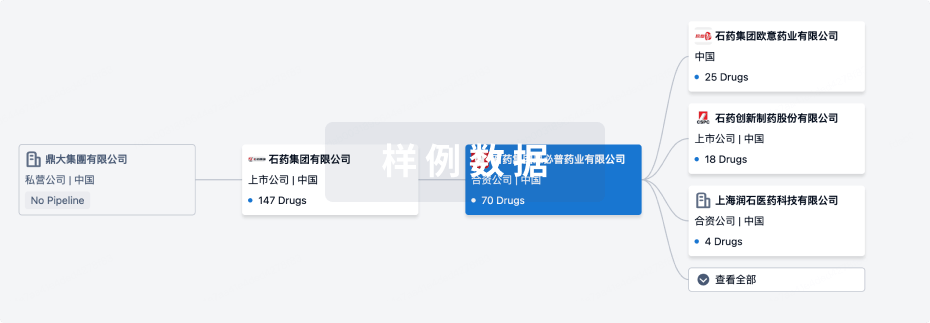
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月10日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
1
2
临床前
临床2期
1
2
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
PDAC(ImmuneMed) | 胰腺导管腺癌 更多 | 临床前 |
cGvHD(ImmuneMed) | 移植物抗宿主病 更多 | 临床前 |
WO2023027507 ( vimentin )专利挖掘 | 营养和代谢疾病 更多 | 药物发现 |
Burfiralimab ( vimentin ) | 新型冠状病毒感染 更多 | 终止 |
IM-02 | 肿瘤 更多 | 无进展 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
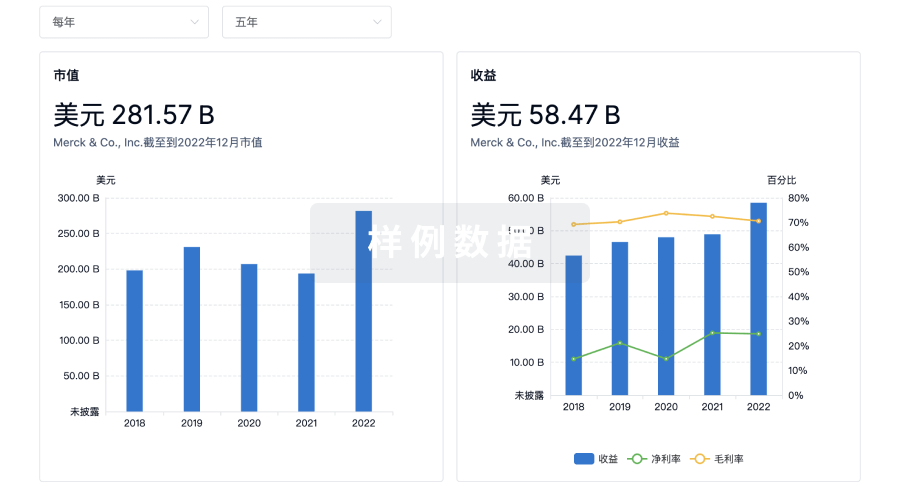
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用