预约演示
更新于:2025-05-07
Maoming People's Hospital
中国广东省
中国广东省
更新于:2025-05-07
概览
关联
26
项与 Maoming People's Hospital 相关的临床试验NCT06763666
A Multicenter, Prospective, Randomized Controlled Study Comparing the Efficacy and Safety of CLAG(Cladribine, Cytarabine and G-CSF) Combined With Venetoclax and CLAG in the Treatment of Relapsed/Refractory Acute Myeloid Leukemia
This is a multicenter, prospective, randomized controlled clinical study comparing the efficacy and safety of CLAG+VEN and CLAG regimens in relapsed/refractory(r/r) AML.
开始日期2025-02-01 |
申办/合作机构 |
NCT06526455
Efficacy and Safety of Vonorasan Versus Esomeprazole in the Treatment of Ulcers After Endoscopic Submucosal Dissection (ESD): a Multicentre, Parallel-design, Double-blind, Randomised Controlled Study
The purpose of this clinical trial is to find out the effectiveness of voronasan in combination with aluminum phosphate gel in the treatment of post-operative ESD ulcers. It will also find out about the safety of vunorasan in combination with aluminum phosphate gel. The main questions it aims to answer are:
1. Do vonorasan in combination with aluminum phosphate gel clinically effective in the treatment of post-operative ESD ulcers?
2. What medical problems do participants have when taking drug vonorasan in combination with aluminum phosphate gel? Researchers compared the drug voransen in combination with aluminum phosphate gel to esomeprazole in combination with aluminum phosphate gel to see if voransen in combination with aluminum phosphate gel worked better for post-operative ESD ulcers.
Participants will:
Intravenous lansoprazole 1-3 days after ESD and oral voronasan combined with aluminum phosphate gel or esomeprazole combined with aluminum phosphate gel 3-56 days after ESD.
Record their symptoms, endoscopic ulcer grading, ulcer size and Calculate ulcer healing rate at weeks 2 and 8.
1. Do vonorasan in combination with aluminum phosphate gel clinically effective in the treatment of post-operative ESD ulcers?
2. What medical problems do participants have when taking drug vonorasan in combination with aluminum phosphate gel? Researchers compared the drug voransen in combination with aluminum phosphate gel to esomeprazole in combination with aluminum phosphate gel to see if voransen in combination with aluminum phosphate gel worked better for post-operative ESD ulcers.
Participants will:
Intravenous lansoprazole 1-3 days after ESD and oral voronasan combined with aluminum phosphate gel or esomeprazole combined with aluminum phosphate gel 3-56 days after ESD.
Record their symptoms, endoscopic ulcer grading, ulcer size and Calculate ulcer healing rate at weeks 2 and 8.
开始日期2024-08-01 |
申办/合作机构  广东医科大学附属医院 广东医科大学附属医院 [+4] |
NCT05984511
TACE Plus Atezolizumab/Bevacizumab and I-125 Seeds Brachytherapy for HCC With Branch PVTT: A Phase III, Randomized Clinical Trial
The present study aimed to assess the effectiveness of the combination treatment of Atezolizumab/Bevacizumab, transcatheter arterial chemoembolization (TACE) and I-125 Seeds Brachytherapy (TACE-AB-I) in patients with advanced hepatocellular carcinoma (HCC) and portal vein tumor thrombosis (PVTT). The investigators confirmed that the combination therapy yielded better survival data than the combined administration of Atezolizumab/Bevacizumab and TACE (TACE-AB) in patients with advanced HCC and Type I/II PVTT (Based on Cheng's PVTT classification).
开始日期2023-08-30 |
申办/合作机构  中山大学附属第三医院 中山大学附属第三医院 [+4] |
100 项与 Maoming People's Hospital 相关的临床结果
登录后查看更多信息
0 项与 Maoming People's Hospital 相关的专利(医药)
登录后查看更多信息
621
项与 Maoming People's Hospital 相关的文献(医药)2025-07-01·Drug Resistance Updates
DTX2 attenuates Lenvatinib-induced ferroptosis by suppressing docosahexaenoic acid biosynthesis through HSD17B4-dependent peroxisomal β-oxidation in hepatocellular carcinoma
Article
作者: Li, Zhenchong ; Niu, Xing ; Huang, Fuxin ; Shen, Cheng ; Zhang, Zhongyan ; Huang, Shanzhou ; Zhang, Chuanzhao ; Zhou, Qi ; Hou, Baohua ; Mo, Ke
2025-04-16·Neurospine
Surgical Strategy Analysis of Chiari Malformation With or Without Type II Basilar Invagination According to the Morphological Types of the Atlanto-Occipital Joint: A Retrospective Study of 212 Patients.
Article
作者: Wu, Yanyu ; Lu, Yuntao ; Peng, Lin ; Huang, Qinguo ; Zhou, Qiang ; Li, Hong ; Ye, Junhua
2025-04-01·Journal for ImmunoTherapy of Cancer
Characteristics of second primary malignancies following bispecific antibodies therapy
Article
作者: Tian, Shengyu ; Liu, Dan ; Luo, Baiwei ; Wang, Liang ; Li, Tong ; Guo, Jia ; Zhou, Hongsheng ; Lu, Weixiang ; Lin, Bingyu ; Liang, Xiaojie ; Zhou, Xinyu ; Cai, Zihong ; Jin, Zhihao ; Chen, Keren
6
项与 Maoming People's Hospital 相关的新闻(医药)2025-01-15
·医脉通
院长贪腐不断,权力如何分解?
来源 | “看医界”微信公众号
作者|六花
近日,院长王茂生收受超2亿元回扣的贪腐事件被央视曝光,继2013年“药品回扣门”之后,知名县级三甲医院——高州市人民医院(以下简称“高州医院”)再度被拉上声誉“审判台”,震惊、唏嘘声此起彼伏。
“有钱的上广州,没钱的到高州”——这句曾在粤西地区广为流传的话,道出了高州医院曾经的辉煌。一度因“医术高超、不收红包、药价低廉、看病便宜”美名在外,被誉为公立医院改革“火车头”。高州医院昔日无数光环加身,如今却因接连的回扣事件“黯然失色”。
一度塑造传奇,县级医院的浮沉路
建于1927年的高州医院是一所百年老院。起初,位于广东省茂名市下属县级市的高州医院还只是一个“名不见经传”的普通山区医院。但在2001-2011年间,时任院长钟焕清用十年时间打造出了高州“神话”,使其发展成全国最大的县级医院。在多方媒体关注与报道下,高州医院化身故事主角,“高州模式”一时闻名。
“高州模式”在业内被总结为一种“去行政化”的改革路径。医院主动放弃政府财政补贴,换取更大的经营自主权,同时通过后来被称为“二次议价”的方式,与供应商谈判获取更低的药品折扣。挤出的药品利润,一方面以低于同类医院的收费让利患者;另一方面通过提高薪资水平,替代传统“灰色收入”,激励医生。
这一模式在当时成效显著,获得了患者与政府的高度赞誉。数据显示,2002至2009年间,该院节省的药品采购费高达2.2亿元,显著减轻了病人的药品费用负担。高州医院因此被誉为“平价医院”“百姓医院”,并获得了广东省卫生厅、卫生部以及广东前后两任省委书记张德江和汪洋的高度评价。
2010年,时任卫生部部长的陈竺亲笔写道:“这个案例好,公立医院,尤其是贴近基层的市县级的公立医院要都办成这样,该有多好!”
同年,在全国人大广东团分组讨论会上,钟焕清曾自豪地表示:“高州医院是唯一一个没有红包的医院,任何一个记者、中纪委、省纪委的工作人员去暗访,都没查到我们有收红包。”
然而,2011年4月,钟焕清被调离,医院更换院长后,“高州模式”逐渐消失,高州医院也在“回归”。据《第一财经》报道,钟焕清执掌的2010年,高州医院的药品收入为2亿元,而到了2012年,在门诊量减少的情况下,药品销售额却超过了3亿元。
2013年1月,央视《焦点访谈》更是曝光了该院“医药采购回扣”事件。据报道,该医院收取药品采购25%的回扣,仅茂名的一家医药公司就每年支付药品回扣费365万元。其他医药公司也同样存在类似情况。
事件曝光后,该院时任正副院长被免职并追责。3个月后,时年51岁的王茂生被任命为党委书记、院长,接手高州医院。
王茂生至今从医近40年,曾是茂名市人民医院著名的心胸外科专家,因技术精湛被誉为“王一刀”。这一任命原本寄望于他能以“王一刀”的权威和果断,打击医院内部的不良风气。然而,遗憾的是,从手术台到管理岗位的转变并未让他有效遏制腐败,反而最终深陷回扣丑闻,高州医院也再次陷入舆论的漩涡。
院长贪腐不断,权力如何分解?
医疗腐败贯穿各环节,院长更是首当其冲。曾有业内人士认为,院长成为“高危职位”的根源,与其权力过大缺乏监督有关。
早前,《看医界》曾专访现代医院管理专家、上海冬雷脑科医院集团总院长、原上海市浦南医院院长刘卫东。他认为院长权力过大是很多医院出现管理问题的重要原因,医院应该引入现代管理体系,建立公开透明的决策机制。
而他当时为了更好地管理浦南医院,甚至主动将权力“分出去”。
刘卫东当时在浦南医院引入的现代医院管理模式主要由三部分组成:决策层(党委会、专家委员会、职代会);执行协调层(院长、副院长、行政部门);操作层(各科室、专业委员会、第三方公司)。
决策层由党委会、专家委员会、职代会三部分组成。党委会主要管理干部和重大事项的决策;专家委员会决定医院的发展方向、管理和技术;而职代会主要负责员工福利。三个部门各司其职,所有决策都采取投票表决的形式。
党委会由选举产生,党委书记和院长分设,一般院长兼任党委副书记,院长有一票否决权。刘卫东介绍,党委书记和院长之间有明确的分工,党委书记主要负责管理干部、宣传以及实行监督权等,而院长则负责决策的执行和协调。
专家委员会则是刘卫东的首创,主要负责参与以下事项的决策:1.每年的投资预算,包括投资金额、投哪个科室;2.学科的发展方向;3.人才的引进;4.医疗纠纷的处理等。专家委员会由医院里学历、职称双高的专家(原则上一个专业一个)组成,一般21-23人,保持单数,一年举行两次会议。在专家委员会下面还有57个专业委员会,和职能部门一起负责具体事务,比如抗生素管理小组委员会、院感委员会、病历资料委员会等。专业委员会由专家委员会的人带头,每年开两次会。
职代会由员工代表组成,主要负责职工福利,比如效益工资的分配方案,保险、补贴、退休人员体检等。刘卫东表示,职代会的作用是非常大的,其投票表决的结果受到政府承认,这无形中减少了院长的个人压力。刘卫东举例说:每个科室都觉得自己工作辛苦奖金低,都来找院长给优惠。建立职代会之后,可以让有意见的部门提出绩效分配方案,交给职代会投票表决,所有科室都参与,你的诉求合理与否,民意会给出答案。
刘卫东表示,把院长的权力分出去有几个明显的好处:首先能避免院长专权,出现决策上的错误;其次,决策过程是公开透明的,不会让人怀疑“暗箱操作”;此外,中国作为人情社会,院长会面对来自四面八方的压力和诉求,通过投票表决可以缓解院长的压力,这也是保护自己的一种方式。
责编|亦一
封面图来源|视觉中国
一位工作十多年的医生发五千字长文质问:为什么我做不了一个好医生?
那3名医生在使用“救命药”时,未让患者签署知情同意书,被判定为非法行医?丨医眼看法
医脉通是专业的在线医生平台,“感知世界医学脉搏,助力中国临床决策”是平台的使命。医脉通旗下拥有「临床指南」「用药参考」「医学文献王」「医知源」「e研通」「e脉播」等系列产品,全面满足医学工作者临床决策、获取新知及提升科研效率等方面的需求。
☟戳这里,更有料!
带量采购一致性评价高管变更
2025-01-09
·药渡
作者 | 陈芋
来源 | 赛柏蓝
2025开年,中纪委频繁提及医药反腐,严惩医疗、药品等民生领域“微腐败”。
01
任三甲医院院长9年
收受回扣达2亿元
1月8日,国家医保局转发央视新闻电视专题片《反腐为了人民》,揭露广东茂名高州市人民医院原党委书记、院长王茂生收受巨额回扣的案件细节。
据悉,王茂生从医近40年,早年是茂名市人民医院著名的心胸外科专家,由于技术精湛被誉为“王一刀”。
2013年,媒体曝光高州市人民医院医药采购回扣门事件,39名医务人员、5名药商涉案,主动上缴回扣款医务人员达到382名,追缴违纪金额580多万元,该院时任院长、副院长均被免职追责。
正是这时,王茂生临危受命调任高州市人民医院担任党委书记、院长,之后在该院担任“一把手”9年,从手术台走到管理岗位后,更多医药供应商找上门来。
高州市人民医院是一家三级甲等综合性公立医院,医疗服务覆盖高州及周边广大城乡地区,每年的采购体量不小。虽有回扣门事件的前车之鉴,但王茂生仍在重金引诱下铤而走险,并用各种方式来遮掩受贿行为,试图防范被查处。
据调查,王茂生大部分受贿所得都是找人代持,行贿人在广州、湛江、茂名等地为他购买多套房产、商铺,全部登记在别人名下。他还让医药供应商把部分钱存到以他人名义开的证券账户,但却是他在实际控制。
此外,王茂生还让一医药供应商在当地出资买房,装修时专门设计了一个隐蔽的夹层藏匿收受的现金,外边再用柜子遮挡。
茂名市纪委监委调取和高州市人民医院有业务往来的数百家供应商资料,排查发现,王茂生利用职权为多家供应商在药品、耗材、医疗器械的采购以及工程建设等方面提供帮助,多年来收受的回扣高达2亿余元。
医药领域的腐败典型案件中,一些腐败分子与行贿人常以系统特殊性、行业“潜规则”掩盖权钱交易,请托办事时故意互不挑明。
但腐败终究无法做到完全“无痕”,王茂生一案中的涉案药商也表示:“回扣不可能无缘无故送给他,那都是打在经营成本里面的。”在纪委监委等多部门、多手段追查下,隐匿的腐败行为终将被揭露。
02
2025开年,中纪委频繁提及医药反腐
严惩“微腐败”
1月8日,中纪委官网发布《以正风肃纪反腐实际成效赢得党心民心》一文,再提医药腐败。
文章提到,总书记去年11月在湖北调研时强调,“要深入推进风腐同查同治”“坚持正风肃纪反腐相贯通,以‘同查’严惩风腐交织问题,以‘同治’铲除风腐共性根源”。
湖北孝感市纪委书记、监委主任刘亚锋表示,2025年,将精准确定重点领域监督“小切口”,综合运用“纪巡审”联动、“组组”协作、大数据监督等方式,严肃查处国企、医药、乡村振兴和招投标等重点领域,项目审批、资金拨付、经费使用等重点环节,风腐交织、新型腐败和隐性腐败等重点问题,深化风腐同查同治,增强以案促改促治实效。
这是今年以来,中纪委第八篇提及医药腐败的文章。
中纪委发布的《高质量发展践悟丨在一线经风雨、长才干、壮筋骨》一文同样提到,要加大办案力度,深化整治金融、医药、基建工程等领域腐败问题。
除了整治医药领域“关键少数”、关键岗位,今年,民生领域“微腐败”也被更密集地提及。
1月6日,中央纪委监委驻国家卫健委纪检监察组组长曲孝丽在二十届中央纪委四次全会的采访中表示,将紧盯加重群众看病负担、欺诈骗保、扰乱正常医疗秩序等问题,与综合监督单位党组同题共答、同向发力,坚持露头就打、寸步不让,深入整治医药领域的“微腐败”和妨碍惠民政策落实的“绊脚石”。
1月2日,中纪委在《推进新征程纪检监察工作高质量发展 坚决整治群众身边不正之风和腐败问题》中强调,惩治教育医疗、养老社保、生态环保、安全生产、食品药品安全等民生领域“微腐败”,严查贪污侵占、截留挪用、虚报冒领、吃拿卡要等违纪违法行为,督促各地各部门找准“小切口”分级分类持续深入整治,特别是针对多发性、系统性、同质性问题推动开展行业系统专项整治。
在新一年的反腐工作中,医药作为权力集中、资金密集、资源富集领域仍是整治重点,同时,药品购销等环节中的“微腐败”也将被严查。
END
药渡媒体商务合作
媒体公关 | 新闻&会议发稿
张经理:18600036371(微信同号)
点击下方“药渡“,关注更多精彩内容
免责声明
“药渡”公众号所转载该篇文章来源于其他公众号平台,主要目的在于分享行业相关知识,传递当前最新资讯。图片、文章版权均属于原作者所有,如有侵权,请及时告知,我们会在24小时内删除相关信息。
微信公众号的推送规则又双叒叕改啦,如果您不点个“在看”或者没设为"星标",我们可能就消散在茫茫文海之中~点这里,千万不要错过药渡的最新消息哦!👇👇👇
高管变更带量采购
2025-01-08
·医脉通
今天的医疗圈
发生了哪些与你有关的大事?
更新、更全的医学动态
3分钟一网打尽
********
今日关键词:西藏地震,罕见传染病,医疗反腐
来源 | 医脉通
作者 | 晚报君
新闻60秒
➤华西医院6名专家紧急集结赶赴西藏
@四川卫视 7日9时5分,西藏自治区日喀则市定日县发生6.8级地震,造成重大人员伤亡。接国家卫健委医疗应急司紧急指令,四川大学华西医院迅速组建医疗救治专家组。专家组共计6人,由国家卫生健康委医疗应急工作专家组胸外科专家组组长、四川大学华西医院常务副院长刘伦旭率队并担任组长,集结急诊科、胸外科、重症医学科、创伤医学中心、神经外科、应急管理六个方向的专家,紧急驰援西藏日喀则,对地震伤员开展指导救治工作。
➤《新型抗肿瘤药物临床应用指导原则》印发
@国家卫健委官网 1月7日,国家卫生健康委发布《新型抗肿瘤药物临床应用指导原则(2024年版)》,新版在2023年版基础上修改完善,进一步规范新型抗肿瘤药物临床应用,提高肿瘤治疗的合理用药水平。指导原则指出,抗肿瘤药物临床应用须遵循药品说明书,不能随意超适应证使用,特别是有条件快速批准上市的药品,更应当保证药品说明书的时效性。
➤收回扣高达2亿余元!一名专家型医院院长“落马”
@央视新闻 1月7日,电视专题片《反腐为了人民》第三集《揭开腐败隐身衣》播出。专题片披露了广东省高州市人民医院原党委书记、院长王茂生案的细节。
王茂生,2013年4月至2022年6月,曾任广东省茂名市高州市人民医院党委书记、院长,高州市人大常委会党组成员、副主任。
王茂生从医近40年,早年是茂名市人民医院著名的心胸外科专家,由于技术精湛被誉为“王一刀”。2013年,媒体曝光了高州市人民医院医药采购回扣门事件,正副院长都被免职追责,王茂生临危受命调任该院,担任党委书记、院长。然而,他当了“一把手”之后,逐渐迷失自我。王茂生大部分受贿所得都是找人代持,行贿人在广州、湛江、茂名等地为他购买多套房产、商铺,全部登记在别人名下。他还让医药供应商把部分钱存到以他人名义开的证券账户,但却是他在实际控制。至于现金,他则让商人出资在当地给他买了套房,装修时在阳台上专门设计了一个隐蔽的夹层用来藏收受的钱款,外边再用柜子遮挡。
健康60秒
➤英国新研究:吸一支烟寿命平均缩短20分钟
@新华社 近日,英国卫生和社会保健部在其官网上发布新闻通稿,呼吁烟民在新的一年戒烟。据这篇新闻稿介绍,英国政府委托英国伦敦大学学院针对英国吸烟人士开展的研究指出,吸烟的危害比此前认为的更大。通过长期追踪分析人口健康状况数据,这一刊发在英国《瘾》月刊的研究指出,英国烟民每吸一根烟,预期寿命就会减少约20分钟,相当于平均吸一包20支的香烟可能缩短近7小时寿命。
➤江苏确诊一例罕见传染病
@江阴市人民医院、人民网科普 近日,江苏常州一位男子因身体不适前往江阴市人民医院发热门诊求诊。这位男子表示,10天前,他从非洲回国后,便开始出现发热、咳嗽、乏力以及四肢肌肉酸痛的症状,并伴有心慌、胸闷等。胸部CT结果显示,男子的双肺存在大面积的炎症病变。经过诊断,男子最终确诊为贝纳柯克斯体感染引起的急性传染病,即“Q热”。据悉,这是一种自然疫源性人畜共患病,在自然界中广泛传播,对外界环境的抵抗力很强,在极端环境中可保持长达几个月的感染性。
国际60秒
➤韩医疗界:韩国收入最高与最低群体健康寿命差距最长达近9年
@韩国观察 据韩国医学界5日消息,韩国高丽大学医学院预防医学系教授尹锡俊研究团队通过分析2008年至2020年间的健康保险数据,发现收入水平越高的人群往往健康寿命越长,而不同收入阶层的健康寿命差距最多可达近9年。研究团队根据健康保险缴费金额把收入分为五个等级,进行对比分析后发现,最高收入阶层健康寿命为74.88岁,而最低收入阶层仅为66.22岁,两者之间相差8.66年。研究团队指出,结果表明应该优先关注健康寿命较短的低收入群体,制定相应政策来解决健康不平等问题。
责编|阿泰
封面图来源|医脉通
2024年美国薪酬最高的10大工作,9个与医疗相关!中国医生心怀期待……
医生休班,竟被患者投诉要求回来看病!投诉者:医生就该没日没夜,就该无私奉献
医脉通是专业的在线医生平台,“感知世界医学脉搏,助力中国临床决策”是平台的使命。医脉通旗下拥有「临床指南」「用药参考」「医学文献王」「医知源」「e研通」「e脉播」等系列产品,全面满足医学工作者临床决策、获取新知及提升科研效率等方面的需求。
☟戳这里,更有料!
高管变更加速审批
100 项与 Maoming People's Hospital 相关的药物交易
登录后查看更多信息
100 项与 Maoming People's Hospital 相关的转化医学
登录后查看更多信息
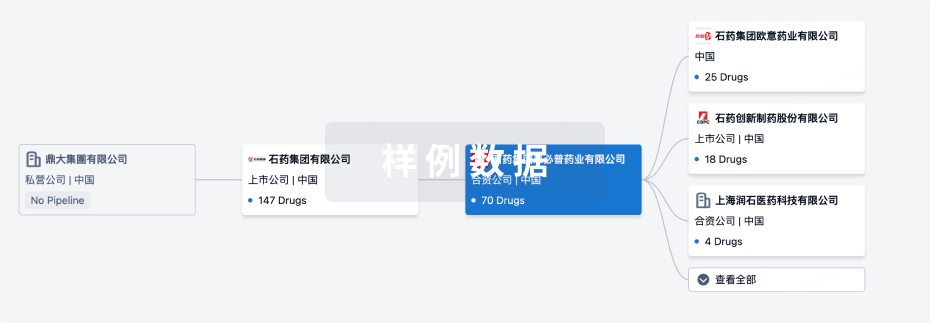
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月02日管线快照
无数据报导
登录后保持更新
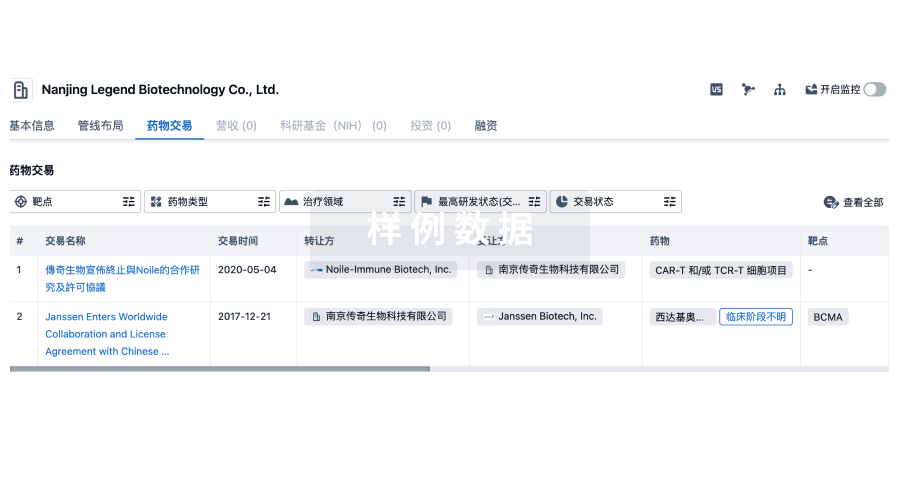
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
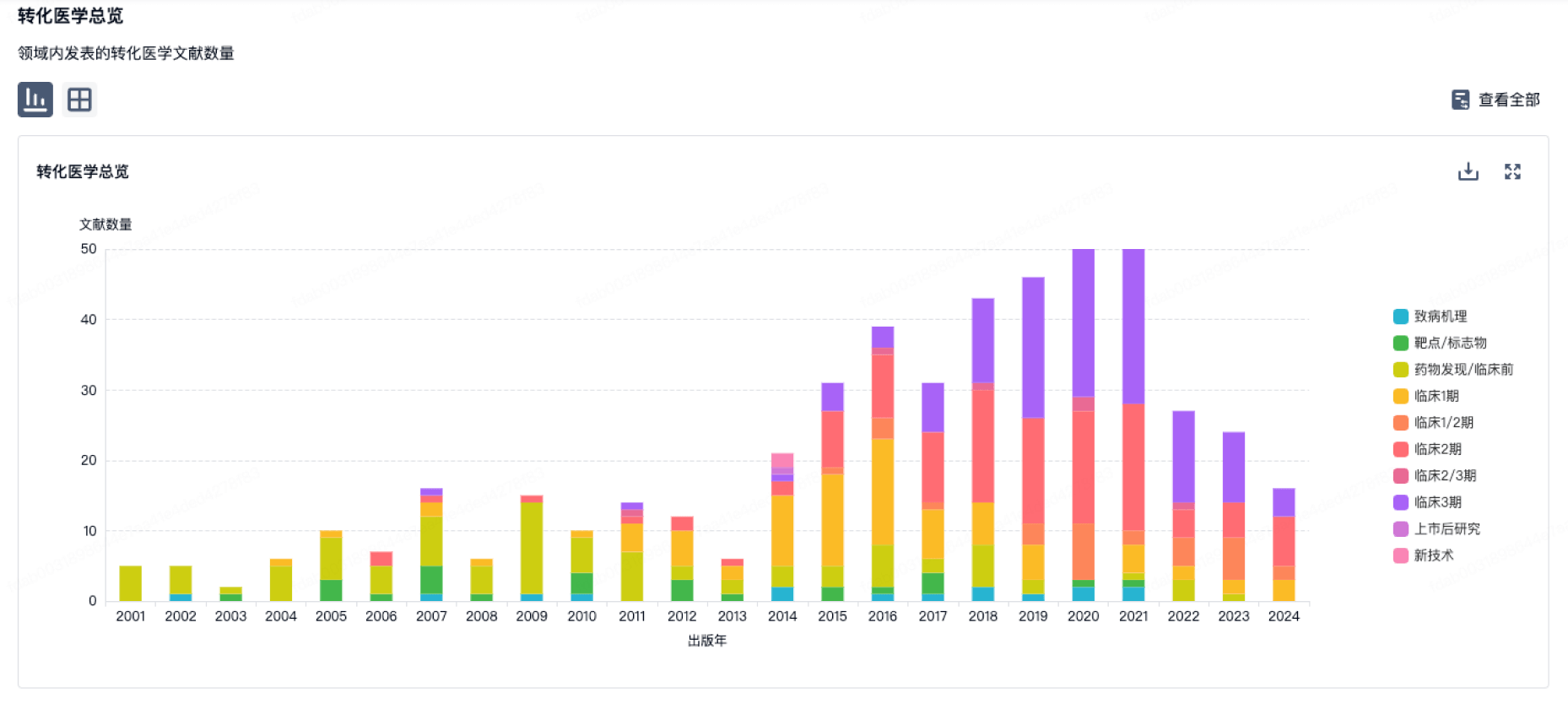
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
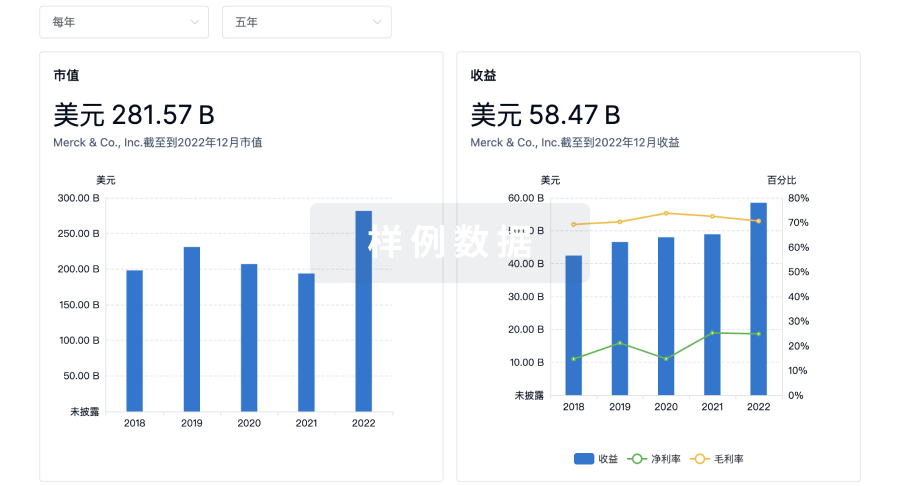
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
