预约演示
更新于:2025-05-07

Karolinska University Hospital
更新于:2025-05-07
概览
标签
肿瘤
泌尿生殖系统疾病
内分泌与代谢疾病
诊断用放射药物
预防性疫苗
多肽偶联核素
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 诊断用放射药物 | 1 |
| 核素偶联药物 | 1 |
| 治疗用放射药物 | 1 |
| 多肽偶联核素 | 1 |
| 预防性疫苗 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| GRPR(胃泌素释放肽前体受体) | 1 |
| CD44v6(CD44v6抗原) | 1 |
关联
6
项与 Karolinska University Hospital 相关的药物靶点 |
作用机制 GRPR拮抗剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制 免疫刺激剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 CD44v6 modulators |
非在研适应症- |
最高研发阶段早期临床1期 |
首次获批国家/地区- |
首次获批日期- |
653
项与 Karolinska University Hospital 相关的临床试验NCT06585358
DoseTB-individualised Dosing by Model-informed Precision Dosing for Pulmonary Tuberculosis
The goal of this observational study is to investigate whether model-informed precision dosing (MIPD), as a clinical support for early individualised dosing in addition to the national TB care program, can optimise the drug exposure of TB drugs during TB treatment.
Main research questions:
In adult patients with drug-susceptible pulmonary tuberculosis, can current dose recommendations and information received from MIPD help clinicians in a timely manner to optimise the drug exposure of TB drugs in the early treatment phase, i.e., the time from PK sampling to dose adjustment (keep or adjust dose)?
Specific aims
I. To perform a process evaluation of early MIPD for rifampicin, isoniazid, pyrazinamide and ethambutol during active TB treatment.
II. To study the target attainment of first-line TB drugs with MIPD.
III. To evaluate model precision of predicted versus detected drug concentrations.
Drug concentrations will be measured in study participants during TB treatment, and drug exposure and the optimal dose will be predicted by MIPD using pharmacokinetic population models.
Main research questions:
In adult patients with drug-susceptible pulmonary tuberculosis, can current dose recommendations and information received from MIPD help clinicians in a timely manner to optimise the drug exposure of TB drugs in the early treatment phase, i.e., the time from PK sampling to dose adjustment (keep or adjust dose)?
Specific aims
I. To perform a process evaluation of early MIPD for rifampicin, isoniazid, pyrazinamide and ethambutol during active TB treatment.
II. To study the target attainment of first-line TB drugs with MIPD.
III. To evaluate model precision of predicted versus detected drug concentrations.
Drug concentrations will be measured in study participants during TB treatment, and drug exposure and the optimal dose will be predicted by MIPD using pharmacokinetic population models.
开始日期2025-10-01 |
申办/合作机构 |
NCT06952348
HYPERtension Reduction Through WALKing Stairs Versus Brisk Walking in Individuals With Increased Cardiometabolic Risk - The HYPERWALK Randomized Controlled Trial
This clinical trial investigates whether incorporating stair walking into daily routines improves physical health in adults at risk of lifestyle-related conditions such as hypertension, type 2 diabetes, and cardiovascular disease. Participants will be randomized into three groups: (1) stair walking combined with brisk walking, (2) brisk walking alone, and (3) a control group receiving standard lifestyle advice without specific exercise instructions.
The primary objective is to assess whether the combination of stair and brisk walking leads to greater reductions in systolic blood pressure compared to brisk walking alone or standard care. Secondary outcomes include changes in cardiometabolic risk factors.
Participants in the stair walking group will be instructed to climb ≥250 steps per day (
5.5 minutes/day or
37.5 minutes/week), or complete an equivalent elevation via inclined slopes, along with ≥75 minutes of brisk walking per week. Those in the brisk walking group will walk ≥150 minutes per week. The control group will receive general lifestyle advice but no tailored physical activity goals or feedback.
Participants in both active groups will aim to double their baseline activity levels. Physical activity will be continuously monitored using wearable devices. The active groups will receive personalized feedback and motivational support throughout the 6-month intervention period.
If effective, this study may offer a simple, scalable, and low-cost intervention model for use in clinical and public health settings, emphasizing personalized goals, remote monitoring, and behavioral support.
The primary objective is to assess whether the combination of stair and brisk walking leads to greater reductions in systolic blood pressure compared to brisk walking alone or standard care. Secondary outcomes include changes in cardiometabolic risk factors.
Participants in the stair walking group will be instructed to climb ≥250 steps per day (
5.5 minutes/day or
37.5 minutes/week), or complete an equivalent elevation via inclined slopes, along with ≥75 minutes of brisk walking per week. Those in the brisk walking group will walk ≥150 minutes per week. The control group will receive general lifestyle advice but no tailored physical activity goals or feedback.
Participants in both active groups will aim to double their baseline activity levels. Physical activity will be continuously monitored using wearable devices. The active groups will receive personalized feedback and motivational support throughout the 6-month intervention period.
If effective, this study may offer a simple, scalable, and low-cost intervention model for use in clinical and public health settings, emphasizing personalized goals, remote monitoring, and behavioral support.
开始日期2025-06-01 |
申办/合作机构 |
NCT06794775
SWE-NEO: Swedish NeoAdjuvant Trial Comparing Anti-PD-1 Monotherapy to Combined Anti-CTLA-4/anti-PD-1 Blockade in Resectable Stage III Melanoma
At present two studies (SWOG S1801 and NADINA) have demonstrated superiority when using neoadjuvant treatment compared to adjuvant treatment only, but no studies have compared PD-1 monotherapy (SWOG 1801 regimen) to the PD-1/CTLA-4 combination (NADINA regimen) therapy. The SWE-NEO study aims to compare these two regimens, where the PD-1/CTLA-4 combination is potentially more effective, but also associated with more side effects.
开始日期2025-04-15 |
100 项与 Karolinska University Hospital 相关的临床结果
登录后查看更多信息
0 项与 Karolinska University Hospital 相关的专利(医药)
登录后查看更多信息
39,269
项与 Karolinska University Hospital 相关的文献(医药)2025-12-31·Journal of Obstetrics and Gynaecology
Surgical outcomes after gender-affirming hysterectomies: a consecutive case series of 72 patients
Article
作者: Alder, Susanna ; Papaikonomou, Kiriaki ; Tebani, Leonora ; Rooda, Ilmatar ; Damdimopoulou, Pauliina ; Dhejne, Cecilia ; Gidlöf, Sebastian
2025-12-31·The Journal of Maternal-Fetal & Neonatal Medicine
Changes in short-term variation of antenatal cardiotocography to identify intraamniotic infection: a historical cohort study
Article
作者: Holzmann, Malin ; Birgisdottir, Brynhildur Tinna ; Hulthén Varli, Ingela ; Åden, Ulrika ; Andersson, Tomas ; Saltvedt, Sissel ; Lu, Ke ; Abtahi, Farhad
2025-12-31·Annals of Medicine
Effects of multidomain lifestyle intervention on frailty among older men and women – a secondary analysis of a randomized clinical trial
Article
作者: Antikainen, Riitta ; Strandberg, Timo ; Soininen, Hilkka ; Lehtisalo, Jenni ; Kyrönlahti, Saila ; Kivipelto, Miia ; Tuomilehto, Jaakko ; Laatikainen, Tiina ; Saarela, Laura ; Kulmala, Jenni ; Havulinna, Satu ; Ngandu, Tiia ; Levälahti, Esko
107
项与 Karolinska University Hospital 相关的新闻(医药)2025-04-10
Gothenburg, April 10, 2025 – Elicera Therapeutics AB (publ), a clinical stage cell and gene therapy company developing next generation cancer treatments based on oncolytic viruses and CAR T-cell therapies, armed with immune-activating properties via the company’s commercially available iTANK platform, today announced that the Data Safety and Monitoring Board (DSMB) has completed its first assessment of the ongoing Phase I/IIa CARMA clinical trial with the CAR T-cell therapy ELC-301 for the treatment of B-cell lymphoma. The DMSB recommended that the study continue as planned.
The dose-escalation study, conducted in collaboration with Uppsala University as sponsor, previously reported a complete response (no detectable tumor) in the first treated patient at the initial follow-up one month after completing treatment, with no serious adverse events observed. Two additional patients have since been treated at the lowest dose level in the first dosing group (cohort 1). Elicera intends to report preliminary results from the study as each dosing cohort is completed. Preliminary efficacy data from the first cohort is expected to be presented at the 7th Swedish Cancer Research Meeting in Malmö on May 22.
Following the DSMB’s recommendation to proceed, treatment of patients in the second cohort at next dose level can now begin.
For further information, please contact:
Jamal El-Mosleh, CEO, Elicera Therapeutics AB (publ)
Phone: +46 (0) 703 31 90 51 jamal.elmosleh@elicera.com
Certified Advisor
Mangold Fondkommission AB
About the CARMA Study CARMA is a phase I/IIa clinical study evaluating the safety and efficacy of the CAR T-cell therapy ELC-301 in the treatment of patients with B-cell lymphoma. The study is divided into a dose-escalation phase (phase I) and a dose-expansion phase (phase IIa). Phase I primarily aims to establish the optimal dose and safety profile in up to 12 patients, while phase IIa will further evaluate the efficacy of the maximum tolerated dose in an additional six patients. Phase I is planned to include three cohorts (dosing groups), with three patients in the first and second cohorts, and six patients in the third dcohort, who are expected to receive the maximum tolerated dose. The CARMA study is being conducted at Uppsala University Hospital and Karolinska University Hospital in Huddinge.
About ELC-301 ELC-301 is a fourth-generation CAR T-cell therapy targeting the CD20 antigen, armed with the company’s iTANK platform to activate a broader and more comprehensive parallel immune response against cancer. CAR T-cells are a form of cell therapy created by genetically modifying a patient’s T-cells to express a synthetic receptor (chimeric antigen receptor, CAR). This receptor is specifically designed to target a single tumor antigen—a molecule visible on the surface of cancer cells—and enables the T-cells to locate, bind to, and destroy the cancer cells. About the iTANK platform The iTANK technology platform has been developed for arming and enhancing CAR T-cells to meet two of the major challenges CAR T-cell therapies face in the treatment of solid tumors: a very diverse set of tumor antigen targets and a very hostile tumor microenvironment. The technology is used to incorporate a transgene into CAR T-cells encoding a neutrophil activating bacterial protein (NAP). NAP secreted from the CAR(NAP) T-cells has been shown to be able to enhance the function of CAR T-cells and importantly activating a parallel bystander immune response against the cancer via CD8+ killer T-cells. This is expected to lead to a broad attack against most antigen targets on cancer cells. The iTANK platform is used to enhance the company’s own CAR T-cells but can also be universally applied to other CAR T-cell therapies under development. Proof-of-concept data was published in Nature Biomedical Engineering in April 2022. The publication, titled “CAR T cells expressing a bacterial virulence factor triggers potent bystander antitumor responses in solid cancers” (DOI number: 10.1038/s41551-022-00875-5) can be found here: https://www-nature-com.libproxy1.nus.edu.sg/articles/s41551-022-00875-5. More information about iTANK platform is available here: https://www.elicera.com/technology
About Elicera Therapeutics AB Elicera Therapeutics AB (publ) has developed the patented gene technology platform iTANK that enables the arming of new and existing CAR T-cell therapies targeting aggressive and relapsing cancer forms. Elicera Therapeutics thereby addresses a well-defined and vast market. The company’s CAR T-cell therapies have shown a potent effect toward solid tumors which are recognized as particularly difficult to treat and constitute the majority of cancer cases. The company addresses a global multibillion market in cell therapy through its offering of non-exclusive licensing of the iTANK-platform to companies in the pharmaceutical industry. Elicera Therapeutics has four internal development projects in immune therapy that separately have the potential to generate substantial value through exclusive out-licensing agreements. The company’s share is traded on Nasdaq First North Growth Market. For additional information, visit www.elicera.com.
细胞疗法临床1期免疫疗法引进/卖出临床2期
2025-04-04
Gothenburg, April 4, 2025 – Elicera Therapeutics AB (publ), a clinical stage cell and gene therapy company developing next generation cancer treatments based on its proprietary commercial technology platform iTANK, today announced that the company’s Chief Scientific Officer, Professor Magnus Essand, has been invited to speak at the Swedish Cancer Research Meeting (SCRM) 2025 in Malmö on May 22.
SCRM is Sweden’s largest cancer research meeting, held every other year, where prominent international researchers are also invited. At SCRM2025, leading representatives from academia, healthcare, and industry will gather to exchange knowledge, present new research findings, and foster collaboration. The goal is to strengthen Sweden’s cancer research ecosystem and create the conditions for joint efforts that can lead to improved treatments and a deeper understanding of cancer.
Magnus Essand, one of the co-founders of Elicera Therapeutics and Professor of Gene Therapy at Uppsala University, will participate as a speaker at SCRM2025. His presentation, titled "Novel cell and gene therapies for the treatment of cancer – The Uppsala experience", will highlight the company’s progress in developing novel cell and gene therapies for cancer treatment.
During his talk, Professor Essand will present Elicera Therapeutics’ CAR T-cell program and the company’s proprietary platform technology, iTANK, which is used to arm CAR T-cells to trigger a broad immune activation against cancer. He will also present preliminary efficacy data from cohort 1 of the ongoing CARMA study, which evaluates the safety and efficacy of ELC-301 – the company’s iTANK-armed CAR T-cell therapy targeting B-cell lymphoma.
In light of this, Elicera has decided not to present the cohort 1 data at the ISCT conference, in order to generate greater impact at SCRM2025. This decision also enables the inclusion of data from a longer follow-up period, which is expected to provide a more informative and valuable data set.
For further information, please contact:
Jamal El-Mosleh, CEO, Elicera Therapeutics AB (publ)
Phone: +46 (0) 703 31 90 51 jamal.elmosleh@elicera.com
Certified Advisor
Mangold Fondkommission AB
About the CARMA Study CARMA is a phase I/IIa clinical study evaluating the safety and efficacy of the CAR T-cell therapy ELC-301 in the treatment of patients with B-cell lymphoma. The study is divided into a dose-escalation phase (phase I) and a dose-expansion phase (phase IIa). Phase I primarily aims to establish the optimal dose and safety profile in up to 12 patients, while phase IIa will further evaluate the efficacy of the maximum tolerated dose in an additional six patients. Phase I is planned to include three cohorts (dosing groups), with three patients in the first and second cohorts, and six patients in the third dcohort, who are expected to receive the maximum tolerated dose. The CARMA study is being conducted at Uppsala University Hospital and Karolinska University Hospital in Huddinge.
About ELC-301 ELC-301 is a fourth-generation CAR T-cell therapy targeting the CD20 antigen, armed with the company’s iTANK platform to activate a broader and more comprehensive parallel immune response against cancer. CAR T-cells are a form of cell therapy created by genetically modifying a patient’s T-cells to express a synthetic receptor (chimeric antigen receptor, CAR). This receptor is specifically designed to target a single tumor antigen—a molecule visible on the surface of cancer cells—and enables the T-cells to locate, bind to, and destroy the cancer cells. About the iTANK platform The iTANK technology platform has been developed for arming and enhancing CAR T-cells to meet two of the major challenges CAR T-cell therapies face in the treatment of solid tumors: a very diverse set of tumor antigen targets and a very hostile tumor microenvironment. The technology is used to incorporate a transgene into CAR T-cells encoding a neutrophil activating bacterial protein (NAP). NAP secreted from the CAR(NAP) T-cells has been shown to be able to enhance the function of CAR T-cells and importantly activating a parallel bystander immune response against the cancer via CD8+ killer T-cells. This is expected to lead to a broad attack against most antigen targets on cancer cells. The iTANK platform is used to enhance the company’s own CAR T-cells but can also be universally applied to other CAR T-cell therapies under development. Proof-of-concept data was published in Nature Biomedical Engineering in April 2022. The publication, titled “CAR T cells expressing a bacterial virulence factor triggers potent bystander antitumor responses in solid cancers” (DOI number: 10.1038/s41551-022-00875-5) can be found here: https://www-nature-com.libproxy1.nus.edu.sg/articles/s41551-022-00875-5. More information about iTANK platform is available here: https://www.elicera.com/technology
About Elicera Therapeutics AB Elicera Therapeutics AB (publ) has developed the patented gene technology platform iTANK that enables the arming of new and existing CAR T-cell therapies targeting aggressive and relapsing cancer forms. Elicera Therapeutics thereby addresses a well-defined and vast market. The company’s CAR T-cell therapies have shown a potent effect toward solid tumors which are recognized as particularly difficult to treat and constitute the majority of cancer cases. The company addresses a global multibillion market in cell therapy through its offering of non-exclusive licensing of the iTANK-platform to companies in the pharmaceutical industry. Elicera Therapeutics has four internal development projects in immune therapy that separately have the potential to generate substantial value through exclusive out-licensing agreements. The company’s share is traded on Nasdaq First North Growth Market. For additional information, visit www.elicera.com.
细胞疗法基因疗法引进/卖出临床1期免疫疗法
2025-03-18
LUND, Sweden, March 18, 2025 /PRNewswire/ --
Oncorena is pleased to announce that the FDA has approved the Company's IND application to initiate the Phase I/II study Oncorella-1: A Phase 1/2, open label, single arm study on safety, tolerability and anti-tumor efficacy of orellanine treatment in patients with metastatic clear-cell or papillary renal cell carcinoma (NCT05287945, ONC001-CL-001).
In the study Oncorella-1, up to 75 patients with severe metastatic renal cancer requiring dialysis will be enrolled. These patients have exhausted their treatment options and ONC175 represents a potentially new first-in-class treatment for patients with urgent unmet medical need.
The study is currently being conducted at Karolinska University Hospital in Stockholm, Sweden.
Börje Haraldsson, CEO & co-founder of Oncorena comments:
"This approval brings us closer to being able to evaluate the potential for this novel treatment in patients in desperate need for new and better options. We are excited to start the first US site, MD Andersson in Houston, Texas, where the study will be led by investigator Professor Nizar Tannir, a world-leading expert in renal cancer."
About ONC175
ONC175 is an investigational drug product under development that contains synthetically produced orellanine as active ingredient. Orellanine is highly specific to the kidney and induces irreversible renal failure. It is clinically well-known that orellanine does not affect organs other than the kidneys.
In pioneering preclinical studies ONC175 demonstrated a powerful and highly organ-specific mode of action capable of eradicating human metastatic renal cancer cells. The primary goal is to develop ONC175 as a potential curative treatment of metastatic renal cell carcinoma in patients with no remaining kidney function, i.e., patients on dialysis.
About kidney cancer
Approximately 400,000 patients are affected by kidney cancer globally according to the WHO. The disease can often be cured by surgery if detected early, but the prognosis is less favorable if there are metastases. Today, the disease is treated with various types of targeted and immuno-active drugs, that seldom are curative. There is therefore a great and urgent unmet medical need for new, effective and safe drugs.
For more information, please contact
Börje Haraldsson, M.D., Ph.D., CEO, and CSO Oncorena AB
E-mail: [email protected]
Phone: +46 70 267 9544
This information was brought to you by Cision
The following files are available for download:
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床研究临床申请免疫疗法
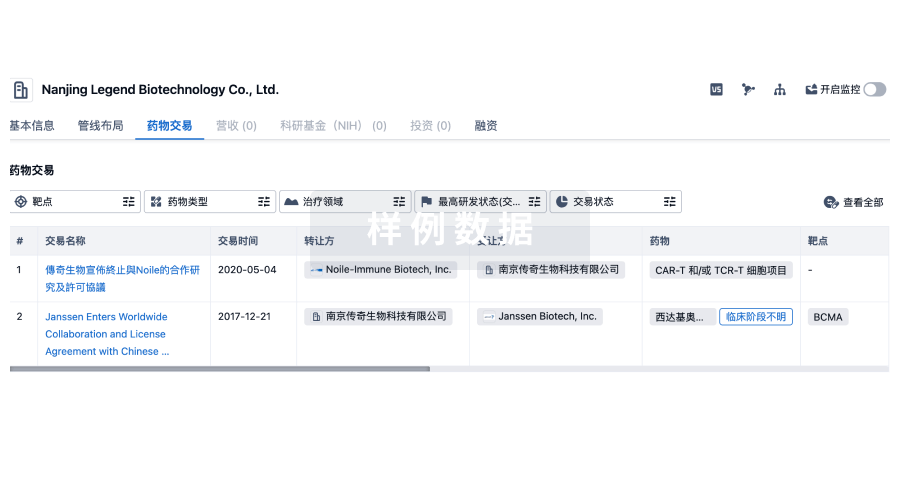
100 项与 Karolinska University Hospital 相关的药物交易
登录后查看更多信息
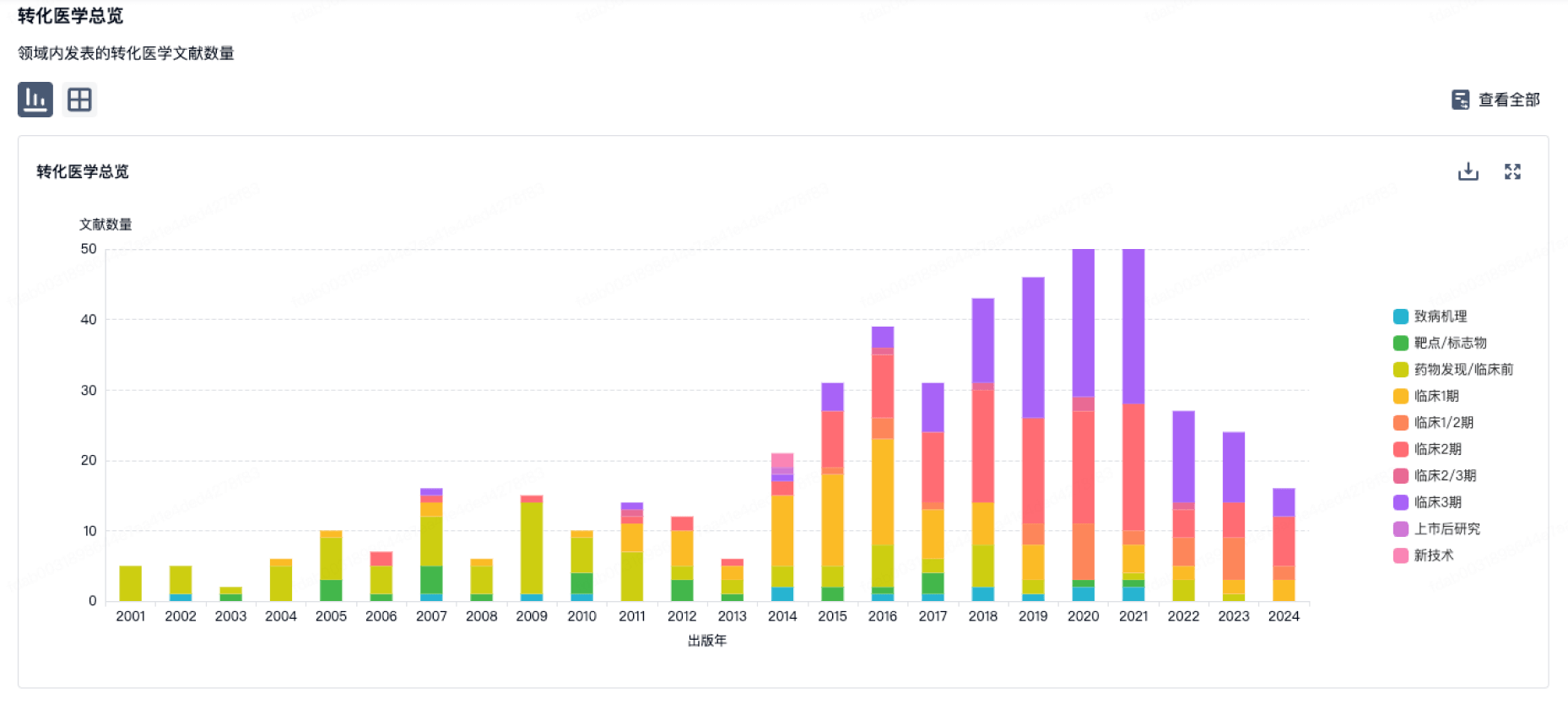
100 项与 Karolinska University Hospital 相关的转化医学
登录后查看更多信息
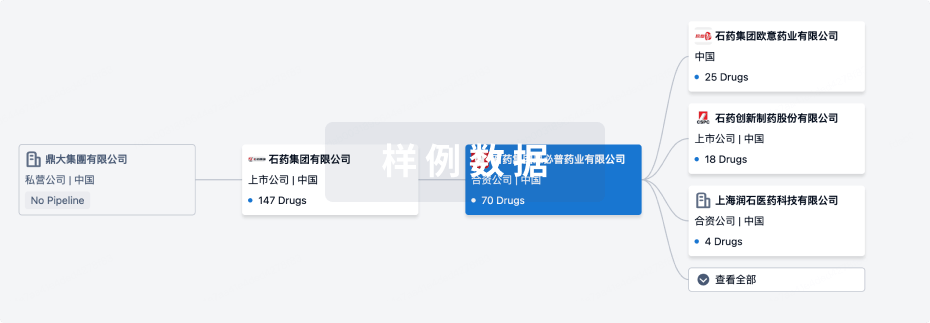
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月11日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床1期
3
3
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
[177Lu]Lu-AKIR001 ( CD44v6 ) | 甲状腺未分化癌 更多 | 临床1期 |
Dendritic cells vaccine(Karolinska University Hospital) | 转移性黑色素瘤 更多 | 临床1期 |
68Ga-NOTA-PEG2-RM26 ( GRPR ) | 前列腺癌 更多 | 临床1期 |
11C-PE2I ( DAT ) | 帕金森病 更多 | 无进展 |
AZD-3043 ( GABAA receptor ) | 镇静 更多 | 无进展 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
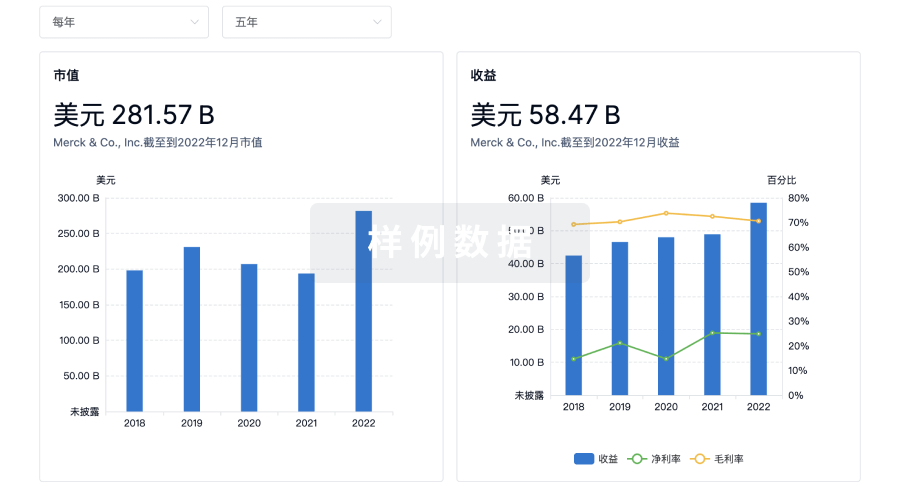
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

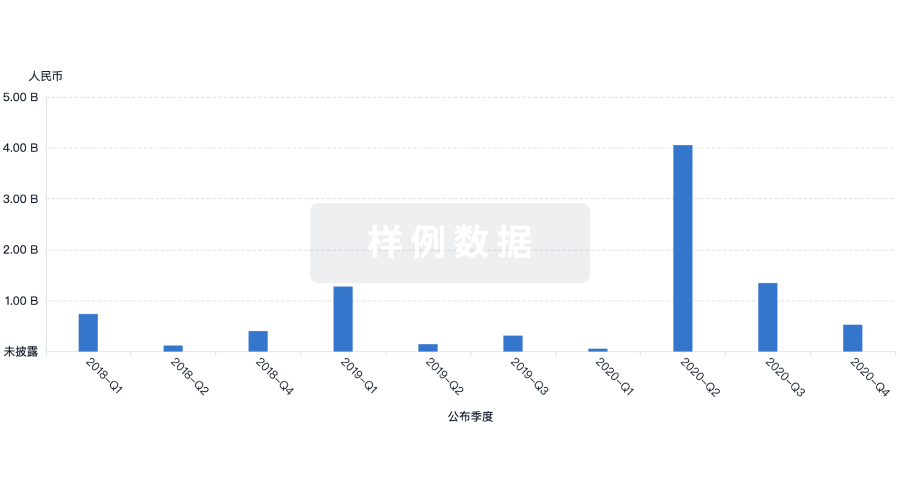
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
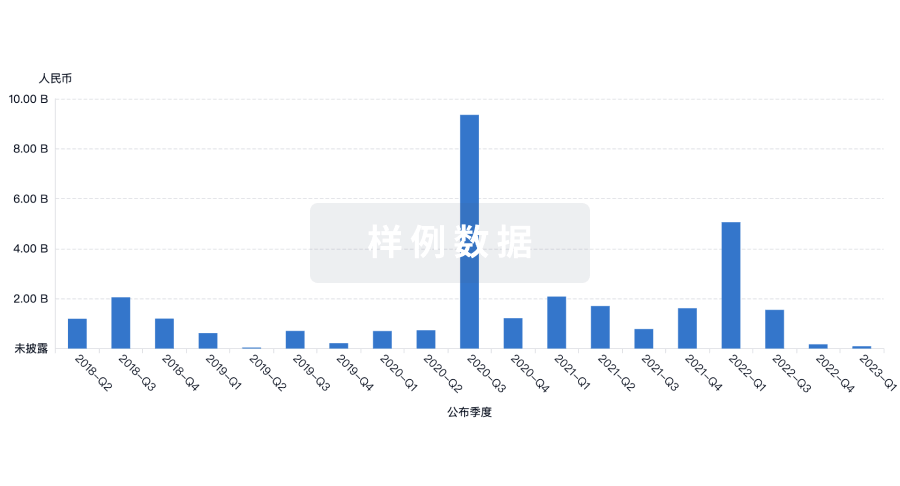
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
