更新于:2024-12-10
MK-4882
更新于:2024-12-10
概要
基本信息
非在研机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)临床前 |
特殊审评- |
结构
分子式C42H50N8O7 |
InChIKeyQKFUCROVTLGTAV-VOIOCNMVSA-N |
CAS号1246470-32-5 |
关联
100 项与 MK-4882 相关的临床结果
登录后查看更多信息
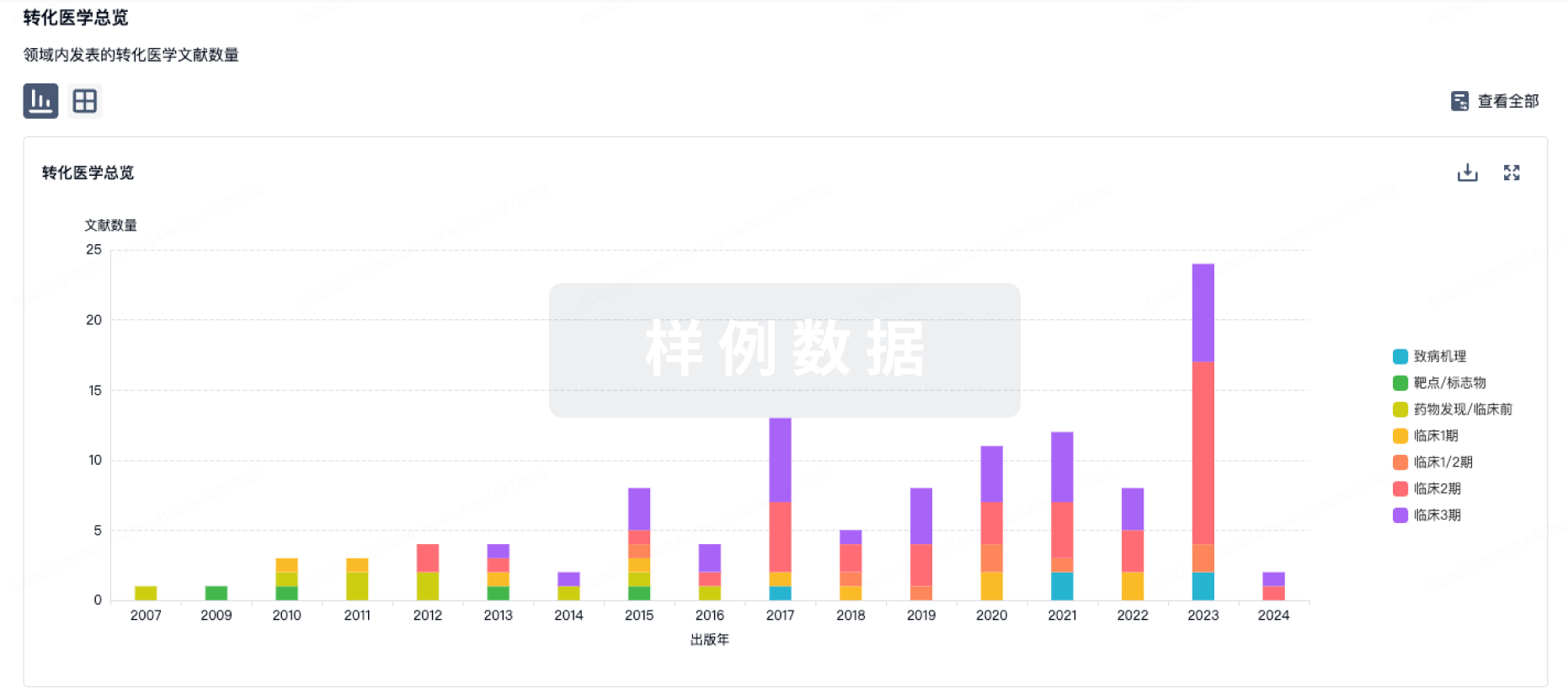
100 项与 MK-4882 相关的转化医学
登录后查看更多信息
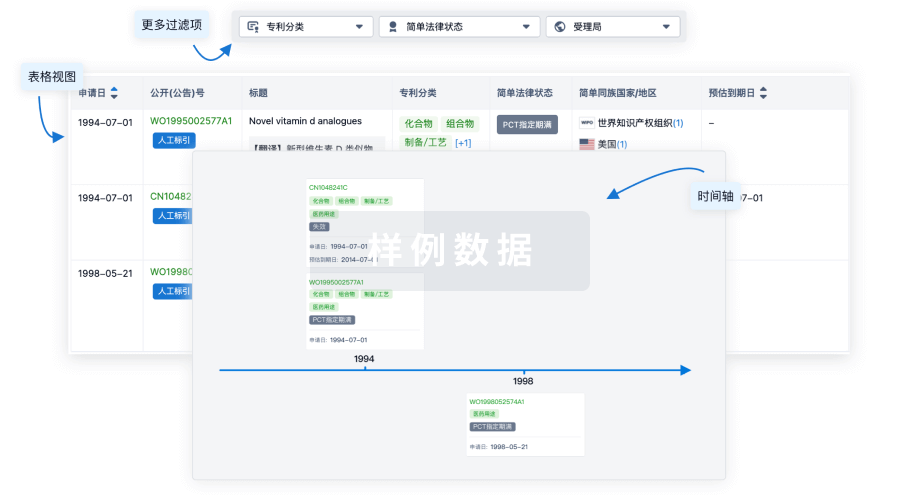
100 项与 MK-4882 相关的专利(医药)
登录后查看更多信息
1
项与 MK-4882 相关的文献(医药)2016-08-01·Bioorganic & medicinal chemistry letters4区 · 医学
Discovery of potent macrocyclic HCV NS5A inhibitors
4区 · 医学
Article
作者: Carr, Donna ; Liu, Rong ; Wong, Michael ; McMonagle, Patricia ; Zeng, Qingbei ; Curry, Stephanie ; Chen, Lei ; Vellekoop, A Samuel ; Zhong, Bin ; Vibulbhan, Bancha ; Ingravallo, Paul ; Selyutin, Oleg ; Dwyer, Michael P ; Martin, Gregory S ; Yu, Wensheng ; Kozlowski, Joseph A ; Asante-Appiah, Ernest ; Nair, Anilkumar G ; Coburn, Craig A ; Lahser, Fred ; Jiang, Yueheng ; Holst, Christian L ; Hu, Bin ; Fells, James ; Ji, Tao ; Tong, Ling ; Rokosz, Laura ; Agrawal, Sony ; Rosenblum, Stuart B
HCV NS5A inhibitors have demonstrated impressive in vitro virologic profiles in HCV replicon assays and robust HCV RNA titer reduction in the clinic making them attractive components for inclusion in an all oral fixed-dose combination (FDC) regimen for the treatment of HCV infection. Merck's effort in this area identified MK-4882 and MK-8325 as early development leads. Herein, we describe the discovery of potent macrocyclic NS5A inhibitors bearing the MK-8325 or MK-4882 core structure.
2
项与 MK-4882 相关的新闻(医药)2021-02-11
According to the World Health Organization (WHO), there are currently 63 vaccines in clinical development for COVID-19 and 179 in preclinical development. In the U.S., two vaccines have been granted emergency use authorization (EUA) by the U.S. Food and Drug Administration (FDA), Pfizer-BioNTech and Moderna. The vaccine candidate developed by Johnson & Johnson has been submitted for EUA and may be authorized by the end of February.
Globally, several other vaccines have been authorized and are being rolled out in various countries and regions, but not necessarily in the U.S. These include AstraZeneca-University of Oxford, Russia’s Sputnik V, Sinovac Biotech, Novavax and CanSino Biologics.
It's unlikely that there will be a long-term market for the 63 vaccines in development or that many of the vaccines in preclinical development will find funding and a rationale for continued development. However, there are some big surprises among the list of major players in the vaccine space who either dropped their programs or have been significantly delayed.
Merck
One of the bigger surprises has been Merck, which is typically a vaccines powerhouse, but was slow to enter the COVID-19 vaccine race and quicker to exit it. The company is the world’s second-largest vaccine manufacturer. The company officially launched efforts to develop a vaccine in May 2020 when it acquired Austria-based Themis and partnered with Florida-based Ridgeback Therapeutics to develop MK-4882, an orally-available antiviral candidate. In November 2020, Merck acquired Maryland-based OncoImmune and its COVID-19 candidate CD24rFc for $425 million in cash upfront.
But in late January 2021, Merck announced it was halting development of its two COVID-19 vaccine candidates, V590 and V591, after poor responses in Phase I trials. They were shifting their attention to advancing two therapeutic drugs, MK-4482 and MK-7110.
And with some apparent pressure, Merck is in talks with the U.S. government and several companies that have vaccines, namely Pfizer and Johnson & Johnson, about assisting in vaccine manufacturing. Even with those efforts, it’s not a matter of flipping a switch, and could take months to begin the manufacturing process.
“I think there’s a broader recognition, certainly within the U.S. government, but governments around the world, that this is a bit more complicated than we had at one time thought,” said Michael Nally, chief marketing officer of Merck. “If there’s a way that we can help think through that, and prepare the world for what we see on the horizon, that’s where we’re focused.”
Sanofi and GlaxoSmithKline
Perhaps even more surprising has been the lackluster results of GlaxoSmithKline (GSK), the largest vaccine maker in the world, and its partnership with Sanofi, also a top vaccine manufacturer. On December 11, 2020, the two companies reported that their COVID-19 vaccine efforts were being delayed after an insufficient immune response in older clinical trial participants. At that time, they reported that their vaccine would not be available until the end of 2021, if at all.
Sanofi reported interim data from its Phase I/II vaccine trial showed an immune response comparable to that seen in recovered COVID-19 patient in participants aged 18 to 49 years. But, in adults aged 50 and older, there was an “insufficient immune response.” In order to provide high-level immune response across all age groups, the companies were going to attempt to refine the concentration of antigen in the vaccine.
Instead of launching into a Phase III trial, they were instead planning a Phase IIb study with an improved antigen formulation. If the data is positive, a Phase III trial might start in the second quarter of 2021. If the results are good—and the rollout of vaccines worldwide don’t make the actual study difficult to complete—the vaccine might be available by the fourth quarter of the year.
Pasteur Institute
France’s Pasteur Institute announced in late January that it was ending development of its COVID-19 vaccine after disappointing Phase I clinical trial results. The Phase I trial began in August 2020 and was well-tolerated, but did not create sufficient immune response.
AstraZeneca-University of Oxford
The AstraZeneca-University of Oxford vaccine is not a failure. But its development has been marred by quite a bit of confounding data and apparent missteps. In April 2020, as the vaccine programs really started moving, the University of Oxford was far ahead of almost everyone with plans to launch a 6,000-participant clinical trial in May. Their head-start was based on earlier work on a coronavirus vaccine in 2019, largely on SARS-CoV, which allowed for a quick shift to SARS-CoV-2, the virus that causes COVID-19. At that point, with a deal with AstraZeneca, they thought they might have a vaccine authorized by September 2020 and were viewed as clear frontrunners.
In September, however, AstraZeneca and Oxford University paused the Phase III COVID-19 trial after report of an unexplained illness—transverse myelitis—in a U.K. patient. Although the trial restarted in the U.K. and other countries within a few days, it was delayed for weeks in the U.S. while investigators pored over the data.
In November, AstraZeneca-Oxford reported high-level results from an interim analysis of the vaccine, with trials in the U.K. and Brazil demonstrating efficacy of up to 90%. But there was a problem, too. One cohort received half-doses of the first dose by accident, and provided confounding results—90% efficacy, compared to 62% efficacy in patients who received the full first dose. The combined analysis demonstrated average efficacy of 70%. In December, it was authorized in the U.K. and other countries—not the U.S., where it has yet to complete a Phase III trial—but has come with its own variety of controversies.
Although designed for two doses to be taken about four weeks apart, the U.K. has staggered the doses by about 12 weeks to extend the supply of the drug. Studies are ongoing to determine if this is an effective strategy.
At the end of January, the vaccine was authorized by the European Union, but they acknowledge there was not enough data to prove if it was effective in people over the age of 55.
And on February 8, South Africa reported that it had halted distribution of the vaccine after data suggested it “provides minimal protection” against mild disease from the South African variant. The study, which had not been peer-reviewed yet, showed the vaccine had high efficacy against the original non-B.1.351 variants found in South Africa, but very low efficacy against the more contagious B.1.351 variant emerging in the country.
Most Read Today
疫苗紧急使用授权合作
2021-01-26
2021年1月25日,默沙东公司宣布,在I期临床反应不佳之后,它将停止开发其两种为V590和V591的COVID-19候选疫苗。他们将注意力转移到开发针对COVID-19的两种治疗药物MK-4482和MK-7110。
默沙东公司在2020年5月收购了位于奥地利的Themis时在疫苗竞赛中来得很晚。同月,默沙东与总部位于佛罗里达州的Ridgeback Therapeutics合作开发了可口服的抗病毒药物MK-4882。去年11月,它以4.25亿美元的前期现金收购了总部位于马里兰州的OncoImmune及其COVID-19候选CD24Fc(MK-7110)。
在I期试验中,V590和V591通常具有良好的耐受性,但该公司报告说,免疫应答不如从COVID-19感染自然恢复的人所观察到的免疫应答低。
默沙东研究实验室总裁Dean Y. Li说
:“我们感谢与我们合作开发这些候选疫苗的合作伙伴以及试验中的志愿者。” “我们坚决致力于为减轻这种大流行给患者,医疗保健系统和社区带来的负担的全球努力做出贡献。”
默沙东公司拥有成功开发疫苗的历史,因此当他们来到COVID-19疫苗领域如此晚时,这让人感到有些惊讶。他们选择了利用弱化病毒的传统方法。V590利用了该公司埃博拉疫苗的技术,而V591技术则基于欧洲使用的麻疹疫苗。该公司仅在2020年底之前完成了I期研究的招募志愿者,而Pfizer-BioNTech和Moderna当时已经在报告III期数据,并已向美国食品和药物管理局(FDA)提交上市以进行紧急使用授权(EUA)。两家公司的COVID-19疫苗都在美国和欧洲范围内使用。
默沙东研究实验室(Merck Research Laboratories)传染病和疫苗临床研究高级副总裁Nick Kartsonis表示,I期临床试验的结果“
令人失望,令人有些意外
”。与其他COVID-19疫苗相比,两种疫苗产生的中和抗体都更少。
我们没有前进所需的一切。
”
联邦政府的“Operation Warp Speed”为六项疫苗项目的开发提供了财政支持,其中一项就是Moderna。辉瑞和BioNTech尽管获得了提供疫苗的合同,但并未获得开发支持。默沙东公司不是Operation Warp Speed旗下投资组合公司之一。相反,它与国际艾滋病疫苗倡议(IAVI)合作,并获得了一些政府研究资金。两种疫苗均设计为单次注射,而不是Moderna和Pfizer-BioNTech疫苗的两次注射。辉瑞-BioNTech的注射间隔约21天,而Moderna的注射间隔约28天。
其他两种治疗剂是MK-7110,以前是CD124Fc,是通过OncoImmune收购获得的。它是潜在的一流的重组融合蛋白,可调节对SARS-CoV-2病毒的炎症反应。它主要通过靶向新型免疫途径检查点来发挥作用。来自III期试验的中期数据表明,中度至重度COVID-19住院患者的死亡或呼吸衰竭风险降低了50%。他们预计第一季度将全面读取数据。2020年12月,默沙东公司与美国政府签署了一项供应协议,以提高该药的生产和分销水平。
第二种药物molnupiravir(MK-4482)是与Ridgeback Bio合作开发的口服抗病毒药物。这项正在进行中的II/III期临床试验正在住院患者以及门诊患者中进行。研究预计将在2021年5月结束,但默沙东公司计划在第一季度发布初步疗效数据。
尽管辉瑞-BioNTech和Moderna疫苗项目以及其他有希望的COVID-19疫苗取得了巨大的成功,例如强生公司,英国授权的牛津阿斯利康大学和Novavax公司。2020年12月,赛诺菲和葛兰素史克推迟了其III期临床试验的启动,原因是临床试验中老年患者的免疫反应不足。结果,他们将所有可用的可能性推迟到2021年底,如果有的话。
强生疫苗的 III期试验可能已经准备在本周或下周进行数据读出。该公司于2021年1月14日发布了有关该疫苗的I/II期中期数据,并指出该疫苗已经产生了至少71天的免疫应答。71天的天数与年龄在18至55岁的参与者的中期数据相关。
数据表明该疫苗可诱导免疫反应,并且通常具有良好的耐受性。在第29天的90%以上的志愿者和在57天的18至55岁之间的100%的志愿者中,单次接种疫苗后观察到了针对SARS-CoV-2(引起COVID-19的病毒)的中和抗体。
由阿斯利康和牛津大学开发的第四种疫苗已在英国获得批准,但距离在美国甚至已经提交疫苗还有几个月的时间。该药物已于2020年12月30日由英国MHRA授权。像辉瑞BioNTech和Moderna注射一样需要两剂,间隔三到四个星期。
英国的授权基于在英国和巴西进行的临床试验数据。美国的审评仍在进行中。有趣的是,据报道,在美国,该试验中的某些人有资格接受辉瑞BioNTech疫苗或Moderna疫苗。
正在研发的另一种疫苗是Novavax。澳大利亚TGA于本周批准了该公司疫苗的临时决定,这意味着该公司可以申请临时注册,这是在提交临床数据以供临时批准之前的步骤。Novavax还在进行一项单独的英国试验,该试验完成了15,000多名志愿者的报名。预计本季度将进行数据读取。在美国,Novavax试验于2020年12月28日开始。
版权声明:本文转自医药合作投融资联盟,如不希望被转载的媒体或个人可与我们联系,我们将立即删除
【关于药融圈】药融圈围绕我国生物医药产业链,针对生物医药大数据、技术和资本投资、药融园(产业园)等开展系列系统性工作,促进我国生物医药产业健康发展,完善产业链,共同面对全球合作和竞争。
点分享
点点赞点在看
疫苗合作并购抗体
100 项与 MK-4882 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 丙型肝炎 | 临床前 | 美国 | 2013-10-14 | |
| 丙型肝炎 | 临床前 | 中国 | 2013-10-14 |
登录后查看更多信息
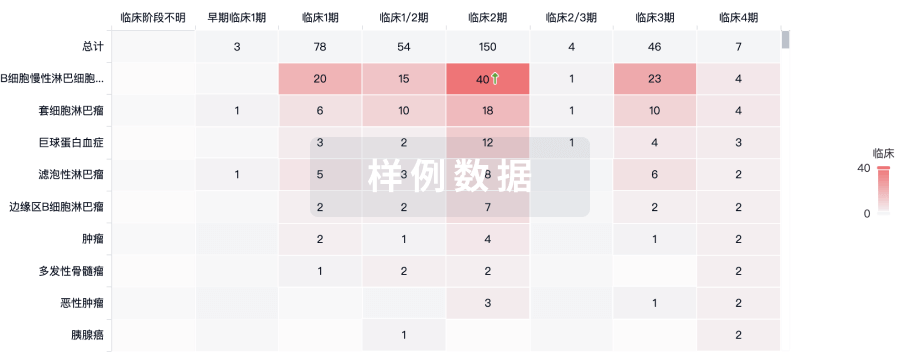
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


