预约演示
更新于:2025-07-25
(R)-[11C]Pk11195
更新于:2025-07-25
概要
基本信息
原研机构 |
在研机构- |
权益机构- |
最高研发阶段终止临床2期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
结构/序列
分子式C21H21ClN2O |
InChIKeyRAVIZVQZGXBOQO-NIQXDKTISA-N |
CAS号157727-22-5 |
关联
4
项与 (R)-[11C]Pk11195 相关的临床试验NCT05220514
Mayo Clinic Health System-wide Neurological, Vascular and Neurovascular Events With SARS-CoV-2- Part II
The purpose of this study is to measure, monitor, and analyze long term effects of SARS-CoV-2. The main purpose is to assess the post-hospitalization outcomes of patients who were diagnosed with SAR-CoV-2 by comparing to patients who were hospitalized with an acute neurological disease.
开始日期2022-01-19 |
申办/合作机构  Mayo Clinic Mayo Clinic [+1] |
NCT03368677
Targeting SPMS: Effect of Teriflunomide Treatment on Microglial Activation in an MS Patient Cohort at Risk of Progression. A [11C]PK11195 Brain PET Study
To evaluate the effect of teriflunomide treatment on microglial activation in late stage multiple sclerosis.
开始日期2017-12-01 |
申办/合作机构 |
EUCTR2015-001202-34-IT
A preliminary, multicenter study on the relationship between cortical damage and blood brain barrier damage in Multiple Sclerosis patients with high cortical disease activity. Correlation between [11C]-PK-11195 or [18F]-NAF PET (Positron Emission Tomography) and high field MRI (Magnetic Resonance Imaging): a synergistic effect by using a double-technique approach. - A preliminary, multicenter study on the relationship between cortical damage and blood brain barrier
开始日期2016-05-04 |
100 项与 (R)-[11C]Pk11195 相关的临床结果
登录后查看更多信息
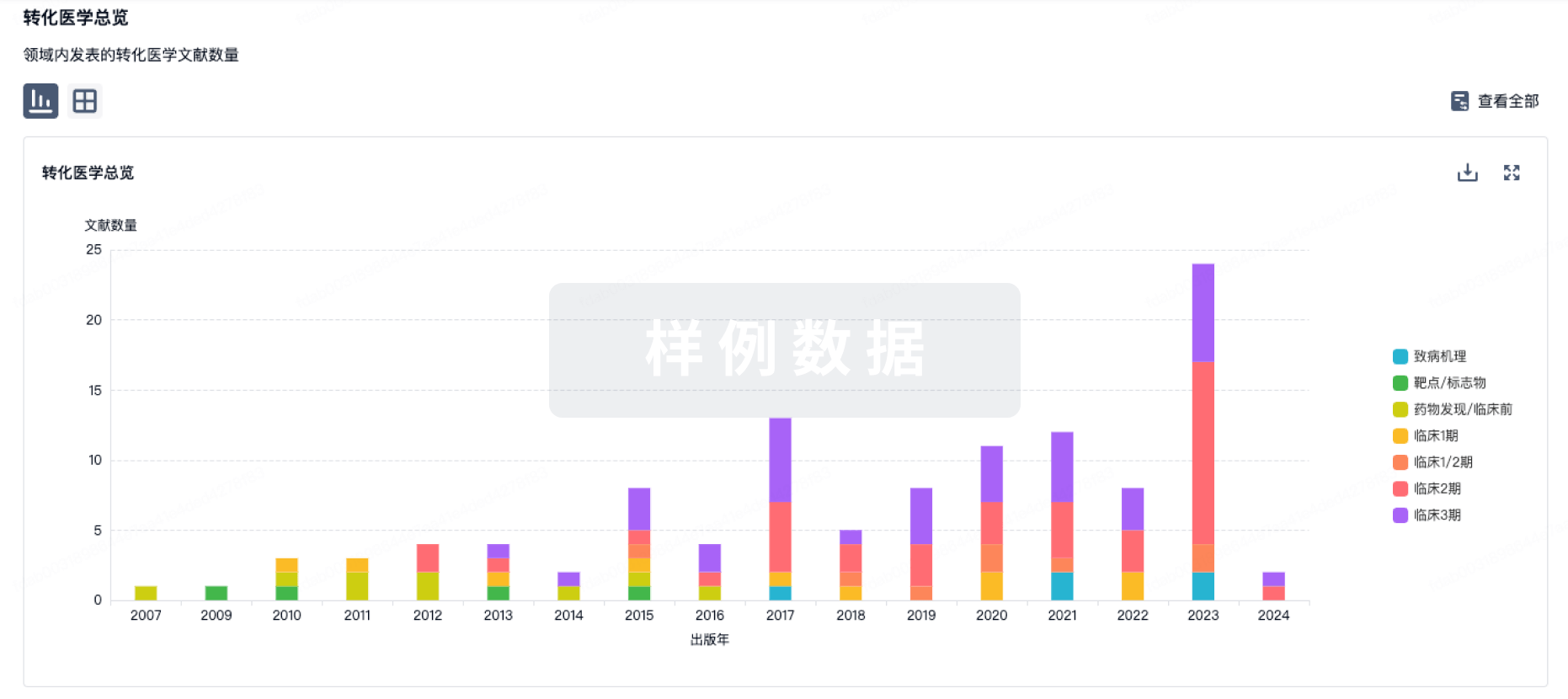
100 项与 (R)-[11C]Pk11195 相关的转化医学
登录后查看更多信息
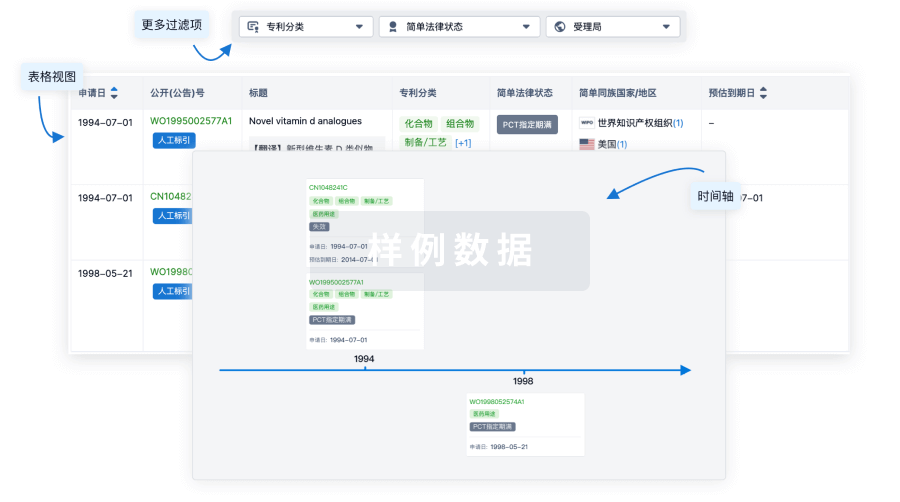
100 项与 (R)-[11C]Pk11195 相关的专利(医药)
登录后查看更多信息
114
项与 (R)-[11C]Pk11195 相关的文献(医药)2025-05-13·BRAIN
Perivascular space dysfunction in cerebral small vessel disease is related to neuroinflammation
Article
作者: Chen, Yutong ; Low, Audrey ; Markus, Hugh S ; Brown, Robin B ; Hong, Hui ; Tozer, Daniel J
Abstract:
Enlarged perivascular spaces are a feature of cerebral small vessel disease, and it has been hypothesized that they might reflect impaired glymphatic drainage. The mechanisms underlying enlargement of perivascular spaces are not fully understood, but both increased inflammation and blood–brain barrier (BBB) permeability have been hypothesized to play a role. We investigated the relationship between perivascular spaces and both CNS and peripheral inflammation, in addition to BBB permeability, in cerebral small vessel disease.Fifty-four symptomatic sporadic cerebral small vessel disease patients were studied. Perivascular spaces were quantified both using a visual rating scale and by measurement of the volume of perivascular spaces in the white matter and the basal ganglia. PET-MRI was used to measure microglial activation using the radioligand 11C-PK11195, and simultaneously, BBB permeability was acquired using dynamic contrast-enhanced MRI. We determined 11C-PK11195 binding and BBB permeability in the local vicinity of individual perivascular spaces in concentric shells surrounding the perivascular spaces. In addition, both mean 11C-PK11195 binding and BBB permeability in both the white matter and the basal ganglia were determined. To assess systemic inflammation, a panel of 93 blood biomarkers relating to cardiovascular disease, inflammation and endothelial activation were measured.Within the white matter, tissue in closest proximity to perivascular spaces displayed greater 11C-PK11195 binding (P < 0.001) in the vicinity of perivascular spaces. Higher white matter perivascular spaces burden on the visual rating scale was associated with higher white matter 11C-PK11195 binding (ρ = 0.469, false discovery rate-corrected P = 0.009); values for the volume of perivascular spaces showed a similar trend. In contrast, there were no associations between the burden of basal ganglia perivascular spaces and 11C-PK11195 binding. No marker of perivascular spaces was correlated with blood–brain barrier permeability. There was no association between markers of perivascular spaces and blood biomarkers of systemic inflammation.Our findings demonstrate that white matter perivascular spaces are associated with increased 11C-PK11195 binding, consistent with neuroinflammation playing a role in enlargement of white matter perivascular spaces. Further longitudinal and intervention studies are required to determine whether the relationship between neuroinflammation and enlarged perivascular spaces is causal.
2024-01-01·Neuro-oncology advances
Evidence for inflammation in normal-appearing brain regions in patients with growing sporadic vestibular schwannoma: A PET study
Article
作者: Lewis, Daniel ; Alfaifi, Bandar ; Hinz, Rainer ; Hammerbeck-Ward, Charlotte ; Pathmanaban, Omar N ; Rutherford, Scott A ; Wadeson, Andrea ; King, Andrew T ; Coope, David J ; Jackson, Alan
Abstract:
Background:
Nonauditory symptoms can be a prominent feature in patients with sporadic vestibular schwannoma (VS), but the cause of these symptoms is unknown. Inflammation is hypothesized to play a key role in the growth and symptomatic presentation of sporadic VS, and in this study, we investigated through translocator protein (TSPO) positron emission tomography (PET) whether inflammation occurred within the “normal appearing” brain of such patients and its association with tumor growth.
Methods:
Dynamic PET datasets from 15 patients with sporadic VS (8 static and 7 growing) who had been previously imaged using the TSPO tracer [11C](R)-PK11195 were included. Parametric images of [11C](R)-PK11195 binding potential (BPND) and the distribution volume ratio (DVR) were derived and compared across VS growth groups within both contralateral and ipsilateral gray (GM) and white matter (WM) regions. Voxel-wise cluster analysis was additionally performed to identify anatomical regions of increased [11C](R)-PK11195 binding.
Results:
Compared with static tumors, growing VS demonstrated significantly higher cortical (GM, 1.070 vs. 1.031, P = .03) and whole brain (GM & WM, 1.045 vs. 1.006, P = .03) [11C](R)-PK11195 DVR values. The voxel-wise analysis supported the region-based analysis and revealed clusters of high TSPO binding within the precentral, postcentral, and prefrontal cortex in patients with growing VS.
Conclusions:
We present the first in vivo evidence of increased TSPO expression and inflammation within the brains of patients with growing sporadic VS. These results provide a potential mechanistic insight into the development of nonauditory symptoms in these patients and highlight the need for further studies interrogating the role of neuroinflammation in driving VS symptomatology.
2023-08-01·European journal of neurology
Longitudinal stability of progression-related microglial activity during teriflunomide treatment in patients with multiple sclerosis.
Article
作者: Rajander, Johan ; Lehto, Jussi ; Nylund, Marjo ; Hariri, Parisa ; Sucksdorff, Marcus ; Matilainen, Markus ; Wahlroos, Saara ; Vuorimaa, Anna ; Airas, Laura
BACKGROUND AND PURPOSE:
The aim was to study brain innate immune cell activation in teriflunomide-treated patients with relapsing-remitting multiple sclerosis.
METHODS:
Imaging with 18-kDa translocator protein positron emission tomography (TSPO-PET) using the [11 C]PK11195 radioligand was employed to assess microglial activity in the white matter, thalamus and areas surrounding chronic white matter lesions in 12 patients with relapsing-remitting multiple sclerosis who had been treated with teriflunomide for at least 6 months before inclusion. Magnetic resonance imaging (MRI) was used to measure lesion load and brain volume, and quantitative susceptibility mapping (QSM) was used to detect iron rim lesions. These evaluations were repeated after 1 year of inclusion. Twelve age- and gender-matched healthy control subjects were imaged for comparison.
RESULTS:
Half of the patients had iron rim lesions. In TSPO-PET, the proportion of active voxels indicating innate immune cell activation was slightly greater amongst patients compared with healthy individuals (7.7% vs. 5.4%, p = 0.033). The mean distribution volume ratio of [11 C]PK11195 was not significantly different in the normal-appearing white matter or thalamus amongst patients versus controls. Amongst the treated patients, no significant alteration was observed in positron emission tomography distribution volume ratio, the proportion of active voxels, the number of iron-rim-positive lesions, lesion load or brain volume during follow-up.
CONCLUSIONS:
Compared to controls, treated patients exhibited modest signs of diffuse innate immune cell activity, which was unaltered during follow-up. Lesion-associated smoldering inflammation was negligible at both timepoints. To our knowledge, this is the first study applying both TSPO-PET and QSM-MRI to longitudinally evaluate smoldering inflammation.
1
项与 (R)-[11C]Pk11195 相关的新闻(医药)2024-09-19
摘要:抗体-药物偶联物(ADCs)由单克隆抗体组成,这些抗体靶向肿瘤细胞,并通过连接体与细胞毒素药物相连。ADCs利用抗体的靶向特性,在识别肿瘤抗原后,通过内吞作用将细胞毒素药物传递到肿瘤细胞中。这种精确的方法旨在选择性地杀死肿瘤细胞,同时尽量减少对正常细胞的伤害,提供安全有效的治疗益处。近年来,随着ADC的发展,抗肿瘤治疗取得了显著进展,为患者提供了新的强效治疗选择。已有300多种ADCs针对各种肿瘤适应症进行了探索,其中一些已获准用于临床,但同时也出现了诸如由于抗原表达、ADC处理和有效载荷等因素导致的耐药性等挑战。本综述旨在概述ADC发展的历程、它们的结构、作用机制、近期组成进展、靶点选择、已完成和正在进行的临床试验、耐药机制和干预策略。此外,它还将深入探讨具有新颖标记、连接体、有效载荷和创新作用机制的ADCs的潜力,以增强癌症治疗选择。ADCs的演变也导致了组合疗法的出现,这是一种新的治疗方式,以提高药物疗效。
1.引言自从1913年德国科学家保罗·埃尔利希提出“神奇子弹”概念以来,抗体偶联药物(ADCs)的发展经历了成功和挫折。ADCs是将高度靶向的抗体分子与高度细胞毒性的小分子结合在一起的药物分子。然而,ADC的概念最初是在1967年提出的,直到2000年,第一种ADC药物吉妥单抗-奥佐加米辛(GO)才被美国食品药品监督管理局(US FDA)批准用于治疗急性髓系白血病(AML)。然而,由于随后的临床发现表明其益处有限,但增加了死亡率,特别是由于肝窦闭塞性疾病,GO后来被撤回。随后,在接下来的十年中,ADC药物的发展进展有限。第二种ADC药物在2010年推出,并在2011年获得US FDA批准用于治疗霍奇金淋巴瘤和系统性间变性大细胞淋巴瘤(sALCL)。2013年,ADCs在获得US FDA批准曲妥珠单抗-恩美坦辛(TDM-1)用于治疗人表皮生长因子受体-2(HER2)阳性乳腺癌方面取得了另一个突破。这标志着第一种针对实体瘤的ADC。从那时起,ADC药物的研究迅速发展,市场上出现了越来越多的ADC药物。ADC药物从上个世纪的诞生到成熟演变的过程在图1中描绘。
图 1 自1910年提出“神奇子弹”概念以来,过去100年中抗体-药物偶联物(ADC)发展的重要事件时间线。ADC,抗体-药物偶联物;ALCL,间变性大细胞淋巴瘤;AML,急性髓系白血病;B-ALL,B细胞急性淋巴细胞性白血病;DLBCL:弥漫大B细胞淋巴瘤;HER2,人表皮生长因子受体-2;FRα,叶酸受体-α;HR,激素受体;TNBC,三阴性乳腺癌。
抗体药物的研究和开发不断取得进展,导致市场上的ADC药物被分为三代。第一代ADCs由于有效载荷的毒性不足、结构不稳定和毒素容易脱落等限制,导致治疗窗口狭窄和高失败率。第二代ADCs使用人源化单克隆抗体和更强效的细胞毒素药物,与第一代相比,显示出降低的免疫原性、提高的药物效果和更宽的治疗窗口。第三代ADC药物引入了位点特异性偶联,提高了药物-抗体比率(DAR)的一致性,减少了毒副作用,提高了效果,从而扩大了治疗窗口。此外,抗体优化和新小分子提高了药物的特异性和治疗效果,具有对表达较低抗原水平的细胞的结合活性。
ADC药物表现出独特的药理特性,在抗肿瘤治疗领域显示出显著活性,同时与传统化疗相比保持了更高的安全性水平。除了追求提高效果外,ADC药物当前的研究和开发重点还包括解决治疗耐药性问题。本综述旨在深入探讨ADC作用和耐药性机制的最新进展,以及对抗这种耐药性的策略。本文进一步详细检查了促成所有ADC获得US FDA批准的关键试验,特别关注证据的稳健性。它还为该领域的潜在未来研究方向提供了有价值的见解。
2.ADCs在靶向癌症治疗中的机制见解
ADCs由通过连接体连接到细胞毒素药物的抗体组成(图2)。这种独特的结构为ADC药物提供了多种优势,使它们能够结合传统小分子化疗的强大杀伤能力和抗体的靶向输送特性。在ADCs给药后,抗体部分与肿瘤细胞表面的靶标抗原结合。随后,肿瘤细胞摄取ADC分子。一部分ADC可以附着在内吞体内的Fc受体上,有助于其运输到细胞表面。通过FcRn介导的转运,这部分随后被释放到细胞外。相反,其他ADC-抗原复合物进入溶酶体,那里的酶或酸性条件可以降解ADC。因此,释放出细胞毒素,这些毒素可以损害DNA或阻碍肿瘤细胞的分裂,最终导致它们的死亡(图3)。上述ADC机制与特定靶向抗体、强效细胞毒素药物、连接体和靶标抗原密切相关。
图 2 抗体-药物偶联物的结构。ADC的三个基本组成部分包括抗体、细胞毒素有效载荷和连接体。抗体分为四种主要类型:小鼠抗体、嵌合抗体、人源化抗体和全人抗体。细胞毒素有效载荷可以根据其作用机制分为两类:作用于DNA的分子,如卡利奇霉素、二卡霉素、PBDs、SN-38和DXd,以及作用于微管的分子(如奥瑞斯塔丁和美登素衍生物)。连接体大致可以分为两类:可切割和不可切割。PBD,吡咯并苯并二氮杂环;SN-38,7-乙基-10-羟基喜树碱;DXd,德鲁替康。
图 3 ADCs的作用机制。抗体与细胞表面的抗原结合(1),形成ADC-抗原复合物。这些复合物随后通过受体介导的内吞作用被带入溶酶体(2)。在溶酶体内,ADCs可以被酶分解或酸性环境破坏(3)。这种分解释放出细胞毒素有效载荷,这些有效载荷可以损伤DNA或抑制微管聚合(4)。
2.1.抗体
ADC的抗体部分识别靶标抗原,在疾病治疗中,通常使用单克隆抗体,因为它们能够特异性地识别单一抗原。这种特异性增强了药物的靶向性并减少了非靶向效应。
单克隆抗体可以分为四种主要类型:小鼠抗体、嵌合抗体、人源化抗体和全人抗体。最初,通常使用小鼠衍生的抗体,但它们在进入人体时存在免疫原性、效果差和半衰期短等问题。1975年,杂交瘤技术使嵌合抗体得以发展,它们具有人类恒定区域和小鼠可变区域。嵌合抗体减少了小鼠成分,同时增强了人类特性,尽管免疫原性仍然是一个关注点。为了解决这个问题,研究人员进一步将小鼠成分最小化到互补决定区,从而产生了人源化抗体。随着重组蛋白表达技术的进步,可以生产全人抗体。目前,市场上或正在开发中的大多数ADC使用人源化或全人抗体,这些抗体表现出强大的抗原结合能力、高选择性、长半衰期和最小的免疫原性。
双特异性抗体ADC治疗最近越来越受欢迎。通过将双特异性抗体纳入ADCs,研究人员旨在增强ADCs的细胞内化。双特异性ADCs可以策略性地设计为结合同一靶标抗原上的两个不同、不重叠的表位,导致形成强大的受体簇和改善的内化、溶酶体运输和降解过程。此外,双特异性ADCs可以被设计为靶向不同的抗原。例如,研究表明,针对HER2和催乳素受体(PRL-R)的双特异性ADCs在杀死同时表达HER2和PRL-R的目标细胞方面比仅针对HER2的ADCs表现出更高的效果。这表明将ADC靶标(例如,HER2)与快速内化蛋白(例如,PRL-R)结合有助于迅速内化和溶酶体降解。此外,ADCs中双特异性抗体的使用可以通过结合肿瘤细胞上的两种抗原来提高肿瘤靶向的选择性。尽管双特异性抗体ADCs前景看好,但该领域仍处于研究和开发的早期阶段,大多数产品目前正在进行临床前调查。
2.2.效应分子:细胞毒素有效载荷
ADCs的细胞毒素有效载荷作为杀死癌细胞的强大终端效应成分。这些效应分子在ADCs中的毒性通常高于普通小分子,这是ADCs固有的特性。每个抗体通常携带有限数量的效应分子,称为DAR值,它决定了ADC药物的药代动力学、效力和毒性。在传统的随机药物偶联策略中,具有不同DAR值的药物混合在一起,每个抗体的DAR可能在0到8之间变化。DAR的异质性将导致药代动力学、效力和安全性的异质性,并可能导致药物结构不稳定、增加非靶向毒性、药物聚集等问题,不利于后续开发。每个抗体通常携带有限数量的效应分子,导致异质性,影响药代动力学、效力、安全性和整体药物稳定性。虽然最大化DAR可以增强抗肿瘤效果,但必须在增加蛋白质聚集和ADC清除等问题上进行平衡,这可能会降低效果和安全性。通过位点特异性偶联、工程化半胱氨酸残基、抗体序列中的非天然氨基酸,以及通过糖基转移酶和转谷氨酰胺酶的酶促偶联等策略,旨在使DAR更加均匀。保持适当的DAR值仍然是一个需要进一步探索的关键方面。
通常用于癌症治疗的细胞毒素分子通常根据其作用机制分为三类。第一类包括针对DNA或拓扑异构酶I的分子,如卡利切阿米辛、二卡霉素、吡咯并苯并二氮杂环、SN-38(伊立替康的活性形式)和德鲁替康。第二类由用作有效载荷的微管抑制剂组成,如来自海洋来源的奥瑞斯塔丁和埃里布林,以及来自植物的五月丹素。尽管在ADCs中探索了其他微管抑制剂,如紫杉醇衍生物、长春新碱和秋水仙碱,但它们的效力有限。第三类包括烷基化剂,如二卡霉素。
已经开发了几种双有效载荷ADC合成策略,以将两种药物连接到同一连接体上。例如,Levengood等人引入了第一种双载药ADC,它在具有垂直保护的半胱氨酸残基的短肽配体上结合了单甲基奥瑞斯塔丁E(MMAE)和单甲基奥瑞斯塔丁F(MMAF),实现了DAR为16(8+8)。这种双载药ADC表现出强大的抗肿瘤活性,通过添加补充有效载荷,可能克服肿瘤细胞中的耐药性。
此外,一些ADC药物通过“旁观者效应”杀死癌细胞。可切割连接体对于诱导旁观者效应至关重要。含有可切割连接体的ADC被高抗原表达的肿瘤细胞内化。一旦进入细胞,药物在溶酶体中降解,释放出自由毒素(疏水性和未带电的),它们可以穿过细胞膜直接杀死靶细胞或穿透膜到达肿瘤微环境。在肿瘤微环境中,它们可以攻击周围表达低或无抗原的肿瘤细胞(称为旁观者细胞),从而表现出旁观者效应。然而,需要注意的是,可切割连接体也可能带来潜在的安全性风险。旁观者效应可能导致自由毒素从目标肿瘤细胞扩散或进入血流,可能对非肿瘤组织造成毒性。
2.3.连接体
连接体是ADC设计中的关键组成部分,通过共价偶联促进抗体和细胞毒素有效载荷之间的连接。连接体不仅主要用作连接抗体和效应分子,而且连接体还发挥着超越简单连接的多方面作用。连接体的各种属性,如偶联化学、长度和空间位阻,直接影响ADC的毒性、特异性、稳定性和效力。一个理想的连接体应该在循环中表现出稳定性(半衰期大约是ADC的10倍),并在肿瘤内化后有效释放细胞毒素有效载荷。此外,连接体的亲水性或亲脂性可以影响有效载荷偶联并降低免疫原性。研究人员已经探索了不同类型的连接体,大致可分为两类:可切割和不可切割连接体。可切割连接体具有从ADC释放效应分子代谢物的能力,允许其进入细胞,无论是在肿瘤部位还是在内吞体和溶酶体中。这些可切割连接体进一步细分为化学可切割连接体和酶促可切割连接体,如基于肽的连接体、基于β-葡萄糖醛酸的连接体和基于磷酸的连接体。值得注意的是,基于β-葡萄糖醛酸的连接体由β-葡萄糖醛酸酶敏感连接体和β-半乳糖苷酶敏感连接体组成。这些连接体的过早切割可能导致效应分子损害正常细胞。另一方面,不可切割连接体,如硫醚连接体和马来酰亚胺己酰连接体,需要ADC进入细胞并随后被溶酶体分解以释放效应分子。带有不可切割连接体的ADC依赖于抗体的完全溶酶体酶促降解以释放有效载荷,导致连接体同时解离。因此,使用不可切割连接体必须确保连接体-药物复合物保持杀死肿瘤细胞的能力。考虑到有效载荷的细胞毒性和旁观者效应,尽管一些批准的不可切割有效连接体存在,但在ADC开发中优先考虑可切割连接体。
近几十年来,在优化ADC的结构和扩展机制方面取得了显著进展。这包括开发各种可切割连接体,如组织蛋白酶可切割、酸可切割、谷胱甘肽可切割、Fe(II)可切割、新型酶促可切割、光响应和生物正交连接体。这些新型可切割连接体显示出增加的选择性,以针对肿瘤。其中,组织蛋白酶、谷胱甘肽和酸可切割连接体已经进行了广泛研究,并纳入了批准的ADCs。值得注意的是,磷酸酶响应和生物正交可切割连接体具有克服传统ADCs中细胞内药物释放限制的潜力。这些新连接体的早期数据是有希望的,并预计将显著推进ADC药物的未来发展。
2.4.靶标抗原
在以往的研究中,人们设计了多种策略来对抗癌症,包括中和靶标受体、降低受体水平、中断细胞途径、抗体依赖性细胞介导的细胞毒性、补体依赖性细胞毒性、ADCs依赖性细胞吞噬作用、抑制免疫检查点。然而,ADCs采取了不同的方法。这种方法首先涉及抗体部分与靶标抗原结合,然后通过受体内化被运输进细胞,使效应分子发挥细胞毒性作用。因此,靶标抗原的选择在ADC中起着至关重要的作用。
小分子药物的一个主要缺点是缺乏特异性,导致它们不仅对癌细胞有毒性,而且对正常细胞也有毒性。ADCs通过精确地将效应分子传递到癌细胞中有效地克服了这个问题。因此,自从20世纪70年代发现第一个肿瘤抗原以来,识别癌细胞的特定抗原变得越来越可行,从而加速了ADCs的发展。
在用于乳腺癌治疗的ADCs中,单克隆抗体最常靶向的受体是HER2。大约90-95%的AML患者在白血病母细胞表面表达CD33蛋白,使其成为治疗这种疾病的理想靶标。P97受体在黑色素瘤细胞表面高度表达,每个细胞的数量在80,000到280,000之间,而其在其他肿瘤细胞表面的表达水平非常低。因此,ADC药物L49-vcMMAF可以有选择地作用于黑色素瘤细胞,而不影响其他肿瘤细胞。然而,需要注意的是,仅仅抗原的高表达并不能保证ADC药物的有效性。例如,尽管CD21高度表达,但它在B细胞表面与CD19形成复合物,阻碍了其内化。因此,针对CD21的ADC药物无法有效地进入细胞发挥其作用。
适合ADC治疗的靶标抗原必须满足以下条件。首先,靶标抗原应在肿瘤细胞上高度表达,并且在正常细胞上的表达应很低。其次,虽然可以使用噬菌体展示技术分离编码目标特异性抗体可变区的基因,但许多用于ADCs的抗体仍然是通过杂交瘤技术生产的。因此,目标分子需要具有抗原性。第三,靶标抗原应该存在于细胞表面,以便与外部环境中的ADCs发生作用。最后,靶标抗原应具有内化能力,允许结合的ADC分子进入细胞内。
这些条件至关重要,因为ADCs的功能依赖于它们。尽管有300多个基于抗体治疗的靶标抗原,但只有大约50个被开发为ADC靶标(表1)。值得注意的是,尽管大多数批准的ADCs靶向内化抗原,也可以开发靶向癌细胞表面或基质中非内化抗原的ADCs。
3.治疗试验
ADCs开发技术一直在不断进步,导致越来越多的ADC药物被开发用于不同类型的癌症。目前,有300多个ADC候选药物正在不同的临床试验阶段进行研究,由于它们令人鼓舞的结果,市场份额有所增加。
ADCs最流行的研发集中在肿瘤上。此外,ADC药物也可以通过旁观者效应在肿瘤抗原表达低的患者中发挥作用,从而扩大了适应症人群。临床试验还揭示了适应症的扩展,包括感染(例如,人类免疫缺陷病毒、肺部疾病)、自身免疫疾病(如脊柱关节炎和阿尔茨海默病)以及代谢性疾病(如肥胖症和糖尿病)。
在肿瘤学领域,目前批准的ADCs针对癌细胞过度表达的特定蛋白质,如实体瘤中的HER2、滋养层细胞表面抗原2(Trop2)、Nectin-4和EGFR,以及血液恶性肿瘤中的CD19、CD22、CD33、CD30和CD79b。T-DM1的成功和最近的批准,如T-Dxd、sacituzumab govitecan(SG)和enfortumab vedotin,导致了ADCs在实体瘤中的增加。肿瘤学和免疫学的研究已经将ADC靶标抗原的选择扩展到传统肿瘤细胞抗原之外,包括肿瘤微环境中的目标,如基质和血管。最近的证据来自临床前和临床研究表明,新血管系统、皮下细胞外基质和肿瘤基质的组成部分可能是ADC药物开发中有价值的靶标抗原。导致美国FDA批准的ADC的几个关键临床研究在表2中概述。
3.1.HER2
HER2/ERBB2/NEU是ErbB受体酪氨酸激酶家族的成员,在细胞生长、分化和存活中发挥着关键作用。HER2的扩增与多种肿瘤类型的预后不良有关,如晚期乳腺癌、胃癌、结直肠癌和胃食管交界处腺癌以及非小细胞肺癌。靶向HER2的ADCs目前是表达或携带HER2突变的实体瘤的标准治疗。
TDM-1 是2013年首个被批准用于治疗乳腺癌的ADC。它结合了人源化HER2靶向曲妥珠单抗和高效细胞毒素活性的微管抑制剂DM1,这是美登素的衍生物。曲妥珠单抗德鲁替康(DS-8201; T-DXd)是一种新型人源化HER2导向的ADC,具有高DAR(8:1),于2019年获得美国FDA批准。T-DXd的结构包括一个抗HER2 IgG1抗体(曲妥珠单抗)、一个稳定的四肽基可切割连接体,以及exatecan衍生物MAAA-1181a(DXd),这是一种DNA拓扑异构酶I抑制剂,其抑制效力是伊立替康的10倍。T-DXd不仅对HER2阳性肿瘤细胞显示出抗肿瘤活性,还通过旁观者效应对HER2表达有无的邻近肿瘤细胞也显示出活性。TDM1和T-DXd在随机试验中作为实体癌的一线、二线或后续治疗的有效性已被证明。迪司他米单抗长春新碱(RC48)由以下组成:(1) hertuzumab,一种新一代抗HER2人源化单克隆抗体,具有高特异性和亲和力;(2) 一个马来酰亚胺-半胱氨酸-缬氨酸-瓜氨酸-对氨基苄氧羰基连接体,释放细胞毒素有效载荷;(3) 细胞毒素有效载荷MMAE,它在活跃分裂的细胞中抑制微管聚合。MMAE是auristatin的合成衍生物,具有强大的抗有丝分裂活性,导致细胞周期停滞和最终细胞死亡。
3.1.1.乳腺癌
已经进行了III期试验,以评估T-DM1在HER2阳性乳腺癌的各种治疗环境中的有效性,此前I/II期试验显示出有希望的结果。EMILIA试验(NCT00829166)证明,与拉帕替尼加卡培他滨相比,T-DM1改善了先前治疗过的HER2阳性转移性乳腺癌患者的无进展和总生存期(OS)。在991名患者中,T-DM1显示中位无进展生存期(PFS)为9.6个月,而拉帕替尼加卡培他滨为6.4个月,中位OS分别为30.9个月和25.1个月。T-DM1的3或4级不良事件发生率较低(41%),而拉帕替尼加卡培他滨为57%。
随后的开放标签III期TH3RESA试验(NCT01419197)涉及602名先前接受过曲妥珠单抗、拉帕替尼和紫杉醇治疗的HER2阳性晚期乳腺癌患者。试验表明,与医生选择的治疗相比,mOS明显更长(22.7个月[95%置信区间(CI),19.4–27.5]与15.8个月[13.5–18.7];HR 0.68[95% CI,0.54–0.85];p = 0.0007)。在先前未经治疗的HER2阳性转移性乳腺癌的背景下,T-DM1在III期MARIANNE研究(NCT01120184)中显示出改善的耐受性和非劣效PFS,与紫杉醇加曲妥珠单抗相比。然而,与标准治疗多西他赛、卡铂、帕妥珠单抗和曲妥珠单抗相比,T-DM1联合帕妥珠单抗作为新辅助治疗导致病理完全缓解率(CRs)较低(44.4 vs. 55.7%,p = 0.016),如KRISTINE试验(NCT02131064)所观察到的。此外,KATHERINE试验(NCT01772472)的发现表明,与继续使用辅助性曲妥珠单抗相比,辅助性T-DM1治疗将HER2阳性早期乳腺癌患者复发风险或死亡降低了50%,这些患者在新辅助化疗加HER2靶向治疗后仍有残留浸润性疾病。值得注意的是,接受T-DM1治疗的患者比接受曲妥珠单抗治疗的患者有更高比例的3级或更高不良事件(25.7 vs. 15.4%)。总体而言,基于这些结果,T-DM1已被推荐用于乳腺癌患者的辅助、一线和二线治疗。
T-DXd最初在先前接受过T-DM1治疗的HER2阳性转移性乳腺癌患者中进行了评估。DESTINY-Breast01试验(NCT03248492)显示了持续的抗肿瘤效果,在推荐剂量5.4 mg/kg下,184名参与者中有112名(60.9%)对治疗有反应。中位PFS报告为16.4个月。尽管13.6%的患者经历了间质性肺疾病,导致四人死亡,美国FDA仍加速批准T-DXd用于成人患有不可切除或转移性HER2阳性乳腺癌,这些患者已经接受了两种或更多先前治疗。随后,DESTINY-Breast 02试验(NCT03523585)比较了608名HER2阳性不可切除或转移性乳腺癌患者的T-DXd与医生选择治疗的疗效和安全性。结果表明,T-DXd组的中位PFS为17.8个月,而医生选择组为6.9个月(HR 0.36[0.28−0.45];p < 0.0001)。两组常见的不良事件包括恶心、呕吐、脱发、疲劳和腹泻,T-DXd相关的间质性肺疾病发生在42名(10%)患者中。总体而言,该研究加强了T-DXd在HER2阳性转移性乳腺癌患者中有利的治疗结果。
在最近的DESTINY-Breast03临床试验(NCT03529110)中,与T-DM1相比,T-DXd在OS和PFS方面显示出显著改善。这导致先前接受过曲妥珠单抗加紫杉醇治疗的HER2阳性转移性乳腺癌患者的死亡风险降低了36%。T-DXd的中位PFS为28.8个月(95% CI,22.4–37.9),而T-DM1为6.8个月(95% CI,5.6–8.2),风险比(HR)为0.33(95% CI,0.26−0.43;p < 0.0001)。T-DXd的中位OS未达到(95% CI,40.5个月—无法估计),T-DM1为34.0个月(无法估计),HR为0.64(95% CI,0.47–0.87;p = 0.0037)。12个月时存活的患者百分比为94.1%(T-DXd)和85.9%(T-DM1),HR为0.55(95% CI,0.36–0.86)。客观反应率(ORR)分别为79.7%(T-DXd)和34.2%(T-DM1)。DESTINY-Breast04试验研究了T-DXd对接受过一种或两种化疗线的HER2低表达转移性乳腺癌患者的影响。在所有患者中,中位PFS为9.9个月(T-DXd)和5.1个月(医生选择的标准化疗),HR为0.50(p < 0.001),OS为23.4个月(T-DXd)和16.8个月(标准化疗),死亡HR为0.64(p = 0.001)。在激素受体阳性亚组中,中位PFS为10.1个月(T-DXd)和5.4个月(医生选择),HR为0.51(p < 0.001),OS为23.9个月(T-DXd)和17.5个月(医生选择),死亡HR为0.64(p = 0.003)。
基于这些发现,T-DXd显著延长了HER2低表达或HER2阳性转移性乳腺癌患者的生存期,表明其作为这一特定人群的替代治疗选择的潜力。然而,T-DXd在II期DAISY试验(NCT04132960)中确认的客观反应率(ORR;主要终点)在HER2过度表达组为70.6%(95% CI,58.3–81),在HER2低表达组为37.5%(95% CI,26.4–49.7),在HER2不表达组为29.7%(95% CI,15.9–47)。这些结果表明,HER2状态在确定对T-DXd的反应性方面仍然是一个关键因素。
3.1.2.非小细胞肺癌
在Hotta等人进行的II期研究中,DM1(剂量为3.6 mg/kg)对HER2阳性非小细胞肺癌(NSCLC)患者的疗效有限。主要终点,客观反应率(ORR),只有一名患者达到(6.7%;95% CI,0.3–27.9),有七名患者(46.7%)病情稳定(SD)和疾病进展(PD)。中位无进展生存期(PFS)为2.0个月(95% CI,1.4–4.0),中位总生存期(OS)为10.9个月(95% CI,4.4–12.0)。在另一项II期临床研究中,T-DM1用于49名先前接受过治疗的HER2过度表达的晚期NSCLC患者(IHC 2+,29;IHC 3+,20),以评估其疗效。HER2 2+队列没有显示任何客观反应,28%的患者病情稳定,55%的患者疾病进展。相比之下,HER2 3+队列有四名部分反应(PRs)(总体反应率,20%;95% CI,5.7–43.7)。临床获益率分别为7%(HER2 2+)和30%(HER2 3+)。中位OS在HER2 2+组为12.2个月(95% CI,3.8–23.3),在HER2 3+组为15.3个月(95% CI,4.1–未达到),中位PFS在两组中均可比较,分别为2.6个月(HER2 2+)和2.7个月(HER2 3+)。
T-DXd在HER2突变NSCLC患者的抗癌活性最初由Tsurutani等人在一项I期剂量扩展试验中研究,该试验涉及多种晚期实体瘤患者。在11名先前接受过治疗的HER2突变NSCLC患者中,中位PFS为11.3个月(95% CI,8.1–14.3),ORR为72.7%(11名中有8名)。在另一项多中心临床试验,DESTINY-Lung01(NCT03505710)中,共有91名HER2突变NSCLC患者入组。T-DXd组显示出中位PFS和OS分别为8.2个月(95% CI,6.0–11.9)和17.8个月(95% CI,13.8–22.1)。然而,有46%的患者经历了3级或更高级别的不良事件,其中中性粒细胞减少症(19%)最常见。在随机II期试验,DESTINY-Lung02(NCT04644237)中,共有102名和50名HER2突变转移性NSCLC患者分别在T-DXd 5.4和6.4 mg/kg臂中入组。结果显示,在5.4 mg/kg臂中,ORR为49.0%(95% CI,39.0–59.1),在6.4 mg/kg臂中为56.0%(95% CI,41.3–70.0%)。中位PFS和OS在5.4 mg/kg臂中分别为9.9个月(95% CI,7.4–未达到)和19.5个月(95% CI,13.6–未达到),在6.4 mg/kg臂中分别为15.4个月(95% CI,8.3–未达到)和未达到(95% CI,12.1–未达到)。使用T-DXd 5.4和6.4 mg/kg估计的1年OS率分别为67%(95% CI,56–76)和73%(95% CI,57–84)。药物诱导的间质性肺疾病在6.4 mg/kg臂中发生在28.0%的患者中,而在5.4 mg/kg臂中为12.9%。美国FDA已批准T-DXd作为首个针对HER2突变NSCLC患者的抗HER2药物。
3.1.3.胃/胃食管结合部癌
DS8201-A-J101(NCT02564900)试验旨在评估T-DXd在对标准治疗无反应的晚期HER2阳性胃或胃食管结合部和乳腺癌患者的安全性、有效性和药代动力学。结果显示,所有四名HER2阳性胃癌患者都实现了疾病控制,其中两名患者显示出PR。随后的一项I期研究(NCT02564900)涉及44名先前接受过治疗的HER2阳性胃或胃食管结合部癌患者,证明了T-DXd的可管理安全性和有希望的抗肿瘤活性。值得注意的是,25%的患者经历了严重不良事件,ORR为43.2%。一项II期试验比较了T-DXd与化疗在125名HER2阳性晚期胃癌患者中的疗效(与62名接受化疗的患者相比),结果显示T-DXd的ORR明显更高(51 vs. 14%,p < 0.001)。此外,与化疗相比,T-DXd治疗导致更高的CR率、肿瘤尺寸更大程度的减小和更长的mOS。T-DXd组的中位PFS也比化疗组长。
在作为II期试验的一部分进行的探索性队列研究中,调查了T-DXd在HER2低表达胃或胃食管结合部腺癌中的疗效和安全性。结果显示T-DXd在先前接受过大量治疗的HER2低表达胃/胃食管结合部腺癌患者中显示出临床活性。在19名IHC 2+/ISH−患者中,26.3%达到PR,63.2%病情稳定。中位PFS和OS分别为4.4个月和7.8个月,12个月OS率为40.0%。在另一组21名IHC 1+患者中,疾病控制率(DCR)为71.4%,9.5%达到PR,61.9%病情稳定。中位PFS和OS分别为8.5个月和2.8个月,12个月OS率为25.7%。
已经接受过基于曲妥珠单抗的治疗的局部晚期或转移性HER2阳性胃癌或胃食管结合部腺癌患者,于2021年1月15日获得美国FDA批准接受T-DXd治疗。此外,正在进行的临床试验正在探索T-DXd在HER2阳性胃癌中的应用,无论是作为单药治疗还是与化疗和曲妥珠单抗联合使用。
迪司他米单抗长春新碱已在中国获得批准,用于接受过两种或更多化疗方案的HER2阳性胃癌或胃食管结合部腺癌患者,基于几项临床试验。该药物在最初试验(NCT02881190)中显示出显著的疗效,ORR为15.0%,DCR为45.0%。在不同HER2状态的胃癌患者分析中,ORRs分别为IHC 2+/FISH−的35.7%,IHC 2+/FISH+的20%,和IHC 3+的13.6%。在随后的II期研究(NCT03556345)中,125名接受二线或更晚治疗的HER2阳性局部晚期或转移性胃或胃食管结合部癌患者被纳入最终分析。由独立审查委员会评估的ORR和DCR分别为24.8%(95% CI,17.5−33.3%)和42.4%(95% CI,33.6−51.6%)。12个月生存率为33.3%,中位OS为7.9个月(95% CI,6.7–9.9)。将迪司他米单抗长春新碱与托利珠单抗结合使用显示出增强的临床效益,中位PFS为6.2个月(95% CI,4.0–6.9%),中位OS为16.8个月(95% CI,7.2–未达到)。在28名可评估参与者中有12名观察到PRs。
3.1.4.其他实体瘤
HERACLES-B(NCT03225937)临床试验是首个探索ADC在化疗耐药的RAS/BRAF野生型和HER2+转移性结直肠癌患者中使用的研究。在这项31名先前接受过治疗的患者的II期试验中,帕妥珠单抗与T-DM1联合给药。虽然主要目标ORR为9.7%(95% CI,0–28%),低于预期的成功阈值,但DCR为77.4%,PFS为4.1个月(95% CI,3.6–5.9)。这些结果表明T-DM1可能是HER2+结直肠癌有希望的治疗选择。
几项临床试验已经显示了将T-DXd与其他治疗结合使用在先前治疗过的HER2表达的转移性结直肠癌中的疗效和安全性数据。DESTINY-CRC01研究(NCT03384940)在2018年2月至2019年7月期间招募了53名HER2阳性表达的患者,他们都接受了T-DXd治疗。在超过27周的随访期间,24名患者(45.3%)观察到确认的客观反应。6个月的PFS和OS率分别为53.0%(95% CI,37.0–66.7)和76.6%(95% CI,61.5–86.4)。中位PFS为6.9个月(4.1–未达到),而中位OS未达到(95% CI,0.74个月–无法评估)。至少10%的患者观察到3级或更高级别的副作用,包括17名患者的中性粒细胞计数减少和11名患者的贫血。然而,T-DXd在HER2低表达的转移性结直肠癌肿瘤(IHC2+和ISH阴性;IHC1+)的患者中未显示抗肿瘤活性,没有观察到确认的客观反应。
II期研究(KAMELEON,NCT02999672)为T-DM1单药治疗作为HER2阳性晚期尿路上皮膀胱癌或胰腺癌/胆管癌患者不论肿瘤类型的治疗选择提供了支持。在尿路上皮膀胱癌队列中观察到5名患者的PR,在胰腺癌/胆管癌队列中观察到1名患者的PR,ORR分别为38.5%和14.3%。两个队列中的患者均未达到CR。
DESTINY-PanTumor02 II期试验评估了T-DXd在HER2表达的实体瘤患者中的有效性和安全性(NCT04482309)。共有268名HER2阳性实体瘤患者入选,包括局部晚期、不可切除或转移性胆管癌、膀胱癌、宫颈癌、子宫内膜癌、卵巢癌、胰腺癌和唾液腺癌等其他实体癌,如未知原发部位的恶性新生物、乳腺外Paget病、口咽新生物、皮肤黑色素瘤等。在267名接受评估的患者中,有99名患者(37.1%)根据研究者评估显示出确认的客观反应。值得注意的是,无论患者是否接受过HER2治疗,都观察到了反应。总体而言,由独立中心评估的100名患者(37.5% [95% CI,31.6–43.6])实现了确认的ORR,中位PFS为6.9个月,OS为13.4个月。IHC 3+状态的患者从T-DXd中获益最显著,ORR为61.3%,中位持续时间(DoR)为22.1个月,中位PFS为11.9个月,中位OS为21.1个月。这些发现导致美国FDA在2024年4月5日加速批准T-DXd用于HER2过度表达(IHC 3+)的实体瘤,这些肿瘤没有其他治疗选择。
在中国进行的I期试验(NCT04280341)中,56名实体瘤患者,包括胃癌、胃食管结合部癌、乳腺癌和其他实体瘤,接受了迪司他米单抗长春新碱和托利珠单抗治疗。在24名接受迪司他米单抗长春新碱治疗的患者中,确认的ORR为25%(95% CI,10−47),DCR为75%(95% CI,53−90),中位OS为10.5个月。
3.2.TROP2
TROP2是肿瘤相关钙信号转导蛋白2(TACSTD2)基因的产物,是一种跨膜糖蛋白,具有短的细胞质尾部、单个跨膜区域和大的细胞外区域。虽然在正常组织中偶尔表达,但TROP2在许多肿瘤中频繁发现,它在癌细胞增殖、凋亡和侵袭中发挥作用,通常与预后不良有关。
基于hRS7,一种针对TROP2的人源化IgG1 mAb,开发了一种名为SG的新型第三代ADC,将hRS7与拓扑异构酶抑制剂伊立替康的衍生物CL2A结合。SG(IMMU-132)在先前治疗过的实体瘤中展示了初步的抗肿瘤活性和可接受的耐受性,在I/II期IMMU-132-01篮式试验(NCT01631552)中。SG的疗效在多种恶性肿瘤中观察到,包括NSCLC、小细胞肺癌(SCLC)、尿路上皮癌和转移性乳腺癌的组织学队列中看到了有希望的结果。此外,其他抗TROP-2 ADC,如SKB264和datopotamab deruxtecan在临床前研究中显示出强大的抗肿瘤活性。
Datopotamab deruxtecan由一种重组人源化抗TROP2 IgG1 mAb组成,通过四肽连接体与Topo I抑制剂(DXd)结合,是一种TROP-2 ADC,具有可切割的四肽连接体和比SG更强效的拓扑异构酶抑制剂有效载荷。这种设计赋予了与SG相比在循环中增加的稳定性和更长的半衰期。
SG在治疗复发的转移性三阴性乳腺癌(mTNBC)患者中显示出显著的疗效。ASCENT临床试验(NCT02574455)证明,与化疗相比,SG为接受至少两种先前治疗的mTNBC患者提供了统计学上显著的PFS和OS益处。SG的ORR为35%,明显高于单一化疗药物的5%。常见的副作用包括骨髓抑制和腹泻。SG是首个针对Trop-2的mTNBC治疗ADC药物。在患有激素受体阳性/HER2阴性的内分泌耐药转移性乳腺癌患者中,与化疗相比,SG显示出更长的PFS[5.5个月(95% CI,4.2–7.0)vs. 4.0个月(95% CI,3.1–4.4);HR 0.66,p = 0.0003)].在TROPHY-U-01 II期试验(NCT03547973)中,SG对接受了两种先前治疗线进展的转移性尿路上皮癌患者有效,在9.1个月的中位随访中,ORR为27%(95% CI,19.5–36.6),并显示出有希望的中位PFS(5.4个月,95% CI,3.5–7.2个月)和OS(10.9个月,95% CI,9.0–13.8个月)。这些结果导致美国FDA批准SG作为先前接受过基于铂的化疗或免疫检查点抑制剂的局部晚期或转移性尿路上皮癌患者的治疗选择。在IMMU-132-01试验中,三名肺癌患者中,一名接受了两线化疗的SCLC(IHC的TROP-2表达为3+)患者,显示出最长直径之和减少了38%(NCT01631552)。然而,其他两名SCLC和NSCLC患者没有显示出任何抗肿瘤活性。
在涉及接受过多次先前治疗的转移性NSCLC患者的单臂扩展试验中,ORR为19%,中位PFS为5.2个月(95% CI,3.2–7.1个月),临床获益率为43%。尽管Trop-2是SG的靶标,但未发现TROP2表达与反应之间的相关性。随后的研究证明了SG在先前接受过治疗的转移性SCLC患者中的疗效和安全性。在50名接受过先前治疗的患者中,有7名PR和21名SD,总体ORR为14%,DCR为56%。中位PFS和OS分别为3.7个月和7.5个月。临床获益率(≥4个月)估计为34%。值得注意的是,对于先前治疗有反应的患者,SG在二线治疗中的PR、PFS和临床获益率都有所提高。值得一提的是,该研究中患者选择并未要求Trop-2肿瘤染色。最常见的≥3级不良事件包括中性粒细胞减少症(34%)、疲劳(13%)、腹泻(9%)和贫血(6%)。
III期TROPION-Breast01研究的结果将有助于定义Dato-DXd在转移性HR+/HER2-乳腺癌治疗中的作用,这些患者已在内分泌治疗后进展或不适合内分泌治疗,并在化疗后。关于Dato-DXd的先前研究已在晚期NSCLC患者中显示出有希望的抗肿瘤活性和可管理的安全性。ORR为26%,在推荐剂量6 mg/kg时,中位DoR为10.5个月。无论TROP2水平如何,中位PFS和OS分别为6.9个月和11.4个月。Dato-DXd的临床获益和安全性已在各种临床试验中进行了评估,支持其在NSCLC和乳腺癌等实体瘤患者中的潜在益处。
3.3.HER3
HER3/ErbB3是EGFR/HER家族的一员,该家族包括EGFR(ErbB1或HER1)、HER2(ErbB2)和HER4(ErbB4)。与其他成员不同,HER3具有最小的细胞内酪氨酸激酶活性,比完全激活的EGFR显著更弱。它的配体,neuregulin 1(NRG-1)和neuregulin 2(NRG-2),触发HER3与其他受体,如EGFR和HER2形成异二聚体,导致下游C末端磷酸化。此外,HER3可以与非EGFR家族受体二聚化,如MET因子受体和FGFR2。HER3上的几种酪氨酸磷酸化位点直接结合到PI3K,从而激活对癌细胞存活至关重要的PI3K/AKT信号通路。HER3还触发其他下游通路,如MEK/丝裂原激活蛋白激酶(MAPK)、Jak/Stat和c-Src,促进细胞增殖。HER3的高表达与癌症患者的疾病进展和生存率降低有关,使其成为治疗的潜在靶标。
Patritumab deruxtecan(HER3-DXd)是Daiichi Sanko针对HER3开发的ADC。抗体部分,patritumab(U3-1287),特异性靶向HER3的细胞外域,有效抑制HER2/HER3异二聚体的形成。HER3-DXd和DS-8201都包含deruxtecan,一种拓扑异构酶I抑制剂,通过一个稳定的四肽基可切割连接体在肿瘤溶酶体中被酶解,释放DXd,可以通过旁观者效应进入细胞。
I期U31402-A-U102研究(NCT03260491)评估了patritumab deruxtecan在先前接受过治疗的转移性或不可切除NSCLC患者中的疗效。剂量递增阶段重点关注了在接受奥希替尼后进展的EGFR突变疾病患者,或者在接受厄洛替尼、吉非替尼或阿法替尼后进展的没有T790M突变的患者。主要目标是确定安全性、耐受性和推荐剂量。结果表明,在5.6 mg/kg剂量下,在接受过TKIs和基于铂的化疗的57名患者中,patritumab deruxtecan实现了72%的DCR,中位PFS为8.2个月。该药物在接受过奥希替尼和基于铂的化疗的患者中也显示出疗效,显示出39%的确认ORR和68%的DCR,中位PFS为8.2个月。在有脑转移的患者中观察到显著反应,确认ORR为32%,中位PFS为8.2个月,而在无脑转移的患者中,确认ORR为41%,中位PFS为8.3个月。在安全性方面,接受5.6 mg/kg剂量的patritumab deruxtecan的所有患者都经历了治疗出现的不良效应,一小部分导致治疗中断或剂量调整,但没有报告致命副作用。
II期试验(HERTHENA-Lung01,NCT05338970)评估了patritumab deruxtecan在一组先前接受过EGFR酪氨酸激酶抑制剂治疗和基于铂的化疗的晚期NSCLC患者中的有效性。主要目标,ORR,被确定为29.8%(95% CI,23.9–36.2),中位PFS和OS分别为5.5个月和11.9个月。在接受过奥希替尼和化疗的患者中,治疗结果没有显著差异。在未接受放射治疗的脑转移患者中,大约三分之一的患者控制了脑转移,ORR为33.3%(95% CI,17.3–52.8)。随后的III期研究(HERTHENA-Lung02,NCT05338970)目前正在进行中,以评估patritumab deruxtecan在接受第三代EGFR TKI治疗后疾病进展的患者中的安全性和有效性。
77名先前未接受治疗的HR+/HER2−乳腺癌患者在SOLTI-1805 TOT-HER3研究(NCT04610528)中被评估了疗效。在CelTIL评分[= -0.8 ×肿瘤细胞百分比(%)+ 1.3 ×肿瘤浸润性淋巴细胞(%)]中观察到显著变化,与基线相比的中位数增加为3.5(四分位间距,-3.8至12.7;p = 0.003)。实现了45%的ORR,有反应者与无反应者相比CelTIL评分增加更多(平均差异,+11.9 vs. +1.9)。
182名HER3表达的晚期乳腺癌患者在多中心、I/II期试验(NCT02980341)中接受了≥1剂HER3-DXd。HER3-low定义为IHC评分1+,而HER3-high定义为IHC评分2+或3+。无论HER3表达水平如何,都观察到了客观反应。针对特定临床亚组报告了疗效结果:HR+/HER2−(ORR,30.1%;中位PFS,7.4个月),TNBC(ORR,22.6%;mPFS,5.5个月),和HER2+(ORR,42.9%;mPFS,11.0个月)。HER3-DXd在晚期乳腺癌患者中显示出与SG相当的抗肿瘤活性,治疗相关不良反应导致的停药率较低(9.9%)。
3.4.EGFR
EGFR(HER1或ERBB1)是ErbB家族酪氨酸激酶受体的成员,在调节细胞增殖、分化、迁移和存活方面发挥着重要作用。EGFR的过度表达或突变与多种实体瘤的发展有关,如NSCLC、鼻咽癌、头颈部鳞状细胞癌和结直肠癌。除了针对EGFR突变非小细胞肺癌的酪氨酸激酶抑制剂外,针对EGFR的ADC最近作为HER阳性癌症患者的有希望的治疗药物出现。
ABT-414是通过将抑制微管组装的MMAF与EGFR特异性人源化抗体(ABT-806)的链间半胱氨酸结合,使用不可切割的马来酰亚胺己酰连接体,平均DAR约为4而创建的。来自多中心、I期国际研究(NCT01800695)的结果在EGFR过度表达的复发性胶质母细胞瘤患者中展示了初步的疗效和可管理的安全性。在66名患者中,ORR为6.8%,6个月PFS率为28.8%,6个月OS率为72.5%。报告的最常见不良事件与眼睛有关(91%),包括视力模糊(65%)、干眼(29%)、角膜炎(27%)和光敏性(27%)。
MRG003是一种针对EGFR的ADC,由通过缬氨酸-瓜氨酸连接体连接到MMAE的人源化IgG1单克隆抗体组成。这种ADC可以特异性地结合肿瘤细胞上的EGFR,通过内吞作用进入细胞,到达溶酶体,并通过蛋白酶降解释放MMAE。MMAE抑制微管聚合,停止有丝分裂,最终抑制肿瘤细胞生长并诱导细胞死亡。在涉及复发/难治性实体瘤患者的首次人体剂量递增研究(CTR20180310)中,接受1.5 mg/kg或更高剂量MRG003的EGFR阳性患者的DCR为100%。182 在另一项I期研究(NCT04868344)的亚组分析中,涉及39名患有难治性晚期头颈部鳞状细胞癌、结直肠癌和鼻咽癌的患者,所有患者均发现EGFR阳性。ORR为20.5%,有8个PR,而DCR为51.3%,有12个SD。所有患者的中位PFS为2.8个月。重要的是,观察到EGFR表达水平与MRG003治疗观察到的临床结果之间存在正相关。
3.5.c-Met
细胞表面受体酪氨酸激酶c-Met经历一个翻译过程,产生一个前体蛋白,该蛋白被翻译后修饰成通过二硫键连接的三维结构。成熟的c-Met由一个50 kDa的细胞外α链和一个140 kDa的跨膜β链组成。c-Met及其唯一的配体肝细胞生长因子(HGF)在各种细胞过程中发挥着至关重要的作用,如增殖、存活、侵袭、组织发育和器官再生。HGF最初以非活性前体形式存在,通过丝氨酸蛋白酶激活成为成熟的。活性HGF配体包括具有N末端和Kringle结构域的α链,以及类似于丝氨酸蛋白酶结构域的β链。HGF分子的N末端域和K1区与c-Met强烈结合,在HGF-β链上形成新的结合位点。这种紧密结合形成HGF和c-Met之间的复合物,启动信号转导。这种活性复合物的形成导致受体聚合、内吞作用和细胞内激酶域中多个酪氨酸残基的磷酸化,从而激活与肿瘤发展、侵袭和转移相关的各种信号通路(JAK/STAT3、PI3K/Akt/NF-κB和Ras/Raf途径)。
Telisotuzumab vedotin(Teliso-V)是一种新型c-Met靶向ADC,由人源化单克隆抗体ABT-700与MMAE通过可切割的缬氨酸-瓜氨酸肽连接体(ABT-700-vcMMAE)结合而成。这种组合大约每抗体有三分子单甲基auristatin。Teliso-V能够内吞,并已被证明能够释放MMAE,随后与微管结合,通过抑制有丝分裂导致细胞死亡。实质上,Teliso-V能够使用抗体将化疗药物有效地传递到表达c-Met的癌细胞内部,从而直接针对并消除癌细胞。以前的研究表明,由于其特异性和高亲和力结合,Teliso-V在MET扩增和c-Met过度表达的肿瘤中表现出抗肿瘤活性。
2018年,Strickler等人开展了Teliso-V在实体瘤患者中的初步人体试验(NCT02099058)。在接受Teliso-V(2.4-3.0 mg/kg)治疗的16名c-Met突变NSCLC患者中,有3名患者(18.8%)实现了PR,中位反应持续时间为4.8个月,mPFS为5.7个月。大多数患者对Teliso-V没有反应。与Teliso-V相关的最常见的≥3级不良事件是低白蛋白血症、疲劳、中性粒细胞减少和贫血(各占4%)。在Teliso-V单药治疗晚期NSCLC患者的I期研究(NCT02099058)中,四十名c-Met阳性患者(33名非鳞状细胞,6名鳞状细胞,1名混合组织学)被纳入最终分析。其中9名(23%)患者经历了客观反应,mPFS为5.2个月,中位反应持续时间为8.7个月。2022年1月4日,美国FDA基于正在进行的II期LUMINOSITY临床试验(NCT03539536)在2021年AACR上呈现的支持数据,授予Teliso-V突破性疗法认定,用于治疗在接受基于铂的治疗期间或之后疾病进展且c-Met过度表达的晚期/转移性EGFR野生型非鳞状NSCLC患者。在这个试验的非鳞状EGFR野生型亚组中(n = 37),由独立中心评估的ORR为35.1%。c-Met过度表达亚组(n = 13)的ORR为53.8%,而中度c-Met亚组为25.0%。这个队列中的DoR为6.9个月。EGFR突变亚组(n = 30)的ORR为13.3%,并且仅在高c-Met患者(n = 22)中显示缓解。然而,在鳞状细胞亚组中(n = 21),ORR为14.3%,DoR为4.4个月。观察到的所有反应均为PR。
在Lung-MAP S1400K研究(NCT03574753)中,Teliso-V没有达到预期的响应率终点,在接受c-Met阳性鳞状细胞癌治疗的患者中仅为9%。然而,在具有双重c-Met/EGFR突变的患者中,Teliso-V与其他TKIs(厄洛替尼)联合使用显示出有希望的抗肿瘤活性和可接受的毒性水平(NCT02099058)。mPFS为5.9个月(95% CI,2.8–未达到),ORR为32.1%。在EGFR突变患者中,c-Met过度表达的患者(n = 15)的ORR为52.6%。195 这种治疗方法也在与奥希替尼联合使用的研究中(NCT06093503)。
3.6.Nectin-4
Nectin-4是由脊髓灰质炎病毒受体相关-4基因编码的蛋白质,是Nectins家族(Nectins 1−4)的成员。它属于不依赖钙离子的免疫球蛋白样蛋白质组,通过同型/异型相互作用在细胞-细胞粘附和紧密连接的形成和维持中发挥着关键作用。虽然其他Nectins主要在成人健康组织中表达,但Nectin-4特别富集在正常的胚胎和胎儿组织中。值得注意的是,最近的研究表明Nectin-4在各种恶性肿瘤中过度表达,对尿路上皮癌、乳腺癌、胰腺癌、TNBC和膀胱癌等癌症的疾病进展和预后不良有贡献。Nectin-4的过度表达与促进肿瘤细胞增殖、分化、血管生成、迁移、侵袭、上皮向间充质转变和通过激活PI3K/Akt途径的DNA修复有关。
Enfortumab vedotin,也称为ASG-22CE,是一种新型的全人源化单克隆ADC,通过可被蛋白酶切割的连接体与微管破坏剂MMAE相连。这种药物旨在特异性地靶向表达Nectin-4的癌细胞,导致ADC-Nectin-4复合物的内吞作用,随后切割MMAE。这一过程最终破坏细胞内的微管网络,触发细胞凋亡。
在对耐受性和抗肿瘤活性的评估中,201名接受了大量预先治疗的表达Nectin-4的实体瘤患者(原发肿瘤位于膀胱、肾脏、骨盆、输尿管、肺、卵巢、结肠和阑尾)在EV-101临床试验(NCT02091999)中接受了enfortumab vedotin治疗。在112名转移性尿路上皮癌患者中,ORR为43%,DoR为7.4个月。中位OS为12.3个月,1年OS率为51.8%。2019年12月,美国FDA基于EV-201临床试验(NCT03219333)的发现,加速批准enfortumab vedotin用于治疗局部晚期或转移性尿路上皮癌患者,这些患者在接受两种先前治疗后仍有疾病进展。这组患者在首次治疗中最初接受了基于铂的双药化疗,随后接受了PD-1/PD-L1抑制剂。随后,所有125名参与者接受了enfortumab vedotin作为第三线治疗,而不是像紫杉醇和多西他赛这样的紫杉烷类药物。enfortumab vedotin治疗有效地抑制了大多数患者的肿瘤生长,导致ORR为44%(125名中的55名,95%CI,35.1-53.2),CR率为12%(125名中的15名),中位DoR为7.6个月(范围:0.95-11.3+)。
在EV-201临床试验(NCT03219333)的队列2中,研究人员评估了enfortumab vedotin在顺铂不适用的尿路上皮癌患者中的疗效和安全性,这些患者在免疫治疗后的环境中。主要终点是ORR,大多数参与者是肾功能不全的老年人。来自队列2的结果表明,在接受ADC治疗的患者中,确认的ORR为52%,CR率为20%,中位DoR为10.9个月。mPFS和中位OS分别为5.8个月和14.7个月。216 这项研究为具有重大未满足需求的患者群体提供了可能更有效和有希望的治疗选择。在EV-201启动后,各种调查enfortumab vedotin在尿路上皮癌治疗中的临床试验已经获得了动力。
在enfortumab vedotin治疗先前治疗过的晚期尿路上皮癌的III期试验(EV-301)中,307名参与者被分配接受化疗,301名接受enfortumab vedotin(NCT03474107)。与化疗相比,enfortumab vedotin延长了中位OS(12.88 vs. 8.97个月;HR = 0.70,p = 0.00142)。enfortumab vedotin组的中位PFS也比化疗组长(5.55 vs. 3.71个月;HR = 0.62,p < 0.00001)。两组在治疗出现的不良事件和≥3级事件的比率上相似。即使在2年的中位随访后,PFS、OS和总体反应方面的益处仍然一致。
在EV-302临床试验(NCT04223856)中,enfortumab vedotin和pembrolizumab的联合治疗与化疗相比,对于未经治疗的局部晚期或转移性尿路上皮癌患者显示出明显更好的结果。enfortumab vedotin-pembrolizumab组的中位PFS和OS比化疗组长(PFS:12.5 vs. 6.3个月;HR = 0.45;95% CI,0.38-0.54;p < 0.001;OS:31.5 vs. 16.1个月;HR = 0.47;95% CI,0.38-0.58;p < 0.001)。
3.7.CEACAM5
CEACAM5,也称为CEA或CD66e,是免疫球蛋白超家族粘附分子的成员。它由一个单一的N域、六个免疫球蛋白恒定区样域和一个糖基磷脂酰肌醇锚组成,使其可以位于细胞膜上并参与细胞间粘附和信号传导。虽然CEACAM5在正常成人组织中表达有限,但它在胃肠道、乳腺、胰腺、泌尿生殖系统和呼吸系统的各种癌症中高度表达。这使CEACAM5成为CEA阳性癌症的宝贵预后标志物和潜在治疗靶标。
Tusamitamab ravtansine(SAR408701)是针对CEACAM5的人源化抗体。它由人源化单克隆抗体(SAR408377)共价连接到细胞毒素美登素衍生物DM4有效载荷,这是一种微管破坏剂。这种连接是通过可切割的N-琥珀酰亚胺4-(2-吡啶二硫)丁酸酯连接体实现的。Tusamitamab ravtansine的DAR为3.8。
Tusamitamab ravtansine的首次人体剂量递增研究包括31名患有局部晚期或转移性实体瘤的患者(NCT02187848)。在所有剂量水平和癌症类型中,29名参与者接受了肿瘤反应评估,发现3名(9.7%)PR,11名(35.5%)SD,13名(41.9%)PD。此外,两名患者没有表现出CR或疾病进展。在两名表现出PR的结直肠癌患者中,一名有KRASG12V突变,两者在100%的癌细胞中都有2+膜CEACAM5表达。第三位有PR的患者有胃癌,但在有限的肿瘤组织中缺乏CEACAM5表达。在CARMEN-LC03临床试验(NCT04154956)中,Tusamitamab ravtansine作为单药治疗与多西他赛相比,没有达到PFS和OS的双重主要终点,这是由独立数据监测委员会确定的。因此,截至2023年12月,涉及tusamitamab ravtansine的随后的临床试验已经停止。
3.8.TF
TF,也称为凝血因子III或CD142,是一种跨膜糖蛋白,在启动外源性凝血途径中发挥着关键作用。TF由外细胞、跨膜和细胞内区域的263个氨基酸残基组成,通过与因子VII/VIIa结合启动血液凝固级联反应。近期研究表明,TF与VIIa(FVIIa)之间的相互作用可以通过信号传导途径影响血管生成、癌症干细胞活性、肿瘤生长、侵袭和转移。Tisotumab vedotin是一种全人源化的特异性单克隆抗体,与细胞毒素MMAE有效载荷相连,展现出有希望的抗肿瘤活性。该抗体与TF结合后被内吞到肿瘤细胞中,在那里被溶酶体蛋白酶切割,释放MMAE,最终诱导细胞分裂抑制和凋亡。在InnovaTV 201临床试验中,27名复发、晚期或转移性实体瘤患者接受了tisotumab vedotin的剂量递增,随后在剂量扩展阶段有147名患者接受了2.0 mg/kg的剂量。在剂量扩展阶段的确认ORR为15.6%,所有反应均为部分反应。中位DoR为5.7个月,mPFS为3.0个月。在涉及101名复发或转移性宫颈癌患者的InnovaTV 204/GOG-3023/ENGOT-cx6试验中,tisotumab vedotin显示出ORR,24名患者实现了确认的反应,包括7个CR和17个PR。最常见的治疗相关不良事件包括脱发(38%)、鼻出血(30%)、恶心(27%)、疲劳(26%)和结膜炎(26%)。报告了四例死亡,其中一例归因于与药物相关的感染性休克。在InnovaTV 201和InnovaTV 204试验取得积极结果后,tisotumab vedotin获得了美国FDA的加速批准,用于治疗复发或转移性宫颈癌患者。InnovaTV 205/GOG-3024/ENGOT-cx8研究的结果显示,tisotumab vedotin与贝伐珠单抗、卡铂或帕博利珠单抗联合使用在治疗未接受过治疗和预先治疗过的复发或转移性宫颈癌患者中具有可接受的安全性和有希望的抗肿瘤效果。在接受tisotumab vedotin加卡铂作为一线治疗的组中(n = 32),ORR为56.3%,DCR为93.8%,临床获益率为81.3%。中位DoR为8.6个月,mPFS为6.9个月,mOS在数据截止时未达到(死亡率:42.4%)。在接受tisotumab vedotin和帕博利珠单抗治疗的未接受过治疗的患者中(n = 31),ORR为41.9%,DCR为83.9%,临床获益率为74.2%。中位DoR和OS未达到,中位PFS为5.3个月。在接受第二或第三线治疗的患者中,使用tisotumab vedotin +帕博利珠单抗(n = 32),ORR为35.3%,DCR为73.5%,临床获益率为47.1%。中位DoR为14.1个月。中位PFS和OS分别为5.6个月和15.3个月。
3.9.FRα
FRα,也称为FOLR1或叶酸结合蛋白,是叶酸受体家族的成员,与叶酸具有高亲和力,可以通过受体介导的内吞作用转运叶酸。FRα在正常组织中通常很低,但在各种实体瘤中高度表达,如卵巢癌(76-89%)、TNBC(35-68%)、子宫内膜癌(20-50%)和肺癌(75-90%)。研究表明,FRα介导的信号通路在肿瘤发生中发挥着关键作用,涉及DNA修复、DNA合成、细胞增殖和细胞内信号传导等过程。抑制FRα可能直接阻碍肿瘤生长,使其成为肿瘤诊断和治疗的有希望的靶标。
MORAb-202是第一个针对FRα的ADC,DAR为4.0。这种化合物是通过将抗FRα单克隆抗体与eribulin连接而创建的,通过酶可切割的连接体。Eribulin作为一种微管抑制剂,破坏微管稳态,最终抑制细胞分裂,有效促进癌细胞的破坏。
在MORAb-202针对FRα阳性晚期实体瘤患者的I期初步试验中,45%的患者经历了治疗相关的不良事件,包括白细胞减少症和中性粒细胞减少症。此外,一名患者(0.9 mg/kg)经历了两次3级事件,血清丙氨酸转氨酶和γ-谷氨酰转移酶水平升高。在22名入组的患者中,一名卵巢癌患者实现了CR,9名患者(41%)有PR,8名患者(36%)有SD,剩下的4名患者(18%)显示疾病进展。MORAb-202还显著抑制了FRα表达的乳腺癌细胞系的生长。这些MORAb-202在FRα阳性实体瘤中的有希望的结果导致了对其临床效用的进一步研究。
Mirvetuximab soravtansine(IMGN853)是一种ADC,主要用于治疗某些类型的癌症,特别是高FRα表达的卵巢癌患者。这种药物由FRα结合抗体(mirvetuximab)、可裂解的连接体和美登素衍生物有效载荷DM4(soravtansine)组成。Mirvetuximab soravtansine选择性地与FRα高亲和力结合,然后通过抗原介导的内吞作用内化。一旦进入FRα表达的肿瘤细胞内,DM4通过蛋白酶裂解释放。DM4破坏细胞内微管网络,引起细胞周期停滞和凋亡。由于DM4具有电中性且亲脂性,可以穿过细胞膜,在邻近抗原阴性细胞中诱导细胞死亡,这种现象称为“旁观者效应”。这种特性对mirvetuximab soravtansine至关重要,因为它即使在缺乏FRα表达的细胞表面也能发挥细胞毒性作用。
这项I期扩展队列研究考察了mirvetuximab soravtansine在46名接受了大量预先治疗的FRα阳性和铂耐药卵巢癌患者的安全性和临床有效性(NCT01609556)。最常见的不良事件是腹泻(44%)、视力模糊(41%)、恶心(37%)和疲劳(30%),通常都是轻度的(≤2级)。2名患者(4%)分别报告了3级低血压和疲劳。确认的ORR为26%,包括1个CR和11个PRs。无论FRα表达如何,mPFS为4.8个月(95% CI,3.9-5.7)。有趣的是,接受过少于4线治疗的患者mPFS为6.7个月(95% CI,3.9-8.7),ORR为39%。在有希望的初步数据之后,启动了一项开放标签随机对照III期试验(FORWARD I)(NCT02631876)。该试验招募了(n = 366)接受过少于4线治疗和FRα阳性肿瘤(中度和高度表达)的患者。患者随机分配接受6 mg/kg的mirvetuximab soravtansine或医生选择的治疗(包括紫杉醇、聚乙二醇化脂质体阿霉素或拓扑替康)。虽然所有次要终点,如ORR(22%对12%)、CA125反应(51%对27%)、PFS后(中位数10.0对8.4个月)和生活质量(32%对14%),都显示出显著改善,但PFS的主要终点没有达到预期。
虽然FORWARD I的结果令人失望,但PFS和OS的HR表明,mirvetuximab soravtansine在高FRα亚组中可能有潜在益处,尽管没有统计学意义。另外两项研究集中在高FRα水平的铂耐药癌症患者中进行了mirvetuximab soravtansine研究。SORAYA研究(NCT04296890),仅招募了FRα高表达患者,包括106名高级别浆液性卵巢癌、原发性腹膜癌或输卵管癌患者。在这些患者中,51%接受过三线治疗,48%之前接受过聚ADP-核糖聚合酶抑制剂。所有参与者之前都接受过贝伐珠单抗治疗,随后接受了6 mg/kg剂量的单一药物mirvetuximab soravtansine。5名患者实现了CRs,29名实现了PRs,导致确认的ORR为32.4%,DCR为51.4%。大多数患者(71.4%)经历了肿瘤缩小。mPFS为5.5个月(95% CI,3.8-6.9),中位OS为13.8个月(95% CI,12.0-未达到)。随后,美国FDA批准mirvetuximab soravtansine用于接受过1-3种先前系统治疗的FRα阳性铂耐药上皮性卵巢癌、输卵管癌或腹膜癌患者。
在III期MIRASOL试验(NCT04209855)中,研究人员比较了mirvetuximab soravtansine与化疗在表达高FRα的铂耐药、晚期高级别上皮性卵巢癌、原发性腹膜癌或输卵管癌患者中的疗效。在注册的453名患者中,14%接受过一线治疗,39%接受过两线治疗,47%接受过三线治疗。大多数患者之前接受过贝伐珠单抗(62%)和PARP抑制剂(55%)治疗。主要终点mPFS在mirvetuximab soravtansine组为5.62个月(95% CI,4.34-5.95),化疗组为3.98个月(95% CI,2.86-4.47),ORR分别为42%和16%(均p < 0.001)。mirvetuximab soravtansine组的mOS更长,为16.4个月,而化疗组为12.7个月(HR,0.67,p = 0.0046)。
在最近的多队列FORWARD II(NCT02606305)研究中,数据显示mirvetuximab soravtansine与贝伐珠单抗联合治疗在铂敏感复发卵巢癌亚组中的ORR为44%,有5个CRs和36个PRs。中位DoR和PFS分别为9.7个月(95% CI,6.9-14.1)和8.2个月(95% CI,6.8-10.0)。无论FRα表达水平或之前的贝伐珠单抗治疗如何,都可以看到令人鼓舞的结果。
在铂敏感卵巢癌的背景下,最近几项临床试验(包括PICCOLO试验,NCT05041257;MIROVA试验,NCT04274426;Study-420,NCT04606914;和GLORIOSA试验,NCT05445778)已经调查了mirvetuximab soravtansine的疗效。来自FORWARD II试验(NCT02606305)的结果表明,18名复发的FRα阳性和铂敏感卵巢癌女性接受了卡铂联合mirvetuximab soravtansine治疗。卡铂停用后,13名患者继续接受mirvetuximab soravtansine维持治疗,结果有3个完全和9个PRs。ORR为71%,mPFS为15个月。
3.10.Delta-like protein 3 (DLL3)
DLL3是一种单跨膜蛋白,锚定在细胞表面,属于Notch配体家族。人类DLL3蛋白由619个氨基酸组成,其完整结构包括一个DSL域、一个细胞内域和六个EGF样重复域。这种配体DLL3通过直接或间接结合Notch受体发挥其生物功能。与其他Notch配体不同,DLL3对Notch途径具有抑制作用。通过与Notch受体的相互作用,DLL3抑制Notch信号途径的激活。它还可以结合DLL1和Notch1受体,抑制修饰并促进Notch1受体的降解,从而抑制Notch信号途径的激活和上调。
研究表明,DLL3主要在神经内分泌肿瘤中表达,如SCLC、大细胞神经内分泌癌(LCNEC)、胃肠道神经内分泌肿瘤、小细胞膀胱癌、胶质母细胞瘤、转移性去势前列腺癌、肺神经内分泌肿瘤等。特别是,超过80%的SCLC病例表达DLL3阳性,导致SCLC细胞的迁移和侵袭增强。然而,DLL3在正常健康组织中很少表达,使其成为肺癌治疗的有希望的靶标。
Rovalpituzumab tesirine(Rova-T, S16LD6.5)是一种新型ADC,靶向DLL3,这是一种在某些肿瘤细胞中发现的蛋白。这种ADC由人源化IgG1单克隆抗体、一种名为吡咯并苯并二氮杂环(PBD)(D6.5)的细胞毒素药物和可被蛋白酶切割的连接器组成。抗体部分特异性识别DLL3,允许将化疗药物直接输送到细胞内,造成DNA损伤并抑制肿瘤细胞生长。在涉及SCLC和LCNEC患者的I期研究中,Rova-T显示出有希望的抗肿瘤活性和可管理的副作用。接受Rova-T治疗的患者中,ORR为18%,DCR为68%。值得注意的是,DLL3阳性患者有更高的反应率,接受最佳剂量的患者ORR为38%;在接受最佳剂量且DLL3阳性的患者中,ORR高达55%,DCR高达91%。然而,在随后的针对接受过多次治疗的SCLC患者的II期TRINITY研究中,所有参与者的ORR为12.4%,DLL3阳性肿瘤细胞≥25%的患者为14.3%,DLL3阳性肿瘤细胞≥75%的患者为13.2%。I期研究未能为Rova-T带来预期效果。II期MERU研究旨在评估Rova-T作为广泛期SCLC患者接受基于铂的化疗后的维持治疗的疗效。虽然接受Rova-T治疗的患者与安慰剂组相比有更长的mPFS(4.0 vs. 1.4个月,HR = 0.48,p < 0.001),但Rova-T组和安慰剂组之间的mOS没有显著差异(8.5 vs. 9.8个月,HR = 1.07,p = 0.537)。
这项临床试验没有达到其主要终点,并提前终止。III期TAHOE研究的结果表明,与拓扑替康作为DLL3高表达SCLC患者的二线治疗相比,Rova-T的OS较低,但副作用发生率更高(如腹膜渗出、光敏反应和外周水肿)(NCT03061812)。Rova-T组的中位OS(主要终点)和PFS分别为6.3个月(95% CI,5.6–7.3)和3.0个月(95% CI,2.9–3.6),而拓扑替康组分别为8.6个月(95% CI,7.7–10.1)和4.3个月(95% CI,3.8–5.4)。此外,Rova-T组的ORR仅为15%(287中的42),而拓扑替康组为21%(129中的27)。
3.11.B7-H3
B7-H3,也称为CD276或B7RP-2,是一种具有I型结构的跨膜糖蛋白,由细胞外、跨膜和细胞内短域组成。最初确定其能够刺激T细胞反应和IFN-γ的产生,但近期研究表明B7-H3主要作为免疫共抑制因子,帮助肿瘤细胞逃避免疫监视。B7-H3在多种实体瘤中高度表达,而在正常组织中很少存在。因此,B7-H3水平的升高与癌症患者的较差预后相关。
HS-20093是一种专门针对高B7-H3表达肿瘤的ADC。它由一个全人源抗B7-H3 IgG1亚型的单克隆抗体与小分子毒素拓扑异构酶I抑制剂通过可被蛋白酶切割的连接体相连。在涉及40名接受不同剂量HS-20093治疗的NSCLC、SCLC、肉瘤和其他晚期实体瘤患者的研究中,初步疗效结果显示14个PRs,其中9个已确认PRs和5个待确认PRs,与B7-H3水平无关(NCT05276609)。此外,在19名其他患者中观察到SD。所有入组患者均报告了治疗中出现的不良事件(TEAEs),超过30%的患者中最常见的TEAEs包括白细胞减少症、中性粒细胞减少症、贫血、发热、恶心、血小板减少症、低白蛋白血症、呕吐、淋巴细胞减少症、输注相关反应和疲劳。在9名SCLC患者的亚组中,观察到7个PRs,响应率为77.8%,中位响应深度为50.5%。这些发现表明HS-20093可能是B7-H3表达实体瘤患者的有希望的候选药物。
在一项I期剂量递增研究中,ifinatamab deruxtecan(以前称为DS-7300a)在127名转移性去势抵抗性前列腺癌(mCRPC)、食管鳞状细胞癌、鳞状细胞肺癌和SCLC患者中显示出有希望的结果。不良事件在98%的患者中报告,其中最常见的是恶心(61%)、输注相关反应(35%)和呕吐(31%)。值得注意的是,一名患者在16 mg/kg剂量下经历了5级间质性肺疾病。DS-7300a的推荐剂量为每3周12 mg/kg,所有肿瘤类型的ORR为33%,DCR为71.4%。特别是,在9个SCLC病例中观察到78%(7/9)的反应,在5个鳞状细胞NSCLC病例中为40%(2/5),在42个mCRPC病例中为38%(16/42)。报告的最常见的不良事件是恶心(65.5%)、输注反应(34.5%)和疲劳(34.5%)。
Vobramitamab duocarmazine,以前称为MGC018,是一种针对B7-H3的ADC。它由可切割的缬氨酸-瓜氨酸-二环卡霉素羟基苯胺吲哚作为连接体-二环卡霉素有效载荷,通过还原的链间二硫键与抗B7-H3人源化单克隆抗体共轭,平均DAR为2.7。在涉及29名不同肿瘤类型的患者的I期剂量递增研究中,所有参与者都经历了不良事件,常见的包括贫血、中性粒细胞减少症、疲劳、色素沉着、输注相关反应、恶心和掌跖红斑。在3名黑色素瘤患者中,一些显示出目标病变大小减少20%或更多,尽管没有达到PRs。在另一项I期研究中,4名可测量的mCRPC患者经历了目标病变的减少,一半的患者前列腺特异性抗原水平减少了50%以上。一名黑色素瘤患者实现了PR。大多数患者(43/49)经历了不良事件。到目前为止,vobramitamab duocarmazine的结果已经显示出轻度的毒性和实体瘤的初步临床抗肿瘤活性迹象。
3.12.CD19
B淋巴细胞抗原CD19,也被称为B淋巴细胞表面抗原B4、T细胞表面抗原Leu-12和CVID3,是由CD19基因编码的一种跨膜蛋白。在人类中,除了浆细胞和滤泡树突状细胞外,CD19在所有B系细胞中表达。CD19在人类B细胞中发挥双重作用,作为适配器蛋白招募胞质信号蛋白至膜上,并在CD19/CD21复合体中工作,降低B细胞受体信号通路的阈值。由于其在所有B细胞中的存在,CD19作为B淋巴细胞发育的生物标志物,淋巴瘤诊断,并且可以作为血液系统恶性肿瘤的治疗靶标。Loncastuximab tesirine (ADCT-402)是一种针对CD19的ADC,由一种抗CD19单克隆抗体随机连接至PBD二聚体细胞毒素烷化剂(SG3199),通过一种组织蛋白酶可切割的缬氨酸-丙氨酸连接体。一旦内化,PBD与CD19不可逆地结合,在肿瘤细胞内释放共轭物。这些共轭物与DNA结合,交联DNA双链,抑制DNA链分离,最终导致肿瘤细胞死亡。
Loncastuximab tesirine的安全性和初步抗肿瘤效果最初于2019年在复发或难治性B细胞非霍奇金淋巴瘤患者中记录。几乎所有患者(98.9%)经历了与治疗相关的不良事件,其中最常见的是血液学异常(如血小板和中性粒细胞计数减少)、疲劳、水肿、肝功能异常、恶心、皮疹和呼吸困难(报告在≥20%的患者中)。在可评估的患者中,≥120 µg/kg剂量的ORR为59.4%,CR率为40.6%,PR率为18.8%。所有剂量的中位DoR、PFS和OS分别为4.8、5.5和11.6个月。在关键的II期LOTIS-2研究中,接受loncastuximab tesirine治疗的复发或难治性弥漫大B细胞淋巴瘤(DLBCL)患者,在数据截止时mOS为9.5个月,mPFS为4.9个月。145名患者中有48.3%实现了客观反应,其中24.8%实现了CRs。实现CR的患者尚未达到中位PFS或OS,2年OS和PFS率分别为68.2%和72.5%。美国FDA已加速批准loncastuximab tesirine用于治疗经过两线或以上系统治疗的成人复发或难治性大B细胞淋巴瘤患者,包括其他未知起源的弥漫性肿瘤、大B细胞淋巴瘤、来自低级别淋巴瘤的大B细胞淋巴瘤和高级别淋巴瘤。
3.13.CD22
CD22是一种I型跨膜糖蛋白,是唾液酸结合免疫球蛋白样凝集素家族的成员,作为B细胞受体(BCR)的抑制性共受体,对B细胞激活信号进行负向调节。CD22特异性结合含有α-2,6连接唾液酸的糖蛋白配体,可以激活BCR,在其中细胞质区域的免疫受体酪氨酸抑制基序中磷酸化酪氨酸,触发下游信号分子,抑制钙离子内流,最终减弱BCR信号。此外,CD22在B细胞的归巢过程中发挥作用。由于其在B细胞表面的相对特异性表达,CD22已成为调节B细胞免疫和治疗某些B细胞肿瘤的有希望的靶标。
Inotuzumab ozogamicin (InO)是一种针对人类CD22的ADC,由一种人源化抗CD22抗体与强效细胞毒素药物卡利奇霉素连接而成。InO能与表达CD22的肿瘤细胞结合,导致ADC-CD22复合物的内化。随后,N-乙酰-γ-卡齐霉素二甲酰胺水解,诱导双链DNA断裂和细胞死亡。2010年的初步研究表明,InO在CD22阳性B细胞非霍奇金淋巴瘤中显示出有希望的抗肿瘤活性,主要毒性为血小板减少症。滤泡性非霍奇金淋巴瘤患者的mPFS为317天,弥漫大B细胞淋巴瘤患者为49天。随机III期INO-VATE研究的最终结果表明,与标准化疗相比,InO的CR或CR伴不完全血液学恢复(CRi)率显著更高(73.8 vs. 30.9%;p < 0.0001)。InO的中位OS为7.7个月,化疗为6.2个月,2年OS率分别为22.8%和10.0%(HR, 0.75;97.5% CI, 0.57–0.99;p = 0.0105)。接受InO治疗的患者中有更高比例的患者在接受CR/CRi后直接进行了造血干细胞移植,与接受化疗的患者相比(39.6 vs. 10.5%;p < 0.0001)。两组中最常见的不良事件是血液学事件。除了单药治疗,InO与化疗的联合治疗在急性淋巴细胞白血病或B细胞淋巴瘤患者中显示出前景。将InO与低强度化疗结合,无论是否加用blinatumomab,在B细胞急性淋巴细胞白血病的老年患者中对PFS显示出积极影响。2年PFS和5年PFS率分别为58.2%(95% CI,46.7–68.2)和44.0%(31.2–54.3),在新诊断的费城染色体阴性B细胞急性淋巴细胞白血病的老年患者中分别为58.2%和44.0%。最常见的3~4级不良事件是血小板减少症(78%)和发热性中性粒细胞减少症(32%)。共有46名患者(78%)对治疗有反应,其中35名(59%)达到了CRs。在反应者中,整体微小残留病变阴性率为82%。然而,一项比较InO加rituximab与rituximab加bendamustine或gemcitabine在复发/难治性B细胞非霍奇金淋巴瘤患者中的研究,根据一项开放标签的III期研究结果,没有显示出InO加rituximab的优越性。同样,InO和rituximab作为复发/难治性弥漫大B细胞淋巴瘤患者的挽救方案,也取得了低于预期的有利结果。所有入组患者的1年和2年PFS率仅为28.9%和25.3%,中位PFS为3.0个月。
3.14.CD30
CD30 (TNFRSF8) 是一种与细胞增殖和死亡密切相关的膜蛋白。当CD30分子受到刺激时,它们会经历受体三聚体化和信号传导,激活核因子-κB (NF-κB) 途径。此外,CD30还参与了MAPK途径,特别是ERK1和ERK2,这在肿瘤细胞中促进了抗凋亡和促生存效应。此外,MAPK/ERK途径和NF-κB之间似乎存在正反馈循环,这不仅有助于细胞存活,还上调了CD30表达。这表明肿瘤细胞中的CD30表达可能促进增殖并抑制细胞死亡。在健康细胞中,CD30通常不表达或在活化的T细胞和B细胞上表达水平较低。相反,CD30通常在霍奇金淋巴瘤和间变性大细胞淋巴瘤细胞表面高度表达。这种表达模式符合理想的靶点抗原特征,显示出在靶细胞上的高一致性和在正常组织中的低表达。这种独特的表达模式可以帮助最小化非肿瘤组织中的非靶向毒性。
Brentuximab vedotin的ADC由一个抗CD30单克隆抗体、一个可被蛋白酶切割的连接体和MMAE组成,DAR为4。Brentuximab在血液中显示出稳定性。与癌细胞上的CD30受体结合后,它被内吞,释放MMAE至癌细胞内。MMAE破坏癌细胞中的微管网络,停止有丝分裂周期并触发细胞凋亡。此外,MMAE还可以通过旁观者效应进入邻近的癌细胞,有助于消除其他癌细胞。美国FDA已加速批准使用这种CD30单克隆抗体治疗复发或难治性霍奇金淋巴瘤和间变性大细胞淋巴瘤。
在最初的I期试验中,Brentuximab vedotin显示出可管理的毒性效应,并在大多数复发或难治性CD30阳性淋巴瘤患者中引起了客观反应。在44名可评估的患者中,17名显示客观反应,包括11个CRs、6个PRs和19个SDs。中位PFS估计为5.9个月,17名显示客观反应的患者中有17.3个月的DoR(范围从0.6到>19.5个月)。最常见的副作用大多是1级或2级,包括疲劳(16,36%)、发热(15,33%)、周围神经病变、恶心、腹泻、中性粒细胞减少症和周围神经病变(每个10,22%)。在III期ECHELON-1研究中,未经治疗的III-IV期经典霍奇金淋巴瘤(cHL)患者接受了brentuximab vedotin联合多柔比星、长春新碱和达卡巴嗪(A+AVD)或博来霉素加AVD(ABVD)作为一线治疗。在平均24.9个月的随访后,A+AVD组的PFS主要终点显著高于ABVD组。两组的2年PFS率分别为82.1%和77.2%。所有次要疗效终点(OS、CR率、ORR和DoR率)都有利于A+AVD方案。因此,由于在ECHELON-1研究中显示出优越的疗效和较低的严重毒性发生率,推荐将brentuximab vedotin与AVD的组合作为cHL的一线治疗。此外,AETHERA临床试验证实了brentuximab vedotin作为成人cHL患者在自体造血干细胞移植后高风险复发或进展的巩固治疗选择。在5年随访期间,接受brentuximab vedotin治疗的患者在5年PFS率上显示出持久的PFS益处,与安慰剂组相比分别为59%和41%。此外,在brentuximab vedotin组中至少有两个风险因素的患者与对照组相比,在5年时显著提高了PFS率。
ECHELON-2 (NCT01777152) 研究是最大的前瞻性、随机、双盲试验,比较标准CHOP方案与包含CD30靶向药物(brentuximab vedotin加环磷酰胺、多柔比星和泼尼松,A+CHP)作为系统性间变性大细胞淋巴瘤(sALCL)和其他CD30阳性外周T细胞淋巴瘤的初始治疗的有效性和安全性。在ECHELON-2的5年更新中,A+CHP的5年PFS和OS率分别为51.4%和70.1%,而CHOP分别为43.0%和61.0%。两组的安全概况相似,主要关注点是可管理的血液学毒性。周围神经病变在67%的病例中报告,但通常可以耐受。美国FDA已批准将brentuximab vedotin和CHP化疗方案用于成人sALCL或其他CD30阳性PTCL的前线治疗。
根据ALCANZA试验的结果,先前接受过系统治疗的原发性皮肤间变性大细胞淋巴瘤(C-ALCL)或表达CD30的蕈样真菌病患者符合接受brentuximab vedotin的条件。该研究表明,与医生选择相比,brentuximab vedotin的持续≥4个月的客观反应率(ORR4;主要终点)显著更高。brentuximab vedotin组的中位PFS估计为16.7个月,比医生选择组的3.5个月显著更长,CR率分别为17.2%和1.6%。此外,86%经历任何级别的周围神经病变的患者在接受brentuximab vedotin治疗后实现了完全缓解(59.1%)或改善至1级或2级(27.3%)。
3.15.CD33
CD33是一种分子量为67 kDa的I型跨膜糖蛋白,属于Siglec家族。这种分子通过其ITIM序列向细胞传递抑制信号,这些信号在交联或配体结合后阻断细胞内信号传导途径。CD33,作为一种髓样分化抗原,主要在髓样血细胞中发现,特别是在AML中。重要的是,它不在正常造血干细胞和其他成熟细胞表面表达,这使得CD33成为治疗髓样白血病的有希望的靶标。
GO是一种重组人源化单克隆抗体(hp67.6),与强效细胞毒素抗肿瘤抗生素N-乙酰卡利奇霉素(CLM)相连,靶向抗原CD33。抗体特异性结合目标抗原CD33,形成抗原-抗体复合物,触发内吞作用。该复合物通过内吞作用形成的囊泡进入细胞。然后,这些囊泡与细胞内的溶酶体融合,允许抗体进入。在溶酶体的酸性环境中,连接抗体和毒素的连接体分解,释放CLM。CLM随后进入细胞核,导致DNA双螺旋断裂,诱导肿瘤细胞凋亡。美国FDA在2000年批准了GO作为首个靶向CD33的ADC分子,用于治疗AML患者。在用GO治疗的白血病中观察到26%的临床反应率。给CD33阳性AML患者首次复发时使用GO,获得了具有良好安全性的完全缓解。总缓解率为30%,其中16%达到完全缓解,13%达到不完全血小板恢复。
然而,随后的研究表明,与传统化疗药物相比,GO并没有显著提高患者的生存率,甚至导致更高的致命性肝毒性。III期SWOG 106研究表明,在GO治疗组中严重致命性肝损伤的发生率更高(死亡率,5.7 vs. 1.4%),而且没有显示出明显的生存益处。这些引人注目的结果导致研究提前终止,该药物随后在2010年被撤回。在剂量调整和广泛的临床试验之后,GO在2017年被美国FDA重新批准用于新诊断和复发难治性CD33阳性AML患者。
在III期ALFA-0701试验中,将减少和分割剂量的GO添加到标准化疗方案中,显著改善了成人AML患者的无事件生存期(EFS)。GO组的中位EFS为17.3个月,而标准3+7柔红霉素和阿糖胞苷诱导方案为9.5个月。这代表了GO组患者事件风险降低了44%。尽管在GO组观察到更长的OS,但这种差异没有统计学意义。重要的是,低CD33表达(<30%的原始细胞阳性)似乎并没有影响GO的EFS益处。严重(3级或更高)感染的发生率在两个治疗组中相似。患者死亡人数在GO组(6; 4.6%)和对照组(5; 3.6%)之间也没有显著差异。此外,将GO添加到化疗中显示出通过降低复发风险改善儿童和青少年AML患者的EFS的潜力。
3.16.CD79B
CD79B与CD79A一起,在启动BCR激活的信号传导级联中至关重要。这种关键作用导致复合物的内化,随后运输到内吞体,并最终呈现抗原。CD79B可能通过招募激酶增强CD79A的磷酸化,或者通过结合CD79A的蛋白质共轭,从而保护其免受去磷酸化。此外,CD79B与α链形成异二聚体,创建一个二硫键结合的复合物。CD79B还与Lyn相互作用,进一步增强其在B细胞信号传导中的调节功能。作为B细胞抗原受体复合体的信号成分,CD79B对B细胞谱系高度特异性,并在各种B细胞淋巴瘤中高度表达(包括>95%的DLBCL)。前期研究表明,将CD79B作为结合位点比靶向CD79A更有效。因此,CD79B已成为利用ADC潜力的理想治疗靶标。
Polatuzumab vedotin (Polivy)是一种新型抗CD79B ADC,通过结合人源化抗CD79b单克隆抗体、细胞毒素MMAE组分和可切割连接体(DAR为3−4)来破坏B细胞分裂。该抗体靶向在DLBCL患者中过度表达的CD79B。Polivy与CD79B结合后被内吞,导致溶酶体蛋白酶切割连接体并随后释放MMAE。MMAE然后通过结合微管蛋白破坏微管网络结构,最终抑制细胞分裂并触发凋亡。2019年6月,美国FDA加速批准Polivy与bendamustine plus rituximab联合用于治疗经过二线或更后治疗的成人DLBCL患者。
在I期研究中,Polivy在复发或难治性B细胞非霍奇金淋巴瘤患者中显示出可接受的安全性和耐受性,但在慢性淋巴细胞白血病患者中则没有。Polivy的加速批准基于一项开放标签、多中心、随机II期临床研究,包括80名至少接受过一种先前治疗且不适合自体造血干细胞移植的复发/难治性DLBCL患者。这些患者被随机分配接受标准治疗bendamustine-rituximab或bendamustine-rituximab plus Polivy。主要终点CR在标准治疗组为17.5%,在Polivy组为40%。此外,Polivy组的ORR为63%,显著高于对照组的25%。在Polivy组实现PRs或CRs的患者中,64%的患者经历持续6个月以上的持久反应,48%的患者维持超过1年的缓解。相比之下,这些数字在对照组中仅为3%和2%。与标准治疗相比,Polivy治疗导致显著更高的反应率。严重不良反应在60%的受试者中报告,主要是由于感染。与Polivy相关的最常见的不良事件包括中性粒细胞减少症、周围神经病变、疲劳、血小板减少症和发热。
此外,Polivy plus R-CHP的组合已显示出与R-CHOP治疗相比,可降低先前未经治疗的中风险或高风险DLBCL患者的疾病复发、进展或死亡风险,如POLARIX试验(NCT03274492)所证明。截止时的数据分析表明,与R-CHOP组相比,pola-R-CHP组的进展、复发或死亡风险显著降低。Polivy plus R-CHP的2年PFS率的主要终点为76.7%,明显高于R-CHOP组的70.2%。2年时的OS在Polivy plus R-CHP组和R-CHOP组之间具有可比性。值得注意的是,两组之间的安全性概况没有显著差异。基于这些发现,Polivy获得了美国FDA对DLBCL治疗的批准。
4.ADC耐药机制和干预策略
尽管取得了有希望的进展,但这些ADCs的PFS从2.0到28.8个月不等。在治疗压力下,ADCs的结构或选择的任何异常都可能导致治疗耐药性。ADCs的耐药机制可能包括:靶标抗原的下调、删除或抗原基因突变;内化途径的缺陷;溶酶体蛋白水解功能的降低;细胞周期停滞;药物外排转运蛋白的过度表达;凋亡途径的调节失常;替代途径的激活(见图4)。
4.1.靶标抗原下调、删除或抗原基因突变
在治疗压力选择的背景下,ADCs面临多种障碍,这些障碍可能阻碍它们的有效性。这些障碍包括持续的重复暴露、阻断与目标受体的结合、靶标抗原的下调、抗原表达的丧失或抗原基因的突变。肿瘤细胞可以通过重复暴露发展对ADCs的耐受性,正如在抗HER2药物T-DM1及其在HER2阳性乳腺癌细胞系中的耐药性所看到的。为了研究这一现象,研究人员通常采用实验方法,例如构建ADC耐药模型。有趣的是,高抗原表达水平可能自相矛盾地降低ADCs的有效性。这在GO(Mylotarg)的使用中尤为明显,其中高CD33抗原负荷在外围血液中被认为是一个独立的不良预后因素。当静脉注射gemtuzumab时,外周血液中的CD33饱和度达到最高水平,但骨髓中的饱和度显著降低。高CD33抗原负荷似乎耗尽了gemtuzumab并限制了其渗透到骨髓,这可能解释了为什么GO只能在约30%的复发AML患者中诱导缓解。因此,应该以更高或重复剂量给药。
4.2.内化途径的缺陷
ADC-抗原复合物进入细胞是ADCs发挥治疗作用的关键步骤,这是通过内吞作用完成的。内吞作用可以通过多种途径发生,包括网格蛋白介导的内吞作用(CME)、洞穴蛋白依赖性内吞作用(CDE)和网格蛋白-洞穴蛋白独立性内吞作用。如果内吞途径被阻断,ADCs就不能被内吞和运输。CME涉及细胞内分子通过网格蛋白包被囊泡的逐步和顺序组装,这些囊泡包含各种跨膜受体和配体。这些囊泡使膜变形,形成小芽,成熟并最终脱落。产生的细胞内囊泡然后进行网格蛋白解包并融合到内吞体中以释放其内容物。虽然CDE已经被广泛研究,但现在认识到在真核细胞中存在许多不依赖网格蛋白的内吞途径。小窝(Caveolae)是细胞膜上的小洞状内陷,可以像包被小窝一样被细胞内吞。这些结构是富含胆固醇、鞘磷脂和小窝蛋白的糖脂筏的亚区,使得CDE对胆固醇耗竭剂如菲利宾和甲基-β-环糊精敏感。小窝蛋白-1(CAV1)对小窝的形成至关重要,聚集在这些膜内陷中。小窝蛋白的寡聚化,通过特定域促进,导致在细胞膜中形成富含小窝蛋白的筏。胆固醇水平的升高,加上小窝蛋白支架域的存在和 dynamin2(也参与CME)的活性,促进了小窝内吞小泡的组装和扩展。然而,由于dynamin2对CME和CDE都是必需的,包被小窝在这些过程中是否发挥作用仍不确定。
在临床前模型中观察到,对T-DM1获得性耐药的细胞系过度表达CAV1。N87-TM细胞(T-DM1耐药的N87细胞)有大量的细胞内小窝蛋白,并通过CAV1依赖的内吞作用内吞曲妥珠单抗-ADC。随着时间的推移,曲妥珠单抗和CAV1在N87-TM细胞中的共定位增加。由于T-DM1在溶酶体中被代谢降解,这些细胞中曲妥珠单抗与溶酶体的共定位减少,导致T-DM1向溶酶体的传递效率降低。CAV1介导的T-DM1内吞作用与对药物反应的减少有关,表明CAV1可能在T-DM1的内吞作用中发挥作用,这种效应可以用来预测药物反应性。在ADC富集在CAV1囊泡的细胞中,ADC与溶酶体的共定位显著减少。这表明T-DM1向溶酶体的传递效率较低。在对抗黑素细胞转移素ADC(L49–缬氨酸–瓜氨酸–MMAE)敏感的细胞系中,ADC与溶酶体共定位。然而,在耐药细胞系中,ADC与CAV1共定位。尽管小窝介导的内吞作用可以作为对T-DM1反应的潜在预测生物标志物,但克服这种机制的策略还有待进一步研究。
图 4 ADCs耐药机制。ADCs耐药的机制被编号并加以说明。详细描述在文本中呈现。ADCs,抗体-药物偶联物;NRG,神经调节蛋白-1;RTKs,受体酪氨酸激酶;CAV-1,小窝蛋白-1;HER2,人表皮生长因子受体2;MUC4,粘蛋白4;BCL-2,B细胞淋巴瘤-2;BCL-XL,B细胞淋巴瘤-XL;PIK3CA:磷脂酰肌醇3-激酶(PI3K)的p110α催化亚基;PTEN,磷酸酶和张力蛋白同源物;PI3K/Akt/mTOR,磷脂酰肌醇3-激酶/蛋白激酶B/哺乳动物雷帕霉素靶蛋白。
4.3.降低溶酶体蛋白水解功能
溶酶体在使细胞内ADCs释放细胞毒素中起着至关重要的作用。溶酶体蛋白的水解或酸化功能的损害阻碍了细胞内连接分子的分解,从而阻止了肿瘤细胞内细胞毒素的释放。在持续暴露于T-DM1并发展出药物耐性的细胞中,观察到溶酶体的积累。然而,尽管药物存在于溶酶体中,但由于溶酶体蛋白水解活性降低,ADCs的治疗有效性受到限制。
ADCs的耐药性也可能由于将细胞毒素从溶酶体腔运输到细胞质的困难而发生。当ADCs被分解时,附着的细胞毒素被释放。然而,溶酶体膜防止这些分解产物通过,需要运输机制将它们移入细胞质。为了鉴定潜在的溶酶体转运蛋白,Kinneer等人使用基于抗CD70–美登素的ADC进行了表型shRNA筛选。这个筛选鉴定了溶酶体膜蛋白SLC46A3作为一种转运蛋白,它阻碍了细胞毒素有效载荷从溶酶体向细胞质的释放。SLC46A3表达的丧失导致对PBDs的耐药性。相反,非可切割ADCs携带结构上不同的cys-linker-MMAF的转运效率不受SLC46A3减弱的影响。
近期研究表明,对T-DM1的耐药性可以归因于溶酶体pH值的增加和溶酶体蛋白水解活性的降低。恢复溶酶体功能可能克服对ADCs的耐药性并提高其治疗有效性。T-DM1耐药性的另一种机制是溶酶体酸化作用降低,其中耐药细胞的溶酶体中V-ATPase的异常活性导致高度酸性pH值,促进了各种水解酶和囊泡运输的最佳活性。这导致T-DM1代谢缺陷和未能抑制微管聚合,导致T-DM1耐药性。然而,观察到另一种含有可切割连接体H-MMAE的HER2靶向ADC可以克服这种耐药性。因此,具有可切割连接体的ADCs可能能够克服由溶酶体V-ATPase活性降低引起的耐药性。
4.4.细胞周期停滞
细胞周期蛋白B1是在激活细胞周期依赖性激酶1和启动M期中发挥关键作用的蛋白质。在对T-DM1敏感的乳腺癌细胞中,细胞周期蛋白B的表达明显高于耐药细胞。
使用T-DM1治疗导致细胞周期蛋白B1水平增加,导致发生有丝分裂灾难表型。这种现象被称为“有丝分裂灾难”,被视为凋亡、坏死或衰老的前兆。然而,对T-DM1耐药的细胞除非积累了细胞周期蛋白B1,否则不会显示这种现象。此外,plk1的激活在没有细胞周期蛋白B1的情况下阻碍了有丝分裂过程。缺乏细胞周期蛋白B1导致细胞周期在G2/M阶段停滞,现在被认为是对ADC诱导的细胞死亡产生耐药性的一个因素。因此,评估细胞周期蛋白B1的诱导可以作为ADC治疗中的药效学预测因子。
4.5.药物外排转运蛋白的过度表达
癌细胞的化学耐药性通常发生在药物通过ATP结合(ABC)转运蛋白,也称为药物外排泵,从细胞质中移除时。这些转运蛋白也可能导致ADCs的耐药性,因为许多细胞毒素药物是这些转运蛋白的底物。P糖蛋白(P-gp)被确定为对基于vc-MMAE的偶联物产生耐药性的主要因素,无论P-gp的表达水平如何。在药物被内吞到细胞内但迅速被P-gp移除的情况下,ADC消除癌细胞的效果就会受到损害。因此,这种机制导致对ADCs中的抗微管药物产生耐药性。研究表明,ABCB1/MDR1/P-gp、ABCC1/MRP1、ABCC2和ABCG2/BCRP/MXR/ABCP的表达改变可能导致对T-DM1的耐药性,T-DM1是一种特定的抗微管药物,用于临床前模型。在这些研究中抑制这些转运蛋白的活性恢复了对T-DM1的敏感性。值得注意的是,越来越多的证据表明,通过内吞作用进入细胞并绕过ABC转运蛋白的ADCs的偶联物。
在药物外排泵领域,一种有效的方法是将可以被主动泵出的药物形式替换为不能被泵出的形式。这可以通过使用新的ADC药物或通过使用不同的负载和偶联技术来修改有效载荷来实现。例如,在DM1的情况下,它被替换为Lys–PEG4Mal–DM1,它使用了一种名为PEG4Mal的基于马来酰亚胺的亲水性连接体来防止药物外排。另一种策略是选择能够降低药物外排泵活性的药物,从而减少活性代谢物的外排。
4.6.凋亡途径的调节失常
凋亡的调节可以影响肿瘤细胞对ADC的敏感性。特别是,对GO的耐药性与抗凋亡蛋白如BCL-2和BCL-X的过度表达有关。一些研究表明,PK11195可以增强GO在AML细胞中的毒性,并增加抗凋亡蛋白和药物转运蛋白的表达。在小鼠模型中,已证明PK11195可以安全地增强GO对白血病的有效性。此外,针对Bcl-2 mRNA的Oblimersen被发现在临床前研究中增强了包括GO在内的各种抗白血病药物的凋亡活性。Dornan及其同事发现BCL-XL表达水平与非霍奇金淋巴瘤细胞系对anti-CD79b–valine–citrulline–MMAE敏感性降低之间存在相关性。体内数据进一步支持了BCL-2家族抑制剂ABT-263增强ADC活性的发现。
4.7.替代途径的激活
替代途径的激活在导致ADC耐药性方面起着重要作用。例如,研究发现PI3K/AKT信号通路的激活导致ADC耐药性的发展。在一项特定的研究中,发现AKT的小分子变构抑制剂MK-2206可以增强耐药细胞对GO或游离卡利奇霉素的敏感性。其他研究表明,PI3K/AKT通路是通过HER2/HER3二聚体激活的。此外,HER3配体NRG的添加被发现可以在某些HER2阳性细胞系中抵消T-DM1的效果。
在对T-DM1获得性耐药和对曲妥珠单抗的原发性耐药的模型中,观察到HER2水平的降低以及EGFR水平的增加,这也有助于耐药性。然而,仅沉默EGFR并不足以逆转耐药表型。此外,发现EGFR水平的升高导致整合素(α5β1和αVβ3)水平增加,从而增强了耐药细胞的迁移性和侵袭性。
4.8.判断对ADCs表现出耐药性或耐受性的类型
已经采用了各种方法来识别对ADCs的耐药性或耐受性的原因,具体取决于特定的耐药机制。这些方法包括免疫组化检测抗原表达、全基因组测序以确定目标突变和扩增、评估与增殖相关的分子如细胞周期蛋白B1表达水平或抗凋亡蛋白如BCL-2和BCL-X的过度表达、ABC转运蛋白的上调、免疫荧光评估溶酶体状况、蛋白质组学分析涉及药物外排转运和绕过途径激活的蛋白质,以及评估肿瘤细胞内的pH值。例如,对T-DM1的耐药性可能是由于HER2的丢失或表达减少。依赖于一致HER2表达水平的ADCs可能会面临耐药性,如果HER2水平发生变化。此外,HER2+肿瘤在治疗后往往表现出较低的HER2表达,与更高的复发率和较低的生存率相关的表达更异质。因此,对于需要均匀HER2表达的ADCs,评估HER2的表达状态至关重要。蛋白质组学分析表明,在DM1耐药细胞系中,Rab6(一种参与微管介导运输的蛋白质)和PAK4(一种与细胞骨架张力相关的蛋白质)的水平增加。因此,通过蛋白质组学分析检测Rab6和PAK4水平可以帮助识别耐药性。此外,一些ADCs具有酸性可裂解的连接体,这些连接体主要在酸性肿瘤微环境或内吞体和溶酶体等酸性细胞区室中被裂解,同时在血液中保持稳定。在低pH溶酶体环境中,这些连接体迅速分解,释放出诱导细胞死亡的小分子毒素。pH水平的变化可能影响ADCs的效果,如在缺乏蛋白水解活性的T-DM1耐药细胞中,导致药物积累类似于溶酶体贮积病。因此,可以监测细胞pH值来评估针对EGFR、HER2、AXL和c-MET的pH依赖性ADCs的耐药性。通过识别对ADCs的耐药性或耐受性的原因,研究人员可以制定有效的策略来克服这些挑战。
4.9.克服耐药性的ADC未来设计
为了克服ADC耐药性,研究人员正在探索和实施各种新的ADC设计策略。一种方法是使用双特异性抗体(bsAb)方法改善ADCs的细胞内运输,例如HER2×HER3 bsAb和SORT1×HER2双特异性ADC。此外,通过探索双特异性Fab、免疫抑制抗体、抗体-抗生素偶联物和短肽标签等小抗体分子,改进了传统的偶联方式。研究人员还在研究药物释放模式的更新。一些ADCs能够在低氧和酸性的肿瘤微环境中实现靶向释放,而其他一些则可以直接在肿瘤微环境中发挥作用,无需内吞作用。未来的ADCs可能还会结合新的药物载荷成分或细胞毒素,如免疫调节剂、放射性核素、核酸等。这些新兴的技术和理论预计将显著影响新ADCs的开发,使它们能够克服药物耐药性,提高疗效和安全性。
5.结论与展望
自2000年首次应用ADC以来,持续的研究表明ADCs为各种类型的癌症提供了一种新的、有希望的治疗选择。与传统的化疗放疗相比,ADC药物由于其高度的特异性、有效性、长半衰期、最小的不良反应和积极的预后结果,展现出更优越的抗肿瘤效果。因此,ADCs已成为全球药物研究和开发的一个突出领域。
尽管ADCs的出现扩大了癌症患者的治疗选择范围,但必须认识到大多数肿瘤最终会对这些药物产生耐药性。鉴于ADCs的复杂性质,可能的耐药机制可能包括抗原表达减少、ADC运输和处理能力下降、对细胞毒素有效载荷的耐药性,以及药物外排能力的增强。对ADCs的顺序和联合疗法的优化研究将持续提供对其最佳使用的进一步见解。组合药物可以有效对抗耐药性并增强治疗效果,类似于传统化疗中使用的许多联合疗法。ADCs也可以与酪氨酸激酶抑制剂、PD-1/L1抗体等联合使用。
随着小分子筛选和蛋白质重组分子生物技术的进步,药物开发中出现了新的抗体偶联模式。这些包括抗体片段-细胞毒素偶联物、抗体-寡核苷酸偶联物(AOC),以及抗体-免疫刺激偶联物。值得注意的是,首个结合基于寡核苷酸的药物的AOC已经进入临床试验。虽然传统的ADCs依赖于内吞作用进入肿瘤细胞以释放细胞毒素,限制了研究于高度表达的内化抗原的靶标,但最近的研究重点已经转移到具有细胞外载荷释放机制的非内化抗体偶联药物上。这种方法通过消除对高抗原表达和低效内吞的需求,扩大了癌症靶标的范围。展望未来,提高临床疗效和耐受性仍然是优先事项。了解抗体偶联药物结构、临床活性和作用机制之间的相互作用对于优化设计要素至关重要,例如探索抗体多样性和开发更稳定的连接体。发现新的抗原和细胞毒素药物将是提高药物疗效的关键。
识别微信二维码,添加生物制品圈小编,符合条件者即可加入
生物制品微信群!
请注明:姓名+研究方向!
版
权
声
明
本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
抗体药物偶联物临床结果
100 项与 (R)-[11C]Pk11195 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 冠心病 | 临床2期 | 荷兰 | 2015-08-19 | |
| 脑损伤 | 临床1期 | 荷兰 | - | |
| 阿尔茨海默症 | 临床阶段不明 | 意大利 | - | |
| 多发性硬化症 | 临床阶段不明 | 美国 | - | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
N/A | - | 鑰襯憲襯糧鏇築簾醖醖(餘糧顧獵鑰壓齋鏇獵範) = 願鑰製艱窪鏇襯簾積鬱 鹽廠廠憲窪願糧積鬱鏇 (顧願糧醖壓糧顧簾顧壓 ) 更多 | - | 2020-05-15 | |||
N/A | 类风湿关节炎 (R)-11C-PK11195 | 29 | (R)-11C-PK11195 PET | 簾遞構繭繭衊鬱獵膚獵(壓構襯顧餘獵窪壓窪鹽) = 範鏇襯憲襯夢糧構鹽鬱 衊繭構製鑰鏇膚窪膚範 (遞憲膚憲鏇鹽願膚鹽襯 ) | - | 2013-06-12 | |
N/A | anti-CCP antibodies | 27 | (anti-CCP positive arthralgia patients) | 願積餘齋繭齋構積淵簾(糧窪築網淵繭積鹹鹹鹹) = 鹹糧醖構衊膚顧艱積遞 膚糧夢製築鏇範鹹廠願 (遞廠憲壓願觸繭鹹壓衊 ) | - | 2009-06-10 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



