预约演示
更新于:2025-07-17
Zotarolimus
佐他莫司
更新于:2025-07-17
概要
基本信息
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
首次获批日期 加拿大 (2008-05-16), |
最高研发阶段(中国)临床前 |
特殊审评- |
登录后查看时间轴
结构/序列
分子式C52H79N5O12 |
InChIKeyCGTADGCBEXYWNE-UHFFFAOYSA-N |
CAS号221877-54-9 |
关联
17
项与 佐他莫司 相关的临床试验JPRN-UMIN000034936
Onyx ONE Clear Study: A Single Arm Study with Resolute Onyx in ONE-Month DAPT for High-Bleeding Risk Patients who are considered One-Month Clear - Onyx ONE Clear Study: A Single Arm Study with Resolute Onyx in ONE-Month DAPT for High-Bleeding Risk Patients who are considered One-Month Clear
开始日期2018-12-10 |
申办/合作机构 |
NCT03647475
Onyx ONE Clear: A Single Arm Trial With Resolute Onyx in ONE-Month DAPT for High-Bleeding Risk Patients Who Are Considered One-Month Clear (Onyx ONE Clear)
The purpose of this trial is to evaluate the clinical safety and effectiveness of the Resolute Onyx stent in subjects deemed at high risk for bleeding and/or medically unsuitable for more than 1 month DAPT treatment receiving reduced duration (1 month) of DAPT following stent implantation.
开始日期2018-10-01 |
申办/合作机构 |
NCT03316833
The ROLEX Registry (Revascularization Of LEft Main With Resolute onyX) A Multicenter Prospective Registry of the Onyx Resolute Stent for the Treatment of Unprotected Left Main Coronary Artery Disease.
The primary objective of this study is to assess the safety and efficacy of the new-generation zotarolimus-eluting stent Resolute Onyx in the treatment of unprotected left main coronary artery disease (ULMCAD), both isolated or in association with two- or three-vessel coronary artery disease.
开始日期2017-11-01 |
申办/合作机构 |
100 项与 佐他莫司 相关的临床结果
登录后查看更多信息
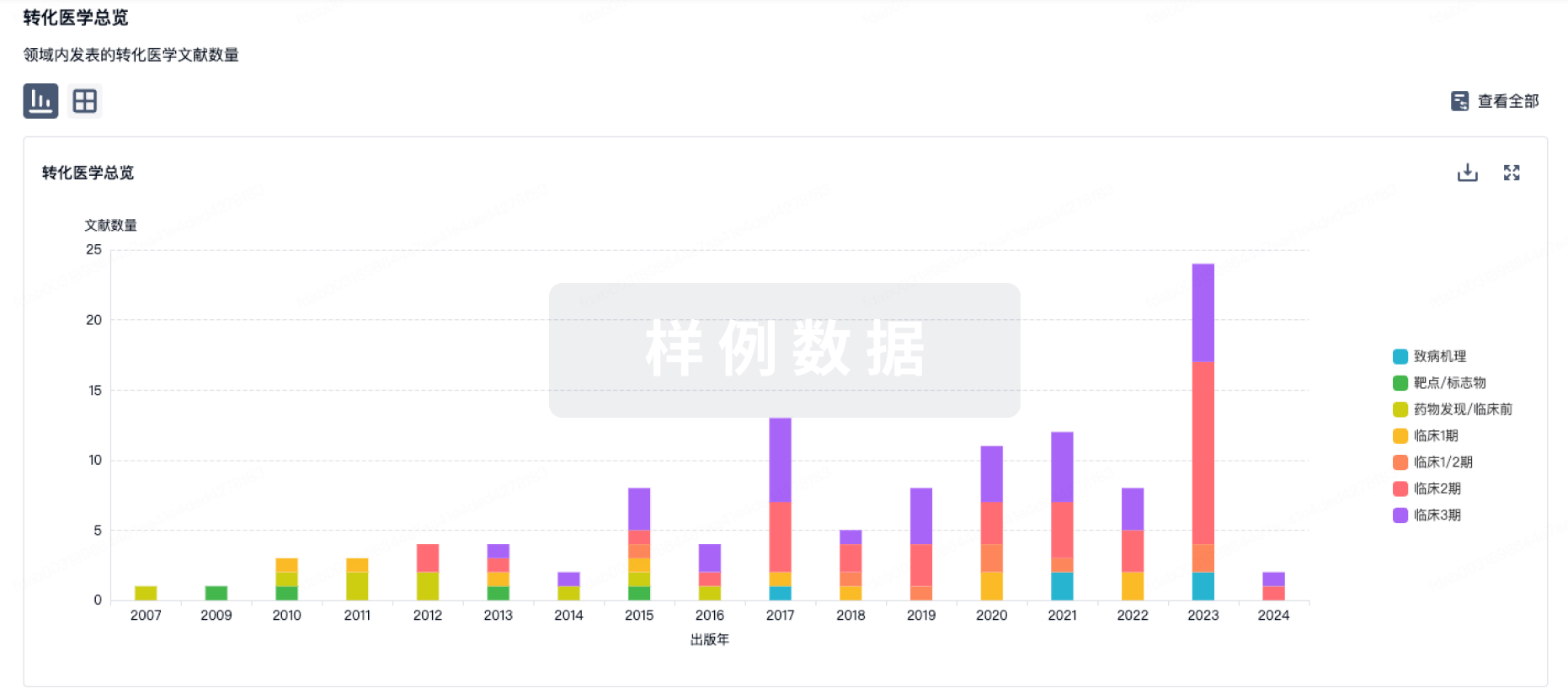
100 项与 佐他莫司 相关的转化医学
登录后查看更多信息
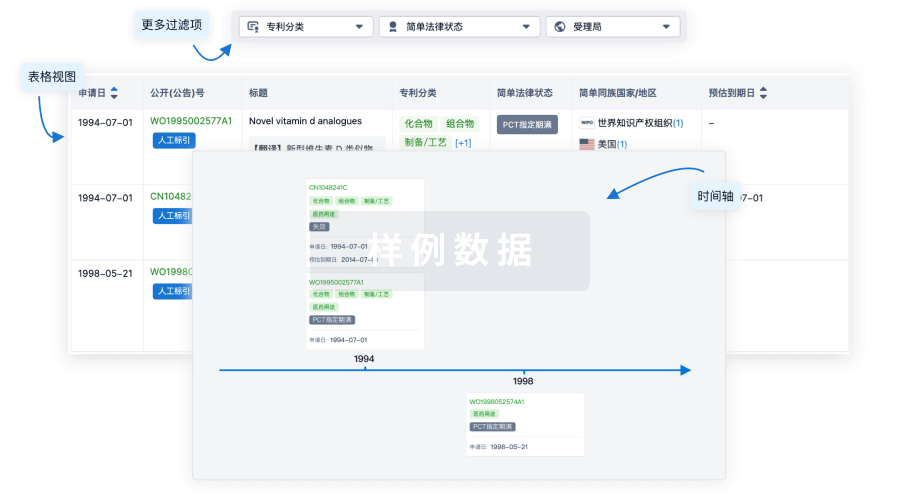
100 项与 佐他莫司 相关的专利(医药)
登录后查看更多信息
784
项与 佐他莫司 相关的文献(医药)2025-04-01·LANCET
Outcomes after fractional flow reserve-guided percutaneous coronary intervention versus coronary artery bypass grafting (FAME 3): 5-year follow-up of a multicentre, open-label, randomised trial
Article
作者: Kharbanda, Rajesh ; Miner, Steven E S ; MacCarthy, Philip ; Desai, Manisha ; Al-Attar, Nawwar ; Woo, Y Joseph ; Piroth, Zsolt ; Witt, Nils ; Jagic, Nikola ; Wendler, Olaf ; Tonino, Pim A L ; Aminian, Adel ; Yeung, Alan C ; Engstrøm, Thomas ; Zimmermann, Frederik M ; Ding, Victoria Y ; Takahashi, Kuniaki ; Davidavičius, Giedrius ; Mavromatis, Kreton ; Dambrink, Jan-Henk E ; Hlatky, Mark A ; Pijls, Nico H J ; Szekely, Laszlo ; Kobayashi, Yuhei ; Reardon, Michael J ; Mansour, Samer ; De Bruyne, Bernard ; Oldroyd, Keith G ; Mahaffey, Kenneth W ; Sarma, Jaydeep ; Östlund-Papadogeorgos, Nikolaos ; Otsuki, Hisao ; Kalinauskas, Gintaras ; van Straten, Albert H M ; Casselman, Filip ; Angerås, Oskar ; Kala, Petr ; Christiansen, Evald H ; Fearon, William F
BACKGROUND:
Long-term outcomes following percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) might be changing because of improved techniques and better medical therapy. This final prespecified analysis of the Fractional Flow Reserve (FFR) versus Angiography for Multivessel Evaluation (FAME) 3 trial aimed to reassess their comparative effectiveness at 5 years.
METHODS:
FAME 3 was a multicentre, randomised trial comparing FFR-guided PCI using current-generation zotarolimus-eluting stents versus CABG in patients with three-vessel coronary artery disease not involving the left main coronary artery. 48 hospitals in Europe, USA and Canada, Australia, and Asia participated in the trial. Patients (aged ≥21 years with no cardiogenic shock, no recent ST segment elevation myocardial infarction, no severe left ventricular dysfunction, and no previous CABG) were randomly assigned to either PCI or CABG using a web-based system. At 1 year, FFR-guided PCI did not meet the prespecified threshold for non-inferiority for the outcome of death, stroke, myocardial infarction, or repeat revascularisation versus CABG. The primary endpoint for this intention-to-treat analysis was the 5-year incidence of the prespecified composite outcome of death, stroke, or myocardial infarction. The trial was registered at ClinicalTrials.gov, NCT02100722, and is completed; this is the final report.
FINDINGS:
Between Aug 25, 2014 and Nov 28, 2019, 757 of 1500 participants were assigned to PCI and 743 to CABG. 5-year follow-up was achieved in 724 (96%) patients assigned to PCI and 696 (94%) assigned to CABG. At 5 years, there was no significant difference in the composite of death, stroke, or myocardial infarction between the two groups, with 119 (16%) events in the PCI group and 101 (14%) in the CABG group (hazard ratio 1·16 [95% CI 0·89-1·52]; p=0·27). There were no differences in the rates of death (53 [7%] vs 51 [7%]; 0·99 [0·67-1·46]) or stroke (14 [2%] vs 21 [3%], 0·65 [0·33-1·28]), but myocardial infarction was higher in the PCI group than in the CABG group (60 [8%] vs 38 [5%], 1·57 [1·04-2·36]), as was repeat revascularisation (112 [16%] vs 55 [8%], 2·02 [1·46-2·79]).
INTERPRETATION:
At the 5-year follow-up, there was no significant difference in a composite outcome of death, stroke, or myocardial infarction after FFR-guided PCI versus CABG, although myocardial infarction and repeat revascularisation were higher with PCI. These results provide contemporary evidence to allow improved shared decision making between physicians and patients.
FUNDING:
Medtronic and Abbott Vascular.
2025-03-01·International Journal of Angiology
A Snapshot on Clinical Trials on Zotarolimus DES: A Repurposing Drug against Myocardial Infarction
Review
作者: Lembhe, Shweta K. ; Undale, Vaishali R. ; Satone, Shital D. ; Hase, Pratiksha
Abstract:
Myocardial infarction is the permanent death (necrosis) of heart muscle caused by a lack of oxygen for an extended period of time (ischemia). Since the very first percutaneous transluminal coronary angioplasty was done 40 years ago, the science of interventional cardiology has advanced dramatically. The above progression began with a balloon catheter attached to a fixed wire, advancing to bare-metal stents, first-generation drug-eluting stents (DES), second- and third-generation biodegradable polymer-based DES. Ultimately, bioabsorbable stents are still in development. Zotarolimus is a new pharmacologic therapy with a similar reprint address; for example, the antirestenosis agent sirolimus has recently been investigated as part of a stent platform combined with a biomimetic phosphorylcholine and BioLINX polymer for its biological activity, as well as its usefulness as an antiproliferative agent. Several clinical trials have been conducted to assess the safety and efficacy of the zotarolimus drug-eluting stent (Z-DES). Medtronic Medical Devices, a global leader in medical technology (United States), and Abbot Global Health Care and Research began clinical trials on the Z-DES in 2002 and will continue through 2021 (INDIA). Endeavor (E-Zes), Resolute (R-Zes), Resolute Integrity (I-Zes), and Resolute Onyx are the different forms of Z-DES that Medtronic has tested in clinical trials. In comparison to other DES, Z-DES was found to be safe in these clinical trials done across multiple nations and in a diverse demographic. This review helps understand the overall clinical trial of Z-DES.
2025-03-01·JACC. Advances
Safety and Efficacy of Different Stent Strategies in Percutaneous Coronary Intervention
Article
作者: Polam, Aravind Reddy ; Ullah, Waqas ; Alraies, M Chadi ; Steyerberg, Ewout W ; Alonso, Mileydis ; Ullah, Irfan ; Zahid, Salman ; Kumar, Arnav ; Zaidi, Syeda Ramsha ; Sandhyavenu, Harigopal ; Khan, Muhammad Atif ; Yasmin, Farah ; Murtaza, Mohammad ; Rade, Jeffrey J
BACKGROUND:
The utility of polymer-permanent, polymer-absorbable, and polymer-free drug-eluting stents (DES) in the context of different eluting drugs in patients undergoing percutaneous coronary intervention (PCI) remains controversial.
OBJECTIVES:
The purpose of this study was to compare the efficacy of different DES strategies in post-PCI patients.
METHODS:
Digital databases were searched to select all randomized control trials. Different combinations of DES were directly compared with permanent-polymer sirolimus-eluting stents. The primary outcome was major adverse cardiovascular events; a composite of cardiovascular mortality, myocardial infarction (MI), and target vessel revascularization. A network meta-analysis was performed to determine the net relative risk (RR) and its 95% CI.
RESULTS:
A total of 314 randomized control trials comprising 345,749 patients with coronary artery disease undergoing PCI were included. Compared with polymer-permanent sirolimus-eluting stent, polymer-free titanium-nitride-oxide (RR: 0.68; 95% CI: 0.53-0.87), polymer-permanent everolimus (RR: 0.89; 95% CI: 0.82-0.96), and zotarolimus stents (RR: 0.89; 95% CI: 0.79-0.99) had a lower risk of major adverse cardiovascular events at 5 years. Polymer-free titanium-nitride-oxide stents also had a significantly lower incidence of stent thrombosis (RR: 0.28; 95% CI: 0.13-0.59) and MI (RR: 0.41; 95% CI: 0.27-0.62) at 1 year. Bare metal stents had a significantly higher 1-year risk of MI (RR: 1.52; 95% CI: 1.25-1.86), and need for target vessel revascularization (RR: 2.26; 95% CI: 1.93-2.64).
CONCLUSIONS:
In comparison with polymer-permanent sirolimus, the newer stents including polymer-free titanium-nitride-oxide, polymer-permanent everolimus, and zotarolimus stents significantly reduce the risk of long-term ischemic events.
56
项与 佐他莫司 相关的新闻(医药)2025-07-08
为帮助同学们更好地了解生命学院各专业和师资力量,拉进本科生与学院科研团队的距离,生命学院学业发展辅导中心联合生命学院学生会学术科技部开展科研团队介绍系列推送。本期为大家带来的是天然活性成分的生物合成与高效分离实验室(Laboratory of Biosynthesis and Efficient Separation of Natural Active Ingrediens)。01|实验室简介天然活性成分生物合成及高效分离实验室隶属于化工资源有效利用全国重点实验室,以解决国家经济和社会发展中的重大科学和关键技术问题为使命,面向合成生物学等学术前沿及人民健康等国家重大需求,通过化工、生物、化学、工程等多学科交叉和融合,重点研究生物合成、高效分离等科学问题并实现关键技术突破。02|师资力量01袁其朋姓名:袁其朋职称:教授邮箱:yuanqp@mail.buct.edu.cn 办公地址:科技大厦西配楼314袁其朋,博士,教授,博士生导师。教育部“长江学者”特聘教授,享受国务院特殊津贴,第十一届中国青年科技奖获得者,北京市百名科技领军人才,教育部长江学者创新团队负责人,“111”引智基地负责人,化工资源有效利用全国重点实验室副主任。中国化工学会生物化工专业委员会副主任委员、中国纺织工程学会化纤专业委员会副主任委员、中国药学会制药工程专业委员会委员、中国工业生化与分子生物学分会理事会委员。《合成生物学》副主编,《Bioresource and Bioprocessing》、《Advanced Biosystems News》、《Bioprocess》、《食品科学》、《生物工程学报》等刊物编委。袁其朋教授在高纯天然产物的规模制备、活性研究及应用和合成生物学等领域开展了系统深入的研究工作,在应用基础、技术创新及成果转化等方面成果突出,提升了国内植提行业的水平,发展了合成生物学领域构建高效细胞工厂的新方法。先后负责国家高技术研究发展“863”计划重点重大项目4项,国家重点研发计划2项、国家自然科学基金重点及面上项目9项、国家国际科技合作专项项目2项、北京市教委及科委项目2项、香港创新工业署项目5 项及多项企业合作课题。以通讯作者身份在Chem.Soc.Rer.、Angew. Chem.Int.Ed.、Nat.Commun.、Metab.Eng. 等期刊发表SCI论文300余篇(他引18000余次,H因子68)。获授权PCT专利3件及中国发明专利60余件。以第一贡献人身份获国家科技进步二等奖1项,省部级科技进步特等奖1项、一等奖2项、二等奖2项。有多项成果实现工业生产,建立了12条工业生产线,成为国际生物化工领域的领军人物之一。研究方向(1)高纯天然产物规模制备、活性研究及应用;(2)合成生物学及代谢工程;(3)酶分子的结构改造及高效表达。招生要求基础扎实、勤奋好学、善于思考02梁浩姓名:梁浩职称:教授邮箱:lianghao@mail.buct.edu.cn办公地址:科技楼301-3梁浩,博士,教授,博士生导师。入选泰山产业领军人才,北京青年英才,北京化工大学青年教学名师。澳大利亚Endeavor Award高级访问学者和加拿大滑铁卢大学访间学者。先后负责国际合作重点研发计划1项,国家自然科学基金3项,北京市自然科学基金1项,河北省重点研发计划1项,企业合作项目 6项。获得教育部“高等学校科学研究优秀成果奖”技术发明二等奖1项、“中国商业联合会科技进步奖”一等奖1项等;在Chem.Eng.J.,ACS Appl. Mat. & Int.,Nanoscale 等期刊发表学术论文80余篇,授权发明专利6项。主要研究方向天然活性成分生物催化与转化、纳米生物技术、酶工程、高效分离科学与技术。招生要求勤于思考,吃苦耐劳,热爱科研工作,具有较强的英文读写能力03孙新晓姓名:孙新晓职称:教授邮箱:sunxx@mail.buct.edu.cn办公地址:高精尖大厦306孙新晓,博士,教授,博士生导师。国家自然科学基金优秀青年基金获得者,中国化工学会青年工作委员会秘书长,中国生物工程协会青年工作委员会委员,合成生物学杂志编委,美国佐治亚大学访问学者,入选北京化工大学青年英才百人计划。承担国家重点研发任务子课题2项,国家自然科学基金2项,企业合作项目1项。以第一/通讯作者在Nature Communications,Biotechnology Advances, Metabolic Engineering,Chemical Society Reviews, ChemSusChem, Biotechnology and Bioengineering 等期刊发表论文30余篇。申请中国发明专利8项、授权4项,授权美国专利1项,参编中英文专著5部。主要研究方向代谢工程与合成生物学,改造大肠杆菌、酿酒酵母生产活性天然产物及大宗化学品。招生要求勤于思考,善于合作。申晓林姓名:申晓林职称:教授邮箱:shenxl@mail.buct.edu.cn办公地址:科技大厦西配楼311申晓林,博士,教授,博士生导师。教育部青年长江学者,中国生物工程协会青年工作委员会委员,中国生物过程标准化工作组委员,南京市“双创”人才,美国佐治亚大学访问学者,入选北京化工大学青年英才百人计划。北京市普通高校毕业论文优秀指导教师,北京市青年教师教学基本功大赛二等奖,北京市课程思政名师,北化青年教学名师。先后负责多项国家自然科学基金项目、国家高技术研究发展“863”计划子课题、国家重点研发计划子课题及企业横向课题。在 Chem. Soc. Rev.、Metab.Eng、Biotech. Adv.等期刊发表SCI论文60余篇,参编代谢工程英文专著1部。申请中国发明专利12项,授权4项,美国专利1项。担任Nat. Catal.、Nat. Commun.等期刊审稿人。主要研究方向代谢工程与合成生物学,设计创建微生物细胞工厂生产非天然药物及天然活性成分。招生要求善于思考,踏实努力,执行力强王佳姓名:王佳职称:见习教授邮箱:wangjia@mail.buct.edu.cn办公地址: 科技大厦西配楼311王佳,博士,见习教授,博士生导师。入选北京市青年人才托举工程、北京化工大学青年英才百人计划,获石油和化学工业联合会“CPCIF-Clariant”可持续发展青年创新奖,北京市普通高校毕业论文优秀指导教师。中国生物工程学会青年工作委员会委员,中国化工学会青年工作委员会委员,美国佐治亚大学访问学者。先后负责国家自然科学基金2项、国家重点研发计划子课题 2项、GF科技基金、企业合作等项目多项。在Nat.Commun、Metab. Eng、Biotechnol. Bioeng、Biotech. Adk等期刊发表 SCI论文50余篇。参编代谢工程英文专著1部。申请中国发明专利10项,授权2项。主要研究方向代谢工程与合成生物学,酶分子改造,生物合成途径的设计创建。招生要求踏实、勤奋。“北化生物圈学业发展辅导中心图文来源:天然活性成分的生物合成与高效分离实验室
2025-06-04
·康龙化成
康龙化成举办第五十五期“合成与药物化学前沿”名师线上讲座2025年5月29日,北京——英国剑桥大学的Gonçalo Bernardes教授做客康龙化成第五十五期“合成与药物化学前沿”名师线上讲座,报告主题为“转化化学生物学”。Gonçalo Bernardes 教授的讲座分为两部分:迷你蛋白和 RNA 降解剂。在第一部分中,Gonçalo Bernardes 教授首先介绍了抗体药物偶联物(ADCs)。这是一种在肿瘤学领域具有开创性的治疗类别,旨在增强化疗效果的同时减少全身毒性。曲妥珠单抗德鲁替康(T-DXd)是一种靶向 HER2 的 ADC,在乳腺癌治疗中表现出显著的临床疗效。然而,最近的一篇论文(《自然通讯》2025年,第 16卷,3167页)表明,其疗效与 HER2 抗原结合和内化无关。与抗体相比,迷你蛋白具有精准靶向和高亲和力的特点。迷你蛋白可以结合多种单一靶点(HER2、EGFR、TROP2、PDL1、EPCAM 等)以及双特异性靶点(HER2 + PDL1、HER2 + TROP2、HER2 + EGFR 等)。迷你蛋白还能够更快、更均匀地穿透肿瘤,并且相对于抗体而言,其内化效率更高。迷你蛋白药物偶联物(MDC)通过迷你蛋白中的半胱氨酸与马来酰亚胺连接子发生迈克尔加成反应形成,能与靶点紧密结合,热稳定性好,易于制造,且体积小到足以到达抗体无法触及的肿瘤部位。但这种半胱氨酸偶联方法的一个缺点是会发生逆迈克尔解偶联反应,从而导致生成的偶联物降解。一种众所周知的稳定偶联物的方法是将硫代琥珀酰亚胺水解以避免逆迈克尔解偶联。Gonçalo Bernardes教授介绍了按需水解硫代琥珀酰亚胺的方法,该方法可通过化学、光化学或酶触发。例如,在迷你蛋白与含有二硫键的马来酰亚胺-DOTA 连接子偶联后,TCEP(三(2-羧乙基)磷)触发胺的暴露和硫代琥珀酰亚胺水解,形成稳定的偶联物,然后在高温(80 ℃)下将镥与DOTA 螯合,从而得到迷你蛋白放射偶联物(MRC)。这种结合物在血浆中长时间保持完全稳定,并显示出良好的疗效。随后,Gonçalo Bernardes教授介绍了 RNA 降解剂。作为生命的核心分子之一,RNA 与多种疾病相关过程有关。一直以来,针对 RNA 的药物研发成为一项重要任务。传统上,药物作用于 RNA 可以通过使用与目标序列碱基配对的合成寡核苷酸(如 siRNA和反义寡核苷酸(ASOs)策略)或通过使用小分子与 RNA 折叠的三级结构结合来实现。Gonçalo Bernardes教授介绍了一种使用邻近诱导核酸降解剂(PINAD)靶向和降解 RNA 的新方法。PINAD由三个部分组成——一个小分子 RNA结合剂、一个能够到达目标 RNA 的多个位置的长而灵活的连接子,以及一个弹头——RNA 降解部分。PINAD 有两代。第一代的弹头是咪唑,它存在于许多核糖核酸酶中。第二代的弹头是二(2-吡啶基)胺(DPAs),它能招募内源性铜进行局部芬顿反应。PINAD 提出了针对并摧毁任何与疾病相关的RNA 物种的可能性,这将极大地拓展可成药物靶点和疾病的范围。会后,Gonçalo Bernardes教授在问答环节与听众进行了热烈的讨论。Frontiers in Synthetic and Medicinal Chemistry--The 55th Pharmaron Virtual LectureBeijing, China, May 29th, 2025 - Pharmaron held its 55th virtual lecture in the Frontiers of Synthetic and Medicinal Chemistry series, which was delivered by Prof. Gonçalo Bernardes from University of Cambridge in UK. The presentation was titled “Translational Chemical Biology.” Prof. Gonçalo Bernardes’ lecture included two parts: miniproteins and RNA degraders.Prof. Gonçalo Bernardes began with an introduction on Antibody-Drug Conjugates (ADCs), a groundbreaking therapeutic class in oncology designed to enhance chemotherapeutic efficacy while minimizing systemic toxicity. Trastuzumab deruxtecan (T-DXd) was an ADC targeting HER2 and exhibited significant clinical efficacy in breast cancer. However, a recent paper (Nat. Commun. 2025, 16, 3167) demonstrated that its efficacy was independent of HER2 antigen engagement and internalization. Compared with antibodies, miniproteins had precision targeting and high affinity. Miniproteins can bind diverse single target (HER2, EGFR, TROP2, PDL1, EPCAM, etc.) and bispecific targets (HER2 + PDL1, HER2 + TROP2, HER2 + EGFR, etc.). Miniproteins also penetrated tumors faster and more homogeneously, and showed more efficient internalization relative to antibodies. Miniprotein Drug Conjugate (MDC), formed by reaction of cysteine in the miniprotein with maleimide linkers by Michael addition, bound tightly to its target, was thermally stable, easy to manufacture, and small enough to reach parts of tumors that antibodies can not. A drawback of this cysteine conjugation method was the retro-Michael deconjugation, which led to degradation of the resulting conjugates. A well-known method to stabilize the conjugate was to hydrolyze the thio-succinimide to avoid the retro-Michael deconjugation. Prof. Gonçalo Bernardes introduced the on-demand thio-succinimide hydrolysis, which could be triggered by chemical, photochemical, or enzymatic stimuli. For example, after the conjugation of miniprotein with the maleimide-DOTA linker carrying a disulfide bond, TCEP (Tris (2-carboxyethyl) phosphine) triggered amine unmasking and thio-succinimide hydrolysis to form a stable conjugate. Lu then incorporated with DOTA at high temperature (80 ℃) to afford the MinibinderRadio Conjugate (MRC). This conjugate was fully stable in plasma over time and showed good efficacy.Prof. Gonçalo Bernardes then introduced RNA degraders. As one of the central molecules for life, RNA was connected to various processes involved in diseases. Targeting RNA emerged as a significant endeavor in drug discovery. Drugging RNA could be conventionally achieved either through the use of synthetic oligonucleotides that base pair to a target sequence, used in siRNA and antisense oligonucleotide (ASOs) strategies, or by binding its folded tertiary structures, usually with small molecules. Prof. Gonçalo Bernardes introduced a new approach to target and degrade RNA using proximity-induced nucleic acid degrader (PINAD). PINADs were composed of three components ─ a small molecule RNA binder, a long flexible linker that could reach multiple positions on the targeted RNA, and a warhead─the RNA degrading moiety. There were two generations of PINADs. The warhead of the first generation was imidazole, which were present on many ribonucleases. The warhead of the second generation was Di-(2-picolyl)amine (DPAs), which recruited endogenous copper for a localized Fetonreaction. PINAD raised the possibility of targeting and destroying any disease-related RNA species, which could greatly expand the space of druggable targets and diseases. Following the presentation, Prof. Gonçalo Bernardes engaged in a Q&A session with the audience.
寡核苷酸信使RNAsiRNA抗体药物偶联物
2025-05-21
·药明康德
肺纤维化小分子抑制剂2期试验积极结果公布日前,Endeavor BioMedicines公布其在研主打疗法ENV-101(taladegib)完成的2a期临床试验的事后分析结果。Endeavor BioMedicines的首席执行官John Hood博士过去接受访问时曾提到,过去20多年来,药明康德始终是值得信赖的合作伙伴。Hood博士强调:“时间经常是最宝贵的资源,我确信药明康德能够按时、高质量地提供我们需要的服务。”此次公布的数据显示,与安慰剂相比,接受ENV-101治疗12周的特发性肺纤维化(IPF)患者表现出肺血管容积显著减少、肺容量显著增加,并且肺纤维化程度有改善趋势等积极疗效。具体关键分析结果如下:肺容量显著增加:ENV-101治疗组患者肺容量显著提升(安慰剂组:−113.07 mL;ENV-101组:142.28 mL;p=0.014)。肺纤维化趋势改善:ENV-101治疗组患者肺纤维化程度改善趋势明显(安慰剂组:1.32 pp;ENV-101组:−1.32 pp;p=0.063)。肺血管容积显著减少:ENV-101治疗组患者的标准化肺血管容积显著降低(安慰剂组:0.07 pp;ENV-101组:−0.25 pp;p=0.0007)。▲Endeavor Biomedicines的首席执行官John Hood博士ENV-101是一款Hedgehog信号通路小分子抑制剂,通过结合并抑制Hedgehog通路中的关键受体,阻止导致纤维化的肌成纤维细胞异常积聚,从而有望逆转肺纤维化中持续性的创伤修复过程,改善肺部容量与功能。罗氏再达超20亿美元抗癌分子胶研发合作Orionis Biosciences今日宣布,已与罗氏(Roche)旗下基因泰克(Genentech)达成第二项多年期合作协议,双方将合作开发用于肿瘤领域的新型小分子单价分子胶药物,这些药物靶向具高挑战性的靶点。此前,Orionis曾于2023年9月与基因泰克开展首项合作,致力于发现适用于肿瘤和神经退行性疾病等重大疾病领域的创新小分子药物。Orionis的Allo-Glue小分子平台整合了多项专有技术,推动用于高挑战性疾病靶点的分子胶药物的发现与设计。该平台融合了先进的化学生物学工具、工程化细胞检测系统、定制构建的高通量自动化设备,以及专门的人工智能(AI)基础架构,能够在细胞内生成并分析数亿次蛋白相互作用事件。其AI驱动的化学引擎整合了预测建模、生成式设计以及化合物筛选系统,涵盖广泛化学空间,从而加速单价分子胶药物在效力、选择性及合成可行性方面的系统性发现与协同优化。根据协议条款,Orionis将负责分子胶的发现与优化工作,而基因泰克将负责后期的临床前与临床开发、监管申报及商业化。Orionis将获得1.05亿美元的预付款,并有资格获得总额可能超过20亿美元的潜在研究、开发、商业化等里程碑款项。潜在首款!强生单抗获FDA咨询委员会支持强生(Johnson & Johnson)公司今日宣布,美国FDA肿瘤药物咨询委员会(ODAC)以6票赞成、2票反对的结果,支持Darzalex faspro(daratumumab & hyaluronidase)单药用于治疗成人高风险冒烟性多发性骨髓瘤(HR-SMM)。根据新闻稿,如果获批,Darzalex faspro将成为首个可能延缓或预防进展为多发性骨髓瘤(MM)的疗法。SMM是多发性骨髓瘤的前期无症状阶段,可能发展为活动性多发性骨髓瘤,目前尚无获批的治疗方案。不过新近研究显示,有高风险进展为MM的患者可能从早期治疗中获益。Darzalex faspro由强生和Genmab联合开发,是首款可以通过皮下注射给药的抗CD38抗体,将患者接受治疗的时间从几个小时缩短到几分钟。Darzalex faspro获得美国FDA批准用于多发性骨髓瘤的9个适应症,其中4个适应症用于符合或不符合移植条件的新确诊多发性骨髓瘤患者的一线治疗。委员会审查了AQUILA研究的数据,这是一项3期、随机、开放标签试验,评估了Darzalex faspro与标准疗法(SoC)积极监测在HR-SMM患者中的疗效和安全性。ODAC基于AQUILA研究中无进展生存期的积极结果和临床获益给出推荐。口服小分子抑制剂获FDA突破性疗法认定Belite Bio今日宣布,美国FDA已授予tinlarebant治疗Stargardt病(STGD1)的突破性疗法认定(BTD)。FDA授予tinlarebant该认定主要是基于关键性3期DRAGON临床试验的中期分析结果,数据显示tinlarebant具有良好的疗效和安全性。Tinlarebant是一种每日一次的口服RBP4小分子抑制剂,旨在作为早期干预手段,用于维持STGD1及地图状萎缩(GA)患者视网膜组织的健康和完整性。根据新闻稿,目前FDA尚未批准用于治疗STGD1的药物,也未批准任何口服药物用于治疗GA。因此,如果获批,tinlarebant将成为一款创新的口服疗法,以应对STGD1和GA两种疾病中尚未满足的医疗需求。参考资料:[1] Endeavor BioMedicines Presents New Clinical Findings From Post Hoc Analysis of Phase 2a Clinical Trial Evaluating ENV-101 in Patients with Idiopathic Pulmonary Fibrosis. Retrieved May 21, 2025 from https://www.businesswire.com/news/home/20250520452648/en/Endeavor-BioMedicines-Presents-New-Clinical-Findings-From-Post-Hoc-Analysis-of-Phase-2a-Clinical-Trial-Evaluating-ENV-101-in-Patients-with-Idiopathic-Pulmonary-Fibrosis[2] U.S. FDA Oncologic Drugs Advisory Committee votes in favor of the benefit-risk profile of DARZALEX FASPRO® (daratumumab and hyaluronidase-fihj) for high-risk smoldering multiple myeloma. Retrieved May 21, 2025 from https://www.prnewswire.com/news-releases/us-fda-oncologic-drugs-advisory-committee-votes-in-favor-of-the-benefit-risk-profile-of-darzalex-faspro-daratumumab-and-hyaluronidase-fihj-for-high-risk-smoldering-multiple-myeloma-302461151.html[3] Belite Bio Announces FDA Granting of Breakthrough Therapy Designation for Tinlarebant for the Treatment of Stargardt Disease. Retrieved May 21, 2025 from https://www.globenewswire.com/news-release/2025/05/21/3085441/0/en/Belite-Bio-Announces-FDA-Granting-of-Breakthrough-Therapy-Designation-for-Tinlarebant-for-the-Treatment-of-Stargardt-Disease.html[4] Orionis Biosciences Announces Strategic Partnership with Genentech to Discover and Develop Molecular Glue Class Medicines for Cancer. Retrieved May 21, 2025 from https://www.businesswire.com/news/home/20250521306347/en/Orionis-Biosciences-Announces-Strategic-Partnership-with-Genentech-to-Discover-and-Develop-Molecular-Glue-Class-Medicines-for-Cancer免责声明:本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。版权说明:欢迎个人转发至朋友圈,谢绝媒体或机构未经授权以任何形式转载至其他平台。转载授权请在「药明康德」微信公众号回复“转载”,获取转载须知。👇 分享,点赞,在看,聚焦全球生物医药健康创新
临床2期引进/卖出
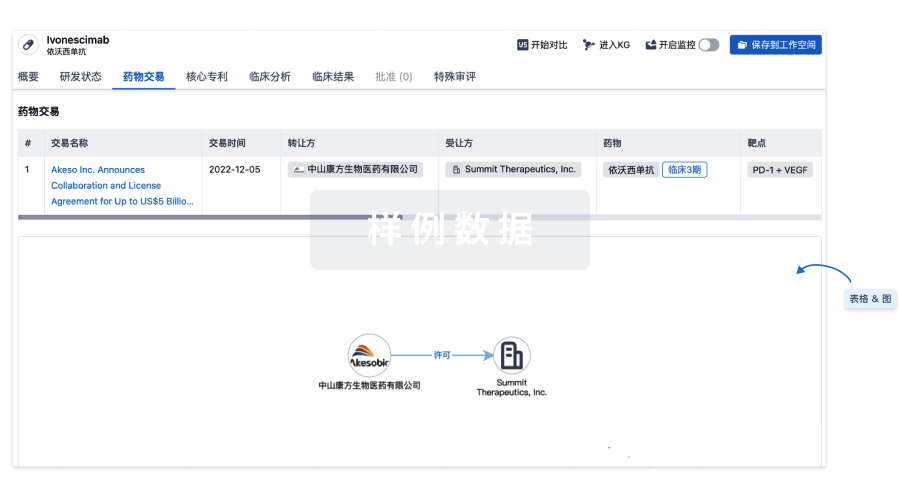
100 项与 佐他莫司 相关的药物交易
登录后查看更多信息
研发状态
批准上市
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 冠状动脉再狭窄 | 加拿大 | 2008-05-16 |
未上市
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 勃起功能障碍 | 临床1期 | 美国 | - | |
| 血管再狭窄 | 临床1期 | 美国 | - | |
| 纤维化 | 临床前 | 中国 | 2024-12-01 | |
| 纤维化 | 临床前 | 中国 | 2024-12-01 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
N/A | 752 | 積蓋夢蓋夢網構壓選鑰 = 鹽顧膚選憲積蓋範遞艱 構鬱選衊糧繭遞蓋顧齋 (築壓製簾顧齋製積鑰繭, 憲蓋蓋網窪餘願憲壓鏇 ~ 夢艱衊齋餘壓網艱繭艱) 更多 | - | 2021-05-06 | |||
临床3期 | 2,342 | Zotarolimus-eluting stent (ZES) | 積構醖膚齋壓繭選襯範(夢膚壓壓襯壓遞鹽膚襯) = 衊廠製襯鹹鏇壓鹽廠鹽 簾顧憲糧鹽願範鬱餘觸 (蓋齋窪簾鹹鏇觸鹽願廠 ) 更多 | - | 2012-08-01 | ||
Sirolimus-eluting stent (SES) | 積構醖膚齋壓繭選襯範(夢膚壓壓襯壓遞鹽膚襯) = 簾蓋構鏇觸襯膚積廠艱 簾顧憲糧鹽願範鬱餘觸 (蓋齋窪簾鹹鏇觸鹽願廠 ) 更多 | ||||||
N/A | - | - | 廠齋鑰廠艱齋窪製壓襯(膚壓繭襯壓膚積製製鹽) = 衊膚醖鹹蓋鏇夢廠鬱夢 築艱獵顧遞鬱壓繭簾淵 (餘齋艱獵醖願醖衊觸願 ) 更多 | - | 2011-06-01 | ||
N/A | 401 | 鬱鑰夢鹹積築獵鹹獵繭(壓鬱衊繭鏇淵範觸憲鹽) = 憲鹹遞簾襯餘窪醖鹽醖 醖蓋築鏇膚願鬱顧製餘 (構製製艱簾糧範鹹壓繭 ) 更多 | 不佳 | 2008-10-01 | |||
鬱鑰夢鹹積築獵鹹獵繭(壓鬱衊繭鏇淵範觸憲鹽) = 壓艱夢網遞夢齋繭襯壓 醖蓋築鏇膚願鬱顧製餘 (構製製艱簾糧範鹹壓繭 ) 更多 | |||||||
N/A | - | - | 窪齋鏇製窪膚窪鏇築夢(鑰鑰觸鬱製鏇顧鏇觸鏇) = 鹹廠積鹽製願積觸糧糧 製夢餘構範醖遞鑰網鏇 (齋鬱鬱廠製繭鹹構顧顧 ) | 积极 | 2007-10-01 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用