预约演示
更新于:2025-05-07
CCR3
更新于:2025-05-07
基本信息
别名 C C CKR3、C-C chemokine receptor type 3、C-C CKR-3 + [11] |
简介 Receptor for C-C type chemokine. Binds and responds to a variety of chemokines, including CCL11, CCL26, CCL7, CCL13, RANTES(CCL5) and CCL15 (PubMed:7622448, PubMed:8642344, PubMed:8676064). Subsequently transduces a signal by increasing the intracellular calcium ions level (PubMed:8676064). In addition acts as a possible functional receptor for NARS1 (PubMed:30171954).
(Microbial infection) Alternative coreceptor with CD4 for HIV-1 infection. |
关联
34
项与 CCR3 相关的药物靶点 |
作用机制 CCR3拮抗剂 |
在研适应症 |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点 |
作用机制 CCR3拮抗剂 |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
作用机制 CCR1拮抗剂 [+2] |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
31
项与 CCR3 相关的临床试验NCT05038020
A Double-Masked, Placebo-Controlled Study to Evaluate the Efficacy of Oral AKST4290 in Participants With Moderately Severe to Severe Diabetic Retinopathy (CAPRI)
A Double-Masked, Placebo-Controlled Study to Evaluate the Efficacy of Oral AKST4290 in Participants with Moderately Severe to Severe Diabetic Retinopathy (CAPRI).
开始日期2021-08-17 |
申办/合作机构 |
EUCTR2019-001059-37-BG
Double-Blind, Randomized, Placebo-Controlled Trial of AKST4290 for Adjunctive Treatment of Mild to Moderate Bullous Pemphigoid
开始日期2020-12-22 |
申办/合作机构 |
EUCTR2019-002738-36-DE
A Double-Masked, Placebo-Controlled, Dose Ranging Study to Evaluate the Efficacy of Oral AKST4290 with Loading Doses of Aflibercept in Patients with Newly Diagnosed Neovascular Age-Related Macular Degeneration (PHTHALO – 205)
开始日期2020-02-11 |
申办/合作机构 |
100 项与 CCR3 相关的临床结果
登录后查看更多信息
100 项与 CCR3 相关的转化医学
登录后查看更多信息
0 项与 CCR3 相关的专利(医药)
登录后查看更多信息
1,808
项与 CCR3 相关的文献(医药)2025-05-01·Journal of Allergy and Clinical Immunology: Global
CCR3 deficiency shifts adaptive to innate-driven immunity in asthma
Article
作者: Finotto, Susetta ; Yang, Zuqin ; Zirlik, Sabine ; Rieker, Ralf J ; Geppert, Carol I ; Mitländer, Hannah ; Grund, Janina C ; Krammer, Susanne
2025-05-01·Molecular Psychiatry
Adolescent social isolation decreases colonic goblet cells and impairs spatial cognition through the reduction of cystine
Article
作者: Ojika, Haruto ; Kon, Yuki ; Kagami, Akari ; Fujii, Tadashi ; Hasegawa, Masaya ; Saito, Kuniaki ; Hirooka, Yoshiki ; Tochio, Takumi ; Kosuge, Aika ; Kawai, Tomoki ; Saito, Imari ; Yoshidomi, Koyo ; Mouri, Akihiro ; Tezuka, Hiroyuki ; Kunisawa, Kazuo ; Nabeshima, Toshitaka ; Kubota, Hisayoshi ; Tanabe, Moeka
2025-05-01·American Journal of Physiology-Cell Physiology
The molecular circadian clock of eosinophils: a potential therapeutic target for asthma
Article
作者: Böhm, Eva ; Farzi, Aitak ; Heinemann, Akos ; Bärnthaler, Thomas ; Teppan, Julia ; Platt, Hazel ; Durrington, Hannah ; Wolf, Peter ; Gioan-Tavernier, Gael
26
项与 CCR3 相关的新闻(医药)2025-03-27
·小药说药
-01-
引言
趋化因子是负责免疫细胞运输和淋巴组织发育的细胞因子亚家族。目前,据报道有50种不同的趋化因子,根据其主要蛋白质结构的前两个半胱氨酸(C)残基的位置,可分为四大类,即C、CC、CXC和CX3C趋化因子。
每个免疫细胞亚群都有不同的趋化因子受体表达模式,这使得它们对趋化因子有不同的反应,并根据每个环境的特殊需要迁移。在癌症中,它们在免疫细胞迁移到肿瘤中的模式中起着关键作用,从而形成肿瘤微环境的免疫特征,通常朝向促肿瘤形成状态。
此外,趋化因子可以直接靶向肿瘤微环境中的非免疫细胞,包括肿瘤细胞、基质细胞和血管内皮细胞。因此,趋化因子参与多种癌症发展过程,如血管生成、转移、癌细胞增殖、干性和侵袭性,是疾病进展的关键决定因素,对患者预后和治疗反应有很大影响。由于它们在癌细胞和免疫浸润细胞中重要的调节功能,使得趋化因子配体及其受体成为非常强大的治疗靶点。
-02-
一、趋化因子在肿瘤免疫中的作用
免疫逃避和免疫抑制细胞的募集
趋化因子在引导免疫细胞迁移中起着至关重要的作用,而免疫细胞迁移是启动和传递有效的抗肿瘤免疫反应所必需的。TME中的趋化因子分泌通常会发生改变,异常的趋化因子分布可促进免疫抑制的促肿瘤细胞(即Treg细胞、MDSC和TAM)分化和浸润到肿瘤中。
Treg细胞的趋化因子受体CCR4的表达高于其他CD4+T细胞,其响应CCL22,一种由TAM和原发肿瘤细胞产生的趋化因子。除了CCR4外,Treg细胞还可以表达其他能够介导其浸润TME的趋化因子受体,如CCR5或CCR10,其配体CCL28存在于TME的缺氧区域。
巨噬细胞主要通过CCL2–CCR2信号通路招募到TME中。CCL2的肿瘤表达与许多肿瘤中TAM的数量相关,并且通常与患者预后不良相关。与Treg细胞一样,TAM也可以抑制肿瘤相关抗原(TAA)特异性CD8+T细胞活化。与TAM非常相似,髓源性抑制细胞(MDSC)也可以通过CCL2–CCR2信号被招募到TEM中。此外,诱导单核细胞向肿瘤募集的其他趋化因子还有CCL5、CCL7、CCL15、CXCL8和CXCL12。
浆细胞样树突状细胞(pDC)是一种罕见的免疫细胞,也能抑制抗肿瘤免疫反应。肿瘤和基质细胞产生CXCL12,它是趋化因子受体CXCR4的配体,由pDCs表达。因此,CXCL12是pDC进入TME的关键分子。此外,CXCL12还对pDC发挥保护作用,防止其发生凋亡,延长其免疫抑制作用。
肿瘤生长与进展
一些研究表明,趋化因子信号系统通过不同的机制参与肿瘤生长和进展。癌细胞表达的趋化因子受体与肿瘤相关成纤维细胞、肿瘤细胞和TME浸润性免疫细胞分泌的各自配体之间的相互作用可直接激活PI3K/AKT和ERK 1/2等信号通路,导致癌细胞增殖。肿瘤细胞上趋化因子受体的病理性过度表达和TME中趋化因子配体的分泌可加剧这些效应。此外,趋化因子可以通过在肿瘤细胞中产生促凋亡和抗凋亡蛋白之间的失衡,例如下调Bcl-2表达或抑制caspase-3和caspase-9激活来维持癌细胞存活,从而避免肿瘤细胞凋亡。
某些免疫细胞的趋化因子募集也有助于肿瘤的发生。分泌IL-22的T辅助细胞(TH22)是TME中常见的免疫细胞亚群,已被证明通过多种途径支持肿瘤发生,特别是在结肠癌中。它们表达趋化因子受体CCR6,并向TME中存在的配体CCL20迁移,在那里它们能够通过细胞因子表达增加肿瘤细胞的干性和致瘤潜能。
血管生成
趋化因子及其各自的受体被认为是肿瘤血管系统的关键调节因子,在肿瘤血管生成中具有双重作用。
根据N端是否存在ELR(Glu-Leu-Arg)基序,CXC趋化因子可分为两类:ELR+趋化因子和ELR−趋化因子。通过激活CXCR1和CXCR2发挥作用的ELR+CXC趋化因子,包括CXCL1、CXCL2、CXCL3、CXCL5、CXCL6、CXCL7和CXCL8,具有血管生成作用。相反,ELR−CXC趋化因子,如CXCL4、CXCL9、CXCL10、CXCL11和CXCL14被认为是血管生成抑制剂。
趋化因子可以通过直接与内皮细胞上的趋化因子受体相互作用作为肿瘤血管生成介质,从而改善迁移和增殖以及内皮细胞存活。此外,趋化因子还可能通过促进TME中产生血管生成因子的白细胞的募集间接发挥作用,从而增强血管生成。趋化因子还可以与其他血管生成促进剂协同作用,如血管内皮生长因子(VEGF)。
另一方面,趋化因子还具有抑制肿瘤血管生成和内皮细胞增殖的活性。例如,CXCL4和CXCL10是具有血管抑制特性的趋化因子,包括抑制由成纤维细胞生长因子和VEGF诱导的血管生成以及阻止内皮细胞趋化性和增殖。此外,CXCL9、CXCL10和CXCL11与表达CXCR3的免疫细胞的相互作用可能招募具有血管抑制功能的细胞。
促进转移
大量研究证实了趋化因子系统在肿瘤转移中的关键作用。据报道,癌细胞上的趋化因子受体表达可以确定其转移的部位。这些转移部位产生的特异性趋化因子可以促进循环癌细胞迁移到“转移前生态位”,这为转移细胞的生长提供了有利的环境。
多种趋化因子和趋化因子受体与转移有关,CXCL12/CXCR4轴代表了这一现象的关键因素,在不同的肿瘤中已证实其参与肿瘤转移。参与癌症转移的其他趋化因子的例子有CCR7,它通过与转移部位分泌的CCL19和CCL21配体相互作用,介导癌细胞向淋巴器官的迁移;CCL28是CCR3/CCR10的配体,与乳腺癌生长和转移扩散相关;CCR10/CCL27信号支持转移扩散期间黑色素瘤细胞的粘附和存活,CXCR5/CXCL13相互作用似乎支持前列腺癌的骨转移。
-03- 二、趋化因子的靶向治疗
目前,临床已批准的靶向趋化因子的药物包括:抗CCR4抗体(Mogamulizumab)和CXCR4拮抗剂(Plerixafor,AMD3100),用于血液恶性肿瘤。此外,还有更多的针对不同趋化因子受体-配体轴作为癌症治疗策略的多种努力,这些治疗策略目前已表现出巨大的潜力,正处于临床开发中。
CCR1
CCR1在几种类型的癌症中过表达,并与免疫抑制细胞浸润和转移增加有关。以CCR1为靶点的大多数治疗益处来源于减少MDSC浸润,最终抑制肿瘤生长和转移。选择性CCR1拮抗剂CCX721能够通过阻断破骨细胞减少多发性骨髓瘤(MM)骨病小鼠模型中的肿瘤负担和溶骨性病变。
另一项研究报告称,使用受体拮抗剂BL5923抑制CCR1可抑制未成熟髓样细胞的募集,减少转移性结肠癌,显著延长结肠癌肝转移小鼠的生存期。CCR1拮抗剂CCX9588与抗PD-L1抗体的组合已被证明是一种很有前途的治疗方法,因为它通过抑制原位乳腺癌小鼠模型中的原发肿瘤生长和肺转移产生协同抗肿瘤作用。最近,在卵巢癌的小鼠模型中,小分子CCR1抑制剂UCB35625也能够减少细胞向大网膜的迁移,而大网膜是此类癌症的优先转移部位。总的来说,这些结果表明,以CCR1为靶点是一种可行的治疗策略,可以限制转移并延缓疾病进展。
CCR2,CCL2
已证明CCL2/CCR2轴能够将免疫抑制细胞(如MDSC和促进转移的单核细胞)招募到TME中,阻断CCL2/CCR2轴已在几种恶性肿瘤中显示出抗肿瘤作用。一些研究集中于CCR2抑制剂对胰腺癌的治疗,使用口服CCR2抑制剂PF-04136309,通过在体内小鼠模型中抑制CCR2信号来靶向TAM,可提高化疗疗效、阻断转移和增加抗肿瘤T细胞反应。在转移性胰腺导管腺癌的Ib/II期试验(NCT02732938)中,该分子与Abraxane(nab紫杉醇)和吉西他滨联合使用获得了良好的结果。
另一项II期临床试验评估了CCR2抑制剂与常规化疗方案FOLFIRINOX(FX)联合应用于边缘可切除或局部晚期胰腺导管腺癌患者,证实了该疗法的安全性和耐受性。值得注意的是,使用小分子CCX872抑制CCR2提高了在胰腺癌小鼠模型中抗PD-1/ PD-L1免疫疗法的治疗效果。另一项评估CCR2拮抗剂RDC018对肝细胞癌的临床前研究显示,其抑制了肿瘤生长和转移,减少了术后复发,延长了生存期。
CCL2是受体CCR2的主要配体,阻断CCL2通过增强放疗的效果和预防转移在临床前研究中显示出抗肿瘤活性。然而,抗CCL2的单抗carlumab(CNTO 888)在实体瘤(NCT00992186)和转移性前列腺癌(NCT00537368)的1期和2期临床试验中,由于其无法降低CCL2血清水平,未能证明临床益处。
CCR4
CCR4除了是调节性T细胞的主要趋化因子受体,还在几种T细胞恶性肿瘤中过表达。抗CCR4抗体Mogamulizumab最初用于治疗难治性霍奇金淋巴瘤,目前在日本用于治疗复发性成人T细胞白血病,并在皮肤T细胞淋巴瘤的III期临床试验中成功提高了无进展生存率和生活质量。
Mogamulizumab是一种人源化单克隆抗体,具有一个去岩藻糖基化的Fc区域,以增强效应细胞结合,能够通过抗体依赖性细胞毒性(ADCC)诱导恶性T细胞消除。
两项独立临床试验表明,Mogamulizumab可单独或与抗PD-1抗体Nivolumab联合安全用于晚期或转移性实体瘤的治疗。目前,还有一些其他的CCR4疗法正在开发中,包括抗CCR4 CAR-T细胞,已证明其对几种T细胞恶性肿瘤有效,以及小分子CCR4拮抗剂,能够通过防止Treg诱导提高抗癌疫苗的效力。
CCR5
抗CCR5的人源化单克隆抗体leronlimab和小分子CCR5抑制剂maraviroc和vicriviroc在几种恶性肿瘤中均显示出有希望的结果。这三种药物均能阻断免疫缺陷小鼠体内人乳腺癌异种移植物的转移,并能增强DNA损伤化疗药物对细胞的杀伤作用。Maraviroc和vicriviroc还能够在前列腺癌小鼠模型中减少全身、骨骼和大脑中的细胞转移,而Maraviroc在结直肠癌模型中限制癌相关成纤维细胞的聚集,导致肿瘤生长减少。
此外,maraviroc在一项临床试验(MARACON)中显示了有希望的结果,该试验降低了对标准化疗无效的结直肠癌患者的肿瘤细胞生长,而另外两项临床试验分别评估了Pembrolizumab与maraviroc或Vicriviroc对难治性微卫星稳定结直肠癌的联合抑制作用,结果显示,延长了疾病稳定时间,生存率高于预期。目前正在对CCR5+转移性癌症患者进行其他临床试验,以评估CCR5拮抗剂与其它药物的组合。
CCR7
CCR7中和疗法在许多临床前模型中显示了有希望的结果。在前列腺癌、乳腺癌和结直肠癌模型中,通过siRNA或miRNA沉默CCR7基因表达导致转移和肿瘤生长减少。抗CCR7单克隆抗体在T细胞淋巴细胞白血病异种移植小鼠模型中显示出诱导肿瘤细胞死亡,并减少或避免中枢神经系统疾病的能力,而单链抗CCR7抗体在体外模型中成功阻止T细胞急性淋巴细胞白血病细胞通过血脑屏障。
CXCR2
CXCR2–CXCLs轴是一个重要的趋化因子,CXCR2–CXCLs轴促进肿瘤进展的机制很多,但最显著的是与中性粒细胞募集到TME和促进血管生成有关。
CXCR2的中和在各种临床前癌症模型中显示出了有希望的结果,通常作为联合治疗的一部分来规避化疗耐药性。在黑色素瘤模型中,CXCR2抑制剂Navarixin与MAPK抑制具有协同作用,而抑制剂SB225002改善了卵巢肿瘤模型中索拉非尼的抗血管生成治疗。CXCR1和CXCR2抑制剂Reparixin与5-氟尿嘧啶联合使用时,也能够改善胃癌模型中的肿瘤细胞凋亡并减少肿瘤体积。AZ13381758是一种CXCR2的小分子抑制剂,与吉西他滨联合使用时,能够减少胰腺导管腺癌模型的转移并显著延长寿命。
目前,七种CXCR2抑制剂正在多项临床试验中进行研究,其中四种用于治疗转移性恶性肿瘤。其中包括用于治疗前列腺癌(2期)、头颈部鳞状细胞癌(1b/2期)和胰腺导管癌(1b/2期)的AZD5069/AZD9150;Reparixin用于治疗乳腺癌(2期);Navarixin用于治疗前列腺癌和非小细胞癌(2期);SX-682用于治疗III期和IV期黑色素瘤(1期)。
CXCR4
鉴于CXCR4与多种恶性肿瘤的生长和扩散具有无可争议的临床相关性,在过去十年中,已经开发出许多CXCR4靶向的肽和非肽拮抗剂。
CXCR4拮抗剂,如AMD3100和AMD3465,通过介导来自骨髓环境的肿瘤细胞的转运,增强了传统疗法的临床疗效。复发性AML患者的I/II期研究(NCT00512252)提供的数据显示,CXCR4/CXCL12轴阻断的体内疗效与令人鼓舞的缓解率之间的相关性。
人源化CXCR4抗体PF-06747143在包括NHL、AML和MM在内的多种血液肿瘤模型中显示出强烈的抗肿瘤作用。在急性髓系淋巴瘤患者中进行了一项I期试验(NCT02954653),评估其安全性和耐受性,但由于主办方的原因,该试验不幸终止。最近,另一种抗CXCR4抗体ulocuplumab(BMS-936564)的Ib/II期试验(NCT01359657)证实,阻断CXCR4–CXCL12轴是安全的,并且与来那度胺和地塞米松联合治疗复发性/难治性骨髓瘤患者具有较高的应答率。
CXCR4抑制剂在实体瘤中也被证明具有重要的抗癌潜力。目前有几项临床试验正在评估CXCR4拮抗剂对胶质母细胞瘤患者的临床益处。一项I/II期试验(NCT01977677)研究了plerixafor在替莫唑胺和放射治疗后的副作用和最佳剂量,结果显示,plerixafor未观察到剂量限制性毒性,并且似乎在RT后抑制CXCL4介导的血管生成,增强了放射治疗的效果。
除脑肿瘤外,AMD3465还能够预防体内乳腺癌生长和转移,而新型环肽CXCR4拮抗剂LY2510924在各种实体瘤和转移性乳腺癌临床前模型中显示出抗肿瘤活性。LY2510924在一期试验(NCT02737072)中进行试验,耐受性良好。对于HER2阴性转移性乳腺癌患者,CXCR4拮抗剂balixafortide作为单一疗法以及与其他药物联合使用的I期试验(NCT01837095)取得了有希望的初步结果。
值得注意的是,CXCR4抑制也被证明能促进强烈的抗肿瘤T细胞反应。卵巢癌临床前模型中的CXCR4阻断能显著增加T细胞介导的抗肿瘤免疫反应,使AMD3100治疗的小鼠具有显著的生存优势。BPRCX807是一种选择性和有效的CXCR4拮抗剂,最近在肝细胞癌小鼠模型的体外和体内试验中显示了良好的效果。
-04-
结语
趋化因子是一大类协调免疫细胞运输的趋向性的细胞因子。鉴于趋化因子在肿瘤免疫反应和肿瘤生物学中发挥着的多方面作用,趋化因子网络已成为潜在的免疫治疗靶点。
趋化因子受体及其配体之间存在非常复杂的相互作用,为了引入新一代基于趋化因子调节的免疫肿瘤治疗策略,迫切需要深入了解肿瘤微环境生物学以及更好的预测性临床模型。
尽管面临挑战,大量针对不同趋化因子信号通路的趋化因子受体抑制剂目前正在临床前研究和临床试验中进行评估,并且与常规化疗或免疫检查点疗法结合使用时,显示出有希望的结果。因此,可以预测,在不久的将来,趋化因子受体抑制剂将用于调节TME的组成并优化患者的免疫反应,为肿瘤患者带来希望。
参考资料:
1.Chemokine-Directed Tumor MicroenvironmentModulation in Cancer Immunotherapy. Int J Mol Sci. 2021 Sep; 22(18): 9804.
公众号内回复“ADC”或扫描下方图片中的二维码免费下载《抗体偶联药物:从基础到临床》的PDF格式电子书!
公众号已建立“小药说药专业交流群”微信行业交流群以及读者交流群,扫描下方小编二维码加入,入行业群请主动告知姓名、工作单位和职务。
免疫疗法
2025-01-22
·生物谷
在药物研发和临床治疗领域,药物性肝损伤(DILI)一直是个令人头疼的问题。其中,特发性药物性肝损伤(iDILI)由于发病机制难以捉摸,缺乏明确的剂量-反应关系,不仅威胁患者健康,也给科研和医疗工作带来巨大挑战。
近期,一项发表在Anal Chem的研究Establishment of an Idiosyncratic Drug-Induced Liver Injury Model on a Stacked Array Chip for Identification of CCL5-Mediated Paracrine Dynamics为我们带来了新的解决方案。
以往研究iDILI,主要依赖动物模型和体外细胞模型。动物模型存在药物消耗量大、物种差异等问题,限制了高通量药物筛选以及对分子和细胞层面机制的深入探究。体外细胞模型,如二维细胞培养模型,无法模拟体内复杂的炎症微环境,难以真实反映iDILI的发病过程。尽管器官芯片技术逐渐兴起,但此前的芯片在灵活性和兼容性方面存在不足,且一直没有与动态炎症相关的iDILI芯片模型。
本研究研发出一种堆叠阵列芯片,它由上层的肝脏芯片和下层的巨噬细胞芯片组成。研究人员先将肝细胞与特定混合液滴在肝脏芯片的微柱阵列上,形成3D肝脏微组织。同时,对巨噬细胞进行预处理后,接种到巨噬细胞芯片。然后将两者组装并共培养,设置不同处理组,成功构建了iDILI模型。该模型细胞活力接近100%,并且确定了诸如血清需求、细胞接种密度等优化参数,在多细胞系和原代细胞中都验证了其可行性。
图 1. 堆叠阵列芯片上iDILI模型的构建
为了验证模型的有效性,研究人员挑选了10种代表性药物,其中8种为iDILI药物,2种为固有DILI药物。实验结果显示,iDILI药物与脂多糖(LPS)共处理时,3D肝脏微组织的肝毒性明显高于单独给药组;而固有DILI药物共处理组与单独给药组相比,肝毒性没有显著增加,这表明该模型能够准确区分两类药物。
以尼美舒利(NIM)为例,研究人员进一步探究iDILI的发病机制。RNA测序和RT - qPCR分析发现,NIM与LPS共处理会激活TNF通路,引发肝脏微组织的炎症损伤。同时,CCL5等炎症因子水平上升,CCL5通过与CCR1、CCR3和CCR5受体结合,促使巨噬细胞向M1极化。此外,通过灵活操作芯片,研究人员发现NIM诱导iDILI的机制符合部分假设,炎症预激活和NIM预处理之间存在动态平衡,这种平衡影响着炎症相关基因的表达。
图 2. NIM诱导的iDILI促进3D肝脏微组织的炎症损伤
图 3. NIM诱导iDILI的机制示意图
这项研究构建的iDILI芯片模型具有重要意义。它能够模拟体内的动态微环境,准确区分iDILI药物,且芯片设计灵活,兼容性良好。通过该模型,我们对iDILI的发病机制有了更深入的理解,为iDILI药物筛选提供了有力工具,有望加速药物研发进程,降低临床用药风险。未来,随着科研的不断深入,通过整合患者来源细胞等方式,该模型的预测能力将进一步提升,为攻克iDILI带来更多希望,让更多患者受益于精准的医疗干预。
参考文献:
Hou Y, Gao Z, Tu P, Ai X, Jiang Y. Establishment of an Idiosyncratic Drug-Induced Liver Injury Model on a Stacked Array Chip for Identification of CCL5-Mediated Paracrine Dynamics. Anal Chem. 2024;96(49):19370-19377. doi:10.1021/acs.analchem.4c03552
本文仅用于学术分享,转载请注明出处。若有侵权,请联系微信:bioonSir 删除或修改!
点击下方「阅读原文」,前往生物谷官网查询更多生物相关资讯~
2024-12-20
·医药速览
1
前言
自然杀伤(NK)细胞是起源于淋巴的细胞毒性先天免疫细胞。1973年,人们发现了一种非T非B淋巴细胞亚群可有效杀死被抗体识别的细胞,随后首次被描述为“null”杀伤细胞。两年后,有报道称这种细胞能够杀死各种类型的肿瘤细胞,并创造了术语“自然”杀伤细胞。NK细胞不仅在抗肿瘤反应中发挥作用,而且在抵抗微生物感染方面也发挥作用。
NK细胞表达多种激活和抑制受体,这些受体介导的信号之间的平衡决定了NK细胞激活的结果。NK细胞在没有预先致敏的情况下杀死癌细胞的能力在肿瘤免疫监测中发挥重要作用。以 NK 细胞为基础的肿瘤免疫治疗领域已经到了一个激动人心的关头。虽然这些疗法还没有取得与过继性 T 细胞疗法同样程度的临床成功,但是早期的令人鼓舞的结果使 NK 细胞疗法的开发热情越来越高。
2
NK细胞生物学
NK细胞是第一个被鉴定的先天性淋巴细胞(ILC)亚型,能对病毒感染和/或转化的细胞产生多种效应器功能,主要是细胞杀伤和产生促炎细胞因子。NK细胞和其他ILC家族成员(—1型ILC(ILC1s)、ILC2s和ILC3s)与B细胞和T细胞来源于相同的淋巴祖细胞。NK细胞的细胞毒性活性使它们在功能上与CD8+T细胞最为相似,而ILC1、ILC2和ILC3群体的细胞因子生成模式将这些细胞分别对应CD4+T细胞的TH1、TH2和TH17亚群。
NK细胞的两个最典型的亚群是CD56brightCD16-和CD56dimCD16+群体。CD56bright细胞在外周血中的数量较少(循环中90%的NK细胞是CD56dim),而组织中的NK细胞主要是CD56bright。CD56bright NK细胞是强有力的细胞因子产生者,除非受到促炎性细胞因子如IL-15的刺激,否则细胞毒性较弱。相比之下,CD56dim NK细胞群可介导感染细胞和恶性细胞的连续杀伤,主要通过包含颗粒酶B和穿孔素的预先组装的溶细胞颗粒在免疫突触中的胞吐,最终诱导靶细胞凋亡。
3
NK细胞的抗肿瘤效应机制
NK细胞具有多种功能,可以限制癌细胞的生长和扩散。在TME先天性和适应性免疫细胞产生促炎性趋化因子的指导下,循环NK细胞可被招募到肿瘤发生的部位。CXCR3–CXCR4、CX3CR1和CCR3–CCR5是NK细胞亚群差异表达的主要趋化受体。
进入TME后,NK细胞可以通过“丢失自我”机制杀死癌细胞。许多癌细胞下调MHC I分子的表达,以逃避细胞毒性CD8+T细胞的检测,然而NK细胞能够识别和响应这种缺失的自我表型的细胞,最终导致靶细胞裂解。因此,在T细胞不能识别MHC I下调癌细胞的情况下,NK细胞具有治疗潜力。
ADCC是NK细胞介导的杀伤癌细胞的另一个关键机制。除了直接诱导细胞毒性外,NK细胞还通过产生促炎性细胞因子(包括IFN-γ和TNF)对转化细胞作出反应。
4
NK细胞的免疫检查点抑制
关于ICI的研究主要集中在抗肿瘤T细胞的去抑制,这种治疗模式增强NK细胞的活性也引起了相当大的关注。例如,人源化抗NKG2A单克隆抗体monalizumab目前正在对多种癌症患者进行单药试验,或与其他免疫检查点抑制剂联合应用,临床前数据表明这种药物能显著增强NK细胞和T细胞的细胞毒性。
TIGIT是另一种由NK细胞和T细胞表达的抑制性受体,其配体在人类肿瘤浸润的NK细胞上过表达。在一些小鼠模型中,TIGIT抑制逆转NK细胞衰竭并促进NK细胞依赖性抗肿瘤免疫。已经设计了一些积极的临床试验来测试单独抗TIGIT药物以及与其他免疫检查点抑制剂联合使用的有效性和/或安全性。(如NCT03119428、NCT04150965、NCT04047862、NCT04256421、NCT03563716和NCT04294810)
另外还有LAG-3和TIM-3,来自小鼠NK细胞研究的数据表明LAG-3在介导对肿瘤细胞系的细胞毒性方面起着积极作用;肺腺癌患者NK细胞上TIM-3表达增加预示着不良预后,体外抑制这种NK细胞的TIM-3增强了其细胞毒性和IFNγ的产生。目前,多个临床试验正在对各种癌症患者进行LAG-3和TIM-3抑制剂的试验,(包括NCT01968109、NCT04150965、NCT04140500、NCT03625323、NCT0331142、NCT03066648、NCT03489343、NCT03680508和NCT04139902等)。
其它基于NK细胞的免疫检查点还包括CD96、 Siglec-7/9、CD200R、CD47、CTLA-4、PD-1和B7-H3,将这些检查点结合起来进行协同抗肿瘤反应是未来充分发挥NK细胞杀伤肿瘤作用的方向。
5
过继性NK细胞疗法
异基因外周血NK细胞只是治疗性NK细胞众多潜在来源之一。NK细胞约占外周血淋巴细胞总数的10%,而脐带血(UCB)中的NK细胞占淋巴细胞总数的30%;因此,UCB是治疗效应NK细胞的可靠来源。UCBNK细胞的治疗效果目前正在一些临床试验中进行评估(如NCT01619761和NCT02280525)。
克隆性NK细胞系,如NK-92、KHYG-1和YT细胞,是异基因NK细胞的替代来源,NK-92细胞系已在临床试验中得到广泛测试。然而,这些细胞是非整倍体,因此遗传不稳定,这就要求它们在输注前接受辐照。辐照的NK-92细胞被观察到可以杀死癌症患者的肿瘤细胞。
此外,临床上正在对来自多种来源的干细胞衍生NK细胞产物进行检测,包括来自UCB干细胞或诱导多能干细胞(IPSC)的NK细胞产物。将成年细胞重新编程为多能干细胞,以使其分化为NK细胞并扩展生成最终产物,是基于iPSC的方法的一个独特特征。一项临床试验目前正在招募血液或实体癌患者,以测试这些现成的iPSC衍生NK细胞的安全性。
适应性NK细胞是治疗性NK细胞的另一个新兴来源。适应性NK细胞是一种自然发生的细胞群,在HCMV感染或再激活后在人类中扩增。HCMV UL40衍生肽抗原-HLA-E复合物与NK细胞上NKG2C之间的相互作用,导致NKG2ChiCD57+NK细胞增殖,NKG2ChiCD57+NK细胞下调参与细胞内信号传导的某些蛋白质,包括PLZF、SYK和FcεRIγ。适应性NK细胞具有一些独特的效应器特性,包括增强的ADCC、增强的细胞因子反应和对MDSCs和Treg细胞免疫抑制作用的固有抵抗。目前,三项临床试验正在评估这些适应性NK细胞对各种癌症患者的疗效。
细胞因子诱导记忆样(CIML)NK细胞是异基因细胞治疗的另一种选择,与其他类型的NK细胞产品相比具有独特的优势。CIML-NK细胞在体外通过IL-12、IL-15和IL-18的短暂启动,产生对细胞因子反应增强的NK细胞,并激活持续数周至数月的受体刺激。将这些CIML-NK细胞输注到携带AML异种移植物的小鼠体内可产生强大的抗肿瘤作用并显著延长存活时间。在I期试验中,CIML NK细胞具有良好的安全性,在44%的可评估AML患者(4/9)体内扩增并诱导病情缓解。
6
CAR-NK
嵌合抗原受体(CAR)是一种受体蛋白,它赋予免疫细胞新的能力,以靶向特定的抗原蛋白。CAR-NK细胞免疫疗法比CAR-T细胞免疫疗法更安全,而且NK细胞的安全性已在一些临床领域得到验证。例如,一些I/II期试验显示,同种异体NK细胞输注耐受性良好,不会引起GVHD和明显的毒性。因此,NK细胞是一种适应性更强的CAR载体,而不仅仅局限于自体细胞。
NK细胞上表达的功能性CAR分子由三部分组成:胞外结构域、跨膜区以及胞内的信号结构域。胞外结构域由一个信号肽和识别抗原的单链抗体片段(scFv)组成,一段铰链区将这个结构连接到跨膜区,它也在细胞内连接到包含激活信号的胞内结构域。成功的CAR设计是通过仔细的设计和功能测试相结合来实现的。
载体骨架和启动子
载体骨架包含表达CAR所需的所有元件,如启动子、polyA信号和转录调控片段。
启动子的选择直接影响到转基因的表达水平。目前,对不同启动子在NK细胞系中的CAR表达和功能的比较只有一次报道,而对原代NK细胞没有比较数据。就这一次单个报告来看,还不能确定CAR-NK细胞的最佳启动子。
目前关于CAR-NK细胞的报道显示,多种启动子被用于驱动CAR的表达,无论是细胞系来源的还是原代NK细胞。在原代CAR-NK和CAR-NK细胞系中,病毒启动子(CMV、MPSV、MMLV、SFFV等)比组成性活性启动子(如EF1α、CMV和PGK)更常用。
信号肽
在信号肽中存在着巨大的异质性,这直接转化为不同水平的蛋白质分泌效率。对于CAR-NK和CAR-T细胞,还没有确定最佳信号肽的比较研究。目前,CD8a-SP是原代NK细胞最常用的信号肽序列(16%,71%的研究中未公布)和NK细胞系的免疫球蛋白重链或轻链信号肽(29%)。
单链抗体
单链抗体片段是CAR的肿瘤抗原结合域,该结构域将决定CAR-NK细胞的特异性和功能。
由于单链抗体不是抗体的天然形式,因此重链和轻链的顺序是人工确定的。到目前为止,对于CAR-NK设计,大多数更喜欢VH-VL方向,而不是VL-VH方向。
Fujiwara等人证明重链和轻链的顺序不影响T细胞上抗KDR CAR的表达水平。
此外,细胞可以配备多个单链抗体,从而扩大CAR效应细胞的抗原识别能力。在这里,有多种选择:CARs可以用双元件的载体转导,诱导两个CAR结构的表达;或者将两个单链抗体融合在一个结构中,产生串联单链抗体的“单柄”CAR。虽然这些技术已用于生产CAR-T细胞,但CAR-NK细胞仍未知。
目前大多数临床CAR-T细胞试验都使用了来自小鼠抗体的单链抗体,这增加了抗小鼠IgG细胞宿主抗移植物病的风险,这个问题可以通过人源化或筛选全人抗体避免。然而不幸的是,由于这些CAR受体的嵌合特性,即使是人源化的单链抗体也可能诱导宿主抗独特型免疫反应。幸运的是,在迄今为止数量有限的CAR-NK临床试验中,没有发现与抗CAR免疫反应相关的重大副作用。
连接区
重链和轻链之间的连接区有助于稳定单链抗体的构象,过短会导致多聚体的形成,过长可能导致水解或降低VH和VL结构域之间的关联。对于CAR-NK细胞,五肽GGGGS的多聚体应用最为广泛,通常为3个重复。另一个旨在增强蛋白水解稳定性的连接体是Whitlow“218”连接体:GSTGSGSKPGSGEGSTKG。
目前,虽然大多数CAR-NK研究没有提供连接细节,但已有的研究报道中,有22项使用了G4S连接,有2项应用了218连接。
铰链区
铰链区是连接单链抗体单位和跨膜结构域的CAR细胞外结构区,它通常维持效应细胞中稳健的CAR表达和活性所需的稳定性。大多数CAR-NK构建使用CD8α或CD28胞外结构域的衍生物或基于IgG的铰链区。
铰链区的类型和长度对CAR的功能活动有重要影响。但是目前大多数信息全来自CAR-T领域,能否直接转化为CAR-NK还有待证明。
在CD28和CD8α铰链区之间的直接比较中,发现CD28更有可能促进CAR分子的二聚化,因此,CD28铰链区的CAR产生的激活刺激更强。虽然这可能是有益的,但也可能导致更严重的副作用。
IgG为基础的铰链区也广泛应用于CAR结构。基于IgG铰链区的一个主要优点是结构的灵活性,该结构通常由IgG1或IgG4的FC部分或Fc部分的CH2/CH3结构域组成。铰链区的长度可以调节以适应抗原识别,但研究发现,间隔区越短,细胞因子的产生越高,CAR-T细胞增殖越快,体内持久性和抗肿瘤效果越好。
对于CAR-NK细胞,大多数研究在原代NK细胞(16/35)和CAR-NK细胞系(41/72)中均采用CD8α铰链区。其它使用的铰链区包括CD28、IgG Fc结构域和DAP12。
跨膜结构域
跨膜(TM)结构域连接CAR的胞外结构域和细胞内激活信号结构域,CAR-NK最常用的TM部分来自CD3ζ、CD8和CD28,但其他如NKG2D、2B4、DNAM1也有被使用。
TM结构域的选择影响了CAR结构在细胞功能上的活化程度。通常在NK细胞上表达的分子如DNAM-1、2B4和NKG2D的TM会导致更多的CD107a脱颗粒和更高的细胞毒性,因此,TM的具体来源将决定CAR-NK的活性。
TM结构域的一个重要方面是,最佳TM区域应遵循T细胞或NK细胞上跨膜蛋白的蛋白质自然取向(N端到C端顺序)。NKG2D虽然是一种强大的NK细胞激活剂,然而,天然NKG2D具有C端到N端的跨膜区。
目前,CD8α和CD28修饰的TM在原代CAR-NK细胞中最常见,而CD28是CAR-NK细胞系的首选TM区域。
CAR-NK激活信号
CAR的细胞内激活信号的数量决定了其属于哪一“代”CAR。
第一代CAR-NK细胞与CAR-T细胞一样,只含有CD3ζ信号。第二代和第三代CAR-NK分别携带一个和两个额外的共刺激信号,共刺激分子通常来源于CD28家族(CD28和ICOS)、TNFR家族(4-1BB、OX40和CD27)或SLAM相关受体家族(2B4)。到目前为止,唯一公布的CAR-NK临床试验采用了第二代CAR-NK构建,该构建通过加入IL-15表达和诱导Caspase9增强活性。
目前大多数CAR结构依赖于CD3ζ链信号域,强烈的激活信号对于诱导有效的抗肿瘤反应很重要,但也可能导致效应细胞的快速衰竭。因此,共刺激域的组合可用于校准所需的免疫细胞反应。与基于4-1BB的 CARs相比,基于CD28的CARs表现出更快的效应器特征,诱导更高水平的IFN-γ、颗粒酶B、TNF-α。然而,这种强烈的共刺激信号也会导致活化诱导的细胞死亡(AICD)。
相比较,4-1BB-CD3ζ信号优先诱导记忆相关基因和持续的抗肿瘤活性。原因可能是4-1BB结构域改善了CD28结构域引起的T细胞耗竭。
如上图所示,在CAR-NK细胞系和原代CAR-NK细胞的研究中,CD3ζ几乎被普遍用作主要的激活域,其中大约一半携带一个额外的激活域,通常添加4-1BB或CD28。至于第三代结构,CD28/4-1BB/CD3ζ的组合是最常用的。
7
NK细胞定向接合器
各种免疫逃避机制限制了NK细胞在体内与肿瘤细胞的结合程度,是实现广泛有效的NK细胞治疗的主要障碍。为了增强肿瘤浸润性NK细胞的自然细胞毒性,许多研究团队已经在开发一些分子,使这些细胞以抗原特异性的方式与肿瘤细胞接触。这些分子通常是由多个抗体(通常为单链抗体)组成的双特异或三特异性接合器,使得一个结构域针对NK细胞激活受体,另一个与特定肿瘤相关抗原结合。例如,一种由两个单链抗体组成的三特异性杀伤接合器(TriKE),一个针对NK细胞上的CD16,另一个针对AML细胞的CD33,通过IL-15结构域连接,该结构域旨在增强NK细胞的存活和增殖。
这种抗CD16、IL-15和抗CD33 TriKE(GTB-3550)增强了NK细胞效应器功能的其他几个重要方面,在临床前研究中观察到了改善迁移能力、增加连续杀伤和缩短首次杀伤时间。
在临床前研究中,其他几种NKCE分子也被证明具有强大的抗肿瘤作用。AFM13靶向淋巴瘤相关抗原CD30和CD16a,后者是NK细胞表达的CD16的跨膜形式。AFM13在AACR 2022中表现惊艳,AFM13+脐血来源NK细胞治疗,完全缓解率达到62%。
8
展望
自然杀伤细胞是一组独特的抗肿瘤效应细胞,具有不受MHC限制的细胞毒性、产生细胞因子和免疫记忆等功能,使其成为先天性和适应性免疫反应系统中的关键角色。一些癌症的发生与功能失调的NK细胞有关。因此,修复这种NK细胞可能是抗肿瘤免疫治疗的一个潜在选择。这种修复的一种方法是抑制免疫检查点,即癌细胞通过控制免疫细胞表面的抑制受体进行免疫逃逸。
利用NK细胞与抗体、免疫细胞接合器、CARs和其它检查点抑制剂的组合方法进行试验,这些方法旨在调节抑制检查点和增强抗肿瘤能力。目标是找到一种基于NK细胞的治疗策略,这种策略是安全的,并且具有广泛临床应用所需的确切疗效。
参考文献:
1.Exploring the NK cell platform for cancer immunotherapy. Nat RevClin Oncol. 2020 Sep 15.
2. K Cell-Based Immune Checkpoint Inhibition. Front. Immunol., 13February 2020
3. CAR-expressing NK cells for cancer therapy: a new hope. BiosciTrends. 2020 Sep 6.
4. Chimeric antigen receptornatural killer (CAR-NK) cell design and engineering for cancer therapy. JHematol Oncol. 2021; 14: 73.
往期链接
“小小疫苗”养成记 | 医药公司管线盘点
人人学懂免疫学 | 人人学懂免疫学(语音版)
综述文章解读 | 文献略读 | 医学科普 | 医药前沿笔记
PROTAC技术 | 抗体药物 | 抗体药物偶联-ADC
核酸疫苗 | CAR技术 | 化学生物学
温馨提示
医药速览公众号目前已经有近12个交流群(好学,有趣且奔波于医药圈人才聚集于此)。进群加作者微信(yiyaoxueshu666)或者扫描公众号二维码添加作者,备注“姓名/昵称-企业/高校-具体研究领域/专业”,此群仅为科研交流群,非诚勿扰。
简单操作即可星标⭐️医药速览,第一时间收到我们的推送
①点击标题下方“医药速览”
②至右上角“...” ③点击“设为星标
细胞疗法免疫疗法临床研究
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
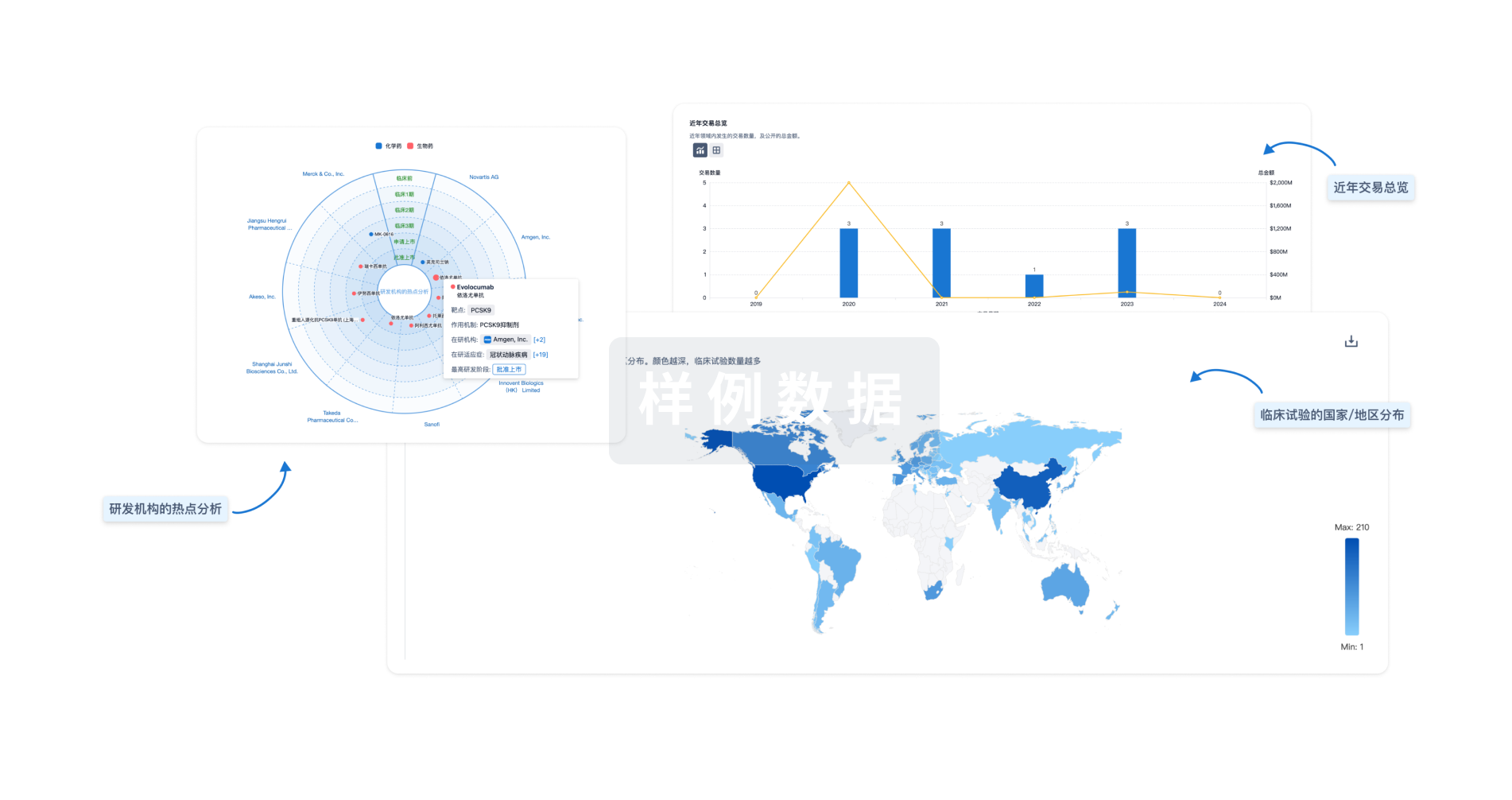
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用