预约演示
更新于:2025-05-07
生长因子受体
更新于:2025-05-07
基本信息
别名- |
简介- |
关联
23
项与 生长因子受体 相关的药物CN117986257
专利挖掘作用机制- |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段药物发现 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点 |
作用机制 生长因子受体调节剂 |
在研机构- |
在研适应症- |
非在研适应症 |
最高研发阶段终止 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
8
项与 生长因子受体 相关的临床试验CTIS2022-501935-18-00
Abdominal Aortic Aneurysm Stabilization with Truncal Cells: Controlled Clinical Trial with Historical Cohorts. - HULP-STEM-EVAR-2020
开始日期2024-06-13 |
NCT02554019
A Prospective, Double-blind, Randomized, Placebo-controlled, Repeated Dose, Multicentre Phase IIa Proof-of-Concept Study With BT063 in Subjects With Systemic Lupus Erythematosus
The purpose of this study is to evaluate the safety and efficacy of repeated intravenous infusions of the study drug BT063 in patients with Systemic Lupus Erythematosus (SLE) compared with people who receive a placebo.
开始日期2015-09-28 |
申办/合作机构 |
EUCTR2014-005526-35-PL
A Prospective, Double-blind, Randomized, Placebo-controlled, Repeated dose, Multicentre Phase IIa Proof-of-Concept Study with BT063 in Subjects with Systemic Lupus Erythematosus (BT063 in SLE)
开始日期2015-09-12 |
申办/合作机构 |
100 项与 生长因子受体 相关的临床结果
登录后查看更多信息
100 项与 生长因子受体 相关的转化医学
登录后查看更多信息
0 项与 生长因子受体 相关的专利(医药)
登录后查看更多信息
2,199
项与 生长因子受体 相关的文献(医药)2025-03-18·Journal of Virology
RAF1 promotes successful human cytomegalovirus replication and is regulated by AMPK-mediated phosphorylation during infection
Article
作者: Munger, Joshua C. ; Pack, Ludia J. ; Dunn, Diana M.
2025-02-01·International Journal of Biological Macromolecules
NIR-responsive injectable nanocomposite hydrogels with enhanced angiogenesis for promoting full-thickness wound healing
Article
作者: Yu, Guiting ; Wang, Yiyu ; Wang, Xinyu ; Jin, Zheng ; Zhao, Kai ; Shi, Jian ; Lin, Yuhong ; Niu, Chunqing ; Li, Binbin ; Wu, Xiaona ; Liu, Chibo
2025-01-01·Cancer Genomics - Proteomics
Regulation and Function of CCL2 and N-Myc in Retinoic Acid-treated Neuroblastoma Cells
Article
作者: Schmidt, Berit ; Waetzig, Vicki ; Pommert, Nina Sophie ; Tim, Vera ; Murra, Nanke ; Kaehler, Meike ; Issa, Reema Sami ; Cascorbi, Ingolf ; Bruckmueller, Henrike
107
项与 生长因子受体 相关的新闻(医药)2025-05-01
希望之城在 AACR 上展示的最新研究成果,其亮点涵盖人工智能、精准医疗及免疫疗法等多个前沿领域。全美顶尖癌症研究机构希望之城将亮相美国癌症研究协会(AACR)年度会议。希望之城是美国规模最大、技术最先进的癌症研究与治疗中心之一,其国家医疗中心被《美国新闻与世界报道》评为全美癌症治疗前五强。在4月25日至30日于芝加哥举办的这场学术盛会上,希望之城的研究团队通过 74 场专题报告、全体会议、学术研讨及海报展示等形式,分享了其创新的临床试验成果、突破性诊断技术及治疗方案的最新进展。David W. CraigPh.D.除大会期间的系列研究成果展示外,希望之城贝克曼研究所综合转化科学系教授兼创始系主任 David W. Craig 博士压轴主持了题为《预测肿瘤学的机遇》的闭幕全体会议(美国中部时间4月30日周三上午8:00-10:00)。此外,他还于周五下午4:46-5:06主持了一场教育专场会议,探讨了如何运用多组学生物分析技术解析实体瘤异质性细胞群的基因特征。Michael CaligiuriM.D.美国中部时间4月26日周六上午10时至11时30分,希望之城国家医疗中心前院长、血液&造血细胞移植学系教授 Michael A. Caligiuri 医学博士主持了一场名为“自然杀伤细胞(NK细胞)临床应用新进展”的专题研讨会,并发表题为《先天免疫淋巴细胞谱系研究——聚焦 NK 细胞》的学术报告。同日早间8时至9时30分,Caligiuri 教授还主持了“学术创业启航篇:从实验室到临床的转化路径”研讨会,系统阐述基础研究成果向临床应用转化的关键实施步骤。Hope S. RugoM.D.在诊疗新进展专题会上,最近加入希望之城担任女性癌症项目主任的 Hope Rugo 医学博士于4月28日周一下1:25 至 1:45发表了一项名为《抗体药物偶联物(ADC)毒性管理新策略》的专题报告。此外,Rugo 博士还以特邀专家身份,出席次日上午10:15至中午12:15举行的“生物制剂与T细胞衔接器临床试验”全体会议研讨环节。希望之城在 AACR 年会上公布的研究成果亮点包括:新型免疫疗法 III 期临床试验取得突破性进展鼻咽癌——这个关乎人体呼吸与吞咽功能的重要咽喉部位恶性肿瘤虽属罕见,但在中国、北非等地区却呈现高发态势。针对复发性或转移性鼻咽癌的治疗,一项创新性免疫疗法与标准化疗的联合治疗方案展现出显著疗效。基于这种名为派安普利单抗(penpulimab)的新药 III 期临床试验数据,美国食品药品管理局(FDA)于上周正式批准其联合顺铂/卡铂与吉西他滨方案,用于复发性或转移性鼻咽癌成人患者的一线治疗。同时,FDA 也批准该药物作为单药疗法,适用于铂类化疗期间或之后出现病情进展、且至少接受过一种其他疗法的同类患者。Aditya ShreenivasM.D., M.S.4月27日周日,美国中部时间下午3:50-4:00,肿瘤内科专家 Aditya Shreenivas 医学博士在临床试验专题研讨会上,重磅发布题为《派安普利单抗(Penpulimab)对比安慰剂联合化疗作为复发性或转移性鼻咽癌一线治疗的全球多中心随机双盲III期临床试验(AK105-304)》的核心数据。 派安普利单抗(Penpulimab)作为新型抗 PD-1 抑制剂,能有效激活免疫系统对癌细胞的识别与攻击机制。先前的研究表明,PD-1 抑制剂与化疗的联合治疗作为亚洲患者的一线治疗方法具有良好疗效,在此基础上,该试验在 III 期阶段纳入了 291 名来自亚洲和非亚洲国家的患者。这些患者分别接受了派安普利单抗与标准化疗的联合治疗以及安慰剂加化疗的治疗。研究结果表明,接受派安普利单抗联合治疗组患者的中位无进展生存期达 9.63 个月,较对照组 7 个月显著延长,疾病进展风险降低 55%。研究人员同样也发现了接受派安普利单抗联合治疗的患者组安全性良好,不良反应可控。希望之城(全球46个试验中心之一)该研究负责人 Shreenivas 博士强调道:“派安普利单抗的独特价值在于其经结构优化的抗 PD-1 抗体特性,旨在提升疗效的同时有效降低免疫相关副作用。这项研究证明了使用派安普利单抗加化疗有望成为复发性或转移性鼻咽癌患者新的一线治疗选择。”他还提及到,该药物已在中国获批用于复发难治性经典霍奇金淋巴瘤及转移性鳞状非小细胞肺癌治疗。此次研究成果有望推动其在更多国家与适应症领域的获批进程。Shreenivas 博士指出,该临床试验的后续研究方向将聚焦于疗效预测模型的建立。研究团队已针对不同特征亚组展开深度分析,包括存在肝转移病灶的患者、差异化蛋白表达水平群体,以及爱泼斯坦-巴尔病毒(EB病毒)DNA载量各异的病例。EB病毒已被确认为鼻咽癌的重要致病因子。该临床试验由开发派安普利单抗的中国康方生物(Akeso)医药公司赞助。研究人员利用创新技术进一步了解了卵巢癌、前列腺癌和乳腺癌患者的治疗响应卵巢癌对于最常见的高级别浆液性卵巢癌(恶性程度最高亚型),患者对免疫治疗的响应存在显著个体差异。为解析这种异质性并实现精准治疗,希望之城的研究团队和来自加州大学由 Jing Qian(希望之城首席科学官、Irell & Manella 癌症中心主任以及贝克曼研究所 Morgan & Helen Chu 冠名主任的 John D. Carpten 博士实验室博士生)领导的科研团队,试图描述出对治疗有不同响应的患者肿瘤环境中的癌细胞和免疫细胞的特征。研究团队运用前沿的空间转录组技术以绘制癌细胞与免疫细胞的相互作用图谱,从而揭示出不同免疫治疗响应性的肿瘤组织中,免疫细胞行为模式与群体构成的动态差异。作为医学研究领域快速发展的突破性技术,空间转录组学方法能够精确定位组织中基因表达的空间分布特征,为肿瘤微环境研究提供全新视角。对此,研究负责人 Qian 表示:“未来,这种方法可以帮助筛选免疫治疗潜在获益人群以及为治疗无响应者发掘新的干预靶点。最终,这将推动高级别浆液性卵巢癌迈向精准免疫治疗新时代。”据悉,研究团队下一步将构建细胞模型并扩大临床样本规模,重点探究特定免疫细胞亚群的靶向调控对提升卵巢癌免疫治疗响应的作用机制。Qian 博士于4月27日周日美国中部时间下午2:00-5:00,在最新突破性研究海报专场发布了题为《空间转录组学解析免疫检查点抑制剂不同响应程度揭示高级别浆液性卵巢癌肿瘤和免疫微环境差异》的研究成果。前列腺癌最新研究表明,种族因素与疾病生物学特征之间存在的复杂相互作用,可能导致转移性激素敏感性前列腺癌(mHSPC)在不同人种患者中呈现差异化表现。为探究西班牙裔与非西班牙裔患者肿瘤组织的生物学差异,希望之城医学中心肿瘤内科 Tanya Barauskas Dorff 教授领衔的研究团队,从现有临床试验中获取了治疗前前列腺活检标本进行深度分析。研究团队采用数字空间分析技术——这项能在组织水平精确定位基因与蛋白表达的前沿技术,对 mHSPC 患者的肿瘤微环境进行了高精度解析。研究发现,西班牙裔与非西班牙裔患者在 Foxp3、PARP 和 STING 等关键蛋白的表达水平上存在显著差异,而这些蛋白正是多种抗癌药物的作用靶点。Tanya Barauskas DorffM.D.Dorff 博士介绍道:“通过对不同种族背景患者样本的深度分析,我们有望揭示导致治疗反应差异的潜在因素。随着更多组织样本检测工作的完成,我们将把分子特征与临床疗效进行关联分析,从而筛选出最具转化价值的候选生物标志物。” 研究团队计划进一步扩大样本多样性,并将分子特征数据与 2026 年初公布的临床试验结果进行系统比对。该项目第一作者、血液学与肿瘤学研究员 Peter Zang 博士于4月29日周二美国中部时间下午2:00-5:00,在题为《基于GeoMx数字空间分析技术的西裔/非西裔mHSPC患者差异蛋白表达研究》的海报展示中汇报了团队的最新发现。乳腺癌肿瘤内科&治疗研究部博士后研究员 Sydney Grant 和助理教授 Aritro Nath 博士于4月27日周二上午9:00至中午12:00(美国中部时间)发布了“基于多模态数据融合与生存变分自编码器的乳腺癌无复发生存期预测系统”的海报演讲,重点介绍该团队开发的一种基于人工智能的强大新方法,用于预测乳腺癌患者的无复发生存期。这项研究突破性地拓展了生成式 AI 模型的临床应用维度,通过整合远超传统生物标志物范畴的多源真实世界数据,构建出更精准、更具个性化的癌症预后预测体系。Aritro NathPh.D.Nath 博士强调道:“该成果有望催生新型临床检测技术。在初诊阶段即可为治疗决策提供科学依据,推动肿瘤诊疗真正迈向精准化时代。例如,AI 系统能精准判别需要强化治疗的高危患者与可避免过度治疗的适宜人群。” 该团队目前正在努力扩展他们的模型,以预测哪种类型的治疗或药物类别对个别患者最有效,目标是在临床上利用人工智能指导治疗选择。新技术识别西班牙裔和拉丁裔患者早发结直肠癌的独特基因变化Enrique Velazquez Villarreal, M.D., Ph.D., M.P.H., M.S.结直肠癌高居癌症致死率第二位,近年来年轻患者比例显著攀升,其中西班牙裔与拉丁裔人群尤为突出。综合转化科学系助理教授 Enrique Velazquez Villarreal 博士团队最新研究发现,该族群早发结直肠癌存在独特的基因变异特征,这些发现为揭示肿瘤发生发展机制提供了关键线索。 论文第一作者 Francisco (Paco) Carranza 博士强调:“这是首个针对洛杉矶地区西裔群体的结直肠癌基因组深度研究。这个长期被科研忽视的族群,其遗传特征将帮助我们开发更精准的靶向治疗方案。”研究团队采用 DNA/RNA 测序结合 10x Genomics Visium 空间转录组技术,首次实现肿瘤微环境中基因表达谱的精准定位。这种创新方法不仅揭示了癌细胞与免疫系统的动态互作机制,更发现了该族群特异的疾病发展规律。重点研究如何消除西裔群体结直肠癌医疗差异的 Velazquez Villarreal 博士表示:“这项研究推动我们向‘医疗平等’的愿景迈进——让不同族裔的患者都能获得最优治疗方案。”据悉,Carranza 和他的合作者计划采用升级版 10x Genomics Visium 平台开展单细胞精度研究。这项突破性技术有望为个体化治疗提供更精细的分子图谱,并为新型临床试验设计奠定基础。Carranza 博士于4月28日周一美国中部时间14:35-14:50,在《基于空间转录组学的西裔早发结直肠癌MYC基因与WNT信号通路多组学分析》专题研讨会上汇报了团队的这项创新成果。希望之城研发的 AI 医疗助手让精准医疗普惠可及、更具包容性Velazquez Villarreal 博士还将在海报上展示其实验室开发的新型精准医疗人工智能工具,该工具可解决整合多源异构数据的关键难题,从而促进癌症研究的公平性。这款名为“精准医学人工智能代理”(PM-AI)的智能对话系统,具备自然语言理解与复杂数据分析的双重能力。它创新性地将临床资料、基因组数据与社会经济因素(如收入水平、医疗可及性等)进行多维关联,使科学家更容易以更全面、更包容的方式研究癌症。Velazquez Villarreal 博士指出:“PM-AI 极大降低了复杂医疗数据的分析门槛,它能帮助研究者精准识别不同人群的最优治疗方案。这意味着未来患者将获得融合遗传特征、健康档案与社会环境等多维度的个体化诊疗,特别是让医疗资源匮乏群体也能享受精准医疗的福祉。”他说,研究团队计划将 PM-AI 应用于更多类型的癌症,并整合更多类型的数据,从而不断扩展 PM-AI 的功能。这一创新工具未来将服务于三大目标:辅助临床决策、优化研究设计、最终实现精准医疗的全民可及。这项题为《PM-AI 智能诊疗系统:基于临床-基因组-社会健康数据的整合分析推进精准医疗与健康公平》的研究,作为 AACR 首个采用"AI 对话代理"尖端技术的入选成果,于4月27日周日美国中部时间14:00-17:00进行了专题海报展示。突破性联合疗法破解 ER+ 乳腺癌耐药难题作为乳腺癌最常见亚型,雌激素受体阳性(ER+)患者中有 30%-50% 会对一线内分泌治疗产生耐药,最终进展为晚期癌症。现有细胞周期抑制剂虽能延缓转移性 ER+ 乳腺癌进展,但耐药性问题同样日益凸显。现在,希望之城科学家的最新研究发现,对细胞周期抑制剂产生耐药的 ER+ 乳腺癌会通过动态重构细胞凋亡通路与增殖通路(调控细胞分裂与生长的关键路径)来维持生存。为攻克这一难题,研究团队创新性地探索靶向生长因子受体的联合治疗方案,旨在实现双重调控——同步阻断癌细胞增殖通路并持续激活凋亡通路,从而延长治疗有效期。通过整合前沿的短期/长期细胞模型实验与数理计算分析,团队成功验证了细胞周期抑制剂瑞博西利(ribociclib)联合生长因子抑制剂阿法替尼(afatinib)的创新疗法。该方案展现出对乳腺癌细胞生长的持久抑制效果。Andrea BildPh.D.“尽管靶向疗法已显著改善激素依赖性乳腺癌疗效,但耐药性仍是制约长期获益的关键瓶颈。”本研究通讯作者、肿瘤内科 Andrea Bild 教授指出,“我们提出的动态调控策略,为提升现有疗法的持续有效性提供了新思路。” 下一步,研究团队的目标是将他们的研究成果转化为临床实践,造福患者。Bild 博士说,为此,他们将扩大时间计算和数学建模的使用范围,以监测分子随时间的变化,并确定可指导未来治疗策略的动态生物标志物。Bild实验室博士研究生 Kimya Karimi 于4月29日周二美国中部时间15:05-15:20,在《ER+ 乳腺癌细胞周期抑制剂耐药内在机制及破解策略》专题研讨会上汇报了这项突破性发现。关于希望之城希望之城的使命是将未来的治愈方法带给今天有所需要的人。希望之城成立于 1913 年,现已发展成为美国最大的癌症研究和治疗机构之一,也是糖尿病和其他危及生命疾病的主要研究中心之一。希望之城的研究为众多突破性癌症药物以及人类合成胰岛素和单克隆抗体奠定了基础。希望之城以美国国家癌症研究所指定的独立性综合癌症中心为核心,为患者带来了独特的综合性护理模式,涵盖了癌症护理、研究和开发、学术和培训以及创新计划。希望之城不断发展的全国性系统包括位于洛杉矶的主院区、遍布南加州的临床护理网点、位于加利福尼亚州橙县的新癌症中心以及位于亚特兰大、芝加哥和凤凰城的治疗网点。希望之城的附属机构包括转化基因组学研究所和 AccessHopeTM 等。如欲了解关于希望之城的更多信息,请通过我们的微信公众号或下方联系方式与我们取得联系。
AACR会议临床结果临床3期抗体药物偶联物
2025-04-17
点击上方蓝字 关注我们编者按近年来,随着乳腺癌诊疗技术的快速发展、创新疗法的广泛应用以及靶向药物的普及,我国乳腺癌患者的生存预后显著改善,5年生存率已提升至83.2%[1],逐步接近国际先进水平。随着患者生存期的延长,治疗安全性的管理成为临床关注的重点。国内外多部指南和专家共识建议,对于HER-2阳性早期乳腺癌患者,在完成含曲妥珠单抗的辅助治疗后,可序贯奈拉替尼强化治疗,以进一步降低复发风险,提高治愈率。然而,腹泻作为奈拉替尼等小分子靶向药物的常见不良反应,可能影响患者的生活质量和治疗依从性。因此,及早识别并妥善处理腹泻问题,对于减少药物减量或停药、确保治疗效果最大化具有重要意义。本文通过一例右乳浸润性导管癌患者的治疗案例,探讨奈拉替尼相关腹泻的管理策略。该患者术后接受化疗联合曲妥珠单抗和帕妥珠单抗(HP)辅助治疗约1年,此后,患者接受奈拉替尼强化辅助治疗,按照3-4-6剂量递增方式给药(第一周3片/天,第二周4片/天,第三周及以后6片/天),目前病情稳定。值得注意的是,在奈拉替尼治疗初期,患者常规使用洛哌丁胺预防腹泻,但仍出现腹泻症状,之后服用江苏省中医院特色中药制剂-温脾实肠颗粒,腹泻症状迅速好转。截至目前,患者未出现其他不良反应,整体状况良好。病例分享专家简介王聪江苏省中医院乳腺外科中医师 博士研究生发表SCI2篇,中文核心论文10篇,科技核心论文5篇,主持院级课题一项,市级课题一项曾获中华中医药科技进步二等奖作为编委编书两本《许芝银乳腺病临证精要》、《外科常见病外治疗法》获得国家发明专利1项江苏省中医药学会乳腺病专委会青年委员中华中医药学会外科分会疮疡专业委员会委员江苏省整合医学研究会围手术处理专业委员会委员病例介绍患者基本信息患者:女,年龄45岁,未绝经,体重60kg。主诉:发现右乳肿块半年。家族史:否认家族性肿瘤病史及其他遗传病史。既往史:既往健康,无基础疾病。现病史:患者半年前因“右乳肿块”至我院行穿刺活检,病理提示:(右乳肿块穿刺标本):浸润性乳腺癌,非特殊类型(浸润性导管癌),Nottingham分级:2级,未见明确脉管内癌栓及神经侵犯。免疫组化结果:ER(约2%弱+),PR(约5%弱+),Her-2(3+),Ki67(约50%+)。入院见:患者神清,精神可,无恶寒发热,无头晕头痛,无胸闷胸痛,无恶心呕吐,无腹痛腹泻,纳寐可,二便调。近期体重未见明显变化。辅助检查· 乳腺彩超1、右乳9点见一个低回声区,大小约0.53*0.63cm,呈直立生长,边缘成角、毛刺,内部回声不均匀,肿块内未见强回声,BIRADS 5类;2、右乳10点见一个低回声区,大小约1.4*0.9cm,边缘成角、毛刺,内部回声不均匀,肿块内未见强回声,BIRADS 5类。图1 乳腺彩超结果· 乳腺钼靶1、双乳腺体密度混合型ACR c型;2、双乳小叶增生伴瘤化;右乳外上象限多发结节,考虑BIRADS 4B类,建议进一步MR检查。图2 乳腺DR结果· 乳腺核磁共振(MRI)1、双侧乳腺呈多量型(ACR-c型);2、右乳上方结节影,考虑为乳腺癌,BIRADS 6类,右乳外上结节及小片状强化灶,BIRADS 4a类,DCIS待排除;3、双侧乳腺增生,BIRADS 2类。图3 乳腺MRI结果· CT1、右乳后上方结节影,伴右侧腋下多枚淋巴结,建议乳腺核磁MRI平扫+增强进一步检查;2、右肺下叶及左肺下叶胸膜下少许间质增生,或可能由肺坠积效应所致;3、肝脏钙化灶4、胸腰椎轻度退行性变。图4 CT结果· 病理(右乳肿块穿刺病理):浸润性乳腺癌,非特殊类型(浸润性导管癌),Nottingham分级:2级,未见明确脉管内癌栓及神经侵犯。免疫组化结果:ER(约2%弱+),PR(约5%弱+),Her-2(3+),Ki67(约50%+)。图5 穿刺活检结果· 实验室检查血常规(白细胞、中性粒细胞计数、血红蛋白、血小板)、生化(肝肾功能ALT等)均正常,心肺功能正常,肿瘤指标(CEA、CA125、CA153、CA199)均未见异常。临床诊断:右乳浸润性导管癌,cT1bN1aM0。治疗经过一、手术治疗2023-08-11排除手术禁忌,遂在全麻下行“右单侧乳房根治性切除伴同侧腋窝前哨淋巴结活检术+右腋下淋巴结根治性切除术”。术中快速病理(右腋下淋巴结):查及美兰染色淋巴结(1/3)枚见癌转移;非美兰染色淋巴结1枚未见癌转移(0/1)。结合常规及免疫组化,支持为浸润性导管癌转移。术后常规病理提示:(右乳癌单纯切除标本):1.常规及免疫组化标记,支持浸润性导管癌,Nottingham分级:2级(腺体形成3分,核级2分,核分裂1分,总分6分),肿瘤最大径0.9cm,未见明确脉管内癌栓及神经侵犯;另见乳腺导管原位癌(DCIS,高级别,粉刺型实体型)伴微浸润(微小浸润性乳腺癌,浸润灶最大径1mm,可见小叶癌化。免疫组化结果:ER(30%,弱-中等+),PR(约20%,中等+),Her-2(3+),Ki67(约8%+)。病理分期:T1bN1a(sn)。FISH检测:HER-2基因为阳性。诊断:右乳浸润性导管癌,pT1bN1aM0。二、术后辅助治疗辅助治疗为EC-THP方案,具体用药如下:于2023-08-25、09-15、10-06、10-27行术后第1、2、3、4次辅助化疗(EC方案,具体用药:注射用表柔比星140mg;环磷酰胺850mg)。11-18、12-09、12-30、2024-01-20行术后第5、6、7、8次辅助化疗,方案T(多西他赛)140mg。2023-11-17行第1次HP双靶向治疗(首剂均为负荷剂量),具体方案:帕妥珠单抗 840mg+曲妥珠单抗(汉曲优®)8mg/kg,每三周一周期;之后HP双靶方案降至常规剂量,具体方案:帕妥珠单抗 420mg+曲妥珠单抗(汉曲优®)6mg/kg,2024年10月21日结束HP双靶治疗。三、强化辅助治疗2024年12月给予奈拉替尼(汉奈佳®40mg/片)强化治疗至今。给药方案:3+4+6剂量递增给药。第一周3片/天,未出现腹泻,第二周4片/天,每天出现腹泻2-3次,第三周开始6片/天,腹泻次数增加至每天4-6次且有便血,加用江苏省中医院特色中药制剂-温脾实肠颗粒,服用一周左右,腹泻明显改善,腹泻控制在每天1-2次。后续恢复正常。专家点评点评专家简介宋波洋 教授江苏省中医院乳腺外科副主任医师2013年复旦大学附属肿瘤医院乳腺外科研修乳腺癌手术及综合治疗,师从江苏省国医名师许芝银教授。第六批全国名老中医经验继承人南京医学会普外分会甲乳学组成员江苏省中医药学会乳腺专委会委员兼秘书中国中药学会肿瘤药物研究专业委员会委员中华中医药学会外治分会青委会委员积极管理腹泻不良反应,分级应对提高治疗依从性HER-2阳性乳腺癌患者接受TKI治疗过程中,可能引起的不良反应包括腹泻、药物性肝损伤、恶心、呕吐、皮肤毒性、心脏毒性和口腔黏膜炎等,其中腹泻是为最常见的不良反应,研究提示抗 HER2-TKIs 引起的≥3级腹泻的发生率为 6%~40%[2]。腹泻可能导致脱水、电解质紊乱、营养不良、疲劳和肾功能不全等问题,均会降低患者的生存质量和用药依从性[3-4]。多项研究表明,腹泻是导致 TKIs 类药物减量或停药的主要原因,会影响临床疗效[3-7]。此外,相比其他抗 HER2 靶向治疗,抗 HER2-TKIs 药物通常需要每日服用,持续数月至数年,这无疑给患者治疗的长期管理带来挑战[4]。因此,如何有效预防和管理抗 HER2-TKIs 相关腹泻,提高患者接受抗 HER2-TKIs 治疗的依从性,成为临床关注的重点。腹泻作为抗 HER2-TKIs 治疗中最常见的不良反应,其具体机制尚未完全明确[2,8],深入探索其机制有助于发现更有效的治疗策略。有研究表明HER2-TKIs引发腹泻可能有以下机制:①肠道上皮细胞EGFR信号通路抑制导致绒毛萎缩;②氯离子通道过度激活引发分泌性腹泻;③肠道微生物群α-防御素表达异常。值得注意的是,携带UGT1A1基因多态性及基线存在慢性肠病的患者,发生3级以上腹泻的风险增加3-5倍。根据 NCI-CTCAE 的分级,并结合患者是否出现其他情况,《HER2 阳性乳腺癌 TKIs 治疗相关腹泻管理的多学科专家共识》将抗 HER2-TKIs 相关腹泻可分为“单纯性腹泻”和“复杂性腹泻”。1~2 级腹泻且无其他伴随情况的患者被归类为单纯性腹泻,可采取保守治疗措施。≥3 级腹泻患者或 1~2 级腹泻伴下述任何 1 种情况的患者:中重度绞痛、≥2 级恶心/呕吐、发热、脓毒症、中性粒细胞减少、出血、脱水,应归类为复杂性腹泻,需给予积极管理[9]。单纯性腹泻的处理 [9]对于被诊断为单纯性腹泻的患者,建议采取包括饮食和生活习惯调整、口服补液和洛哌丁胺治疗在内的保守治疗措施。在腹泻症状缓解至≤1级或基线水平后,可以考虑恢复正常剂量继续抗HER2-TKIs 治疗。复杂性腹泻的处理 [9]对于复杂性腹泻患者,建议立即暂停抗 HER2-TKI 治疗,并考虑同时暂停任何联合化疗药。患者住院应接受多学科团队评估,并密切监测生命体征及血尿便指标。治疗中应积极采取止泻措施,包括给予洛哌丁胺±复方地芬诺酯等其他止泻药物。对于存在可疑感染的患者给予广谱抗生素治疗。若患者在 48 h 内症状无明显改善建议加用奥曲肽以增强腹泻治疗效果。腹泻缓解至≤1 级或基线水平后,依据缓解难易程度进行剂量调整重新开始抗 HER2-TKIs 治疗。对于 4 级腹泻的患者应永久停用 HER2-TKIs。中医药调腹泻独具特色,精准施治彰显疗效优势中医称腹泻为“泄泻”,首载于《内经》,古将大便溏薄而势缓者称为泄,大便清稀如水而势急者称为泻,今统称为泄泻。分子靶向药物相关性腹泻亦属“泄泻”范畴。其病位在脾胃,脾阳不足、中焦失运是泄泻发生的关键病机。恶性肿瘤患者体质多虚,脏腑亏虚,《EGFR-TKI不良反应管理专家共识》指出[10],泄泻的发生与“药毒”(TKI攻伐脾胃)及“体虚”(久病脾虚、中焦不运)密切相关。TKI属攻伐之品,易伤脾阳,致中焦虚寒,运化失司,水湿下注,发为泄泻。温脾实肠颗粒出自江苏省中医院特色制剂[11],其功效为温阳健脾、调运中焦,主要用于久泻脾虚、中肠不运之证,如慢性结肠炎、肠易激综合征及肿瘤放化疗或靶向治疗相关性腹泻,症见下腹隐痛、肛门坠胀、便溏不实者。方中党参、白术、炙甘草健脾益气;炮姜炭、吴茱萸温中散寒,振奋脾阳;肉豆蔻、乌药温肾暖脾,固肠止泻;木香、厚朴行气调中,疏通壅滞;白芍柔肝缓急,防风升清止泻;神曲消食助运。全方以温补脾阳为核心,兼顾行气化湿、固肠止泻,契合脾虚中寒、气滞湿阻之病机。既往临床实践表明,温脾实肠颗粒可有效缓解靶向药物引起的腹泻,尤其适用于脾阳不足、中焦虚寒型患者。其温阳之力较强,可改善患者畏寒、腹痛等虚寒症状,同时调节肠道功能,减少便溏频次。本例患者经辨证,在奈拉替尼治疗一周内即给予温脾实肠颗粒治疗后腹泻明显好转。当然,本病例中温脾实肠颗粒的用法属于“既病防变”,用于发病之初中期,患者在奈拉替尼治疗期间出现腹泻伴下腹冷痛,辨证为脾阳虚衰,予温脾实肠颗粒治疗后症状显著缓解。中医强调“治未病”,在开始TKI治疗前,可通过体质辨识(如阳虚、气虚等)预判腹泻风险。对脾阳不足者,提前给予温脾实肠颗粒温补中焦,可降低腹泻发生率;若腹泻已发,则根据寒热虚实调整剂量或配伍(如湿热者可加黄连,气滞甚者增木香)。同时,需注重饮食调护,嘱患者忌生冷、油腻、高纤维及乳制品,宜少食多餐,以温热易消化食物为主,辅以山药、生姜等温中食材,以助药力。温脾实肠颗粒以温阳健脾、调运中焦为法,针对TKI相关性腹泻的脾虚中寒证型,体现中医“辨证施治”与“未病先防”的优势,与西医分级管理结合,可全面提升患者生活质量及治疗依从性。参考文献上下滑动查看更多内容[1] Tao X, et al. Asia Pac J Clin Oncol, 2023 Dec19(5):645-654[2] 王碧芸, 葛睿, 江泽飞, 等. 乳腺癌靶向人表皮生长因子受体2酪氨酸激酶抑制剂不良反应管理共识[J]. 中华肿瘤杂志, 2020, 42(10): 798-806.[3] Liu J, Yan S, Du J, et al. Mechanism and treatment of diarrhea associated with tyrosine kinase inhibitors[J]. Heliyon, 2024, 10(6): e27531.[4] Secombe K R, Van Sebille Y Z A, Mayo B J, et al. Diarrhea Induced by Small Molecule Tyrosine Kinase Inhibitors Compared With Chemotherapy: Potential Role of the Microbiome[J]. Integrative Cancer Therapies, 2020, 19: 1534735420928493.[5] Chan A, Moy B, Mansi J, et al. Final Efficacy Results of Neratinib in HER2-positive Hormone Receptor-positive Early-stage Breast Cancer From the Phase III ExteNET Trial[J]. Clinical Breast Cancer, 2021, 21(1): 80-91.e7.[6] Frankel C, Palmieri F M. Lapatinib Side-Effect Management[J]. Clinical Journal of Oncology Nursing, 2010, 14(2): 223-233.[7] Xu B, Yan M, Ma F, et al. Pyrotinib plus capecitabine versus lapatinib plus capecitabine for the treatment of HER2-positive metastatic breast cancer (PHOEBE): a multicentre, open-label, randomised, controlled, phase 3 trial[J]. The Lancet Oncology, 2021, 22(3): 351-360.[8] Wu J, Jiang Z, Liu Z, et al. Neoadjuvant pyrotinib, trastuzumab, and docetaxel for HER2-positive breast cancer (PHEDRA): a double-blind, randomized phase 3 trial[J]. BMC Medicine, 2022, 20(1): 498.[9],中国抗癌协会乳腺肿瘤整合康复专业委员会,HER2 阳性乳腺癌 TKIs 治疗相关腹泻管理的多学科专家共识,中国肿瘤临床 2025 年第 52 卷[10]王碧芸,葛睿,江泽飞,等.乳腺癌靶向人表皮生长因子受体2酪氨酸激酶抑制剂不良反应管理共识[J].中华肿瘤杂志,2020,42(10):798-806.[11]朱吾元. 温脾实肠法组方治疗脾阳不足型泄泻机理的初步研究[D]. 南京中医药大学, 2011(来源:《肿瘤瞭望》编辑部)声 明凡署名原创的文章版权属《肿瘤瞭望》所有,欢迎分享、转载。本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
2025-04-07
Subcutaneous (SC) amivantamab offers patients greater convenience, reducing administration time from hours to minutes and with a five-fold reduction in infusion-related reactions compared to the IV formulation
1
European Commission (EC) approval based on positive results from the Phase 3 PALOMA-3 study
1
BEERSE, Belgium I April 07, 2025 I
Janssen-Cilag International NV, a Johnson & Johnson company, today announced that the European Commission (EC) has approved an extension of marketing authorisation for a subcutaneous (SC) formulation of RYBREVANT
®
(amivantamab), in combination with LAZCLUZE
®
(lazertinib) for the first-line treatment of adult patients with advanced non-small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 19 deletions (ex19del) or exon 21 L858R substitution mutations, and as a monotherapy for the treatment of adult patients with advanced NSCLC with activating EGFR exon 20 insertion mutations after failure of platinum-based therapy. For these indications, it is recommended that SC amivantamab is administered weekly from Weeks 1 to 4 (total of four doses), then every two weeks starting at Week 5 onwards.
1
This approval follows the
recent presentation
of final overall survival (OS) results from the Phase 3 MARIPOSA study (
NCT04487080
), at the 2025 European Lung Cancer Congress (ELCC), showing statistically superior OS with intravenous (IV) amivantamab plus lazertinib versus osimertinib monotherapy in the first-line treatment of patients with advanced EGFR ex19del or L858R substitution mutated NSCLC (hazard ratio [HR], 0.75; 95 percent Confidence Interval [CI], 0.61-0.92; P<0.005).
2
“While great strides have been made in the treatment of EGFR-mutated non-small cell lung cancer, a critical need still exists for treatment approaches that are not only effective but also more convenient for patients, while optimising experience in the clinic,” said Silvia Novello, M.D., Ph.D., Professor of Medical Oncology in the Oncology Department at San Luigi Hospital in Orbassano, University of Turin, Italy.* “The approval of subcutaneous amivantamab will have a meaningful impact on clinical practice, offering patients greater convenience and an improved treatment experience, without compromising on the well-established efficacy of intravenous amivantamab.”
The EC approval is supported by positive results from the Phase 3 PALOMA-3 study (
NCT05388669
), which evaluated non-inferiority of pharmacokinetics (PK) in addition to efficacy and safety of SC amivantamab (administered via manual injection) compared to IV amivantamab (the already approved route of administration), both in combination with lazertinib, in patients with EGFR-mutated advanced or metastatic NSCLC after disease progression on osimertinib and platinum-based chemotherapy.
1,3
The study demonstrated that SC amivantamab was non-inferior to IV amivantamab, meeting both co-primary PK endpoints as measured by amivantamab levels in the blood (C
trough
and area under the serum concentration time curve from Cycle 2 day 1 to 15).
1
At a median follow-up of 7 months, the overall response rate (a secondary endpoint) was 30 percent (95 percent confidence interval [CI], 24–37) in the SC arm and 33 percent (95 percent CI, 26–39) for IV (relative risk, 0.92; 95 percent CI, 0.70–1.23;
P
=0.001), meeting the non-inferiority criteria.
1
Administration time for SC amivantamab was approximately five minutes, and results showed a five-fold reduction in infusion-related reactions (IRRs) compared to IV administration.
1
These results were featured as an oral presentation at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting and published in the
Journal of Clinical Oncology
.
1,4
“The approval of subcutaneous amivantamab represents a welcome improvement of the treatment experience for both patients living with EGFR-mutated advanced non-small cell lung cancer and the healthcare professionals who support them,” said Henar Hevia, PhD., Senior Director, EMEA Therapeutic Area Lead, Oncology, Johnson & Johnson Innovative Medicine. “This advancement presents an important opportunity to reduce the treatment burden, improve quality of life and give patients more time to focus on what truly matters to them.”
The rate of IRRs for patients treated with SC amivantamab combined with lazertinib was shown to be approximately five-fold lower than that observed with the IV formulation (13 percent vs 66 percent, respectively).
1
The majority of IRRs were grades 1 and 2, with one patient experiencing a grade 3 IRR in the SC arm.
1
Preventive blood thinning (prophylactic anticoagulation) was used in most patients in the PALOMA-3 study.
1
Patients receiving prophylactic anticoagulation had lower rates of venous thromboembolic events (VTEs) (10 percent) than those who did not receive prophylaxis (21 percent).
1
Furthermore, VTE incidence was numerically lower in the SC arm vs the IV arm (9 percent vs 14 percent) regardless of anticoagulation status.
1
Severe bleeding risk (grade 3 to 4) was low among patients receiving anticoagulants in both the SC (2 percent) and IV (0.6 percent) arms.
1
Otherwise, the overall safety profile of SC amivantamab is consistent with the known profile of IV administration.
1
The most common all-grade adverse events of any cause that occurred for SC amivantamab compared to IV, were paronychia (54 percent vs 51 percent), hypoalbuminaemia (47 percent vs 37 percent) and rash (46 percent vs 43 percent), respectively.
1
“At Johnson & Johnson, we are dedicated to patient-centered innovation in our mission to address the critical unmet needs in lung cancer treatment and care,” said Joshua Bauml, M.D., Vice President, Lung Cancer Disease Area Stronghold Leader, Johnson & Johnson Innovative Medicine. “Our ongoing focus on advancing the clinical development programme for amivantamab reflects our confidence in its potential to become a standard of care for EGFR-and MET-driven lung cancer.”
#ENDS#
About Amivantamab
Amivantamab is a fully-human EGFR-MET bispecific antibody that acts by targeting tumours with activating and resistance EGFR mutations and MET mutations and amplifications, and by harnessing the immune system.
5,6,7,8
The European Commission (EC) has approved amivantamab in the following indications:
8
Intravenous amivantamab:
Subcutaneous amivantamab:
The recommended dose regimen for SC amivantamab for these indications is 1600 mg (2240 mg for body weight ≥80kg) administered weekly from Weeks 1 to 4 (total of four doses), then every two weeks starting at Week 5 onwards (Q2W).
8
When given in combination with lazertinib, it is recommended to administer SC amivantamab any time after lazertinib when given on the same day.
8
Subcutaneous amivantamab is co-formulated with recombinant human hyaluronidase PH20 (rHuPH20), Halozyme’s ENHANZE
®
drug delivery technology.
1
For a full list of adverse events and information on dosage and administration, contraindications and other precautions when using amivantamab, please refer to the
Summary of Product Characteristics
.
8
▼ In line with EMA regulations for new medicines, amivantamab is subject to additional monitoring.
About Lazertinib
In 2018, Janssen Biotech, Inc. entered into a license and collaboration agreement with Yuhan Corporation for the development of lazertinib. Lazertinib is an oral, third-generation, brain-penetrant EGFR tyrosine kinase inhibitor (TKI) that targets both the T790M mutation and activating EGFR mutations while sparing wild-type EGFR.
9
An analysis of the efficacy and safety of lazertinib from the Phase 3 study LASER301 was published in
The Journal of Clinical Oncology
in 2023.
9
In January 2025, the European Commission EC approved a marketing authorisation for lazertinib, in combination with amivantamab, for the first-line treatment of adult patients with advanced NSCLC with EGFR exon 19 deletion or exon 21 L858R substitution mutations.
10
For a full list of adverse events and information on dosage and administration, contraindications and other precautions when using lazertinib, please refer to the
Summary of Product Characteristics
.
11
▼ In line with EMA regulations for new medicines, lazertinib is subject to additional monitoring.
About PALOMA-3
PALOMA-3 (
NCT05388669
), which enrolled 418 patients, is a randomised, open-label Phase 3 study evaluating the non-inferiority of pharmacokinetics (PK), efficacy and safety of subcutaneous amivantamab (administered via manual injection) combined with lazertinib compared to IV amivantamab and lazertinib in patients with EGFR-mutated advanced or metastatic NSCLC after progression on osimertinib and platinum-based chemotherapy.
1
The co-primary PK endpoints of the study were trough concentration (C
trough
on Cycle [C] 2 Day [D] 1 or C4D1) and C2 area under the curve (AUCD1-D15).
1
Key secondary endpoints were objective response rate (ORR) and progression-free survival (PFS).
1
Overall survival was a predefined exploratory endpoint.
1
Prophylactic anticoagulation was recommended for the first four months of treatment.
1
About Non-Small Cell Lung Cancer
In Europe, it is estimated that 484,306 people were diagnosed with lung cancer in 2022.
12
NSCLC accounts for 85 percent of all lung cancer cases.
13
Lung cancer is Europe’s biggest cancer killer, with more deaths than breast cancer and prostate cancer combined.
12
The main subtypes of NSCLC are adenocarcinoma, squamous cell carcinoma and large cell carcinoma.
13
Among the most common driver mutations in NSCLC are alterations in EGFR, which is a receptor tyrosine kinase controlling cell growth and division.
13,14
EGFR mutations are present in 10 to 15 percent of Western patients with NSCLC with adenocarcinoma histology and occur in 40 to 50 percent of Asian patients.
15,16,17,18
EGFR ex19del or EGFR exon 21 L858R mutations are the most common EGFR mutations.
19
The five-year survival rate for all patients with advanced NSCLC and EGFR mutations treated with EGFR TKIs is less than 20 percent and between 25-32 percent of patients receiving the current first-line standard of care, osimertinib, do not survive long enough to reach second-line treatment.
20,21,22,23,24,25,26
EGFR exon 20 insertion (ex20ins) mutations are the third most prevalent activating EGFR mutation.
27
Patients with EGFR ex20ins mutations have a real-world five-year OS of eight percent in the frontline setting, which is worse than patients with EGFR ex19del or L858R mutations, who have a real-world five-year OS of 19 percent.
21
About Johnson & Johnson
At Johnson & Johnson, we believe health is everything. Our strength in healthcare innovation empowers us to build a world where complex diseases are prevented, treated, and cured, where treatments are smarter and less invasive, and solutions are personal. Through our expertise in Innovative Medicine and MedTech, we are uniquely positioned to innovate across the full spectrum of healthcare solutions today to deliver the breakthroughs of tomorrow and profoundly impact health for humanity.
Learn more at
https://innovativemedicine.jnj.com/emea/
. Follow us at
http://www.linkedin.com/company/jnj-innovative-medicine-emea
. Janssen-Cilag International NV, Janssen Research & Development, LLC, Janssen Biotech, Inc. and Janssen-Cilag, S.A. are Johnson & Johnson companies.
References
1
Leighl NB et al. Subcutaneous Versus Intravenous Amivantamab, Both in Combination With Lazertinib, in Refractory Epidermal Growth Factor Receptor–Mutated Non–Small Cell Lung Cancer: Primary Results From the Phase III PALOMA-3 Study.
ASCO Journal of Clinical Oncology
. 2024;42(3):3593-3605.
2
Yang J, et al. Amivantamab Plus Lazertinib vs Osimertinib in First-line (1L) EGFR-mutant (EGFRm) Advanced NSCLC: Final Overall Survival (OS) from the Phase 3 MARIPOSA Study. 2025 European Lung Cancer Congress. March 26, 2025.
3
ClinicalTrials.gov. A Study of Lazertinib With Subcutaneous Amivantamab Compared With Intravenous Amivantamab in Participants With Epidermal Growth Factor Receptor (EGFR)-Mutated Advanced or Metastatic Non-small Cell Lung Cancer (PALOMA-3).
https://clinicaltrials.gov/ct2/show/NCT05388669
. Accessed April 2025.
4
Leighl N, et al. Subcutaneous Amivantamab Plus Lazertinib Vs Intravenous Amivantamab Plus Lazertinib In EGFR-mutated, Advanced Non-small Cell Lung Cancer (NSCLC): PALOMA-3, A Phase 3, Global, Randomized, Controlled Trial. 2024 American Society of Clinical Oncology Annual Meeting. May 31, 2024.
5
Moores SL, et al. A Novel Bispecific Antibody Targeting EGFR and cMet Is Effective against EGFR Inhibitor-Resistant Lung Tumors.
Cancer Res
2016;76(13)(suppl 27216193):3942-3953.
6
Grugan KD, et al. Fc-mediated activity of EGFR x c-Met bispecific antibody JNJ-61186372 enhanced killing of lung cancer cells.
Mabs
. 2017;9(1):114-126.
7
Yun J, et al. Antitumor Activity of Amivantamab (JNJ-61186372), an EGFR–MET Bispecific Antibody, in Diverse Models of EGFR Exon 20 Insertion–Driven NSCLC.
Cancer Discov
. 2020;10(8):1194-1209.
8
European Medicines Agency. Amivantamab Summary of Product Characteristics. January 2025. Available at:
https://www.ema.europa.eu/en/documents/product-information/rybrevant-epar-product-information_en.pdf
. Accessed: April 2025.
9
Cho, BC, et al. Lazertinib versus gefitinib as first-line treatment in patients with
EGFR
-mutated advanced non-small-cell lung cancer: Results From LASER301. J Clin Oncol. 2023;41(26):4208-4217.
10
Innovativemedicine.jnj.com/EMEA. European Commission approves LAZCLUZE®▼ (lazertinib) in combination with RYBREVANT®▼ (amivantamab) for the first-line treatment of patients with EGFR-mutated advanced non-small cell lung cancer. Available at:
https://www.jnj.com/media-center/press-releases/european-commission-approves-lazcluze-lazertinib-in-combination-with-rybrevant-amivantamab-for-the-first-line-treatment-of-patients-with-egfr-mutated-advanced-non-small-cell-lung-cancer
. Accessed: April 2025
11
European Medicines Agency. Lazcluze. January 2025. Available at:
https://www.ema.europa.eu/en/medicines/human/EPAR/lazcluze
. Accessed April 2025.
12
Global Cancer Observatory. Cancer Today. Available at:
https://gco.iarc.fr/en
. Accessed April 2025.
13
Zappa C, et al. Non-small cell lung cancer: current treatment and future advances.
Transl Lung Cancer Res
. 2016;5(3):288–300.
14
Wee P, Wang Z. Epidermal Growth Factor Receptor Cell Proliferation Signaling Pathways. Cancers. 2017;9(5):52.
15
Pennell NA, et al. A phase II trial pf adjuvant erlotinib in patients with resected epidermal growth factor receptor-mutant non-small cell lung cancer.
J Clin Oncol
. 2019;37(7);97-104.
16
Burnett H, et al. Epidemiological and clinical burden of EGFR exon 20 insertion in advanced non-small cell lung cancer: a systematic literature review. Abstract presented at: World Conference on Lung Cancer Annual Meeting; January 29, 2021; Singapore.
17
Zhang YL, et al. The prevalence of EGFR mutation in patients with non-small cell lung cancer: a systematic review and meta-analysis.
Oncotarget
. 2016;7(48):78985-78993.
18
Midha A, et al. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: a systematic review and global map by ethnicity.
Am J Cancer Res
. 2015;5(9):2892-2911.
19
American Lung Association. EGFR and Lung Cancer. Available at:
https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/symptoms-diagnosis/biomarker-testing/egfr
. Accessed April 2025.
20
Lin JJ, et al. Five-Year Survival in EGFR-Mutant Metastatic Lung Adenocarcinoma Treated with EGFR-TKIs. J Thorac Oncol 2016 Apr;11(4):556-65.
21
Girard N, et al. Comparative clinical outcomes for patients with NSCLC harboring EGFR exon 20 insertion mutations and common EGFR mutations. Abstract presented at: World Conference on Lung Cancer Annual Meeting; January 29, 2021; Singapore.
22
Shao J et al. The number of brain metastases predicts the survival of non-small cell lung cancer patients with EGFRR mutation status.
Cancer Rep (Hoboken).
2022;5(9): e1550.
23
Achrol A et al. Brain metastases.
Nat Rev Dis Primers
. 2019;17(5): 5.
24
Rangachari D et al. Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small-cell lung cancers.
Lung Cancer
. 2015;88(1): 108-111.
25
Nieva J, et al. A real-world (rw) observational study of long-term survival (LTS) and treatment patterns after first-line (1L) osimertinib in patients (pts) with epidermal growth factor receptor (EGFR) mutation-positive (m) advanced non-small cell lung cancer (NSCLC).
Ann Oncol
. 2023;34, S774.
26
Girard N, Leighl NB, Ohe Y, et al. Mortality among EGFR-mutated advanced NSCLC patients after starting frontline osimertinib treatment: a real-world, US attrition analysis. Presented at: the European Lung Cancer Congress; March 29-April 1, 2023; Copenhagen, Denmark. Poster 19P.
27
Arcila, M. et al. EGFR exon 20 insertion mutations in lung adenocarcinomas: prevalence, molecular heterogeneity, and clinicopathologic characteristics. Mol Cancer Ther. 2013 Feb; 12(2):220-9.
SOURCE:
Johnson & Johnson
临床结果临床3期ASCO会议上市批准引进/卖出
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
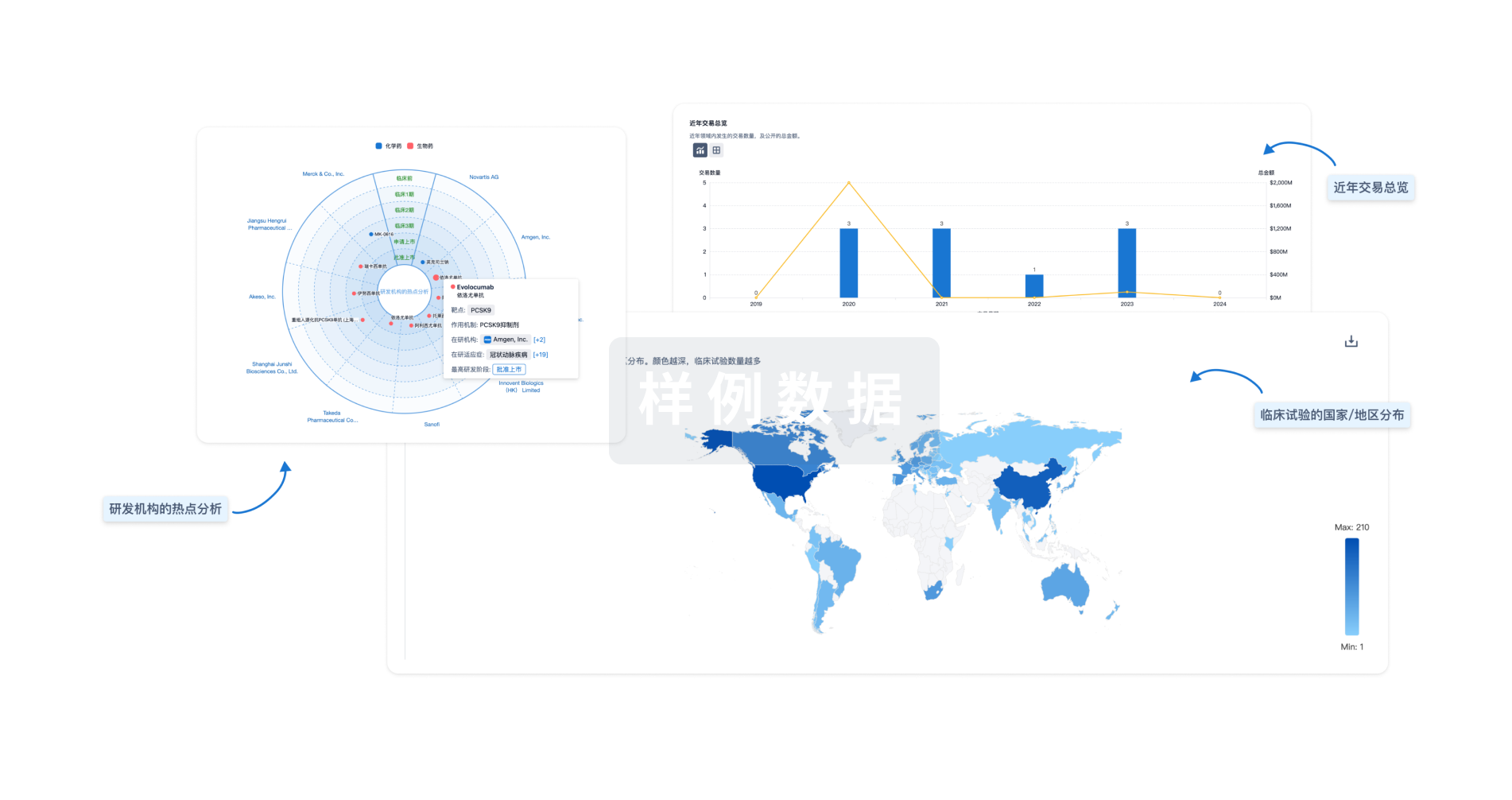
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



