预约演示
更新于:2025-05-07
EDA
更新于:2025-05-07
基本信息
别名 Ectodermal dysplasia protein、ectodysplasin A、Ectodysplasin-A + [15] |
简介 Cytokine which is involved in epithelial-mesenchymal signaling during morphogenesis of ectodermal organs. Functions as a ligand activating the DEATH-domain containing receptors EDAR and EDA2R (PubMed:11039935, PubMed:27144394, PubMed:34582123, PubMed:8696334). May also play a role in cell adhesion (By similarity).
Binds only to the receptor EDAR, while isoform 3 binds exclusively to the receptor EDA2R.
Binds only to the receptor EDA2R. |
关联
1
项与 EDA 相关的药物靶点 |
作用机制 EDA刺激剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
4
项与 EDA 相关的临床试验NCT04980638
A Prospective, Open-label, Genotype-match Controlled, Multicenter Clinical Trial to Investigate the Efficacy and Safety of Intra-amniotic ER004 as a Prenatal Treatment for Male Subjects With XLHED
This is an open-label, prospective, genotype-match controlled for primary estimand, non randomized, multicenter, international Phase 2 clinical trial designed to investigate the efficacy and safety of ER004 administered intraamniotically as a treatment for unborn XLHED male subjects.
开始日期2022-04-26 |
申办/合作机构  EspeRare Foundation EspeRare Foundation [+2] |
NCT01992289
Extension Study of XLHED-Affected Male Subjects Treated With EDI200 in Protocol ECP-002
The goal of the ECP-002e extension study is to continue the evaluation of all EDI200-treated ECP-002 subjects up to age 10 yrs. No additional study drug administration is planned. The efficacy evaluations will incorporate growth and development parameters, frequency of infections and hospitalizations, and age-appropriate assessments of ectoderm-derived organ function. The safety evaluations will include physical examinations, adverse events and concomitant medication documentation, and laboratory testing. Funding Source - FDA OOPD
开始日期2014-03-01 |
申办/合作机构 |
NCT01775462
A Phase 2 Open-label, Dose-escalation Study to Evaluate the Safety, Pharmacokinetics, Immunogenicity and Pharmacodynamics/Efficacy of EDI200, an EDA-A1 Replacement Protein, Administered to Male Infants With X-Linked Hypohidrotic Ectodermal Dysplasia (XLHED)
This Phase 2 first-in-neonate EDI200 study will enroll treatment-naïve, XLHED-affected male newborns in the first two weeks of life. All subjects will meet entry criteria including documentation of an Ectodysplasin (EDA) mutation associated with XLHED. Following Baseline evaluations, EDI200 dosing will be initiated between day-of-life 2 and 14, with each study subject receiving 2 doses/week for a total of 5 doses. The study will enroll subjects in two cohorts with subjects in cohort 1 dosed at 3 mg/kg/dose, associated with partial efficacy, and cohort 2 dosed at 10 mg/kg/dose where enhanced efficacy was demonstrated in the most relevant preclinical model. Given the challenge of identifying families where the subject is yet to be born, it is expected that cohort size and time for recruitment will be variable.
开始日期2013-04-01 |
申办/合作机构 |
100 项与 EDA 相关的临床结果
登录后查看更多信息
100 项与 EDA 相关的转化医学
登录后查看更多信息
0 项与 EDA 相关的专利(医药)
登录后查看更多信息
3,080
项与 EDA 相关的文献(医药)2025-07-30·Rapid communications in mass spectrometry : RCM
HR-MS Analysis of the Covalent Binding of Edaravone to 5-Formylpyrimidine Bases and a DNA Oligonucleotide Containing a 5-Formylcytidine Residue.
Article
作者: Thuru, Xavier ; Regnault, Romain ; Bailly, Christian ; Kouach, Mostafa ; Goossens, Jean-François ; Goossens, Laurence
2025-06-01·Life Sciences
Edaravone targets PDGFRβ to attenuate VSMC phenotypic transition
Article
作者: Estau, Dannya ; Li, Zijian ; Tang, Xueqing ; Huang, Xiaoru
2025-05-01·International Immunopharmacology
Edaravone alleviates Pseudomonas aeruginosa associated-acute lung injury by inhibiting inflammation and promoting anti-microbial peptide production
Article
作者: Song, Yuanlin ; Xu, Jian ; Wang, Jian ; Song, Juan ; Li, Yufan ; Chen, Cuicui ; Tong, Lin ; Zeng, Yingying
8
项与 EDA 相关的新闻(医药)2025-03-14
·生物谷
本文研究结果表明,靶向作用外异蛋白A2受体或许代表了一种非常有前途的药物性策略,其或能减缓机体衰老相关表型的发展。
如今科学家们进行了大量努力识别出了能作为机体衰老生物标志物的特征,然而,开发旨在减少衰老对机体有害影响的基于药物的干预措施或许是缺乏的,这在很大程度上归咎于组织特异性、性别相关的差异,以及在识别可操控靶点上的难度,这或许对于科学家们而言仍然是一大挑战。
近日,一篇发表在国际杂志Nature Communications上题为“Increased ectodysplasin-A2-receptor EDA2R is a ubiquitous hallmark of aging and mediates parainflammatory responses”的研究报告中,来自意大利米兰比科卡大学等机构的科学家们通过研究发现一种“炎性”基因或会加速机体衰老,文章中,研究人员识别出了一种新型基因或许是导致机体衰老的关键因素,相关研究结果有望帮助开发新型抗衰老疗法。
年龄相关的疾病与机体炎症密切相关,慢性炎症(尽管程度较低)会导致包括心血管疾病、糖尿病、神经变性和肌肉减少症等多种疾病,其严重影响着机体健康和寿命。这项研究中,研究人员通过联合研究提出了外异蛋白A2受体(EDA2R,Ectodysplasin A2 Receptor)在这一过程中发挥作用的开创性见解。EDA2R是肿瘤坏死因子受体家族的重要成员,其能特异性地结合EDA-A2蛋白,且会参与细胞凋亡(细胞死亡)和机体的炎性信号转导过程。
通过分析来自基因型-组织表达数据库(Genotype-Tissue Expression database)中的数据,研究人员发现了EDA2R表达和机体衰老之间令人惊讶与组织无关的关联性;在多种不同的人类器官和组织中,EDA2R一直是与人类机体衰老相关的顶级基因(top gene)。随后研究人员在啮齿类动物中进一步验证了这些研究发现,而且加速衰老的效果尤为明显,EDA2R表达水平的升高与炎症和血管功能异常(这些是机体衰老的标志)相关的转录改变有关。
早衰模型中EDA2R的表达与衰老和上调的跨物种关联性
然而,研究人员通过研究发现,EDA2R的功能并不仅仅是机体慢性炎症的生物标志物,而是机体衰老过程本身的潜在驱动因素。在细胞模型中,EDA2R的过表达会诱发炎性信号并破坏肌肉的健康通路,这就能模拟衰老驱动的肌肉减少症、肌肉质量和力量的进行性缺失的关键特征,相反,对EDA2R的抑制或能减缓这些有害影响的发生。为了扩展研究者的分析,他们还研究了来自5,228名个体机体的血液样本,同时揭示了EDA2R的表达与全身性炎症之间的强烈相关性,比如C反应蛋白水平的升高等。
研究者Akhmetov说道,这些研究结果表明,EDA2R/EDA-A2在介导年龄相关的炎症和机体组织退行性过程中发挥着关键作用。靶向作用EDA2R或为管理年龄相关的疾病能开辟新的路径,包括肌肉减少症、心血管疾病、神经变性疾病和代谢性疾病等。本文研究结果或能为科学家们未来的研究奠定一定的基础,能帮助开发新型干预措施来调节EDA2R信号并减少衰老所产生的影响。
目前有研究证据表明,减少EDA2R的水平或许是有益的。有文献和初步研究数据表明,卡路里限制、体育锻炼、膳食补充银杏以及服用广泛使用的血糖调节性药物二甲双胍或能降低动物模型和人类受试者机体中的EDA2R水平,这或许就能为减缓衰老相关的炎性过程并增强机体总体的健康结局提供一种新的策略。
综上,本文研究结果表明,靶向作用外异蛋白A2受体或许代表了一种非常有前途的药物性策略,其或能减缓机体衰老相关表型的发展。(生物谷Bioon.com)
参考文献:
Barbera, M.C., Guarrera, L., Re Cecconi, A.D. et al. Increased ectodysplasin-A2-receptor EDA2R is a ubiquitous hallmark of aging and mediates parainflammatory responses. Nat Commun 16, 1898 (2025). doi:10.1038/s41467-025-56918-3
临床结果临床1期
2024-11-25
·生物谷
全球大约有35亿人因为各种口腔疾病而苦恼,其中牙齿缺失尤其常见。与那些幸运的鲨鱼相比——它们可以一生中无数次更换牙齿,我们人类只有两次机会:先是乳牙,然后是恒牙。一旦恒牙“不幸离开”,剩下的选择似乎就只有种植牙或者戴假牙了。
但是,这些传统方法不仅成本高昂,过程复杂,还有可能带来感染、排斥等麻烦。那么,有没有什么办法可以让我们的牙齿像鲨鱼那样“重生”呢?答案是:科学家们正在努力让这变成现实!
基因调控:用小干扰RNA敲除USAG-1
2021年,高桥胜团队在《Scientific Reports》发表了一项题为"Local application of Usag‑1 siRNA can promote tooth regeneration in Runx2‑deficient mice"的研究,他们发现了一个叫做Usag‑1的基因,这个基因在牙齿发育过程中扮演着“刹车”的角色。
研究中,他们聚焦于Usag‑1(Uterine sensitization-associated gene-1)这一在牙齿发育中起抑制作用的基因,同时结合研究了Runx2基因的功能。研究人员通过设计两种小干扰RNA(siRNA)分子,分别针对Usag‑1和Runx2基因进行了干预实验,探索它们在牙齿发育中的作用。
首先,他们在小鼠牙齿发育上皮细胞系mHAT9d中转染了两种siRNA,发现Usag‑1基因敲低显著促进了牙齿发育,而Runx2基因敲低则起到抑制作用。随后,研究团队将经过siRNA处理的下颌骨移植到小鼠肾囊,并通过组织学分析和3D微计算机断层扫描(3D micro-CT)技术,观察到Usag‑1 siRNA处理显著增加了形成的牙齿结构数量,而Runx2 siRNA处理则抑制了牙齿发育。
Usag‑1基因沉默挽救了Runx2基因沉默所抑制的牙齿形成
(图片来源:Scientific Reports 2021)
更重要的是,该研究还在Runx2基因敲除小鼠模型中进一步验证了Usag‑1 siRNA的作用。尽管Runx2基因缺失会抑制牙齿发育,但通过局部应用Usag‑1 siRNA,研究团队成功部分恢复了Runx2基因敲除小鼠的牙齿发育。这一发现表明,USAG-1在牙齿再生中扮演了重要角色,为基因治疗提供了全新的潜在靶点,同时也为缺牙患者带来了切实可行的治疗希望。
抗体治疗:中和USAG-1促进牙齿发育
同年,高桥胜团队在《Science Advances》发表的另一项题为“Anti–USAG-1 therapy for tooth regeneration through enhanced BMP signaling”的研究,将牙齿再生研究推向了新高度。这次,他们采用了单克隆抗体技术,探索通过中和USAG-1蛋白以促进牙齿发育的可能性。
他们发现,USAG-1蛋白能够通过与骨形态发生蛋白(BMP)信号通路相互作用,抑制牙齿的自然生长,而特定的单克隆抗体可以阻断这种作用,显著改善牙齿再生效果。
USAG-1中和抗体使EDA1突变小鼠牙齿恢复和全牙再生
(图片来源:Science Advances 2021)
研究团队筛选出五种USAG-1中和抗体,分别分析了它们对BMP和Wnt信号通路的影响、与USAG-1蛋白的结合能力,以及中和USAG-1功能的效率。结果表明,这些抗体不仅能够解除USAG-1对BMP和Wnt信号的抑制,还能够显著促进牙齿发育。在小鼠和非啮齿动物雪貂模型中,这些抗体在恢复缺失牙齿以及诱导超数牙齿形成方面表现出卓越的效果。例如,在基因突变导致牙齿缺失的小鼠模型中,系统性给予USAG-1抗体不仅恢复了牙齿数量,还显著改善了牙齿的生长质量;而在正常雪貂模型中,抗体还能促进额外牙齿的生长,为牙齿再生治疗的普适性提供了重要佐证。
USAG-1中和抗体促进非啮齿类动物雪貂上颌额外牙齿的生长
(图片来源:Science Advances 2021)
为进一步揭示抗体如何实现其作用,团队对两种具有代表性的USAG-1中和抗体进行了表位图谱分析,确定了它们结合USAG-1蛋白的关键区域。这一研究不仅为理解抗体作用机制提供了新见解,也为未来药物设计提供了坚实基础。通过抗体治疗手段,研究团队成功实现了从基因调控到功能干预的跨越,为牙齿再生治疗带来了更多可能性!
牙齿再生技术的历史与未来展望
基于近二十年的研究,2023年,该团队在《Regenerative Therapy》上发表了一篇题为"Advances in tooth agenesis and tooth regeneration"的综述性文章,对牙齿再生技术的进展进行了全面回顾。
他们提出了一个令人兴奋的概念——“第三套牙齿(third dentition)”。这意味着,未来我们或许可以通过失活USAG-1基因,让成年人也能拥有第三次长牙的机会。这不仅仅是对牙齿发育过程中先天性缺失问题的解决,更是对晚期牙齿再生的一次革命。
研究指出,通过失活USAG-1基因,科学家不仅能显著改善早期牙齿发育中的先天性缺失问题,还能够恢复晚期牙齿发育,甚至在双基因敲除小鼠中成功诱导了新牙形成。这些成果为理解牙齿再生的分子机制提供了关键线索。
此外,综述还指出,未来的研究需进一步明确USAG-1的致病变异、关键相互作用基因以及蛋白质功能。这些因素不仅有助于开发更有效的生物标志物,还能推动牙齿再生相关药物的个性化设计。借助下一代测序、质谱和高分辨率成像等技术,科学家能够精准识别牙齿缺失的遗传变异,从而改善早期诊断与治疗方案。
牙齿再生研究进展的时间线
(图片来源:Regenerative Therapy 2023)
牙齿再生——从梦想走向现实!
更为振奋的是,基于这些研究成果的首个人体试验已经开展。今年9月至2026年8月,京都大学医院计划在30名30至64岁之间、至少缺失一颗臼齿的男性患者中,测试USAG-1抗体药物的安全性与有效性。这种药物通过静脉注射,激活BMP信号传导,显著促进牙齿再生,且在动物试验中未见明显副作用。如果试验成功,这款牙齿再生药物有望在2030年正式上市,为全球数十亿牙齿缺失患者提供一种革命性的治疗手段!
从基因调控到抗体治疗,从分子靶点发现到临床转化,该团队的研究已经为牙齿再生领域奠定了坚实基础。这项技术不仅安全、自然,还可能彻底改变现有的口腔治疗模式。未来的某一天,当牙齿缺失不再需要繁琐的种植牙手术,而是通过一剂药物让新牙自然生长,所有患者的生活质量都将得到显著提升。
科学的进步正在将“牙齿再生”从梦想变为现实。我们有理由相信,随着研究的不断深入,这项技术预期在不久的将来造福更多患者,为人类健康书写新的篇章!
参考文献:
[1] Mishima S, Takahashi K, Kiso H, et al. Local application of Usag-1 siRNA can promote tooth regeneration in Runx2-deficient mice. Sci Rep. 2021;11(1):13674.
[2] Murashima-Suginami A, Kiso H, Tokita Y, et al. Anti-USAG-1 therapy for tooth regeneration through enhanced BMP signaling. Sci Adv. 2021;7(7):eabf1798.
[3] Ravi V, Murashima-Suginami A, Kiso H, et al. Advances in tooth agenesis and tooth regeneration. Regen Ther. 2023;22:160-168.
撰文 | Shawn
编辑 | lcc
部分文字来源于网络,本文仅用于分享,转载请注明出处。若有侵权,请联系微信:bioonSir 删除或修改!
精彩推荐:
1、晚睡晚起,但睡够8小时,也有害健康吗?Nature研究回答:是的!生物钟紊乱会导致脂肪代谢异常,与调控昼夜节律的IL-17相关
2、为什么初恋最难忘?我们对第一个出场的人印象更好?最新研究:人的「出场顺序」很重要,人们对后来遇到的个体的描述会变得负面
3、Nature重磅:患癌8年,她用自己实验室培养的病毒,治好了自身的癌症!并顺手发了篇SCI
4、被子越重,睡得越香!最新研究显示:盖上7kg左右的厚被子,显著改善睡眠!原因竟是...
5、你知道「葛根」能减肥吗?最新Nature研究:葛根素可以调节DMV神经元活性,使小肠绒毛长度缩短,减少脂肪吸收面积,实现减肥效果
点击下方「阅读原文」,前往生物谷官网查询更多生物相关资讯~
siRNA临床研究基因疗法
2024-07-22
·药智网
有目共睹,ADC药物已是继PD-1单抗肿瘤药之后,肿瘤研发领域的最大热点。而随着越来越多ADC药物的持续上市,全球ADC市场规模也在快速增长。但是,ADC药物逐渐内卷的竞争趋势下,在价值百亿的ADC市场赛道中,如何跑出差异化,却成为每个玩家都迫切面临的难题。
为此,有的企业选择在靶向分子上下功夫,避开抗体,以多肽、小分子等新的靶向载体为突破,诞生了PDC、SMDC等区别于ADC的技术类型;而另一些企业却将差异化目光放到了有效载荷之上,利用有效载荷的多样化来凸显差异化。
比如以放射性核素、PROTAC分子作为有效载荷的新技术,以各种“药效蛋白”作为治疗性payload的大胆尝试。
蛋白效应偶联物优势明显
所谓蛋白效应偶联物,即将药效蛋白(细胞因子、蛋白毒素与免疫细胞)与靶向性分子链接在一起,在原来药效蛋白的基础上增加靶向性或其他,减少药效蛋白的系统性毒性,其原理上与熟知的ADC机理相似,在兼具了药效蛋白与偶联药物的特点的同时,也有其特殊优势:
相较传统药效蛋白,蛋白效应偶联物理论上可以拥有更强的有效性、更低的毒副作用、更特异性的靶点与更高的效价,当其与化疗、放疗等其他抗肿瘤治疗方式结合时,抗肿瘤特性还会显著增强。
而相较传统ADC,蛋白效应偶联物可以拥有更强的靶向毒性,更广的适应范围,可以应用于更多非肿瘤领域,如多数自免疾病。
现在来看,靶向分子与药效蛋白发挥协同效应,明显可以产生1+1>2的作用,达成更高效的治疗需求。但同时,由于药效蛋白与靶向分子的诸多链接限制,对于蛋白偶联物领域而言,也有不少值得进一步研究的内容。
细胞因子
药效蛋白偶联物的开始
就现阶段而言,药效蛋白作为效应分子在偶联药物领域的例子并没有想象中那么多,近年来陆续出现的蛋白毒素、细胞因子与免疫细胞已是较为前沿的研究成果,而其中又以“细胞因子偶联物”的研究最具代表性。
过去几十年,随着细胞因子的持续发现,其被广泛应用于抗肿瘤与抗感染方面,但与此同时,应用越广,其凸显出的局限性也越强,比如半衰期短,治疗窗口窄,毒副作用大等,这普遍存在于多数药效蛋白中。
而抗体偶联细胞因子(immunocytokine),即通过特异性抗体将细胞因子引导至肿瘤微环境等疾病局部,再由细胞因子发挥其作用(如激活或者抑制免疫细胞),如此一来,可以有效降低肿瘤外毒性,以此扩大细胞因子的治疗窗口,因而,近年来也有越来越多的“抗体偶联细胞因子”相继进入临床阶段。
品种
原研单位
许可单位
靶点
临床阶段
Nidlegy
Philogen SpA
印度太阳药业有限公司
TNFA;EDB-FN;IL-2
注册申请
L19-TNF;Fibromun
Philogen SpA
-
TNFA;EDB-FN
临床Ⅲ期
IBI-363
信达生物制药(苏州)有限公司
-
IL-2;PD-1
临床Ⅱ期
RO6874281;simlukafusp alfa
罗氏制药
-
AFAP1L2;FAP-alpha;IL-2
临床Ⅱ期
SAR-445877
赛诺菲
-
IL15;PD-1
临床Ⅱ期
OXS-3550
University of Minnesota
OXIS International Inc
IL15;CD16;CD33
临床Ⅱ期
PF-06687234
Philogen SpA
辉瑞公司
IL10;CD29;EDA-FN
临床Ⅱ期
IBB-0979
盛禾(中国)生物制药有限公司
-
IL10;CD276
临床Ⅱ期
SNG-2005
EMD Lexigen Research Center Corp;EMD Serono Inc
Alopexx Oncology LLC
CD20
临床Ⅱ期
APN-301
Apeiron Biologics GmbH;默克
-
IL-2
临床Ⅱ期
ANV-419
Anaveon AG;University of Zurich
-
IL-2
临床Ⅱ期
TAK-573
武田药品工业株式会社
-
IFN-alpha-2;CD38
临床Ⅱ期
Darleukin;L19-IL2
Philogen SpA
Maastricht University Medical Center
EDB-FN;IL-2
临床Ⅱ期
NHS-IL2-LT
默克
-
IL-2;IL2R
临床Ⅱ期
STAR-0602
Marengo Therapeutics
-
TCRBV
临床Ⅱ期
RG-7835
罗氏制药
-
CD25
临床Ⅱ期
IAE-0972
盛禾(中国)生物制药有限公司
-
IL10;EGFR
临床Ⅱ期
F16IL2
PhiloGene Inc
-
IL-2;Tenascin
临床Ⅱ期
M-9241
默克
National Cancer Institute
IL12R
临床Ⅱ期
PDS0301
PDS Biotechnology Corp
-
IL-12
临床Ⅱ期
IAP-0971
盛禾(中国)生物制药有限公司
-
IL15;PD-1
临床Ⅱ期
数据来源:药智数据
截至目前,全球已有数十款在研的抗体偶联细胞因子药物,其有效载荷主要集中在IL-2,IFN-γ,EPO等类型。其中由Philogen开发的Nidlegy是抗体偶联细胞因子领域中进度最靠前的管线,目前已向欧洲药品管理局(EMA)提交了上市申请,一旦获批,或将成为第一款上市的抗体偶联细胞因子产品。
而作为 Philogen 专有的生物制药产品,Nidlegy是专为治疗皮肤癌而设计。结构上由 L19IL2 和 L19TNF 组成,其中L19 抗体对纤连蛋白的额外结构域 B 具有特异性,其Ⅲ期PIVOTAL研究显示,治疗组复发或死亡风险降低了41%,中位RFS延长了一倍以上,且患者组实现病理学完全缓解(pCR)的比例为21%。
而国内领域,研究进度较靠前的则是信达生物的一款PD-1/IL-2(IBI363),其采取非对称二聚体设计,IL-2经过改造保留CD25(IL2Rɑ)活性以最大化疗效和高选择性,同时减少对Rβγ 结合以降低系统毒性。既可以阻断PD-1/PD-L1免疫抑制通路,又可以通过IL-15激活免疫细胞;同时,PD-L1抗体还能将IL-15靶向到PD-L1+的肿瘤微环境,选择性激活肿瘤浸润CD8+T细胞和NK细胞,降低IL-15全身性副作用。
综上可知,抗体偶联细胞因子的技术方向,因其强大的靶向肿瘤和延长细胞因子半衰期的能力,以及其对多个靶点的协同抗肿瘤作用,目前已经成为效应蛋白偶联物领域最具前景的疗法,成了创新biotech脱颖而出的重要资本。
不过,尽管表面上看抗体偶联细胞因子领域似乎前景广阔,但对于“药效蛋白偶联物”领域而言,仍是成功的个别例子,占据极小的部分,放眼整个药效蛋白偶联领域,仍有大量药效蛋白缺乏有效的偶联方式。
化学修饰+蛋白
药效蛋白偶联物的未来
就技术层面而言,如何想将任一蛋白进行修饰偶联,而不需要考虑药效蛋白的针对性与特殊性,是现阶段专家在研究中主要的思考方向。
目前来看,通过化学偶联修饰方式与药效蛋白相结合是比较切实可行的方法。比如PEG/mPEG修饰、氨甲酰化修饰、硫酸化修饰与磷酸化修饰。
PEG/mPEG偶联蛋白
所谓PEG,是一种被广泛应用于蛋白质和多肽等生物聚合物进行共价修饰的高分子材料;mPEG则是将PEG其中一端进行封端后的产物;而PEG/mPEG化修饰就是将其与药物共价结合,以改善药物的药代动力学、药效学和免疫学特性,从而增强其治疗效果的一种药物技术。
通常情况下,PEG/mPEG由于提高水溶性、减少酶水解、降低毒性和免疫原性、延长体内半衰期、改变组织分布以及增加药物分子的靶向位点浓度等特点,被主要考虑用作生物分子偶联的起始材料。
图片来源:西宝生物
而在众多与PEG偶联的生物大分子中,脂类、蛋白质、小分子药物和其他疏水性聚合物已被广泛研究,并被用来制造用于药物输送和成像的纳米载体,对于蛋白质而言,其没有对蛋白种类的显示,简单来讲就是局限于细胞因子、免疫细胞等种类,理论上可以与所有蛋白质进行PEG偶联。
在原理上,蛋白质的PEG修饰之所以有一系列优势,主要是由于蛋白质PEG修饰后,偶联物使原有蛋白质的分子量增大,空间结构发生改变,一方面可以是使其可以逃避肾小球滤过作用,在血液循环中停留更长的时间;另一方面修饰剂会使得蛋白质表面抗原决定簇掩盖起来,避开免疫系统识别;甚至修饰剂作用下,蛋白质药物还能不易被各种蛋白酶的攻击,降解速率明显降低。
图注:聚乙二醇修饰蛋白示意图
资料来源:键凯科技招股说明书
从蛋白质PEG修饰到mPEG修饰,如今在该领域范围内,已经有了许多蛋白质的聚乙二醇化修饰物作为药物取得了较好的结果,可行性上得到了充分验证。
1991年,第一种经聚乙二醇化修饰的蛋白质类药物PEG-腺苷脱氨酶被FDA批准上市,用于治疗一种严重的儿童免疫缺陷症;
2001年,用聚乙二醇修饰的干扰素(PEG-INTRON)经FDA批准上市,用于治疗慢性丙型肝炎;
2010年,通过赖氨酸偶联进行聚乙二醇化的普瑞凯希Krystexxa(pegloticase)被FDA批准用于治疗痛风,实现每月一针的注射频率。
2024年,J.P. Morgan大会上,由 Ascendis Pharma 原研开发的一款在研 PTH 激素原药(TransCon PTH )亮相,由母药 PTH(1-34) 和支链甲氧基聚乙二醇 (mPEG) 载体通过专有连接剂瞬时结合而成,正在开发用于治疗成人甲状旁腺功能减退症,可以实现24 小时的正常生理范围内提供稳定的 PTH 水平。
并且,作为化学偶联修饰中最主要的存在,PEG/mPEG修饰还成功为化学修饰蛋白建立了良好的开端,也为后续企业更多在研化学修饰方法,提供了良好的模板,比如氨甲酰化、硫酸化、磷酸化等。
小结
总结来看,由于药效蛋白本身诸多优势,目前通过偶联方式将药效蛋白进行系列改装已成为了现实,最切实有用的方法可以参考“抗体+蛋白毒素、抗体+细胞因子”。
但是,无论是细胞因子、蛋白毒素,还是免疫细胞,其都只能代表药效蛋白中较小部分,蛋白偶联仍存在明显的局限性与针对性,好在以PEG/mPEG为首的化学偶联修饰技术之下,研究者们似乎在寻找针对任何蛋白偶联方法上已经有了些许突破。
未来,随着更多如PEG/mPEG化、氨甲酰化、硫酸化、磷酸化等化学偶联修饰方法的发现,整个药效蛋白市场或许也将发生巨大重构,我们拭目以待。
来源 | 博药(药智网获取授权转载)
撰稿 | 头孢
责任编辑 | 八角
声明:本文系药智网转载内容,图片、文字版权归原作者所有,转载目的在于传递更多信息,并不代表本平台观点。如涉及作品内容、版权和其它问题,请在本平台留言,我们将在第一时间删除。
商务合作 | 王存星 19922864877(同微信)
阅读原文,是受欢迎的文章哦
抗体药物偶联物多肽偶联药物蛋白降解靶向嵌合体
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
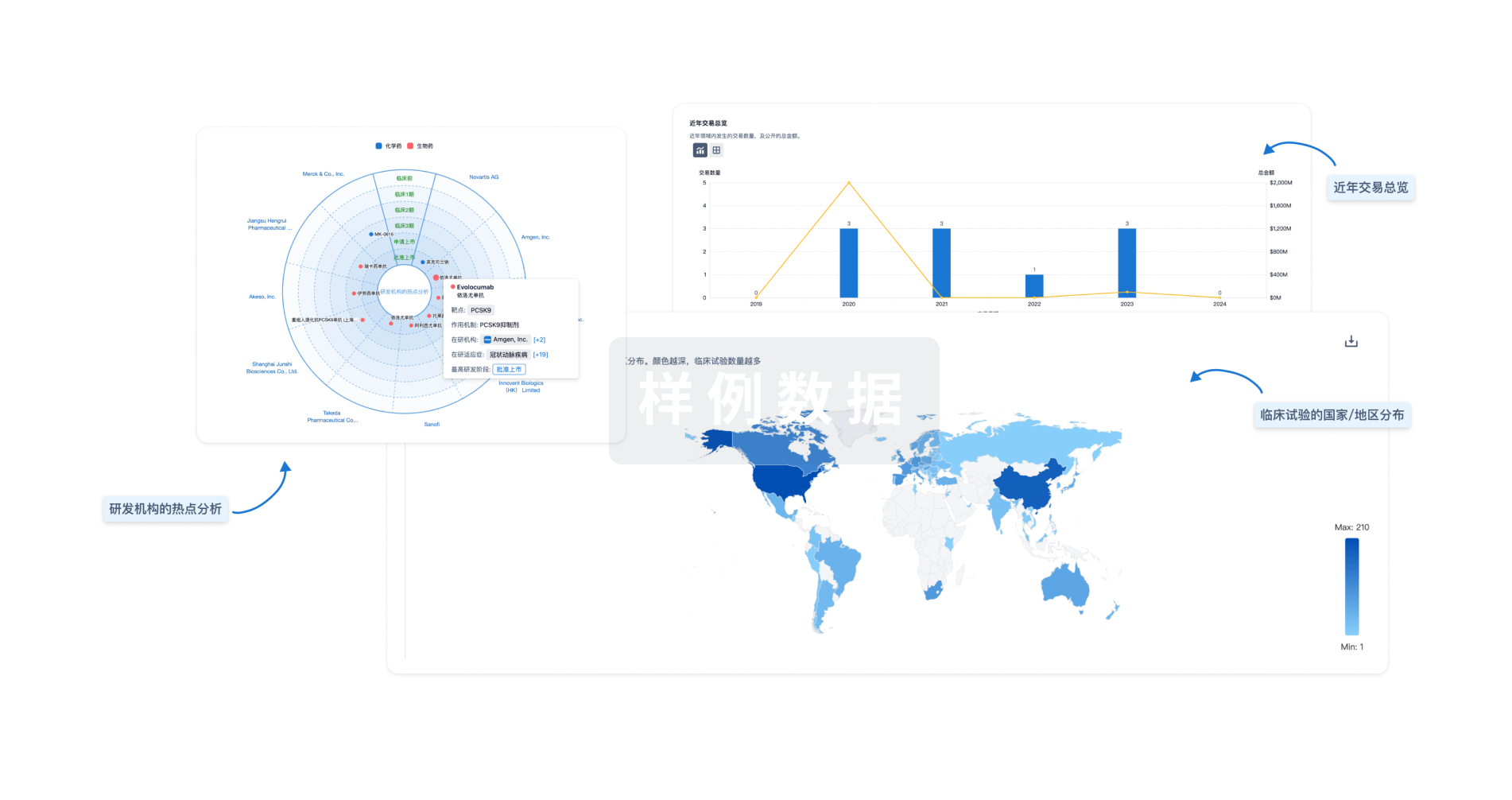
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
